Abstract
This article modifies the traditional functional leadership model to accommodate contemporary needs in healthcare leadership based on two findings. First, the article argues that it is important that the ideal healthcare leadership emphasizes the outcomes of the patient care more than processes and structures used to deliver such care; and secondly, that the leadership must strive to attain effectiveness of their care provision and not merely targeting the attractive option of efficient operations. Based on these premises, the paper reviews the traditional Functional Leadership Model and the three elements that define the type of leadership an organization has namely, the tasks, the individuals, and the team. The article argues that concentrating on any one of these elements is not ideal and proposes adding a new element to the model to construct a novel Functional Result-Oriented healthcare leadership model. The recommended Functional-Results Oriented leadership model embosses the results element on top of the other three elements so that every effort on healthcare leadership is directed towards attaining excellent patient outcomes.
Introduction
This article seeks to propose a Functional Results-Oriented Leadership Model, which is a modification of the traditional functional leadership model. First, the article will provide a brief overview of the traditional functional leadership model. This model is based on the Three Circles leadership model postulated in the late 1950’s by John Adair.1 The model conceives the role of leadership as a desirable set of behaviors which help a particular group within a singular setting perform their tasks and reach their group goals.2 Leadership is not conceived as person-specific, but as traits attributable to an organization or team and which help them to effectively achieve their organization/team goals effectively.1 The model postulates that a leadership function must necessarily meet the needs of three areas namely; the predefined task, the team and the individuals forming the team.1
The Traditional leadership Model
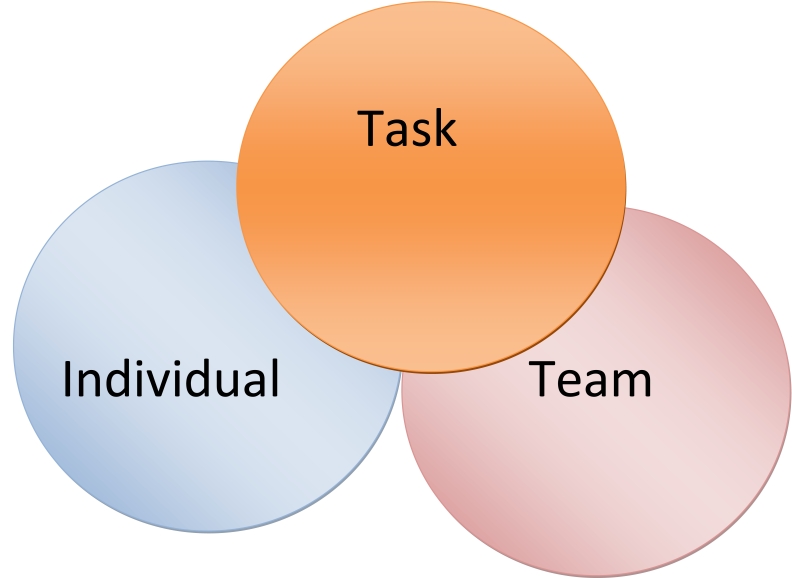
This model is based on three areas, which are seen as core areas in leadership. These three areas include the tasks performed by the organization, the relationship of the people working in an organization and the input of each individual working in the organization.3 The relationship between these three areas is in a union as indicated by the following Venn diagram.
This model has been used with great success in the British and Canadian military. However, it has come under great criticism by theorists who later claimed that it is an over simplification of the very complex role of leadership.4 According to the theory; leadership behaviors should be divided into three distinct types based on which of the above three areas they prioritize.5 The first type of behavior is substantive, which refers to behaviors that are only directly relevant to getting the organization’s tasks done.4 It prioritizes the task more than either the team or the individual.6 Leaders who prioritize substantive behaviors are always proposing workable solutions or providing crucial information to solve the challenges that lie between the staff and high performance.4 The following Venn diagram (diagram 1) can represent this scenario or type of leadership.
Diagram 1.
Venn diagram
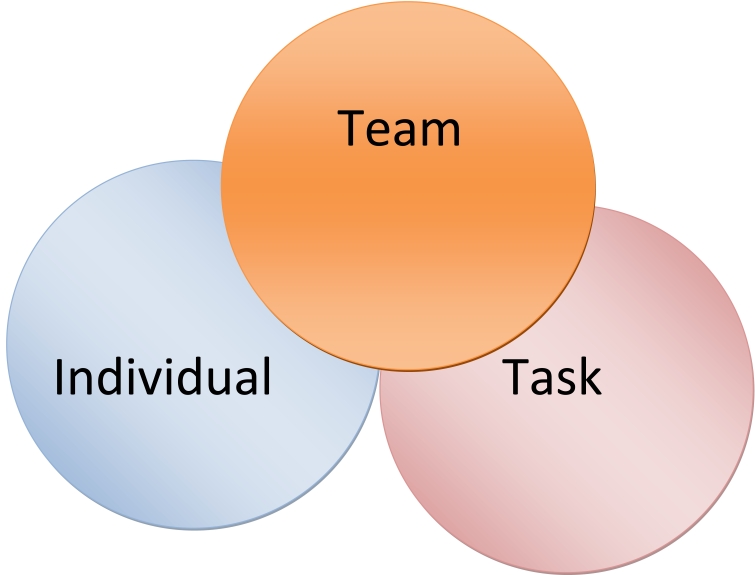
The second type of leadership behavior focuses more on the group/ team, rather than either the task or the individuals.4 The healthcare industry relies on teamwork to accomplish goals and thus, this aspect of leadership is quite important.7 This type of leadership is called procedural leadership, since its typical behaviors are those that seek to establish beneficial team playing, team exchange and team participation. It regards every decision from a group perspective, by developing particular group procedures that help the team members to work together.4,8 The test of good leadership here becomes the level of agreement and relationship among the organization/team members.7 The following Venn diagram (diagram 2) illustrates this type of behavior.
Diagram 2.
Venn diagram
The third type of leadership, according to the functional leadership model, is maintenance leadership whose typical behaviors tend to prioritize the individual employee or staff member over both the team in which he or she works or the tasks he or she is assigned.4 This type of behavior always strives to improve the individual participation, satisfaction and achievement.9 In a group setting for instance, a maintenance leader will always encourage the silent and shy members to join a discussion. Such leaders tend to satisfy employees first as a way of boosting their performance by developing their skills, giving satisfactory compensation, offering good benefits and counseling.10 The following Venn diagram (diagram 3) illustrates this type of behavior.
Diagram 3.
Venn diagram
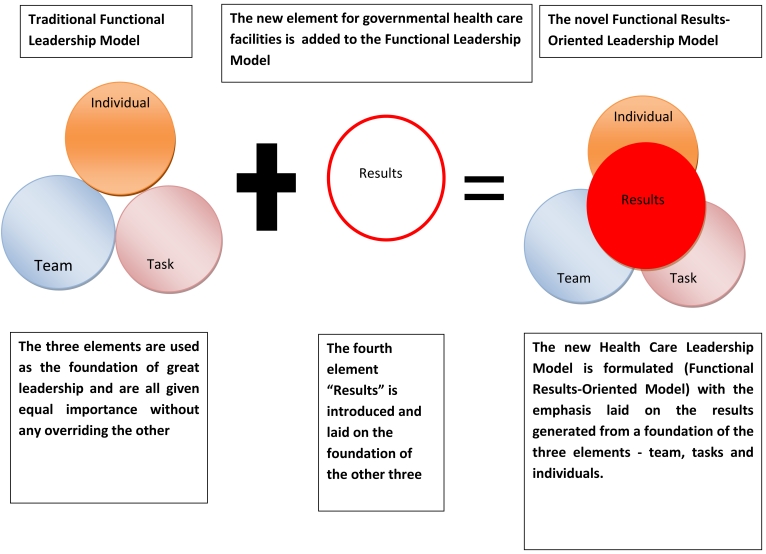
The Functional Results-Oriented leadership model proposed in this article introduces a fourth element that is very crucial in healthcare provision.11 In this model, results become the center circle embossed on the three other circles of tasks, individuals and teams.
Contemporary Issues in Health Care Leadership
One of the dominating issues in contemporary healthcare leadership practice is whether the leaders should prioritize the processes of delivering care. Other important issues include; the structural framework of healthcare institutions and the outcomes of the healthcare programs when striving for more efficient and effective care provision.12,13 Rubin, Pronovost and Diette (as cited by Shortell, 2006) stated that healthcare can be measured by studying the processes, structure and outcomes of healthcare programs, as well as the organizations.14 Arguably, the most important of the three (structure, process and outcomes) in healthcare quality management is and should be the outcome.15 A good structure that does not achieve the objectives of a healthcare institution or program is worthless and much more of a waste of public resources or private investment.16 Similarly, effective bureaucratic processes that still do not help patients in their needs, are worthless.16 When patients get quality outcomes from medical care, the objective of the healthcare institution or program is attained.17
As such, healthcare leaders have their primary mandate as serving the interests of the patients by providing excellent care outcomes.11 Their performance is only judged from the outcome of their administration since very few patients will want to know how things are run (processes) or who is senior or answerable to whom, in a hospital (structure).18 Ideally, both processes and structures are measures adopted to improve the outcomes.12 How good the processes are and how good the structures are can and should only be evaluated based on the outcomes. In healthcare leadership; the leaders must be adept at changing the structures and processes of healthcare provision until they are able to facilitate efficient and effective care, thus generating excellent care outcomes.13,18 The leadership model instituted in a healthcare facility, be it a not-for-profit, for-profit or governmental organization, must focus primarily on initiating, adjusting, improving and constantly reviewing the structures and processes of care provision as a means of amplifying the patient outcomes.11,16,19
Furthermore, contemporary leadership practices in healthcare provision tend to emphasize on effective care more than the efficiency with which such care is provided.13 For instance, a not-for-profit hospital with limited number of staff and operating alone in a poor community may believe in giving quality care to its patients. Yet, while they may provide effective care to a few patients, they will be unable to cater for the high demand for medical care services in the area. In this regard, they will be offering efficient care ineffectively. The fact that healthcare is evaluated based on what it achieves and not on how it achieves it makes efficiency by itself unsatisfactory.12,18
On the other hand, it is impossible to provide effective care inefficiently.16 Effective leadership is associated with improved performance in health institution.20 If the systems and the practitioners are inefficient, the healthcare provided will not be effective.16 Patient records will be lost, departments in their respective fields will not collaborate to help patients, there will be no sense of responsibility or accountability, and duplicate and inconsistent efforts would indicate that much efforts were exerted to produce little results.21 All these are symptoms of inefficiency, which mean that patients are not given efficient care.16,22
The analysis provided above depicts two important points relevant to any consideration of an ideal leadership model for a healthcare institution. First, it is important that the ideal healthcare leadership emphasize the outcomes of the patient care more than the processes and structures used to deliver such care, and secondly, that the leadership must strive to attain effectiveness of their care provision and not merely targeting the attractive option of efficient operations.13
Constructs of the Functional Results-Oriented Health Care Leadership Model
The Functional Results-Oriented leadership model is perfectly fitting to a governmental healthcare organization, one tailor-made to meet the needs and challenges of effective and efficient healthcare provision. The reasoning is simple. If healthcare leaders concentrate on the individual staff, they will forget the patient who is primarily the single most important person to any healthcare program. Again, there is no guarantee that individual healthcare providers will provide effective and efficient care when they are tended to excellently. Nonetheless, while not being the priority, individual attention is necessary since without motivation, every other strategy in health care provision will fail.13,23
The task by itself cannot be the focus of healthcare leadership. To begin with, when a doctor sees a patient and recommends treatment, his or her task remains unfinished. The task gets done when such a patient recovers from the illnesses, succeeds in preventing a disease or is helped to manage the medical condition diagnosed.24,25 This brings in many people starting with administrative staff, support staff, nurses, clinicians, laboratory technicians, etc.13 That means that a single patient is a task for too many people, each of whom contributes to the patient outcomes.13
Finally, healthcare leadership cannot solely concentrate on the team since good and efficient teamwork as discussed in the introductory sections of the article is not an adequate indicator of excellent healthcare provision.22 A team can work very well and still be ineffective. Effectiveness in healthcare, as already discussed, must always be prioritized over efficient teamwork and care processes.11 The quality of the team must, therefore, be assured to ensure that the goals are achieved.26
This model introduces a fourth element that was not conceived by the earlier functional leadership model, one that is of utmost importance in healthcare. The fourth element is results (patient outcomes). The introductory argument helped illustrate how the patient outcomes are the only indicator of good healthcare leadership, since they constitute the primary mandate of every healthcare establishment.13,27 No matter how perfect the healthcare team is; no matter how motivated the care staff are; no matter how well the care procedures are articulated and practiced, the yardstick of good healthcare leadership is patient outcomes, the results of care.22,28 The following diagram (diagram 4) illustrates how the Functional Results-Oriented leadership model can work.
Diagram 4.
Functional Results-Oriented leadership model
Relevance of the Functional Results-Oriented Health Care Leadership Model
This model of leadership was proposed in this article because it fits perfectly to the healthcare organization setting, be it for-profit, not-for-profit or governmental. For instance; any medical staff, irrespective of their discipline or specialization, (of which there are hundreds in any one hospital) can qualify for a leadership position without necessarily imposing other requirements.11 There are very good leaders who are nurses, others are surgeons, laboratory technicians, obstetricians and others are still general practitioners.24 Healthcare leaders must be handpicked based on their abilities, their personal traits, their credibility, or their potential; and not based on which area of healthcare provision they are qualified to work in.24
The Functional Results-Oriented leadership model emphasizes on the process that an organization uses in its leadership rather than the individual entrusted to lead. It is not about the person assigned the leadership role but the particular role they are assigned and their ability to deliver results in that role. Instead of spending time, effort and many resources looking for an ideal leader (individual), this model primarily requires that the healthcare establishment spend the effort and resources in developing the leadership role that will allow for effective and efficient carte provision before identifying the person who can adequately fit that role.13
The conglomeration of the three types of leadership behaviors as posted by the functional leadership model into a singular behavior that uses the team, tasks and individuals to work towards desired results; thus enabling any healthcare professional member to perform effectively in leadership.11 Again, as posted in the foregoing section analysis, healthcare provision must be geared towards getting desired patient outcomes and not the processes of care of the organization structures of a healthcare facility.24,29 This model emphasizes on results, where teams are assigned tasks and individuals are held accountable for their contribution or lack of, to the team’s attainment. Results take center stage in this model.
This model is applicable in any size and type of healthcare organization, but particularly for large governmental healthcare organizations. As Shortell (2006) notes, healthcare facilities from governmental, for-profit or not-for-profit, require a similar management structure but for their operating principles.13 Although the aspirations and targets may differ, the mandate remains centered on patient care. The greatest advantage of this healthcare leadership model is that it uses the staff talents (individual), their teamwork potential (team) and the mission or mandate of the institutions such as delivering effective and efficient healthcare (tasks) in a balanced way and all targeted at achieving excellent patient outcomes (Results). As such, the leaders consider individual motivation factors (individuals) with the primary goals of ensuring good results, they deliberate on ideal teamwork procedures and communication channels (team), again with the primary goals of ensuring good results; and finally, they assign protocols on care provision in terms of correct procedures and processes (tasks) the primary goals of ensuring good results. Everything is easily configured towards one ultimate objective, that of achieving excellent patient outcomes.
The Functional Results-Oriented model is supremely applicable in healthcare organizations, more so in governmental establishments. Its greatest advantage is that, it uses the staff talents (individual), their teamwork potential (team) and the mission or mandate of the institutions such as delivering effective and efficient healthcare (tasks) in a balanced way and all targeted at achieving excellent patient outcomes (Results). As such, tasks, individuals and teams become the foundation on which results are generated. Further research should be aimed at the usefulness of this model in private health establishments to examine its effectiveness.
References
- 1.Gardner G. Functional Leadership and Popularity in Small Groups. Hum Relat 1956;9:491-509 . 10.1177/001872675600900407 [DOI] [Google Scholar]
- 2.Kermally S. Gurus on People Management. London: Thorogood, 2005. [Google Scholar]
- 3.Hanson W, Randal F. Complexity and leader competencies in healthcare. British Journal of Healthcare Management 2011;17:284-290 [Google Scholar]
- 4.Northouse P. (ED). Leadership: Theory and Practice. 4th Edition. New York: Sage Publications, Inc. 2006 [Google Scholar]
- 5.Adair J. Develop Your Leadership Skills: Develop Yourself as a Leader; Lead at a Strategic Level; Grow Leaders in Your Organisation. London: Kogan Page Publishers, 2010. [Google Scholar]
- 6.Eng RC. Mountaneering: Freedom of the Hills. Washington: The Mountaineers Books, 2010. [Google Scholar]
- 7.Heinemann, GD and A MZ. Team performance in health care: assessment and development. New York: Springer, 2002. [Google Scholar]
- 8.Hannah ST, Fred OW, Louis WF. Leadership in Action Teams: Team Leader and Members' Authenticity, Authenticity Strength, and Team Outcomes. Person Psychol 2011;64:771-802 [Google Scholar]
- 9.Clark, Jand Lynn C. Management for nurses and health care professionals. Edinburgh: Elsevier Health Sciences, 1997.
- 10.Williams C, Terry C, Ike H. MGMT. Mason, OH: Cengage Learning, 2011 [Google Scholar]
- 11.Pelote V, Pelote V, Route L. Masterpieces in health care leadership: cases and analysis for best practice. London: Jones and Bartlett Publishers Inc, 2007 [Google Scholar]
- 12.Jasper M, Jumaa M. Effective healthcare leadership. Oxford: Blackwell Publishing. 2005 [Google Scholar]
- 13.Shortell S. Health Care Management. Albany: Delmar Thompson Learning, 2006. [Google Scholar]
- 14.Rubin H, Pronovost P, Diette G. The advantages and disadvantages of process- based measures of health care quality. International Journal for Quality in Health 2001;13:4669-474 [DOI] [PubMed] [Google Scholar]
- 15.Butler JR. The ethics of health care rationing. London: Cassell, 1999. [Google Scholar]
- 16.Gilmer T. The Costs of Non-beneficial Treatment in the Intensive Care Setting. Health Aff 2005;24:961-971 . 10.1377/hlthaff.24.4.961 [DOI] [PubMed] [Google Scholar]
- 17.American Hospital Association. "Fast Facts on U.S. Hospitals from AHA Hospital Statistics". Hospital Connect. 2010 Retrieved 16 July 2010, from http://www.hospitalconnect.com/aha/resource_center/fastfacts/fast_facts_US_hospitals.html
- 18.Galbraith J. Designing Organizations: An Executive Guide to Strategy, Structure, and Process. San Francisco: Jossey-Bass Publishing, 2001 [Google Scholar]
- 19.Jones R. Oxford textbook of primary medical care. Oxford: Oxford University Press, 2004. [Google Scholar]
- 20.Burns, LR, Elizabeth HB and Bryan JW. Shortell and Kaluzny's Healthcare Management: Organization Design and Behavior. Boston: Cengage Learning, 2011. [Google Scholar]
- 21.Manley K, Valerie W. International practice development in nursing and healthcare. Hoboken, NJ: John Wiley & Sons, 2008. [Google Scholar]
- 22.Jaffe S. Health Policy Brief: Key Issues in Health Reform. Health Affairs. 2009 Retrieved 20 July 2010, From http://www.rwjf.org/files/research/82409healthaffairs7.pdf
- 23.Buchbinder and Nancy HS. Introduction to Health Care Management. Burlington, MA: Jones & Bartlett Publishers, 2011. [Google Scholar]
- 24.Almgren G. Health care politics, policy, and services: a social justice analysis. New York: Springer Publishing Company, 2007 [Google Scholar]
- 25.Draper E. The company doctor: risk, responsibility, and corporate professionalism. New York: Russell Sage Foundation, 2003. [Google Scholar]
- 26.Price A, Andrew S. Essential Skills for Managing in Healthcare. Oxon, OX: Radcliffe Publishing, 2010 [Google Scholar]
- 27.Marshall E, Joseph FC. Transformational Leadership in Nursing: From Expert Clinician to Influential Leader. New York: Springer Publishing Company, 2010. [Google Scholar]
- 28.Sines D, Mary S, Janice F. Community Health Care Nursing. Hoboken, NJ: John Wiley and Sons, 2009. [Google Scholar]
- 29.Hertz HS. Health Care Criteria for Performance Excellence. Washington: DIANE Publishing, 2000. [Google Scholar]