Abstract
Objective
The authors of this study collaborated in the analysis of public health survey data in order to inform future statewide interventions that could systematically enhance depression screening and mental health service use for women of reproductive age. The primary objective of the study was to empirically inform and test the program theory components of a motivational interviewing intervention that we anticipate will guide statewide practice and policy priorities.
Methods
Data were examined from a survey of healthcare practitioners statewide (n=1498) regarding their practices with and perceptions of perinatal depression care for women. Confirmatory factor analysis (CFA) was used to measure two latent constructs: health provider confidence in the ability to diagnose and treat and the importance placed on screening and treatment. Structural equation modeling (SEM) was used to test a program theory supporting motivational interviewing using a model implied relationship between confidence and importance on screening and treatment/referral practices.
Results
The data fit the model; the model provisionally supports motivational interviewing as an intervention influencing provider attitudes and practices surrounding perinatal depression screening and treatment/referral.
Conclusions
Ultimately, study findings support statewide public health efforts to expand the role of health providers in recognizing and responding to perinatal depression and suggest that motivational interviewing techniques that augment importance and confidence may lead to enhanced screening and referral/treatment outcomes for pregnant and postpartum women.
Introduction
Perinatal depression has become an instrumental focus within many statewide public health outreach efforts because of its documented impact on the longitudinal health and emotional well-being of both mothers and infants.1,2 Although the literature demonstrates the efficacy of a range of supportive, behavioral, psychopharmacologic, and alternative interventions for perinatal depression,3–7 concern remains that women are not being adequately screened, assessed, or referred for intervention when symptoms are identified.
Policy initiatives regarding perinatal depression
Policymakers and women's health advocates alike express a desire to increase the number of women screened for depression and subsequently link depressed women to treatment. In 2002, the U.S. Preventive Services Task Force (USPSTF) made specific recommendations about the potential benefit of identification and treatment of depression during and around the time of pregnancy.8 In 2009, the National Research Council (NRC) and the Institute of Medicine (IOM) reaffirmed the important linkages between parenting and mental health, urging enhanced screening and intervention efforts during this critical time period of women's life span health.9 In spite of this conceptual support, there are significant gaps evaluating the efficacy of many current practice and policy initiatives related to depression screening and subsequent treatment.
Implementing widespread depression screening by a cadre of trained providers is often the first step in the process of augmenting perinatal mental health. There is a solid literature base describing and evaluating standardized screening instruments that are valid for detecting depression during pregnancy and the postpartum.7 Successful initiatives to expand statewide provider education about depression screening have been effective,2,10 although the impact of universal screening programs on referral or service utilization patterns is less definitive. For example, the study by Segre et al. based in an urban Healthy Start project describes a specific training approach to perinatal depression screening that effectively enhanced screening rates statewide; however, the study was not able to demonstrate evidence of corresponding diagnostic identification, treatment, or a change in clinical outcomes associated with enhanced screening.10 Additionally, research examining the impact of New Jersey's legislated efforts to screen women potentially experiencing postpartum depression (PPD) indicates that in spite of widespread provider screening, lower-income women in particular did not experience any significant change in receipt of mental health services after that policy's implementation.11 A consistent issue raised across studies is the gap between identification and treatment; specifically, the availability of adequate mental health services and successful linkage from health provider screening to these services, particularly for low-income women.
The concerns and experiences of front-line healthcare providers are integral to the success of large-scale policy and practice initiatives. Although this study focuses predominantly on physicians, there is an important but distinct body of literature about the implementation and success of perinatal depression screening in maternal and child health settings, including both U.S. and international studies of nurses and home visitors. There are also published studies from public health efforts within the United States, such as Healthy Start, where depression screening is conducted by nurses, social workers, and paraprofessional home visitors within communities at elevated risk for fetal and infant mortality.2,12,13 It is the formal medical provider sector, however, that is the focus of the present study because many women seek formal healthcare during pregnancy and the postpartum, even if they did not have health providers.11 Best practices for healthcare providers are readily available, including written guidelines for physicians about screening and referral of pregnant and postpartum women, complete with algorithms to help guide appropriate clinical decision making.14–16 In spite of these successes, moving from increased provider knowledge about screening and treatment/referral to real-world translation and implementation of screening and intervention by these health professionals has been a larger challenge.
Specific attention recently has been directed to the two healthcare provider groups most likely to have widespread contact with women during and around the time of pregnancy: obstetrician/gynecologists and pediatricians. Among obstetricians/gynecologists, several authors point to the need for more consistency in both recommended screening and treatment and referral services; however, the perceived responsibility for depression screening is also reportedly high in this group.16–18 Pediatricians, however, have mixed responses to maternal depression screening. It is noteworthy that pediatricians are essentially asked to perform depression screening on their patient's family member. This extension of practice to a nonpatient population may create an ethical challenge for pediatric providers, although they are often prompted by their physician colleagues to take stronger and more active roles in screening and referral as an extension of their care and advocacy for infants and young children.19–21
The present study is grounded within this growing evidence base informing public health approaches to perinatal depression screening and intervention by healthcare providers. Rigorous program evaluation emphasizes the importance of selecting intervention approaches that measure both the process of change (often referred to as “program theory”) and the outcomes of a program or service. In this study, the authors evaluate the fit of a selected future intervention model by examining the process components of the intervention (program theory) that we believe may lead to actual, desirable practice changes. Specifically, we consider whether motivational interviewing22,23 should be applied as an evidence-informed intervention model for future provider education. Therefore, we have selected two elements associated with the process of change in motivational interviewing (importance and confidence) and modeled these constructs as two components of a program theory predicting current screening and treatment/referral practices among healthcare providers.
Motivational interviewing as an intervention strategy asserts that altering the perceived importance of the desired change and confidence in the ability to affect the change will overcome ambivalence and move the individual toward desirable action.22 For healthcare providers in particular, knowledge about perinatal depression screening may not be enough to produce a desired change in practice behaviors. Given the assumption that ambivalence may stand in the way of change for some individuals, those respondents who were already engaged in high levels of screening and treatment/referral may have overcome their ambivalence because of heightened importance and confidence regarding perinatal depression screening and treatment. Formally evaluating the degree to which importance and confidence may already be linked to desirable practice outcomes would then lend support to a corresponding intervention model (motivational interviewing) that uses the same constructs to assert a program theory of change.
In order to evaluate whether the constructs of importance and confidence within motivational interviewing were indeed conceptually linked with desirable outcomes of enhanced depression screening and treatment/referral, this study reanalyzed data from the statewide survey of healthcare providers to conceptually model and empirically test this program theory. Structural equation modeling (SEM) provides an analytic framework that addresses the question of exactly how well this particular program theory fits with enhanced screening and treatment/referral practices, which are the desired outcomes of our statewide provider education program. A structural model with a good fit will offer an empirically informed direction for future statewide provider training efforts.
Project background
The Virginia Department of Health (VDH) has been actively working in the area of perinatal depression screening and intervention throughout the past decade. From 2005 to the present, major initiatives between VDH and its academic, community, and healthcare provider partners have included the formation of an expert panel on perinatal depression and the development of a free web-based training course for healthcare providers through a state university's on-line continuing medical education (CME) program. Considerable effort has been put into the development of comprehensive provider training as well as implementation of enhanced reimbursement guidelines that allow health providers to bill for parental depression screening conducted during pregnancy, as well as the child's health visits. Currently, statewide partnerships are developing expanded provider training that encourages widespread screening and brief intervention efforts (some of which are based in motivational interviewing) that target perinatal depression concomitantly with substance abuse and interpersonal violence.
The current study builds on these existing statewide infrastructure enhancements promoting perinatal depression screening and treatment/referral among prescribing health providers. From data already collected through our partnership, we empirically tested a structural equation model that depicted healthcare providers' perceived importance of depression screening and their confidence in their ability to screen and treat/refer as causally influencing their actual practices with regard to screening and treatment/referral. Three sequential research questions guide this study: (1) What are the perceptions and practices of healthcare providers related to perinatal depression following recent statewide provider education approaches and service enhancements? (descriptive data). (2) To what extent do the surveyed perceptions of healthcare providers reflect constructs of importance and confidence? (measurement/confirmatory factor models). (3) To what extent does the program theory implied by motivational interviewing (integrating the constructs of importance and confidence) explain the relationship between provider perceptions and practices and offer a framework for future healthcare provider training? (structural equation model).
Materials and Methods
The data on which the present study was based were collected by the VDH from July 2008 to January 2009. This mailed survey of prescribing healthcare providers was conducted at the conclusion of a 4-year perinatal depression provider education campaign; at the start of that campaign in 2005, a baseline version of the survey had been administered. This study focuses solely on the follow-up perinatal provider survey data in order to examine trends after a statewide knowledge-based educational campaign. The follow-up provider survey data were collected and retained by the VDH. The first author completed a secondary data analysis with the deidentified data in partnership with the health department. The Institutional Review Boards for VDH and Virginia Commonwealth University determined this secondary analysis to be exempt.
Sample
In an effort to generate an adequate (and representative) statewide healthcare provider sample, a complete listing of physicians, nurse practitioners, and certified nurse midwives was purchased from the Medical Marketing Service (MMS). In an attempt to ensure that the sampling frame was representative of the eligible Virginia workforce, the proportion of physicians, nurse practitioners, and certified nurse midwives employed statewide was calculated and applied to the sampling frame by MMS. To be included in the sample, healthcare providers had to have a license to practice in Virginia and a mailing address in Virginia. Physicians comprised 70% of the eligible provider population and, therefore, constituted 70% of the sample (6987 eligible and 4970 randomly sampled). Physician specialties included in the sample were adolescent medicine, family practice, general medicine, general preventive medicine, internal medicine, maternal and fetal medicine, internal medicine-pediatrics, neonatal-perinatal medicine, obstetrics and gynecology, obstetrics, obstetrics and gynecology critical care, pediatrics, and reproductive endocrinology. Nurse practitioners, who comprise 27% of the workforce, were sampled from within the practice specialties of adult medicine, family medicine, internal medicine, and women's health (2677 eligible and 723 randomly sampled). Certified nurse midwives made up 3% of the eligible population; all 318 eligible certified nurse midwives were included in the sample because of the small size of this subpopulation. In addition, a number of nonprescribing healthcare providers (RNs and social workers) responded to the survey. Their responses were retained for the analysis, although it is likely that the mailed survey was passed from a prescribing provider to them.
The follow-up provider survey used for this study had an overall response rate of 25.3% (1498 of 5931), which was a slight improvement over the 20% response rate from the original baseline survey in 2005. We examined postsurvey response rates by provider type to further assess sample representativeness. Response rates differed only slightly by provider type; nurse practitioners had a response rate of 29%, certified nurse midwives had a response rate of 23%, and physicians had a response rate of 21%.
Measures
The 36-item survey instrument used in this study was originally piloted in Eastern Virginia and subsequently reviewed and finalized by an expert panel of over 50 providers, academics, and public health personnel statewide representing all major healthcare and mental health advocacy groups. Survey items included demographic information, self-reported attitudes and beliefs regarding perinatal depression (7-point scale), a section on routine practices (only completed by those who had managed a case involving perinatal depression) measured via 5-point Likert-type scale items, a series of descriptive dichotomous questions assessing barriers and facilitators to treatment, and as a final section containing 5-point Likert-type scale questions about satisfaction with training and desire for future education and training resources. The survey was designed for nongeneralizable evaluative purposes; therefore, formal psychometric analyses had not been conducted before this study.
Analysis
The initial analysis focused on describing current statewide provider practices. Specifically, the descriptive analysis used SPSS 19.0 to identify significant areas of similarity and difference based on provider specialization, geographic setting of practice, and experience managing (diagnosing or treating) a case of perinatal depression. After this descriptive evaluation report for public health surveillance, the authors recognized that there were important preliminary findings that if reanalyzed, could inform the next steps of program development across the state, as previously described. Because we planned to focus our model on causal paths that influenced both screening and treatment/referral patterns, only those providers who identified that they had managed (diagnosed or treated) a case of perinatal depression in their current practice (referred to as Managed case in Table 1) were included in the statistical modeling analysis.
Table 1.
Survey Sample Demographics (Including Raw Percentage)
| Demographic characteristic | Overall sample (n=1498) | Managed case (n=859) |
|---|---|---|
| Gender | ||
| Female | 893 (59.6%) | 527 (61.4%) |
| Male | 604 (40.4%) | 332 (38.6%) |
| Race | ||
| White, non-Hispanic | 1093 (73.0%) | 680 (79.2%) |
| African American | 81 (5.4%) | 35 (4.1%) |
| Hispanic ethnicity, any race | 38 (2.5%) | 24 (2.8%) |
| Asian | 187 (12.5%) | 72 (8.4%) |
| Other | 63 (4.2%) | 33 (3.8%) |
| Physicians | 999 (67.5%) | 561 (65.3%) |
| Family medicine | 299 (20.4%) | 216 (25.1%) |
| Obstetrics/gynecology | 178 (12.0%) | 164 (19.1%) |
| Pediatrics | 250 (16.7%) | 73 (8.5%) |
| Other MD | 272 (18.4%) | 108 (12.6%) |
| Other professionals | 330 (22.0%) | 196 (22.8%) |
| Nurse practitioner or physician assistant | 213 (14.2%) | 109 (12.7%) |
| Nurse midwife | 74 (4.9%) | 64 (7.5%) |
| Registered nurse or social worker | 26 (1.7%) | 23 (2.7%) |
| Practice setting | ||
| Private practice | 980 (65.4%) | 629 (73.2%) |
| Hospital | 235 (15.7%) | 102 (11.9%) |
| Health department | 39 (2.6%) | 24 (2.8%) |
| Home health or other | 277 (18.5%) | 126 (14.7%) |
| Geography | ||
| Urban | 356 (23.8%) | 175 (20.4%) |
| Suburban | 821 (54.8%) | 487 (56.7%) |
| Rural | 262 (17.5%) | 170 (19.8%) |
| Years in practice | ||
| ≥ 16 | 855 (57.1%) | 481 (56.0%) |
| 11–16 | 250 (16.7%) | 144 (16.8%) |
| 6–10 | 253 (16.9%) | 160 (18.6%) |
| 1–5 | 136 (9.1%) | 72 (8.4%) |
The emergence of mathematical and statistical modeling as a progressive alternative to traditional use of null hypothesis statistical testing allows for the prospect of interpreting data not as fact unto itself but as stemming from a larger conceptual and theoretical knowledge base that is defined by theories and models.24 When engaging in statistical modeling, the goal is to fit and test a model by applying local data to it and then determine if the fit of the data to the model empirically supports a theoretically grounded causal explanation. As previously discussed, the program theory model for this study is based in the change process components of a motivational interviewing intervention. The fit of the model, as conceptualized, was evaluated through confirmatory factor analysis (CFA) and SEM using MPlus 6.1.25,26
Although the provider survey was originally designed for program evaluation, the instrument contained several individual items related to provider attitudes and beliefs about the importance of perinatal depression screening and treatment/referral as well as confidence in the ability to successfully engage in these tasks. The authors entered into both CFA and SEM with the knowledge that measurement error and item response sets could create measurement challenges, particularly with regard to correlated residuals among the specific items either within or between latent constructs. Additionally, to account for nonnormality among the item distributions, we used maximum likelihood estimation with robust standard errors (MLR) as an analytic option within MPlus.26
Results
In the overall sample (n=1498), the majority of respondents were physicians (67.5%), with the additional 22% comprising other professionals, including nurse practitioners (14.2%), nurse midwives (4.9%), and RNs and social workers (1.7%), who were not intentionally sampled but did respond. The breakdown of the study sample by demographic features, specific professional specialization, setting of practice, and years of experience is provided in Table 1. Within the overall sample, 71% routinely (all of the time or often) assessed for perinatal depression among pregnant and postpartum women during healthcare visits. These findings are relatively consistent with other statewide surveillance systems; the state's 2007–2008 Pregnancy Risk Assessment Monitoring System (PRAMS) data showed that 78% of women reported that a healthcare provider had spoken to them about PPD.27
Among those providers who had ever managed (diagnosed or treated) a case, 51.6% indicated that they routinely (all of the time or often) either treat or refer patients with perinatal depression, 33.5% reported occasional treatment/referral, and 12.7% indicated they rarely or never treated or referred in routine practice. Ways of responding to perinatal depression included referring to a mental health specialist (81%), prescribing medication (74.9%), counseling by the provider in the office (41.7%), involving a partner or family member (39.3%), referring to a support group (32%), providing written information about depression (23.9%), referring to a primary care provider (18.9%), using an in-house mental health specialist (11.9%), and counseling in office by another health provider (9.9%); only 3% reported no routine form of treatment. Inadequate time was the most commonly reported barrier to treatment/referral (41.4%), followed by inadequate available treatment services (24.4%), inadequate reimbursement (17.8%), and inadequate provider knowledge/skills (15.8%).
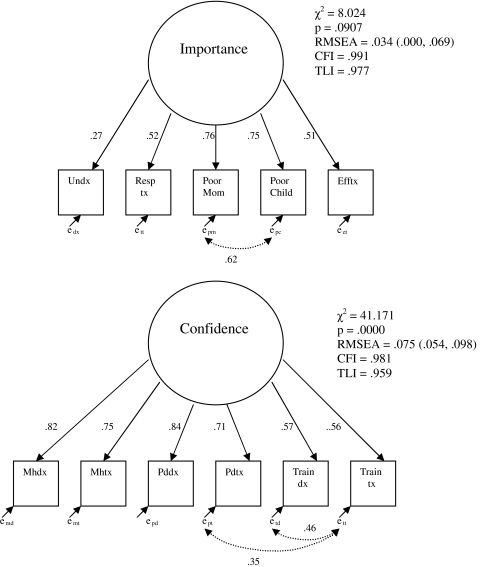
Confirmatory factor analysis
Two latent constructs were tested using CFA. The first construct, importance of perinatal depression screening and treatment/referral, was initially theorized to consist of six items. Items included the degree to which the respondent believed that depression goes undiagnosed, that she or he was responsible for treatment, that she or was responsible for screening, that depression led to poor outcomes for mothers, that depression led to poor outcomes for children, and that there are effective treatments available. Initial factor loadings indicated that the item, felt responsible for screening, had a very low factor loading (<0.15) and nearly universal endorsement by all participants; social desirability bias was also a concern with this item. Once it was removed from the model, factor loadings on all remaining items were between 0.27 and 0.76, which suggests that the removed item may have been highly correlated with the other items, reducing empirical strength of the CFA model. One restriction was placed on the model between the residuals for items addressing poor outcomes for mothers and children based on conceptual realization that there was significant overlap in these constructs; this correlation was indeed significant (0.62, p<0.0005). The CFA model as specified was able to be identified with fit statistics well within accepted standards (chi-square=8.02, df=4, p=0.09, root mean square error of approximations [RMSEA]=0.034, comparative fit index [CFI]=0.991, Tucker-Lewis index [TLI]=0.977). The model supports the latent construct of importance as comprising these five items.
The second construct, confidence in the ability to screen and treat perinatal depression, comprised six total items; four items measured areas of confidence about perinatal depression screening, perinatal depression treatment, mental health screening, and mental health treatment, and two items rated their current level of professional training regarding perinatal depression diagnosis as well as perinatal depression treatment. The final CFA model produced factor loadings ranging from 0.56 to 0.84. Two restrictions were placed on the model based on the conceptualized overlap between the two adequacy of training items and between the self-assessed adequacy of training regarding treatment and self-reported confidence in perinatal depression treatment items; both correlations were significant (0.46 and 0.35, respectively, p<0.0005). The final model did not result in an insignificant chi-square value (chi-square=41.17, df=15, p<0.0005) but had acceptable fit statistics (RMSEA=0.075, CFI=0.981, TLI=0.959). Based on these fit statistics, the latent construct of confidence in depression screening and treatment ability was also retained. Figure 1 depicts the final CFA models with the standardized factor loadings.
FIG. 1.
Confirmatory factor analysis (CFA) models for latent variables (standardized factor loadings).
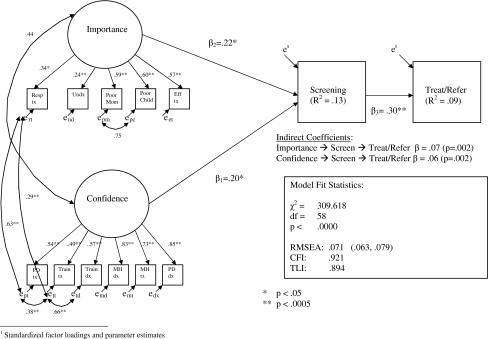
Specification of program theory
In order to test the program theory based in motivational interviewing, we specified a conceptual model linking importance and confidence, the latent constructs we identified through CFA, with two outcome variables: frequency of provider screening of all pregnant/postpartum women and frequency of treatment/referral to treatment. Both outcome variables were measured with items that used a 5 point scale (all of the time, often, sometimes, rarely, never). We conceptualized a model where confidence and importance were correlated with each other, and these two latent constructs together directly influenced perinatal depression screening, which in turn influenced perinatal depression treatment/referral.
Additionally, we consulted modification indices and added two additional path coefficients, correlating the residuals among the treatment responsibility, training adequacy, and confidence items. Freeing these parameters aligned our conceptual assumptions with empirical support to address probable measurement error.28,29 The chi-square value of the final standard error of the means (SEM) model remained significant (chi-square=309.62, df=58, p<0.0005) but had fit statistics we deemed to be acceptable (RMSEA=0.071, CFI=0.921, TLI=0.890).28 It is noteworthy that all path coefficients in the final model were significant at the 0.05 level, as were both of the conceptualized indirect paths leading from importance and confidence through screening and treatment/referral outcomes. The R2 values for the two outcome variables are rather low (0.13 for screening and 0.09 for treatment/referral), which also attests to the probable influence of measurement error in the outcome variables. Overall, these findings support the theorized relationships between constructs in the model, as consistent with a program theory based in motivational interviewing. The final model containing all factor loadings and standardized path coefficients is shown in Figure 2.
FIG. 2.
Program theory structural equation model: Motivational interviewing components informing key outcomes (standardized factor loadings and parameter estimates). RMSEA, Root Mean Square Error of Approximation; CFI, Comparative Fit Index; TLI, Tucker-Lewis Index.
A final test of model rigor was conducted by evaluating a hypothesized alternative model, also based in motivational interviewing. This nested comparison technique is used to assess the best fit among similar models. In the alternative model, we conceptualized importance having a direct relationship on confidence, and we added an additional regression path assessing the direct relationship between these latent constructs. When the alternative model was tested, confidence was not significantly related to screening, the indirect path involving confidence was not significant, and the overall model had less goodness-of-fit than our primary model (chi-square=537.32, df=60, p<0.0005; RMSEA=0.09, CFI=0.85, TLI=0.81). Therefore, we retained our original model as the best fit.
Discussion
This study and its analytic approach open a dialogue about healthcare providers' motivation to screen and subsequently treat/refer women experiencing perinatal depression. Our study found that two constructs, importance and confidence, predicted providers' implementation of perinatal depression screening and treatment/referral. As shown in the model, these constructs work in tandem to influence desirable outcomes. The fit of the model suggests that motivational interviewing, assessed through its program theory components of importance and confidence, may be useful as a provider-focused intervention strategy to enhance screening and treatment/referral outcomes statewide. These results provide an evidence-based foundation on which to consider innovative training strategies that build provider confidence and enhance perceived importance of prioritizing perinatal depression screening and treatment in routine practice.
Before this study, the statewide service infrastructure had been enhanced through training, instrument availability, and reimbursement to facilitate the desirable outcomes of perinatal depression screening and treatment/referral. With this preexisting service infrastructure in place, this study's findings assert that further augmentation to services is possible by altering provider importance and confidence, as suggested by motivational interviewing as an intervention model. At present, we are moving forward with the findings from this study to consider the specific ways in which motivational interviewing can serve as both a strategy to motivate providers to screen and treat/refer and provide a technique applicable to women with perinatal depression encountered in their practice.
One specific future initiative will be to partner regionally and build confidence among providers regarding service availability options by creating a more fluid connection between available support resources for women experiencing perinatal depression. We intend to move forward by defining and categorizing the multitiered interventions available (including supportive home visiting, psychoeducation, and peer support, as well as specialty mental health programs) in order to facilitate referrals based on symptoms, severity, and service preferences. Motivational interviewing simultaneously offers a framework for a brief engagement to treatment intervention that can be used by these same health providers in their community practice. Statewide trainings to augment provider confidence will also focus on these motivational interviewing skills for use with patients who are ambivalent about help seeking for perinatal depression.
As a training technique, motivational interviewing can also be used to help providers identify their own motivations for (and ambivalence about) engaging in screening and intervention, which in turn may help them motivate clients within their particular geographic regions and service settings. Ultimately, the program theory implied by motivational interviewing offers a framework from which we can address existing ambivalence within both healthcare providers and consumers, creating meaningful pathways for collaborative intervention development.
The theoretical and statistical modeling framework of our study may help address the concerns previously encountered in other widespread screening initiatives where an action step (i.e., mandatory screening) preceded a theory of change.10,11 Notably, the empirical support for motivational interviewing generated through this study makes a distinct contribution by defining the causal mechanisms through which we assert the desirable change is taking place. Articulating causal pathways enhances our ability to understand how and why particular strategies work, how they can be measured, and what is the contribution of the strategy to proximal outcomes (e.g., augmenting importance and confidence of providers) as well as ultimate outcomes (e.g., enhanced perinatal depression screening and intervention). Theoretically informing an intervention lends support to the process of change as well as the resulting outcomes, which helps us better understand breakdowns in program efficacy so that needed interventions can be adapted by altering the specific components through which we assert that change is taking place.
There are a number of limitations to this study. First, the survey data were not originally collected with the intention of statistical modeling. Inherent measurement error, such as social desirability and participant response set patterns, may have influenced the quality of the data and measurement accuracy, ultimately reducing model fit and strength. The inability to assume conditional independence is a limitation in both the measurement model and the structural model. Attention to measurement rigor and consistency across subsequent evaluations statewide is crucial to assessing the intervention model's true effect.
A second major limitation is the inability to detect differences based on provider specialization in the structural model, given the small size of specific provider specialty subgroups. For example, only 72 respondents who had ever managed (diagnosed or treated) a case of perinatal depression were pediatricians; consequently, we lacked sufficient power to consider multigroup SEM in spite of the fact that descriptive data suggested different patterns of perceptions, screening, and treatment practices for this group. An additional limitation of this and other model identification procedures is that there may be additional explanatory models of behavioral change that would be theoretically plausible or even superior if they could be empirically tested. We were, for example, unable to measure or evaluate specific learning styles or didactic techniques that may influence the retention of information and its application to practice, as we did not include such questions on the provider survey.
An additional limitation is the potential uniqueness of our sample, whether related to who ultimately responded or to state-level differences in Virginia's providers as compared with other states or countries. We consulted with the Office of Health Professions to evaluate how well our sample represented the demographic makeup of Virginia's healthcare provider workforce. However, no specific data had been collected on race, ethnicity, or gender for providers before the current biennium. Nationally, almost 70% of health providers self-report as non-Hispanic white, and approximately 71% are male.30 Our survey demographics reveal a higher percentage of women than this national norm but a similar racial composition of our overall sample. This could be accounted for in part by the selected specialties within our sampling frame, which may attract more female providers.
Similarly, we cannot be certain about what motivated respondents to participate in this study. Although response rates are relatively stable among provider groups, the overall response rate of 25% suggests that many providers' experiences are not necessarily included in study results. Because this was a voluntary survey undertaken in a public health context, we had no way to incentivize providers or mandate response. It is difficult to assess the degree to which responding providers were more or less likely to have a higher degree of motivation for screening and referring women than nonresponding providers; one assumption may be that our sample reflects providers who were already more motivated, based on their participation. The variance of responses observed within the data, however, suggests that the sample included a range of responses among all those who had managed a case of perinatal depression, ranging from those who did not formally screen or treat/refer women at all to those who regularly integrated these recommended practices into routine care. As previously described, perceived barriers to screening and treatment/referral also indicate tangible (time, reimbursement) barriers as well as acknowledgment of inadequate knowledge and skills among providers. This attests to some degree of variability within respondents' motivations and actions.
In spite of these limitations, this study reflects our best attempt to garner information on current provider practices statewide. Ultimately, we see the results of this study as having impact on our state's program and policy based on those who responded and, in doing so, allowed their experiences to inform future public health policy and practice. The authors recognize that within our assumptions there could be unintentional sampling error and self-report bias based the views of those providers who chose to respond to the survey. An examination of widespread actual practices could produce different results. Future research could be conducted to compare the reported practices contained within this survey with insurance claims data, for example, to assess the degree to which reported provider actions match with actual reimbursement claims.
Conclusions
This study offers an empirically and theoretically grounded approach to the delivery of women's health and mental health services surrounding perinatal depression. Rather than simply focusing on knowledge enhancement or practice mandates, we may be at a critical juncture to consider motivational influences (and ambivalence) that may impact healthcare providers' screening practices, recognition and identification of symptoms, and intervention and linkage to multisector community and mental health services. Simultaneously, future research to identify meaningful tiers of mental health interventions for pregnant and postpartum women with varying levels of depressive symptoms must also continue, so that women and families have access to relevant, responsive, and accessible services after identification by healthcare providers.
Healthcare, mental health, social service, and public health providers need to collaborate in the development of a responsive service infrastructure. We assert that there is a role for future professional training that integrates motivational interviewing in order to achieve this successful collaboration. Moving the program theory supported by our findings into a statewide intervention model will involve multidisciplinary trainings that strive to overcome ambivalence to screening and treatment/referral by augmenting the importance of screening and linkage to treatment by an array of health professionals, as well as bolstering confidence in the techniques, training, resources, and supports needed to effectively engage in these desirable practice behaviors. Collaborative efforts that strengthen the intersections among primary and specialty healthcare, public health, community services, mental health, and academic research institutions are essential to forward momentum in securing a healthy future for both women and infants.
Acknowledgments
The project described was supported by the Virginia Department of Health Maternal and Child Health Black Grant and CTSA Grant Number UL1TR00058 from the National Center for Advancing Translational Sciences to the Virginia Commonwealth University Center for Clinical and Translational Research, supporting the first author's KL2 award. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
We thank and acknowledge colleagues Kia J. Bentley, Pat Dattalo, and Levent Dumenci from Virginia Commonwealth University and Derek Chapman and Diane Helentjaris from the Virginia Department of Health for their helpful review and feedback.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Field T. Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behav Dev. 2010;33:1. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Segre LS. Brock RL. O'Hara MW. Gorman LL. Engeldinger J. Disseminating perinatal depression screening as a public health initiative: A train-the-trainer approach. Matern Child Health J. 2011;15:814–821. doi: 10.1007/s10995-010-0644-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists. ACOG practice bulletin number 92: Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2008;111:1001–1020. doi: 10.1097/AOG.0b013e31816fd910. [DOI] [PubMed] [Google Scholar]
- 4.Bledsoe SE. Grote NK. Treating depression during pregnancy and the postpartum: A preliminary meta-analysis. Res Soc Work Pract. 2006;16:109–120. [Google Scholar]
- 5.Boyd RC. Pearson JL. Blehar MC. Prevention and treatment of depression in pregnancy and the postpartum period—Summary of a maternal depression roundtable: A U.S. perspective. Arch Womens Ment Health. 2002;4:79–82. [Google Scholar]
- 6.Weissman MM. Recent non-medication trials of interpersonal psychotherapy for depression. Int J Neuropsychopharmacol. 2007;10:117–122. doi: 10.1017/S1461145706006936. [DOI] [PubMed] [Google Scholar]
- 7.Boyd RC. Le HN. Somberg R. Review of screening instruments for postpartum depression. Arch Womens Ment Health. 2005;8:141–153. doi: 10.1007/s00737-005-0096-6. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Preventive Services Task Force. Clinical Guidelines: Screening for depression: Recommendations and Rationale. Ann Intern Med. 2002;136:760–764. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- 9.National Research Council and Institute of Medicine. Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 10.Yonkers KA. Smith MV. Lin H. Howell HB. Shao L. Rosenheck RA. Depression screening of perinatal women: An evaluation of the Healthy Start depression initiative. Psychiatr Serv. 2009;60:322–328. doi: 10.1176/appi.ps.60.3.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kozhimannil K. Adams A. Soumerai S. Busch A. Huskamp H. New Jersey's efforts to improve postpartum depression care did not change treatment patterns for women on medicaid. Health Aff. 2011;30:293. doi: 10.1377/hlthaff.2009.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Price SK. Proctor EK. A rural perspective on perinatal depression: Prevalence, correlates, and implications for help-seeking among low-income women. J Rural Health. 2009;25:158–166. doi: 10.1111/j.1748-0361.2009.00212.x. [DOI] [PubMed] [Google Scholar]
- 13.Baker L. Cross S. Greaver L. Wei G. Lewis R. Healthy Start CORPS. Prevalence of postpartum depression in a Native American population. Matern Child Health J. 2005;9:21–25. doi: 10.1007/s10995-005-2448-2. [DOI] [PubMed] [Google Scholar]
- 14.Altshuler LL. Cohen LS. Moline ML, et al. Treatment of depression in women: A summary of the expert consensus guidelines. J Psychiatr Pract. 2001;7:185–208. doi: 10.1097/00131746-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Peindl KS. Wisner KL. Hanusa BH. Identifying depression in the first postpartum year: Guidelines for office-based screening and referral. J Affect Disord. 2004;80:37–44. doi: 10.1016/S0165-0327(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 16.Delatte R. Cao H. Meltzer-Brody S. Menard MK. Universal screening for postpartum depression: An inquiry into provider attitudes and practice. Am J Obstet Gynecol. 2009;200:e63–64. doi: 10.1016/j.ajog.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 17.Goodman J. Tyer-Viola L. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. J Womens Health. 2010;19:477–490. doi: 10.1089/jwh.2008.1352. [DOI] [PubMed] [Google Scholar]
- 18.Leddy M. Haaga D. Gray J. Schulkin J. Postpartum mental health screening and diagnosis by obstetrician-gynecologists. J Psychosom Obstet Gynecol. 2011;32:27–34. doi: 10.3109/0167482X.2010.547639. [DOI] [PubMed] [Google Scholar]
- 19.Chaudron LH. Szilagyi PG. Kitzman HJ. Wadkins HI. Conwell Y. Detection of postpartum depressive symptoms by screening at well-child visits. Pediatrics. 2004;113:551–558. doi: 10.1542/peds.113.3.551. [DOI] [PubMed] [Google Scholar]
- 20.Chaudron LH. Szilagyi PG. Campbell AT. Mounts KO. McInerny TK. Legal and ethical considerations: Risks and benefits of postpartum depression screening at well-child visits. Pediatrics. 2007;119:123–128. doi: 10.1542/peds.2006-2122. [DOI] [PubMed] [Google Scholar]
- 21.Earls MF. Committee on Psychosocial Aspects of Child and Family Health, American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126:1032–1039. doi: 10.1542/peds.2010-2348. [DOI] [PubMed] [Google Scholar]
- 22.Miller WR. Rollnick S. Motivational interviewing: Preparing people for change. 2nd. New York: Guilford Press; 2002. [Google Scholar]
- 23.Rollnick S. Miller WR. Butler CC. Motivational interviewing in health care: Helping patients change behavior. New York: Guildford Press; 2008. [Google Scholar]
- 24.Rodgers JL. The epistomology of mathematical and statistical modeling: A quiet revolution. Am Psychologist. 2010;65:1–12. doi: 10.1037/a0018326. [DOI] [PubMed] [Google Scholar]
- 25.Mulaik SA. Linear causal modeling with structural equations. Boca Raton, FL: Chapman & Hall/CRC Press; 2010. [Google Scholar]
- 26.Muthén BO. Muthén L. MPlus Version 6.1 [Software] Los Angeles, CA: Author; 2010. [Google Scholar]
- 27.Virginia Department of Health. Virginia Pregnancy Risk Assessment Monitoring System (5 UR6 DP000470-04) 2007. [Apr 25;2011 ].
- 28.Saris WE. Satorra A. van der Veld WM. Testing structural equation models or detection of misspecifications? Structural Equation Modeling. 2009;16:561–582. [Google Scholar]
- 29.Grewal R. Cote JA. Baumgartner H. Multicollinearity and measurement error in structural equation models: Implications for theory testing. Market Sci. 2004;23:519–529. [Google Scholar]
- 30.Physician facts, trends, Virginia and U.S., 2008. Richmond: Virginia Department of Health Professions Healthcare Workforce Data Center; 2010. [Google Scholar]