Abstract
Background
Primary care providers (PCPs) in safety net settings face barriers to optimizing care for patients with diabetes. We conducted this study to assess PCPs' perspectives on the effectiveness of two language-concordant diabetes self-management support programs.
Methods
One year postintervention, we surveyed PCPs whose patients with diabetes participated in a three-arm multiclinic randomized controlled trial comparing usual care (UC), weekly automated telephone self-management (ATSM) support with nurse care management, and monthly group medical visits (GMVs). We compared PCP perspectives on patient activation to create and achieve goals, quality of care, and barriers to care using regression models accounting for within-PCP clustering.
Results
Of 113 eligible PCPs caring for 330 enrolled patients, 87 PCPs (77%) responded to surveys about 245 (74%) enrolled patients. Intervention patients were more likely to be perceived by PCPs as activated to create and achieve goals for chronic care when compared with UC patients (standardized effect size, ATSM vs UC, +0.41, p = 0.01; GMV vs UC, +0.31, p = 0.05). Primary care providers rated quality of care as higher for patients exposed to ATSM compared to UC (odds ratio 3.6, p < 0.01). Compared with GMV patients, ATSM patients were more likely to be perceived by PCPs as overcoming barriers related to limited English proficiency (82% ATSM vs 44% GMV, p = 0.01) and managing medications (80% ATSM vs 53% GMV, p = 0.01).
Conclusions
Primary care providers perceived that patients receiving ATSM support had overcome barriers, participated more actively, and received higher quality diabetes care. These views of clinician stakeholders lend additional evidence for the potential to upscale ATSM more broadly to support PCPs in their care of diverse, multilinguistic populations.
Keywords: chronic disease care, health disparities, health literacy, limited English proficiency, self-management, underserved population
Introduction
Primary care providers (PCPs) face numerous barriers to optimizing care for patients with chronic medical conditions, particularly in settings serving vulnerable populations for whom social conditions promote chronic diseases and make their management more challenging.1,2 In a study of working conditions in clinics caring for patients with diabetes, hypertension, and congestive heart failure, half of PCPs reported time pressure during visits and chaotic work pace, and over a quarter reported burnout.2 Meanwhile, PCPs in clinics serving higher proportions of minority populations cared for more patients with high medical and psychosocial complexity, limited English proficiency, and limited health literacy, but reported less access to resources for chronic disease care.1 Delivering care in such underresourced, chaotic working conditions may leave PCPs at higher risk for burnout,2 with implications for workforce retention in safety net settings caring for uninsured, Medicaid, and other vulnerable patients with high needs.3
Self-management support (SMS) programs offer crucial systems-level strategies to offset the challenges PCPs face in delivering chronic disease care, while also improving outcomes in chronic disease, by providing individualized assessment, collaborative goal setting, skills enhancement, follow-up, and access to resources and continuity of care.4–6 A variety of different strategies has proven successful in promoting patient self-management of chronic medical conditions.7,8 Sarkar and colleagues9 found that patients in safety net settings with limited English proficiency and limited health literacy are interested in accessing SMS. Primary care providers play a key role in integrating SMS into chronic disease care delivery, and PCPs who perceive that SMS programs are not effective or accessible to their patients may be less likely to employ these resources for their patients.10–12 Primary care providers may be ambivalent about the importance and benefits of SMS and concerned about sharing responsibility for disease management with other professional educators or even with patients them-selves.12–14 However, favorable attitudes may increase the likelihood that they will recommend SMS programs to their patients, particularly if those systems provide useful information about patients' concerns and behaviors in a manner integrated within patient-centered medical homes.
In the current health care reform environment, PCPs in safety net settings are also grappling with the potential promises and pitfalls of health information technology (HIT) as a tool for chronic disease self-management. In response to Medicaid and Medicare incentives arising from the 2009 Health Information Technology for Economic and Clinical Health Act, safety net settings are required to integrate electronic health records into the care environment and must strive to meet “meaningful use” criteria, including patient education and tracking of quality indicators.15–17 With these additional opportunities and pressures, it is important to understand how providers perceive the potential benefits of HIT in assisting with chronic disease care and patient self-management.
Automated telephone self-management (ATSM) is an example of a HIT tool (telehealth or use of telecommunications technologies to deliver health-related services) that can assist with SMS in chronic disease care.18 In our three-arm, practice-based trial comparing group medical visits (GMVs), ATSM, and usual care (UC) for patients with poorly controlled diabetes, we found that low income, linguistically diverse patients had high levels of engagement with both SMS strategies, resulting in improvements in their assessment of their chronic disease care and diabetes self-efficacy.19,20 Although they experienced no differences in glycemic control, patients exposed to ATSM had greater improvements in self-management behavior, fewer bed days per month, and less interference in their daily activities, with a cost utility for functional outcomes comparable to other diabetes prevention and treatment interventions.20,21
We conducted this study to compare PCPs' perspectives on the effectiveness of these two strategies on improving quality of care and self-management for linguistically diverse persons with diabetes.
Methods
The Improving Diabetes Efforts across Language and Literacy (IDEALL) project was an initiative to improve diabetes care in a practice-based research network that includes the Community Health Network of San Francisco (CHNSF), the integrated delivery system of the San Francisco Department of Public Health.19–21
Intervention
Patients were randomized to one of three study arms for 9 months (see Appendix A):
Usual care provided by patients' primary care clinics
Automated telephone self-management support with nurse care management, as an adjunct to UC
Group medical visits with physician and health educator facilitation, as an adjunct to UC.
Patients in the ATSM arm received weekly automated telephone calls during which they received prerecorded health education messages and a rotating set of questions regarding their self-management behaviors and health status. Depending on how a patient responded to a query, the patient heard a different automated health education message in the form of a narrative tailored to that response. Prespecified out-of-range responses also triggered subsequent phone calls from a nurse care manager. Of 112 patients in the ATSM arm, 94% completed ≥ 1 ATSM call (mean = 22 of 39 weeks) and 95% received ≥ 1 care manager call back (mean = 9.2).20
The GMV arm consisted of 90 min monthly sessions with 6–10 participants. All patient interactions with ATSM care managers or GMV cofacilitators, including action plans created and achieved, were communicated with PCPs. Of 113 patients in the GMV arm, 69% attended ≥ 1 GMV (mean = 4.8 of 9 visits).20
Patients in the UC group and in both intervention groups received standard diabetes care provided by their PCPs and any diabetes education, nutritional counseling, or subspecialty endocrinology care that was recommended by their PCPs. While PCPs were responsible for medical care in both the UC and intervention groups, they had no role in the interventions, neither participating in the group visits nor supervising care managers completing follow-up phone calls for ATSM triggers.
Eligible participants were English-, Spanish-, or Cantonese-speaking adults with type 2 diabetes, a most recent hemoglobin A1c (HbA1c) ≥ 8.0%, and ≥ 1 primary care visit at one of the four participating CHNSF clinics. Before enrollment, PCPs excluded patients who died, moved away, had moderate to severe dementia, or whom they did not expect to live through the year. Of note, 86% of eligible patients were deemed eligible by clinicians.19 Research assistants excluded patients who planned to travel more than 3 months during the intervention; were too ill or unable to travel to a GMV; lacked phone access; or were unable to hear, see, or follow instructions using a telephone keypad. Detailed descriptions of interventions, patient eligibility, and recruitment are available.19
Study Design and Sample Population
At 1 year after patient enrollment, we conducted a survey of each patient's PCP. Eligible PCPs were physicians, resident physicians, nurse practitioners, or physician assistants providing primary care for at least one patient participating in the trial. Primary care providers were not blinded to the assignment of their patients. The first survey for each PCP also collected provider demographic data.
Data Collection
In 2006, PCP participants received written questionnaires by mail, with email reminders. Primary care providers completed one questionnaire for each patient participant in the study, as well as a one-time questionnaire about their personal characteristics such as gender, years of practice, size of primary care panel, and proportion of patients with diabetes in their panel.
Patient engagement, activation, and goal setting in diverse patient populations have been associated with improved self-management behaviors (including medication adherence) and medical outcomes, including HbA1c and patient satisfaction with PCPs and care.6,22–24 So, for patients assigned to any arm, PCPs responded to the following items:
How much more or less likely is your patient to engage in health-related goal setting (e.g., diet, exercise, etc.) now, compared to 1 year ago? (1 = “much less likely” to 5 = “much more likely”)
How much more or less of an active role do you think your patient is playing in taking care of his or her diabetes now, compared to 1 year ago? (1 = “much less likely” to 5 = “much more likely”)
How would you rate the overall quality of diabetes care your patient received in the last 12 months? (5= “excellent,” 4 = “very good,” 3 = “good,” 2 = “fair,” 1 = “poor”)
Primary care providers indicated whether ATSM and/or GMV should be expanded to more patients with diabetes or patients with other chronic illnesses, such as asthma, heart failure, and depression.
Finally, on the patient-specific questionnaire, PCPs reported their agreement (1 = “strongly agree” to 5 = “strongly disagree”) that patients were affected by 13 potential barriers to diabetes care, as drawn from the literature about chronic disease care in safety net settings.5,25–30 For patients in the intervention arms only, PCPs reported the extent to which they agreed (1 = “strongly agree” to 5 = “strongly disagree”) that the intervention (ATSM or GMV) helped their patient overcome these barriers.
Primary care provider participants received a $5 coupon for a local coffee shop. The study was approved by the Institutional Review Board of the University of California, San Francisco.
Data Analysis
Most questionnaire items were patient-specific and were analyzed at the patient level, controlling for PCP-clustering in regression analyses. For items about PCP attitudes in general (whether ATSM and/or GMV should be expanded), we collected only one response for each PCP and analyzed data at the PCP level.
To test for differences in perceived patient activation, we summed the response for the items related to goal setting and taking an active role (range 2–10) and compared ATSM, GMV, and UC by calculating standardized effect sizes using logistic regression models accounting for within-PCP clustering. To test for differences in perceived quality of care, we dichotomized responses into “fair” or “poor” vs “excellent,” “very good,” or “good” and compared ATSM, GMV, and UC using logistic regression models, using generalized estimating equations to account for within-PCP clustering.31
We dichotomized the data for the analysis because data was not normally distributed for all responses. We calculated the proportion of patients for whom PCPs agreed or strongly agreed that barriers to diabetes care existed. For providers who agreed or strongly agreed that a barrier existed for a patient in an intervention arm, we analyzed whether PCPs agreed that the intervention helped the patient overcome the barrier by dichotomizing responses into “strongly agree” or “agree” vs “neutral,” “disagree,” or “strongly disagree.” We calculated the proportion of patients in ATSM and GMV arms for which PCPs perceived the intervention helped overcome ≥ 1 barrier. We compared ATSM and GMV using logistic regression models with generalized estimating equations to account for within-PCP clustering.
Results
Participants
Of 113 eligible PCPs caring for 330 enrolled patients, 87 PCPs (77%) responded to surveys about 245 (74%) patients (average 2.8 patients per PCP, range 1–14). Response rates did not differ significantly by patient trial arm. Of the PCPs, 62% were women. Just over half (56%) were residents, and among those not in training, the average for years in practice was 15.5 (standard deviation 8.8). Respondents reported that an average of 32% of their patient panels was composed of patients with diabetes. Among their patients, 34% were in the UC arm, 32% in the GMV arm, and 34% in the ATSM arm; 44% of their patients spoke Spanish, 12% spoke Cantonese, and 44% spoke English.
PCP Perspectives on Patient Activation
When comparing their patients to 1 year prior, PCPs classified more patients exposed to ATSM (58.7%) and GMV (52.6%) as more likely to engage in health-related goal setting, compared with 33.3% of UC patients (both p < 0.05). While PCPs perceived that 44.7% of UC patients were more likely to play an active role in caring for their diabetes, this estimate was higher for ATSM-exposed patients (65.8%, p = 0.01) and GMV-exposed patients (54.9%, p = 0.25). Automated telephone self-management and GMV had larger effect sizes than UC for these two items summed (ATSM vs UC, +0.41, p = 0.01; GMV vs UC, +0.31, p = 0.05).
PCP Perspectives on Quality of Care
Primary care providers rated the quality of care as poor or bad for 37.2% of UC patients, 26.9% of GMV patients, and 14.3% of ATSM patients. Accounting for within-PCP clustering, the odds of PCPs rating the quality of care as poor or bad was lower among patients exposed to ATSM compared to patients in UC (odds ratio 0.38, p < 0.01), but not significantly different among patients exposed to GMV (odds ratio 0.72, p = 0.20). Most PCPs agreed that both ATSM and GMV should be expanded to more patients with diabetes (88%) and other chronic diseases (98%).
PCP Perspectives on Barriers to Care
Table 1 depicts diabetes care barriers reported by clinicians in all study arms. In over two-thirds of patient-specific survey assessments, PCPs reported difficulty in accessing community resources for self-management, difficulty in keeping up with patients between visits, lacking time during visits to provide optimal care, and a need to focus their visits on multiple or urgent problems rather than diabetes self-management.
Table 1.
Perceptions of Primary Care Providers (n = 87) about Barriers to Diabetes Care Experienced by Their Patients (n = 245) at Four Urban Clinics
| Barriers to optimal care | Proportion of study patients facing barrier (%) |
|---|---|
| Difficulty accessing community resources that could improve self-management | 78.2 |
| Difficulty keeping up with patient's progress between visits | 68.8 |
| Not enough time in clinic visits to provide optimal care | 69.0 |
| Visits spent dealing with multiple/urgent problems, not diabetes self-management | 67.7 |
| I cannot see patient frequently enough to closely monitor health issues | 61.0 |
| Limited health literacy interferes with optimal care | 61.0 |
| Inadequate self-management resources for patients with limited health literacy or limited English proficiency | 60.0 |
| Patient has problems managing medications | 58.5 |
| I do not know how to best support patient's ability to self-manage diabetes | 57.9 |
| I have not understood patient's health beliefs/how they influence diabetes care | 51.9 |
| Patient's care is often fragmented (may not show for visits, “lost to follow-up”) | 51.9 |
| Patient has not received multidisciplinary/team-based care | 50.7 |
| Limited English proficiency interferes with optimal care | 38.2 |
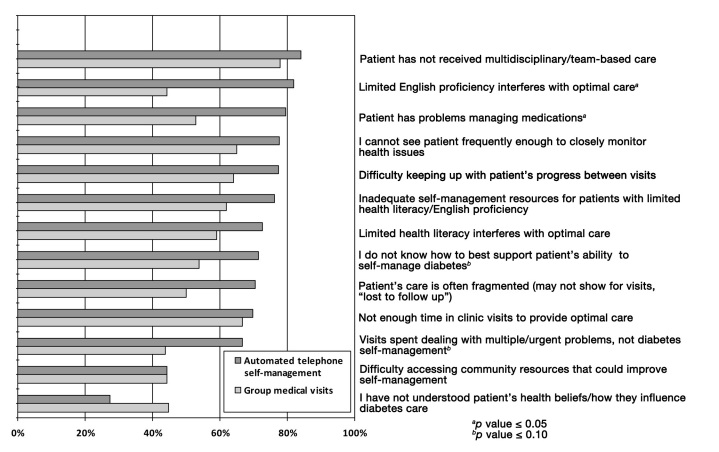
Primary care providers caring for intervention arm patients reported that the intervention helped overcome at least one barrier for 68% of ATSM patients and 60% of GMV patients. Figure 1 illustrates differences in the PCPs' perceptions that the IDEALL intervention helped their patients overcome barriers to their diabetes management. The most common barriers described as having been helped by both types of interventions were lack of multidisciplinary/team-based care, ability to see the patient frequently enough to closely monitor his or her health issues, difficulty keeping up with the patient's progress between visits, and inadequate self-management resources for patients with low health literacy or limited English proficiency. Primary care providers perceived that patients exposed to ATSM were helped significantly more than patients exposed to GMV for the following barriers: limited English proficiency interferes with optimal care (82% ATSM vs 44% GMV, p = 0.01) and patient has problems managing medications (80% ATSM vs 53% GMV, p = 0.01). More ATSM patients were perceived to have been helped with the barriers of spending visits on multiple/urgent problems (67% ATSM vs 44% GMV, p = 0.06) and not knowing how to support a patient's self-management (71% ATSM vs 54% GMV, p = 0.07), but these did not reach statistical significance.
Figure 1.
Proportion of primary care providers (n = 87) who perceived self-management support interventions helped overcome barriers to optimal diabetes care for intervention patients (n = 162): comparison between automated telephone self-management and group medical visits.
Discussion
In this post-randomized controlled trial survey of practice-based clinicians, SMS intervention strategies with ATSM and GMV were associated with PCP perceptions that patients were more activated to set goals and care for their diabetes. Only ATSM was associated with better ratings of the quality of care provided to their patients. Primary care providers perceived multiple benefits to SMS and felt that ATSM particularly helped patients for whom limited English proficiency and medication management were barriers to care.
The attitudes of health care professionals towards SMS programs are important for two reasons: (1) their role in facilitating patient access to these programs and integrating SMS into chronic disease care settings,12 and (2) the potential to improve PCP satisfaction and reduce frustration as they care for medically and psychosocially vulnerable patients. Although SMS has been shown to improve the quality of care and health for patients with chronic medical conditions, including diabetes,4,5,7,8,20 the few studies examining PCP perceptions suggest they are ambivalent about the importance and benefits of SMS.12–14 A qualitative study of PCPs in the United Kingdom revealed concerns about sharing responsibility and control for disease management with their patients who could become overconfident or fail to seek clinician help when indicated.13 Similarly, a study of PCPs in the United States and United Kingdom found that clinicians felt that the most important aspect of patient self-management was following PCP medical advice, more than promoting patients' capacity to make independent judgments and/or to take independent actions in self-care.14 Moreover, PCPs may be ambivalent about who should assume primary responsibility for supporting patient self-management. Within the context of a short medical encounter and competing demands, PCPs may not feel they can prioritize SMS within their own agenda, deferring this role to other providers such as nurses.13 However, in a national study of physicians about diabetes self-management education programs, some physicians were concerned that external educators would provide information that conflicted with their own advice or even result in patients switching PCPs.12 On the other hand, diabetes educators saw PCP encouragement as a key factor in helping patients to engage in SMS programs.12
Our research suggests that ATSM holds promise to engage not only patients19,20 but also clinicians. This may be due to a variety of reasons. Occurring outside the context of the usual medical encounter, ATSM offers a clinician-efficient, HIT-enhanced approach to SMS, free of the time constraints and competing responsibilities of clinicians.13 Out-of-range triggers for safety issues may be integrated into the existing primary care delivery system, allowing clinicians to be looped back into the conversation and minimizing their concerns about overconfident patients or contradictory educator recommendations.12,13
By offering SMS free of jargon and in multiple languages, ATSM offers a systems-level, standardized approach to chronic disease support in safety net settings, ensuring that education, goal setting, and action planning is not promoted or withheld based on clinician assumptions about an individual patient's capacity for self-care.11 Primary care providers may perceive that ATSM helps them serve an unmet need and desire for SMS by patients facing barriers in other aspects of chronic disease care.9 In addition, ATSM offers a systematic strategy to overcome communication barriers that have been associated with lower PCP satisfaction and self-efficacy in patient encounters, such as limited health literacy or limited English proficiency.1,32 As PCPs and primary care practices work to meet meaningful use criteria in the implementation of electronic health record systems, this form of HIT also provides alternative methods for patient education and promotion of improved chronic disease outcomes for diverse, multilinguistic populations.15,16 Ultimately, by improving PCPs' perceptions of the quality of care delivered to vulnerable populations, ATSM may have the potential to reduce clinician stress in safety net settings and enhance their professional satisfaction.1
Finally, clinicians are key stakeholders in the process of practice-based research,33–36 and the assessment of their perceptions is crucial to evaluating the comparative effectiveness of different SMS strategies.37 The congruence of both patient and PCP perceptions that ATSM improved the quality of their diabetes care strengthens the evidence for ATSM as a technological resource for chronic disease care delivery in the modern patient-centered medical home.
This study was not designed to examine the potentially synergistic effects of SMS involving both ATSM and GMV. Given the benefits of each intervention perceived by PCPs and experienced by patients,20 future SMS implementation studies could explore the impact and cost-effectiveness of combining these interventions, with ATSM occurring between and informing the content of GMV sessions.
The limitations of this study should be acknowledged. First, PCPs were not blinded to the study arm of their patients, and their beliefs about the advantages and disadvantages of ATSM or GMV may have influenced their reports about their patients. Second, because the survey was conducted postintervention, PCP reports about how their patients changed compared with the prior year may be subject to recall bias, but because this was a randomized controlled trial, we do not expect recall to have differed by arm. Third, our sample size may not be sufficient to detect all differences in PCP perceptions among ATSM, GMV, and UC. Fourth, persons with visual and hearing impairment are an important population receiving care in safety net settings who deserve SMS, and future implementation studies should tailor SMS to their needs, including adaptation of ATSM for use with telephone relay systems and sign language interpretation for GMV visits. Finally, these findings from one urban safety net health system may not be generalizable to other primary care practice settings. However, our previously published measures of the reach of this intervention—as measured by participation among clinics, clinicians, and patients, patient representativeness, and patient engagement with ATSM—support its relevance to safety net settings serving linguistically diverse, vulnerable patients.19
Conclusions
In summary, safety net PCPs serving a diverse population perceived that patients participating in a diabetes ATSM support program had overcome barriers, participated more actively, and received higher quality diabetes care. Given the promising patient-centered, functional, and cost-effectiveness outcomes of the patient study, these views of clinician stakeholders lend additional evidence for the potential to upscale ATSM more broadly in diabetes care, harnessing HIT to support PCPs in their care of diverse, multilinguistic populations.
Glossary
Abbreviations
- (ATSM)
automated telephone self-management
- (CHNSF)
Community Health Network of San Francisco
- (GMV)
group medical visit
- (HbA1c)
hemoglobin A1c
- (HIT)
health information technology
- (IDEALL)
Improving Diabetes Efforts across Language and Literacy
- (PCP)
primary care provider
- (RCT)
randomized controlled trial
- (SMS)
self-management support
- (UC)
usual care
Appendix A: The IDEALL Project Self-Management Support Models
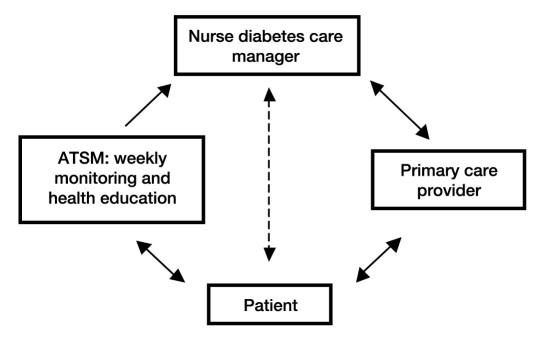
Figure A1.
The automated telephone self-management system. The ATSM system provides weekly calls with rotating queries, in the patient's native language, regarding self-care (e.g., symptoms, medication adherence, diet, physical activity, self-monitoring of blood glucose, smoking); psychosocial issues (e.g., coping, depressive symptoms); and referrals for preventive services (e.g., ophthalmologist). Patients respond via touch-tone commands. Depending on the response to an individual item, patients also receive automated health education messages in the form of narratives. Patients answering “out of range” on ≥1 item, based on predetermined clinical thresholds, receive a call back from a language concordant care manager within 48 h. The care manager helps patients problem-solve around the issue identified in the report, with a focus on collaborative goal setting with action plans. All patient interactions with ATSM care managers, including action plans created and achieved, were communicated with PCPs.
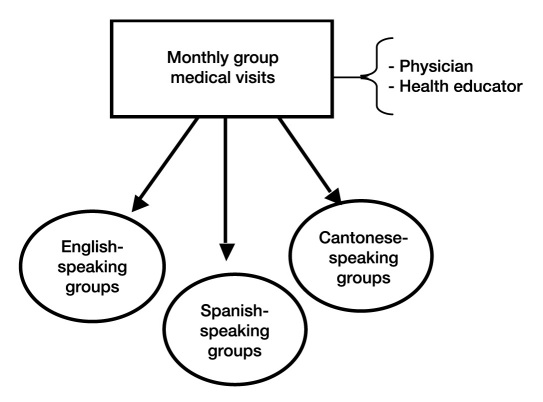
Figure A2.
Group medical visit model. A GMV involves language-specific monthly group medical visits for 9 months. Group medical visits involve 6–10 patients, are cofacilitated by a language concordant primary care physician and health educator, last 90 min, and share the same basic structure: (1) group check-in, in which participants report any problems or progress with action plans and the group facilitates problem solving, adjustment, and/or recommitment to action plans; (2) discussion of common concerns or modeling of self-management practices; (3) social break with healthy snacks; (4) short planning session to select subsequent topics; and (5) brief, individualized care to patients with unmet medical needs. All patient interactions with GMV cofacilitators, including action plans created and achieved, were communicated with PCPs.
Funding
Agency for Healthcare Research and Quality Grant 1R21HS014864-01.
Disclosures
Portions of this data were presented in abstract form at the Society of General Internal Medicine Annual Meeting in Pittsburgh, PA, April 2008.
References
- 1.Varkey AB, Manwell LB, Williams ES, Ibrahim SA, Brown RL, Bobula JA, Horner-Ibler BA, Schwartz MD, Konrad TR, Wiltshire JC, Linzer M MEMO Investigators. Separate and unequal: clinics where minority and nonminority patients receive primary care. Arch Intern Med. 2009;169(3):243–250. doi: 10.1001/archinternmed.2008.559. [DOI] [PubMed] [Google Scholar]
- 2.Linzer M, Manwell LB, Williams ES, Bobula JA, Brown RL, Varkey AB, Man B, McMurray JE, Maguire A, Horner-Ibler B, Schwartz MD MEMO (Minimizing Error, Maximizing Outcome) Investigators. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(1):28–36. doi: 10.7326/0003-4819-151-1-200907070-00006. W6-9. [DOI] [PubMed] [Google Scholar]
- 3.Lewin ME, Altman SH Institute of Medicine. America's Health Care Safety Net. Washington, D.C: National Academy Press; 2000. Committee on the Changing Market, Managed Care, and the Future Viability of Safety Net Providers; p. 281. [Google Scholar]
- 4.Fisher EB, Brownson CA, O'Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. Am J Public Health. 2005;95(9):1523–1535. doi: 10.2105/AJPH.2005.066084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001. Committee on Quality of Health Care in America. [Google Scholar]
- 6.Naik AD, Palmer N, Petersen NJ, Street RL, Jr., Rao R, Suarez-Almazor M, Haidet P. Comparative effectiveness of goal setting in diabetes mellitus group clinics: randomized clinical trial. Arch Intern Med. 2011;171(5):453–459. doi: 10.1001/archinternmed.2011.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364(9444):1523–1537. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 8.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164(15):1641–1649. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 9.Sarkar U, Piette JD, Gonzales R, Lessler D, Chew LD, Reilly B, Johnson J, Brunt M, Huang J, Regenstein M, Schillinger D. Preferences for self-management support: findings from a survey of diabetes patients in safety-net health systems. Patient Educ Couns. 2008;70(1):102–110. doi: 10.1016/j.pec.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cabana MD, Chaffin DC, Jarlsberg LG, Thyne SM, Clark NM. Selective provision of asthma self-management tools to families. Pediatrics. 2008;121(4):e900–e905. doi: 10.1542/peds.2007-1559. [DOI] [PubMed] [Google Scholar]
- 11.Tan NC, Tay IH, Ngoh A, Tan M. A qualitative study of factors influencing family physicians' prescription of the written asthma action plan in primary care in Singapore. Singapore Med J. 2009;50(2):160–164. [PubMed] [Google Scholar]
- 12.Peyrot M, Rubin RR, Funnell MM, Siminerio LM. Access to diabetes self-management education: results of national surveys of patients, educators, and physicians. Diabetes Educ. 2009;35(2):246. doi: 10.1177/0145721708329546. 248, 252–6, 258–63. [DOI] [PubMed] [Google Scholar]
- 13.Blakeman T, MacDonald W, Bower P, Gately C, Chew-Graham C. A qualitative study of GPs' attitudes to self-management of chronic disease. Br J Gen Pract. 2006;56(527):407–414. [PMC free article] [PubMed] [Google Scholar]
- 14.Hibbard JH, Collins PA, Mahoney E, Baker LH. The development and testing of a measure assessing clinician beliefs about patient self-management. Health Expect. 2010;13(1):65–72. doi: 10.1111/j.1369-7625.2009.00571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jha AK. Meaningful use of electronic health records: the road ahead. JAMA. 2010;304(15):1709–1710. doi: 10.1001/jama.2010.1497. [DOI] [PubMed] [Google Scholar]
- 16.Hsiao CJ, Hing E, Socey TC, Cai B. Atlanta, GA: CDC National Center of Health Statistics; 2010. Electronic Medical Record/Electronic Health Record Systems of Office-Based Physicians: United States, 2009 and Preliminary 2010 State Estimates. [Google Scholar]
- 17.Krist AH, Woolf SH. A vision for patient-centered health information systems. JAMA. 2011;305(3):300–301. doi: 10.1001/jama.2010.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Telehealth. Washington, D.C.: U.S. Department of Health and Human Services. 2009. http://healthit.hhs.gov/portal/server.pt/document/849768/healthit_gov__telehealth. Accessed Nov 20, 2011.
- 19.Schillinger D, Hammer H, Wang F, Palacios J, McLean I, Tang A, Youmans S, Handley M. Seeing in 3-D: examining the reach of diabetes self-management support strategies in a public health care system. Health Educ Behav. 2008;35(5):664–682. doi: 10.1177/1090198106296772. [DOI] [PubMed] [Google Scholar]
- 20.Schillinger D, Handley M, Wang F, Hammer H. Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes: a three-arm practical clinical trial. Diabetes Care. 2009;32(4):559–566. doi: 10.2337/dc08-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Handley MA, Shumway M, Schillinger D. Cost-effectiveness of automated telephone self-management support with nurse care management among patients with diabetes. Ann Fam Med. 2008;6(6):512–518. doi: 10.1370/afm.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Med Care. 2005;43(10):960–969. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- 23.Alegria M, Sribney W, Perez D, Laderman M, Keefe K. The role of patient activation on patient–provider communication and quality of care for US and foreign born Latino patients. J Gen Intern Med. 2009;24(Suppl 3):534–541. doi: 10.1007/s11606-009-1074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8(5):410–417. doi: 10.1370/afm.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52(3):315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 26.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 27.Institute of Medicine. Washington, D.C: National Academy Press; 2004. Health Literacy: A Prescription to End Confusion. [Google Scholar]
- 28.Regenstein M, Huang J, Schillinger D, Lessler D, Reilly B, Brunt M, Johnson J, Piette J. Washington, D.C: National Public Health and Hospital Institute; 2005. Caring for patients with diabetes in safety net hospitals and health systems: what patients say about their care. [Google Scholar]
- 29.Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC, Society of General Internal Medicine (SGIM) Career Satisfaction Study Group (CSSG) Predicting and preventing physician burnout: results from the United States and The Netherlands. Am J Med. 2001;111(2):170–175. doi: 10.1016/s0002-9343(01)00814-2. [DOI] [PubMed] [Google Scholar]
- 30.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 31.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 32.Seligman HK, Wang FF, Palacios JL, Wilson CC, Daher C, Piette JD, Schillinger D. Physician notification of their diabetes patients' limited health literacy. A randomized, controlled trial. J Gen Intern Med. 2005;20(11):1001–1007. doi: 10.1111/j.1525-1497.2005.00189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Genel M, Dobs A. Translating clinical research into practice: practice-based research networks—a promising solution. J Investig Med. 2003;51(2):64–71. doi: 10.1136/jim-51-02-07. [DOI] [PubMed] [Google Scholar]
- 34.Mold JW, Peterson KA. Primary care practice-based research networks: working at the interface between research and quality improvement. Ann Fam Med. 2005;3(Suppl 1):S12–S20. doi: 10.1370/afm.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nagykaldi Z, Mold JW, Robinson A, Niebauer L, Ford A. Practice facilitators and practice-based research networks. J Am Board Fam Med. 2006;19(5):506–510. doi: 10.3122/jabfm.19.5.506. [DOI] [PubMed] [Google Scholar]
- 36.Rust G, Cooper LA. How can practice-based research contribute to the elimination of health disparities? J Am Board Fam Med. 2007;20(2):105–114. doi: 10.3122/jabfm.2007.02.060131. [DOI] [PubMed] [Google Scholar]
- 37.Schmittdiel JA, Grumbach K, Selby JV. System-based participatory research in health care: an approach for sustainable translational research and quality improvement. Ann Fam Med. 2010;8(3):256–259. doi: 10.1370/afm.1117. [DOI] [PMC free article] [PubMed] [Google Scholar]