Abstract
Radicular cysts arising from deciduous teeth are rare. This report presents a case of radicular cyst associated with a primary molar following pulp therapy and discusses the relationship between pulp therapy and the rapid growth of the cyst. The treatment consisted of enucleation of the cyst sac and extraction of the involved primary teeth and 20 months follow up of the patient. Early diagnosis of the lesion would have lead to a less aggressive treatment plan.
Keywords: Reticular cyst, Primary molar, Pulpotomy
INTRODUCTION
Radicular and residual cysts are the most common cystic lesions of the jaws, but radicular cysts are relatively rare in the primary dentition because of the distinct biological cycle of primary teeth. The frequency of radicular cysts in permanent dentition is about 7–54%, while in primary dentition this figure is approximately 0.5–3.3% of the total number of radicular cysts in both the primary and permanent dentition [1–3]. Most radicular cysts of the primary dentition are associated with mandibular molars [3]. Radicular cysts originate from epithelial remnants of the periodontal ligament as a result of inflammation and associated infiltration of inflammatory cells which is generally a consequence of pulp necrosis. These cysts commonly involve the apex of the affected tooth [4]. It seems that caries are the most frequent etiologic factor associated with radicular cysts in primary dentition [3]. Most reported cases of radicular cysts were in molar teeth with apical infection caused by caries. It has been reported that radicular cysts associated with primary incisor teeth are very rare [5,6]. Pulp therapy is recommended for treatment of primary teeth with pulpitis or apical periodontitis. Side effects of pulp therapy treatments may include cyst formation, delayed eruption or enamel defects of permanent successor teeth. It seems that there may be a relationship between the intracanal medicaments used for pulp therapies and the distinctive intraepithelial inclusions which are found in cyst walls that may provide a site for prolonged antigenic stimulation [3,5,7].
Cyst formation in children may cause bony expansion and resorption, delayed eruption, malposition, enamel defects or damaging of the developing permanent successors [3,8,9]. One of the most suitable treatment options for these cases is complete enucleation of the cyst with extraction of the associated primary teeth and preservation of the permanent teeth. In most cases normal alignment of the permanent teeth will occur spontaneously even if their initial positions are very unfavorable [10,11].
CASE REPORT
A healthy 5-year-old boy was referred to the pediatrics department of Shahid Beheshti School of Dental Medicine, Tehran, Iran, with the chief complaint of a painful swelling located in the mandibular left buccal region (Fig 1).
Figure 1.
2×2 cm expansion of the buccal cortical plate is seen in the left mandibular buccal region.
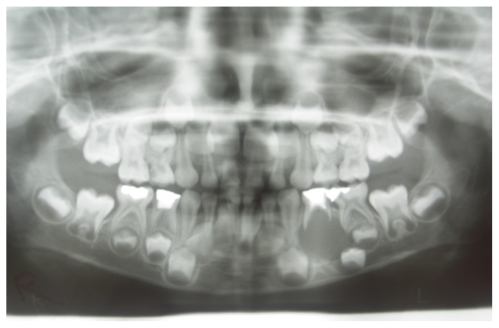
The patient’s dental history indicated that the first primary molar had received conventional pulpotomy treatment one year before and the left second primary molar had a defective Class II amalgam filling with recurrent caries. Clinical examination revealed marked grade I mobility of the mandibular left first primary molar and a palpable expansion of the buccal plate with crepitus on the mandibular left primary molar region extending 2×2 cm. The panoramic radiograph showed a round radiolucent unilocular lesion with smooth and well defined borders, extending 22×23 mm in the periapical area of the mandibular left primary first molar. The expansion of the lesion had pushed the permanent first bicuspid very close to the lower border of the mandible (Fig 2). Based on the patient’s history and clinical and radiographic examinations, the differential diagnosis of the lesion was radicular cyst or dentigerous cyst and the treatment plan was surgical enucleation of the lesion. Other treatments required for the patient consisted of pulpotomy and restoration of teeth number A, B, I, J, K and T, extraction of tooth number S and band and loop space maintainer to maintain the E space in the mandible.
Figure 2.
Panoramic radiograph shows a well-defined radiolucency in the periapical area of the mandibular left primary first molar.
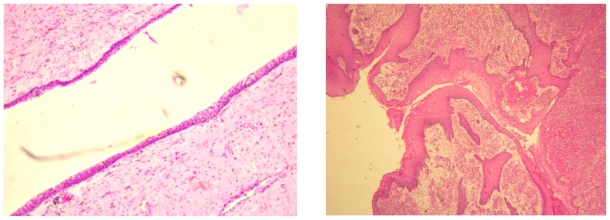
Consent form was signed by the patient’s parents and the patient was scheduled for the surgery. At the day of surgery, standard disinfection protocols were followed and the area was anesthetized by block and infiltration injection of Lidocaine HCl with 1:100000 epinephrine. Initially, a needle biopsy was taken from the lesion and the result of aspiration was a light-yellow odorless liquid that was immediately sent to lab for cytopathologic evaluation. The results approved the cystic nature of the lesion. An incision was made from the left canine to the left second primary molar along the gingival margin and the site was exposed. The buccal cortical plate was considerably thin at the area over the lesion that had to be removed, but the lingual plate was left intact. The cystic lining was then enucleated and was sent for histopathologic examination. A decision was made by the surgeon and the pediatric dentist at the time of surgery to extract the first primary molar because it was involved with cystic lining and the prognosis was considered to be very poor. The surgical site was then rinsed with normal saline and after the bleeding was controlled, the flap was sutured back and primary closure was achieved. The patient was advised to use iboprufen 200mg every 4 hours in case of pain until pain relief. Seven days later, the patient came back for post-surgical examination and suture removal. The histopathologic features were inconsistent with the clinical diagnosis of radicular cyst. The cystic cavity was lined by varying thickness of nonkeratinized stratified squamous epithelium with arch shaped appearance and exocytosis in the underlying connective tissue that was severely infiltrated by chronic inflammatory cells. Extravasated RBCs, hemosiderin pigments and Russell bodies were also seen (Fig 3). At 3 months recall, clinical and radiographic examination was performed to evaluate the healing process (Fig 4). Oral examination revealed good healing of soft tissues and radiographic examination showed that the bony lesion seemed to be healing and there was reduction in size compared to the preoperative radiographs. The first bicuspid was also in an improved position. The patient was then scheduled for the remaining required dental treatment and was also referred to an orthodontist for orthodontic evaluation. At 20 months recall radiographic and clinical evaluations indicated successful treatment (Fig 5).
Figure 3.
Varying thickness of nonkeratinized stratified squamous epithelium with arch shaped appearance is evident (H&E staining, 40x magnification).
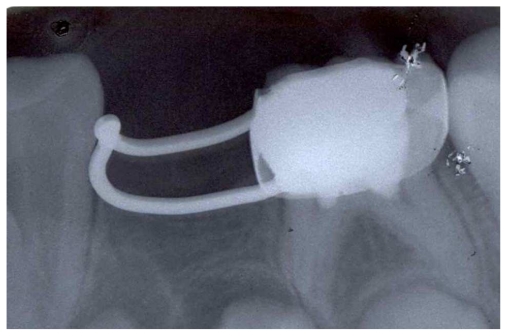
Figure 4.
Periapical radiograph 3 months after surgery
Figure 5.
Periapical radiograph 20 months after surgery
DISCUSSION
It has been believed that radicular cysts arise from the epithelial remnants in the periodontal ligament as a result of inflammation [8]. Although these pathologic lesions in children are considered to be rare, some factors may cause an underestimation of the real prevalence of these lesions. Usually periapical radiolucencies related to primary teeth are neglected and in many cases they resolve after tooth extraction [12]. Many radicular cysts are asymptomatic and are discovered when periapical radiographs are taken. Pulp and inter radicular infections in primary teeth have a tendency to drainage more than permanent teeth [8,12,13]. In fact pulp therapy of primary teeth does not always have good prognosis [14,15] and is affected by many factors such as root canal curves, presence of accessory canals and root resorptions. In some cases after pulp therapy, pulp and periradicular inflammation steadily progresses without any signs or symptoms; thus, long term follow-up of these treatments in primary teeth is essential [16]. Most radicular cysts in the primary dentition are associated with mandibular molars with extensive dental caries [3], but it may happen in maxillary primary molars too [17]. Periapical radiolucencies of primary teeth may be misdiagnosed as a periapical granuloma or a dentigerous cyst of the permanent successor. Dentigerous cysts are characterized by a well-defined unilocular radiolucency in the pericoronal area of an un-erupted permanent tooth and cortical margins are continuous with the follicle at the cemento-enamel junction of the permanent tooth [1,13]. The common signs of radicular cysts are expansion of the buccal cortical plate, well-defined radiolucency, thin reactive cortex and displacement of permanent successor teeth [8]. In the present case, a preoperative diagnosis of dentigerous cyst was made, but during the surgical procedure, no association between the cystic lining and the follicle of the first permanent premolar was found. After histopathologic examination, the final diagnosis was made as radicular cyst. Hill reported that the growth rate of a radicular cyst in the primary dentition is approximately 4 mm each year [18]. In our report, the growth rate appeared to be faster. Intracanal medicaments used for pulpotomy have been mentioned as possible stimulating factors for rapid growth of the cysts [13]; but in our case, since pulpotomy of the left mandibular first primary molar was performed in a private office, no information was available about the materials and no judgments could be made regarding this matter. On the other hand, Grundy et al. has mentioned that pulp therapeutic agents may produce antigenic and necrotic products in the root canal system which may act as an antigenic stimulant for the peri radicular region. Considering the extremely low incidence of radicular cysts and its unknown correlation with pulp therapeutic agents, prohibition of pulp treatment of the primary teeth still could not be recommended [19]. As mentioned earlier, complete enucleation of the cyst and preservation of the permanent successor teeth is recommended as the most suitable treatment option in these cases [8,10,11]. Marsupialization of the cystic lesion and using a resin appliance with projection for decompressing the lesion is a more conservative treatment technique [12,17]. In these cases, the patients’ and parents’ cooperation is needed for success of treatment and long term follow ups are mandatory.
CONCLUSION
The reported case is one of the rare occasions of radicular cyst occuring in primary dentition in a similar pattern to the earlier reports.
Early diagnosis proves very important, and regular clinical and radiographic follow up for pulp treated primary teeth is strongly recommended.
REFERENCES
- 1.Neville B, Damm D, Allen C, Bouquot J. Oral and Maxillofacial Pathology. 3rd ed. Chapter 3 Elsevier; 2008. [Google Scholar]
- 2.Bhaskar SN. Oral surgery--oral pathology conference No. 17, Walter Reed Army Medical Center. Periapical lesions--types, incidence, and clinical features. Oral Surg Oral Med Oral Pathol. 1966 May;21(5):657–71. doi: 10.1016/0030-4220(66)90044-2. [DOI] [PubMed] [Google Scholar]
- 3.Mass E, Kaplan I, Hirshberg A. A clinical and histopathological study of radicular cysts associated with primary molars. J Oral Pathol Med. 1995 Nov;24(10):458–461. doi: 10.1111/j.1600-0714.1995.tb01134.x. [DOI] [PubMed] [Google Scholar]
- 4.Shear M, Speight P. Cysts of the oral region. 4th ed. Copenhagen: Wiley-Black well Munksgaard; 2007. Radicular and residual cysts; pp. 123–42. [Google Scholar]
- 5.Lustmann J, Shear M. Radicular cysts arising from deciduous teeth. Review of the literature and report of 23 cases. Inter J Oral Surg. 1985 Apr;14(2):153–61. doi: 10.1016/s0300-9785(85)80087-9. [DOI] [PubMed] [Google Scholar]
- 6.Smith AT, Cowpe JG. Radicular cyst arising from a traumatized primary incisor: a case report of a rare complication that emphasizes the need for regular follow up. Dent Update. 2005 Mar;32(2):109–10. 113. doi: 10.12968/denu.2005.32.2.109. [DOI] [PubMed] [Google Scholar]
- 7.Savage NW, Adkins KF, Weir AV, Grundy GE. A histological study of cystic lesions following pulp therapy in deciduous molars. J Oral Pathol. 1986 Apr;15(4):209–12. doi: 10.1111/j.1600-0714.1986.tb00609.x. [DOI] [PubMed] [Google Scholar]
- 8.Ramakrishna Y, Verma D. Radicular cyst associated with a deciduous molar: A case report with unusual clinical presentation. J Indian Soc Pedod Prev Dent. 2006 Sep;24(3):158–60. doi: 10.4103/0970-4388.27899. [DOI] [PubMed] [Google Scholar]
- 9.Caldwell RE, Freilich MM, Sandor GK. Two radicular cysts associated with endodontically treated primary teeth: rationale for long-term follow-up. Ont Dent. 1999 Oct;76(8):29–33. [PubMed] [Google Scholar]
- 10.Gandhi S, Franklin DL. Presentation of a radicular cyst associated with a primary molar. Eur Arch Paediatr Dent. 2008 Mar;9(1):56–9. doi: 10.1007/BF03321598. [DOI] [PubMed] [Google Scholar]
- 11.Chiu WK, Sham AS, Hung JN. Spontaneous alignment of permanent successors after enucleation of odontogenic cysts associated with primary teeth. Br J Oral Maxillofac Surg. 2008 Jan;46(1):42–5. doi: 10.1016/j.bjoms.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 12.Delbem AC, Cunha RF. Conservative treatment of a radicular cyst in a 5-year-old child: a case report. Int J Paediatr Dent. 2003 Nov;13(6):447–50. doi: 10.1046/j.1365-263x.2003.00452.x. [DOI] [PubMed] [Google Scholar]
- 13.Eidelman E, Holan G, Fuks AB. Mineral trioxide aggregate vs. formocresol in pulpotomized primary molars: a preliminary report. Pediatr Dent. 2001 Jan-Feb;23(1):15–8. [PubMed] [Google Scholar]
- 14.Patchett CL, Srinivasan V, Waterhouse PJ. Is there life after Buckley’s formocresol? Part II - Development of a protocol for the management of extensive caries in the primary molar. Int J Paediatr Dent. 2006 May;16(3):199–206. doi: 10.1111/j.1365-263X.2006.00687.x. [DOI] [PubMed] [Google Scholar]
- 15.Yawaka Y, Kaga M, Osanai M, Fukui A, Oguchi H. Delayed eruption of premolars with periodontitis of primary predecessors and a cystic lesion: a case report. Int J Paediatr Dent. 2002 Jan;12(1):53–60. doi: 10.1046/j.0960-7439.2001.00323.x. [DOI] [PubMed] [Google Scholar]
- 16.Johann AC, Gomes Cde O, Mesquita RA. Radicular cyst: a case report treated with conservative therapy. J Clin Pediatr Dent. 2006 Fall;31(1):66–7. doi: 10.17796/jcpd.31.1.p721888v762270h3. [DOI] [PubMed] [Google Scholar]
- 17.Takiguchi M, Fujiwara T, Sobue S, Ooshima T. Radicular cyst associated with a primary molar following pulp therapy: a case report. Int J Paediatr Dent. 2001 Nov;11(6):452–5. [PubMed] [Google Scholar]
- 18.Hill FJ. Cystic lesions associated with deciduous teeth. Proc Br Paedod Soc. 1987;8:9–12. [PubMed] [Google Scholar]
- 19.Grundy GE, Adkins KF, Savage NW. Cysts associated with deciduous molars following pulp therapy. Aust Dent J. 1984 Aug;29(4):249–56. doi: 10.1111/j.1834-7819.1984.tb06067.x. [DOI] [PubMed] [Google Scholar]