Abstract
We detected two cases of right atrial angiosarcoma that had a similar appearance on imaging studies. Although the surgical findings were similar for the two patients, one had a clear resection margin, while the other had tumor cells in the resection margin on frozen biopsy. We suggest that preoperative data on magnetic resonance imaging and computed tomography in patients with angiosarcomas may not predict the exact extent of surgical resection or prognostic outcomes.
Keywords: Heart neoplasms, Malignant tumor, Hemangiosarcoma
CASE REPORTS
1) Case 1
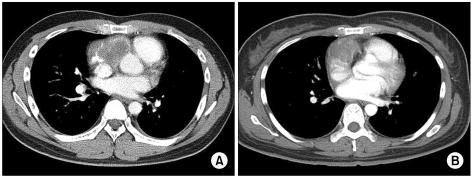
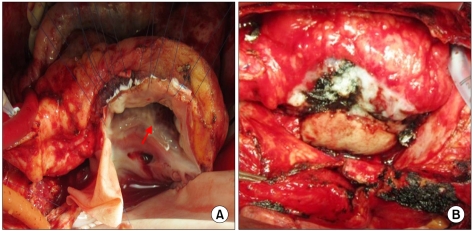
A 31-year-old previous healthy male visited a local emergency center because of dyspnea and left chest discomfort. A chest X-ray detected cardiomegaly and bilateral pleural effusion. A transthoracic echocardiogram (TTE) was performed and detected an impending cardiac tamponade and right atrial (RA) mass. Although the patient underwent pericardiocentesis, the dyspnea did not improve. For further evaluation of the RA mass, magnetic resonance imaging (MRI), computed tomography (CT) (Fig. 1A), and tissue biopsy were performed; the mass proved to be an angiosarcoma on tissue biopsy. The patient was then transferred to our hospital for a second opinion, and we planned to perform a surgical resection and adjuvant chemotherapy. The surgery included standard median sternotomy and selective cannulation of the right femoral artery, right femoral vein, and superior vena cava (SVC). Moderate hypothermic cardiopulmonary bypass at an esophageal temperature of 27℃ was performed. There was a large mass (6×5 cm) on the RA, SVC, inferior vena cava (IVC), and atrioventricular groove. The RA, SVC, IVC, and the angiosarcoma were excised. During surgery the leaflet of the tricuspid anterior and part of the posterior leaflet were injured, so we closed the annulus portion of the injured leaflet using interrupted sutures. No metastatic cancer cells were seen on the resection margins on frozen biopsy. The RA, SVC, and IVC were reconstructed using bovine pericardium (Fig. 2). The RA mass proved to be an angiosarcoma and the resection margin was clear on permanent pathology.
Fig. 1.
Preoperative computed tomography (CT) findings. (A) The CT findings of the case 1 patient. (B) The CT findings of the case 2 patient.
Fig. 2.
Intraoperative findings of the case 1 patient. (A) After we excised the tumor including the right atrial (RA), superior vena cava (SVC), inferior vena cava (IVC), and atrioventricular groove, the red arrow indicates the annulus portion of the injured leaflet using interrupted sutures. (B) This picture shows that the RA, SVC, and IVC were reconstructed using bovine pericardium.
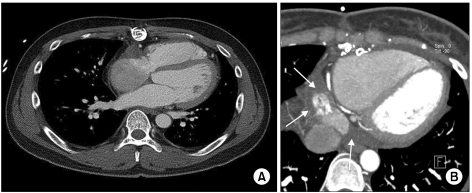
The postoperative course was uneventful. The follow-up TTE obtained on the seventh postoperative day showed no remaining mass. The patient was discharged on the eighth postoperative day and underwent adjuvant chemotherapy with paclitaxel. The patient has been doing well five months after being discharged from the hospital (Fig. 3A).
Fig. 3.
Computed tomography (CT) findings obtained three months following surgery. (A) The CT findings of the case 1 patient. There were no metastatic findings. (B) The CT findings of the case 2 patient. There were ill-defined, lobulating, heterogeneously enhancing mass lesions in the right atrial and extending into the pericardial space. These findings suggested aggravation of the remaining angiosarcoma (arrows).
2) Case 2
A 37-year-old previously healthy female, who was a hepatitis B virus carrier, visited the emergency department of a local hospital because of dyspnea (New York Heart Association class II) and a sudden onset of syncope. Cardiomegaly was detected on her chest X-ray. A TTE was performed, which showed a large amount of pericardial effusion and RA mass. After the patient underwent pericardiocentesis, her symptoms improved and she was transferred to our hospital for further work-up. No distant metastasis was seen on positron emission tomography. As a large mass in the RA anterior wall and an atrioventricular groove were detected on MRI and CT (Fig. 1B), the patient was scheduled to undergo heart transplantation; however, she was unable to undergo heart transplant surgery for two months because she tested positive for human leukocyte antigen on the immunological test. Our next best option was to remove the RA mass. The patient's surgery progressed similarly to that of the Case 1 patient. There was a large mass (4×5 cm) on the RA anterior wall and the mass widely adhered to the pericardium. Although the RA wall mass and pericardium were sufficiently removed including the RA, SVC, IVC, and septal tissue, tumor cells were detected on frozen biopsy. Therefore, we removed more of the RA wall, SVC, and IVC. However, as other tumor cells were detected, we assumed that there was widespread infiltration of tumor cells into the RA wall. We could not continue the operation because the cardiac tissue looked normal. The RA mass proved to be an angiosarcoma and the tumor cells made an invasion into the RA wall margin on permanent pathology.
The patient was extubated 10 hours postoperatively and underwent an uncomplicated recovery. A follow-up TTE on the fourth postoperative day showed no remaining RA mass. The patient was discharged on the ninth postoperative day after having had no postoperative complications. In the outpatient clinic four months later, CT was performed and showed aggravation of the angiosarcoma (Fig. 3B). She is currently undergoing radiation therapy and symptoms of congestive heart failure have not developed.
DISCUSSION
Primary cardiac tumors are rare, with an autopsy incidence ranging from 0.001% to 0.03%. Approximately 75% of primary cardiac tumors are benign, while 25% are malignant. In adults, angiosarcomas or rhabdomyosarcomas are the most common malignant tumors. Angiosarcomas occur more often in males and almost all are found in the RA. As angiosarcomas grow rapidly, metastasis and widespread local infiltration are common findings. Dyspnea on exertion is the most common symptom, with other common symptoms including congestive heart failure, pericardial effusion, pleuritic pain, and non-specific signs of disseminated malignancy, such as fever and weight loss [1]. The prognosis for patients with malignant cardiac tumors remains poor with some reports indicating a median survival of six to eight months.
In many cases, there is an abnormal chest X-ray finding of cardiomegaly; however, this is not a specific finding for angiosarcoma. Echocardiography is helpful for diagnosing patients with angiosarcoma. Chest CT scanning and MRI with enhancement are helpful imaging modalities for tumor evaluation as these tumors appear as contrast-enhanced masses, and these imaging modalities are also able to evaluate adjacent organs for metastasis and seeding [2].
Complete surgical resection is the most successful treatment for improving the patient's survival rate. Many patients have not survived due to the mass size of the tumor, surgeons lacking experience with extended cardiac resections, and the uncertainty of the diagnosis regarding invasion and metastasis. Many studies have suggested that adjuvant chemotherapy and radiotherapy after surgical resection can improve the survival rate of these patients. Bakaeen et al. [3] reported that patients who have undergone surgical resection, radiofrequency ablation, or radiation treatment had a median survival rate of 47 months (range, 16 to 119 months), whereas patients who underwent only surgical resection had a median survival rate of 25 months (range, 8 to 34 months). However, the use of chemotherapy and radiation therapy following surgical resection remains controversial [3,4]. If the surgical margins are involved with tumor or disease progression, these patients are considered for orthotopic transplantation, although there are still concerns regarding tumor growth following treatment with immunosuppressive drugs [4,5].
In our experience, tumor invasion of the resection margin of angiosarcomas is unpredictable. As mentioned above, although prognosis for patients with angiosarcoma is very poor, multimodal treatment can be helpful for these patients. Therefore, optimal imaging studies must precede surgical resection. However, imaging studies do not provide the exact extent of surgical resection, and as a result surgeons must keep in mind that angiosarcoma can infiltrate the tissue nearby the mass.
References
- 1.Shapiro LM. Cardiac tumours: diagnosis and management. Heart. 2001;85:218–222. doi: 10.1136/heart.85.2.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simpson L, Kumar SK, Okuno SH, et al. Malignant primary cardiac tumors: review of a single institution experience. Cancer. 2008;112:2440–2446. doi: 10.1002/cncr.23459. [DOI] [PubMed] [Google Scholar]
- 3.Bakaeen FG, Jaroszewski DE, Rice DC, et al. Outcomes after surgical resection of cardiac sarcoma in the multimodality treatment era. J Thorac Cardiovasc Surg. 2009;137:1454–1460. doi: 10.1016/j.jtcvs.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 4.Kodali D, Seetharaman K. Primary cardiac angiosarcoma. Sarcoma. 2006;2006:39130. doi: 10.1155/SRCM/2006/39130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Talbot SM, Taub RN, Keohan ML, Edwards N, Galantowicz ME, Schulman LL. Combined heart and lung transplantation for unresectable primary cardiac sarcoma. J Thorac Cardiovasc Surg. 2002;124:1145–1148. doi: 10.1067/mtc.2002.126495. [DOI] [PubMed] [Google Scholar]