Abstract
Obesity increases the risk of adverse outcomes during acute critical illnesses such as burns, severe trauma, and acute pancreatitis. Although individuals with more body fat and higher serum cytokines and lipase are more likely to experience problems, the roles that these characteristics play are not clear. We used severe acute pancreatitis as a representative disease to investigate the effects of obesity on local organ function and systemic processes. In obese humans, we found that an increase in the volume of intrapancreatic adipocytes was associated with more extensive pancreatic necrosis during acute pancreatitis and that acute pancreatitis was associated with multisystem organ failure in obese individuals. In vitro studies of pancreatic acinar cells showed that unsaturated fatty acids were proinflammatory, releasing intracellular calcium, inhibiting mitochondrial complexes I and V, and causing necrosis. Saturated fatty acids had no such effects. Inhibition of lipolysis in obese (ob/ob) mice with induced pancreatitis prevented a rise in serum unsaturated fatty acids and prevented renal injury, lung injury, systemic inflammation, hypocalcemia, reduced pancreatic necrosis, and mortality. Thus, therapeutic approaches that target unsaturated fatty acid–mediated lipotoxicity may reduce adverse outcomes in obese patients with critical illnesses such as severe acute pancreatitis.
INTRODUCTION
Obese individuals have an increased risk of developing multisystem organ failure in acute inflammatory conditions such as severe burns (1, 2), severe trauma (3), critical illness (4), and acute pancreatitis (AP) (5, 6). Pancreatitis is associated with the release of destructive digestive enzymes from pancreatic acinar cells into the pancreas itself. When AP is initiated by diverse stimuli, including alcohol consumption and gallstones (7–9), obese patients are more prone to severe AP (SAP). This is a concern because SAP results in 40 to 50% mortality when complicated by acute renal failure, respiratory failure, hypocalcemia, and other manifestations of multisystem organ failure or by large areas of pancreatic necrosis (10, 11). Patients with SAP have increased visceral fat (12), higher serum cytokines [for example, interleukin-6 (IL-6) and monocyte chemotactic protein 1 (MCP-1)], and adipokines (for example, resistin and visfatin) (5, 13), but it is unclear whether these are markers or mediators of injury. With no effective therapies, the current management standard is supportive care and managing complications when they occur (14).
SAP is therefore a relevant disease in which to study both the local effects of a visceral fat depot [that is, intrapancreatic adipocytes (15); hereafter referred to as intrapancreatic fat (IPF) (16)] and the multi-system organ failure related to obesity. To explore the mechanisms that cause worse outcomes in obese patients with SAP, we examined the relationship of disease severity to patient BMI, to the amount of IPF and pancreatic necrosis at the time of autopsy, and to the characteristics of samples removed during surgical debridement from patients with SAP. We also studied the interplay between adipocytes and pancreatic parenchyma on the cellular level in a coculture system, which simulated the unpolarized basolateral release of acinar enzymes noted in human disease (17). This helped to determine the role of lipolysis-mediated formation of nonesterified fatty acid (NEFA) and adipokine changes in AP. We then characterized the role of different classes of NEFA [saturated fatty acids (SFAs) and unsaturated fatty acids (UFAs)] in deleterious outcomes and the cause-effect relationship between SFAs, UFAs, and cytokines in vitro. We finally verified findings from these experiments in an obese animal pancreatitis model [using IL-12 and IL-18 (18)], chosen because of its clinical relevance (19–22) in that pancreatitis causes reproducible lethality in obese mice but not in lean mice (23).
RESULTS
IPF worsens pancreatic necrosis in obesity
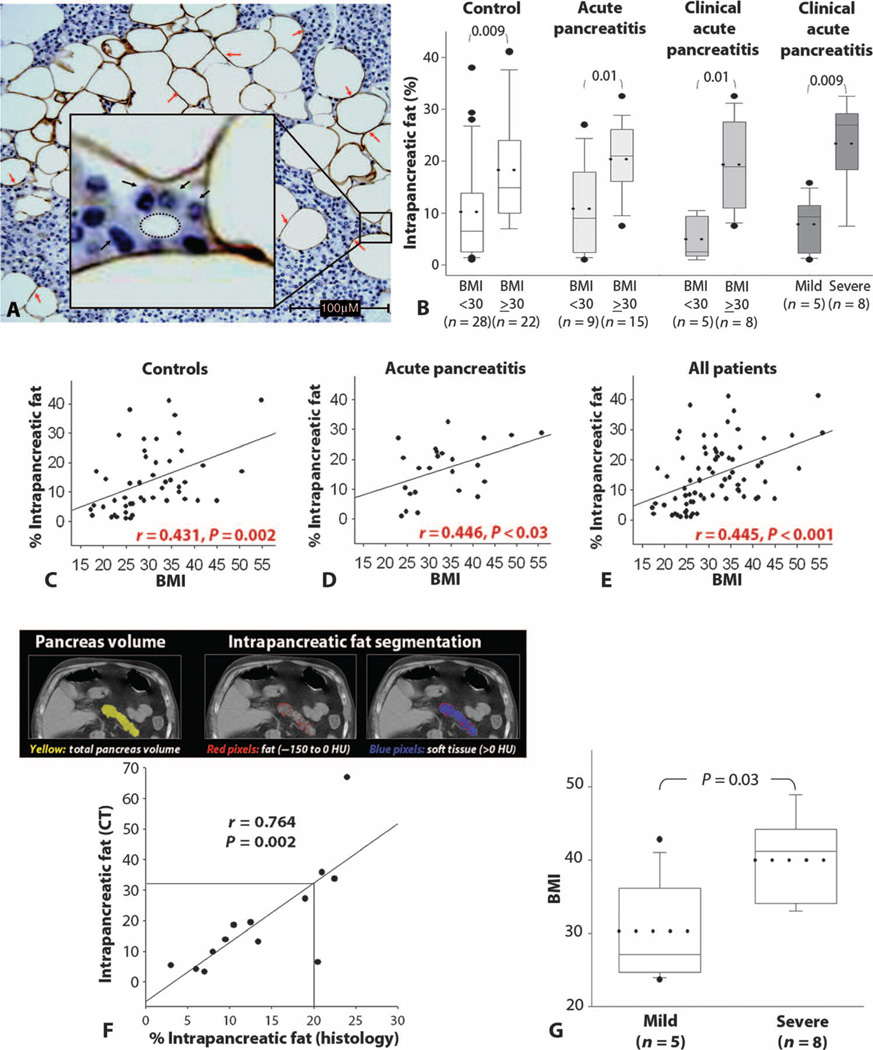
Pancreatic tissues sections, harvested at the time of autopsy from control patients (50 individuals) and 24 patients with an autopsy diagnosis of AP (of which 13 fulfilled clinical criteria for AP), were studied histologically (Table 1). Immunostaining revealed that cells morphologically resembling adipocytes were positive for the adipocyte marker perilipin (Fig. 1A). We referred to these regions as IPF. IPF area was measured as a percentage of total histological area, as described in Materials and Methods. IPF area as measured by histology was increased in patients with a body mass index (BMI) of ≥30 irrespective of disease state (Fig. 1, B to E). This was verified for 13 patients who had abdominal computed tomography (CT) scans before a diagnosis of pancreatitis or who were controls (Fig. 1F and fig. S1). Patients with SAP had higher BMIs (Fig. 1G) and more IPF than those with mild AP (Fig. 1B).
Table 1.
Autopsy cases (50 controls and 24 AP cases). Values shown are means ± SD. There was no significant difference between the two groups.
| Controls (n = 50) | AP (n = 24) | P | |
|---|---|---|---|
| Age (years) | 64 ± 16 | 59 ± 15 | 0.221 |
| Sex (female:male) | 23:27 | 6:18 | 0.126 |
| BMI | 30.2 ± 8.1 | 33.3 ± 8.5 | 0.130 |
Fig. 1.
Relationship between IPF and BMI. (A) Immunohistochemistry of human pancreatic section showing the staining of the adipocyte marker perilipin (stained brown, red arrows) in IPF. (Inset) Adipocytes normally abut the parenchymal basal surface (black arrows) and not the lumen (dashed oval), which carries exocrine pancreatic secretions. Scale bar, 100 µm. (B) IPF as a percentage of total area in controls (white), AP patients on autopsy (light gray), clinical AP patients with BMI of <30 or ≥30 (dark gray), and clinically mild AP and SAP patients. The dots within the bars indicate the mean, and the horizontal line within the bars indicates the median. P values are indicated for each pair. (C to E) Correlation between BMI and percentage IPF in controls (C), AP patients (D), and all patients (E). Each dot represents the value for an individual patient. (F) Correlation between IPF measured by noncontrast CT (thresholding method) and histology at autopsy [Hounsfield units (HU)]. (G) BMI of patients with mild and severe pancreatitis. The dots within the bars indicate the mean, and the horizontal line within the bars indicates the median.
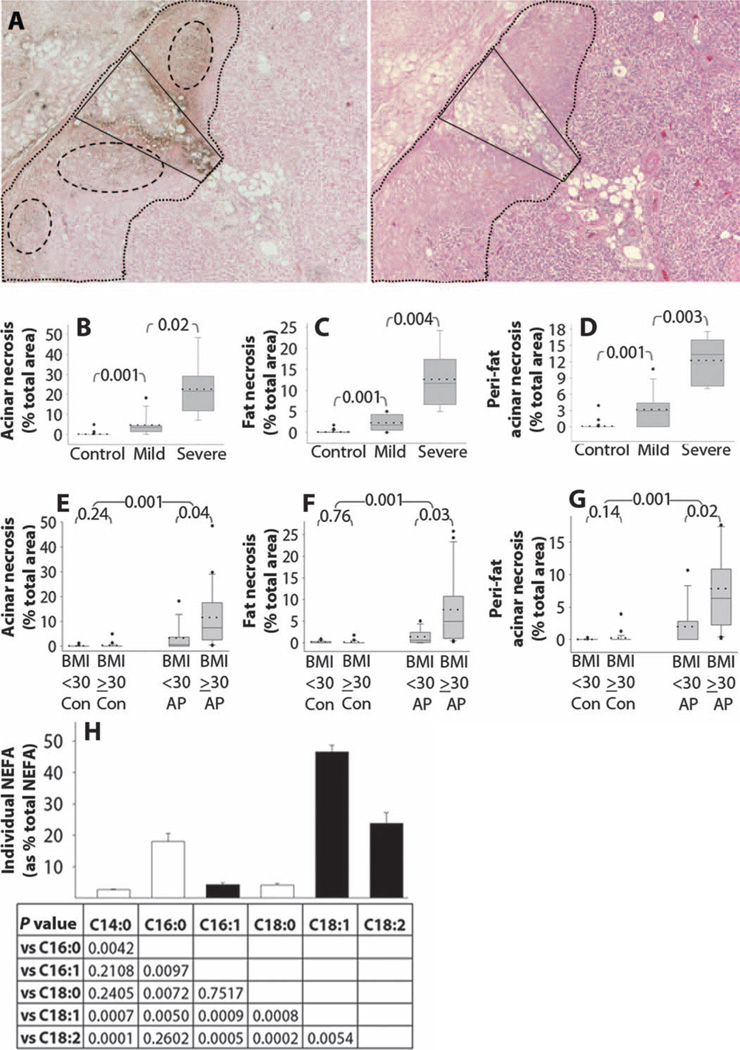
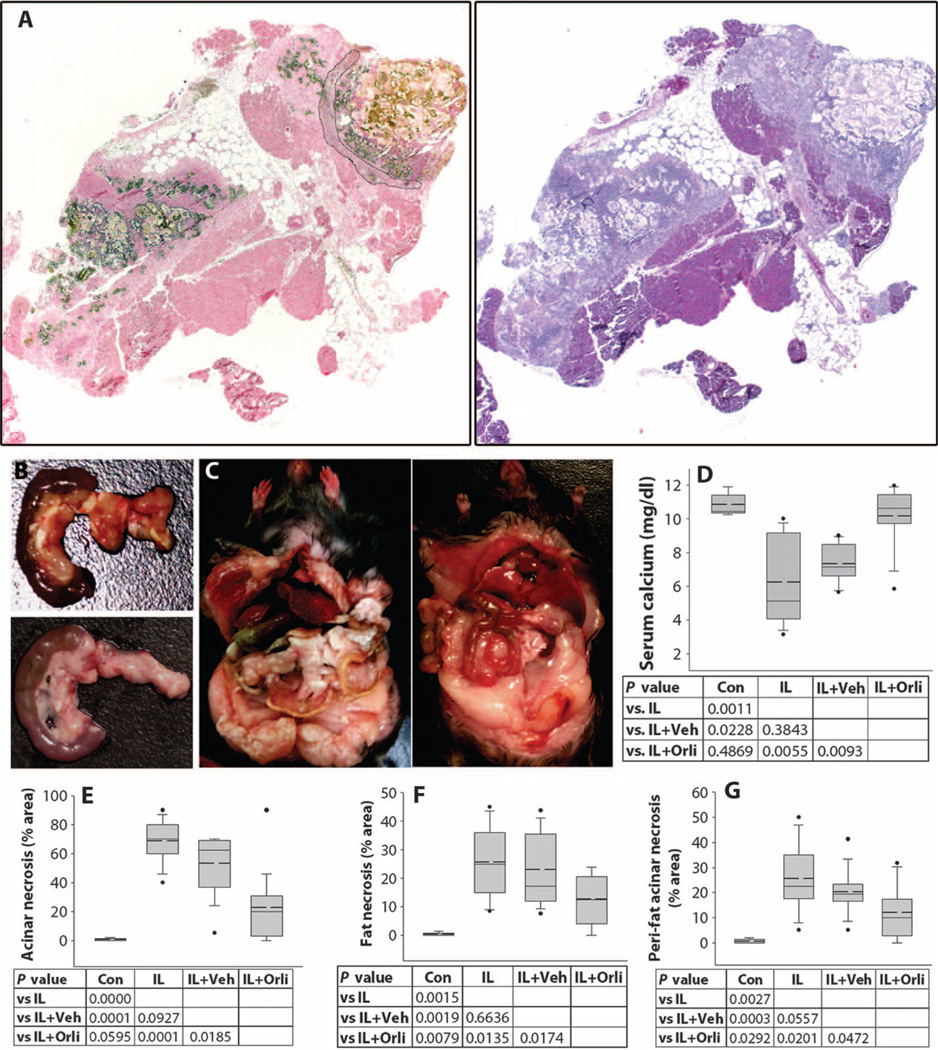
Pancreatic sections obtained during autopsies of patients with AP revealed that pancreatic necrosis occurred predominantly around areas with necrosis of IPF (Fig. 2, A to D). SAP and obese patients had more fat necrosis and higher acinar necrosis surrounding areas of fat necrosis (peri-fat acinar necrosis) (Fig. 2, B to G) than did patients with mild AP or nonobese patients, respectively. These changes were unlikely to be a postmortem artifact because autopsy specimens from control patients had insignificant amounts of fat necrosis and acinar necrosis (Fig. 2, B to G). Further evidence for these changes having taken place before death was provided by the infiltration of CD68-positive macrophages around fat necrosis but not normal fat (fig. S2).
Fig. 2.
Relationship between acinar necrosis, fat necrosis, and NEFAs. (A) Human pancreatitis serial sections stained for calcium with von Kossa (left) and hematoxylin and eosin (H&E) (right), showing fat necrosis (adipocytes in quadrangle staining dark brown on von Kossa and cheesy blue gray on H&E) and parenchymal injury (dotted lines) around calcium staining (dashed ovals). (B to D) Acinar necrosis (B), fat necrosis (C), and peri-fat acinar necrosis (D) box plots in controls (50 patients), clinically mild AP (8 patients), and SAP groups (5 patients). (E to G) Acinar necrosis (E), fat necrosis (F), and peri-fat acinar necrosis (G) in nonobese controls (BMI < 30 Con; n = 30), AP patients (BMI < 30 AP; n = 8), obese controls (BMI ≥ 30 Con; n = 20), and AP patients (BMI ≥ 30 AP; n = 16). The dots within the bars in (B) to (G) indicate the mean, and the horizontal line within the bars indicates the median. (H) NEFA composition in human pancreatic necrosis debridement fluid with individual NEFAs expressed as a percentage of total NEFA content. Each bar depicts the NEFA mentioned below the corresponding bar in the top row of the table. White bars, SFAs; black bars, UFAs. Numbers in the table below show P values between individual NEFAs mentioned in the rows and columns.
Von Kossa staining, in which silver cations replace calcium to yield a brown color (24), revealed that areas of fat necrosis and surrounding peri-fat acinar necrosis were rich in calcium (dashed ovals, Fig. 2A), suggesting that NEFAs released into the parenchyma had undergone saponification. Measurement of NEFA in pancreatic necrosis debridement fluid from six obese SAP patients (mean BMI, 36.7 ± 4.7) showed a mean concentration of 7.8 ± 2.9 mM, of which 75.3% was UFAs (Fig. 2H), with NEFA concentrations as high as 65 mM in supernatant fluid from debridement tissue homogenates. These findings suggest that NEFAs generated from increased IPF in obese individuals may exacerbate local pancreatic injury during AP.
Lipolysis regulates necrosis and resistin levels
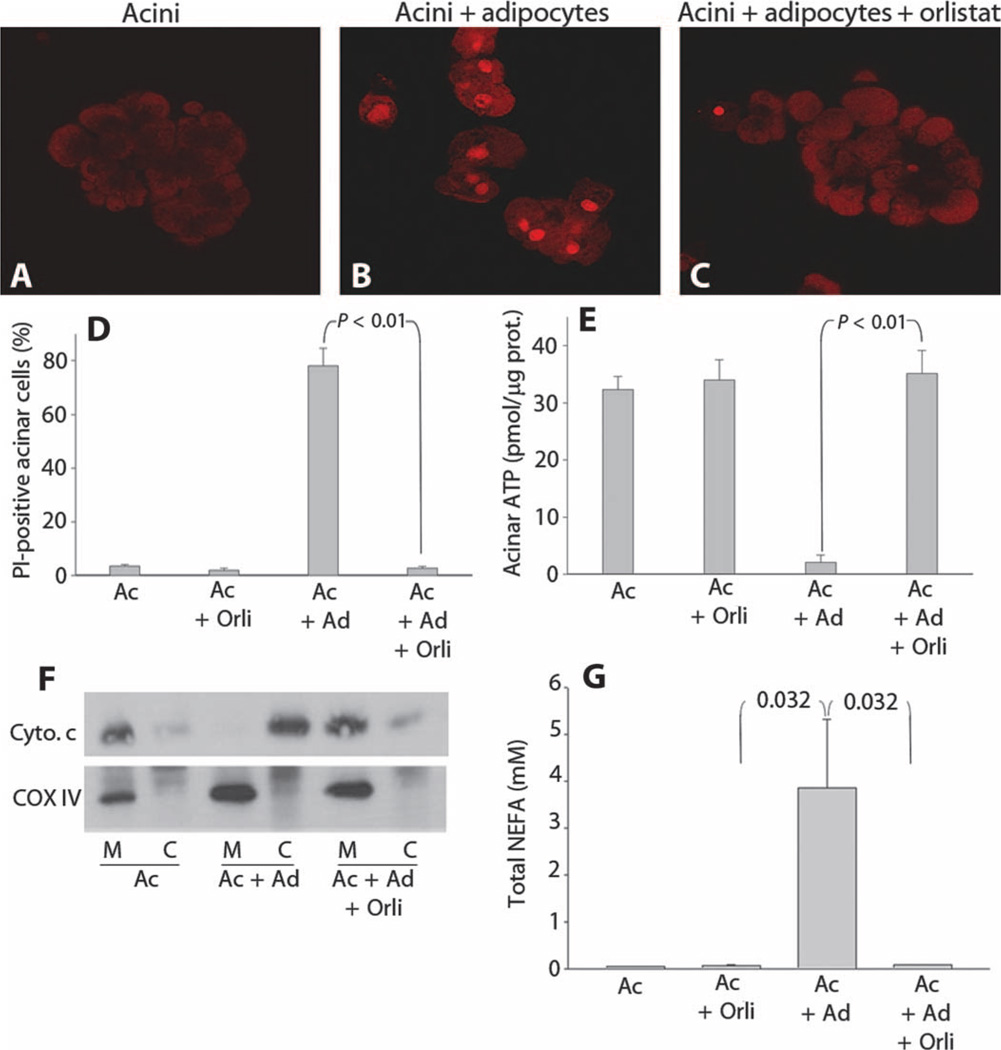
Pancreatic acinar cells, which are polarized, normally release their digestive enzymes from the apical pole (25) into the ductal lumen (Fig. 1A, inset). These enzymes normally do not contact the basal surface where adipocytes are located. Disruption of apically directed, polarized trafficking, such as from an insult that causes pancreatitis (25–27), results in interstitial leakage of enzymes and other macromolecules during pancreatitis (17). To explore whether this macromolecular diffusion contributes to fat-induced acinar necrosis, we simulated pathological interstitial leakage by coculturing adipocytes and pancreatic acini using a Transwell system in which the 3-µm pores allowed macromolecular diffusion (fig. S3) while avoiding contamination of one cell type by the other (fig. S4A). When individually cultured, each cell type appeared morphologically and physiologically normal (figs. S5 and S6). However, coculture resulted in acinar cell necrosis, as evidenced by propidium iodide (PI) staining, a drop in adenosine 5′-triphosphate (ATP) levels, and cytochrome c leakage (Fig. 3, A to F) in the absence of increased active caspase-3 or an increase in the lipidated amounts of the autophagic marker LC3-II (fig. S4). These changes in acinar cells were accompanied by a large increase in NEFA (Fig. 3G) and resistin concentrations in the medium (fig. S7), which were similar to those observed in debridement fluid (Fig. 2H) and serum, respectively, of patients with SAP (13). These changes in acinar cells in vitro were completely prevented by the pancreatic lipase inhibitor (28, 29) orlistat (50 µM), which preserved acinar cell viability and function at control levels (Fig. 3, C to G, and figs. S6 and S7). Therefore, we conclude that lipolysis regulates NEFA formation, acinar necrosis, and resistin levels in the coculture system.
Fig. 3.
Lipolysis of adipocyte triglycerides causes acinar cell necrosis. (A to C) PI uptake in (A) control acini, cocultured with adipocytes (B) and adipocytes and 50 µM orlistat (C). (D) Percentage of acinar cells positive for PI uptake after culture alone (Ac), with 50 µM orlistat (Ac + Orli), adipocytes (Ac + Ad), or 50 µM orlistat (Ac + Ad + Orli). (E) ATP levels in acinar cells treated as in (D). (F) Cytochrome c (upper panel) in mitochondrial (M) and cytoplasmic (C) fractions of Ac, Ac + Ad, and Ac + Ad + Orli. (Lower panel) Mitochondrial marker COX IV. (G) Total NEFA concentrations in the medium of acini cells treated as in (D).
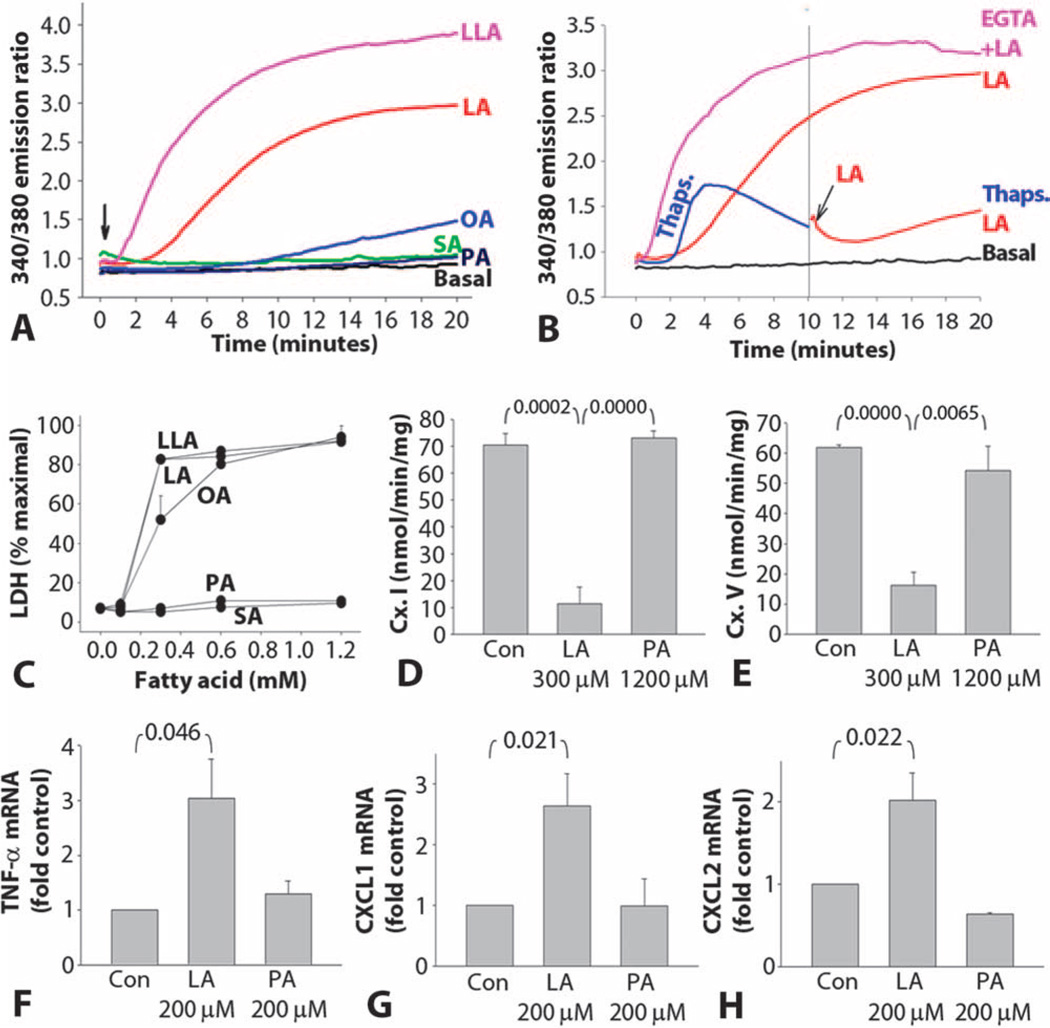
UFAs induce necrosis and are proinflammatory
To determine which fatty acids are responsible for acinar cell necrosis in coculture, we exposed acinar cells to individual fatty acids at concentrations less than or equal to those in coculture or debridement fluid. Intracellular calcium concentrations were increased when acinar cells were treated with UFAs (Fig. 4A). We concluded that these fatty acids came from an intracellular pool because the calcium increase was inhibited by the calcium adenosine triphosphatase (ATPase) inhibitor thapsigargin (30), but not by the extracellular calcium chelator EGTA (Fig. 4B). UFAs also caused lactate dehydrogenase (LDH) leakage into the medium (Fig. 4C and fig. S8A). Both the LDH leakage and the intracellular calcium increase were dose-dependent (Fig. 4C and fig. S8B). Chelation of the intracellular calcium pool with BAPTA [1,2-bis(2-aminophenoxy)ethane-N,N,N′,N′-tetraacetic acid] partially prevented LDH leakage and cytochrome c release, although this protection was not sustained beyond 3 hours (fig. S9). Linoleic acid (300 µM) but not palmitic acid (1200 µM) inhibited mitochondrial complexes I and V (Fig. 4, D and E, and fig. S10), causing a drop in ATP concentrations and necrotic cell death (fig. S11). Additionally, sublethal concentrations (200 µM) of linoleic acid [which increased cytosolic calcium (fig. S9B)] but not palmitic acid increased mRNA levels for tumor necrosis factor–α (TNF-α) and the neutrophil chemoattractants CXCL1 and CXCL2 (Fig. 4, F to H). These findings support the hypothesis that UFAs generated as a result of lipolysis induce acinar cell necrosis and are proinflammatory.
Fig. 4.
UFAs induce acinar necrosis and inflammatory mediator generation. (A) Intra-acinar calcium concentrations (expressed as 340/380 emission ratio) in response to addition (arrow) of 600 µM fatty acids (LLA, linolenic acid; LA, linoleic acid; OA, oleic acid; SA, stearic acid; PA, palmitic acid). (B) Effect of depletion of endoplasmic reticulum calcium with thapsigargin (1 µM) (blue line) and depletion of extracellular calcium by chelation with EGTA (1 mM added 10 min before adding linoleic acid, pink) on 600 µM linoleic acid–induced intracellular calcium increase. (C) Leakage of LDH from acinar cells 5 hours after treatment with fatty acids as in (A). (D and E) Effect of linoleic and palmitic acids on mitochondrial complex (Cx.) I and V activity in acini. (F) Effect of linoleic and palmitic acids on TNF-α RNA in acini. (G) Effect of linoleic and palmitic acids on CXCL1 mRNA in acini. (H) Effect of linoleic and palmitic acid CXCL2 mRNA. Data are expressed as means ± SEM.
Lipolysis contributes to pancreatic necrosis
In response to IL-12 and IL-18, ob/ob mice developed pancreatitis that was associated with an increase in serum amylase and lipase levels (fig. S13). Pancreata of ob/ob mice contained 26 ± 2.1% fat (Fig. 5A). Von Kossa staining revealed increased calcium staining in areas of fat necrosis (Fig. 5, A and F) and surrounding peri-fat acinar necrosis (Fig. 5, A and G). The peri-fat acinar necrosis contributed significantly to total acinar necrosis (Fig. 5, A, E, and G). Grossly, pancreata of mice with pancreatitis had saponification, seen as chalky deposits (Fig. 5B, upper image), which also were seen throughout the fat in the peritoneal cavity (Fig. 5C, left image) and were accompanied by hypocalcemia (Fig. 5D). Orlistat treatment significantly inhibited all these changes in ob/ob mice with pancreatitis on gross (Fig. 5, B, lower image, and C, right image), histologic (Fig. 5, E to G), and biochemical (Fig. 5D and fig. S12) evaluation, supporting the hypothesis that local release of lipolysis products worsens acinar injury during AP.
Fig. 5.
Lipolysis exacerbates pancreatic damage in obese mice. (A) Von Kossa–stained (left) and H&E-stained (right) serial sections showing pancreatic fat necrosis (black and brown at left, lighter blue at right), surrounding parenchymal injury (pink at left, blue areas with loss of cellular detail at right). Dotted area, saponified parenchymal fat. (B) Gross images of the pancreas from vehicle-treated (top) or orlistat-treated (lower) animals with pancreatitis. White, areas of saponification. (C) Gross images of the peritoneal cavity from vehicle-treated (left) or orlistat-treated (right) animals with pancreatitis. White, areas of saponification. Note that orlistat prevents saponification. (D to G) Serum calcium (D), pancreatic necrosis (E), fat necrosis (F), and peri-fat acinar necrosis (G) (expressed as % of total area) were measured in control (Con), pancreatitis (IL), pancreatitis and vehicle-treated (IL + Veh), or pancreatitis and orlistat-treated (IL + Orli) animals. Dashed lines depict means. P values are shown in the table below.
Lipotoxicity results in multisystem organ failure
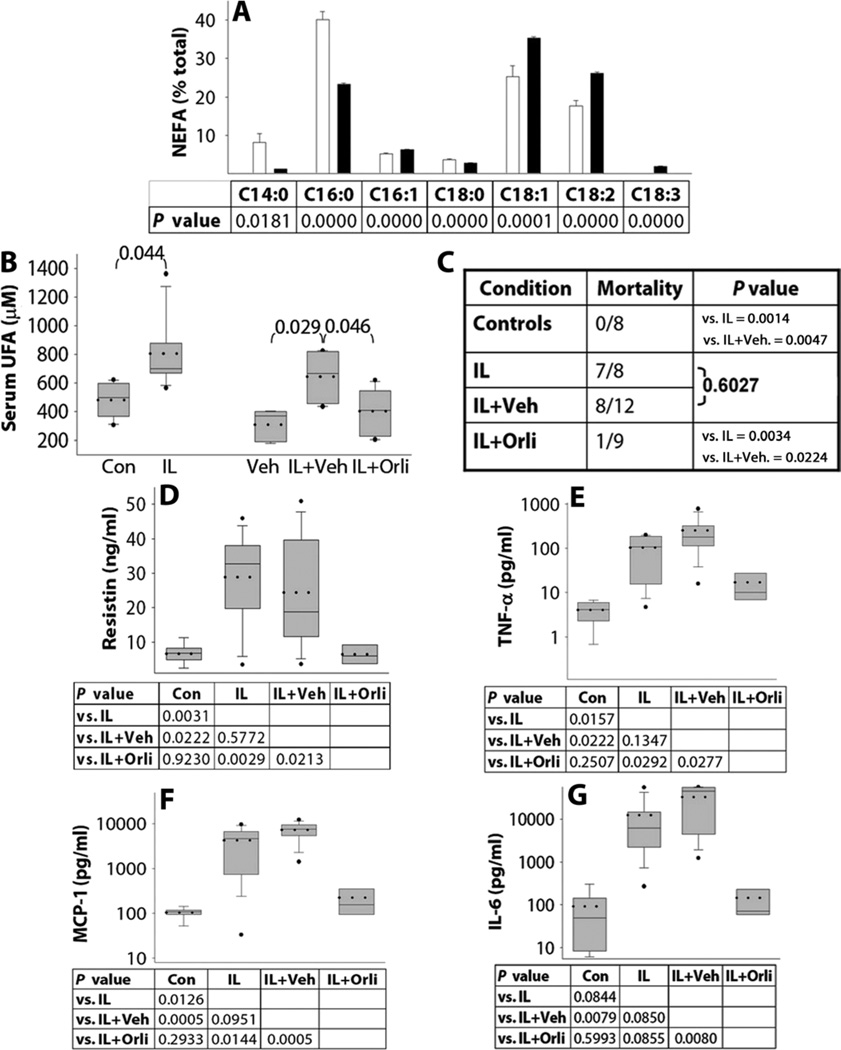
Evaluation of the triglyceride composition of visceral adipose tissue showed UFAs to be significantly increased in obese mice (73% versus 48%, P = 0.003) compared to lean mice (Fig. 6A), with a corresponding relative decrease in SFAs. Pancreatitis resulted in a significant increase in serum UFA concentrations and in mortality, both of which were significantly reduced in orlistat-treated animals (Fig. 6, B and C). SFA levels were not significantly reduced by orlistat (fig. S13). Orlistat also normalized serum resistin, TNF-α, MCP-1, and IL-6 (Fig. 6, D to G), suggesting that it reduced systemic inflammation.
Fig. 6.
Serum UFA, adipokines, cytokines, and mortality in obese mice are reduced by inhibiting lipolysis. (A) NEFAs in adipose tissue triglyceride of lean (white bars) and obese mice (black bars). P values between lean and obesemice are indicated beloweach NEFA. (B) SerumUFAs (µM) in controls animals (Con) and animals with pancreatitis (IL), vehicle (Veh), pancreatitis with vehicle (IL + Veh), and orlistat treatment (IL + Orli). (C) Seven-day mortality in ob/ob mice treated as in (B). (D to G) Serum adipokines and cytokines. Dotted lines depict means. P values are shown below.
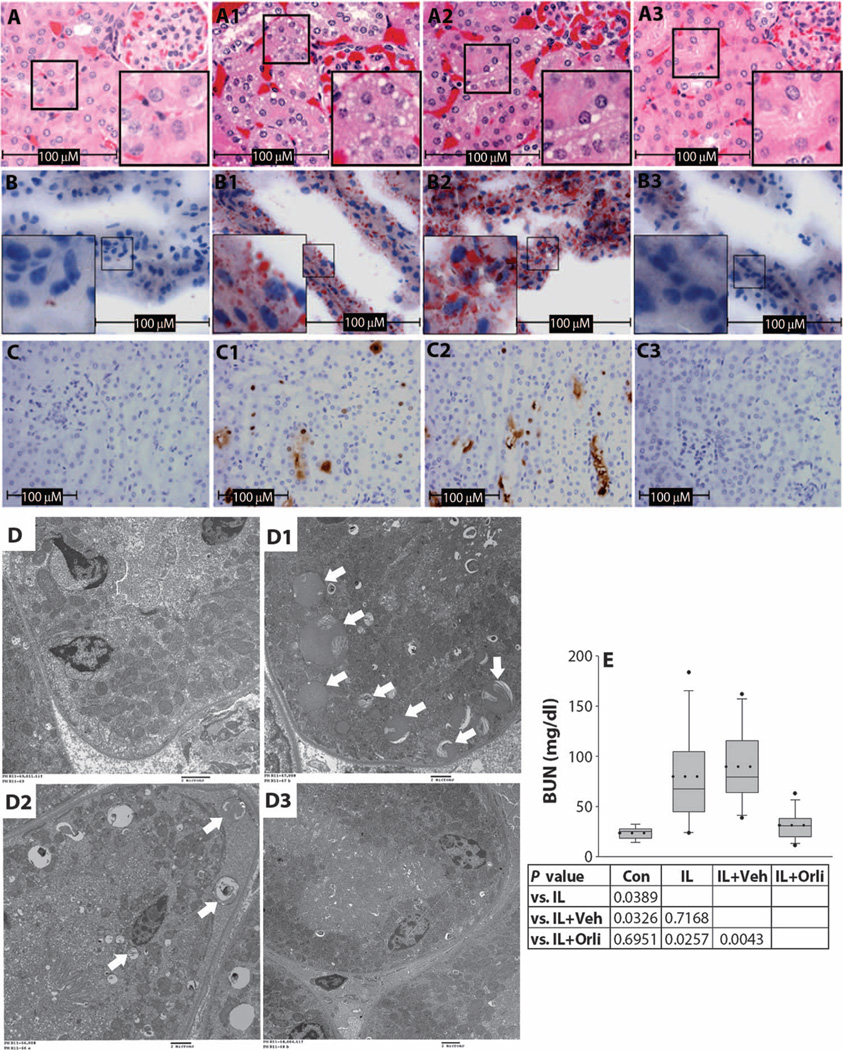
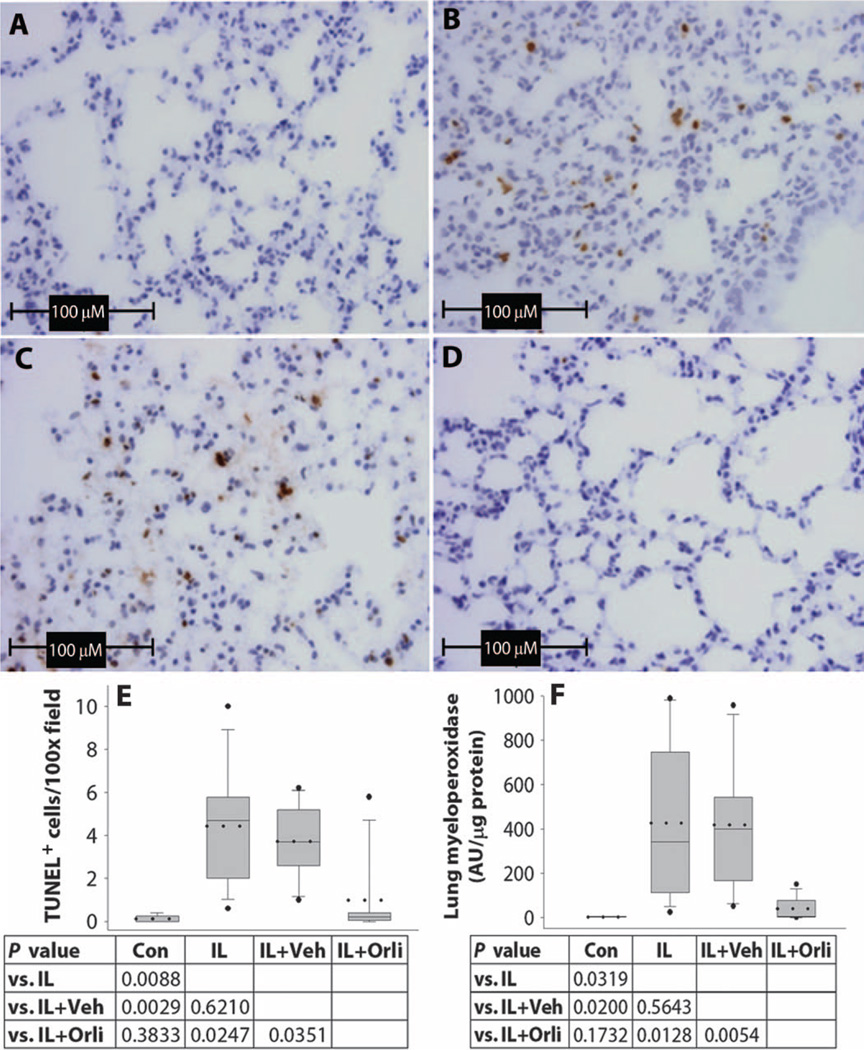
Damage in ob/ob mice included numerous renal abnormalities. These included tubular vacuoles (Fig. 7A, 1 and 2) that stained positive for fat with oil red O (Fig. 7B, 1 and 2), tubular apoptosis and injury (Fig. 7C, 1 and 2), mitochondrial swelling and saponification (Fig. 7D, 1 and 2), and associated renal failure with high blood urea nitrogen (BUN) levels (Fig. 7E). Renal tubular damage was also noted in autopsies of SAP patients with acute renal failure (fig. S14). All of these changes noted in mice with pancreatitis were normalized in the orlistat-treated animals (Fig. 7, A3, B3, C3, and D3) to values similar to those of controls (Fig. 7, A to D). Lung injury that was similar to the injury induced by oleic acid infusion (31, 32), and manifested as increased apoptotic cells (Fig. 8, B, C, and E) and lung myeloperoxidase levels (Fig. 8F), was also significantly reduced in the orlistat-treated group (Fig. 8, D to F). These data suggest that UFAs generated as a result of lipolysis may result in systemic inflammation and multisystem organ failure.
Fig. 7.
Renal tubular lipotoxicity and renal failure are reduced by inhibiting lipolysis. (A to C) Mouse kidney sections stained with (A) H&E, (B) oil red O, and (C) TUNEL (terminal deoxynucleotidyl transferase–mediated deoxyuridine triphosphate nick end labeling) stain in control (A to C), pancreatitis (A1, B1, and C1), pancreatitis with vehicle (A2, B2, and C2), and pancreatitis with orlistat treatment (A3, B3, and C3) groups. (D) Electron microscopy of renal tubules from control mice (D), mice with pancreatitis (D1), mice with pancreatitis + vehicle (D2), and mice with pancreatitis + orlistat (D3) showing lipid vacuoles, some of which have dense deposits of calcification (arrows) and mitochondrial swelling. Scale bar, 2 µm. (E) Serum BUN in controls animals (Con) and animals with pancreatitis (IL), pancreatitis with vehicle (IL + Veh), and orlistat treatment (IL + Orli). Dotted lines depict means, and the whiskers indicate the 5th and 95th percentile, with the dots above and below plots indicating values outside this range. P values are shown below.
Fig. 8.
Lung injury and inflammation are reduced by inhibiting lipolysis. (A to D) Lung sections with TUNEL staining in control (A), pancreatitis (B), pancreatitis with vehicle (C), and pancreatitis with orlistat treatment (D) groups showing apoptotic cells. (E) Number of apoptotic cells in lung sections. (F) Lung myeloperoxidase in control animals (Con) and animals with pancreatitis (IL), pancreatitis with vehicle (IL + Veh), and orlistat treatment (IL + Orli). Dotted lines depict means. The whiskers indicate the 5th and 95th percentile, with the dots above and below plots indicating values outside this range. P values are shown below.
DISCUSSION
We show here that local and systemic lipotoxicity contributes to multisystem organ failure and worse clinical outcomes in obese patients and in mice with pancreatitis. These effects are a result of UFAs, generated locally from IPF (see schematic diagram of fig. S15), that induce necrotic cell death through intracellular calcium release and inhibition of mitochondrial complexes I and V. The accumulation of oil red O–positive vacuoles in renal tubules along with mitochondrial swelling, tubular injury, and saponification in the kidneys of mice and patients dying of renal failure indicates the presence of systemic lipotoxicity. UFAs at sublethal concentrations also up-regulated inflammatory mediators. Inhibition of lipolysis in vitro and in vivo inhibited the generation of resistin [recently shown to be of adipocyte origin in humans (33)] and other inflammatory mediators such as TNF-α, MCP-1, and IL-6. Thus, lipids seem to exert toxic effects through both a direct cellular toxic action and an indirect effect mediated by up-regulation of inflammatory mediators such as TNF-α and IL-6, which may independently exacerbate local and systemic injury.
UFAs comprised 73 to 75% of the NEFAs in human pancreatitis debridement fluid and visceral adipose triglyceride content of obese mice but only 48% in lean mice. This larger proportion of UFAs, combined with the doubling of intrapancreatic adipocyte mass that occurred with obesity, could result in as much as a 300% increase in UFA concentrations locally and in the serum upon lipolysis, which is sufficient to cause local and systemic lipotoxicity. Similarly, secretion of lipolytic enzymes from acinar cells into a medium containing chylomicrons resulted in damage to the acinar cells, as indicated by LDH leakage (34). This effect was decreased in the presence of orlistat (35), supporting our hypothesis that unpolarized release of lipase causes lipolysis of adipocyte triglyceride and thereby acinar injury.
How do the lipolytic enzymes come into contact with the triglycerides? Although the stimulus for triglyceride release from adipocytes is unknown, adipocytes express a G protein (heterotrimeric guanosine 5′-triphosphate–binding protein)–coupled receptor activated proteolytically by trypsin (protease-activated receptor 4) (36, 37). Trypsin also increases the lipolytic response of adipocytes to adrenergic agents such as norepinephrine and isoproterenol (38). Addition of a serine protease–specific trypsin inhibitor (39) reduced the generation of glycerol when we cocultured adipocytes and acinar cells to 80% of that generated in its absence. This may partially explain how interstitial leakage of pancreatic enzymes affects lipolysis of adipocyte triglyceride. It is unlikely that fat within acinar cells contributes to obesity-associated adverse outcomes, because there is little evidence for fat accumulation within the acinar cell. Vacuoles thought to represent severe fat accumulation in the pancreas (40) can be seen on electron microscopy to be within cells that, unlike acinar cells, are nonpolarized, without the lumen-facing dense granules or basal nuclei. Additionally, vacuoles with a similar appearance may form in acinar cells as a result of altered vesicular trafficking during early cerulein pancreatitis or autophagy (41–43) in nonobese animals, which supports the nonspecific nature of this morphology.
The increase in serum UFAs with pancreatitis and the decrease with orlistat treatment were smaller in magnitude than the corresponding changes in serum cytokines and markers of renal and lung injury. This may be a result of saponification and renal excretion of serum UFAs, eventually resulting in tubular toxicity (44, 45). Additionally, the larger systemic and in vitro effects of orlistat compared to its local pancreatic effects may result from its limited permeability across membranes, as shown by its inability to significantly reduce isoproterenol-induced lipolysis. Orlistat inhibits lipogenesis in several cancer cell lines, but not in normal cells (for example, prostate epithelial cells) (46). These findings, along with orlistat’s limited entry into normal cells, indicate that its protective effect is not likely to be a result of inhibition of lipogenesis in our primary cell culture systems.
Although the exact lipases contributing to the adverse outcomes associated with obesity in pancreatitis remain uncharacterized, there are several that may have potential roles. Pancreatic acinar cells have four lipases [pancreatic triglyceride lipase (PTL), carboxyester lipase (CEL), and pancreatic lipase–like protein 1 and 2 (PLRP1 and PLRP2)] (47). Genetic knockout studies suggest redundancy of pancreatic lipases in lipolysis of dietary fat, with PTL/CEL knockout mice having normal weight gain. Although PLRP2 knockout mice exhibit a slight delay in weight gain before 3 weeks of age, the adults have normal fecal fat and are morphologically indistinguishable from their wild-type littermates (48). This redundancy is likely to contribute to the lipolysis of visceral adipose triglycerides, which result in NEFA formation and their downstream deleterious effects. Moreover, along with these four lipases, one or more of lipases from the infiltrating visceral adipocytes may contribute to lipolysis as well (49). Therefore, the identification of the specific lipases contributing to obesity-associated adverse outcomes of pancreatitis with a genetic approach may be challenging.
Our studies suggest that the UFAs generated from lipolysis contribute to the inflammation, necrosis, multisystem organ failure, and mortality in AP associated with obesity and that inhibition of lipolysis reduces these adverse outcomes. UFAs administered through various routes have replicated individual parts of the pathophysiology of multisystem organ failure, further supporting our conclusions. Dettelbach et al. noted hypocalcemia and intraperitoneal saponification by intraperitoneal instillation of oleic or linoleic acid, but not palmitic or stearic acid (50). Oleic acid administered intravenously at concentrations found in our study results in acute respiratory distress syndrome with lung myeloperoxidase increase and apoptosis (31, 32). Oleic acid and linoleic acid injected into the pancreatic duct induce pancreatitis (51). Similarly, UFAs can elevate serum creatinine (50) and cause renal tubular toxicity (52, 53).
The studies mentioned above, along with our work, demonstrate a pathogenic role of UFA-mediated lipotoxicity and lead us to hypothesize that this lipotoxicity may mediate adverse outcomes in acute illnesses. These findings are likely to apply to clinical circumstances such as severe burns, trauma, and other critical illness in addition to AP (54–58), in which worse outcomes have been noted in patients with elevated serum NEFAs. Elevated serum lipase levels in patients with burns (59), hemorrhagic shock (60), and critical illnesses (61) predict an adverse outcome, supporting a potential role of lipolysis in these clinical situations. The increased serum UFA concentrations (57), UFA/SFA ratios (58), and UFA metabolites (62) that have been seen in these acute illnesses are consistent with their contributing to UFA-mediated lipotoxicity.
The rapidity with which UFA caused release of intracellular calcium, inhibition of mitochondrial complexes I and V, acinar necrosis, and inflammatory mediator up-regulation in our studies, with renal, lung injury, and mortality occurring in a matter of days, is typical of the acute illnesses discussed (54–58). This time course is in contrast to chronic illnesses such as atherosclerosis, diabetes, and congestive heart failure, which progress over weeks to several months (63–66). Lipotoxicity in these chronic illnesses is from intracellular accumulation of excess SFAs or their metabolites (65, 67, 68), resulting in a reactive oxygen species formation (69), an endoplasmic reticulum stress response (70, 71), mitochondrial membrane damage (72), and apoptotic cell death (71, 73). Thus, acute UFA lipotoxicity is likely distinct from the chronic effects of excess SFAs.
In summary, we have shown that lipotoxicity contributes to the inflammatory response, multisystem organ failure, and necrotic acinar cell death in AP. Our findings suggest that inhibition of lipolysis may represent a viable therapeutic strategy in limiting local and systemic lipotoxicity, and the poor outcomes, associated with SAP. This condition, as well as other severe acute inflammatory conditions, currently has no specific therapy, especially in obese individuals. After identification of the responsible lipase or lipases, clinical studies should be designed to target these enzymes to test the efficacy of this approach in improving clinical outcomes during these devastating illnesses.
MATERIALS AND METHODS
All materials and methods are described in detail in the Supplementary Material.
Supplementary Material
Acknowledgments
We thank M. Kienholz, R. Brand, M. Lowe, and D. Whitcomb for a critical appraisal of this manuscript.
Funding: Supported by grant number UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the NIH, and NIH Roadmap for Medical Research (S.N. and V.P.S.), and award number R01DK092460 (V.P.S.) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Footnotes
SUPPLEMENTARY MATERIAL
www.sciencetranslationalmedicine.org/cgi/content/full/3/107/107ra110/DC1
Materials and Methods
Fig. S1. Quantification of IPF by CT method 1 and its correlation with histology.
Fig. S2. Immunohistochemistry showing CD68-positive macrophages accumulate around areas of peri-fat acinar necrosis.
Fig. S3. Schematic showing the setup of the coculture system and sources used for assays.
Fig. S4. Acinar cell death in coculture lacks evidence of autophagy and apoptosis.
Fig. S5. Effect of orlistat on isoproterenol-induced glycerol release by adipocytes.
Fig. S6. Orlistat prevents death and retains functionality of acinar cells in acinar adipocyte coculture.
Fig. S7. Inhibition of lipolysis prevents increase in resistin.
Fig. S8. Time course of NEFA-induced LDH leakage and dose response of linoleic acid–induced increase in intracellular calcium.
Fig. S9. Effect of intracellular calcium chelation on linoleic-induced acinar injury.
Fig. S10. Mitochondrial complexes II and IV and citrate synthase are not affected by fatty acids.
Fig. S11. Linoleic acid induces necrotic cell death.
Fig. S12. Lipase inhibition significantly reduces serum amylase and lipase during pancreatitis.
Fig. S13. Lipase inhibition does not reduce serum SFAs significantly during pancreatitis.
Fig. S14. Patients dying with acute renal failure during acute pancreatitis have renal tubular damage.
Fig. S15. Schematic showing potential mechanisms of obesity-induced severe pancreatitis.
Fig. S16. Representative images of pancreatic sections showing amount of intrapancreatic fat as quantified by the pathologist.
References
The contents of the manuscript are solely the responsibility of the authors and do not necessarily represent the official view of NCRR, NIDDK, or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overviewtranslational.asp. Also supported by a startup package from the University of Pittsburgh Department of Medicine (V.P.S.).
Author contributions: S.N. designed the methodologies for, provided access to, and supervised the analysis of autopsy data and histological analysis, and provided funding for the project. C.A. analyzed and quantified intrapancreatic fat, necrosis, and peri-fat acinar necrosis. J.P.D. measured, analyzed, and interpreted the NEFA concentrations. L.S.O. conducted the experiments involving Western blotting. C.J.B. supervised the calcium studies and interpretation of the data. S.S.S. designed, conducted, and interpreted the mitochondrial complex activity assays. C.D. executed the animal model of pancreatitis. J.M.K. conducted and analyzed the calcium studies. K.L. identified SAP patients and provided the pancreatic necrosis debridement fluid. K.T.B. designed and supervised the analysis and interpretation of CT data. A.F. designed and conducted the measurements on CT data. J.B. helped in designing and supervised the analysis and interpretation of polymerase chain reaction (PCR) data. S.L. conducted and analyzed the PCR studies. T.M. conducted, analyzed, and interpreted electron microscopy data. L.N. helped design and interpret autopsy studies. G.I.P. provided data on CT scans and clinical severity of endoscopic retrograde cholangiopancreatography pancreatitis. D.Y. analyzed and interpreted clinical statistics. V.P.S. designed and supervised the overall execution of the project, conducted and interpreted experimental in vitro and in vivo studies, and provided funding for the project.
Competing interests: The authors declare that they have no competing interests.
REFERENCES AND NOTES
- 1.Ghanem AM, Sen S, Philp B, Dziewulski P, Shelley OP. Body mass index (BMI) and mortality in patients with severe burns: Is there a “tilt point” at which obesity influences outcome? Burns. 2011;37:208–214. doi: 10.1016/j.burns.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 2.Neville AL, Brown CV, Weng J, Demetriades D, Velmahos GC. Obesity is an independent risk factor of mortality in severely injured blunt trauma patients. Arch. Surg. 2004;139:983–987. doi: 10.1001/archsurg.139.9.983. [DOI] [PubMed] [Google Scholar]
- 3.Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A. Obesity increases risk of organ failure after severe trauma. J. Am. Coll. Surg. 2006;203:539–545. doi: 10.1016/j.jamcollsurg.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 4.Oliveros H, Villamor E. Obesity and mortality in critically ill adults: A systematic review and meta-analysis. Obesity. 2008;16:515–521. doi: 10.1038/oby.2007.102. [DOI] [PubMed] [Google Scholar]
- 5.Papachristou GI, Papachristou DJ, Avula H, Slivka A, Whitcomb DC. Obesity increases the severity of acute pancreatitis: Performance of APACHE-O score and correlation with the inflammatory response. Pancreatology. 2006;6:279–285. doi: 10.1159/000092689. [DOI] [PubMed] [Google Scholar]
- 6.Porter KA, Banks PA. Obesity as a predictor of severity in acute pancreatitis. Int. J. Pancreatol. 1991;10:247–252. doi: 10.1007/BF02924162. [DOI] [PubMed] [Google Scholar]
- 7.Perides G, Laukkarinen JM, Vassileva G, Steer ML. Biliary acute pancreatitis in mice is mediated by the G-protein–coupled cell surface bile acid receptor Gpbar1. Gastroenterology. 2010;138:715–725. doi: 10.1053/j.gastro.2009.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pandol SJ, Raraty M. Pathobiology of alcoholic pancreatitis. Pancreatology. 2007;7:105–114. doi: 10.1159/000104235. [DOI] [PubMed] [Google Scholar]
- 9.Whitcomb DC. Clinical practice. Acute pancreatitis. N. Engl. J. Med. 2006;354:2142–2150. doi: 10.1056/NEJMcp054958. [DOI] [PubMed] [Google Scholar]
- 10.Heiss P, Bruennler T, Salzberger B, Lang S, Langgartner J, Feuerbach S, Schoelmerich J, Hamer OW. Severe acute pancreatitis requiring drainage therapy: Findings on computed tomography as predictor of patient outcome. Pancreatology. 2010;10:726–733. doi: 10.1159/000320710. [DOI] [PubMed] [Google Scholar]
- 11.Vege SS, Gardner TB, Chari ST, Munukuti P, Pearson RK, Clain JE, Petersen BT, Baron TH, Farnell MB, Sarr MG. Low mortality and high morbidity in severe acute pancreatitis without organ failure: A case for revising the Atlanta classification to include “moderately severe acute pancreatitis”. Am. J. Gastroenterol. 2009;104:710–715. doi: 10.1038/ajg.2008.77. [DOI] [PubMed] [Google Scholar]
- 12.Duarte-Rojo A, Sosa-Lozano LA, Saúl A, Herrera-Cáceres JO, Hernández-Cárdenas C, Vázquez-Lamadrid J, Robles-Díaz G. Methods for measuring abdominal obesity in the prediction of severe acute pancreatitis, and their correlation with abdominal fat areas assessed by computed tomography. Aliment. Pharmacol. Ther. 2010;32:244–253. doi: 10.1111/j.1365-2036.2010.04321.x. [DOI] [PubMed] [Google Scholar]
- 13.Schäffler A, Hamer O, Dickopf J, Goetz A, Landfried K, Voelk M, Herfarth H, Kopp A, Büchler C, Schölmerich J, Brünnler T. Admission resistin levels predict peripancreatic necrosis and clinical severity in acute pancreatitis. Am. J. Gastroenterol. 2010;105:2474–2484. doi: 10.1038/ajg.2010.278. [DOI] [PubMed] [Google Scholar]
- 14.Banks PA, Freeman ML. Practice Parameters Committee of the American College of Gastroenterology, Practice guidelines in acute pancreatitis. Am. J. Gastroenterol. 2006;101:2379–2400. doi: 10.1111/j.1572-0241.2006.00856.x. [DOI] [PubMed] [Google Scholar]
- 15.Pinnick KE, Collins SC, Londos C, Gauguier D, Clark A, Fielding BA. Pancreatic ectopic fat is characterized by adipocyte infiltration and altered lipid composition. Obesity. 2008;16:522–530. doi: 10.1038/oby.2007.110. [DOI] [PubMed] [Google Scholar]
- 16.Saisho Y, Butler AE, Meier JJ, Monchamp T, Allen-Auerbach M, Rizza RA, Butler PC. Pancreas volumes in humans from birth to age one hundred taking into account sex, obesity, and presence of type-2 diabetes. Clin. Anat. 2007;20:933–942. doi: 10.1002/ca.20543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klöppel G, Dreyer T, Willemer S, Kern HF, Adler G. Human acute pancreatitis: Its pathogenesis in the light of immunocytochemical and ultrastructural findings in acinar cells. Virchows Arch. A Pathol. Anat. Histopathol. 1986;409:791–803. doi: 10.1007/BF00710764. [DOI] [PubMed] [Google Scholar]
- 18.Sennello JA, Fayad R, Pini M, Gove ME, Ponemone V, Cabay RJ, Siegmund B, Dinarello CA, Fantuzzi G. Interleukin-18, together with interleukin-12, induces severe acute pancreatitis in obese but not in nonobese leptin-deficient mice. Proc. Natl. Acad. Sci. U.S.A. 2008;105:8085–8090. doi: 10.1073/pnas.0804091105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pezzilli R, Miniero R, Cappelletti O, Barakat B. Behavior of serum interleukin 12 in human acute pancreatitis. Pancreas. 1999;18:247–251. doi: 10.1097/00006676-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Rau B, Baumgart K, Paszkowski AS, Mayer JM, Beger HG. Clinical relevance of caspase-1 activated cytokines in acute pancreatitis: High correlation of serum interleukin-18 with pancreatic necrosis and systemic complications. Crit. Care Med. 2001;29:1556–1562. doi: 10.1097/00003246-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Ueda T, Takeyama Y, Yasuda T, Matsumura N, Sawa H, Nakajima T, Ajiki T, Fujino Y, Suzuki Y, Kuroda Y. Significant elevation of serum interleukin-18 levels in patients with acute pancreatitis. J. Gastroenterol. 2006;41:158–165. doi: 10.1007/s00535-005-1735-4. [DOI] [PubMed] [Google Scholar]
- 22.Wereszczynska-Siemiatkowska U, Mroczko B, Siemiatkowski A. Serum profiles of interleukin-18 in different severity forms of human acute pancreatitis. Scand. J. Gastroenterol. 2002;37:1097–1102. doi: 10.1080/003655202320378310. [DOI] [PubMed] [Google Scholar]
- 23.Pini M, Sennello JA, Cabay RJ, Fantuzzi G. Effect of diet-induced obesity on acute pancreatitis induced by administration of interleukin-12 plus interleukin-18 in mice. Obesity. 2010;18:476–481. doi: 10.1038/oby.2009.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Puchtler H, Meloan SN. Demonstration of phosphates in calcium deposits: A modification of von Kossa’s reaction. Histochemistry. 1978;56:177–185. doi: 10.1007/BF00495978. [DOI] [PubMed] [Google Scholar]
- 25.Gaisano HY, Lutz MP, Leser J, Sheu L, Lynch G, Tang L, Tamori Y, Trimble WS, Salapatek AM. Supramaximal cholecystokinin displaces Munc18c from the pancreatic acinar basal surface, redirecting apical exocytosis to the basal membrane. J. Clin. Invest. 2001;108:1597–1611. doi: 10.1172/JCI9110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lam PP, Cosen Binker LI, Lugea A, Pandol SJ, Gaisano HY. Alcohol redirects CCK-mediated apical exocytosis to the acinar basolateral membrane in alcoholic pancreatitis. Traffic. 2007;8:605–617. doi: 10.1111/j.1600-0854.2007.00557.x. [DOI] [PubMed] [Google Scholar]
- 27.Fallon MB, Gorelick FS, Anderson JM, Mennone A, Saluja A, Steer ML. Effect of cerulein hyperstimulation on the paracellular barrier of rat exocrine pancreas. Gastroenterology. 1995;108:1863–1872. doi: 10.1016/0016-5085(95)90151-5. [DOI] [PubMed] [Google Scholar]
- 28.Sternby B, Hartmann D, Borgström B, Nilsson A. Degree of in vivo inhibition of human gastric and pancreatic lipases by orlistat (tetrahydrolipstatin, THL) in the stomach and small intestine. Clin. Nutr. 2002;21:395–402. doi: 10.1054/clnu.2002.0565. [DOI] [PubMed] [Google Scholar]
- 29.Borgström B. Mode of action of tetrahydrolipstatin: A derivative of the naturally occurring lipase inhibitor lipstatin. Biochim. Biophys. Acta. 1988;962:308–316. doi: 10.1016/0005-2760(88)90260-3. [DOI] [PubMed] [Google Scholar]
- 30.Michelangeli F, East JM. A diversity of SERCA Ca2+ pump inhibitors. Biochem. Soc. Trans. 2011;39:789–797. doi: 10.1042/BST0390789. [DOI] [PubMed] [Google Scholar]
- 31.Hussain N, Wu F, Zhu L, Thrall RS, Kresch MJ. Neutrophil apoptosis during the development and resolution of oleic acid-induced acute lung injury in the rat. Am. J. Respir. Cell Mol. Biol. 1998;19:867–874. doi: 10.1165/ajrcmb.19.6.3118. [DOI] [PubMed] [Google Scholar]
- 32.Lai JP, Bao S, Davis IC, Knoell DL. Inhibition of the phosphatase PTEN protects mice against oleic acid-induced acute lung injury. Br. J. Pharmacol. 2009;156:189–200. doi: 10.1111/j.1476-5381.2008.00020.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ye ZW, Wu XM, Jiang JG. Expression changes of angiotensin II pathways and bioactive mediators during human preadipocytes-visceral differentiation. Metabolism. 2009;58:1288–1296. doi: 10.1016/j.metabol.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Sternfeld L, Yang F, Rodriguez JA, Ross C, Hayden MR, Carriere F, Liu G, Hofer W, Schulz I. Enhanced susceptibility to pancreatitis in severe hypertriglyceridaemic lipoprotein lipase-deficient mice and agonist-like function of pancreatic lipase in pancreatic cells. Gut. 2009;58:422–430. doi: 10.1136/gut.2007.146258. [DOI] [PubMed] [Google Scholar]
- 35.Yang F, Wang Y, Sternfeld L, Rodriguez JA, Ross C, Hayden MR, Carriere F, Liu G, Schulz I. The role of free fatty acids, pancreatic lipase and Ca2+ signalling in injury of isolated acinar cells and pancreatitis model in lipoprotein lipase-deficient mice. Acta Physiol. 2009;195:13–28. doi: 10.1111/j.1748-1716.2008.01933.x. [DOI] [PubMed] [Google Scholar]
- 36.Asfaha S, Cenac N, Houle S, Altier C, Papez MD, Nguyen C, Steinhoff M, Chapman K, Zamponi GW, Vergnolle N. Protease-activated receptor-4: A novel mechanism of inflammatory pain modulation. Br. J. Pharmacol. 2007;150:176–185. doi: 10.1038/sj.bjp.0706975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strande JL, Phillips SA. Thrombin increases inflammatory cytokine and angiogenic growth factor secretion in human adipose cells in vitro. J. Inflamm. 2009;6:4. doi: 10.1186/1476-9255-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giudicelli Y, Provin D, Pecquery R, Nordmann R. Influence of trypsin on lipolysis in human fat cells. Comparison with rat adipocytes. Biochim. Biophys. Acta. 1976;450:358–366. doi: 10.1016/0005-2760(76)90009-6. [DOI] [PubMed] [Google Scholar]
- 39.Ribeiro JK, Cunha DD, Fook JM, Sales MP. New properties of the soybean trypsin inhibitor: Inhibition of human neutrophil elastase and its effect on acute pulmonary injury. Eur. J. Pharmacol. 2010;644:238–244. doi: 10.1016/j.ejphar.2010.06.067. [DOI] [PubMed] [Google Scholar]
- 40.Lee Y, Lingvay I, Szczepaniak LS, Ravazzola M, Orci L, Unger RH. Pancreatic steatosis: Harbinger of type 2 diabetes in obese rodents. Int. J. Obes. 2010;34:396–400. doi: 10.1038/ijo.2009.245. [DOI] [PubMed] [Google Scholar]
- 41.Mareninova OA, Hermann K, French SW, O’Konski MS, Pandol SJ, Webster P, Erickson AH, Katunuma N, Gorelick FS, Gukovsky I, Gukovskaya AS. Impaired autophagic flux mediates acinar cell vacuole formation and trypsinogen activation in rodent models of acute pancreatitis. J. Clin. Invest. 2009;119:3340–3355. doi: 10.1172/JCI38674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saito I, Hashimoto S, Saluja A, Steer ML, Meldolesi J. Intracellular transport of pancreatic zymogens during caerulein supramaximal stimulation. Am. J. Physiol. 1987;253:G517–G526. doi: 10.1152/ajpgi.1987.253.4.G517. [DOI] [PubMed] [Google Scholar]
- 43.Watanabe O, Baccino FM, Steer ML, Meldolesi J. Supramaximal caerulein stimulation and ultrastructure of rat pancreatic acinar cell: Early morphological changes during development of experimental pancreatitis. Am. J. Physiol. 1984;246:G457–G467. doi: 10.1152/ajpgi.1984.246.4.G457. [DOI] [PubMed] [Google Scholar]
- 44.Hagenfeldt L. Renal excretion of free fatty acids. Clin. Chim. Acta. 1971;32:471–474. doi: 10.1016/0009-8981(71)90450-5. [DOI] [PubMed] [Google Scholar]
- 45.Kamijo A, Kimura K, Sugaya T, Yamanouchi M, Hase H, Kaneko T, Hirata Y, Goto A, Fujita T, Omata M. Urinary free fatty acids bound to albumin aggravate tubulointerstitial damage. Kidney Int. 2002;62:1628–1637. doi: 10.1046/j.1523-1755.2002.00618.x. [DOI] [PubMed] [Google Scholar]
- 46.Kridel SJ, Axelrod F, Rozenkrantz N, Smith JW. Orlistat is a novel inhibitor of fatty acid synthase with antitumor activity. Cancer Res. 2004;64:2070–2075. doi: 10.1158/0008-5472.can-03-3645. [DOI] [PubMed] [Google Scholar]
- 47.Lowe ME. The triglyceride lipases of the pancreas. J. Lipid Res. 2002;43:2007–2016. doi: 10.1194/jlr.r200012-jlr200. [DOI] [PubMed] [Google Scholar]
- 48.Lowe ME, Kaplan MH, Jackson-Grusby L, D’Agostino D, Grusby MJ. Decreased neonatal dietary fat absorption and T cell cytotoxicity in pancreatic lipase-related protein 2-deficient mice. J. Biol. Chem. 1998;273:31215–31221. doi: 10.1074/jbc.273.47.31215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bézaire V, Langin D. Regulation of adipose tissue lipolysis revisited. Proc. Nutr. Soc. 2009;68:350–360. doi: 10.1017/S0029665109990279. [DOI] [PubMed] [Google Scholar]
- 50.Dettelbach MA, Deftos LJ, Stewart AF. Intraperitoneal free fatty acids induce severe hypocalcemia in rats: A model for the hypocalcemia of pancreatitis. J. Bone Miner. Res. 1990;5:1249–1255. doi: 10.1002/jbmr.5650051210. [DOI] [PubMed] [Google Scholar]
- 51.Willemer S, Elsässer HP, Kern HF, Adler G. Tubular complexes in cerulein- and oleic acid-induced pancreatitis in rats: Glycoconjugate pattern, immunocytochemical, and ultrastructural findings. Pancreas. 1987;2:669–675. doi: 10.1097/00006676-198711000-00008. [DOI] [PubMed] [Google Scholar]
- 52.Ishola DA, Jr, Post JA, van Timmeren MM, Bakker SJ, Goldschmeding R, Koomans HA, Braam B, Joles JA. Albumin-bound fatty acids induce mitochondrial oxidant stress and impair antioxidant responses in proximal tubular cells. Kidney Int. 2006;70:724–731. doi: 10.1038/sj.ki.5001629. [DOI] [PubMed] [Google Scholar]
- 53.Moran JH, Nowak G, Grant DF. Analysis of the toxic effects of linoleic acid, 12,13-cis-epoxyoctadecenoic acid, and 12,13-dihydroxyoctadecenoic acid in rabbit renal cortical mitochondria. Toxicol. Appl. Pharmacol. 2001;172:150–161. doi: 10.1006/taap.2001.9149. [DOI] [PubMed] [Google Scholar]
- 54.Jeschke MG, Finnerty CC, Kulp GA, Przkora R, Mlcak RP, Herndon DN. Combination of recombinant human growth hormone and propranolol decreases hypermetabolism and inflammation in severely burned children. Pediatr. Crit. Care Med. 2008;9:209–216. doi: 10.1097/PCC.0b013e318166d414. [DOI] [PubMed] [Google Scholar]
- 55.Jeschke MG, Klein D, Herndon DN. Insulin treatment improves the systemic inflammatory reaction to severe trauma. Ann. Surg. 2004;239:553–560. doi: 10.1097/01.sla.0000118569.10289.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Domschke S, Malfertheiner P, Uhl W, Buchler M, Domschke W. Free fatty acids in serum of patients with acute necrotizing or edematous pancreatitis. Int. J. Pancreatol. 1993;13:105–110. doi: 10.1007/BF02786078. [DOI] [PubMed] [Google Scholar]
- 57.Sztefko K, Panek J. Serum free fatty acid concentration in patients with acute pancreatitis. Pancreatology. 2001;1:230–236. doi: 10.1159/000055816. [DOI] [PubMed] [Google Scholar]
- 58.Cogo PE, Giordano G, Badon T, Orzali A, Zimmermann IU, Zacchello F, Sauer PJ, Carnielli VP. Simultaneous measurement of the rates of appearance of palmitic and linoleic acid in critically ill infants. Pediatr. Res. 1997;41:178–182. doi: 10.1203/00006450-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 59.Ryan CM, Sheridan RL, Schoenfeld DA, Warshaw AL, Tompkins RG. Postburn pancreatitis. Ann. Surg. 1995;222:163–170. doi: 10.1097/00000658-199508000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Malinoski DJ, Hadjizacharia P, Salim A, Kim H, Dolich MO, Cinat M, Barrios C, Lekawa ME, Hoyt DB. Elevated serum pancreatic enzyme levels after hemorrhagic shock predict organ failure and death. J. Trauma. 2009;67:445–449. doi: 10.1097/TA.0b013e3181b5dc11. [DOI] [PubMed] [Google Scholar]
- 61.Manjuck J, Zein J, Carpati C, Astiz M. Clinical significance of increased lipase levels on admission to the ICU. Chest. 2005;127:246–250. doi: 10.1378/chest.127.1.246. [DOI] [PubMed] [Google Scholar]
- 62.Kosaka K, Suzuki K, Hayakawa M, Sugiyama S, Ozawa T. Leukotoxin, a linoleate epoxide: Its implication in the late death of patients with extensive burns. Mol. Cell. Biochem. 1994;139:141–148. doi: 10.1007/BF01081737. [DOI] [PubMed] [Google Scholar]
- 63.Chiu HC, Kovacs A, Ford DA, Hsu FF, Garcia R, Herrero P, Saffitz JE, Schaffer JE. A novel mouse model of lipotoxic cardiomyopathy. J. Clin. Invest. 2001;107:813–822. doi: 10.1172/JCI10947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cummings BP, Digitale EK, Stanhope KL, Graham JL, Baskin DG, Reed BJ, Sweet IR, Griffen SC, Havel PJ. Development and characterization of a novel rat model of type 2 diabetes mellitus: The UC Davis type 2 diabetes mellitus UCD-T2DM rat. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008;295:R1782–R1793. doi: 10.1152/ajpregu.90635.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhou YT, Grayburn P, Karim A, Shimabukuro M, Higa M, Baetens D, Orci L, Unger RH. Lipotoxic heart disease in obese rats: Implications for human obesity. Proc. Natl. Acad. Sci. U.S.A. 2000;97:1784–1789. doi: 10.1073/pnas.97.4.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bemelmans WJ, Lefrandt JD, Feskens EJ, Broer J, Tervaert JW, May JF, Smit AJ. Change in saturated fat intake is associated with progression of carotid and femoral intimamedia thickness, and with levels of soluble intercellular adhesion molecule-1. Atherosclerosis. 2002;163:113–120. doi: 10.1016/s0021-9150(01)00747-x. [DOI] [PubMed] [Google Scholar]
- 67.Lee Y, Hirose H, Ohneda M, Johnson JH, McGarry JD, Unger RH. β-Cell lipotoxicity in the pathogenesis of non-insulin-dependent diabetes mellitus of obese rats: Impairment in adipocyte–β-cell relationships. Proc. Natl. Acad. Sci. U.S.A. 1994;91:10878–10882. doi: 10.1073/pnas.91.23.10878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shimabukuro M, Zhou YT, Levi M, Unger RH. Fatty acid-induced β cell apoptosis: A link between obesity and diabetes. Proc. Natl. Acad. Sci. U.S.A. 1998;95:2498–2502. doi: 10.1073/pnas.95.5.2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee Y, Naseem RH, Park BH, Garry DJ, Richardson JA, Schaffer JE, Unger RH. α-Lipoic acid prevents lipotoxic cardiomyopathy in acyl CoA-synthase transgenic mice. Biochem. Biophys. Res. Commun. 2006;344:446–452. doi: 10.1016/j.bbrc.2006.03.062. [DOI] [PubMed] [Google Scholar]
- 70.Peng G, Li L, Liu Y, Pu J, Zhang S, Yu J, Zhao J, Liu P. Oleate blocks palmitate-induced abnormal lipid distribution, endoplasmic reticulum expansion and stress, and insulin resistance in skeletal muscle. Endocrinology. 2011;152:2206–2218. doi: 10.1210/en.2010-1369. [DOI] [PubMed] [Google Scholar]
- 71.Borradaile NM, Han X, Harp JD, Gale SE, Ory DS, Schaffer JE. Disruption of endoplasmic reticulum structure and integrity in lipotoxic cell death. J. Lipid Res. 2006;47:2726–2737. doi: 10.1194/jlr.M600299-JLR200. [DOI] [PubMed] [Google Scholar]
- 72.Ostrander DB, Sparagna GC, Amoscato AA, McMillin JB, Dowhan W. Decreased cardiolipin synthesis corresponds with cytochrome c release in palmitate-induced cardiomyocyte apoptosis. J. Biol. Chem. 2001;276:38061–38067. doi: 10.1074/jbc.M107067200. [DOI] [PubMed] [Google Scholar]
- 73.Listenberger LL, Ory DS, Schaffer JE. Palmitate-induced apoptosis can occur through a ceramide-independent pathway. J. Biol. Chem. 2001;276:14890–14895. doi: 10.1074/jbc.M010286200. [DOI] [PubMed] [Google Scholar]
- 74.Singh VP, Bren GD, Algeciras-Schimnich A, Schnepple D, Navina S, Rizza SA, Dawra RK, Saluja AK, Chari ST, Vege SS, Badley AD. Nelfinavir/ritonavir reduces acinar injury but not inflammation during mouse caerulein pancreatitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2009;296:G1040–G1046. doi: 10.1152/ajpgi.90642.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alcantara EN., Jr Functioning acinar cell carcinoma of the pancreas. Can. Med. Assoc. J. 1962;87:970–973. [PMC free article] [PubMed] [Google Scholar]
- 76.Pasyk K. Studies on subcutaneous fat necrosis of the newborn. Virchows Arch. A Pathol. Anat. Histol. 1978;379:243–259. doi: 10.1007/BF00432639. [DOI] [PubMed] [Google Scholar]
- 77.Kodama Y, Ng CS, Wu TT, Ayers GD, Curley SA, Abdalla EK, Vauthey JN, Charnsangavej C. Comparison of CT methods for determining the fat content of the liver. AJR Am. J. Roentgenol. 2007;188:1307–1312. doi: 10.2214/AJR.06.0992. [DOI] [PubMed] [Google Scholar]
- 78.Singh VP, Saluja AK, Bhagat L, van Acker GJ, Song AM, Soltoff SP, Cantley LC, Steer ML. Phosphatidylinositol 3-kinase-dependent activation of trypsinogen modulates the severity of acute pancreatitis. J. Clin. Invest. 2001;108:1387–1395. doi: 10.1172/JCI12874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Singh VP, McNiven MA. Src-mediated cortactin phosphorylation regulates actin localization and injurious blebbing in acinar cells. Mol. Biol. Cell. 2008;19:2339–2347. doi: 10.1091/mbc.E07-11-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Singh VP, Saluja AK, Bhagat L, Hietaranta AJ, Song A, Mykoniatis A, Van Acker GJ, Steer ML. Serine protease inhibitor causes F-actin redistribution and inhibition of calcium-mediated secretion in pancreatic acini. Gastroenterology. 2001;120:1818–1827. doi: 10.1053/gast.2001.24883. [DOI] [PubMed] [Google Scholar]
- 81.Viswanadha S, Londos C. Determination of lipolysis in isolated primary adipocytes. Methods Mol. Biol. 2008;456:299–306. doi: 10.1007/978-1-59745-245-8_22. [DOI] [PubMed] [Google Scholar]
- 82.Arnould S, Takahashi M, Camadro JM. Acylation stabilizes a protease-resistant conformation of protoporphyrinogen oxidase, the molecular target of diphenyl ether-type herbicides. Proc. Natl. Acad. Sci. U.S.A. 1999;96:14825–14830. doi: 10.1073/pnas.96.26.14825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hietaranta AJ, Singh VP, Bhagat L, van Acker GJ, Song AM, Mykoniatis A, Steer ML, Saluja AK. Water immersion stress prevents caerulein-induced pancreatic acinar cell NF-κB activation by attenuating caerulein-induced intracellular Ca2+ changes. J. Biol. Chem. 2001;276:18742–18747. doi: 10.1074/jbc.M009721200. [DOI] [PubMed] [Google Scholar]
- 84.Orlichenko LS, Behari J, Yeh TH, Liu S, Stolz DB, Saluja AK, Singh VP. Transcriptional regulation of CXC-ELR chemokines KC and MIP-2 in mouse pancreatic acini. Am. J. Physiol. Gastrointest. Liver Physiol. 2010;299:G867–G876. doi: 10.1152/ajpgi.00177.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Phillips PA, Yang L, Shulkes A, Vonlaufen A, Poljak A, Bustamante S, Warren A, Xu Z, Guilhaus M, Pirola R, Apte MV, Wilson JS. Pancreatic stellate cells produce acetylcholine and may play a role in pancreatic exocrine secretion. Proc. Natl. Acad. Sci. U.S.A. 2010;107:17397–17402. doi: 10.1073/pnas.1000359107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carvalho MA, Zecchin KG, Seguin F, Bastos DC, Agostini M, Rangel AL, Veiga SS, Raposo HF, Oliveira HC, Loda M, Coletta RD, Graner E. Fatty acid synthase inhibition with orlistat promotes apoptosis and reduces cell growth and lymph node metastasis in a mouse melanoma model. Int. J. Cancer. 2008;123:2557–2565. doi: 10.1002/ijc.23835. [DOI] [PubMed] [Google Scholar]
- 87.Kangani CO, Kelley DE, Delany JP. New method for GC/FID and GC–C-IRMS analysis of plasma free fatty acid concentration and isotopic enrichment. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2008;873:95–101. doi: 10.1016/j.jchromb.2008.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gukovskaya AS, Mareninova OA, Odinokova IV, Sung KF, Lugea A, Fischer L, Wang YL, Gukovsky I, Pandol SJ. Cell death in pancreatitis: Effects of alcohol. J. Gastroenterol. Hepatol. 2006;21 Suppl. 3:S10–S13. doi: 10.1111/j.1440-1746.2006.04571.x. [DOI] [PubMed] [Google Scholar]
- 89.Shiva S, Sack MN, Greer JJ, Duranski M, Ringwood LA, Burwell L, Wang X, MacArthur PH, Shoja A, Raghavachari N, Calvert JW, Brookes PS, Lefer DJ, Gladwin MT. Nitrite augments tolerance to ischemia/reperfusion injury via the modulation of mitochondrial electron transfer. J. Exp. Med. 2007;204:2089–2102. doi: 10.1084/jem.20070198. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.