Abstract
This study grouped treatment-seeking individuals (n=1825) by common patterns of 12-step attendance using 5 waves of data (75% interviewed year-9) to isolate unique characteristics and use-related outcomes distinguishing each class profile. The high class reported the highest attendance and abstention. The descending class reported high baseline alcohol severity, long treatment episodes, and high initial attendance and abstinence; but by year-5 their attendance and abstinence dropped. The early-drop class, which started with high attendance and abstinence but with low problem severity, reported no attendance after year 1. The rising class, with fairly high alcohol and psychiatric severity throughout, reported initially low attendance, followed by increasing attendance paralleling their abstention. Last, the low and no classes, which reported low problem-severity and very low/no attendance, had the lowest abstention. Female gender and high alcohol severity predicted attendance all years. Consistent with a sustained benefit for 12-step exposure, abstinence patterns aligned much like attendance profiles.
Keywords: Alcoholics Anonymous, 12-step groups, latent class growth analysis, trajectories analysis, alcohol and drug outcomes
1. Introduction
Alcoholics Anonymous (AA) and similar 12-step groups like Narcotics Anonymous (NA) and Cocaine Anonymous (CA) are a widely-used source of help in the United States for individuals with substance use problems. Though treatment philosophies vary across formal treatment programs (e.g. cognitive behavioral, motivational enhancement, relapse prevention, twelve step facilitation, eclectic), most providers routinely recommend 12-step group attendance to their clients during and following treatment (Humphreys, 2003; McElrath, 1997; Slaymaker & Sheehan, 2008). This use of 12-step groups as an adjunct to specialized treatment and as aftercare has longstanding research support. For example, a 1993 meta-analysis of 107 studies found better initial outcomes occurred when formal treatment was combined with AA attendance (Emrick, Tonigan, Montgomery, & Little, 1993). Likewise, a more current longitudinal study of initially untreated individuals followed for 16 years obtained similar results (Rudolf H. Moos & Moos, 2006). Although there is less empirical evidence, treatment-seeking individuals with drug use disorders also appear to benefit from greater 12-step attendance (Crape, Latkin, Laris, & Knowlton, 2002; D. M. Donovan & Wells, 2007; Fiorentine, 1999; Gossop, Stewart, & Marsden, 2008; Humphreys, 2004; Kissin, McLeod, & McKay, 2003; Witbrodt & Kaskutas, 2005). This paper adds to the literature by using latent class growth analysis (LCGA) techniques to examine latent classes of 12-step attendance trajectories, and associations between the trajectories and substance use and related outcomes among adults with substance use disorders who were treated in a private, integrated health caredelivery systemsetting and were followed for nearly a decade. We know of only one other lo ngitudinal study of private managed care clients’ (n=227) use of various mutual-aid groups (Kelly, Stout, Zywiak, & Schneider, 2006). This 3-year study used lagged-panel hierarchical linear modeling andd id not focus specifically on distinct groups of long-term 12-step attendance trajectories among these individuals.
While empirical evidence showing the association between 12-step attendance and abstention has increased, longitudinal research conducted across several years is still limited to just a few studies that have looked at drinking outcomes as related to attendance (Kaskutas et al., 2005; Kaskutas, Bond, & Ammon Avalos, 2009; McKellar, Ilgen, Moos, & Moos, 2008; McKellar, Stewart, & Humphreys, 2003; Rudolf H. Moos & Moos, 2005; Rudolf H. Moos & Moos, 2006; Timko, Moos, Finney, & Connell, 2002). Building on the work by Moos and colleagues, which found that individuals with extended AA participation had better 16-year alcohol outcomes than those with a shorter duration of attendance, another longitudinal study found that both the duration and the intensity of AA attendance affected abstinence rates (Kaskutas, Bond, et al., 2009). Though not scientific research (only active members participate), AA membership surveys also suggest that long-term engagement results in long-term abstention. The 2007 AA membership survey shows that almost half the current members reported being sober for 5 or more years and 33% for more than 10 years (Alcoholics Anonymous, 2007). Comparable NA membership data on years of being drug free are very similar (Narcotics Anonymous World Services, 2010). See (Kaskutas, Ye, Greenfield, Witbrodt, & Bond, 2008; Laudet, 2008) for a related reviews.
Still, the direct relationship between 12-step attendance and abstinence remains uncertain in part because randomized clinical trials that direct and restrict attendance are difficult to conduct with such a freely available source of support as AA (and NA/CA). This relationship becomes even more blurred when attendance is studied over longer follow-up periods and as people transition in and out of both formal treatment programs and 12-step groups. In addition, only scant research has focused on outcomes other than actual alcohol and drug use (e.g., abstention status, percent days abstinent, drinks-per-drinking-day (Tonigan, 2008)).
This paper uses a LCGA approach to identify distinct patterns of 12-step attendance over time (trajectories of latent classes), while simultaneously testing for other influences associated with these attendance patterns (Nagin & Tremblay, 2001). Once these trajectories are established, we then study alcohol- and drug- related outcomes associated with each attendance class. In LCGA a single outcome variable measured at multiple time points, in our case the number of meetings attended at each follow-up, is used to identify clusters of individuals (latent classes) who share common patterns of over time (Bengt Muthén, 2001). The LCGA model assumes that individuals belong to one of ‘k’ latent classes (determined in the analytic process); and within a given class, all individuals have the same average trajectory over time, and this trajectory varies across the classes. This approach has the advantage over more conventional growth modeling approaches that assume individuals come from a single population, that a single growth trajectory can approximate everyone in the population, and that covariates that affect the growth factors influence everyone in the same way (Jung & Wickrama, 2008). A rationale for approaching longitudinal data in this manner is provided by Nagin who uses an analogy of clinical diagnostic classifications: we know that not everyone with the same diagnosis is identical; however, we also recognize that such groupings are meaningful and helpful in both clinical practice and research (Nagin, 1999). A number of substance use studies have used LCGA techniques, with more looking at drinking and drug use trajectories among younger persons (Anderson, Ramo, Cummins, & Brown, 2010; Chung, Maisto, Cornelius, & Martin, 2004; Goudriaan, Grekin, & Sher, 2007; Greenbaum, Del Boca, Darkes, Wang, & Goldman, 2005; Jackson, Sher, Gotham, & Wood, 2001; Oxford et al., 2003) than adults (Chassin, Fora, & King, 2004; Delucchi, Matzger, & Weisner, 2004; Genberg et al., 2011; Grella & Lovinger, in press; Hser, Huang, Brecht, Li, & Evans, 2008). Only a few published papers have used these analytical techniques to model classes of AA attendance over time (Kaskutas, et al., 2005; Kaskutas, Bond, et al., 2009; Witbrodt & Delucchi, in press).
We build on work by Kaskutas (2005 and 2009) that respectively described AA (but not NA or CA) attendance trajectories across 5- and 7- years among a heterogeneous sample (n=586) of alcohol-dependent individuals (some were also drug dependent) recruited from representative public and private treatment programs and the general population within a single California county. In both the 5- and 7-year analyses, four attendance patterns were delineated: high attendance over time, descending attendance over time, medium but steady attendance over time, and very low attendance at all follow-ups. While a very modest decline in attendance was observed in the high attendance class at the 5-year follow-up, this became much more apparent by the next follow-up 2 years later. At all but that last follow-up, past 30-day alcohol abstinence rates were highest for the high attendance class; but by year 7, the abstinence rate for the high attendance class was similar to that of the descending class. Providers will be interested in knowing whether this decline in attendance will continue, whether abstinence will correspondingly decrease, and whether other attendance classes will emerge with expanded time.
We address these questions here, but we extend the follow-up period to 9 years, we triple the overall sample size (thus constraints on the number of classes are loosened), we include individuals who are also drug dependent (but not alcohol dependent), and we consider NA and CA, as well as AA. Additionally, we adjust within our LCGA for factors known to be associated with 12-step attendance. The sample for the current study also differs in that it only includes individuals seeking outpatient treatment within a private, integrated health care delivery system. Outpatient treatment represents the predominant mode of treatment in the U.S. (about 80%). Though managed health care delivery systems are major treatment providers serving both private and public sector clients (Substance Abuse and Mental Health Services Administration & Office of Applied Studies, 2008), there is almost no long term research of 12-step involvement that has focused on such private populations (Chi, Kaskutas, Sterling, Campbell, & Weisner, 2009). Such health plans, which are similar in organizational structure to the setting studied here, have increased in number and provide care for a significant portion of the insured U.S. population (HMO Research Network, 2009). Examining the relationship of 12-sep attendance over time with alcohol and drug use outcomes is important for understanding the relevance of 12-step in a more stably insured sample with high access to both behavioral and other medical services.
This paper uses a conceptual approach that draws from the longitudinal treatment outcome literature, including research on treatment careers and the natural course of treated populations (Hser, Anglin, Grella, Longshore, & Prendergast, 1997; Joe, Chastain, & Simpson, 1990; Simpson, 1990; Vaillant, 1996a), as well, as the medical utilization literature focused on predisposing, enabling, and severity factors that serve to either facilitate or impede help seeking (Aday et al., 1999; Andersen & Newman, 1973; Vaillant, 1996b). Under this conceptual help-seeking model, predisposing factors are characteristics that exist prior to problem onsetand descri be the propensity to seek out services; enabling factors are influences that distinguish between formal and informal resources available that influence doing something about one’s problem; and need factors are measures of imperative problem severity. We specifically examine demographic (predisposing), formal treatment utilization (enabling), and use-related problem severity (need) variables empirically identified as predictors of 12-step attendance. For example, a 1996 meta-analysis that found more prior external help-seeking for alcohol problems and greater problem severity were the primary predictors of AA attendance (Tonigan, Toscova, & Miller, 1996). Subsequent studies with treatment samples have also found greater substance use severity to be a consistent predictor of 12-step attendance (Bogenschutz, 2008; Brown, O’Grady, Farrell, Flechner, & Nurco, 2001; Orwat et al., 2011; Sheehan et al., 1998; Tucker, Vuchinich, & Rippens, 2004; Weiss et al., 2000; Witbrodt, Bond, & Delucchi, 2009). Demographic characteristics associated with 12-step attendance have been less consistent predictors, in part because measures of 12-step participation have been inconsistent across studies. Mixed results have been found for age (Brown, et al., 2001; Lemke & Moos, 2003; Satre, Mertens, Areán, & Weisner, 2004; Sussman, 2010) and gender (Del Boca & Mattson, 2001; Kelly, et al., 2006; Satre, et al., 2004; Timko, et al., 2002; Weisner, Ray, Mertens, Satre, & Moore, 2003; Witbrodt & Delucchi, in press), as well as variables related to socioeconomic status (Heinz, Wu, Witkiewitz, Epstein, & Preston, 2009; Humphreys, Moos, & Finney, 1995; Kaskutas, et al., 2008; Timko, Billow, & DeBenedetti, 2006; Timko, Finney, Moos, & Steinbaum, 1993).
2. Material and methods
2.1 Study design and study sample
Because more potential classes can be delineated in LCGA when larger samples sizes are available, we combined participants from two randomized controlled trials that were conducted at the same Kaiser Permanente Chemical Dependency Recovery Program (CDRP) in Sacramento, California and that used the same study design, recruitment methods, and treatment programs. Other papers have reported on these combined samples (Satre, Blow, Chi, & Weisner, 2007; Weisner, Parthasarathy, Moore, & Mertens, 2010). Kaiser Permanente is a private, integrated health care delivery system, serving 40% of the insured population in the Sacramento area. The health plan provides chemical dependency treatment services internally, rather than referring to contracted programs. This CDRP site was chosen for the two studies because it served a heterogeneous client population. Participants (n=1951) were recruited between 1994 and 1998 (Weisner et al., 2000; Weisner, Mertens, Parthsarathy, & Moore, 2001).
2.2 Treatment program
The CDRP provided traditional outpatient and day hospital programs. Both programs were abstinence-based and offered the same content, including supportive group therapy, education, relapse prevention, and family therapy, with individual counseling available as needed. The day treatment provided four times the intensity of the outpatient program during the first 3 weeks. Both programs lasted 8 weeks, with 10 months of aftercare available (Weisner, et al., 2001). All patients (in both programs and both studies) were required to attend two 12-step meetings in the community each week and they were also required to attend an onsite meeting. “Buddies” were available to those who were uncomfortable going to a meeting alone. The 12-step philosophy was incorporated into some group sessions.
2.3 Recruitment and follow-up
All patients ages 18 or older with substance-use disorders who requested treatment and met standard treatment admission criteria were eligible for the study. Patients deemed medically ready and not in need of detoxification by medical intake evaluation staff were introduced to the study and provided an informed consent by research staff independent of the CDRP. Those who refused randomization or were unable to be randomized but agreed to participate in other aspects of the studies were also recruited and received “treatment assignment as usual.” Research staff conducted follow-up interviews by telephone at 1, 5, 7, and 9 years, with response rates of 86%, 81%, 84%, and 75%, respectively. Refer to (Weisner, et al., 2000; Weisner, et al., 2001) for further details. Annual Institutional Review Board approval was obtained from the Kaiser Research Foundation Institute and the University of California, San Francisco.
2.4 Measures
2.4.1 Formal treatment, demographic characteristics, and problem severity (covariates)
The baseline interview provided demographic information used to describe the sample. The Diagnostic Interview Schedule for Psychoactive Substance Dependence (American Psychiatric Association, 1994) was used to assess baseline substance use diagnosis (categorized here as alcohol dependence, drug dependence, both alcohol and drug dependence or abuse). Data extracted from the health plan’s automated database were used to obtain information on treatment utilization, age and gender. Duration in the index treatment was measured by the number of days between intake and the last treatment visit. The number of treatment readmissions between follow-up interviews was dichotomized (yes/no) at analysis due to negatively skewed distributions (mostly 0 and 1 values). Addiction Severity Indices (ASI) for the alcohol, drug, and psychiatric domains were collected at all five interviews. The ASI assesses past 30-day problem severity, with values ranging from 0 to 1 and higher scores indicating higher levels of severity (McLellan et al., 1992).
2.4.2 12-step attendance (LCGA outcome)
At the 1-, 5-, 7- and 9- year interviews, individuals were asked the number of 12-step meetings they attended in the prior 12 months (prior 6 months at 1-year post-treatment interview). At analysis, these attendance data were capped at 365 (180) days to adjust for a few outliers (<10 cases at any interview). Because these data were negatively skewed and kurtotic, we transformed the attendance variables at each interview using a shifted base-10 log (plus one) to achieve more normal distributions (Box & Cox, 1964; Carroll & Ruppert, 1988).
2.4.3 Auxiliary outcomes
After constructing 12-step attendance classes, we tested how our identified classes compared on four substance-related outcome measures over time. Our primary measure was past 30-day abstinence from alcohol and other drugs. Abstention is consistent with the 12-step programs’ abstinence-based philosophy and it is the intended goal of Kaiser’s CDRP. Given the chronic and relapsing nature of substance dependence (McLellan, Lewis, O’Brien, & Kleber, 2000; Weisner, Delucchi, Matzger, & Schmidt, 2003), we also tested how the attendance classes compared on ASI severity (the 3 domains described above) at all follow-ups.
2.4.4 Validity of self-report of alcohol and drug use
Random urine screens for detection of alcohol and drug use (alcohol, barbiturates, benzodiazepines, cocaine, cannabis/THC, opiates, phencyclidine, and amphetamines) and breath analysis for alcohol use were conducted at all follow-ups. These allowed us to validate self-report data. Comparisons in a random subsample of 304 subjects at 5-years yielded rates of reporting no use but testing positive for a substance of 3.6% for alcohol and between 0.7% for opiates and 4.9% for marijuana (Weisner, Ray, et al., 2003).
2.5 Statistical analysis
To begin the LCGA, we first specified an unconditional single-class growth model for logged 12-step attendance as a starting point to see how the data looked overall in terms of fit and shape. We then built models with successively more classes to determine a final model that best described the data. A zero-inflated censored model was used. The zero-inflation step was employed to deal with the large number of zero values for attendance. Here, two growth models are estimated: first, one for attendance for those individuals who are able to assume values of zero and above, and then one for the zero inflation part of attendance, that is, the probability of only being able to assume the value zero. Bayesian information criteria (lower values are better) (Nylund, Muthén, & Asparouhov, 2004), posterior probabilities (the likelihood of correct class assignment), and entropy (a measure of classification uncertainly) (L. K. Muthén & Muthén, 2008b) statistics were used to select the final model. Analysis was conducted using Mplus, Version 5.1 (L. K. Muthén & Muthén, 2007).
Next, selected covariates (see 2.4.1) were screened individually to more precisely specify the final model that included only the combination of covariates that exerted a strong influence on class shapes and membership (Bengt Muthén, 2004). Mplus software uses a full-information maximum likelihood estimation under the assumption that data are missing at random (Little & Rubin, 2002; Bengt Muthén & Shedden, 1999). In theory this method provides the same result as multiple imputation and it means that no bias is introduced by using only cases with data at every interview. By default Mplus excluded cases (n=126) with only baseline data (L. K. Muthén & Muthén, 2008a). Among the retained cases, 77% were interviewed at three or more of the four follow-ups. Lastly, the LCGA class membership data were transferred to an external file and merged with our time-varying auxiliary outcome variables, along with those baseline covariates retained in the final LCGA model. Generalized estimating equations (GEE) with an exchangeable correlation structures were used to test for associations between class membership and the four outcomes over time. GEE models (4 panels), controlling for baseline influences, were estimated in Stata, Version 10 (Stata Corp, 2007).
3. Results
3.1 Participants
Males and females (37%) included in these analyses (n=1825) were mostly White (74%), less than half were married/cohabitating (45%), over half were employed full-or part-time (60%), the majority had high school or higher educations (86%), just over half were alcohol dependent (59%), and about half (48%) were drug dependent (Table 1, “included cases” column). Of those with a drug diagnosis most were dependent on stimulants (56%), marijuana (33%), cocaine (18%), or painkillers (9%). The index treatment duration lasted about 2 months on average. Compared with included cases, participants excluded from the LCGA analyses (n=126) were less likely to be female (29% vs. 37%), slightly older (40 vs. 37 years) and more likely be both alcohol and drug dependent (23% vs. 18%), and their treatment stays were much shorter on average (23 days vs. 65 days).
Table 1.
Baseline characteristics for the total sample and included and excluded cases in the LCGA model.
| (n) | All cases (1951) | Included cases (1825) | Excluded cases (126) |
|---|---|---|---|
| Women (%) | 36 | 37 | 29 c |
| Age (mean) | 37 | 37 | 40 c |
| Age categories (%) | |||
| 18–39 | 60 | 60 | 55 |
| 40–54 | 34 | 34 | 37 |
| 55+ | 6 | 6 | 9 |
| Ethnicity (%) | |||
| White | 74 | 74 | 75 |
| African American | 11 | 11 | 12 |
| Hispanic | 9 | 9 | 9 |
| Other | 5 | 5 | 5 |
| Married/partnered (%) | 45 | 45 | 51 |
| Employed, full/part (%) | 59 | 60 | 54 |
| Income ≥ 40,000 (%) | 39 | 39 | 32 |
| Education (%) | |||
| < high school | 14 | 14 | 21 |
| high school | 48 | 48 | 52 |
| > high school | 37 | 38 | 27 |
| Diagnosis (%) | |||
| Alcohol only dependent | 40 | 41 | 36 |
| Drug only dependent | 29 | 30 | 23 |
| Alc. & drug dependent | 19 | 18 | 23 b |
| Substance abuse | 12 | 12 | 18 |
| ASI alcohol (mean) (se) | .417 (.007) | .417 (.007) | .428 (.027) |
| ASI drug (mean) (se) | .125 (.119) | .125 (.120) | .116 (.010) |
| ASI psychiatric (mean) (se) | .404 (.006) | .404 (.006) | .403 (.022) |
| Treatment days (mean) (se) | 62 (2.2) | 65 (2.3) | 23 a(3.7) |
p<.001,
p<.01,
p<.05
3.2 Building 12-step attendance trajectories
In comparing model fit among four-class (BIC= 15040), five-class (BIC=14973) and six-class (BIC=14907) solutions in unconditional LCGA models (no covariates included), a six-class model was selected. The Vuong-Lo-Mendell-Rubin (VLMR) likelihood test (Lo, Mendell, & Rubin, 2001) for a five-versus six- class solution was significant at p<.001, indicating the six-class solution was a better fit for the data. Table 2 displays the mean posterior probabilities for most likely membership assignment adjusted for the retained covariates. These range between .74 and .83 percent.
Table 2.
Mean posterior probability of latent profile group membership (row) by latent profile group assigned to (column)
| High (457) | Descending (220) | Rising (93) | Early-drop (291) | Low (154) | No (608) | |
|---|---|---|---|---|---|---|
| High | .81 | .08 | .07 | .02 | .01 | <.01 |
| Descending | .11 | .81 | .02 | .01 | .03 | <.01 |
| Rising | .09 | .02 | .82 | <.01 | .06 | 0 |
| Early-drop | .08 | .07 | .01 | .77 | .04 | .02 |
| Late-drop | .03 | .07 | .10 | .04 | .74 | 0 |
| No | .03 | .02 | .01 | .09 | .02 | .83 |
Note: 2 cases were dropped in the final LCGA model because of missing data on baseline help-seeking covariates.
3.3 Shapes of the 12-step attendance classes
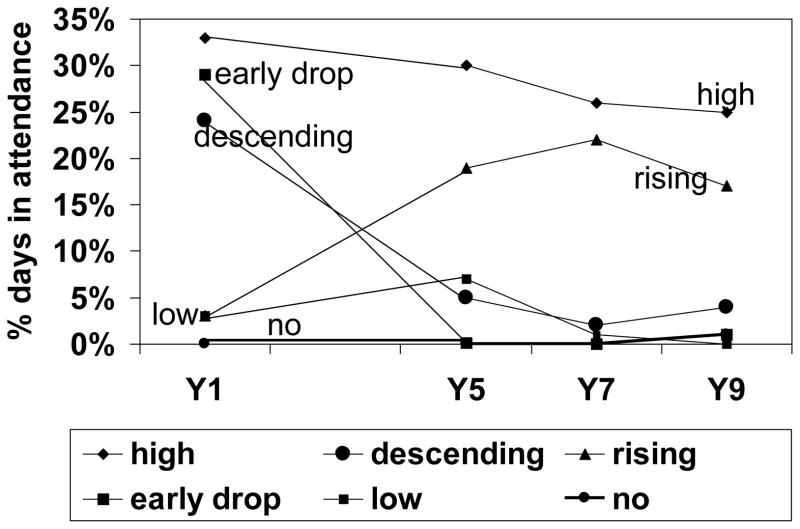
Figure 1 plots actual 12-step attendance by class membership. We chose to express attendance as the average percent days in attendance (APDA) rather than the average number of days in attendance to standardize our time periods, that is, because 1-year follow-up data asked about prior 6-month post-treatment attendance and other follow-ups asked about prior 12-month attendance. For descriptive purposes and based on attendance patterns, we labeled the six attendance trajectories as high (n=457; APDA varying 25-33% over time), descending (n=220; APDA varying 2–24%), rising (n=93; APDA varying 3–22%), early-drop (n=291; APDA varying 0–29%), low (n=154; APDA varying 0–7%) and no (n=608) attendance. Based on the predicted posterior probability assignments, individuals assigned to the no 12-step attendance class could have some level of attendance (because they had a 17% chance of being assigned to another class). Actual attendance data, however, showed that all these individuals reported no attendance at the 1-, 5-, and 7- year follow-ups; a few individuals reported some attendance at year 9 (mean = .03 and range 1 to 4 meetings).
Figure 1.
12-Step Meeting Attendance
3.4 LCGA parameters
Table 3 displays the parameter estimates, their standard errors, and tests of significance for the final LCGA model that included covariates exerting influence on the growth factors. Substance use diagnosis, baseline ASI drug severity and ASI psychiatric severity, ethnicity, education, marital status, and treatment readmission variables were dropped because they exerted little influence on the final trajectories. Significant covariates retained for the final model were gender, age, baseline ASI alcohol severity and days in the index treatment episode. For each class shown in Table 3, the linear component (i.e., slope) reflects the estimated significant change up or down over time in the latent trajectory of attendance and the quadratic component reflects whether the change significantly departs from a straight line. Except for the no 12-step attendance class where the slope and quadratic terms were not significant (consistent with attendance being flat over time for that trajectory), all parameters for the other five classes were significant at p<.05, indicating that average attendance for these classes over time was not steady but instead changed at some point. Note that the signs for the slope and quadratic terms are reversed for the rising and low classes compared to others (i.e., positive slopes and negative quadratic terms), reflecting the strong linear change and an initial increase followed by a downward turn.
Table 3.
Estimates, standard errors and tests of significance by class membership
| Class & parameter | Estimate | SE | p-value |
|---|---|---|---|
| High | |||
| Intercept | 4.461 | 0.157 | a |
| Slope | −0.281 | 0.127 | c |
| Quadratic | 0.043 | 0.017 | c |
| Descending | |||
| Intercept | 4.137 | 0.177 | a |
| Slope | −0.933 | 0.194 | a |
| Quadratic | 0.096 | 0.026 | b |
| Rising | |||
| Intercept | 2.029 | 0.192 | a |
| Slope | 0.635 | 0.166 | a |
| Quadratic | −0.044 | 0.021 | c |
| Early-drop | |||
| Intercept | 4.038 | 0.181 | a |
| Slope | −2.288 | 0.229 | a |
| Quadratic | .199 | 0.031 | a |
| Low | |||
| Intercept | 2.155 | 0.183 | a |
| Slope | 1.197 | 0.295 | a |
| Quadratic | −0.274 | 0.050 | a |
| No | |||
| Intercept | −11.027 | 0.343 | a |
| Slope | −1.694 | 0.000 | |
| Quadratic | .357 | 0.000 | |
| Intercept inflation | 0.000 | 0.000 | |
| Slope inflation | 0.213 | 0.049 | a |
| Quadratic inflation | −0.022 | 0.007 | b |
p<.001,
p<.01,
p<.05
3.5 Factors associated with class membership
Regressing class membership on the four retained covariates (gender, age, baseline ASI alcohol problem severity, and index treatment days) resulted in 15 pair-wise comparisons for each covariate in the Mplus model-building output. For simplicity, we display the actual distributions of these four predictor variables (percents and means) within each class rather than showing the beta coefficients produced in Mplus (Table 4). The significant pair-wise differences underlying the influence of these variables on class membership (i.e., Mplus output) are provided in the last column. We also display data for those covariates not retained in the final LCGA model.
Table 4.
Distribution of significant baseline (multivariate) predictors of class membership retained in the final LCG model, as well as those tested but not retained due to lack of significance.
| Retained | aHigh | bDescend | cRising | dEarly-drop | eLow | fNo | p-value < .05 |
|---|---|---|---|---|---|---|---|
| Women (%) | 44 | 49 | 48 | 25 | 38 | 31 | abc>df |
| Age (se) | 36 (.45) | 40 (.74) | 34 (.87) | 41 (.60) | 37 (.90) | 36 (.45) | bd>acf |
| ASI alc (mean) (se) | .47 (.02) | .48 (.02) | .52 (.03) | .37 (.02) | .34 (.03) | .38 (.01) | ac>def |
| Treat. Days (mean) (se) | 82 (5.2) | 81 (7.4) | 45 (5.4) | 134 (7.7) | 49 (5.9) | 19 (1.4) |
d>abcef f<abcde, ab>cef |
| Not retained | |||||||
| Ethnicity (%) | |||||||
| White | 78 | 76 | 69 | 72 | 76 | 72 | |
| African American | 9 | 10 | 12 | 15 | 11 | 11 | |
| Hispanic | 8 | 11 | 16 | 8 | 8 | 10 | |
| Other ethnicity | 5 | 3 | 3 | 5 | 5 | 6 | |
| Education (%) | |||||||
| < high school | 12 | 16 | 22 | 10 | 13 | 15 | |
| high school | 45 | 42 | 40 | 46 | 55 | 53 | |
| > high school | 43 | 42 | 38 | 44 | 33 | 32 | |
| Married/partner (%) | 45 | 45 | 42 | 48 | 42 | 43 | |
| Diagnosis (%) | |||||||
| Alc. depend. | 47 | 46 | 39 | 38 | 31 | 38 | |
| Drug depend. | 27 | 25 | 26 | 28 | 40 | 32 | |
| Alc/drug depend. | 19 | 21 | 28 | 16 | 14 | 18 | |
| Subst. abuse | 8 | 7 | 8 | 18 | 15 | 13 | |
| ASI drug (mean) (se) | .13 (.01) | .13 (.01) | .14 (.01) | .11 (.01) | .14 (.01) | .12 (.01) | |
| ASI psych (mean) (se) | .43 (.01) | .43 (.02) | .47 (.03) | .35 (.02) | .40 (.02) | .39 (.01) | |
| Readmission (%) | |||||||
| Years 1–5 | 52 | 48 | 43 | 44 | 40 | 33 | |
| Years 6–7 | 7 | 4 | 8 | 1 | 1 | 1 | |
| Years 8–9 | 7 | 3 | 5 | 1 | 1 | 1 | |
‘a, b, c, d, e’ denotes class membership (e.g., High) and represents significant pair-wise comparisons produced in the Mplus categorical latent variable (class) regression analyses.
As displayed in Table 4, more women were in the three classes that attended meetings at all follow-ups (high, descending, and rising classes; 44%, 49% & 48% respectively) than those who dropped out before year 9 (early-drop & no; 25% & 31%). Individuals in the descending and early-drop classes were older on average (40 & 41 years respectively) than those in the high, rising, and no 12-step attendance classes (36, 34 & 36 years respectively). Those in the high and rising classes reported greater baseline ASI alcohol severity on average (.47 & .52) than those in the three classes that did not stay engaged over the full 9 years (early-drop, low& no classes; ≤ .38). Individuals in the early-drop class had longer average treatment episodes (134 days) than all other classes, and individuals in the no 12-step attendance class had shorter treatment episodes (19 days) than all other classes.
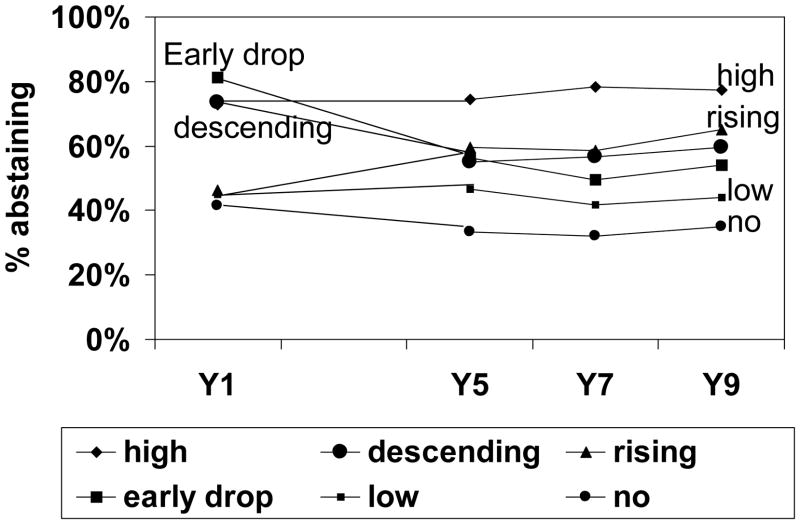
3.6 Abstinence patterns over 9 years
Figure 2 displays the actual (unadjusted) past 30-day alcohol and drug abstinence rates from simple cross tabulations (class membership by abstinence at each follow-up). About three-fourths of the individuals in the high attendance class reported past 30-day abstinence at all follow-ups (ranging between 73%–78%). Two other classes that also started high on attendance at year 1, the descending and early-drop classes (from Figure 1), looked similar in years 5, 7, and 9 in terms of abstinence rates (between 55% & 59% and 50% & 56% respectively). Rates for individuals in the rising class were lowest in year 1 (46%) and increased in later years (from 60% at year 5 to 65% at year 9). Rates for the low class fluctuated between 42% and 47% at all follow-ups. Despite their lack of 12-step attendance (Figure 1), the no attendance class had abstinence rates of 42% at year 1 and lower but stable rates at remaining follow-ups (between 32% & 35%).
Figure 2.
Alcohol and Drug Abstinent, past 30 days
GEE longitudinal models (adjusted) predicting abstinence as a function of class membership (results not shown) supported Figure 2. Individuals in the high attendance class had significantly (p-values <.003) better abstinence outcomes over time than those in all other classes, and those in the no attendance class had lower abstinence rates than individuals in all other classes. We applied a Bonferroni correction (p = .05/15 = .003)to correct for the multiple pair -wise comparisons in this and other GEE analyses (i.e., ASI severity outcomes).
3.7 ASI alcohol, drug, and psychiatric severity over 9 years
The GEE analysis indicated that individuals in the high attendance class had significantly (p<.003) lower ASI alcohol severity over time than those in the rising class. Table 5 displays actual (unadjusted) mean scores of the three ASI severity variables by class membership. There were no significant (p<.003) differences in ASI drug scores over time between the classes. Regarding psychiatric severity over time, individuals in the early-drop and no attendance classes had lower ASI psychiatric scores than those in the high and rising classes.
Table 5.
Distribution of actual ASI severity scores by AA attendance class at each interview
| Baseline | Year 1 | Year 5 | Year 7 | Year 9 | p ≤ .003 | |
|---|---|---|---|---|---|---|
| ASI alcohol | ||||||
| a High | .465 | .109 | .073 | .055 | .049 | |
| b Descending | .477 | .086 | .087 | .086 | .079 | |
| c Rising | .516 | .187 | .112 | .086 | .097 | c>a |
| d Early-drop | .374 | .054 | .062 | .079 | .058 | |
| e Low | .339 | .105 | .090 | .084 | .090 | |
| f No | .384 | .091 | .093 | .092 | .093 | |
| ASI drug | ||||||
| a High | .127 | .019 | .016 | .019 | .027 | |
| b Descending | .128 | .023 | .015 | .031 | .023 | |
| c Rising | .135 | .031 | .017 | .027 | .031 | |
| d Early-drop | .114 | .019 | .012 | .022 | .023 | |
| e Low | .137 | .029 | .029 | .036 | .030 | |
| f No | .124 | .017 | .017 | .020 | .026 | |
| ASI psychiatric | ||||||
| a High | .433 | .180 | .188 | .193 | .182 | a>d,f |
| b Descending | .427 | .153 | .166 | .188 | .171 | b>d,f |
| c Rising | .467 | .158 | .255 | .255 | .263 | |
| d Early-drop | .353 | .111 | .134 | .132 | .130 | |
| e Low | .405 | .147 | .188 | .176 | .184 | |
| f No | .389 | .104 | .148 | .167 | .145 | |
‘a, b, c, d, e’ denotes class membership (e.g., a High) and represents significant pairwise comparisons between attendance classes in longitudinal GEE models.
3.8 Post-hoc analyses
To understand better the outcomes in the classes with lower attendance rates and to consider if their severity levels may not have “required” abstinence, we examined the proportion who were “non-problem” users at each follow-up. Non-problem use was defined as: 1) used alcohol, but had no days of drinking five or more drinks in a day, and drank only four times per month or less in the past year; or used marijuana, but not more than once per month in the past year; 2) had no other drug use in the prior year; 3) had no problems with friends or family, violent behavior, or suicidal ideations in the prior month; and 4) had no arrests, jail/prison, electronic home surveillance, or visitations with a probation or parole in the prior year (Mertens, Flisher, Satre, & Weisner, 2008). This definition is consistent with other “non-problem use” and “remission” definitions in the literature (P. Ouimette, Moos, & Finney, 2003; P. C. Ouimette, Kimerling, Shaw, & Moos, 2000)) Among those in the early drop class, 11%, 14%, and 12% were non-problem users at the 5, 7, and 9 year follow-ups respectively; in the no class 13%, 12%, and 11% respectively; and in the low attendance group 10%, 5%, and 12% respectively. These are about 2 to 4 times higher than the rates in the high attendance group (2%, 3%, 3% respectively), descending (7%, 6%, and 3%, respectively) and rising (5%, 3%, and 4%, respectively) attendance classes.
4. Discussion
Highlighting the main results, six distinct 12-step attendance classes were delineated with this sample of integrated health care system treatment seekers. Most individuals populated either the high attendance class (a fourth of the sample) or the no attendance class (a third of the sample). Though their attendance declined somewhat over time, those in the high class reported the highest stable pattern of past 30-day alcohol and drug abstinence over time, and those in the no attendance class reported the lowest pattern of abstinence. Among individuals in the four other classes, abstinence patterns for the most reflected attendance patterns at 1- and 5- years, followed with abstinence patterns becoming more stable at later follow-ups. Four of several help-seeking factors associated with 12-step attendance in prior studies were associated with class membership in the final LCGA model, gender and age (predisposing factors), baseline ASI alcohol severity (a need factor), and index treatment days (an enabling factor). We discuss these findings and their implications more fully below.
4.1 Help-seeking (predisposing, need, and enabling) predictors of class membership
The three trajectory classes whose members reported attendance at all follow-ups (the high, descending, and rising classes) had proportionately more women and greater baseline alcohol severity. Because one of the most robust predictors of 12-step attendance in the literature is problem severity (Bogenschutz, 2008; Emrick, et al., 1993), our finding that ASI alcohol severity predicted membership in the classes with repeated 12-step exposure across 9 years is not surprising. At the other extreme, individuals whose alcohol problems were less severe at baseline tended to congregate in the classes that either never attended meetings (the no class) or who dropped their attendance sooner (the early-drop class) or later (the low class). These findings are consistent with prior research on 12-step engagement and dropout (Connors, Tonigan, & Miller, 2001; Kaskutas, et al., 2008; Tonigan, Bogenschutz, & Miller, 2006).
Although there now are a number of evidence-based 12-step facilitation approaches available that help clients connect with the 12-step culture (Dennis M. Donovan & Floyd, 2008; Kaskutas, Subbaraman, Witbrodt, & Zemore, 2009; Nowinski, Baker, & Carroll, 1992; Timko & Debenedetti, 2007) and initiate the longer term recovery process, our findings also show that some individuals (e.g., those in the no attendance class) respond to other interventions outside the formal treatment system, for example, from a physician or the church or supportive family and friends. These results support recommendations coming out of a 2003 workshop (Humphreys et al., 2004) advising clinicians to become familiar with empirically-validated techniques and to thoughtfully address the diversity of client characteristics in their practice. Finally, more research is needed on those with lower severity to examine if they may be more appropriate for treatment programs which emphasize non-problem use, at least in the long-term.
Our result that women, rather than men, disproportionately populated those classes that stayed connected with 12-step groups over time also is of clinical relevance to providers who may be concerned about recommending 12-step groups to their female clients. It adds to a growing but mixed literature on men’s and women’s use of 12-step groups (Bogenschutz, 2008; Timko, 2008). One concern about referring women to groups like AA or NA has been that the 12-step philosophy, especially the focus on “powerlessness” and “making amends”, may detract from personal autonomy (Kelly, et al., 2006; Timko, 2008). Based on the gender distributions within the 6 classes, our longitudinal findings add to that empirical evidence which shows that women attend at least equally to men and that they appear to get as much or more out of their participation (Rudolf H. Moos, Moos, & Timko, 2006; Timko, et al., 2002; Witbrodt & Delucchi, in press).
Two other help-seeking factors, age and length of stay, also predicted class membership, but not in any consistent way. For example, those in the two classes that reported high 12-step attendance early on, but little or none subsequently (the descending and early-drop classes) were older than those in the other classes. The longest average length of treatment was among those who terminated their 12-step attendance the soonest (the early-drop class), rather than, say, among the high class. Given the emphasis on length of stay in the field, we will discuss these findings further in our summary of the trajectories’ profiles and after a discussion of how abstinence over time tracked with the attendance trajectories. Lastly, a number of other help-seeking factors tested with this private, integrated health care sample did not meaningfully differentiate one class from another, suggesting that they probably do not moderate longitudinal attendance trajectories.
4.2 12-step attendance class membership and longitudinal outcomes
The only requirement for membership in AA is “a desire to stop drinking” (Alcoholics Anonymous, 2001, page 562), and the fellowship’s stated primary purpose is to “stay sober and to help others to achieve sobriety” (Alcoholics Anonymous, 1958). Likewise, NA and CA fellowships, which were granted AA’s permission to use the AA steps and traditions in 1953, take a similar stance (Laudet, 2008). Meetings often end with “keep coming back,” and AA folklore has it that those who do not keep coming back are the ones who will start drinking again. Thus, we might expect that the rates of abstinence would be higher over time among the classes who kept coming back, which here is the high, descending, and rising classes. Indeed, by the 9-year interview abstinence rates were the highest in those respective classes (78%, 60%, and 65%). Hence, it does appear the case that coming back bodes well for abstinence. Results also reinforce an emerging literature (Rudolph H. Moos & Moos, 2004; Rudolf H. Moos & Moos, 2006; Ritsher, Moos, & Finney, 2002) regarding a key role for high initial levels of attendance following treatment, reflected by the fairly high rate of abstinence (54% at year 9) among the early-drop class whose attendance at year 1 had been close to that of the high class. Clinicians may do well to foster higher attendance early on for those clients amenable to these groups.
Despite reported higher average psychiatric scores over time, individuals in the high and rising classes reported abstinence rates which paralleled their (high/rising) 12-step attendance. This is contrasted against the Project MATCH results which found that outpatient alcohol-dependent clients with lower ASI psychiatric severity reported better outcomes after TSF treatment than after CBT, but no added benefit was found for those with higher psychiatric severity scores. Mean baseline scores for Project MATCH outpatient participants were 0.19 (SD .19) (Cooney et al., 2001), much lower than mean baseline ASI scores reported by those in our sample with alcohol and drug use disorders. We are at a loss to explain fully these differences. Although consistent empirical evidence supporting the value of 12-step participation for dually-diagnosed individuals is still lacking (Bogenschutz & Akin, 2000), our findings add support to the argument that when those with greater psychiatric severity become linked to self-help groups they seem to benefit from that involvement, and as put forward by Timko, these groups may well offer an element of continuity of care that reduces relapse risk (Timko, 2008).
Complicating the role of 12-step attendance on abstinence, the no and low classes reported relatively high rates of abstention (about 35% and 45% respectively) at every follow-up, despite their very limited attendance trajectories. These rates among our alcohol and drug dependent treatment clients are very similar to those found in the parallel AA attendance trajectories’ analyses conducted with the community sample of alcohol-dependent individuals (Kaskutas, 2005; 2009), and they are consistent with the large literature on natural recovery that consistently finds a considerable band of individuals who maintain abstinence with little or no treatment or any ongoing service utilization (Bischof, Rumpf, Hapke, Meyer, & John, 1996; Cohen, Feinn, Arias, & Kranzler, 2007; Dawson et al., 2005; Granfield & Cloud, 2001). Moreover, we saw that an additional 11% or more of both the non-attending and early drop classes were non-problem users at each of the long-term follow-ups, and there were some additional non-problem users in the low-attending class (between 5% and 12% at the long-term follow-ups). These results reinforce that 12-step attendance may not be indicated for all treatment clients (Cloud & Kingree, 2008; Humphreys, et al., 2004).
4.3 Profiling the characteristics of each 12-step attendance class
We begin with the class that stayed in treatment the longest, the early-drop class (n=291) whose attendance and abstinence rates at the 1-year follow-up were similar to that observed for the high class, but reported attending no meetings at 5, 7, or 9 years. They had low ASI alcohol (and psychiatric) severity scores at baseline, which remained so over time. Considering their especially long treatment episodes along with their relatively low problem severity, we would hypothesize that many in this class may have been mandated to treatment by their employers, dutifully attending 12-step meetings early on and then stopping. We were unable to look at referral pathways here, but hope to do so in future studies.
In contrast to the high attendance year 1 for the early-drop class, attendance the year after treatment was very low for the low class (and remained so over time) and was nonexistent for the large (n=608) no class. Alcohol (and psychiatric) problem severity was never high in these classes (especially relative to the high class), and it did not increase at follow-ups. Because of their low problem profile, it may be that these groups may not identify well with those they would meet at 12-step meetings (and possibly in treatment); and as noted above, they seem to have found some other path to recovery. These individuals remain a compelling group for further study.
The rising class could be characterized as having had moderate lengths of stay in treatment but quite low 12-step attendance the year following treatment, coupled with fairly high alcohol (particularly early in their trajectory) and psychiatric severity throughout the study period. Yet by year 9, they were averaging about five meetings a month (extrapolated from APDA), and 60% reported they were abstinent. While it is not possible to ascertain causality with our study, these results are consistent with this group having benefited from its 12-step attendance, although the treatment episode that began at study entry may not have endeared them to these groups. It is equally likely that these individuals were not ready to give up their use at that time. Although a fairly small class (5% of the total sample), their problem profile (which included psychiatric problems) and their behavior over time seem to reflect the cycling nature of many individuals seen in treatment settings (and eventually in 12-step groups).
The descending class (n=220) looks much like the high class (n=457) in several ways: high alcohol and psychiatric severity at baseline, treatment episodes in excess of 80 days, a large number of 12-step meetings the year following treatment entry and high abstinence rates (over 70%) at the 1-year interview. But unlike the high class (who continued to attend a large number of meetings at the subsequent follow-ups and whose abstinence rates over time were significantly higher as well), attendance for the descending class dropped steeply by year 5 (but still averaged about one meeting a month by year 9, a point when 60% reported past 30-day abstinence). Our thoughts for the descending class are that their psychiatric severity at 1 and 5 years was lower than the high class but their alcohol problems were as severe, and perhaps they benefited greatly from their index treatment stay and their initial high dose of exposure which they sustained over time (albeit at modest levels).
We conclude with the high class that initiated treatment with high past 30-day alcohol severity and which subsequently reported the highest attendance over time. With the highest abstinence rates and lowest follow-up ASI alcohol severity, the group presents a compelling case for a causal connection between attendance and remission from severe substance use problems in a private integrated health care treatment sample.
4.4 Comparing 12-step meeting trajectories between study sample
How did the 12-step attendance of private integrated health care alcohol and drug disordered treatment clients compare to AA attendance in Kaskutas’ (2009) treated and untreated alcohol-dependent individuals over time? The latter work identified four classes of AA attendance: high, medium, descending, and low. Because those analyses required a priori that each class be populated by at least 5% of the total sample, the number of distinct classes that could be identified was restricted as a function of the sample size. Did the same attendance patterns emerge with our larger sample of alcohol and drug dependent clients when looking at 12-step attendance? Indeed, four of the six classes found for the integrated health care treatment sample looked much like Kaskutas’ four classes in terms of their shapes, providing further evidence for the robustness of those attendance patterns over time. Did our descending and high classes have similar abstinence rates, as had been found in the prior study? Not quite. Our high and descending classes both reported high levels of abstention at 7- and 9- years, but the two did not converge to the degree observed in Kaskutas’ work. Individuals in our high class had past-30-day alcohol and drug abstinence rates 20% greater than those in the descending class at the last three follow-ups, whereas abstinence rates over time or at later follow-ups were more similar in these two groups among Kaskutas’ treated and untreated alcohol-dependent sample. Keep in mind that the prior trajectories’ work focused on AA attendance and abstinence from alcohol and in an alcohol-dependent sample, whereas the current sample also includes drug-only dependent individuals and the current study’s attendance measure includes AA, NA, and CA groups and our outcome was total abstinence from alcohol and drugs. We suspect that the higher abstinence in our high class may be due in part to this being a more stably insured or employed population. This also highlights the value (and complexity) of replicating findings with similar techniques but different samples. Finally, did anything new emerge? Our larger sample size allowed the identification of two classes not seen before, the rising and early-drop classes, while at the same time detecting four classes similar to those detected in the prior work.
4.5 Limitations
We enumerate limitations with this work. As is frequently the case, we relied on self-reported data for past-30-day alcohol and drug abstention at all follow-ups. As well, 12-step attendance was a self-reported aggregate covering prior 12-month periods (6 months at year 1), thus we lack full information on patterns of attendance and other 12-step behaviors and practices also known to influence recovery (Dennis M. Donovan & Floyd, 2008). Further, we have considerable gaps in data between follow-ups. Though attrition is always a problem with longitudinal data, the use of LCGA techniques minimized this concern and follow-up rates were comparable to other substance use studies. Similarly, among the n=126 cases dropped from the analysis, the loss was not equal across the diagnostic classifications. As a secondary data analysis, we lacked baseline measures for prior 12-step involvement and treatment episodes. Undoubtedly, prior treatment (and prior 12-step involvement) exposures may have influenced subsequent attendance for some study participants. However, some evidence suggests that 12-step attendance prior to treatment does not predict posttreatment drinking outcomes (Tonigan, Miller, & Connors, 2001). Last, these results will generalize best to other private, integrated health care or similarly insured populations.
4.6 Implications
Our results reflect those summarized in a recent literature review, that is, treatment program content that includes and facilitates 12-step participation appears to facilitate better post-treatment participation (Dennis M. Donovan & Floyd, 2008), and especially in the year after treatment initiation as shown for the majority of our study sample. Still, some individuals do not attend and do fare well in terms of abstinence (like the no attendance group). These findings suggest that providers might do well to encourage participation in 12-step groups when appropriate (such as when problem severity is high) while avoiding indiscriminant and generalized prescriptions (Cloud & Kingree, 2008).
Acknowledgments
This secondary analysis was supported by grants from the National Institute on Alcohol Abuse and Alcoholism (RO1AA10359) and the National Institute on Drug Abuse (R37DA10572 and R01DA08728).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aday LA, Begley CE, Lairson DR, Slater CH, Richard AJ, Montoya ID. A framework for assessing the effectiveness, efficiency, and equity of behavioral healthcare. The American Journal of Managed Care. 1999;5(Special Issue):SP25–SP44. [PubMed] [Google Scholar]
- Alcoholics Anonymous. A.A. Preamble. The A.A. Grapevine; 1958. [accessed 06/14/10]. [ http://www.aa.org/en_pdfs/smf-92_en.pdf. ] [Google Scholar]
- Alcoholics Anonymous. The Big Book Online. 4. New York: Alcoholics Anonymous World Services, Inc; 2001. http://www.aa.org/bigbookonline/index.cfm. [Google Scholar]
- Alcoholics Anonymous. Estimates of AA groups and members. General Service Office, Alcoholics Anonymous; 2007. [ www.aa.org/lang/en/subpage.cfm?page=74] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Andersen R, Newman JP. Societal and individual determinants of medical utilization in the United States. Millbank Memorial Fund Quarterly. 1973;51:95–124. [PubMed] [Google Scholar]
- Anderson KG, Ramo DE, Cummins KM, Brown SA. Alcohol and drug involvement after adolescent treatment and functioning during emerging adulthood. Drug and Alcohol Dependence. 2010;107(2–3):171–181. doi: 10.1016/j.drugalcdep.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischof G, Rumpf HJ, Hapke U, Meyer C, John U. Factors influencing remission from alcohol dependence without formal help in a representative population sample. Addiction. 1996;96(9):1327–1336. doi: 10.1046/j.1360-0443.2001.969132712.x. [DOI] [PubMed] [Google Scholar]
- Bogenschutz MP. Individual and contextual factors that influence AA affiliation and outcomes. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and spirituality in addiction recovery. Vol. 18. New York: Springer; 2008. pp. 413–433. [DOI] [PubMed] [Google Scholar]
- Bogenschutz MP, Akin SJ. 12-step participation and attitudes toward 12-step meetings in dual diagnosis patients. Alcoholism Treatment Quarterly. 2000;18(4):31–45. [Google Scholar]
- Box GEP, Cox DR. An analysis of transformations. Journal of the Royal Statistical Society. 1964;77:209–210. [Google Scholar]
- Brown BS, O’Grady KE, Farrell EV, Flechner IS, Nurco DN. Factors associated with frequency of 12-step attendance by drug abuse clients. American Journal of Drug and Alcohol Abuse. 2001;27(1):147–160. doi: 10.1081/ada-100103124. [DOI] [PubMed] [Google Scholar]
- Carroll RJ, Ruppert D. Transformation and Weighting in Regression. New York, NY: Chapman and Hall; 1988. [Google Scholar]
- Chassin L, Fora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: the effects of familial alcoholism and personality. Journal of Abnormal Psychology. 2004;113(4):483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Chi FW, Kaskutas LA, Sterling S, Campbell CI, Weisner C. Twelve-step affiliation and three-year substance use outcomes among adolescents: social support and religious service attendance as potential mediators. Addiction. 2009;104(6):927–939. doi: 10.1111/j.1360-0443.2009.02524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung T, Maisto SA, Cornelius JR, Martin CS. Adolescents’ alcohol and drug use trajectories in the year following treatment. Journal of Studies on Alcohol. 2004;65(1):105–114. doi: 10.15288/jsa.2004.65.105. [DOI] [PubMed] [Google Scholar]
- Cloud RN, Kingree JB. Concerns about dose and underutilization of twelve-step programs: models, scales, and theory that inform treatment planning. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and Spirituality in Addiction Recovery. Vol. 18. New York: Springer; 2008. pp. 283–301. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence. 2007;86(2–3):214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Connors GJ, Tonigan JS, Miller WR. A longitudinal model of intake symptomatology, AA participation, and outcome: retrospective study of the Project MATCH outpatient and aftercare samples. Journal of Studies on Alcohol. 2001;62(6):817–825. doi: 10.15288/jsa.2001.62.817. [DOI] [PubMed] [Google Scholar]
- Cooney N, Anton RF, Carbonari J, Carroll KM, Randall C, Roberts J. Matching clients to alcoholism treatment based on psychopathology. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and Causal Chain Analyses. Vol. 8. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. pp. 82–97. [Google Scholar]
- Crape BL, Latkin CA, Laris AS, Knowlton AR. The effects of sponsorship in 12-step treatment of injection drug users. Drug and Alcohol Dependence. 2002;65(3):291–301. doi: 10.1016/s0376-8716(01)00175-2. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. Recovery from DSM-IV alcohol dependence: United States, 2001–2002. Addiction. 2005;100(3):281–292. doi: 10.1111/j.1360-0443.2004.00964.x. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Mattson ME. The gender matching hypothesis. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and causal chain analyses. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. pp. 186–203. [Google Scholar]
- Delucchi KL, Matzger H, Weisner C. Dependent and problem drinking over 5 years: a latent class growth analysis. Drug and Alcohol Dependence. 2004;74(3):235–244. doi: 10.1016/j.drugalcdep.2003.12.014. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Floyd AS. Facilitating involvement in 12-step programs. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and Spirituality in Addiction Recovery. Vol. 18. New York: Springer; 2008. pp. 303–320. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Wells EA. Tweaking 12-step: the potential role of 12-step self-help group involvement in methamphetamine recovery. Addiction. 2007;102(Suppl 1):121–129. doi: 10.1111/j.1360-0443.2007.01773.x. [DOI] [PubMed] [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery HA, Little L. Alcoholics Anonymous: what is currently known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and alternatives. New Brunswick, NJ: Rutgers Center of Alcohol Studies; 1993. pp. 41–78. [Google Scholar]
- Fiorentine R. After drug treatment: are 12-step programs effective in maintaining abstinence? The American Journal of Drug and Alcohol Abuse. 1999;25(1):93–116. doi: 10.1081/ada-100101848. [DOI] [PubMed] [Google Scholar]
- Genberg BL, Gange SJ, Go VF, Celentano DD, Kirk GD, Mehta SH. Trajectories of injection drug use over 20 years (1988–2008) in Baltimore, Maryland. American Journal of Epidemiology. 2011;173(7):829–836. doi: 10.1093/aje/kwq441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Stewart D, Marsden J. Attendence at Narcotics Anonymous and Alcoholics Anonymous meetings, frequency of attendence and substance use outcomes after residential treatment for drug dependence: a 5 year follow-up study. Addiction. 2008;103(1):119–125. doi: 10.1111/j.1360-0443.2007.02050.x. [DOI] [PubMed] [Google Scholar]
- Goudriaan AE, Grekin ER, Sher KJ. Decision making and binge drinking: a longitudinal study. Alcoholism: Clinical and Experimental Research. 2007;31(6):928–938. doi: 10.1111/j.1530-0277.2007.00378.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granfield R, Cloud W. Social context and “natural recovery”: the role of social capital in the resolution of drug-associated problems. Substance Use and Misuse. 2001;36(11):1543–1570. doi: 10.1081/ja-100106963. [DOI] [PubMed] [Google Scholar]
- Greenbaum PE, Del Boca FK, Darkes J, Wang CP, Goldman MS. Variation in the drinking trajectories of freshman college students. Journal of Consulting and Clinical Psychology. 2005;73(2):229–238. doi: 10.1037/0022-006X.73.2.229. [DOI] [PubMed] [Google Scholar]
- Grella CE, Lovinger K. 30-year trajectories of heroin and other drug use among men and women sampled from methadone treatment in California. Drug and Alcohol Dependence. doi: 10.1016/j.drugalcdep.2011.04.004. (in press) [doi:10.1016/j.drugalcdep.2011.04.004] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinz AJ, Wu J, Witkiewitz K, Epstein DH, Preston KL. Marriage and relationship closeness as predictors of cocaine and heroin use. Addictive Behaviors. 2009;34(3):258–263. doi: 10.1016/j.addbeh.2008.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HMO Research Network. Members of the HMO Research Network. HMO Research Network; 2009. [Accessed: 2011-07-06]. Archived by WebCite® at http://www.webcitation.org/5zz44eztd] [Google Scholar]
- Hser YI, Anglin MD, Grella C, Longshore D, Prendergast ML. Drug treatment careers: a conceptual framework and existing research findings. Journal of Substance Abuse Treatment. 1997;14(6):543–558. doi: 10.1016/s0740-5472(97)00016-0. [DOI] [PubMed] [Google Scholar]
- Hser YI, Huang D, Brecht ML, Li L, Evans E. Contrasting trajectories of heroin, cocaine and methamphetamine use. Journal of Addictive Diseases. 2008;27(3):13–21. doi: 10.1080/10550880802122554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K. Alcoholics Anonymous and 12-step alcoholism treatment programs. Recent Developments in Alcoholism. 2003;16:149–164. doi: 10.1007/0-306-47939-7_12. [DOI] [PubMed] [Google Scholar]
- Humphreys K. Circles of Recovery: Self-help organizations for addictions. Cambridge, UK: Cambridge University Press; 2004. [Google Scholar]
- Humphreys K, Moos RH, Finney JW. Two pathways out of problem drinking problems without professional treatment. Addictive Behaviors. 1995;20(4):427–441. doi: 10.1016/0306-4603(95)00005-w. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Wing S, McCarty D, Chappel JN, Gallant L, Haberle B, et al. Self-help organizations for alcohol and drug problems: toward evidence-based practice and policy. Journal of Substance Abuse Treatment. 2004;26(3):151–158. doi: 10.1016/S0740-5472(03)00212-5. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Gotham HJ, Wood PK. Transitioning into and out of large-effect drinking in young adulthood. Journal of Abnormal Psychology. 2001;110(3):378–391. doi: 10.1037//0021-843x.110.3.378. [DOI] [PubMed] [Google Scholar]
- Joe GW, Chastain RL, Simpson DD. Length of careers. In: Simpson DD, Sells SB, editors. Opioid Addiction and Treatment: A 12-year follow-up. Malabar, FL: Robert E. Krieger Publishing Company; 1990. pp. 103–119. [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. [Google Scholar]
- Kaskutas LA, Ammon LN, Delucchi K, Room R, Bond J, Weisner C. Alcoholics Anonymous careers: patterns of AA involvement five years after treatment entry. Alcoholism: Clinical and Experimental Research. 2005;29(11):1983–1990. doi: 10.1097/01.alc.0000187156.88588.de. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA, Bond J, Ammon Avalos L. 7-year trajectories of Alcoholics Anonymous attendance and associations with treatment. Addictive Behaviors. 2009;34(12):1029–1035. doi: 10.1016/j.addbeh.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Subbaraman MS, Witbrodt J, Zemore SE. Effectiveness of Making Alcoholics Anonymous Easier (MAAEZ), a group format 12-step facilitation approach. Journal of Substance Abuse Treatment. 2009;37(3):228–239. doi: 10.1016/j.jsat.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Ye Y, Greenfield TK, Witbrodt J, Bond J. Epidemiology of Alcoholics Anonymous participation. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and spiritual aspects in addiction recovery. Vol. 18. New York: Springer; 2008. pp. 261–282. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Stout R, Zywiak WH, Schneider R. A 3-year study of addiction mutual-help group participation following intensive outpatient treatment. Alcoholism: Clinical and Experimental Research. 2006;30(8):1381–1392. doi: 10.1111/j.1530-0277.2006.00165.x. [DOI] [PubMed] [Google Scholar]
- Kissin W, McLeod C, McKay J. The longitudinal relationship between self-help group attendance and course of recovery. Evaluation and Program Planning. 2003;26(3):311–323. [Google Scholar]
- Laudet AB. The impact of Alcoholics Anonymous on other substance abuse-related twelve-step programs. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and spirituality in addiction recovery. Vol. 18. New York: Springer; 2008. pp. 71–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemke S, Moos RH. Outcomes at 1 and 5 years for older patients with alcohol use disorders. Journal of Substance Abuse Treatment. 2003;24(1):43–50. doi: 10.1016/s0740-5472(02)00321-5. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. [Google Scholar]
- McElrath D. The Minnesota Model. Journal of Psychoactive Drugs. 1997;29(2):141–144. doi: 10.1080/02791072.1997.10400180. [DOI] [PubMed] [Google Scholar]
- McKellar J, Ilgen M, Moos BS, Moos R. Predictors of change in alcohol-related self-efficacy over 16 years. Journal of Substance Abuse Treatment. 2008;35(2):148–155. doi: 10.1016/j.jsat.2007.09.003. [DOI] [PubMed] [Google Scholar]
- McKellar J, Stewart E, Humphreys K. Alcoholics Anonymous involvement and positive alcohol-related outcomes: cause, consequence, or just a correlate? A prospective 2-year study of 2,319 alcohol-dependent men. Journal of Consulting and Clinical Psychology. 2003;71(2):302–308. doi: 10.1037/0022-006x.71.2.302. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. The Journal of the American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Flisher AJ, Satre DD, Weisner C. The role of medical conditions and primary care services in 5-year substance use outcomes among chemical dependency treatment patients. Drug and Alcohol Dependence. 2008;98(1–2):45–53. doi: 10.1016/j.drugalcdep.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Long-term influence of duration and frequency of participation in Alcoholics Anonymous on individuals with alcohol use disorders. Journal of Consulting and Clinical Psychology. 2004;72(1):81–90. doi: 10.1037/0022-006X.72.1.81. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Paths of entry into Alcoholics Anonymous: consequences for participation and remission. Alcoholism: Clinical and Experimental Research. 2005;29(10):1858–1868. doi: 10.1097/01.alc.0000183006.76551.5a. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Participation in treatment and Alcoholics Anonymous: a 16-year follow-up of initially untreated individuals. Journal of Clinical Psychology. 2006;62(6):735–750. doi: 10.1002/jclp.20259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Moos BS, Timko C. Gender, treatment and self-help in remission from alcohol use disorders. Clinical Medicine and Research. 2006;4(3):163–174. doi: 10.3121/cmr.4.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Second-generation structural equation modeling with a combination of categorical and continuous latent variables: new opportunities for latent class/latent growth modeling. In: Collins LM, Sayer A, editors. New Methods for the Analysis of Change. Washington, D.C: American Psychological Association; 2001. pp. 291–322. [Google Scholar]
- Muthén B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. The Sage Handbook of Quantitative Methodology for the Social Sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Muthén B, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55(2):463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén B. Mplus Version 5. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- Muthén LK, Muthén B. Mplus User’s Guide, Version 5. Los Angeles, CA: Muthén & Muthén; 2008a. [Google Scholar]
- Muthén LK, Muthén B. Mplus version 5.1. Los Angeles, CA: Muthén & Muthén; 2008b. [Google Scholar]
- Nagin DS. Analyzing development trajectories: a semi-parametric group-based approach. Psychological Methods. 1999;4:139–157. [Google Scholar]
- Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: a group-based method. Psychological Methods. 2001;6:18–34. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Narcotics Anonymous World Services. Narcotics Anonymous 2009 Membership Survey. Van Nuys, CA: Narcotics Anonymous World Services, Inc; 2010. [Accessed: 2011-06-27]. Archived by WebCite® at http://www.webcitation.org/5zl6xut21. [Google Scholar]
- Nowinski J, Baker S, Carroll K. Twelve step facilitation therapy manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence [Project MATCH monograph series/DHHS publication, no. (ADM) 92-1893] Vol. 1. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Nylund KL, Muthén BO, Asparouhov T. Deciding on the number of classes in latent class analysis: a Monte Carol simulation study. Los Angeles, CA: Department of Advanced Quantitative Methods, Graduate School of Education and Information Studies, UCLA; 2004. [Google Scholar]
- Orwat J, Samet JH, Tompkins CP, Cheng DM, Denato MP, Saitz R. Factors associated with attendance in 12-step groups (Alcoholics Anonymous/Narcotics Anonymous) among adults with alcohol problems living with HIV/AIDS. Drug and Alcohol Dependence. 2011;113(2–3):165–171. doi: 10.1016/j.drugalcdep.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette P, Moos RH, Finney JW. PTSD treatment and 5-year remission among patients with substance use posttraumatic stress disorders. Journal of Consulting and Clinical Psychology. 2003;71(2):410–414. doi: 10.1037/0022-006x.71.2.410. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Kimerling R, Shaw J, Moos RH. Physical and sexual abuse among women and men with substance use disorders. Alcoholism Treatment Quarterly. 2000;18(3):7–17. [Google Scholar]
- Oxford ML, Gilchrist LD, Morrison DM, Gillmore MR, Lohr MJ, Lewis SM. Alcohol use among adolescent mothers: heterogeneity in growth curves, predictors, and outcomes of alcohol use over time. Prevention Science. 2003;4(1):15–26. doi: 10.1023/a:1021730726208. [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Moos RH, Finney JW. Relationship of treatment orientation and continuing care to remission among substance abuse patients. Psychiatric Services. 2002;53:595–601. doi: 10.1176/appi.ps.53.5.595. [DOI] [PubMed] [Google Scholar]
- Satre DD, Blow FC, Chi FW, Weisner C. Gender differences in seven-year alcohol and drug treatment outcomes among older adults. American Journal on Addictions. 2007;16(3):216–221. doi: 10.1080/10550490701375673. [DOI] [PubMed] [Google Scholar]
- Satre DD, Mertens JR, Areán PA, Weisner C. Five-year alcohol and drug treatment outcomes of older adults versus middle-aged and younger adults in a managed care program. Addiction. 2004;99(10):1286–1297. doi: 10.1111/j.1360-0443.2004.00831.x. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–23. [PubMed] [Google Scholar]
- Simpson DD. Longitudinal outcome patterns. In: Simpson DD, Sells SB, editors. Opioid Addiction and Treatment: A 12-year follow-up. Malabar, FL: Robert E. Krieger Publishing Company; 1990. pp. 55–71. [Google Scholar]
- Slaymaker VJ, Sheehan T. The impact of AA on professional treatment. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and spirituality in addiction recovery. Vol. 18. New York: Springer; 2008. pp. 59–70. [DOI] [PubMed] [Google Scholar]
- Stata Corp. Stata Statistical Software: Release 10.0. College Station, TX: Stata Corporation; 2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, & Office of Applied Studies. Data on Substance Abuse Treatment Facilities. Rockville, MD: Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2008. [Accessed: 2011-06-29]. 2007 National Survey of Substance Abuse Treatment Services (N-SSATS): 2007; p. 216. Archived by WebCite® at http://www.webcitation.org/5zoHAgi8G. [Google Scholar]
- Sussman S. A review of Alcoholics Anonymous/Narcotics Anonymous programs for teens. Evaluation and the Health Professions. 2010;33(1):26–55. doi: 10.1177/0163278709356186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C. Outcomes of AA for special populations. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and spirituality in addiction recovery. Vol. 18. New York: Springer; 2008. pp. 373–392. [DOI] [PubMed] [Google Scholar]
- Timko C, Billow R, DeBenedetti A. Determinants of 12-step group affiliation and moderators of the affiliation-abstinence relationship. Drug and Alcohol Dependence. 2006;83(2):111–121. doi: 10.1016/j.drugalcdep.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Timko C, Debenedetti A. A randomized controlled trial of intensive referral to12-step self-help groups: one-year outcomes. Drug and Alcohol Dependence. 2007;90(2–3):270–279. doi: 10.1016/j.drugalcdep.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Timko C, Finney JW, Moos RH, Steinbaum DP. The process of treatment selection among previously untreated help-seeking problem drinkers. Journal of Substance Abuse. 1993;5(3):203–220. doi: 10.1016/0899-3289(93)90064-i. [DOI] [PubMed] [Google Scholar]
- Timko C, Moos RH, Finney JW, Connell EG. Gender differences in help-utilization and the 8-year course of alcohol abuse. Addiction. 2002;97(7):877–889. doi: 10.1046/j.1360-0443.2002.00099.x. [DOI] [PubMed] [Google Scholar]
- Tonigan JS. Alcoholics Anonymous outcomes and benefits. In: Galanter M, Kaskutas LA, editors. Recent Developments in Alcoholism: Research on Alcoholics Anonymous and spirituality in addiction recovery. Vol. 18. New York: Springer; 2008. pp. 357–372. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Bogenschutz MP, Miller WR. Is alcoholism typology a predictor of both Alcoholics Anonymous affiliation and disaffiliation after treatment? Journal of Substance Abuse Treatment. 2006;30(4):323–330. doi: 10.1016/j.jsat.2006.02.008. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Miller WR, Connors GJ. Prior Alcoholics Anonymous involvement and treatment outcome. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and causal chain analyses. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. pp. 276–284. [Google Scholar]
- Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. Journal of Studies on Alcohol. 1996;57(1):65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Rippens PD. Different variables are associated with help-seeking patterns and long-term outcomes among problem drinkers. Addictive Behaviors. 2004;29(2):433–439. doi: 10.1016/j.addbeh.2003.08.015. [DOI] [PubMed] [Google Scholar]
- Vaillant GE. Addictions over the life course: Therapeutic implications. In: Edwards G, Dare C, editors. Psychotherapy, Psychological Treatments and the Addictions. London: Cambridge University Press; 1996a. pp. 3–18. [Google Scholar]
- Vaillant GE. A long-term follow-up of male alcohol abuse. Archives of General Psychiatry. 1996b;53(3):243–249. doi: 10.1001/archpsyc.1996.01830030065010. [DOI] [PubMed] [Google Scholar]
- Weisner C, Delucchi K, Matzger H, Schmidt L. The role of community services and informal support on five-year drinking trajectories of alcohol dependent and problem drinkers. Journal of Studies on Alcohol. 2003;64(6):862–873. doi: 10.15288/jsa.2003.64.862. [DOI] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthasarathy S, Moore C, Hunkeler E, Hu TW, et al. The outcome and cost of alcohol and drug treatment in an HMO: day hospital versus traditional outpatient regimens. Health Services Research. 2000;35(4):791–812. [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Mertens J, Parthsarathy S, Moore C. Integrating primary medical care with addiction treatment: a randomized controlled trial. The Journal of the American Medical Association. 2001;286(14):1715–1723. doi: 10.1001/jama.286.14.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Parthasarathy S, Moore C, Mertens JR. Individuals receiving addiction treatment: are medical costs of their family members reduced? Addiction. 2010;105(7):1226–1234. doi: 10.1111/j.1360-0443.2010.02947.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisner C, Ray GT, Mertens J, Satre DD, Moore C. Short-term alcohol and drug treatment outcomes predict long-term outcome. Drug and Alcohol Dependence. 2003;71(3):281–294. doi: 10.1016/s0376-8716(03)00167-4. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Gallop R, Luborsky L, Siqueland L, Frank A, et al. Predictors of self-help group attendance in cocaine-dependent patients. Journal of Studies on Alcohol. 2000;61(5):714–719. doi: 10.15288/jsa.2000.61.714. [DOI] [PubMed] [Google Scholar]
- Witbrodt J, Bond J, Delucchi K. Predictors of Alcoholics Anonymous Utilization among US Males and Females: A Longitudinal Analysis. 35th Annual Alcohol Epidemiological Symposium of the Kettil Bruun Society for Social And Epidemiological Research on Alcohol; Copenhagen, Denmark. June 1–5.2009. [Google Scholar]
- Witbrodt J, Delucchi K. Do women differ from men on Alcoholics Anonymous participation and abstinence? A multi-wave analysis of treatment seekers. Alcoholism: Clinical and Experimental Research. doi: 10.1111/j.1530-0277.2011.01573.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witbrodt J, Kaskutas LA. Does diagnosis matter? Differential effects of 12-step participation and social networks on abstinence. The American Journal of Drug and Alcohol Abuse. 2005;31(4):685–707. doi: 10.1081/ada-68486. [DOI] [PubMed] [Google Scholar]