Abstract
A 31-year-old female was referred from other hospital due to migrating chest pain, mild cough, and blood-tinged sputum for three days before admission. Laboratory tests were unremarkable. Chest computed tomography revealed an elliptical necrotic mass at the left anterior mediastinum, measuring 7×3×4 cm. With the impression of mediastinal abscess or loculated empyema, thoracoscopic resection was performed. There was severe pleural adhesion around the mass. The mass could be resected by the wedge resection of the adhesed upper lobe tissue of left lung around the mass. Final pathologic diagnosis was ectopic pancreas.
Keywords: Mediastinal disease, Pancreas, Chorisroma
CASE REPORT
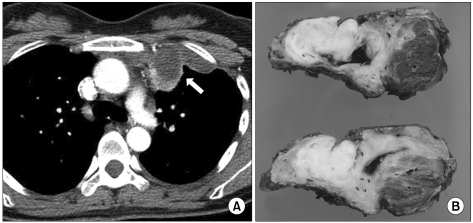
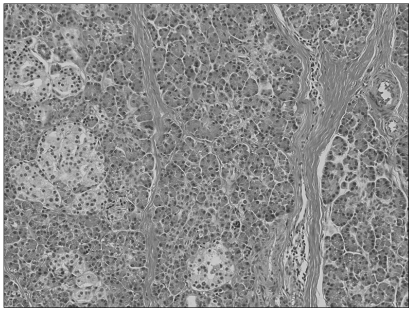
A 31-year-old female was referred with a three day history of migrating chest pain, mild cough, and blood-tinged sputum. Her breathing sounds were clear without rales or wheezing. Her body temperature was normal. Laboratory tests were unremarkable. Chest radiography showed an opacity at the medial side of the left upper lung field that seemed to be an elongated mass. A chest computed tomography revealed an elliptical necrotic mass measuring 7×3×4 cm at the left anterior mediastinum with consolidation of the adjacent left upper lung (Fig. 1A). The mass was located over the aortic arch and the main pulmonary artery without any signs of compression or invasion. The remaining area of the lungs and mediastinum were normal. The mass had a thickened wall with mild regional enhancement. A surgical resection was performed because the mass was thought to be a mediastinal abscess or loculated empyema. A thoracoscopy revealed severe pleural adhesion with hypervascularity on the left upper lung, especially around the mass. After adhesiolysis was performed, the mass was dissected from the surrounding mediastinal tissues and isolated from the mediastinum. Because of dense adhesion with the lung, we performed a wedge resection of the left upper lobe. Grossly, the mass was hard, had an oval shaped contour, and had a cyst filled with turbid dark bloody fluid. Macroscopically, the mass was composed of pale-yellowish fibroadipose tissue and cystic lesions that contained dark-brown mucinous material (Fig. 1A). Microscopically, the fibroadipose tissue was determined to be pancreatic tissue with a normal acinar structure and islets of pancreas (Fig. 2). There was no evidence of epithelial tissue, muscle fiber, or a bony compartment to suggest the occurrence of a teratoma.
Fig. 1.
Computed tomography image and the corresponding macroscopic image of the specimen. A necrotic mass with mild rim enhancement at the left anterior mediastinum (A). The mass was composed of a pale-yellowish solid portion and cystic portion. The wall of the cystic portion was thick and had dense adhesion with the adjacent lung (B).
Fig. 2.
Microscopic findings of the solid portion revealed a normal acinar structure and islets of the pancreas (H&E, ×200).
DISCUSSION
Ectopic pancreas is defined as pancreatic tissue without anatomical or vascular connection to the main body of the pancreas. Ectopic pancreas is discovered in approximately 2% of all autopsies [1] and most of the ectopic pancreatic tissue was located in the gastrointestinal tract [1,2]. The pancreatic tissue is often found in a mediastinal teratoma that is composed of ectodermal, mesodermal, and endodermal tissue [3]. Pancreatic tissue in teratomas originates from endodermal tissue, but an ectopic pancreas does not contain other germ cell lines such as those of hair, teeth or bone. Mediastinal ectopic pancreas is rarely reported. The etiology of ectopic pancreas is still obscure, but there are two different hypotheses. Abnormal differentiation of pluripotent epithelial cells at the ventral primary foregut is one of the hypotheses, and the migration of some cells from the pancreatic bud to a different site is the other hypothesis [1]. Most mediastinal ectopic pancreatic masses are mainly located in the anterior mediastinum and grow toward the right. However, in the present case, the mass was located in the left anterior mediastinum. The computed tomography findings of the ectopic mediastinal pancreas were cystic or cystic-solid and the cyst wall and the solid portion of the lesion were slightly enhanced [4]. The symptoms of ectopic pancreas vary according to its location. Most patients are young and the male-to-female ratio is approximately balanced [4]. Patients complain of nonspecific symptoms, such as shortness of breath, high fever, chest pain, or no symptoms at all. The mass is usually very large in asymptomatic patients at the time of discovery. A large mass compresses adjacent structures, and pericardial effusion or tamponade can develop if the cyst ruptures into the pericardium [5]. The blood-tinged sputum found in this patient might be the result of lung injury due to enzyme-containing ectopic pancreas or compression. These features were different from other patients in previous case reports. The treatment of choice for mediastinal ectopic pancreas is surgical resection. It is difficult to distinguish ectopic pancreas from tumors in the mediastinum, especially cystic teratomas, using imaging studies. There is a lack of long term follow-up data on mediastinal ectopic pancreas, other than one report by Tamura et al. [4], which followed a patient with mediastinal ectopic pancreas for eight years after the operation, and no recurrence or metastasis was found [6].
References
- 1.Perez-Ordonez B, Wesson DE, Smith CR, Asa SL. A pancreatic cyst of the anterior mediastinum. Mod Pathol. 1996;9:210–214. [PubMed] [Google Scholar]
- 2.Cagirici U, Ozbaran M, Veral A, Posacioglu H. Ectopic mediastinal pancreas. Eur J Cardiothorac Surg. 2001;19:514–515. doi: 10.1016/s1010-7940(01)00606-6. [DOI] [PubMed] [Google Scholar]
- 3.Cho S, Lee EB. The differences between ruptured and unruptured mediastinal teratoma. Korean J Thorac Cardiovasc Surg. 2009;42:355–360. [Google Scholar]
- 4.Tamura Y, Takahama M, Kushibe K, Taniguchi S. Ectopic pancreas in the anterior mediastinum. Jpn J Thorac Cardiovasc Surg. 2005;53:498–501. doi: 10.1007/s11748-005-0095-6. [DOI] [PubMed] [Google Scholar]
- 5.von Schweinitz D, Wittekind C, Freihorst J. Mediastinal sequestration with ectopic pancreatic tissue. Z Kinderchir. 1990;45:249–250. [PubMed] [Google Scholar]
- 6.Wang W, Li K, Qin W, Sun H, Zhao C. Ectopic pancreas in mediastinum: report of 2 cases and review of the literature. J Thorac Imaging. 2007;22:256–258. doi: 10.1097/01.rti.0000213587.44719.a7. [DOI] [PubMed] [Google Scholar]