ABSTRACT
Purpose: To analyze weekend physiotherapy services in acute-care community hospitals across Canada. Method: Questionnaires were mailed to acute-care community hospitals (institutions with >100 inpatient beds, excluding psychiatric, mental health, paediatric, rehabilitation, tertiary, and long-term care facilities) across Canada from January to April 2010. The questionnaire collected information on patient referral criteria, staffing, workload, and compensation for weekend physiotherapy services and on the availability of other rehabilitation health professionals. Results: Of 146 community hospitals deemed eligible, 104 (71%) responded. Weekend physiotherapy was offered at 69% of hospitals across Canada, but this rate varied: ≥75% in all regions except Quebec (30%). Hospitals with a high proportion of acute-care beds were more likely to offer weekend physiotherapy services (logistic regression, p=0.021). Services differed among Saturdays, Sundays, and holidays in terms of the numbers of both physiotherapists and physiotherapy assistants working (Kruskal–Wallis, p<0.02 for each). Physiotherapists were predominantly compensated via time off in lieu. Of hospitals not offering weekend physiotherapy, 53% reported that it would benefit patients; most perceived staffing and financial barriers. Social-work services were offered on the weekend at 24% of hospitals and occupational therapy at 16%. Conclusions: Substantial regional variation exists in access to weekend physiotherapy services in acute-care community hospitals. To address the importance of this variation, research on the efficacy and cost-effectiveness of such services is required.
Key Words: rehabilitation; hospitals, community; delivery of health care; health services research
RÉSUMÉ
Objectif : Analyser les services de physiothérapie offerts durant les fins de semaine dans les hôpitaux communautaires de soins de courte durée d'un bout à l'autre du Canada. Méthode : De janvier à avril 2010, des questionnaires ont été postés aux hôpitaux communautaires de soins de courte durée (établissements comptant plus de 100 lits pour hospitalisation, excluant les lits en psychiatrie, en santé mentale, en pédiatrie, en réadaptation, les soins tertiaires et les établissements de soins prolongés) partout au Canada. Le questionnaire visait à recueillir de l'information sur les critères justifiant le renvoi en consultation, le personnel, la charge de travail et la rémunération pour des services de physiothérapie offerts les fins de semaine, et sur la disponibilité d'autres professionnels de la santé œuvrant en réadaptation. Résultats : Des 146 hôpitaux communautaires admissibles, 104 (71 %) ont répondu. Des services de physiothérapie étaient offerts les fins de semaine dans 69 % des hôpitaux au Canada, mais cette proportion varie : ≥75 % dans toutes les régions, sauf au Québec (30 %). Il était plus probable que des services de physiothérapie soient offerts les fins de semaine dans les hôpitaux qui disposent d'une forte proportion de lits en soins de courte durée (régression logistique, p=0,021). Le nombre de physiothérapeutes et d'assistants-physiothérapeutes en poste les samedis, les dimanches et les jours fériés varie, ce qui explique que les services sont différents les samedis, les dimanches et les jours fériés (Kruskal-Wallis, p<0,02 pour chaque profession). Les physiothérapeutes étaient principalement rémunérés par des congés compensatoires. Parmi les hôpitaux n'offrant pas de physiothérapie les fins de semaine, 53 % ont fait savoir que de tels services seraient profitables pour les patients, mais que le manque de personnel et les restrictions financières les empêchaient de les offrir. Des services de travailleurs sociaux étaient offerts les fins de semaine dans 24 % des hôpitaux, et des services en ergothérapie dans 16 % des hôpitaux. Conclusions : L'accès à des services de physiothérapie les fins de semaine fait l'objet de disparités régionales importantes dans les hôpitaux communautaires de soins de courte durée. La mesure de l'étendue de ces disparités pourrait être établie par des recherches sur l'efficacité et sur la rentabilité de tels services.
Mots clés : réadaptation; hôpitaux, communautaires, communauté; prestation de soins; recherche en soins de santé
Physiotherapy (PT) is recognized as an essential component of the health care team in many settings.1–3 While historically physicians and nurses have provided 24-hour, 7-day-per-week acute care, this has not been standard in service provision by physiotherapists. Frequency and intensity of PT service delivery in hospital are important because they can influence length of stay,4,5 health care spending,6 and patient satisfaction.7 However, evidence on the efficacy and cost-effectiveness of weekend physiotherapy (WPT) is sparse and equivocal,8–10 largely because there have been few well-designed studies.11
Variation in the availability of WPT service has been observed around the world.12,13 In Canada, there are only limited data on availability of WPT service, particularly in community hospital settings.6,14 In the late 1990s, McAuley first documented provision of WPT in Canada, in a study encompassing nine similarly sized acute-care hospitals from four provinces.6 The author presented workload variables for Saturdays, Sundays, and holidays; compiled the criteria used by each site to refer patients to WPT care; and showed that 30% of the weekend caseload might be appropriate for service by physical therapy assistants. Soon after, a survey of 26 facilities14 (general hospitals, rehabilitation hospitals, and long-term care facilities) in the Greater Toronto Area included similar workload and staffing variables for WPT services but stratified the results by institution affiliation (academic vs. non-academic). Significant differences were found in some workload variables by institution affiliation.14 The authors cautioned that these findings may be less applicable to communities where academic and non-academic facilities are not found in the same geographic area.14
Recently, a prospective workload assessment of physiotherapists working on weekends was conducted in three Toronto-area tertiary-care hospitals.15 The authors found variation among these hospitals in terms of weekend and evening PT service delivery, the ability of physiotherapists working on weekends to share the workload, and the proportion of physical therapists completing unpaid overtime. This variation appeared to be related to the institutions' management structures (departmental vs. programme management).15 A survey of tertiary-care hospitals across Canada16 found a 10% higher rate of provision of WPT than a survey of a broader range of hospital types performed a decade earlier.14
Since earlier findings suggest that differences in access to weekend and evening service delivery are likely between academic and non-academic facilities,13,14 investigations into facilities outside the tertiary setting should be conducted. Furthermore, we know of no current national review of criteria used to refer patients for WPT care in community hospitals, no recent estimate of the staffing of physiotherapist assistants in community hospitals, and no surveys of weekend staffing of other rehabilitation health professionals in the acute-care setting.
The purpose of our study was to analyze WPT services in acute-care community hospitals across Canada. Our specific objectives were (1) to review WPT service with respect to patient referral criteria, staffing, workload, scope of services, and the weekend availability of other rehabilitation health professions; and (2) to assess the availability of WPT services in community hospitals across provinces and territories in Canada.
METHODS
Study design
We conducted a survey from January to April 2010 to gather information on PT services available in community hospitals across Canada. Questionnaires were administered by mail, using a modified Dillman approach.17 Approval for this study was obtained from the Ethics Review Board at the University of Toronto.
Eligibility criteria
All community hospitals in Canada were considered for inclusion in this study. A community hospital was operationally defined as an institution with a minimum of 100 in-patient beds, offering acute care and not considered a tertiary-care centre. To ensure consistency (and prevent overlap) with a recent survey of WPT in tertiary-care centres,16 a tertiary-care centre was defined as having both an affiliation with a university medical school in research and teaching capacities and having at least one intensive-care unit. Hospitals offering only psychiatric, mental-health, paediatric, rehabilitation, or long-term care were excluded, as our focus in this study was on adult acute care. The minimum of 100 in-patient beds was set to improve homogeneity of the surveyed institutions in terms of their service requirements.
Sample
A total of 271 potential community hospitals were identified, using the Canadian Health Facilities Directory (2005 ed.).18 Eligibility criteria were confirmed by consulting the hospitals' official Web sites and/or the appropriate regional health authorities. Address changes and site closures were also identified via returned mail and confirmed via official hospital Web sites.
Questionnaire
The questionnaire was modelled on a telephone-administered questionnaire from a recent study describing WPT services in tertiary-care institutions across Canada.16 Modifications were made to tailor questions to the community hospital setting and to add new items addressing the availability of other rehabilitation health services—in particular, occupational therapy (OT), speech-language pathology (SLP), and social work (SW).
Section A of the questionnaire (see Appendix online) consisted of 14 items related to PT organizational structure at the institution, facility demographic information (e.g., total number of hospital beds, number of physiotherapists and physiotherapist assistants employed at each facility), hospital services available, and availability of other rehabilitation health professionals during the week and on the weekend. PT organizational structures were defined on the questionnaire as departmentalized (a central PT or rehabilitation department manages PT matters), programme management (physiotherapists work directly for a particular service rather than for a PT department), or matrix (combination of the above). Facilities not currently offering WPT care were asked to complete items relating to the perceived need for and barriers to WPT care. Section B consisted of 20 items addressing WPT service, including staffing patterns (e.g., numbers of physiotherapists and physiotherapist assistants, average working hours); referral criteria for WPT services; and workload details (e.g., hours worked by physiotherapists and physiotherapist assistants, numbers of patients seen) and responsibilities of the WPT staff.
The questionnaire was pilot-tested by six physiotherapists working in community hospitals in Ontario. Based on their comments, minor formatting and wording changes were made to improve clarity before the questionnaires were mailed to hospital sites. The questionnaire and accompanying documents were translated from English to French by a Francophone bilingual physiotherapist.
Mailing procedure
Each hospital was mailed a survey package containing a cover letter, questionnaire, and refusal card in English and a postage-paid self-addressed envelope; hospitals in the city of Ottawa and the provinces of Quebec and New Brunswick were mailed packages in both English and French. Survey packages were addressed to “Professional Practice Leader / Manager of Physical Therapy / Physiotherapy.” Respondents were asked to coordinate with any other managers of PT services at their facility to compile answers to the questionnaire items. Each questionnaire was labelled with a unique identifier to enable tracking of facility responses while maintaining confidentiality. All hospitals were asked to complete Section A (descriptive hospital information); those offering PT services on the weekend were also asked to complete Section B (items on WPT service).
After 2 weeks, a reminder letter was mailed to each hospital; 2 weeks after the reminder letter, hospitals that had not yet replied were sent an additional package containing a reminder letter and a second copy of the questionnaire. Consent to participate in the study was implied by the return of completed surveys. Investigators contacted participants via e-mail if further clarification of responses was required.
Data analysis
Data analysis was conducted using the Statistical Package for Social Sciences, version 18.0 (SPSS Inc., Chicago, IL). Responses in French were translated into English and checked by two of the investigators at the data-entry stage. If a response to a numerical item was given as a range, the midpoint of the range was entered and used in subsequent analyses (e.g., “10–15” was entered as “12.5”), although the original range was noted in the database as well.
To assess WPT services, descriptive statistics (e.g., mean, median, standard deviation, range) were calculated for variables describing staffing and workload details. Comparisons of variables among weekend days (Saturdays, Sundays, and holidays) were performed using Kruskal–Wallis tests (for non-normal continuous or integer variables) or chi-square tests (for categorical data). Post-hoc pair-wise comparisons between days were made using Mann–Whitney U tests. Comparisons of continuous variables between sites that offered WPT service and sites that did not were performed by fitting univariate logistic regression equations. Responses to open-ended questions (e.g., referral criteria) were grouped into categories for descriptive analysis. Significance was set at p<0.05.
To describe potential variability in service delivery among geographic regions, the percentage of eligible responding community hospitals offering WPT services in each region was tabulated. Because of the small numbers of hospitals in some provinces and territories, hospitals were pooled into geographic regions.
RESULTS
Response
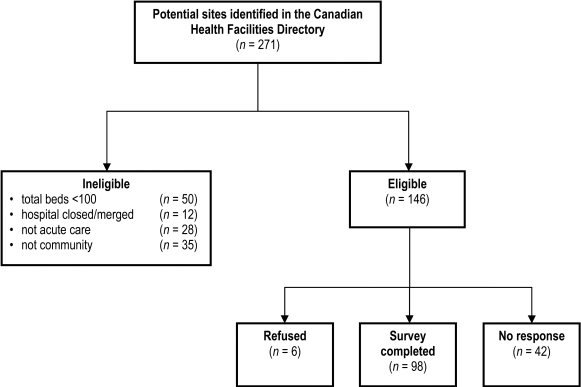
Of the 146 sites deemed to be eligible acute-care community hospitals, 98 (67%) completed and returned the questionnaire; an additional 6 eligible sites responded but declined to participate (see Figure 1), for an overall response rate of 71% (104/146). Responses to our survey were received from all provinces and territories except the Yukon and Nunavut, where no eligible facilities were identified. Representation of the sample by region is presented in Table 1.
Figure 1.
Site identification and response.
Table 1.
Community Hospitals Offering Weekend Physiotherapy Service by Region.
| Region | No. (%) of hospitals |
% of hospitals offering WPT service |
|---|---|---|
| BC | 15 (15.3) | 93.3 |
| AB, SK, MB, NT | 16 (16.3) | 75.0 |
| ON | 30 (30.6) | 86.7 |
| QC | 27 (27.6) | 29.6 |
| NB, NS, PE, NL | 10 (10.2) | 80.0 |
| Total | 98 (100) | 69.4 |
WPT=weekend physiotherapy; BC=British Columbia; AB=Alberta; SK=Saskatchewan MB=Manitoba; NT=Northwest Territories; ON=Ontario; QC=Quebec; NB=New Brunswick; NS=Nova Scotia; PE=Prince Edward Island; NL=Newfoundland.
Sample
Community hospitals included in the study ranged in size from 100 to 852 in-patient beds (see Table 2); 51% of sites (50) had fewer than 220 beds. These sites ranged in numbers of acute-care in-patient beds from 14 to 800, but for 82% of hospitals (80), at least one-half of in-patient beds were listed as acute care. The majority of sites (67%, 66) used departmental management of PT services (see Table 2).
Table 2.
General Characteristics of Participating Hospitals (n=98*)
| Variable | Mean (SD)* | Median | Range |
|---|---|---|---|
| Beds | |||
| Total number of hospital beds | 252.4 (144.8) | 217.5 | 100–852 |
| Proportion of total beds that are acute-care† | 0.70 (0.2) | 0.72 | 0.05–1 |
| Physiotherapy staff | |||
| Total no. of PTs | 15.0 (10.4) | 12.0 | 1–45 |
| No. of full-time PTs | 9.1 (6.2) | 8.0 | 0–32 |
| No. of part-time PTs | 3.9 (4.2) | 2.0 | 0–21 |
| No. of casual PTs | 2.3 (3.3) | 1.0 | 0–19 |
| No. of full-time PTAs† | 3.8 (3.6) | 3.0 | 0–18 |
| No. of part-time PTAs† | 1.8 (2.1) | 1.0 | 0–11 |
| No. of casual PTAs‡ | 1.6 (2.4) | 1.0 | 0–17 |
| Management structure; no. (%) | |||
| Departmentalized | 66 (67.3) | — | — |
| Programme management | 9 (9.2) | — | — |
| Matrix | 23 (23.5) | — | — |
Unless otherwise specified.
n=96.
n=93.
PT=physiotherapist; PTA=physiotherapist assistant (includes other assistance staff, such as physical therapist assistant / occupational therapy assistant [PTA/OTA], thérapeute en réadaptation physique [Quebec], and kinesiologist).
All 98 hospitals employed physiotherapists (mean 15, range 1–45), and 95% (93) also employed physiotherapist assistants (and other related support staff, such as physiotherapist assistant / occupational therapist assistant [PTA/OTA], thérapeute en réadaptation physique [TRP] in Quebec, and kinesiologist) in their full (weekday and weekend) PT service (see Table 2). Staffing models included a combination of full-time, part-time, and casual/contract physiotherapists and physiotherapist assistants (see Table 2).
Seventeen percent (17) of community hospitals that completed the survey offered regularly scheduled PT care outside of normal business hours during the week (beyond 8 a.m.–4 p.m. or 9 a.m.–5 p.m.). At sites offering this service, an average of 2 (SD 1.2) hours was offered each weekday (range 0.4–5.0 h/d).
Weekend physiotherapy service
Physiotherapy service was offered on at least one weekend day (Saturdays, Sundays, or holidays) at 69% of community hospitals (68; see Table 2). This proportion varied by region: at least three-quarters of community hospitals reported offering WPT care in most regions, but the proportion in Quebec was only 30% (see Table 1). Among the 68 hospitals offering some weekend care, PT was offered on Saturdays at 67 sites (99%), on Sundays at 55 sites (81%), and on holidays at 54 sites (79%).
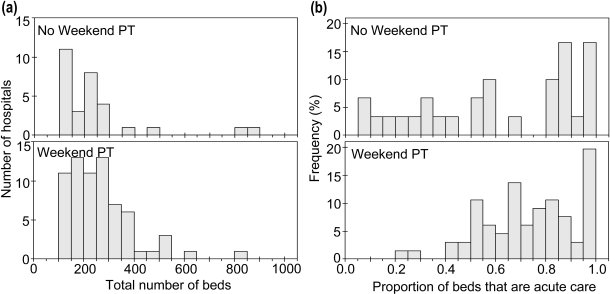
No difference in total bed numbers was found between hospitals that offered WPT care and those that did not (see Figure 2a, logistic regression, β=0.002, p=0.346). However, community hospitals offering WPT care had a significantly higher proportion of acute-care beds (mean 0.74 [SD 0.19]; n=66) than those where WPT was not offered (mean 0.61 [SD 0.31], n=30; logistic regression, β=0.021, p=0.025; see Figure 2b). Because our sample was small, it was not possible to test the hypothesis that availability of weekend care differed by PT management structure.
Figure 2.
Community hospitals that offer weekend physiotherapy (lower panels) or do not (upper panels), distributed according to (a) total number of beds and (b) proportion of beds designated as acute care (bars are shown as % of the hospitals in each panel).
Many criteria were used by community hospitals to establish eligibility for WPT service (see Table 3). The most common groups identified for placement on the weekend list were patients with acute cardiorespiratory issues, new referrals, and patients requiring PT to augment or accelerate discharge from hospital. Patients who had recently had surgery (e.g., following unspecified acute orthopaedic surgery or total hip or knee arthroplasties) were also commonly seen by physiotherapists on the weekend. The 11 most common criteria were each used by at least 20% of hospitals; the remaining criteria were less commonly used (see Table 3).
Table 3.
Common Criteria Used to Identify Patients to Receive Weekend Physiotherapy Service (n=98)
| Common referral criteria* | No. (%) of hospitals using criterion |
|---|---|
| Patients with acute cardiorespiratory issues | 55 (80.9) |
| New referrals | 47 (69.1) |
| Patients requiring PT to augment or accelerate discharge over the weekend or on Monday | 47 (69.1) |
| Patients who underwent acute orthopaedic surgery | 37 (54.4) |
| Patients who underwent THA/TKA | 36 (52.9) |
| Postoperative patients (unspecified surgery) | 32 (47.1) |
| Patients requiring PT to prevent deterioration | 24 (35.3) |
| Patients currently on a care pathway | 22 (32.4) |
| Patients with a neurological condition | 17 (25.0) |
| Patients who underwent major abdominal surgery | 14 (20.6) |
| Patients with burns | 14 (20.6) |
Note: Also reported as identified for WPT were patients who underwent thoracic surgery; were in the intensive care unit; were ventilated; were in the Emergency department / had multiple traumas; underwent heart surgery; underwent breast surgery; underwent spinal surgery; underwent vascular surgery; underwent shoulder surgery; underwent head and/or neck surgery; presented with acute low back pain; sustained frostbite; sustained a hip fracture; sustained a myocardial infarction; had cystic fibrosis; had mobility issues; were using a continuous passive motion machine; had been identified by the weekend physiotherapist; had shown rapid improvement with physiotherapy.
Categories are not mutually exclusive.
PT=physiotherapy; THA=total hip arthroplasty; TKA=total knee arthroplasty.
Lower-priority patients were added to the weekend list if time permitted at 76% of responding facilities (52); 43 sites indicated that they had exclusion criteria to distinguish those patients not eligible for WPT service. Commonly excluded were patients requiring general mobility who could be seen by another staff member, patients awaiting placement in a long-term care facility, patients who could clear chest secretions independently, and patients who were medically unstable.
Staffing and workload
The majority of sites (63%; 42) employed a single physiotherapist on Saturdays (mean 1.6; range 0–6; see Table 4). Physiotherapists each worked an average of 6.2 hours on Saturdays; shifts of 7.0–8.0 hours (37 sites) were three times as common as shifts of 4.0–5.0 hours (13 sites). The number of physiotherapists working on Saturdays was significantly different from the number working on holidays (Mann–Whitney U test, p=0.010). The number working on Saturdays was also different from the number working on Sundays, but this difference was not significant (Mann–Whitney U test, p=0.023; once a Bonferroni correction was applied, the difference became non-significant). No difference among days was found in the number of hours worked per physiotherapist (Kruskal–Wallis test, p=0.186).
Table 4.
Staffing Patterns of Weekend Physiotherapy Services at Community Hospitals
| Variable | Saturday |
Sunday |
Holiday |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean (SD) |
Median | Range | No. of sites responding |
Mean (SD) |
Median | Range | No. of sites responding |
Mean (SD) |
Median | Range | No. of sites responding |
|||
| No. of PTs working* | 1.6 (1.0)† | 1 | 0.0–6.0 | 68 | 1.3 (1.2) | 1 | 0.0–6.0 | 68 | 1.2 (1.1) | 1 | 0.0–6.0 | 68 | |||
| No. of PTAs working‡ | 0.9 (0.8)§ | 1 | 0.0–4.0 | 68 | 0.8 (0.8) | 1 | 0.0–4.0 | 67 | 0.6 (0.8) | 0 | 0.0–4.0 | 68 | |||
| No. of hours worked per PT |
6.2 (1.9) | 7.2 | 0.0–9.0 | 67 | 5.1 (3.1) | 7.0 | 0.0–9.0 | 67 | 4.9 (3.2) | 6.7 | 0.0–9.0 | 65 | |||
| No. of hours worked per PTA¶ |
4.8 (3.4)§ | 7.0 | 0.0–10.5 | 68 | 3.9 (3.6) | 4.0 | 0.0–9.0 | 67 | 3.0 (3.5) | 0.0 | 0.0–9.0 | 68 | |||
Distributions significantly different between days (Kruskal–Wallis test, p=0.020).
Post-hoc pair-wise comparisons show distributions on Saturdays significantly different from on holidays (Mann–Whitney U test, p=0.010).
Distributions significantly different between days (Kruskal–Wallis test, p=0.011).
Post-hoc pair-wise comparisons show distributions on Saturdays significantly different from on holidays (Mann–Whitney U test, p=0.002).
Distributions significantly different between days (Kruskal–Wallis test, p=0.009).
PT=physiotherapist; PTA=physiotherapist assistant.
Of the 68 sites offering WPT service, 48 (71%) employed physiotherapist assistants (including related support staff such as PTA/OTA, TRP [in Quebec], and kinesiologists) for some part of weekend service. However, 18 sites indicated that they did not employ physiotherapist assistants for their PT service on Saturdays; 16 sites did not do so on Sundays, and 24 did not do so on holidays. Significant differences were found between Saturdays and holidays in both the number of physiotherapist assistants working each day and the number of hours they worked (see Table 4; Mann–Whitney U test, p=0.002 for each).
In hospitals that offered PT care on specific weekend days, the number of patients typically seen was very similar across days (for Saturday, Sunday, and holiday, respectively, median 14.5, 14.5, 13.5 patients; at 48, 40, 37 sites where this information was available; range 1–39 patients for each day). The distribution of the number of patients seen did not differ between days (Kruskal–Wallis test, p=0.747).
Nature of weekend physiotherapy service and compensation
The reported clinical responsibilities of the weekend physiotherapist at community hospitals included assessment and treatment of new referrals (99%; 67 sites), ongoing treatment (97%; 66), documentation (93%; 63), workload statistics (91%; 62), and discharge assessment (90%; 61). At all 48 sites that used physiotherapist assistants for weekend care, physiotherapist assistants were involved in providing hands-on assistance to the weekend physiotherapists. Other reported clinical responsibilities of weekend physiotherapist assistants included aiding with patient exercise programmes (73%; 35), carrying out treatment plans other than exercise programmes (73%; 35), and documentation (58%; 28).
The majority of sites offered time off in lieu (i.e., during the week) as compensation for hours worked on the WPT service (57%; 39). Other options reported were compensation included within staff salary (40%; 27), overtime pay (35%; 24), and staff's choice of overtime or time in lieu (25%; 17). Many sites (68%; 46) offered more than one of these options.
Availability of rehabilitation professions
The services of the three rehabilitation health professions mentioned explicitly in our questionnaire (OT, SW, and SLP) were offered on weekdays at the large majority of responding community hospitals (99%, 97%, and 87%, respectively). On weekends, however, this was not the case. Weekend SW service was most commonly available (24% of sites; 24); weekend OT was available at 16% of sites (16), and weekend SLP at 2% of sites (2). Sites that did not offer weekend PT also did not offer weekend OT or SLP, but four sites that did not offer weekend PT did offer weekend SW. Other services also reported to be offered on weekends included pharmacy (8), respiratory therapy (11), and dietetics/nutrition (4).
Attitudes toward weekend care
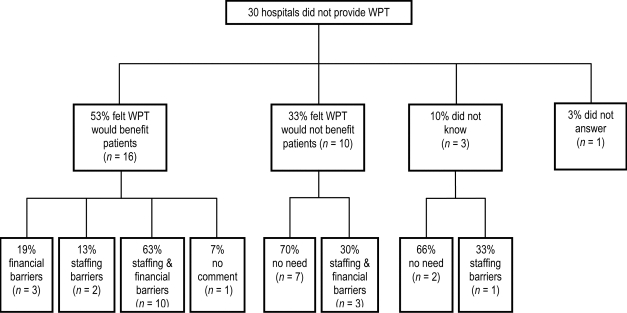
Of the 30 respondents whose hospitals did not provide WPT service, 53% (16) said they felt WPT would benefit patients, 33% (10) thought it would not, and 10% (3) said they did not know (see Figure 3). A few respondents commented on the types of patients who would benefit most from WPT care: older adults (4), patients who have recently had surgery (3), and those with acute chest conditions (2) were specifically identified.
Figure 3.
Opinions on two issues: 1) the potential benefit of weekend physiotherapy (WPT) service and 2) perceived barriers to service indicated by hospitals that do not currently provide WPT service.
Of the 16 respondents who said they believed WPT services would benefit patients, the majority (62%; 10) reported both financial and staffing barriers to offering weekend service. Two commented that a multidisciplinary team would be required on the weekend for care to be effective, creating additional staff costs. Of the 10 respondents who did not feel that WPT would not benefit patients, 70% (7) said they had no need for WPT services; 3 of these indicated that their patients are primarily older adults and that “they need the break.”
DISCUSSION
To our knowledge, this is the largest survey to date of WPT service in Canada and the first to target acute-care community hospitals. Our purpose was to review WPT care in community hospitals in terms of availability, patient selection, staffing, workload, scope of services, and availability of other rehabilitation health professions, as well as to document regional differences. We did not attempt to investigate the effects of frequency and intensity of PT service delivery on patient or hospital outcome measures, although this topic needs further investigation.
We found that WPT care was available in almost 70% of acute-care community hospitals across Canada at the time of the survey (January–April 2010). This is a lower proportion than recently found for tertiary-care centres across Canada (97% of 36)16 and is also lower than that found by a survey of Toronto-area hospitals (a mix of hospital types, 26) in the late 1990s (88%).14 Because our response rate was high, this estimate is likely accurate for community hospitals of the type targeted in our survey. We do note some heterogeneity within this group of community hospitals: we observed variation between hospitals in the proportion of hospital beds designated as acute care and found that the availability of WPT care was related to the proportion of acute-care beds.
Our survey uncovered regional variation in the availability of WPT services, particularly between Quebec and the other regions of Canada included in the sample. Only about 30% of community hospitals in Quebec offered WPT services, whereas the region with the next lowest availability (combining Alberta, Saskatchewan, Manitoba, and the Northwest Territories), offered these services at 75% of its sites. It should be noted that there was a lower response rate from Quebec (55% of eligible sites completed the questionnaire, vs. >70% in other regions), which may have affected the results. It is not surprising to find variations between provinces in how services are managed, funded, and/or staffed, since health care services are administered provincially. We note that Quebec has one of the lowest health care spending rates per capita ($4,891).19 However, British Columbia—the next lowest province in terms of per capita health care spending ($5,254)19—reported the highest regional availability of WPT service in community hospitals. Further investigation into provincial service delivery is required to determine the reasons for regional variation.
We found a lower average number of physiotherapists working on weekend or holiday days (means 1.2–1.6) than previously reported at tertiary sites across Canada (means 2.6–3.0).16 As tertiary-care centres tend to be larger facilities, this difference in staffing may be largely due to a difference in the total number of patients requiring care. The numbers of physiotherapists working on weekend days in this study are comparable to those at community sites sampled by Heck and colleagues,14 where both bed numbers and total number of physiotherapists were smaller than in academic centres. The lower numbers of physiotherapists available on each weekend day at community hospitals may also reflect a smaller number of intensive-care unit (ICU) beds as well as a lower average acuity of patient condition at community hospitals relative to tertiary centres, both of which may lower demand for WPT services, as Heck and colleagues suggested.14
We found that among community hospitals, the most common criteria for referring patients to WPT were acute cardiorespiratory issues, new referrals, and requiring PT to augment or accelerate discharge from hospital. Previous studies of WPT services in tertiary-care hospitals have reported similar referral criteria.6,16 Similar criteria have also been identified in a pooled sample of academic and community hospitals.14 Although the most common criteria are ranked slightly differently by tertiary and community facilities, the indications for WPT service in both facility types cover similar diagnostic categories. As suggested by Campbell and colleagues with respect to tertiary centres,16 criteria used less commonly among community hospitals to refer patients to weekend care may reflect the sub-specialties of particular hospitals and the patient conditions commonly seen in each facility. It is interesting to note that among hospitals not currently offering WPT services, we found varying opinions as to whether particular patient groups (e.g., older adults) required weekend service.
The majority of hospitals that provided WPT service offered time off in lieu during the week as compensation for PT staff working on this service. A survey of Toronto-area hospitals produced similar findings.14 At facilities where weekend care is provided at the expense of weekday care (i.e., therapists away on their “lieu days” are not replaced during the week, and the caseload is spread among the remaining therapists present), overall quality of care may suffer. At facilities where full service is provided 7 days a week, staff schedules and communication tools should be constructed to maximize continuity of patient care.
We believe our survey provides the first description of the availability of other rehabilitation health professional services on weekends and holidays in Canada. Social work was most commonly offered (24% of sites), followed by OT (16%). Our findings differ from those of Hooper and Dijkers,20 who found both OT and SLP to be more commonly available on the weekend (51% and 24%, respectively, on Saturdays and/or Sundays) than SW (14%) in rehabilitation centres in the United States. Several surveyed sites that do not currently offer WPT services reported that a multidisciplinary team would be required to provide effective WPT care. Further investigation into the most appropriate composition of the weekend multidisciplinary team is required.
Our study has several limitations. First, because there is no central, comprehensive list of hospitals and their services in Canada, it is possible that some acute-care community hospitals were not sampled if they were not listed in the 2005 version of the Canadian Health Facilities Directory. However, as we were able to identify hospital closures, mergers, and address changes through mail responses and online information, we do not expect that this would have affected our sampling substantially. Second, we expect that had smaller community hospitals (i.e., with <100 in-patient beds) been included in the survey, the percentage of sites offering WPT care would have been smaller, on the assumption that patients with more serious conditions (and thus more need for high-frequency PT care) would tend to be redirected from these smaller sites to larger, more specialized centres. Given our high response rate, it is likely that we have sampled the majority of facilities within our definition of acute-care community hospitals and that the data presented here are a balanced representation of WPT services in these facilities. Third, because we used a self-report instrument, we were not able to verify the accuracy of participant responses; however, in cases where answers were unclear or incomplete on key issues such as number of beds, number of acute-care beds, and hospital type (community/tertiary), respondents were contacted via e-mail for clarification, if consent for contact had been provided. We were able to obtain all bed numbers, except for the number of acute-care beds in two hospitals, and we were able to obtain hospital types from all respondents.
CONCLUSIONS
Our study provides the first national assessment of WPT care in acute-care community hospitals in Canada and the first comprehensive indication that regional variations exist. Across the country, WPT care is less commonly offered, and tends to be offered by fewer physiotherapists per weekend day, in community hospitals than in tertiary-care centres. However, community and tertiary centres use quite similar referral criteria for weekend care. A small majority of acute-care community hospitals not currently offering WPT believed that such care would benefit patients, but staffing and financial factors are perceived as barriers.
Future studies should focus on the efficacy of WPT services in specific patient groups, using multiple outcome measures, including patient outcomes (e.g., functional goal attainment), cost per patient, patient and clinician satisfaction, and the need for and composition of a multidisciplinary team on weekends. In addition, staffing and compensation models for WPT care may affect both continuity and quality of patient care, and should therefore be studied further. As emergency and trauma care is an emerging role for physiotherapists, one that naturally encompasses evenings and weekends, future investigation into weekend staffing models should include this service. Research into these new areas would be of assistance in making decisions for funding effective care in different settings and would inform the appropriate harmonization of care nationally.
KEY MESSAGES
What is already known on this topic
Some community hospitals across Canada provide weekend physiotherapy (WPT) services. One previous study, published more than a decade ago, described provision of WPT services in academic health science centres and community hospitals. The most recent study describing WPT services investigated tertiary facilities throughout Canada via a telephone-administered questionnaire. No studies have investigated the provision of WPT services in community hospitals at a national level.
What this study adds
To our knowledge, this is the first survey conducted across Canada that describes the provision of WPT services in community hospitals. The results of our survey have enabled us to comment on similarities and differences in WPT service provision between acute-care community and tertiary-care facilities. Our study also adds information on perceived barriers to WPT service provision, presence of other rehabilitation health services over weekends, and regional variations in provision of WPT services.
Physiotherapy Canada 2012; 64(2);178–187; doi:10.3138/ptc.2011-19
REFERENCES
- 1.Fagevik Olsén M, Hahn I, Nordgren S, et al. Randomized controlled trial of prophylactic chest physiotherapy in major abdominal surgery. Br J Surg. 1997;84(11):1535–8. doi: 10.1111/j.1365-2168.1997.02828.x. http://dx.doi.org/10.1002/bjs.1800841111. Medline:9393272. [DOI] [PubMed] [Google Scholar]
- 2.Nunn A, Chan A, Marks R, et al. The impact of reduction of physiotherapy service for patients in an acute hospital [abstract] Physiother Can. 1994;46(suppl 2):161. [Google Scholar]
- 3.Knight LA, Thornton HA, Turner-Stokes L. Management of neurogenic heterotopic ossification: three case histories to illustrate the role of physiotherapy. Physiotherapy. 2003;89(8):471–7. http://dx.doi.org/10.1016/S0031-9406(05)60004-1. [Google Scholar]
- 4.Hughes K, Kuffner L, Dean B. Effect of weekend physical therapy treatment on postoperative length of stay following total hip and total knee arthroplasty. Physiother Can. 1993;45(4):245–9. Medline:10130908. [PubMed] [Google Scholar]
- 5.Pendleton AM, Cannada LK, Guerrero-Bejarano M. Factors affecting length of stay after isolated femoral shaft fractures. J Trauma. 2007;62(3):697–700. doi: 10.1097/01.ta.0000197656.82550.39. http://dx.doi.org/10.1097/01.ta.0000197656.82550.39. Medline:17414350. [DOI] [PubMed] [Google Scholar]
- 6.McAuley C. Evidence-based care: determining the appropriateness of weekend physiotherapy services in an acute care tertiary hospital. Physiother Can. 1999;51:126–32. [Google Scholar]
- 7.van der Peijl ID, Vliet Vlieland TP, Versteegh MI, et al. Exercise therapy after coronary artery bypass graft surgery: a randomized comparison of a high and low frequency exercise therapy program. Ann Thorac Surg. 2004;77(5):1535–41. doi: 10.1016/j.athoracsur.2003.10.091. http://dx.doi.org/10.1016/j.athoracsur.2003.10.091. Medline:15111138. [DOI] [PubMed] [Google Scholar]
- 8.Holden MK, Daniele CA. Comparison of seven- and five-day physical therapy coverage in patients with acute orthopedic disorders. Phys Ther. 1987;67(8):1240–6. doi: 10.1093/ptj/67.8.1240. Medline:3112811. [DOI] [PubMed] [Google Scholar]
- 9.Lang CE. Comparison of 6- and 7-day physical therapy coverage on length of stay and discharge outcome for individuals with total hip and knee arthroplasty. J Orthop Sports Phys Ther. 1998;28(1):15–22. doi: 10.2519/jospt.1998.28.1.15. Medline:9653686. [DOI] [PubMed] [Google Scholar]
- 10.David C, Price N, Price T, et al. Impact of weekend physiotherapy delivery on the throughput of rheumatology inpatients: feasibility study. Physiotherapy. 2003;89(1):25–9. http://dx.doi.org/10.1016/S0031-9406(05)60666-9. [Google Scholar]
- 11.Brusco NK, Paratz J. The effect of additional physiotherapy to hospital inpatients outside of regular business hours: a systematic review. Physiother Theory Pract. 2006;22(6):291–307. doi: 10.1080/09593980601023754. http://dx.doi.org/10.1080/09593980601023754. Medline:17166820. [DOI] [PubMed] [Google Scholar]
- 12.Ntoumenopoulos G, Greenwood KM. Variation in the provision of cardiothoracic physiotherapy in Australian hospitals. Aust J Physiother. 1991;37:29–36. doi: 10.1016/S0004-9514(14)60532-8. [DOI] [PubMed] [Google Scholar]
- 13.Norrenberg M, Vincent JL European Society of Intensive Care Medicine. A profile of European intensive care unit physiotherapists. Intensive Care Med. 2000;26(7):988–94. doi: 10.1007/s001340051292. http://dx.doi.org/10.1007/s001340051292. Medline:10990117. [DOI] [PubMed] [Google Scholar]
- 14.Heck CS, Newton J, Chan A. Weekend physiotherapy service provision: a survey of Toronto area hospitals. Physiother Can. 2001;53:288–97. [Google Scholar]
- 15.Hill K, Brooks D. A description of weekend physiotherapy services in three tertiary hospitals in the greater Toronto area. Physiother Can. 2010;62(2):155–62. doi: 10.3138/physio.62.2.155. http://dx.doi.org/10.3138/physio.62.2.155. Medline:21359048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell L, Bunston R, Colangelo S, et al. The provision of weekend physiotherapy services in tertiary-care hospitals in Canada. Physiother Can. 2010;62(4):347–54. doi: 10.3138/physio.62.4.347. http://dx.doi.org/10.3138/physio.62.4.347. Medline:21886374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dillman D. Mail and internet surveys: the tailored design method. 2nd ed. New York: Wiley; 2000. [Google Scholar]
- 18.Canadian Medical Association. Canadian health facilities directory. 7th ed. Don Mills (ON): Southam Information Products; 2005. [Google Scholar]
- 19.Canadian Institute for Health Information. National health expenditure trends, 1975 to 2009. Ottawa: The Institutes; 2009. [Google Scholar]
- 20.Hooper PJ, Dijkers M. Weekend therapy in rehab hospitals: a survey of costs and benefits. Clin Management. 1987;7(1):16–21. [Google Scholar]