Abstract
Collaboration across disciplines is vital in clinical practice. It is also needed to generate high-quality actionable research, yet few frameworks for interdisciplinary collaboration exit to promote effective communications among researchers with common boals, but varied backgrounds. A review of that has been learned about collaboration was undertaken to determine attributes of effective interdisciplinary collaboration and barriers to its realization in patients undergoing lung transplantation.
Keywords: Lung transplantation, remote monitoring, pulmonary framework model, telemonitoring
INTRODUCTION
Interdisciplinary collaboration is increasingly recognized as a vital component of the conduct of research and providing healthcare. Its importance is underscored in its characterization as a scientific and social imperative.1 A key objective of the National Institutes of Health (NIH)Roadmap is to stimulate the work of interdisciplinary research teams.2 Interdisciplinary research has the potential to improve communication and accelerate discoveries and their translation to practice.3 It has been demonstrated in the clinical realm that the degree of collaboration between health professionals can directly impact patient outcomes.4 Indeed, poor communication or poor collaboration for many years was cited as the leading root cause of sentinel events reported to the Joint Commission of Accreditation of Health Organizations (JCAHO).5 Therefore, an important National Patient Safety goal of 2007 was to improve the effectiveness of communication among caregivers.6 Although the benefits of communication and collaboration have been a focus in clinical realms such as critical care, collaboration and interprofessional behavior remain understudied in research settings.
Nash7 suggests that the major challenge in interdisciplinary research extends to intrapersonal, interpersonal, and systems levels. There is a widespread perception that interdisciplinary collaboration is useful, but there is little evidence from well designed studies that have specifically tested the impact of interdisciplinary collaboration on the quality, effectiveness, or productivity of research teams and organizations.8 This is an important knowledge gap that is worthy of additional exploration because interdisciplinary collaboration in research is considered by some to be the foundation of scientific innovation.9 Bringing together professionals from different disciplines can create a forum for fresh perspectives to be expressed, and new ideas for solutions to be put forth and tested. The intellectual cross-pollination that can emerge from interdisciplinary collaborations is a promising ingredient for catalyzing scientific innovation.
Unfortunately, tangible examples and models or frameworks of interdisciplinary collaboration in research are relatively scarce.3,10 The potential end result of such gaps is that research teams may not fully realize their otherwise achievable synergies, may not perform at peak efficiency, or may not achieve optimal outcomes. In worst case scenarios, collaboration may be left to chance or lack a viable, guiding structure so that researchers may fail to fully understand each other or how best to work in partnership. Consequently, team interactions of persons with diverse views and perspectives may suffer from interdisciplinary conflict or rivalry, chaotic interface, or lower job satisfaction, yielding suboptimal productivity for the research team as a whole. As in all areas of collective human endeavor, maximizing the functioning and productivity of interdisciplinary research teams requires sound understanding of group dynamics, processes, roles, leadership as well as the contextual and environmental factors that affect teams.11
The purpose of this paper is to provide an overview of attributes of effective interdisciplinary collaboration and to identify barriers to its realization in patients undergoing lung transplantation. This paper focuses on the interpersonal aspects of team functioning rather than the administrative, academic (e.g., career path, professional development), financial, and systems issues that are also critical to interdisciplinary research ventures.3,12 Although core competencies have been outlined by Gebbie and colleagues13 and others14 and methods for developing interdisciplinary researchers have been described,7,12 examples of how to implement these have yet to be described. This paper offers practical suggestions for fostering collaboration through constructive interprofessional behaviors in the context of an interdisciplinary research team’s study of home monitoring via spirometry in lung transplantation.
DEFINING THE ISSUES
Collaboration is founded on the premise that individuals have special areas of expertise or capability that can be shared with other partners to enhance their overall capacity for mutual benefit, to increase effectiveness, and to optimally align resources.15 The term “collaboration” has been used interchangeably with terms such as communication, cooperative work, mutual planning, and integration of care.16 For the purpose of this paper, collaboration is defined as working together with others toward mutually agreed upon goals for a specified purpose or project as discussed by Wells and colleagues.17 In this paper, the term interdisciplinary is used, however, it is recognized that other terms, such as transdisciplinary or multidisciplinary, overlap considerably, and may be applied interchangeably. For a more detailed discussion on the definition of interdisciplinary collaboration, see Aboelela and colleagues.18
There have been increasing numbers of published studies that reflect interdisciplinary collaboration across health specialty areas.19, 20, 21, 22, 23 This is likely due, in part, to the increased complexity of large investigations funded through federal grants.9 It may also reflect broader trends in clinical care of expanding scopes of practice and increasing levels of collaboration among disciplines. In absence of a consensual framework for interdisciplinary training,12 the following is offered to describe an approach for interdisciplinary collaboration that can guide clinical research studies.
Attributes
Strong Working Relationships
For individuals to work effectively together in any setting, respectful relationships need to be fostered and maintained (see Table 1). Koch and colleagues24 describe optimal relationships in collaborative teams as respectful, accepting, and trustworthy. By maintaining mutual respect, team members “actively listen” to their colleagues’ concerns, reconcile discrepancies in perspectives, priorities and procedures, convey empathy, and maintain pathways for open communication that allow them to learn from and about each other. Self-awareness allows researchers to relate to and empathize with researchers from different disciplines and allows them to better understand the realities that influence other researchers’ viewpoints.25 It is also important to develop and preserve a sense of genuineness within the context of personal and professional communications. Researchers must be dependable (e.g., come to meetings prepared and on time, accomplish what they agree to between meetings), take responsibility for their limitations or mistakes, offer accurate advice, and maintain integrity consistently in team interactions. Appropriate displays of interpersonal skills, such as warmth and humor, enable researchers to appear more genuine to each other, thereby enhancing the camaraderie and morale within the group. Such characteristics make it easier for team members to get to know one another on a personal level in addition to a professional level. The end result of achieving fundamental levels of respect among research team members is a stronger commitment to achieving success in the shared enterprise.
Table 1.
Vital Characteristics, Importance, and Means to Cultivate Collaboration
| CHARACTERSITIC | IMPORTANCE | ESTABLISHING SOLUTIONS |
|---|---|---|
| Strong Working Relationships | Mutual appreciation of the individuals that work together motivates each team member to do a better job. |
|
| Shared Purpose | Working on agreed upon goals maximizes motivation and productivity of team members. |
|
| Effective Conflict Resolution | Disagreement or conflict may be inevitable when undertaking complex tasks. Effective conflict resolution is necessary to maintain working relationships. |
|
| Adequate Time | Effective collaboration requires adequate time for all team- related tasks. Without it, conflicts may go unresolved, the shared sense of purpose is diluted, and relationships drift. |
|
| Useable Technology | Complex technology may go underused, misused, or frustrate individuals when it does not work properly. |
|
| Role Clarity | Role clarity informs what needs to get done, who is responsible for doing it, and who is accountable if something goes wrong. |
|
| Cultural Respect | Respecting each other’s backgrounds and experiences creates a comfortable interpersonal environment that facilitates a general sharing of ideas and constructive criticism. |
|
Shared Purpose
Members of research teams share commitment to mutually understood goals. All members need to be adequately prepared to complete their respective tasks required to meet these goals. The general purpose of the research is defined at the outset. Broader interests of the group can evolve over time as secondary objectives are realized and refined. Establishing overarching objectives that are consistent with the team’s values is an important aspect of goal setting that keeps the team focused and on task.25
Whereas individual researchers come to the team with their own set of goals,26 the primary role of the principal investigator (PI) is to lead team members toward common objectives specific to the research. The PI for interdisciplinary research can be from any discipline providing that they have the requisite expertise relevant to the objectives of the research and can bring together the unique and diverse perspectives that are central to attaining these goals. Although other team members may assume leadership roles periodically or assume certain leadership duties, a strong leader’s guidance of the group towards the identified objectives is vital. In general, selection of group leadership is based on individuals’ research productivity and funding track record, relative seniority within their field and institution, history with relevant projects, communication and interpersonal skills, and openness to perspectives from diverse disciplines and to the collaborative process.3
Research objectives are most likely to be realized when PIs preside over regularly scheduled meetings3 with clear agendas that focus team members on problem-solving, sharing their work, reviewing progress and preliminary results, and providing group feedback. Such meetings help the team stay on task, identify challenges, address quality, safety, and adherence issues, and continue working towards mutually beneficial and rewarding goals and building relationships within the team. Maintaining study focus and execution is augmented by setting time frames for project milestones and planning for future studies, grant opportunities, and dissemination of findings.27 For example, clarification of timelines for manuscript preparation, plans for disseminating findings at presentations in relevant conferences, and specifying who will lead and work on each project component is essential to advancing the team’s multiple objectives. In assigning tasks, it is important to consider each individual’s background and strengths so that responsibilities match specific members’ skills, time, and capabilities for each undertaking25 and their respective funding support for involvement in the project(s). Whereas face-to-face meetings with entire teams are ideal, efficiencies may be gleaned by scheduling sub-team meetings and capitalizing on existing and emerging technology (e.g., telephone, videoconferencing, or other forms of telecommunications), especially for multi-site investigations.
Effective Conflict Resolution
Group therapy investigators frequently have observed that conflict is inevitable as part of group development.28,29 There is little reason to presume that interdisciplinary research teams would be immune to such dynamics. Achieving effective collaboration may require surmounting challenges, such as resolving disagreements emerging within research teams.25 Differences in opinion may ultimately strengthen the cohesiveness of the team if they are approached and resolved in a respectful manner. Working through conflicts may encourage assertiveness and foster enhanced natural problem-solving abilities within the group.
The interdisciplinary make-up of research groups increases the need for team members to support their positions and solutions with evidence to convince colleagues of their relative merits. It is prudent to recognize that some disagreements arise from being approached from different professional or scientific reference points or are the result of faulty miscommunications rather than products of inter-professional competition, personality mismatch, or intentional ill will. Often, discussion and clarification of the problems to be solved can mitigate miscommunications and prevent conflict. At times, multiple solutions may emerge, or dual tracks can be pursued to allow empirical resolution of vexing or potentially contentious issues.
Barriers
In forming and maintaining interdisciplinary research teams, it is essential to address the foreseeable barriers to collaboration and to identify any new barriers as they are encountered. These included time, technology, role ambiguity, and cultural differences.
Adequate Time
Committing time for research collaboration can be challenging despite the centrality of research in individuals’ professional objectives and institutions’ missions. Collaborative practice and research in the health sciences may involve full-time researchers as well as part-time researchers who also have demanding clinical practices.4 Both clinician and research team members have busy schedules and are often balancing multiple research, teaching, and clinical demands. Setting a regular meeting schedule well in advance maximizes the opportunity for productive clinicians and research staff to calendar and attend research meetings. Reminders of specific duties and timelines along with agenda updates are also helpful.
Useable Technology
The delivery of health care services is increasingly complex and compartmentalized, requiring input from diverse disciplines and specialties. Interventions in research studies may have technical components that practitioners are responsible for managing. For example, biomedical devices are developed by biomedical engineers and computer scientists for use in the field by practitioners with nursing, medical, behavioral, surgical, or pharmacological expertise rather than biomedical engineering competence. As a result, new technologies may need to be mastered by study personnel whose exposure to them may be insufficient to harness their full potential. Consequently, technology may not be used to its fullest advantage (i.e., benefiting from the entire array of potentially relevant functions), may be misused, or study personnel or research subjects may become frustrated when equipment is misunderstood or malfunctions.9 Inviting and including the participation of research team members with requisite expertise for promoting projects’ execution may minimize such problems.
Role Clarity
It is essential to recognize that contributions of diverse team members will enhance the final “product” of the research enterprise, i.e., dissemination of new knowledge. However, without clear boundaries and role identification, it may be difficult to assign tasks or even know whom to approach for specific tasks and responsibilities. Even when team members are clearly identified by their role, the question of “who does what?” may still be unclear. For example, is the team statistician responsible to conduct all of the data analyses for the study? What roles should each research assistant play? How will members articulate responsibilities and work together? Effective teamwork is built on a priori delineation of the research tasks and identification of which member(s) will be accountable to complete them and which individuals will assume more supportive or secondary roles. Similarly, it is prudent to determine how personnel will interact in the event of potential failure to meet objectives or impropriety in the conduct of the research. Roles may change as the research progresses, as team members mature, or as time allocation changes availability. Cross-training allows for greater flexibility for achieving research objectives (i.e., so that there can be a sufficiently “deep bench” of research personnel to compensate for staff turnover, illness, pregnancy, vacation).
Cultural Respect
It is essential that interdisciplinary research team members recognize their own professional culture and biases in order to demonstrate respect for other professional points of view. Professional differences are apparent across clinical and research settings and may need to be addressed formally among research team members in order to create an effective working environment. A prime example is the cultural differences between the disciplines of nursing and medicine that originate from two distinct theoretical frameworks.4 Each profession has its own educational and training paradigm, history, foci of interest, and ethics code that inform individuals’ perspectives and assumptions.7,12 Better understanding of the differences among research team members’ background and expertise may attenuate the intrusion of unnecessary tensions.
An additional consideration is the hierarchical nature of relationships among members of the research team. It is important to promote respect universally and discourage favoritism that could otherwise undermine communication, impair productivity, disrupt the free-flow of ideas among research members, or inhibit constructive expression of dissenting views and interpretations. Recognizing, but limiting the intrusion of hierarchy, and sharing leadership appropriately, allows teams to benefit fully from team members’ unique knowledge, skills, and other valuable contributions, and decreases the probability that team performance will be undermined by real or perceived inequalities in power or status.4.
APPLICATION
Case Study of Collaboration in the Context of a Home Spirometry Study
Although the complexity of the challenges and magnitude of the barriers to interdisciplinary research collaboration are appreciable, team-based research is critical to achieving scientific objectives. This section describes a case of interdisciplinary collaboration in the context of a clinical trial of home spirometry for lung transplant recipients. Selected experiences of our interdisciplinary team’s efforts to optimize attributes of interdisciplinary collaboration and illustrate the model are presented.
The long-term objective for home telehealth programs is to improve the health status of specific patient populations. In this study, lung transplant recipients were provided with home spirometers to detect early acute bronchopulmonary events early in their development, allowing for more timely interventions and improved outcomes.30 In our home monitoring system, transplant recipients recorded respiratory symptoms and performed lung function measurements using home spirometers that automatically transmitted measurements from participants’ homes to our data center via telephone.31,32 These data are evaluated by research and clinic nurses to identify participants exhibiting detectable indications of acute bronchopulmonary events. A computerized triage system was developed to facilitate this labor-intense process using a Bayesian algorithm to interpret the data. A randomized controlled trial comparing manual nurse triage with the computerized triage system in terms of patients’ health and quality of life is the basis for our interdisciplinary research team experience.
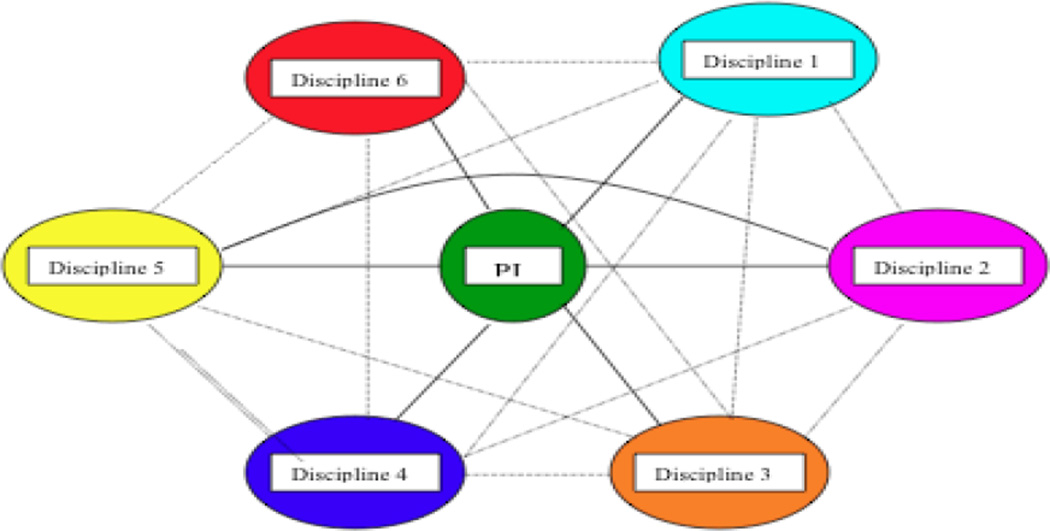
The research team consisted of ten investigators from diverse professional backgrounds. The PI had a background in engineering and health informatics and a lengthy record of conducting interdisciplinary research in this area. The co-investigators, research assistants, and study staff had diverse professional backgrounds including medicine, nursing, psychology, computer science, biostatistics, and health informatics. Figure 1 depicts the web of interactions among team members across disciplines. Most team members were located on the campus of the facility is in this research. There were also consulting team members who attended the meetings periodically from greater distances. The team’s geographic dispersion rendered communications a key element to optimal functioning. Communications took various forms, including via email, phone calls and scheduled face-to-face meetings. The ease of online communication allowed team members to communicate frequently and virtually real-time in addition to the schedule of planned meetings.
Figure 1.
Web of Interaction Among Interdisciplinary Team Members.
Terms for Figure 1: PI = principal investigator; Discipline 1 = Nursing; Discipline 2 = Medicine; Discipline 3 = Psychology; Discipline 4 = Computer Science; Discipline 5 = Biostatistics; Discipline 6 = Health Informatics
Optimizing Attributes of Interdisciplinary Collaboration
Our team used various strategies to cultivate collaboration. Strong working relationships and leadership from the PI were the underpinnings of our collaborative efforts, keeping the team on task and providing clarity in completing and prioritizing ongoing tasks and projects. The PI generously acknowledged the contributions and expertise of all the team members and actively solicited feedback and expertise.
Our collaborative process employed regular face-to-face meetings. Meetings were scheduled bimonthly. The PI planned blocks of meetings months in advance to accommodate student members’ changing academic schedules and reserved conference rooms to take advantage of the institution’s facilities. Consultants, data safety and monitoring board members and guest attendees were invited to selected team meetings. When team members were unable to attend, they communicated their progress and ideas in advance to the PI so as to contribute to the meeting despite their absence. Absent members were contacted by the PI by email or phone following the meeting to clarify any questions or tasks that needed attention. This communication protocol facilitated the teams’ progress. The week prior to each meeting, the PI emailed team members agendas and related items to perpetuate the momentum of the team’s work.
During team meetings, certain regular agenda items were discussed, namely recruitment, adherence, preliminary findings of specific projects, and updates on plans for dissemination of research findings through publications and/or conference presentations. Agendas also included brain-storming, discussion of specific challenges, and other planning. Given the complexity, sensitivity, and potential for legitimately diverging views that can emerge in discussion, it was essential to maintain respectful and empathic attitudes towards one another and the participants. This entailed developing trust in the skills, experience and objectives of all group members. A supportive, respectful conversational tone that reinforced strong working relationships characterized the research meetings. Whereas meetings were generally structured, based on the agenda, they were sufficiently flexible to accommodate the personal experiences of working together and new issues as they arose. The use of humor in discussions facilitated tolerance of different perspectives and a shared sense of purpose even when situations might elicit challenges or stress. Subgroups met, as needed, to address specific aspects of the study.
Overcoming Barriers of Interdisciplinary Collaboration
Our team worked diligently to surmount barriers to interdisciplinary collaboration. One essential part was choosing team members who worked together harmoniously. The PI of this research team had years of experience leading interdisciplinary teams and used his judgment when selecting new members. He modeled a respectful and supportive interpersonal tone, along with a problem-solving focus for the meetings. Ensuring adequate time to accomplish intermediate and longer term objectives was achieved principally by having members commit to two 60–90 minute research meetings per month, or more if necessary during peak periods of activity. Since team members also had clinical and educational obligations, this planning maximized the likelihood that team members could adjust their schedules to attend.
Another potential barrier addressed within the research team was role ambiguity. This barrier was prevented by discussing and clarifying the expectations of roles and in assigning work to team members who were the most qualified, appropriately funded, or otherwise prepared to complete it. The PI guided discussions of the research tasks and designated team members responsible for completing specific tasks. Ambiguity in determining whom to approach with upcoming responsibilities was resolved by contacting the PI between meetings as well as in team meetings.
Another challenge that was encountered was technological complexity. Team members were selected based on their professional and personal qualities and skill sets to perform their responsibilities effectively. Constituting a team with members with varied areas of expertise, facilitated members effectively troubleshooting problems that might otherwise be more frustrating or derailing, and increased the likelihood that technologies were utilized to their reasonably full capability. It also allowed for scientific issues, such as research design, statistical power, etc. to be dealt with effectively early within research processes to minimize the prospect of inadvertent errors in research approaches.
Finally, the research team embraced professional cultural differences among the participating disciplines. Open communication was encouraged to better understand the relative strengths and differences in approaches and perspectives among professions. In general, the focus was on the work at hand. However, diverse topics, including cultural, educational, ethical, and professional differences were, at times, discussed. Strong leadership complemented the respectful dialogue to prevent miscommunications and interdisciplinary tensions.
Promoting successful team dynamics is important for creating positive work environments as well as maximizing the productivity of interdisciplinary research teams. Achieving an appropriate team size (i.e., not too big and not to small) for sharing the workload burdens, while empowering appropriate levels of individual autonomy, supports positive interactions and promotes motivation throughout the team. It is also important that the team membership remain relatively constant. The PI strove to minimize the rate of change of personnel, and to ensure that when membership did change, the work flow and positive interpersonal climate endured within the team. To further complement this dynamic, team members focused on a larger picture of what they each brought to the research enterprise beyond their background, titles, or relative professional status. The co-investigators worked closely with the PI to help direct the study while maintaining their own professional autonomy and outside commitments. Such efforts contributed to team members feeling valued and perceiving their contributions as appreciated. This allowed them to take pride in their unique contributions to the full gestalt of the team effort. By creating a safe and harmonious team environment, team members communicated their thoughts and feelings non-defensively, and enjoyed the interpersonal rewards of a free-flowing and professional exchange. This allowed for robust conversations and sharing of ideas based on diverging areas of both research and clinical expertise.
DISCUSSION
Although the goals, processes, and challenges of research may have distinct features, the key components of successful interdisciplinary collaboration in research are similar to those in other organizations and undertakings. Thus, an interdisciplinary framework may offer guidance for collaboration in the work of critical care nurses whether or not research is part of the scope of individuals’ work. The attributes of interdisciplinary collaboration may be broadly relevant, including the creation and maintenance of strong work relationships, focus on a shared sense of purpose, delegation of tasks to appropriate team members, effective conflict resolution, recognition of professional differences, clarification of roles, and organized approaches to surmounting barriers (e.g., time, funding, other resources, technology, professional, academic challenges). Solid working relationships are essential to team members’ appreciation of each other’s contributions and shared enthusiasm in striving to fulfill scientific objectives. A harmonious interpersonal and interdisciplinary climate offers the potential to maximize productivity and the quality of the work.
As in other complex human endeavor, strong leadership is a foundation of interdisciplinary research. The PI and other team leaders need a clear understanding of the range of skills and expertise needed to accomplish goals, how to screen for it and nurture it within individuals, and what potential contributions specific disciplines bring to the research team. Clarification of team roles and expectations (i.e., what needs to get done, when, by whom, and in what manner) increases the likelihood the team will be successful. Ensuring adequate training for team members in the conduct of research and in dealing with the clinical populations, as well as managing technology and other resource needs is necessary. The PI’s portfolio of responsibilities in conducting interdisciplinary research also includes addressing IRB reviews, funding, regulatory compliance, human resources, and a plethora of administrative and potentially academic issues, as well as monitoring and documenting progress toward research goals. This requires broad knowledge and coordination of various academic entities (e.g., academic health center schools, academic departments) as well as funding agency regulations and processes.
In summary, the interpersonal substrate for interdisciplinary research collaboration comprises diverse components, especially strong communication skills in the PI and other team members across disciplines. An effort to develop strengths within the team and problem-solving for barriers to functional team dynamics may result in minimal disruption to the work flow and help achieve positive outcomes.
The promise of interdisciplinary research is that it has the potential to yield greater scientific contributions than that which can be produced by any specific discipline alone. Arguably, key building blocks to scientific collaboration include the same interpersonal harmony and constructive communication processes inherent in other effectively functioning groups. Interdisciplinary collaborations that fail to produce useful, efficient, creative, or meaningful outcomes relative to what may have been produced by a researcher working independently, raise questions of whether “collaboration” truly occurred and of what barriers or failures within the workgroup may have limited its achievement. The success of interdisciplinary collaboration may be judged both on the soundness of the processes that are inherent within it and on the outcome(s) it produces. Interdisciplinary collaboration that effectively harnesses the strengths and talents of individuals into working teams provides a framework and means of creating a whole that exceeds the sum of its parts.
Highlights.
The purpose of this paper to provide an overview of attributes of effective interdisciplinary collaboration and to identify barriers to its realization in patients undergoing lung transplantation.
Collaborative practice and research in health sciences may involve full-time researchers as well as part-time researchers who also have demanding clinical practices.
The promise of interdisciplinary research is that is has the potential to yield great scientific contributions than that which can be produced by any specific discipline alone.
Acknowledgments
This work was supported in part by NIH grant RO1NR009212
Biographies
Arin VanWormer, PhD, MS, RN is an Assistant Professor of Nursing at the University of Wisconsin - Eau Claire. She has practiced in CCU and SICU.
Ruth Lindquist, PhD, RN, ACNS-BC, FAAN is a professor of Nursing at the University, a Medical-Surgical Clinical Nurse Specialist, and Research Consultant to the Minneapolis Heart Institute at Abbott Northwestern Hospital and Minneapolis Heart Institute Foundation. She has practiced in CCU and SICU.
William Robiner, Ph.D., A.B.P.P. is professor in the Departments of Medicine and Pediatrics and Director of Heath Psychology at the University of Minnesota Medical School.
Stanley Finkelstein PhD, is a Professor of Laboratory Medicine and Pathology in the Medical School and a core faculty member in the Institute of Health Informatics in the Academic Health Center, University of Minnesota. He is a Fellow of the American Institute of Medical and Biological Engineering. He has directed research programs in patient remote monitoring and home telehealth for the past 25 years.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Arin VanWormer, University of Wisconsin - Eau Claire, College of Nursing and Health Sciences, 105 Garfield Ave, 214 Nursing Building, Eau Claire, WI 54702, (p) 715-836-3588; vanworag@uwec.edu.
Ruth Lindquist, University of Minnesota, School of Nursing, 5-140 WDH,308 Harvard Street SE, MPLS, MN 55455, (p) 612-624-5646; (f) 612-625-7180; lindq002@umn.edu.
William Robiner, Department of Medicine and Pediatrics Health Psychology, Departments of Medicine, University of Minnesota Medical School, Mayo Mail Code 741, 420 Delaware Street, MPLS, MN 55455, (p) 612-624-1479; robin005@umn.edu.
Stanley Finkelstein, University of Minnesota, Department of Laboratory Medicine and Pathology, MMC 609, 420 Delaware Street, MPLS, MN 55455, (p) 612-625-6406; stan@umn.edu.
REFERENCES
- 1.Kahn RL, Prager DJ. Interdisciplinary collaborations are a scientific and social imperative. Scientist. 1994;8:12. [Google Scholar]
- 2.National Institutes of Health. Research Teams of the Future. Available at: http://commonfund.nih.gov/researchteams/ Accessed July 30, 2011.
- 3.Morgan GD, Kobus K, Gerlach KK, Neighbors C, Lerman C, Abrams DB, et al. Facilitating transdisciplinary research: The experience of the transdisciplinary tobacco use research centers. Nicotine Tob Res. 2003;5 Suppl 1:S11–S19. doi: 10.1080/14622200310001625537. [DOI] [PubMed] [Google Scholar]
- 4.Fewster-Thuente L, Velsor-Friedrich B. Interdisciplinary collaboration for healthcare professionals. Nurs Admin Quart. 2008;32:40–48. doi: 10.1097/01.NAQ.0000305946.31193.61. [DOI] [PubMed] [Google Scholar]
- 5.Joint Commission on Accreditation of Healthcare Organizations. The Joint Commission guide to improving staff communication. Oakbrook Terrace, IL: Joint Commission Resources; 2005. [Google Scholar]
- 6.Revere A, Eldridge N. JCAHO National Patient Safety Goals for 2007. Available at: http://www.patientsafety.gov/TIPS/Docs/TIPS_JanFeb07.pdf. Accessed July 30, 2011.
- 7.Nash JM. Transdisciplinary training: Key components and prerequisites for success. Am J Prevent Med. 2008;35 Suppl 2:S133–S140. doi: 10.1016/j.amepre.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell PH, Crittenden RA. Interdisciplinary collaboration: Old ideas with new urgency. Wash Publ Health. 2000 Fall;:1–3. [Google Scholar]
- 9.Horwitz AR. Building bridges through collaboration: A pathway for interdisciplinary research. Trends Cell Biol. 2003;13:2–3. doi: 10.1016/s0962-8924(02)00003-x. [DOI] [PubMed] [Google Scholar]
- 10.Kessel F, Rosenfield PL, Anderson NB. Interdisciplinary research: Case studies from health and social science. NY: Oxford University Press; 2008. [Google Scholar]
- 11.Kozlowski WJ, Ilgen DR. Enhancing the Effectiveness of Work Groups and Teams. Psychol Sci Publ Int. 2006;7:77–124. doi: 10.1111/j.1529-1006.2006.00030.x. [DOI] [PubMed] [Google Scholar]
- 12.Nash JM, Collins BN, Loughlin SE, Solbrig M, Harvey R, Krishnan-Sarin S, et al. Training the transdisciplinary scientist: A general framework applied to tobacco use behavior. Nicot Tobac Res. 2003;5 Suppl 1:S41–S53. doi: 10.1080/14622200310001625528. [DOI] [PubMed] [Google Scholar]
- 13.Gebbie KM, Meier BM, Bakken S, Carrasquillo O, Formicola A, Aboelela SW, et al. Training for interdisciplinary health research: Defining the required competencies. J Allied Health. 2008;37:65–70. [PubMed] [Google Scholar]
- 14.McGuire DB. Building and maintaining an interdisciplinary research team. Alz Dis Assoc Dis. 1999;13 suppl 1:S17–S21. doi: 10.1097/00002093-199904001-00006. [DOI] [PubMed] [Google Scholar]
- 15.Torres GW, Margolin FS. The collaboration primer: Proven strategies, considerations and tools to get you started. Chicago: Health Research & Educational Trust; 2003. [Google Scholar]
- 16.Drotar D. Reflections on interdisciplinary collaboration in the new millennium: Perspectives and challenges. J Dev Behav Pediatr. 2003;3:175–180. doi: 10.1097/00004703-200206000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Wells ND, Johnson R, Salyer S. Interdisciplinary collaboration. Clin Nurse Spec. 1998;12:161–168. doi: 10.1097/00002800-199807000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Aboelela SW, Larson E, Bakken S, Carrasquillo O, Formicola A, Glied SA, et al. Defining interdisciplinary research: Conclusions from a critical review of the literature. Health Serv Res. 2007;42:329–346. doi: 10.1111/j.1475-6773.2006.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grey M, Connolly CA. Coming together, keeping together, working together: Interdisciplinary to transdisciplinary research and nursing. Nurs Outlook. 2008;56:102–107. doi: 10.1016/j.outlook.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 20.Heitkemper M, McGrath B, Killien M, Jarrett M, Landis C, Lentz M, et al. The role of centers in fostering interdisciplinary research. Nurs Outlook. 2008;56:115–122. doi: 10.1016/j.outlook.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 21.Kevin LG, Cunningham AJ. Interdisciplinary collaboration in anesthesia research. British J Anaesth. 2002;89:658–659. doi: 10.1093/bja/aef555. [DOI] [PubMed] [Google Scholar]
- 22.McDaniel AM, Champion VL, Kroenke K. A transdisciplinary training program for behavioral oncology and cancer control scientists. Nurs Outlook. 2008;6:123–131. doi: 10.1016/j.outlook.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weaver TE. Enhancing multiple disciplinary teamwork. Nurs Outlook. 2008;56:108–114. doi: 10.1016/j.outlook.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 24.Koch L, Egbert N, Coeling H. Speaking of research: The working alliance as a model for interdisciplinary collaboration. Work. 2005;5:369–373. [PubMed] [Google Scholar]
- 25.Koch LC, Rumrill PD. The working alliance: An interdisciplinary case management strategy for health professionals. Work. 1998;10:55–62. doi: 10.3233/WOR-1998-10109. [DOI] [PubMed] [Google Scholar]
- 26.Wiley S. Collaborations: Challenging, but key. Scientist. 2009;23:29. [Google Scholar]
- 27.D’Zurilla TJ. Problem solving therapy: A social competence approach to clinical intervention. 2nd ed. NY: Springer; 1999. [Google Scholar]
- 28.Tuckman BW. Developmental sequence in small groups. Psychol Bull. 1965;3:384–399. doi: 10.1037/h0022100. [DOI] [PubMed] [Google Scholar]
- 29.Lacoursiere RB. The life cycle of groups. NY: Human Science Press; 1980. [Google Scholar]
- 30.Finkelstein SM, Ratner E. Managing chronic disease through home telehealth. Minn Med. 2006;9:42–45. [PubMed] [Google Scholar]
- 31.Snyder M, Chlan L, Finkelstein SM, Sabati N, Edin-Stibbe C. Home monitoring of pulmonary function. Home Healthcare Nurs. 1998;6:388–393. [PubMed] [Google Scholar]
- 32.Finkelstein S, Scudiero A, Lindgren B, Snyder M, Hertz MI. Decision support for the triage of lung transplant recipients on the basis of home monitoring spirometry and symptom reporting. Heart Lung. 2005;34:201–208. doi: 10.1016/j.hrtlng.2004.09.003. [DOI] [PubMed] [Google Scholar]