Abstract
Objectives
The prevalence of both negative (distress) and positive responses (growth, well-being) to the cancer experience is examined and difficulties in establishing the prevalence of these responses discussed. A conceptual framework for understanding factors associated with psychological health in cancer survivors is presented. Finally, strategies for promoting psychological health in cancer survivors are examined.
Data Sources
Review of the literature.
Conclusions
Psychological health in cancer survivors is defined by the presence or absence of distress as well as the presence or absence of positive well-being and psychological growth. Furthermore, psychological health in cancer survivors is determined by the balance between two classes of factors: the stress and burden posed by the cancer experience and the resources available for coping with this stress and burden.
Implications for nursing practice
In general, promotion of psychological health is based upon the prevention or treatment of distress as well as the encouragement of growth and well-being. Periodic screening for psychological distress across the cancer trajectory is critical to appropriate management of distress.
Introduction: Psychological Health in Cancer Survivors
A range of physical, social, psychological, and existential stressors are associated with cancer diagnosis and treatment. These multiple and often chronic stressors can cause cancer patients and survivors to experience considerable distress. Distress is a generic term that encompasses a variety of psychological responses including depression, sadness, anxiety, fear, worry, anger, or panic. The experience of distress in the immediate aftermath of a cancer diagnosis is not unexpected. Nor is it surprising that cancer patients may experience distress while undergoing treatment for their disease. Less well recognized, however, is the potential for cancer survivors to experience distress attributable to their cancer experience long after completion of primary cancer treatment and indeed across the survivorship trajectory.
Consistent with a view that good health encompasses more than simply the absence of disease, psychological health in cancer survivors encompasses more than simply the presence or absence of distress. Rather, understanding of the psychological health of cancer survivors requires consideration of the potential for survivors to also manifest psychological responses associated with enhanced psychological adjustment and well-being. In other words, psychological health in cancer survivors is determined by both the presence or absence of distress as well as the presence or absence of a variety of positive psychological responses often subsumed under the concept of “posttraumatic growth” [1-3]. These positive psychological responses include such things as enhanced self-esteem, greater life appreciation and meaning, heightened spirituality, benefit-finding, or greater feelings of peacefulness and purposefulness. Interestingly, some evidence suggests that distress and growth are not mutually exclusive. Rather, elements of both positive (growth, well-being) and negative (distress) psychological adjustment can be experienced concurrently by cancer survivors [2].
The remainder of this paper will be devoted to discussion of the psychological health of cancer survivors. We will focus upon both negative (distress) and positive (growth, well-being) psychological responses evidenced by cancer survivors. We will address the prevalence of specific psychological responses that can be important determinants of the psychological health of cancer survivors, offer a framework for understanding “risk” factors for these responses, and discuss the promotion of psychological health in cancer survivors. Due to space limitations, our discussion will necessarily be an overview rather than an in depth treatment of these topics. Furthermore, our discussion of psychological health in cancer survivors will focus upon psychological responses and consequently we will not focus upon other late or long term effects often present in cancer survivors including sexual dysfunction, sleep disturbance, fatigue, or cognitive impairment. However, these are important phenomena associated with the cancer experience and their presence or absence can certainly influence the psychological health of cancer survivors.
When considering the psychological health of cancer survivors, the research literature has typically emphasized the potential for depression and anxiety. The prevalence of depression in individuals with cancer has been estimated to range from 0% to 58% [4-5]. The prevalence of anxiety disorders has been estimated to be 6% to 23% [6]. The wide range represented by these estimates reflects the difficulties involved in identifying the prevalence of specific psychological responses associated with the cancer experience. Foremost among these difficulties is the lack of consensus about how to define when a particular response is present or absent. In order to identify cases of depression or anxiety in cancer survivors some studies employ formal psychiatric diagnostic criteria, others use cut-off scores on a questionnaire, while others might use a survivor’s response to a single item or question. Thus, the presence or absence of “depression” or “anxiety” in cancer survivors is defined in a variety of ways. Wide variability across research studies in prevalence estimates for depression and anxiety also stems from wide variability in the case mix present both within and across study samples. Risk for depression or anxiety in a cancer survivor likely varies as a function of type of cancer diagnosis, disease stage at diagnosis, type of treatment received, age, race and ethnicity, gender, and time point in the survivorship trajectory when these responses are assessed. Variability in these factors across studies limits contributes to the wide range of prevalence estimates for depression and anxiety found in the literature.
The difficulties associated with identifying precise prevalence estimates for depression and anxiety in cancer survivors are equally present when positive psychological responses (growth, well-being) are considered. The lack of consensus regarding how to define or measure the presence or absence of these positive psychological responses is particularly pronounced. The absence of an appropriate taxonomy and set of definitional criteria make it impossible to estimate the prevalence of positive psychological responses, such as enhanced self-esteem or self-efficacy, greater sense of meaning in life, etc. in cancer survivors. Consequently, we know positive psychological responses are present in cancer survivors but really have no good idea of their prevalence and associated factors. Clearly, there is much research opportunity in this area. For the field to advance, however, there will need to be greater consensus regarding how to define and measure specific positive psychological responses.
While depression and anxiety have served as the focus of research examining negative psychological responses in cancer survivors, other types of distress have received attention of late. Many disease-free cancer survivors experience some degree of anxiety over the possibility of a cancer recurrence [7]. If persistent and severe, such fears can be distressing and can negatively impact quality of life. While self-report inventories have been developed to measure fear of recurrence [8], there is no agreement regarding how much fear of recurrence must be present (or for how long) to constitute a clinically significant “case” for the purpose of estimating its prevalence. Until consensus is developed regarding the defining characteristics of “fear of recurrence” it is impossible to estimate its prevalence in cancer survivors.
Feeling one’s future may be cut short is a central element in the fear of cancer recurrence. It is also one of the defining symptoms used to diagnose posttraumatic stress disorder (PTSD). The possibility that cancer survivors might experience PTSD as a result of trauma associated with their cancer experience has been a recent focus of study [9]. It has been estimated that 0-32% of cancer survivors experience PTSD linked to their cancer experience following completion of cancer treatment [9]. This would appear to exceed the base rate of PTSD in the general population, estimated to be in the 1-4% range [10]. However, application of the PTSD concept to understanding psychological response to cancer diagnosis and treatment is not without its difficulties [9]. Several of the defining symptoms associated with PTSD, including memory, sleep, and concentration difficulties, and physical reactions in response to cancer-related stimuli, could be direct effects of disease or treatment and thus not represent a psychological response to trauma. Furthermore, some degree of foreboding about the future is a natural response to a very real threat of recurrence. Nevertheless, whether representative of “true” PTSD or not, research has shown cancer survivors can evidence a constellation of distressing symptoms that are associated with a formal diagnosis of PTSD.
Despite the difficulties noted in identifying the prevalence of distress and positive psychological responses in cancer survivors, some simple generalizations can be offered. First, due to the lack of definitional criteria, virtually nothing is known about the prevalence of positive psychological responses. Second, in general, serious psychiatric disorders, such as major depression or PTSD, are uncommon in cancer survivors [11]. However, cancer survivors do appear to possess at least slightly higher risk for major depression and PTSD, relative to the general population, with certain subgroups appearing to be particularly vulnerable [12-13]. Third, less severe “adjustment” disorders, characterized by the presence of either a depressed or anxious mood or a mixture of both, are a likely consequence of cancer diagnosis and treatment. Derogatis et al. reported a 32% prevalence rate for adjustment disorders in a heterogeneous group of cancer patients [11]. Adjustment disorders are particularly likely in the immediate aftermath of a cancer diagnosis or relatively early in the cancer trajectory as the individual confronts the multiple stressors associated with diagnosis of a life-threatening disease and initiation of an aggressive and often lengthy course of treatment. The prevalence of adjustment disorder later in the survivorship trajectory is largely unknown, however. At this time, a well-done epidemiologic investigation of the prevalence of mild psychiatric disorders, such as adjustment disorder or depressive episodes, in cancer survivors would constitute a significant contribution to the literature.
Factors Associated With Psychological Health in Cancer Survivors
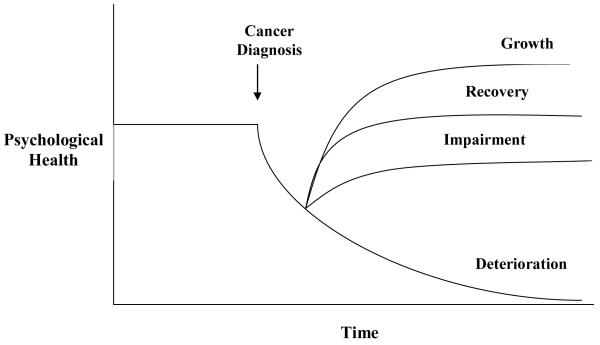
The psychological health of cancer survivors varies widely both across individuals and across time. Figure 1 shows several temporal trajectories of psychological health that might be evidenced. Almost all survivors experience some psychological dislocation in the immediate aftermath of a cancer diagnosis. Many survivors eventually recover from their cancer experience, restore their psychological equilibrium, and reestablish their premorbid level of psychological health. Other survivors rebound from the initial diagnosis and treatment but never recover fully. They may experience minor physical, psychological or social impairments as a result of their cancer experience and thus never quite return to their premorbid level of psychological health. While these two trajectories define the majority of survivors, the cancer experience has a more profound impact on other survivors. For some, a cancer initiates a deteriorating, downward spiral characterized by physical, psychological, and social impairment, a spiral from which they never recover. These individuals seemingly succumb to their illness and evidence poor psychological health. For others, a cancer diagnosis initiates an upward trend characterized by enhanced psychological and social adjustment. These individuals seemingly “grow” in the aftermath of cancer and evidence enhanced psychological health.
Figure 1.
Temporal Trajectories of Psychological Health in Cancer Survivors.
Identification of factors that influence the trajectory of psychological health evidenced by a cancer survivor is a challenge but is theoretically and clinically important. Theoretically, understanding of factors that influence the trajectory of psychological health can increase understanding of the process of psychological adjustment and recovery. Clinically, understanding of the factors that influence the trajectory of psychological health can enable clinical and public health resources to be targeted toward cancer survivors at greatest risk for poor psychological health.
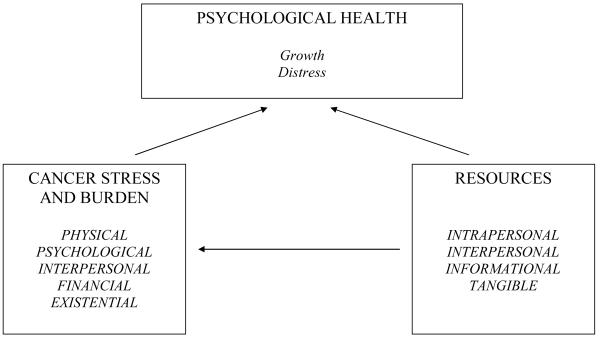
In general, psychological response to the cancer experience is a function of two classes of variables: the stress and burden posed by the cancer experience and the resources available to cope with this stress and burden (See Figure 2). The relative balance of these two factors determines the psychological health of the cancer survivor in the short and long-term. All things being equal, the greater the stress and burden posed by the cancer experience, the greater the risk for poor psychological health. Conversely, the greater the resources available to cope with the stress and burden posed by the cancer experience, the lower the risk for poor psychological health. A couple points should be noted. First, factors can fluctuate across time so the balance between them is dynamic. As one or both factors increase or decrease over time, one would anticipate corresponding changes in psychological health over time. Second, a survivor might be at high risk for poor psychological health even when the stress or burden posed by their cancer experience appears to be low. This would occur if resources were also low. Conversely, an individual might be at low risk for poor psychological health even when the stress or burden posed by their cancer experience appears to be considerable. This similarly paradoxical situation would result if available resources were also considerable.
Figure 2.
Factors associated with psychological health in cancer survivors.
Several additional points are worth noting. First, the stress and burden posed by the cancer experience is multi-faceted. Cancer survivors confront stressors which may be physical, psychological, interpersonal, financial, and/or existential in nature (Figure 2). Consequently, understanding of a survivor’s risk for poor or good psychological health must incorporate information from each of these domains. Second, “stress and burden” is a subjective concept. In other words, “stress is in the eye of the beholder.” The experience of certain physical late effects, such as infertility, fatigue, or weight gain, might be experienced as highly stressful by some cancer survivors while much less stressful by other survivors. Similarly, a poor prognosis might be a persistent source of dread for some cancer survivors while others are more sanguine regarding the same objective prognosis. Consequently, understanding of a survivor’s risk for poor or good psychological health must include not just an objective account of the stresses or burdens confronting them but must also consider their subjective response to those presumed stressors. Finally, the stress and burden posed by the cancer experience is dynamic and fluid across time. Early in the survivorship trajectory, the stress of the cancer experience might be characterized by the existential threat posed by a potentially life-threatening illness, the difficulties involved in making treatment decisions under uncertainty, and anxiety regarding how one will respond to treatment. Later in the survivorship trajectory, the stress of the cancer experience might be characterized by fear that cancer might recur, financial difficulties resulting from loss of employment, difficulties with sexuality and intimacy, or recognition of persistent physical late effects of treatment. Consequently, understanding of a survivor’s risk for poor or good psychological health is based upon knowledge of how the specific stresses and burdens confronting that survivor evolve over time.
The resources available to the survivor to cope with the stress and burden of their cancer experience are also multifaceted. These resources can be grouped into four general categories: intrapersonal, interpersonal, informational, and tangible (Figure 2).
Intrapersonal resources are characteristics which are internal to the cancer survivor. These characteristics might be dispositional in nature and reflect tendencies to think or act in certain ways. When present, these characteristics result in better coping while their absence results in poorer coping. Intrapersonal resources linked to better psychological health in cancer survivors include optimism [14], self-efficacy [15], emotional intelligence [16], and spirituality [17]
Social support is an interpersonal resource which has been linked to better psychological health in cancer patients and survivors [18]. In general, better coping with the stresses and burdens posed by the cancer experience is fostered when the cancer survivor is embedded within a supportive social environment, one which facilitates their efforts to cognitively and emotionally process their cancer experience [19]. Conversely, the presence of social constraints can impede the coping process, resulting in poorer psychological health [16]. Social constraints represent efforts by individuals to prevent or inhibit a cancer survivor from talking about their cancer experience. Such social constraints are thought to inhibit the cognitive and emotional processing critical to the coping process and would thus be considered a risk factor for poor psychological health.
Informational resources are also important determinants of the psychological health of a cancer survivor. Access to accurate and understandable information about their disease, treatment side effects, prognosis, and available support services in their community can be a valuable resource. Greater education is often linked to better psychological health in cancer patients and survivors [20]. More educated individuals might elicit more information from their care providers, seek additional information on their own, or better understand the information that is provided them. Information might foster appropriate expectations about risk for long-term recovery. Inappropriate expectations regarding physical late effects and long-term recovery can increase risk for poorer psychological adjustment in survivors [21]. Interestingly, knowledge may not always be power in the cancer setting. Individuals differ in their preferences with regard to the type, amount, and depth of information they are comfortable with. Some people are monitors and tend to actively seek information and are comfortable with efforts to provide them with as much information as possible. Others are blunters and tend to actively avoid information and thus may be uncomfortable with large amounts of detailed information [22]. So the value of information as a resource in the cancer setting may be moderated by the individual’s information seeking preferences. While information might enhance psychological health for some survivors, the same information might increase risk for poorer psychological health in others.
Finally, coping with the stress and burden posed by the cancer experience is facilitated by access to tangible resources. Cancer survivors receive medical care in a variety of settings including large academic medical centers, small community hospitals, and private physicians’ offices. The type, extent, and quality of psychological support services that are available to survivors differ enormously across these diverse settings. Available support services might include licensed therapists and social workers, support groups, formal “navigator systems” or informal peer-to-peer networks. Special clinics devoted to the medical and support needs of cancer survivors have been developed [23]. Poorer access to these support resources is associated with greater risk for poor psychological health. Mental health resources available in the community represent additional tangible resources that can affect survivors’ psychological health. Finally, while money can’t buy happiness, money can facilitate access to resources (education, vocational retraining, mental health services, child-care or housekeeping assistance) that can foster better coping with the stresses and burdens imposed by the cancer experience and thus impact psychological health.
In conclusion, there is a large literature linking a variety of specific demographic, clinical, dispositional, psychosocial, and health system variables to psychological health in cancer survivors. The results of these studies are mixed, suggesting few individual variables possess strong predictive power in isolation. In general, the focus has been upon identifying “risk factors” for poor psychological health in cancer survivors with less effort devoted to identifying “risk factors” for good psychological health. It should also be noted that risk factors for poor and good psychological health are likely not the obverse of each other. For example, while lack of social support has been linked to poor psychological health, it does not necessarily follow that provision of adequate social support results in good psychological health. Good psychological health might be determined by factors that don’t necessarily correspond to those that determine risk for poor psychological health.
Promotion of Psychological Health in Cancer Survivors
Currently, prevention or minimization of distress is almost always the focus of clinical efforts to promote psychological health in cancer survivors. This is not surprising given the traditional focus in both the mental and physical health professions upon the prevention and treatment of “disease.” However, as psychological health includes elements such as life satisfaction, purpose in life, and self-acceptance, in addition to the absence of distress [24-25], fostering of positive psychological responses in cancer survivors may also be a worthy goal.
Clinical management of distress in cancer survivors is predicated on successful recognition of distress when it is present. To do so, it must be recognized that cancer survivors are at risk for distress and this risk continues to exist across the survivorship trajectory. Individuals who appear to be doing well early in the survivorship trajectory may still be at risk for distress later on in this trajectory. This suggests the continued need for careful monitoring of distress in cancer survivors throughout the entire survivorship trajectory. Implementation of distress screening procedures is essential to the monitoring and management of distress in cancer survivors, as evidence-based distress management intervention can be effective only given successful identification of those in need.
Distress screening requires a systematic approach. In the absence of formal screening procedures, research has repeatedly shown that health care providers are poor at recognizing clinically significant distress in cancer patients and survivors [26]. Fortunately, systematic approaches to distress screening in cancer survivors have been developed [27-28]. Most notably, the National Comprehensive Cancer Network has published detailed guidelines for recognizing and managing distress in cancer survivors [28]. They advocate periodic screening of all cancer survivors using a “distress thermometer” to gauge the magnitude of distress accompanied by a problem checklist to identify potential sources of distress (Figure 3). A rating of “5” or greater on the 10-point distress thermometer is believed to indicate moderate to severe distress that warrants additional follow-up consisting of more in-depth evaluation and treatment, if necessary. While some evidence suggests a thermometer rating of “4” may be a better cut-off for identifying potential cases of clinically significant distress [29], the distress thermometer approach, in general, appears to be a useful means of identifying cancer survivors who could benefit from more thorough distress evaluation and/or intervention procedures. Having said this, however, it must be recognized that any screening approach is not infallible. Some survivors with clinically significant distress might fail to meet whatever distress criterion is used. So while a formal distress screening protocol is certainly recommended, it must be supplemented with sound clinical awareness and judgment.
A large body of research has examined the impact of a variety of psychoeducational interventions for managing distress in cancer patients and survivors. Several excellent reviews and meta-analyses of this literature are available [30-32]. In general, results suggest intervention is beneficial, although effect sizes may be quite modest and benefits are not evident for all types of outcomes, for all types of interventions or across all intervention recipients [33-34]. The few studies that have pre-screened participants and included only those evidencing some threshold level of distress have generally demonstrated stronger benefits of intervention [32].
In considering the benefits of various interventions for managing distress in cancer survivors, it is important to distinguish between interventions intended to prevent distress and interventions intended to treat distress. This important distinction has largely been ignored in the intervention research literature to date. Most intervention studies have included both currently distressed and well-functioning cancer patients and survivors in their study sample, suggesting some ambiguity regarding intervention purpose. If the intent of an intervention is to treat existing distress, then currently well-functioning individuals should be excluded from the target population. On the other hand, if the intent of an intervention is to prevent the development of distress, then individuals already evidencing some threshold level of distress should be excluded from study. Furthermore, what characterizes a successful intervention might differ as a function of whether prevention or treatment of distress is the goal. At this time, few clinical interventions have set out explicitly to prevent distress in cancer patients, and, unfortunately, their efforts have been largely unsuccessful [35].
Finally, while a great deal of intervention research in the cancer setting is available, the relevance of much of this research to the question of how to manage distress in cancer survivors is uncertain. Most intervention studies have been implemented with cancer patients who are relatively early in their cancer trajectory – oftentimes while they are undergoing treatment. Coupled with the typically short follow-up periods over which treatment effects are monitored, much of the existing research may reveal little about distress management in survivors at later points in the cancer trajectory.
In contrast to the large literature focusing upon distress management in cancer patients and survivors, very little research has looked at whether and how positive psychological responses could be fostered in cancer survivors. Antoni et al. [36] and Penedo et al. [37] reported greater benefit finding in breast and prostate cancer patients, respectively, after participating in a group-based, cognitive behavioral stress management intervention. However, the focus of the intervention was on preventing or minimizing distress rather than explicitly fostering benefit-finding or other positive outcomes. In contrast, other researchers have tested interventions explicitly designed to foster positive outcomes such as meaning making [38] or greater self-esteem, optimism, and self-efficacy [39]. While results have been promising additional research is needed to identify which survivors might benefit most from interventions designed to enhance positive outcomes, and when in the cancer trajectory interventions to promote positive outcomes might be most worthwhile
As psychological health should not be equated with the absence of distress [25], it is likely that clinical strategies that successfully minimize distress may not be the same as those which promote positive psychological outcomes (e.g., benefit finding). However, in all fairness, most research examining the impact of interventions designed to manage distress in the cancer setting have not measured changes in positive outcomes. Thus, it is possible more typical distress management interventions may also foster psychological health in its broader sense.
In our view, development of clinical strategies for enhancing positive psychological outcomes in cancer survivors is an important area for further study. Efforts in this regard could benefit from consideration of recent developments in “positive psychology” [40], including research on how to increase psychological well-being in generally healthy individuals. Emmons and McCullough found listing things one is grateful or thankful for increased well-being in college students and individuals with neuromuscular disease relative to comparison groups [41]. Jain et al. found an abbreviated Mindfulness-Based Stress Reduction intervention decreased distress and increased positive psychological states, including increased focused attention, productivity, responsible caretaking, and pleasure, in distressed college students [42]. Finally, Seligman, Steen, Park, and Peterson found using one’s “signature strengths” in new ways, focusing on good things in life and their causal explanations, and writing (and delivering) a gratitude letter to someone led to decreased depressive symptoms and increased happiness [43].
Psychological Health in Cancer Survivors: A Final Thought
The cancer experience is a dynamic entity. Consequently the concept of psychological health in cancer survivors may be a dynamic entity. The physical, psychological, social, and existential stressors associated with cancer diagnosis and treatment today might be markedly different from those that may be associated with cancer diagnosis and treatment tomorrow. Consequently, the spectrum and prevalence of psychological responses, both negative and positive, associated with a specific constellation of disease, treatment, and patient characteristics might change with the passage of time. To appreciate the truth in this assertion, one only needs to consider how the experience of breast cancer has changed over the past 50 years. Early reports from the 1950’s of the psychological impact of breast cancer stressed the potential for anger, anxiety, depression, helplessness, stigma, and social isolation [44]. Today, 50 years later, one is equally likely to hear the psychological impact of breast cancer described in terms of opportunity, empowerment, and social connection [45-46].
References
- 1.Cordova MJ, Andrykowski MA. Responses to cancer diagnosis and treatment: Posttraumatic stress and posttraumatic growth. Semin Clin Neuropsychiatry. 2003;8:286–296. [PubMed] [Google Scholar]
- 2.Cordova MJ, Cunningham LC, Carlson CR, Andrykowski MA. Posttraumatic growth following breast cancer: A controlled comparison study. Health Psychol. 2001;20:176–185. [PubMed] [Google Scholar]
- 3.Stanton AL, Bower JE, Low CA. Posttraumatic growth after cancer. In: Calhoun LG, Tedeschi RG, editors. Handbook of posttraumatic growth: Research and practice. Lawrence Erlbaum Associates, Inc; Mahwah, NJ: 2006. pp. 138–175. [Google Scholar]
- 4.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;32:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 5.Pirl WF. Evidence report on the occurrence, assessment, and treatment of depression in cancer patients. J Natl Cancer Inst Monogr. 2004;32:32–39. doi: 10.1093/jncimonographs/lgh026. [DOI] [PubMed] [Google Scholar]
- 6.Stark DPH, House A. Anxiety in cancer patients. Brit J Cancer. 2000;83:1261–1267. doi: 10.1054/bjoc.2000.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee-Jones C, Humphries G, Dixon R, Hatcher MB. Fear of cancer recurrence: A literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology. 1997;6:95–105. doi: 10.1002/(SICI)1099-1611(199706)6:2<95::AID-PON250>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 8.Vickberg SM. The Concerns About Recurrence Scale (CARS): A systematic measure of women’s fears about the possibility of breast cancer recurrence. Ann Behav Med. 2003;25:16–24. doi: 10.1207/S15324796ABM2501_03. [DOI] [PubMed] [Google Scholar]
- 9.Kangas M, Henry JL, Bryant RA. Posttraumatic stress disorder following cancer. A conceptual and empirical review. Clin Psychol Rev. 2002;22:499–524. doi: 10.1016/s0272-7358(01)00118-0. [DOI] [PubMed] [Google Scholar]
- 10.Sareen J, Cox BJ, Stein MB, Affifi TO, Fleet C, Asmundson GJ. Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosom Med. 2007;69:242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- 11.Derogatis LR, Morrow GR, Fetting D, et al. The prevalence of psychiatric disorders among cancer patients. JAMA. 1983;249:751–756. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 12.Black EK, White CA. Fear of recurrence, sense of coherence, and posttraumatic stress disorder in haematological cancer survivors. Psychooncology. 2005;14:510–515. doi: 10.1002/pon.894. [DOI] [PubMed] [Google Scholar]
- 13.Kangas M, Henry JL, Bryant RA. The course of psychological disorders in the 1st year after cancer diagnosis. J Consult Clin Psychol. 2005;73:763–768. doi: 10.1037/0022-006X.73.4.763. [DOI] [PubMed] [Google Scholar]
- 14.Carver CS, Smith RG, Antoni MH, Petronis VM, Weiss S, Derhagopian RP. Optimistic personality and psychosocial well-being during treatment predicit psychosocial adjustment among long-term survivors of breast cancer. Health Psychol. 2005;24:508–516. doi: 10.1037/0278-6133.24.5.508. [DOI] [PubMed] [Google Scholar]
- 15.Manne SL, Ostroff JS, Norton TR, Fox K, Grana G, Goldstein L. Cancer-specific self-efficacy and psychosocial and functional adaptation to early stage breast cancer. Ann Behav Med. 2006;31:145–154. doi: 10.1207/s15324796abm3102_6. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt JE, Andrykowski MA. The role of social and dispositional variables associated with emotional processing in adjustment to breast cancer: An internet-based study. Health Psychol. 2004;23:259–266. doi: 10.1037/0278-6133.23.3.259. [DOI] [PubMed] [Google Scholar]
- 17.Krupski TL, Kwan L, Fink A, Sonn GA, Maliski S, Litwin MS. Spirituality influences health related quality of life in men with prostate cancer. Psychooncology. 2006;15:121–131. doi: 10.1002/pon.929. [DOI] [PubMed] [Google Scholar]
- 18.Helgeson VS, Cohen S. Social support and adjustment to cancer: Reconciling descriptive, correlational, and intervention research. Health Psychol. 1996;15:135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 19.Lepore SJ. A social-cognitive processing model of emotional adjustment to cancer. In: Baum A, Andersen B, editors. Psychosocial interventions for cancer. American Psychological Association; Washington, DC: 2001. pp. 99–118. [Google Scholar]
- 20.Parker PA, Baile WF, de Moor C, Cohen L. Psychological and demographic predictors of quality of life in a large sample of cancer patients. Psychooncology. 2003;12:183–193. doi: 10.1002/pon.635. [DOI] [PubMed] [Google Scholar]
- 21.Andrykowski MA, Brady MJ, Greiner CB, et al. “Returning to normal” following bone marrow transplantation: Outcomes, expectations, and informed consent. Bone Marrow Transplant. 2005;15:573–581. [PubMed] [Google Scholar]
- 22.Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease: Implications for cancer screening and management. Cancer. 1995;76:161–177. doi: 10.1002/1097-0142(19950715)76:2<167::aid-cncr2820760203>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 23.Hollen PJ, Hobbie WL. Establishing comprehensive follow-up clinics for long-term survivors of cancer: Providing systematic physiological and psychosocial support. Support Care Cancer. 1995;3:40–44. doi: 10.1007/BF00343920. [DOI] [PubMed] [Google Scholar]
- 24.Diener E, Suh EM, Lucas RE, Smith HL. Subjective well-being: Three decades of progress. Psychol Bull. 1999;125:276–302. [Google Scholar]
- 25.Keyes CL, Shmotking D, Ryff CD. Optimizing well-being: The empirical encounter of two traditions. J Pers Soc Psychol. 2002;82:1007–1022. [PubMed] [Google Scholar]
- 26.Passik SD, Dugan W, McDonald MV, Rosenfeld B, Theobald DE, Edgerton S. Oncologists’ recognition of depression in their patients with cancer. J Clin Oncol. 1998;16:1594–1600. doi: 10.1200/JCO.1998.16.4.1594. [DOI] [PubMed] [Google Scholar]
- 27.Loscalzo MJ, Clark KL. Problem-related distress in cancer patients drives requests for help: A prospective study. Oncology. 2007;21:1133–1138. [PubMed] [Google Scholar]
- 28.National Comprehensive Cancer Network (NCCN) Distress management practice guidelines. J Natl Compr Cancer Netw. 2003;1:344–374. doi: 10.6004/jnccn.2003.0031. [DOI] [PubMed] [Google Scholar]
- 29.Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494–1502. doi: 10.1002/cncr.20940. [DOI] [PubMed] [Google Scholar]
- 30.Barsevick AM, Sweeney C, Haney E, Chung E. A systematic, qualitative analysis of psycheducational interventions for depression in patients with cancer. Oncol Nurs Forum. 2002;29:73–84. doi: 10.1188/02.ONF.73-87. [DOI] [PubMed] [Google Scholar]
- 31.Newell SA, Sanson-Fisher RW, Savolainen NJ. Systematic review of psychological therapies for cancer patients: Overview and recommendations for future research. J Natl Cancer Inst. 2002;94:558–584. doi: 10.1093/jnci/94.8.558. [DOI] [PubMed] [Google Scholar]
- 32.Sheard T, Maguire P. The effect of psychological interventions on anxiety and depression in cancer patients: Results of two meta-analyses. Brit J Cancer. 1999;80:1770–1780. doi: 10.1038/sj.bjc.6690596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andrykowski MA, Manne SL. Are psychological interventions effective and accepted by cancer patients? I. Standards and levels of evidence. Ann Behav Med. 2006;32:93–97. doi: 10.1207/s15324796abm3202_3. [DOI] [PubMed] [Google Scholar]
- 34.Manne SL, Andrykowski MA. Are psychological interventions effective and accepted by cancer patients? II. Using empirically supported therapy guidelines to decide. Ann Behav Med. 2006;32:98–103. doi: 10.1207/s15324796abm3202_4. [DOI] [PubMed] [Google Scholar]
- 35.Maunsell E, Brisson J, Deschenes L, Frasure-Smith N. Randomized trial of a psychologic distress screening program after breast cancer: Effects on quality of life. J Clin Oncol. 1996;14:2747–2755. doi: 10.1200/JCO.1996.14.10.2747. [DOI] [PubMed] [Google Scholar]
- 36.Antoni MM, Lehman JM, Kilbourn KM, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early stage-breast cancer. Health Psychol. 2001;20:20–32. doi: 10.1037//0278-6133.20.1.20. 2001. [DOI] [PubMed] [Google Scholar]
- 37.Penedo FJ, Molton I, Dahn JR, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Ann Behav Med. 2006;31:261–270. doi: 10.1207/s15324796abm3103_8. [DOI] [PubMed] [Google Scholar]
- 38.Lee V, Cohen SR, Edgar L, Laizner AM, Gagnon AJ. Meaning-making intervention during breast or colorectal cancer treatment improves self-esteem, optimism, and self-efficacy. Soc Sci Med. 2006;62:3133–3145. doi: 10.1016/j.socscimed.2005.11.041. [DOI] [PubMed] [Google Scholar]
- 39.Rosenbaum E, Garlan RW, Hirschberger N, Siegel AL, Butler LD, Spiegel D. The Life Tape Project: Increasing family social support and symbolic immortality with a brief existential intervention for cancer patients and their families. Omega. 2006;53:321–339. [Google Scholar]
- 40.Snyder CR, Lopez SJ, editors. Handbook of positive psychology. Oxford University Press; New York, NY: 2005. [Google Scholar]
- 41.Emmons RA, McCullough ME. Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. J Pers Soc Psychol. 2003;8:377–389. doi: 10.1037//0022-3514.84.2.377. [DOI] [PubMed] [Google Scholar]
- 42.Jain S, Shapiro SL, Swanick S, et al. A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Ann Behav Med. 2007;33:11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- 43.Seligman MEP, Steen TA, Park N, Peterson C. Positive psychology progress: Empirical validation of interventions. Am Psychol. 2005;60:410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 44.Bard M, Sutherland AM. Psychological impact of cancer and its treatment: IV. Adaptation to radical mastectomy. Cancer. 1955;8:656–672. doi: 10.1002/1097-0142(1955)8:4<656::aid-cncr2820080403>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 45.Coreil J, Wilke J, Pintado I. Cultural models of illness and recovery in breast cancer support groups. Qual Health Res. 2004;14:905–923. doi: 10.1177/1049732304266656. [DOI] [PubMed] [Google Scholar]
- 46.Kinney CK, Rodgers DM, Nash KA, Bray CO. Holistic health for women with breast cancer through a mind, body, and spirit self-empowerment program. J Holist Nurs. 2003;21:260–279. doi: 10.1177/0898010103254919. [DOI] [PubMed] [Google Scholar]