Abstract
African Americans suffer disproportionately from the adverse health consequences of smoking, and also report substantially lower socioeconomic status than Whites and other racial/ethnic groups in the U.S. Although socioeconomic disadvantage is known to have a negative influence on smoking cessation rates and overall health, little is known about the influence of socioeconomic status on smoking cessation specifically among African Americans. Thus, the purpose of the current study was to characterize the impact of several individual- and area-level indicators of socioeconomic status on smoking cessation among African Americans. Data were collected as part of a smoking cessation intervention study for African American smokers (N = 379) recruited from the Houston, Texas, metropolitan area, who participated in the study between 2005 and 2007. The separate and combined influences of individual-level (insurance status, unemployment, education, and income) and area-level (neighborhood unemployment, education, income, and poverty) indicators of socioeconomic status on continuous smoking abstinence were examined across time intervals using continuation ratio logit modeling. Individual-level analyses indicated that unemployment was significantly associated with reduced odds of smoking abstinence, while higher income was associated with greater odds of abstinence. However, only unemployment remained a significant predictor of abstinence when unemployment and income were included in the model together. Area-level analyses indicated that greater neighborhood unemployment and poverty were associated with reduced odds of smoking abstinence, while greater neighborhood education was associated with higher odds of abstinence. However, only neighborhood unemployment remained significantly associated with abstinence status when individual-level income and unemployment were included in the model. Overall, findings suggest that individual- and area-level unemployment have a negative impact on smoking cessation among African Americans. Addressing unemployment through public policy and within smoking cessation interventions, and providing smoking cessation treatment for the unemployed may have a beneficial impact on tobacco-related health disparities.
Keywords: USA, African American, Smoking Cessation, Unemployment, Socioeconomic Status, Tobacco, Neighborhood
Introduction
Members of certain racial/ethnic groups and individuals of low socioeconomic status (SES) suffer disproportionately from the adverse health consequences of smoking (Vidrine et al., 2009). In particular, African Americans have the highest lung cancer incidence and mortality rates when compared to other racial/ethnic groups, as well as the highest overall rates of tobacco-related morbidity and mortality (Fagan et al., 2007). African Americans experience tobacco-related health disparities despite reports of lower daily smoking rates and later onset of smoking (Fagan et al., 2007), and they are less likely to quit smoking than individuals of other racial/ethnic backgrounds (Fagan et al., 2007). Notably, African Americans report substantially lower SES than Whites and other racial/ethnic groups in the U.S. (DeNavas-Walt et al., 2010; Ostrove & Feldman, 1999), and a large body of research indicates that socioeconomic disadvantage has a negative influence on health behavior and health (Adler & Ostrove, 1999).
Current conceptual models of SES and health emphasize the roles of stress/adversity, psychosocial resources, negative emotions/distress, and behavioral health risk factors (Gallo & Matthews, 2003; Matthews & Gallo, 2011). Specifically, socioeconomically deprived individuals may experience greater exposure to stress and adversity (Hatch & Dohrenwend, 2007; McLeod & Kessler, 1990) and possess fewer psychosocial resources (Campbell et al., 1986; Cohen et al., 1999; Turner & Lloyd, 1999), which contribute to distress and negative affect (Schulz et al., 2006; Turner & Lloyd, 1999; Vilhjalmsson, 1993). Greater negative affect and distress have been linked with a variety of unhealthy behaviors including smoking (Gallo & Matthews, 2003). Initial research has indicated that this general model of SES and health may also be applied more specifically to smoking cessation and other health behaviors (Businelle et al., 2010; Kendzor et al., 2009).
Education, occupation, and income are the most commonly used measures of SES in general health and smoking research (Braveman et al., 2005; Schaap & Kunst, 2009; Shavers, 2007), and each of these indicators is hypothesized to have a slightly different influence on health behavior. For example, individuals with more education may possess a greater ability to engage in critical thinking related to health information, and may be more likely to develop social networks that foster socialization to healthier behaviors (Shavers, 2007; Yen & Moss, 1999). Greater education has been linked with an increased likelihood of smoking cessation in numerous studies (Businelle et al., 2010; Finney Rutten et al., 2005; Foulds et al., 2006; Marti, 2010; Wetter et al., 2005). Unemployment has been hypothesized to influence health via economic deprivation and stress, a reduced sense of control over one’s environment, decreased social support, increased social isolation, and the absence of a daily structure to facilitate social interaction, personal status, and identity (Janlert & Hammarström, 2009). Several studies have linked unemployment with a decreased likelihood of successful smoking cessation (Businelle et al., 2010; Foulds et al., 2006; Pisinger et al., 2005; Waldron & Lye, 1989). Low income may influence health through decreased access to resources such as high quality healthcare and medical treatments; and perhaps through increased distress due to stressors such as financial concerns. Studies have shown that lower income is associated with a decreased likelihood of smoking cessation (Businelle et al., 2010; Marti, 2010). Other variables such as lack of health insurance coverage may influence smoking cessation through lack of access to medical care and advice to quit, and lack of prescription coverage for pharmacological treatments. Research has indicated that individuals who are uninsured have decreased odds of successful smoking cessation (Finney Rutten et al., 2005; Foulds et al., 2006).
Area-level neighborhood characteristics reflect the context in which an individual resides and may influence health over and above individual-level SES (Braveman et al., 2005; Shavers, 2007). For example, area-level disadvantage is associated with a variety of characteristics that may influence tobacco use and cessation including higher density and closer proximity of tobacco outlets and convenience stores (Chuang et al., 2005; Siahpush et al., 2010a), higher frequency of tobacco marketing placements (John et al., 2009; Siahpush et al., 2010b), the availability of single cigarettes for purchase (e.g., loosies; Smith et al., 2007; Stillman et al., 2007), and negative affect/depression among residents (Matheson et al., 2006). Recent research indicates that greater density of tobacco outlets and tobacco advertising are associated with higher smoking prevalence (Henriksen et al., 2008), and closer proximity to tobacco outlets is associated with a reduced likelihood of smoking cessation following a quit attempt (Reitzel et al., 2011).
The findings of numerous cross-sectional studies indicate that area-level indicators of socioeconomic disadvantage (e.g., % unemployed, median income, % with < high school education, % living < poverty threshold) are associated with current smoking and level of smoking (Chuang et al., 2005; Datta et al., 2006; Diez Roux et al., 2003; Duncan et al., 1999; Kleinschmidt et al., 1995; Öhlander et al., 2006; Reijneveld, 1998; Ross, 2000; Shohaimi et al., 2003; Stimpson et al., 2007; Van Lenthe & Mackenbach, 2006). Thus, it is plausible that social norms in deprived neighborhoods encourage smoking and discourage smoking cessation (Biener et al., 2010; Smith et al., 2007; Stillman et al., 2007). Moreover, there is some evidence that African Americans may have more frequent contact with members of their social networks, which are more likely to include family members, than other individuals of other racial/ethnic backgrounds (Ajrouch et al., 2001). Therefore, African Americans may be disproportionately influenced by the smoking-related beliefs and smoking behavior of family members and others in their social networks.
Unfortunately, very little is known about the influence of neighborhood socioeconomic deprivation on smoking cessation. The findings of a single prospective study indicated that greater area deprivation was associated with a reduced likelihood of smoking cessation, after accounting for individual-level SES (Giskes et al., 2006). Thus, more research is needed to explore the influence of area-level variables on smoking cessation, particularly among African Americans who are vulnerable to tobacco-related health disparities.
The purpose of the current study was to characterize the impact of several indicators of SES on smoking cessation among African Americans participating in a smoking cessation intervention. The influences of both individual- and area-level SES indicators on smoking cessation were explored. Additionally, the influences of area-level characteristics on smoking cessation were evaluated while accounting for important individual-level SES indicators. Findings will explore the influence of several dimensions of SES on smoking cessation efforts among African Americans. Results may be used to inform policy and improve cessation interventions for African Americans, which would, ideally, contribute to the reduction of tobacco-related health disparities.
Methods
Participants
Data were collected as part of a randomized clinical trial designed to evaluate the efficacy of palmtop computers in a smoking cessation intervention for African American smokers (C Mazas, University of Texas M. D. Anderson Cancer Center, Unpublished Observations, 2010). Individuals were eligible to participate if they were African American, smoked ≥ 5 cigarettes per day for ≥ 12 months, produced expired carbon monoxide levels of ≥ 8 parts per million, were willing to quit smoking within the next 2 weeks, possessed a functioning home telephone number, had a permanent home address, and were able to understand English at a sixth grade literacy level. Individuals were excluded from the study if they reported regular use of tobacco products other than cigarettes, were using pharmacological smoking cessation treatments other than the nicotine patches supplied by the study, reported that the nicotine patch was medically contraindicated, or were pregnant or lactating. Participant recruitment and flow through the study protocol are reported elsewhere (Kendzor et al., 2008).
Procedure
Participants were recruited from the Houston, Texas metropolitan area and were randomly assigned to either a standard smoking cessation treatment that included the nicotine patch, culturally sensitive self-help materials, and individual counseling, or the standard treatment supplemented with treatment delivered via palmtop computer. Data relevant to the current study were collected approximately two weeks prior to the quit day (baseline), and at days 3, 10, 31, and week 26 post-quit between 2005 and 2007. Participants were compensated with $20 gift cards at each visit through day 10 post-quit, and with $40 gift cards at day 31 and week 26 post-quit. Study procedures were approved by the Institutional Review Board of the University of Texas MD Anderson Cancer Center. Informed consent was obtained from all participants.
Participants’ residential addresses were “geocoded” in order to link them with a neighborhood and obtain area-level SES data. Geocoding refers to the process of associating an address with a point in geographic space, which can then be displayed on a map using Environmental Systems Research Institute’s (ESRI) ArcGIS software (version 9.3.1, ESRI, Redlands, CA). An address locator, built using address points from Centerpoint Energy’s Houston metropolitan area address database, was used to set parameters for batch geocoding in ArcGIS. The majority of residential addresses (97%) were geocoded with the batch address locator. Geocoding failures were primarily due to participant reporting of P.O. boxes rather than street addresses.
Measures
Demographics
The Demographic Information Questionnaire is a self-report measure of demographic variables including years of age, gender, and partner status (married/living with partner or single/divorced/separated/widowed).
Tobacco Use
The Tobacco History Questionnaire is a self-report measure of the average number of cigarettes smoked per day prior to quitting, and amount of time after awakening before smoking the first cigarette of the day (≤ 5 minutes or > 5 minutes).
Individual-level Socioeconomic Variables
Individual-level SES variables included insurance status, unemployment, education, and income. Insurance Status included 2 categories: 1) uninsured, or 2) insured (e.g., private/group insurance, Medicare, Medicaid). Unemployment categories included: 1) unemployed and 2) employed. Please note that the unemployed category included those who were unemployed (45%), unable to work or disabled (11.1%), retired (2.4%), homemakers (1%), and other (1.6%). None of the participants reported that they were students. The employed category included those who reported that they were employed full-time (24.6%) or part-time (14.3%). Education included 3 categories: 1) completed <high school, 2) completed high school/some college, and 3) completed ≥vocational or community college degree. Annual Household Income included 3 categories: 1) <$10,000, 2) $10,000-$29,999, and 3) ≥$30,000.
Area-level Socioeconomic Variables
Although there are numerous area-level characteristics that may influence smoking cessation, variables were selected to parallel the individual-level measures of SES utilized in the study. Data were procured from the 2000 U.S. Census and were based on Census tracts, which have been supported as a proxy for neighborhoods in previous health-related research (Jones et al., 2010; Krieger et al., 2003; Ross et al., 2004; Stafford et al., 2008). Four area-level SES variables were examined: 1) the percentage of residents in the neighborhood ≥ 16 years of age who were unemployed (neighborhood unemployment), 2) the percentage of residents in the neighborhood ≥ 25 years of age with ≥ a high school diploma or GED (neighborhood education), 3) median annual household income (neighborhood income), and 4) the percentage of households in the neighborhood with income below the poverty level (neighborhood poverty). Census-based insurance data at the tract level were not available for inclusion.
Continuous Smoking Abstinence
Continuous abstinence was defined as a self-report of complete abstinence from smoking since the quit date at 3 days, 10 days, 31 days, and 26 weeks post-quit, accompanied by either an expired carbon monoxide level of < 10 parts per million or a salivary cotinine level of < 20 ng/ml at each post-quit visit. Participants who reported a lapse and/or produced carbon monoxide or cotinine levels inconsistent with abstinence were considered relapsed.
Statistical Analyses
All analyses were performed using SAS (version 9.2; SAS Institute Inc., Cary, NC). The influence of individual- and area-level SES variables on smoking abstinence was examined through post-quit days 3, 10, 31, and week 26 using continuation ratio logit modeling (PROC GENMOD; Agresti, 2002; Allison, 2001; Bender & Benner, 2000). Continuation ratio logit analysis models the risk of smoking relapse across specific time intervals, where only individuals who were abstinent through the most recent assessment time point were included at each stage of the analysis (i.e., all participants are included in the analyses at time 1, while only abstinent participants from time 1 were included at time 2, etc.). Because of the potential for correlated outcomes among participants residing in the same neighborhood, a generalized estimating equation approach with exchangeable working correlations was used (Ten Have & Uttal, 1994). Data were available to determine abstinence status for 81.5% of participants at day 3, 84% at day 10, 84% at day 31, and 86.2% at 26 weeks. In cases where abstinence status could not be determined due to missing data, participants were considered relapsed consistent with the “intent-to-treat” approach commonly used in other smoking cessation studies (Swan et al., 2010; Webb et al., 2010). Listwise deletion was used to handle other missing data (e.g., covariates) in the analyses.
Analyses were completed in several steps. First, the effect of each individual-level SES variable on abstinence was evaluated separately in a series of models that included the following covariates: time, treatment group, age, gender, partner status, average number of cigarettes smoked per day, and time to first cigarette. Covariates were selected based on their theoretical and empirical associations with cessation in previous research, and every analysis included adjustment for these covariates. Second, the influences of all significant individual-level SES indicators on abstinence were evaluated simultaneously in an adjusted model. Third, the effect of each area-level SES variable on abstinence was evaluated separately in a series of adjusted models. Fourth, the influence of each area-level SES variable on abstinence was evaluated separately in a series of adjusted models that included all significant individual-level SES variables. The homogeneity of significant effects across time intervals was verified by examining their interaction with time.
Secondary analyses were conducted to ensure that any effects would be resilient to the inclusion of participants with missing data on covariates. This was accomplished by assigning individuals with missing data (other than smoking status) to a “missing” category for each variable, in order to retain the remainder of each participant’s data in the analyses. All analyses were conducted as described above. Analyses yielded results that were very similar to those where missing was excluded (see results section below), and are therefore not presented.
Finally, since it is possible that multicollinearity (e.g., correlations > .90; see Tabachnick & Fidell, 2007) might present a problem given the inclusion of multiple indicators of SES in the statistical models, we first evaluated the strength of the correlations among variables. Correlations among the individual-level variables were of weak to moderate strength (r’s ranged from .004 to .409). Similarly, correlations between individual- and area-level variables were also of weak to moderate strength (r’s ranged from .011 to .286). While stronger associations were present among the area-level variables, these variables were not included in the proposed statistical models together (i.e., only one area-level variable at a time was included in a model). Thus, multicollinearity does not appear to present a problem in the current analyses.
Results
Participant Characteristics
A total of 399 African American smokers participated in the study. However, the sample was reduced to 379 participants in the analyses because of missing covariates and/or the inability to geocode the participants’ addresses. The remaining participants resided in 174 Census tracts in the Houston, Texas, metropolitan area (range = 1-10 participants per tract). Participant characteristics are presented in Table 1. The percentage of participants (out of 379) who were continuously abstinent at each time point is presented in Table 2.
Table 1.
Participant characteristics.
| N | Mean (SD) | Range | % | |
|---|---|---|---|---|
|
| ||||
| Individual-Level Characteristics | ||||
| Age (years) | 379 | 42.2 (9.8) | 21-65 | - |
| Female Gender | 379 | - | - | 51.5 |
| Cigarettes Smoked per Day | 379 | 20.6 (12.2) | 5-91 | - |
| Smoke ≤ 5 Minutes of Waking | 379 | - | - | 60.4 |
| Married/Living w/partner | 379 | - | - | 22.2 |
| Uninsured | 374 | - | - | 54.0 |
| Unemployed | 378 | - | - | 61.1 |
| Education | 379 | |||
| < High School | - | - | - | 17.7 |
| High School/Some College | - | - | - | 61.2 |
| ≥ Vocational/Community College Degree | - | - | - | 21.1 |
| Annual Household Income | 305 | |||
| < $10,000 | - | - | - | 47.9 |
| $10,000-$29,999 | - | - | - | 31.8 |
| ≥ $30,000 | - | - | - | 20.3 |
|
| ||||
| Area-Level Characteristics | ||||
|
| ||||
| % Unemployed | 379 | 39.9 (12.6) | 17-75 | - |
| % ≥ High School Education | 379 | 67.7 (14.9) | 24-98 | - |
| Median Annual Household Income | 379 | $30,630 ($11,507) | $6,805-$75,489 | - |
| Poverty (% earning < poverty level) | 379 | 23.3 (12.6) | 1-70 | - |
Table 2.
Total participants who were continuously abstinent over time.
| Time Post-Quit | ||||
|---|---|---|---|---|
|
| ||||
| 3 Days | 10 Days | 31 Days | 26 Weeks | |
| Total Continuously Abstinent (% of sample) |
94 (24.8%) | 54 (14.2%) | 28 (7.4%) | 11 (2.9%) |
Individual-Level Socioeconomic Status
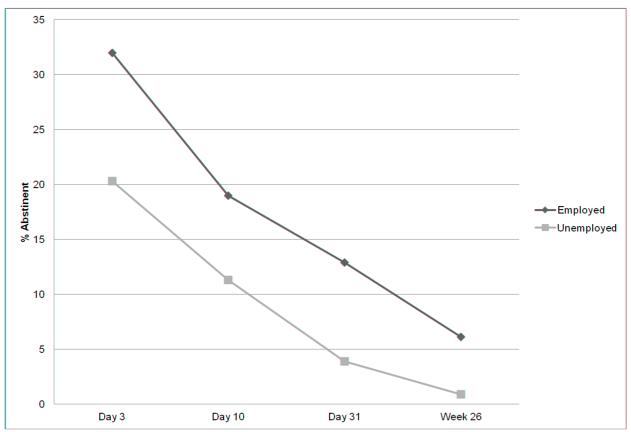
Analyses indicated that unemployed individuals were less likely to be abstinent across time intervals than those who were employed after controlling for all covariates (see Table 3). Individuals earning ≥$30,000 annually were more likely to be abstinent across time intervals than those earning <$10,000 (see Table 3). The effects of unemployment and income on the odds of abstinence did not vary across time intervals (p’s ≥ .37). When unemployment and income were included together in the model along with all covariates, only unemployment remained significantly associated with the odds of abstinence (see Table 4, Model 1), and this effect did not vary across time intervals (p = .59). Additionally, unemployment remained significantly associated with reduced odds of abstinence when all individual-level SES variables (employment, education, income, insurance status) were included in the model (results not presented). The percentage of employed and unemployed participants who were abstinent across post-quit time intervals is depicted in Figure 1.
Table 3.
The influence of each socioeconomic status variable on smoking abstinence through 26 weeks post-quit.
| Odds Ratio (95% CI) | p | |
|---|---|---|
|
| ||
| Individual-Level Characteristics | ||
| Uninsured (reference is Insured) | .76 (.50, 1.15) | .20 |
| Unemployed (reference is Employed) | .55 (.36, .84) | .006 |
| Education | - | .40 |
| < High School | 1.00 | - |
| High School/Some College | 1.27 (.70, 2.32) | .43 |
| ≥ Vocational/Community College Degree | 1.55 (.80, 3.00) | -.20 |
| Annual Household Income | - | .05 |
| < $10,000 | 1.00 | - |
| $10,000-$29,999 | 1.57 (.84, 2.93) | .16 |
| ≥ $30,000 | 2.37 (1.18, 4.78) | .02 |
|
| ||
| Area-Level Characteristics | ||
|
| ||
| % Unemployed | .97 (.95, .98) | < .0001 |
| % ≥ High School Education | 1.01 (1.003, 1.03) | .009 |
| Median Annual Household Income ($1000 units) | 1.01 (.998, 1.03) | .08 |
| Poverty (% earning < poverty level) | .98 (.97, .99) | .002 |
Note: All analyses were adjusted for time interval, treatment group, age, gender, partner status, cigarettes smoked per day, and time to first cigarette
Table 4.
The relationship between individual- and area-level indicators of socioeconomic status and abstinence in African-Americans.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
|
| |||||
| Individual-Level Characteristics | |||||
| Unemployed (reference is Employed) | .59(.36,.98)* | .61(.40,.95)* | .59(.36,.95)* | .60(.36,.98)* | .59(.37,.97)* |
| Annual Household Income | |||||
| < $10,000 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| $10,000-$29,999 | 1.28(.69,2.39) | 1.14(.67,1.93) | 1.28(.71,2.31) | 1.29(.69,2.39) | 1.28(.70,2.36) |
| ≥ $30,000 | 1.78(.89,3.58) | 1.04(.56,1.93) | 1.59(.80,3.14) | 1.59(.78,3.23) | 1.59(.79,3.19) |
|
| |||||
| Area-Level Characteristics | |||||
|
| |||||
| % Unemployed | - | .97(.95,.99)*** | - | - | - |
| % ≥ High School Education | - | - | 1.01(.99,1.02) | - | - |
| Median Annual Household Income ( $1000 units) | - | - | - | 1.01(.99,1.03) | - |
| Poverty (% earning < poverty level) | - | - | - | - | .99(.97,1.01) |
p < .05
p < .001
Note: All models were adjusted for time interval, treatment group, age, gender, partner status, cigarettes smoked per day, and time to first cigarette. Time interval, time to first cigarette, and age were significantly associated with smoking status. Specifically, individuals who were abstinent at time 1 (3 days post-quit) were more likely to be abstinent at time 2 (10 days post-quit) than all participants at time 1 in Models 1-5. Similarly, individuals who were abstinent at time 2 (10 days post-quit) were more likely to be abstinent at time 3 (31 days post-quit) than all participants at time 1 in Models 2 and 3. Earlier time to first cigarette in the morning (≤5 minutes) was associated with relapse in all models except for Model 1, and greater age was significantly associated with abstinence all models except for Model 2. Treatment group, gender, partner status, and cigarettes smoked per day were not significantly associated with smoking status in any of the models.
Figure 1.
Percent of employed and unemployed individuals who were continuously abstinent across post-quit time intervals.
Area-Level Socioeconomic Status
Analyses indicated that neighborhood unemployment (% unemployed), education (% ≥ high school education), and poverty (% earning < poverty level) were each associated with abstinence status across time intervals after controlling for all covariates (see Table 3). Specifically, greater neighborhood unemployment and poverty and were each associated with a reduced likelihood of abstinence, and greater neighborhood education was associated with a higher likelihood of abstinence. The effects of neighborhood unemployment, education, and poverty on smoking cessation did not vary across time intervals (p’s ≥ .19).
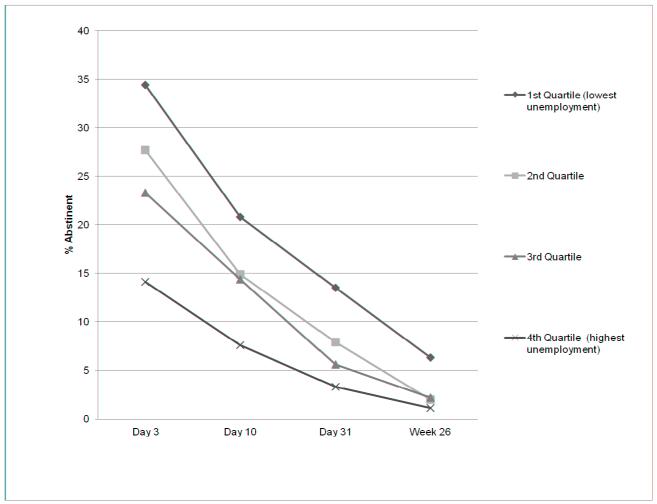
Neighborhood unemployment remained significantly associated with reduced odds of smoking abstinence across time intervals when the significant individual-level SES variables were included in the model (unemployment, income) along with all covariates (see Table 4, model 2). The effect of neighborhood unemployment on smoking abstinence did not vary across time intervals (p = .17). Both individual- and neighborhood-level unemployment remained significantly associated with reduced odds of smoking abstinence when they were included in the model together (see Table 4, model 2). Additionally, individual-level and neighborhood-level unemployment each remained significant predictors of reduced odds of abstinence when all individual-level SES variables (insurance status, unemployment, education, income) were included together in the model (results not presented). In Figure 2, neighborhood unemployment was divided into quartiles to illustrate the relationship between neighborhood unemployment and abstinence across post-quit time intervals.
Figure 2.
Percent continuously abstinent across post-quit time intervals by quartiles of percent unemployed in the neighborhood.
Discussion
The current study prospectively evaluated the influence of both individual- and area-level SES indicators on smoking cessation among African Americans who were enrolled in a smoking cessation intervention. The findings demonstrate that individual-level unemployment and residence in neighborhoods with high rates of unemployment each have a negative influence on smoking cessation among African Americans. In addition, both individual- and neighborhood-level unemployment provided unique predictive information. Thus, unemployment and smoking among unemployed African Americans may be important targets for multi-level smoking cessation efforts.
There are several possible explanations for the negative impact of unemployment on smoking cessation (Gallo & Matthews, 2003; Janlert & Hammarström, 2009). Negative affect may play a key mediating role in the relationship between low SES and poor health behavior (Businelle et al., 2010; Gallo & Matthews, 2003). Daily structure, regular activities, and social support (characteristics associated with employment) may be also important to health (Janlert & Hammarström, 2009). Employment may provide a distraction from the difficulties of smoking cessation and allow for greater access to social support during a quit attempt. Additionally, smoking is often restricted or prohibited at work (Gerlach et al., 1997; Shopland et al., 2001), which may encourage smoking cessation (Longo et al., 2001). In addition, many employers offer health insurance coverage for smoking cessation treatments and provide referrals to cessation programs and quit-lines (Hughes et al., 2011). The economic deprivation associated with unemployment may influence health through increased stress, reduced access to resources and healthcare, and a variety of other pathways (Janlert & Hammarström, 2009). It is also possible that unemployed individuals may be less responsive to any type of smoking cessation treatment. For example, Niederdeppe et al. (2011) found that socioeconomically disadvantaged individuals were less likely to recall ads from a smoking cessation media campaign that provided information about how to quit smoking than ads that conveyed information about why to quit smoking through graphic imagery and testimonials. As such, future research might examine SES differentials among individuals receiving treatment versus those individuals receiving no treatment. Finally, neighborhoods with high rates of unemployment are likely to have a high prevalence of smoking (Van Lenthe & Mackenbach, 2006). Thus, it is plausible that a greater number of unemployed smokers in a neighborhood may influence a cessation attempt by shaping beliefs about the acceptability of smoking via social networks (e.g., friendships with neighbors, participation in local organizations), while also increasing the likelihood of direct interaction with individuals who are smoking. Neighborhoods with high rates of unemployment may be more likely to be characterized by reduced social control of young adults and delinquent behaviors such as smoking. Thus, it is possible that neighborhood unemployment may be more closely associated with community-level social disorganization (see Sampson & Groves, 1989), relative to other measures of socioeconomic disadvantage. However, more research is needed to identify the mechanisms that link individual- and neighborhood-level unemployment with smoking cessation, and to determine the reasons why unemployment is a stronger predictor of smoking cessation than other indicators of SES.
Researchers have suggested that raising the SES of the most economically disadvantaged groups and strengthening safety net policies (e.g., unemployment insurance, job training programs) may shrink the existing socioeconomic gradient in health (Dow et al., 2010). Although more research is needed, policy-related decreases in unemployment may indirectly influence smoking cessation rates and tobacco-related health outcomes. Unemployment rates among African Americans in the U.S. are high (15.5%) relative to Hispanics (11.3%), Whites (7.9%), and Asians (7.1%; Bureau of Statistics, 2011). Potential contributors to unemployment among African Americans include inadequate education, racial/ethnic discrimination, reduced availability of “blue collar” jobs, increasing prevalence of criminal histories (i.e., time incarcerated reduces work experience; limited post-incarceration employment opportunities), greater income availability through criminal activity, and the high financial burden of child support relative to earnings (Holzer et al., 2005). Strategies such as increasing funding for education and job training may reduce unemployment rates and ultimately improve health (Tarlov, 1999). Other novel strategies, such as increasing work experience and suspending child support orders during incarceration, might specifically reduce unemployment among African American males (Holzer et al., 2005). The American Recovery and Reinvestment Act of 2009 (One Hundred Eleventh Congress of the United States of America, 2009) includes provisions for job creation through government sponsored projects, job training, and increased funding for unemployment benefits. Future policy initiatives could focus on the creation of jobs through projects centered in African American neighborhoods with high unemployment and/or smoking rates.
Plausibly, addressing unemployment within smoking cessation interventions or vice versa may also have a beneficial impact. For example, efforts to obtain employment may be encouraged and facilitated among economically disadvantaged individuals during smoking cessation treatment (e.g., referrals to employment services). Other strategies, such as establishing a regular daily schedule of activity as part of treatment (e.g., a behavioral activation approach, see MacPherson et al., 2010) might possibly reduce unemployment-related negative affect, provide distractions from the difficulties of quitting smoking, and allow opportunities for social support. Conversely, individuals receiving unemployment benefits may be offered or referred to smoking cessation treatment.
The current study has several strengths and limitations. One strength is that the separate influences of specific measures of SES on smoking cessation were evaluated. For example, the specific influence of area-level unemployment on smoking cessation was evaluated, whereas other studies have used composite measures of deprivation that combined area-level measures of unemployment along with other area characteristics (e.g., combining area-level measures of educational attainment, unemployment, and employment type; Giskes et al., 2006). Thus, the current study highlights the relative importance of several indicators of SES on smoking cessation outcomes at multiple levels of influence.
Notably, the current study utilized data collected as part of a randomized clinical trial of a smoking cessation intervention, which attracted individuals who were of particularly disadvantaged backgrounds. The majority of participants were uninsured and unemployed, nearly half reported a household income of < $10,000, and a substantial proportion reported that they had not completed high school. Perhaps the study attracted unemployed individuals who had greater flexibility in their schedules to attend study visits and economically disadvantaged individuals who were motivated to participate because of study compensation. Similarly, participants lived in neighborhoods with high rates of unemployment and poverty; limited education, and low household incomes. Study participants were also more likely to be female, heavy smokers, unemployed, and of single marital status than in nationally representative samples of African American smokers (Caraballo et al., 1998; Novotny et al., 1988). Therefore, the findings of the current study are most generalizable to African Americans seeking smoking cessation treatment and may not be representative of African American smokers in general. It is important to note that neither individual- or neighborhood-level unemployment interacted with treatment group (computer-delivered treatment vs. standard treatment) to influence cessation outcomes. Thus, there did not appear to be a differential response to treatment based on unemployment (results not presented, available upon request).
Another limitation is that the analyses did not account for changes in address or unemployment over the study period, and the area-level data were collected prior to participants’ study enrollment as part of the U.S. Census. Therefore, we were not able to account for changes in neighborhood SES that may have occurred between Census data collection and data collection for the current study. Finally, the area-level SES indicators utilized in the study were limited to those collected during the U.S. Census.
Overall, both individual- and neighborhood-level unemployment had a negative impact on smoking cessation. Findings highlight the need for multi-level approaches aimed at reducing unemployment, providing smoking cessation treatment for unemployed individuals, addressing unemployment within smoking cessation treatment interventions, and helping individuals to cope with the negative effects of unemployment during a smoking cessation attempt. Future research must focus on gaining a greater understanding of the mechanisms through which unemployment influences smoking cessation, in order to develop effective approaches for promoting smoking cessation among unemployed African Americans.
Research Highlights.
Findings suggest that both individual and area level unemployment reduced the odds of successful smoking cessation among African Americans.
Public policy aimed at decreasing unemployment may influence smoking cessation rates and tobacco-related health outcomes.
Addressing unemployment within existing smoking cessation interventions may have a beneficial impact on cessation outcomes.
Acknowledgements
This research was supported by grants R01-CA094826, R25T-CA57730, and K07-CA121037 awarded by the National Cancer Institute, grant MRSGT-10-104-01-CPHPS awarded by the American Cancer Society, and grants K01-DP001120 and K01-DP000086 awarded by the Centers for Disease Control and Prevention. This research was also supported, in part, by the National Institutes of Health through MD Anderson Cancer Center Support Grant CA016672. We are grateful for the contributions of the following research team members who were integral in the data collection, database design, and counseling provision on the parent project: Karla Anderson, Jamie Barnes, Shanna Barnett, Barrett Blackmon, Vantrese Camiso, Alex De La Torre, Mark Evans, Debbie Lew, Devin Olivares-Reed, Krystal Robinson, Nikita Robinson, Maribel Robledo, Paul Rowan, and Jim Sikora. We are also grateful for the contributions of Richard Dela Mater who performed the geocoding and procured the US Census data for the project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Annals of the New York Academy of Sciences. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Agresti A, editor. Categorical Data Analysis. John Wiley & Sons, Inc.; Hoboken, New Jersey: 2002. [Google Scholar]
- Ajrouch KJ, Antonucci TC, Janevic MR. Social networks among Blacks and Whites: The interaction between race and age. Journals of Gerontology - Series B Psychological Sciences and Social Sciences. 2001;56:S112–S118. doi: 10.1093/geronb/56.2.s112. [DOI] [PubMed] [Google Scholar]
- Allison PD. Logistic Regression using the SAS System: Theory and Application. SAS Institute and Wiley; Cary, North Carolina: 2001. [Google Scholar]
- America, O.H.E.C.o.t.U.S.o. American Recovery and Reinvestment Act of 2009. 2009. [Google Scholar]
- Bender R, Benner A. Calculating ordinal regression models in SAS and S-Plus. Biometrical Journal. 2000;42:677–699. [Google Scholar]
- Biener L, Hamilton WL, Siegel M, Sullivan EM. Individual, Social-normative, and policy predictors of smoking cessation: A multilevel longitudinal analysis. American Journal of Public Health. 2010;100:547–554. doi: 10.2105/AJPH.2008.150078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, et al. Socioeconomic status in health research: one size does not fit all. Journal of the American Medical Association. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Businelle MS, Kendzor DE, Reitzel LR, Costello TJ, Cofta-Woerpel L, Li Y, et al. Mechanisms linking socioeconomic status to smoking cessation: a structural equation modeling approach. Health Psychology. 2010;29:262–273. doi: 10.1037/a0019285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell KE, Marsden PV, Hurlbert JS. Social resources and socioeconomic status. Social Networks. 1986;8:97–117. [Google Scholar]
- Caraballo RS, Giovino GA, Pechacek TF, Mowery PD, Richter PA, Strauss WJ, et al. Racial and ethnic differences in serum cotinine levels of cigarette smokers: Third National Health and Nutrition Examination Survey, 1988-1991. Journal of the American Medical Association. 1998;280:135–139. doi: 10.1001/jama.280.2.135. [DOI] [PubMed] [Google Scholar]
- Chuang YC, Cubbin C, Ahn D, Winkleby MA. Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. Journal of Epidemiology and Community Health. 2005;59:568–573. doi: 10.1136/jech.2004.029041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Salonen JT, Kaplan GA. The role of psychological characteristics in the relation between socioeconomic status and perceived health. Journal of Applied Social Psychology. 1999;29:445–468. [Google Scholar]
- Datta GD, Subramanian SV, Colditz GA, Kawachi I, Palmer JR, Rosenberg L. Individual, neighborhood, and state-level predictors of smoking among US Black women: A multilevel analysis. Social Science and Medicine. 2006;63:1034–1044. doi: 10.1016/j.socscimed.2006.03.010. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2009. U.S. Government Printing Office; Washington, DC: 2010. [Google Scholar]
- Diez Roux AV, Merkin SS, Hannan P, Jacobs DR, Kiefe CI. Area characteristics, individual-level socioeconomic indicators, and smoking in young adults: The coronary artery disease risk development in young adults study. American Journal of Epidemiology. 2003;157:315–326. doi: 10.1093/aje/kwf207. [DOI] [PubMed] [Google Scholar]
- Dow WH, Schoeni RF, Adler NE, Stewart J. Evaluating the evidence base: Policies and interventions to address socioeconomic status gradients in health. Annals of the New York Academy of Sciences. 2010;1186:240–251. doi: 10.1111/j.1749-6632.2009.05386.x. [DOI] [PubMed] [Google Scholar]
- Duncan C, Jones K, Moon G. Smoking and deprivation: Are there neighbourhood effects? Social Science and Medicine. 1999;48:497–505. doi: 10.1016/s0277-9536(98)00360-8. [DOI] [PubMed] [Google Scholar]
- Fagan P, Moolchan ET, Lawrence D, Fernander A, Ponder PK. Identifying health disparities across the tobacco continuum. Addiction. 2007;102:5–29. doi: 10.1111/j.1360-0443.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- Finney Rutten LJ, Wanke K, Augustson E. Systems and individual factors associated with smoking status: Evidence from HINTS. American Journal of Health Behavior. 2005;29:302–310. doi: 10.5993/ajhb.29.4.2. [DOI] [PubMed] [Google Scholar]
- Foulds J, Gandhi KK, Steinberg MB, Richardson DL, Williams JM, Burke MV, et al. Factors associated with quitting smoking at a tobacco dependence treatment clinic. American Journal of Health Behavior. 2006;30:400–412. doi: 10.5555/ajhb.2006.30.4.400. [DOI] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gerlach KK, Shopland DR, Hartman AM, Gibson JT, Pechacek TF. Workplace smoking policies in the United States: Results from a national survey of more than 100 000 workers. Tobacco Control. 1997;6:199–206. doi: 10.1136/tc.6.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giskes K, Van Lenthe FJ, Turrell G, Brug J, Mackenbach JP. Smokers living in deprived areas are less likely to quit: A longitudinal follow-up. Tobacco Control. 2006;15:485–488. doi: 10.1136/tc.2006.015750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: A review of the research. American Journal of Community Psychology. 2007;40:313–332. doi: 10.1007/s10464-007-9134-z. [DOI] [PubMed] [Google Scholar]
- Henriksen L, Feighery EC, Schleicher NC, Cowling DW, Kline RS, Fortmann SP. Is adolescent smoking related to the density and proximity of tobacco outlets and retail cigarette advertising near schools? Preventive Medicine. 2008;47:210–214. doi: 10.1016/j.ypmed.2008.04.008. [DOI] [PubMed] [Google Scholar]
- Holzer HJ, Offner P, Sorensen E. What explains the continuing decline in labor force activity among young black men1. Labor History. 2005;46:37–55. [Google Scholar]
- Hughes MC, Yette EM, Hannon PA, Harris JR, Tran NM, Reid TR. Promoting tobacco cessation via the workplace: Opportunities for improvement. Tobacco Control. 2011 doi: 10.1136/tc.2010.041038. [DOI] [PubMed] [Google Scholar]
- Janlert U, Hammarström A. Which theory is best? Explanatory models of the relationship between unemployment and health. BMC Public Health. 2009;9 doi: 10.1186/1471-2458-9-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John R, Cheney MK, Azad MR. Point-of-sale marketing of tobacco products: Taking advantage of the socially disadvantaged? Journal of Health Care for the Poor and Underserved. 2009;20:489–506. doi: 10.1353/hpu.0.0147. [DOI] [PubMed] [Google Scholar]
- Jones AP, van Sluijs EMF, Ness AR, Haynes R, Riddoch CJ. Physical activity in children: Does how we define neighbourhood matter? Health and Place. 2010;16:236–241. doi: 10.1016/j.healthplace.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendzor DE, Businelle MS, Mazas CA, Cofta-Woerpel LM, Reitzel LR, Vidrine JI, et al. Pathways between socioeconomic status and modifiable risk factors among African American smokers. Journal of Behavioral Medicine. 2009;32:545–557. doi: 10.1007/s10865-009-9226-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendzor DE, Cofta-Woerpel LM, Mazas CA, Li Y, Vidrine JI, Reitzel LR, et al. Socioeconomic status, negative affect, and modifiable cancer risk factors in African-American smokers. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:2546–2554. doi: 10.1158/1055-9965.EPI-08-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinschmidt I, Hills M, Elliott P. Smoking behaviour can be predicted by neighbourhood deprivation measures. Journal of Epidemiology and Community Health. 1995;49:S72–S77. doi: 10.1136/jech.49.suppl_2.s72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/Ethnicity, Gender, and Monitoring Socioeconomic Gradients in Health: Comparison of Area-Based Socioeconomic Measures - The Public Health Disparities Geocoding Project. American Journal of Public Health. 2003;93:1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo DR, Johnson JC, Kruse RL, Brownson RC, Hewett JE. A prospective investigation of the impact of smoking bans on tobacco cessation and relapse. Tobacco Control. 2001;10:267–272. doi: 10.1136/tc.10.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson L, Tull MT, Matusiewicz AK, Rodman S, Strong DR, Kahler CW, et al. Randomized Controlled Trial of Behavioral Activation Smoking Cessation Treatment for Smokers With Elevated Depressive Symptoms. Journal of Consulting and Clinical Psychology. 2010;78:55–61. doi: 10.1037/a0017939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marti J. Successful smoking cessation and duration of abstinence-an analysis of socioeconomic determinants. International Journal of Environmental Research and Public Health. 2010;7:2789–2799. doi: 10.3390/ijerph7072789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson FI, Moineddin R, Dunn JR, Creatore MI, Gozdyra P, Glazier RH. Urban neighborhoods, chronic stress, gender and depression. Social Science and Medicine. 2006;63:2604–2616. doi: 10.1016/j.socscimed.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annual Review of Psychology. 2011;62:501–530. doi: 10.1146/annurev.psych.031809.130711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesirable life events. Journal of Health and Social Behavior. 1990;31:162–172. [PubMed] [Google Scholar]
- Niederdeppe J, Farrelly MC, Nonnemaker J, Davis KC, Wagner L. Socioeconomic variation in recall and perceived effectiveness of campaign advertisements to promote smoking cessation. Social Science and Medicine. 2011;72:773–780. doi: 10.1016/j.socscimed.2010.12.025. [DOI] [PubMed] [Google Scholar]
- Novotny TE, Warner KE, Kendrick JS, Remington PL. Smoking by blacks and whites: Socioeconomic and demographic differences. American Journal of Public Health. 1988;78:1187–1189. doi: 10.2105/ajph.78.9.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öhlander E, Vikström M, Lindström M, Sundquist K. Neighbourhood non-employment and daily smoking: A population-based study of women and men in Sweden. European Journal of Public Health. 2006;16:78–84. doi: 10.1093/eurpub/cki047. [DOI] [PubMed] [Google Scholar]
- Ostrove JM, Feldman P. Education, income, wealth, and health among Whites and African Americans. Annals of the New York Academy of Sciences. 1999;896:335–337. doi: 10.1111/j.1749-6632.1999.tb08133.x. [DOI] [PubMed] [Google Scholar]
- Pisinger C, Vestbo J, Borch-Johnsen K, Jørgensen T. Smoking cessation intervention in a large randomised population-based study. The Inter99 study. Preventive Medicine. 2005;40:285–292. doi: 10.1016/j.ypmed.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Reijneveld SA. The impact of individual and area characteristics on urban socioeconomic differences in health and smoking. International Journal of Epidemiology. 1998;27:33–40. doi: 10.1093/ije/27.1.33. [DOI] [PubMed] [Google Scholar]
- Reitzel LR, Cromley EK, Li Y, Cao Y, Mater RD, Mazas CA, et al. The effect of tobacco outlet density and proximity on smoking cessation. American Journal of Public Health. 2011;101:315–320. doi: 10.2105/AJPH.2010.191676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE. Walking, exercising, and smoking: Does neighborhood matter? Social Science and Medicine. 2000;51:265–274. doi: 10.1016/s0277-9536(99)00451-7. [DOI] [PubMed] [Google Scholar]
- Ross NA, Tremblay S, Graham K. Neighbourhood influences on health in Montréal, Canada. Social Science and Medicine. 2004;59:1485–1494. doi: 10.1016/j.socscimed.2004.01.016. [DOI] [PubMed] [Google Scholar]
- Sampson RJ, Groves WB. Community Structure and Crime: Testing Social-Disorganization Theory. American Journal of Sociology. 1989;94:774–802. [Google Scholar]
- Schaap MM, Kunst AE. Monitoring of socio-economic inequalities in smoking: Learning from the experiences of recent scientific studies. Public Health. 2009;123:103–109. doi: 10.1016/j.puhe.2008.10.015. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Israel BA, Zenk SN, Parker EA, Lichtenstein R, Shellman-Weir S, et al. Psychosocial stress and social support as mediators of relationships between income, length of residence and depressive symptoms among African American women on Detroit’s eastside. Social Science & Medicine. 2006;62:510–522. doi: 10.1016/j.socscimed.2005.06.028. [DOI] [PubMed] [Google Scholar]
- Shavers VL. Measurement of socioeconomic status in health disparities research. Journal of the National Medical Association. 2007;99:1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Shohaimi S, Luben R, Wareham N, Day N, Bingham S, Welch A, et al. Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class. A cross sectional study in the Norfolk cohort of the European Investigation into Cancer (EPIC-Norfolk) Journal of Epidemiology and Community Health. 2003;57:270–276. doi: 10.1136/jech.57.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shopland DR, Gerlach KK, Burns DM, Hartman AM, Gibson JT. State-specific trends in smoke-free workplace policy coverage: The current population survey tobacco use supplement, 1993 to 1999. Journal of Occupational and Environmental Medicine. 2001;43:680–686. doi: 10.1097/00043764-200108000-00005. [DOI] [PubMed] [Google Scholar]
- Siahpush M, Jones PR, Singh GK, Timsina LR, Martin J. Association of availability of tobacco products with socio-economic and racial/ethnic characteristics of neighbourhoods. Public Health. 2010a;124:525–529. doi: 10.1016/j.puhe.2010.04.010. [DOI] [PubMed] [Google Scholar]
- Siahpush M, Jones PR, Singh GK, Timsina LR, Martin J. The association of tobacco marketing with median income and racial/ethnic characteristics of neighbourhoods in Omaha, Nebraska. Tobacco Control. 2010b;19:256–258. doi: 10.1136/tc.2009.032185. [DOI] [PubMed] [Google Scholar]
- Smith KC, Stillman F, Bone L, Yancey N, Price E, Belin P, et al. Buying and selling “loosies” in Baltimore: The informal exchange of cigarettes in the community context. Journal of Urban Health. 2007;84:494–507. doi: 10.1007/s11524-007-9189-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafford M, Duke-Williams O, Shelton N. Small area inequalities in health: Are we underestimating them? Social Science and Medicine. 2008;67:891–899. doi: 10.1016/j.socscimed.2008.05.028. [DOI] [PubMed] [Google Scholar]
- Statistics B.o.L. The Employment Situation. 2011 Mar; 2011. [Google Scholar]
- Stillman FA, Bone L, Avila-Tang E, Smith K, Yancey N, Street C, et al. Barriers to smoking cessation in inner-city African American young adults. American Journal of Public Health. 2007;97:1405–1408. doi: 10.2105/AJPH.2006.101659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpson JP, Ju H, Raji MA, Eschbach K. Neighborhood deprivation and health risk behaviors in NHANES III. American Journal of Health Behavior. 2007;31:215–222. doi: 10.5555/ajhb.2007.31.2.215. [DOI] [PubMed] [Google Scholar]
- Swan GE, McClure JB, Jack LM, Zbikowski SM, Javitz HS, Catz SL, et al. Behavioral Counseling and Varenicline Treatment for Smoking Cessation. American Journal of Preventive Medicine. 2010;38:482–490. doi: 10.1016/j.amepre.2010.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. Pearson Education, Inc.; Boston: 2007. Cleaning up your act: Screening data prior to Analysis; pp. 60–116. [Google Scholar]
- Tarlov AR. Public policy frameworks for improving population health. Annals of the New York Academy of Sciences. 1999;896:281–293. doi: 10.1111/j.1749-6632.1999.tb08123.x. [DOI] [PubMed] [Google Scholar]
- Ten Have TR, Uttal DH. Subject-specific and population-averaged continuation ration logit models for multiple discrete time survival profiles. Journal of the Royal Statistical Society. Series C, Applied Statistics. 1994;43:371–384. [Google Scholar]
- Turner RJ, Lloyd DA. The stress process and the social distribution of depression. Journal of Health & Social Behavior. 1999;40:374–404. [PubMed] [Google Scholar]
- Van Lenthe FJ, Mackenbach JP. Neighbourhood and individual socioeconomic inequalities in smoking: The role of physical neighbourhood stressors. Journal of Epidemiology and Community Health. 2006;60:699–705. doi: 10.1136/jech.2005.043851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Reitzel LR, Wetter DW. The role of tobacco in cancer health disparities. Current Oncology Reports. 2009;11:475–481. doi: 10.1007/s11912-009-0064-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilhjalmsson R. Life stress, social support and clinical depression: a reanalysis of the literature. Social Science & Medicine. 1993;37:331–342. doi: 10.1016/0277-9536(93)90264-5. [DOI] [PubMed] [Google Scholar]
- Waldron I, Lye D. Employment, unemployment, occupation, and smoking. American Journal of Preventive Medicine. 1989;5:142–149. [PubMed] [Google Scholar]
- Webb MS, de Ybarra DR, Baker EA, Reis IM, Carey MP. Cognitive-Behavioral Therapy to Promote Smoking Cessation Among African American Smokers: A Randomized Clinical Trial. Journal of Consulting and Clinical Psychology. 2010;78:24–33. doi: 10.1037/a0017669. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Cofta-Gunn L, Irvin JE, Fouladi RT, Wright K, Daza P, et al. What accounts for the association of education and smoking cessation? Preventive Medicine. 2005;40:452–460. doi: 10.1016/j.ypmed.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Yen IH, Moss N. Unbundling education: A critical discussion of what education confers and how it lowers risk for diease and death. Annals of the New York Academy of Sciences. 1999;896:350–351. doi: 10.1111/j.1749-6632.1999.tb08138.x. [DOI] [PubMed] [Google Scholar]