Abstract
Objectives
Using data from dentists participating in The Dental Practice-Based Research Network (DPBRN), the study had 2 main objectives: (1) to identify and quantify the types of restorative materials in the existing failed restorations; and (2) to identify and quantify the materials used to repair or replace those failed restorations.
Methods
This cross-sectional study used a consecutive patient/restoration recruitment design. Practitioner-investigators recorded data on consecutive restorations in permanent teeth that needed repair or replacement. Data included the primary reason for repair or replacement, tooth surface(s) involved, restorative materials used, and patient demographics.
Results
Data for 9,875 restorations were collected from 7,502 patients in 197 practices for which 75% of restorations were replaced and 25% repaired. Most of the restorations that were either repaired or replaced were amalgam (56%) for which most (56%) of the material used was direct tooth-colored. The restorative material was 5 times more likely to be changed when the original restoration was amalgam (OR=5.2, p<.001). The likelihood of changing an amalgam restoration differed as a function of the tooth type (OR=3.0, p<.001), arch (OR=6.6, p<.001); and number of surfaces in the original restoration (OR=12.2, p<.001).
Conclusion
The probability of changing from amalgam to another restorative material differed with several characteristics of the original restoration. The change was most likely to take place when (1) the treatment was a replacement; (2) the tooth was not a molar; (3) the tooth was in the maxillary arch; and (4) the original restoration involved a single surface.
Keywords: practice-based research, repair, replacement, decision, defective, restorations
Introduction
Replacement of existing restorations still occupies most of general practitioners' treatment time1-4. The reasons restorations are replaced may vary according to the material in the existing restoration, as well as to other tooth-specific factors5-7. Identifying the materials and tooth-specific variables that can influence a dentist's decision to repair or replace restorations can be valuable when planning new strategies for minimally invasive dentistry. Furthermore, it can provide a new insight to clinicians when considering repair versus replacement of existing restorations. Therefore, using data from dentists participating in The Dental Practice-Based Research Network (DPBRN), the study had 2 main objectives: (1) to identify and quantify the types of restorative materials in the existing failed restorations; and (2) to identify and quantify the materials used to repair or replace those failed restorations. Additionally, the study sought to identify the restorative material and other tooth-specific characteristics associated with the decision to repair or replace the existing restoration by testing the following hypotheses: (1) Dentists are more likely to change restorative materials when the material of the original restoration is amalgam; (2) Restorations that are replaced are more likely to involve a change of restorative material than restorations that are repaired; (3) The likelihood of changing from amalgam restoration differs as a function of other tooth-specific variables, such as tooth type and number of surfaces in the original restoration.
Materials and Methods
Selection and recruitment process
This cross-sectional study included 197 practitioner-investigators participating in the DPBRN were enrolled in this study and recorded data on consecutive defective restorations that needed repair or replacement on permanent teeth. The DPBRN comprises outpatient dental practices mainly from five regions: AL/MS: Alabama/Mississippi; FL/GA: Florida/Georgia; MN: dentists employed by HealthPartners and private practitioners in Minnesota; PDA: Permanente Dental Associates in cooperation with Kaiser Permanente Center for Health Research, Portland, Oregon; and SK (Scandinavia): Denmark, Norway, and Sweden. Practice structures differed by DPBRN region. Dentists from the AL/MS and FL/GA regions were primarily in independent or small group practices, MN and PDA dentists were primarily in large group practices, and SK dentists were in public or private health care settings. This study was approved by the respective Institutional Review Boards of the participating regions. DPBRN practitioner-investigators were recruited through continuing education courses and/or mass mailings to licensed dentists within the participating regions. As part of the eligibility criteria, all dentists completed (1) a DPBRN Enrollment Questionnaire describing their demographic and practice characteristics and certain personal characteristics, (2) an Assessment of Caries Diagnosis and Caries Treatment Questionnaire, (3) training in human subjects protection, and (4) a DPBRN orientation session with the regional coordinator. Copies of the questionnaires and summary data for dentists' demographic and practice characteristics are available at http://www.dpbrn.org/users/publications/Default.aspx. Results from previous studies confirm that dentists in practice-based research networks have much in common with dentists at large8,9.
This study used a consecutive patient/restoration recruitment design and every patient who received a repair or replacement of a restoration on a permanent tooth was asked to participate. Patients who returned for additional appointments while data collection was still ongoing were not eligible for further data collection. Only restorations eligible during the first appointment were enrolled. The practitioner could enroll up to 4 restorations per patient and continued to collect data until information on 50 restorations had been collected. The number of lesions/patient was restricted in order to limit the size of clustering at the patient-level, thus increasing the precision and generalizability of the study. Patient recruitment varied from practice to practice, and on average the recruitment took about 5 months. A consecutive patient/restoration log form was used to record information on eligible restorations whether or not the patient participated in the study. All the data collection forms used for this study are available at http://www.DentalPBRN.org/users/publications/Supplement.aspx.
Variable selection
Restoration replacement was characterized as the entire removal of the existing defective/failed restoration and any adjacent pathologically altered or discolored tooth tissue that was esthetically or functionally unacceptable. Repair was characterized as the removal of part of the existing restoration and any adjacent pathologically altered as well as discolored tooth tissue that was esthetically unacceptable followed by placement of restorative material in the prepared site. Repair also included light grinding and polishing, removal of overhangs, polishing discolored tooth-colored restorations, or sealing margins.
Practitioner-investigators collected data for each enrolled restoration that needed repair or replacement on permanent tooth surfaces. Data collected included: (1) the main reason for repair or replacement of the restoration (previously reported)10; (2) tooth type and tooth surfaces being restored; and (3) the restorative materials used for the old and the new restoration. Dentists diagnosed the need to repair or replace the existing restoration based on the diagnostic methods they typically use in their practice, which consist mainly of visual-tactile in association with radiographic examinations.
Restorative materials were classified as amalgam, direct or indirect resin-based composite (RBC or IRBC), conventional or resin-modified glass-ionomer (GI/RMGI), ceramic or porcelain, cast gold or other metallic-based material, combined metal-ceramic material, and temporary restorative materials. When multiple materials were reported, the material most likely to fail was used for classification. Information about gender, age, race, ethnicity, and insurance coverage of enrolled patients was also recorded.
The Data Collection Form was pre-tested by sixteen DPBRN practitioner-investigators. Pre-testing consisted of assessing the feasibility of the form in the flow of a busy practice environment, as well as the comprehension and intuitiveness of the classification criteria. The pre-testing phase for each of these groups met a test-retest reliability of kappa > 0.70 or ICC > 0.70.
Statistical analysis
A binary logistic model, with Generalized Estimating Equations to adjust for clustering within dental practices and restorations within patients, was used to examine dentist, patient, and restoration variables as predictors of the decision to repair or replace the restoration. The GENLIN procedure within SPSS 19 was used with an exchangeable correlation matrix structure.
Hypothesis 1: Dentists are more likely to change restorative materials when the material of the original restoration is amalgam.
Hypothesis 2: Restorations that are replaced are more likely to involve a change of restorative material than restorations that are repaired.
Hypotheses 3: The likelihood of changing from an amalgam restoration differs as a function of other tooth-specific variables, such as tooth type (molar, premolar, anterior), and the number of surfaces in the original restoration.
For data analysis, the original and treatment materials were combined into three major categories: 1) amalgam; 2) direct tooth-colored restorations (resin-based composite [RBC], compomer, and glass ionomer); and 3) indirect restorations (indirect RBC, ceramic, gold or metallic, and porcelain fused to metal). The dependent variable for this study was “material change” coded as the same material used in treatment as in the original restoration (no change) = 0, a different material was used in treatment (change) = 1. For example, if the original material was amalgam and an indirect restoration material was used in the treatment visit, it was classified as a change and coded 1; whereas, if an indirect restoration material was used for both the original restoration and during the treatment visit, it was classified as no change and coded 0.
The independent variables were coded as follows: Material: amalgam =1, direct tooth-colored restorations and indirect restorations=0; Treatment: repair=1, replacement=0; Tooth: molar=1, pre-molar and anterior=0; Arch: maxillary=1, mandibular=0; Surfaces: 1=1, 2=2, 3+=3.
The first step in the analysis consisted of testing hypothesis 1, which involved the main effect of amalgam as the original restoration material (model = “amalgam”). The second step involved testing hypothesis 2, which was tested by the material × treatment interaction term (model = “amalgam” + “treatment” + “amalgam × treatment”), where treatment meant repair or replacement. The third hypothesis was tested one variable at a time and was supported when the interaction term involving that variable and amalgam was statistically significant. Certain variables – namely, patient variables (age, gender, race, insurance status), dentist variables (SK region, gender, years since dental school graduation) and restoration variables (treatment, tooth site, arch, number of surfaces on the original restoration, secondary caries, the dentist placed the original restoration) were included as control variables if that variable was not being specifically tested in that particular model as part of the hypothesis test. Each hypothesized significant interaction term was interpreted by testing the amalgam variable at each level of the tested variable.
Results
The 197 participating dentists returned data on a total of 9,875 restorations collected from 7,502 patients. Three hundred ninety-one of the restorations resulted in a temporary restoration or the dentist did not specify the treatment. Complete data were not available for an additional 563 restorations; therefore, all subsequent analyses involved 8,921 restorations with complete data from 6,759 patients. Seventy-five percent (n=6,657) of restorations were replaced and 25% (n=2,264) repaired.
Practice and patient characteristics are presented in Table 1. Patients were treated in 197 practices distributed across the DPBRN regions as AL/MS=39, FL/GA=44, PDA=40, MN=36, SK=38. One hundred thirty-eight (70%) providers were male and 59 (30%) were female. Mean number of years since dental school graduation was 21.6 (SD=10.5). The average percent of time spent performing non-implant restorations was 55.8 (SD=19.9). Regarding patient characteristics, 57% were female and 43% were males, and 21% had dental insurance. Patient race was White, 89%; Black or African American, 6%; American Indian or Alaskan native, 1%; Asian, 2%; Native Hawaiian or other Pacific Islander, < 1%; and Other, 1%.
Table 1. Dentists', practices', and patients' characteristics.
| Variable | Mean (SD) or % (n) |
|---|---|
| Dentists'and practices' characteristics (n=197) | |
| Gender (male) | 70% (138) |
| Years since dental school graduation | 21.7 (SD=10.5) |
| Full-time (32+ hours per week in patient care) | 86% (162) |
| Dental chairs per office | 4.0 (SD=2.3) |
| Practice type | |
| - Solo or small group private practice | 58% (114) |
| - Large group practice | 37% (72) |
| - Public health service | 6% (11) |
| Percent of revenue derived from dental insurance | 58% (SD=32) |
| Percent of time spent on non-implant restorative care | 56% (SD=20) |
| Patients'characteristics (n=6,744) | |
| Gender (female) | 57% (3,862) |
| Age | 51.4 (SD=16.0) |
| Hispanic ethnicity (missing=109) | 12% (762) |
| Race (missing=97) | |
| - White | 90% (6,003) |
| - Black or African American | 6% (412) |
| - Asian or Pacific Islander | 1% (86) |
| - American Indian or Alaskan native | <1% (60) |
| - Other | 1% (101) |
| Number of restorations done during the visit | |
| - Single restoration | 76% (5,105) |
| - Two restorations | 18% (1,228) |
| - Three restorations | 5% (311) |
| - Four restorations | 2% (115) |
| Dental insurance or any third party coverage | 21% (1,438) |
The overall percent distribution of the restorative material for the restorations that were repaired or replaced was: 56% (4,999) were amalgam restorations, 37% (3,296) were direct tooth-colored restorations, and 7% (626) were indirect restorations. The distribution of the restorative materials used to repair or replace the failed restorations was 29% (2,559) amalgam, 56% (5,000) direct tooth-colored, and 15% (1,362) indirect restorations. Figure 1 presents the percentages for the replacement material used for each of the original materials. The frequencies for the original restoration material cross-tabulated with the treatment material are presented in Table 2.
Figure 1. Restoration material (%) used by orginal material.
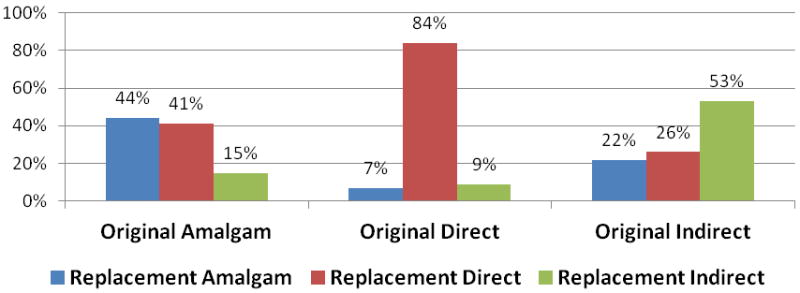
Table 2. Percent distribution of the restorative material used in the new treatment according to the material in the original restoration.
| Treatment material | Amalgam % (n) | Direct tooth-colored % (n) | Indirect % (n) | Total |
|---|---|---|---|---|
| Replacement | ||||
| Original Amalgam | 39% (1,545) | 43% (1,730) | 18% (724) | 3,999 |
| Original Direct tooth-colored | 8% (192) | 79% (1,823) | 12% (282) | 2,297 |
| Original Indirect | 2% (6) | 8% (28) | 91% (327) | 361 |
| Total | 1,743 | 3,581 | 1,333 | 6,657 |
| Repair | ||||
| Original Amalgam | 64% (643) | 34% (336) | 2% (21) | 1,000 |
| Original Direct tooth-colored | 4% (44) | 95% (950) | <1% (5) | 999 |
| Original Indirect | 49% (129) | 50% (133) | 1% (3) | 265 |
| Total | 816 | 1,419 | 29 | 2,264 |
Table 3 shows the percent distribution of the restorative material used in the repair and replacement of restorations in the USA regions and SK regions according to the material in the original restoration. For the SK region, with the exception of the indirect restorative material, the majority of the restorations were either repaired or replaced with direct tooth-colored restorations. The number of indirect restorations had a 3-fold increase after the treatment. The SK variable was statistically significant in testing for a difference in the probability of changing the restoration material (OR = 1.98, p .001 in the test of hypothesis 1) suggesting that SK dentists were more likely than US dentists to change an amalgam material. Exploratory analyses were performed removing SK data from our models with no change found in the interpretation of any of the findings reported below.
Table 3. Percent distribution of the restorative material used in the repair and replacement of restorations in the USA regions and SK regions according to the material in the original restoration.
| Treatment material | Amalgam % (n) | Direct tooth-colored % (n) | Indirect % (n) | Total |
|---|---|---|---|---|
| USA | ||||
| Original Amalgam | 52% (2,180) | 32% (1,322) | 16% (694) | 4,196 |
| Original Direct tooth-colored | 9% (234) | 81% (2,039) | 10% (236) | 2,509 |
| Original Indirect | 24% (135) | 23% (132) | 53% (296) | 563 |
| Total | 2,549 | 3,493 | 1,226 | 7,268 |
| SK | ||||
| Original Amalgam | 1% (8) | 93% (744) | 6% (51) | 803 |
| Original Direct tooth-colored | < 1% (2) | 93% (734) | 7% (51) | 787 |
| Original Indirect | 0% (0) | 46% (29) | 54% (34) | 63 |
| Total | 10 | 1,507 | 136 | 1,653 |
Testing study hypotheses
Regression coefficients tested in hypotheses 1-3 are shown in Table 4.
Table 4.
Regression coefficients tested in hypotheses 1, 2, and 3.
| B (SE) | OR (95% CI) (a) | p value | |
|---|---|---|---|
| Amalgam(b) | 1.7 (.1) | 5.2 (4.6-5.9) | .<001 |
| Amalgam × treatment | 1.4 (.1) | 4.1 (3.2-5.3) | <.001 |
| Repair | .6 (.1) | 1.8 (1.4-2.3) | <.001 |
| Replacement | 2.3 (.1) | 7.8 (6.7-9.2) | <.001 |
| Amalgam × tooth type | 2.3 (.2) | 9.7 (8.1-11.2) | <.001 |
| Molar | 1.1 (.1) | 3.0 (2.5-3.5) | < .001 |
| Premolar | 1.5 (.1) | 4.5 (3.6-5.7) | <.001 |
| Anterior | 5.0 (.4) | 137.2 (62.4-301.9) | <.001 |
| Amalgam × arch | .4 (.1) | 1.6 (1.2-1.9) | <.001 |
| Maxillary | 1.9 (.2) | 6.6 (5.5-8.0) | <.001 |
| Mandibular | 1.4 (.1) | 4.1 (3.4-4.8) | <.001 |
| Amalgam × surfaces | -.7 (.1) | 0.5 (0.4-0.6) | <.001 |
| Single surface | 2.5 (.2) | 12.2 (8.5-17.7) | <.001 |
| 2 surfaces | 1.9 (.1) | 7.0 (5.4-9.0) | <.001 |
| 3+ surfaces | 1.2 (.1) | 3.4 (2.9-4.0) | <.001 |
The dependent variable was “material change” and was coded as material not changed=0 and material changed=1.
All non-amalgam original restoration materials (direct tooth-colored or indirect material) were the reference group.
All models included certain patient characteristics (age, gender, race, insurance status), dentist characteristics (region, gender, years since dental school graduation) and restoration characteristics (treatment, tooth site, arch, number of surfaces on the original restoration, secondary caries, the dentist placed the original restoration) as control variables if not a tested variable in that model.
Hypothesis1: Original material
For repair or replacement of the restorations, the restoration material was 5 times more likely to be changed when the original material was amalgam (OR=5.2, p<.001) than when the original material was a direct tooth-colored or indirect material.
Hypothesis 2: Treatment
The likelihood of changing an amalgam restoration differed as a function of whether the treatment was repair or replacement, as indicated by the significant amalgam × treatment interaction effect (p<.001). When the restoration was repaired, the material was nearly 2 times more likely to be changed when the original material was amalgam (OR=1.9, p<.001) than when the original material was a direct tooth-colored or indirect material; whereas when the restoration was replaced, the material was nearly 8 times more likely to be changed when the original material was amalgam (OR=7.8, p<.001) compared to the other materials.
Hypothesis 3: Tooth-specific variables
The likelihood of changing an amalgam restoration differed as a function of the tooth type, as indicated by the significant amalgam × tooth type interaction effect (p <.001). For restorations that were either repaired or replaced, if the restoration was in a molar tooth, the material was 3 times more likely to be changed when the original material was amalgam (OR=3.0, p<.001) than when the original material was a direct tooth-colored or indirect material; whereas when the restoration was in a premolar tooth, the material was more than 4 times more likely to be changed when the original material was amalgam (OR=4.5, p<.001) compared to the other materials. Furthermore, when the restoration was in an anterior tooth, the material was more than 137 times more likely to be changed when the original material was amalgam (OR=137.2, p<.001). See Table 5. The likelihood of changing an amalgam restoration also differed as a function of the arch, as indicated by the significant amalgam × arch interaction effect (p<.001). When the restoration was in the maxillary arch, the material was more than 6 times more likely to be changed when the original material was amalgam (OR=6.6, p<.001) than when the original material had been a direct tooth-colored or indirect material; whereas when the restoration was in the mandibular arch, the material was 4 times more likely to be changed when the original material was amalgam (OR=4.1, p<.001) compared to the other materials. See Table 6. Finally, the likelihood of changing an amalgam restoration differed as a function of the number of surfaces in the original restoration, as indicated by the significant amalgam × tooth interaction effect (p<.001). When the restoration involved a single surface, the material was 12 times more likely to be changed when the original material was amalgam (OR=12.2, p<.001) than if the original material was a direct tooth-colored or indirect material. When the restoration involved two surfaces, the material was 7 times more likely to be changed when the original material was amalgam (OR=7.0, p<.001) compared to the other materials, whereas, when the restoration involved three or more surfaces, the material was more than 3 times more likely to be changed when the original material was amalgam (OR=3.4, p<.001). See Table 7.
Table 5. Percent distribution of the restorative material used in the new treatment according to the material in the original restoration and tooth type.
| Treatment material | Amalgam % (n) | Direct tooth-colored % (n) | Indirect % (n) | Total |
|---|---|---|---|---|
| Molar | ||||
| Original Amalgam | 46% (1,567) | 40% (1,363) | 14% (488) | 3,418 |
| Original Direct tooth-colored | 14% (153) | 75% (813) | 11% (121) | 1,087 |
| Original Indirect | 27% (6) | 24% (81) | 49% (162) | 334 |
| Total | 1,811 | 2,257 | 771 | 4,839 |
| Premolar | ||||
| Original Amalgam | 41% (606) | 42% (619) | 17% (249) | 1,474 |
| Original Direct tooth-colored | 11% (74) | 79% (527) | 10% (65) | 666 |
| Original Indirect | 19% (29) | 28% (42) | 53% (65) | 152 |
| Total | 709 | 1,188 | 395 | 2,292 |
| Anterior | ||||
| Original Amalgam | 14% (15) | 79% (84) | 8% (8) | 107 |
| Original Direct tooth-colored | <1% (9) | 93% (1,433) | 7% (101) | 1,543 |
| Original Indirect | 11% (15) | 27% (38) | 62% (87) | 140 |
| Total | 39 | 1,555 | 196 | 1,790 |
Table 6. Percent distribution of the restorative material used in the new treatment according to the material in the original restoration and arch.
| Treatment material | Amalgam % (n) | Direct tooth-colored % (n) | Indirect % (n) | Total |
|---|---|---|---|---|
| Maxillary arch | ||||
| Original Amalgam | 45% (1,777) | 40% (1,064) | 15% (402) | 2,643 |
| Original Direct tooth-colored | 6% (118) | 86% (1,751) | 8% (171) | 2,040 |
| Original Indirect | 14% (45) | 24% (74) | 62% (193) | 312 |
| Total | 1,340 | 1,002 | 766 | 4,995 |
| Mandibular arch | ||||
| Original Amalgam | 43% (1,011) | 43% (1,002) | 15% (343) | 2,356 |
| Original Direct tooth-colored | 9% (118) | 81% (1,022) | 9% (116) | 1,256 |
| Original Indirect | 29% (90) | 28% (87) | 44% (137) | 314 |
| Total | 1,219 | 2,111 | 596 | 3,926 |
Table 7. Percent distribution of the restorative material used in the new treatment according to the material in the original restoration and number of surfaces involved.
| Treatment material | Amalgam % (n) | Direct tooth-colored % (n) | Indirect % (n) | Total |
|---|---|---|---|---|
| One surface | ||||
| Original Amalgam | 44% (466) | 55% (582) | 2% (18) | 1,066 |
| Original Direct tooth-colored | 6% (63) | 93% (905) | 1% (10) | 978 |
| Original Indirect | 31% (10 | 50% (16) | 19% (6) | 32 |
| Total | 539 | 1,503 | 34 | 2,076 |
| Two surfaces | ||||
| Original Amalgam | 48% (951) | 44% (874) | 8% (162) | 1,987 |
| Original Direct tooth-colored | 10% (120) | 85% (991) | 5% (54) | 1,165 |
| Original Indirect | 20% (4) | 65% (13) | 15% (3) | 20 |
| Total | 1,075 | 1,878 | 219 | 3,172 |
| Three or more surfaces | ||||
| Original Amalgam | 40% (771) | 31% (610) | 29% (565) | 1,946 |
| Original Direct tooth-colored | 5% (53) | 76% (877) | 19% (223) | 1,153 |
| Original Indirect | 21% (121) | 23% (132) | 56% (321) | 574 |
| Total | 945 | 1,619 | 119 | 3,673 |
Discussion
The longevity of dental restorations is dependent on many factors, including those related to materials, the dentist who placed the restoration, and the patient. The longevity of amalgam restorations has been the main proof of the success of this restorative material, as evidenced by numerous studies3,11-15. However, despite the fact that studies have discussed its safety as a restorative material16-19 amalgam restorations are being replaced, and most likely it is because of its inferior esthetic appearance, alleged adverse health effects, and environmental concerns20-23. Consistent with the fact that the use of amalgam as a restorative material is decreasing in general dental practice11,24,25, amalgam was not the main restorative material used when repair or replacement of restorations took place in the current study. In fact, when repairing and replacing existing restorations, clinicians were significantly more likely to change the restorative material when the material in the original restoration was amalgam. Amalgam has actually been banned from certain countries in Europe, in particular in the Scandinavia region. Indeed, the current study showed that for participants from the Scandinavian region, almost all of the restorations that were either repaired or replaced used direct tooth-colored restorative materials.
Restorations that were replaced were more likely to involve a change of restorative material than restorations that were repaired. When the original material was amalgam and the restoration was repaired, it was then acceptable to some dentists in the US regions to repair existing amalgam restorations using amalgam as the restorative material. Previous studies have shown that repair is an effective treatment alternative to amalgam restorations that were originally considered defective26-28. Laboratory studies have also attested to the success of the amalgam repair29-31. The replacement of defective restorations will lead to loss of healthy tooth structure32-34 and weakening of the tooth, creating an increased risk of cusp fracture. Additionally, it may increase significantly the number of surfaces involved in the restoration. In fact, the results of the current study showed that when the replacement of an existing restoration took place and it had an increase in the number of surfaces involved, dentists opted for an indirect restoration, as evidenced by the 3-fold increase of the number of indirect restorations after treatment.
Direct tooth-colored material was the main choice of material to repair or replace failed restorations by practicing dentists. Resin-based composite (RBC) materials rely on mechanical bonding and they can be placed in small surface areas; therefore, they were probably an appealing option for the repair treatment of defective or failed restorations. Additionally, numerous in vitro studies have reported acceptable bonding strength forces for the repair of RBC materials35-41. Clinical studies have also confirmed the long-term success of restorations that have been repaired with RBC materials42-44. Direct tooth-colored material was also the main choice for the replacement of failed restorations. Previous studies have confirmed that the use of RBC restorations has increased in the last several years45-49. It is possible that patients' expectations for a more-esthetic appearance than that of the existing amalgam material may have influenced the clinician's decision to replace the existing restoration with a tooth-colored material. Studies have confirmed the decline of amalgam as a restorative material in recent years11,50,51.
The likelihood of changing from amalgam when repair or replacement was done differed significantly as a function of tooth-specific variables, such as tooth type, arch location, and the number of surfaces in the original restoration. Premolar and anterior teeth were most likely to receive a change in restorative material when the original restoration was amalgam. Anterior teeth are located in an esthetic zone and premolar teeth are also positioned in a more-esthetic zone when compared to molar teeth; therefore, it would be expected that those teeth would receive a tooth-colored restoration if the restoration had to be replaced. Because molar teeth receive most of the biting forces52 and amalgam materials have performed well in this area, dentists may not have been as likely to change the restorative material when the restoration was in a molar tooth. Also related to the same line of thought, when the number of surfaces in the original restoration was smaller, particularly if the tooth involved one surface and had an amalgam, the restoration was more likely to be changed with a direct tooth-colored material. Occlusal forces may not have been as critical to the decision if the tooth had involved two or less surfaces. Indeed, the study showed a gradual decrease in the tendency to change the restorative material from amalgam to direct tooth-colored materials as the number of surfaces in the original restoration increased. Regarding the arch location, it is unclear why dentists were more likely to change the restorative material when the original restoration was an amalgam and the tooth was located in the maxillary arch. Even though some studies discussed that tooth type and arch location had significant differences in bond strength - with lower bond strength forces on maxillary molar teeth than on mandibular molar teeth53,54 - there have been no clinical studies to substantiate those findings.
In summary, the results of the study showed that amalgam material was not being frequently used in the repair or replacement of defective or failed restorations. Practitioners clearly were more likely to use direct tooth-colored materials to repair or replace existing restorations.
Conclusion
The probability of changing from amalgam to another restorative material differed for most characteristics of the original restoration in which the repair or replacement took place. The change was most likely to take place when (1) the treatment was a replacement; (2) the tooth was not a molar; (3) the tooth was in the maxillary arch; and (4) the original restoration involved a single surface.
Acknowledgments
This work was supported by National Institutes of Health grants U01-DE-16746 and U01-DE-16747. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully.
Footnotes
Competing interests: The authors declare that they have no competing interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Roumanas ED. The frequency of replacement of dental restorations may vary based on a number of variables, including type of material, size of the restoration, and caries risk of the patient. Journal of Evidence-Based Dental Practice. 2010;10:23–24. doi: 10.1016/j.jebdp.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 2.Simecek JW, Diefenderfer KE, Cohen ME. An evaluation of replacement rates for posterior resin-based composite and amalgam restorations in U.S.Navy and Marine Corps recruits. Journal of the American Dental Association. 2009;140:200–209. doi: 10.14219/jada.archive.2009.0134. [DOI] [PubMed] [Google Scholar]
- 3.Soncini JA, Maserejian NN, Trachtenberg F, Tavares M, Hayes C. The longevity of amalgam versus compomer/composite restorations in posterior primary and permanent teeth: findings From the New England Children's Amalgam Trial. Journal of the American Dental Association. 2007;138:763–772. doi: 10.14219/jada.archive.2007.0264. [DOI] [PubMed] [Google Scholar]
- 4.Mjör IA, Moorhead JE, Dahl JE. Reasons for replacement of restorations in permanent teeth in general dental practice. International Dental Journal. 2000;50:361–366. doi: 10.1111/j.1875-595x.2000.tb00569.x. [DOI] [PubMed] [Google Scholar]
- 5.Hickel R, Manhart J. Longevity of restorations in posterior teeth and reasons for failure. Journal of Adhesive Dentistry. 2001;3:45–64. [PubMed] [Google Scholar]
- 6.Gordan VV, Garvan CW, Richman J, Fellows JL, Rindal DB, Qvist V, Heft MW, Williams OD, Gilbert GH The DPBRN Collaborative Group. How dentists diagnose and treat defective restorations: evidence from The Dental PBRN. Operative Dentistry. 2009;34:664–673. doi: 10.2341/08-131-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Opdam NJ, Bronkhorst EM, Cenci MS, Huysmans MC, Wilson NH. Age of failed restorations: A deceptive longevity parameter. Journal of Dentistry. 2011;39:225–230. doi: 10.1016/j.jdent.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, Qvist V DPBRN Collaborative Group. Dentists in practice-based research networks have much in common with dentists at large: evidence from The Dental PBRN. General Dentistry. 2009;57:270–275. [PMC free article] [PubMed] [Google Scholar]
- 9.Makhija SK, Gilbert GH, Rindal DB, Benjamin P, Richman JS, Pihlstrom DJ, Qvist V. DPBRN collaborative group practices participating in a dental PBRN have substantial and advantageous diversity even though as a group they have much in common with dentists at large. BMC Oral Health. 2009;159:26. doi: 10.1186/1472-6831-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gordan VV, Riley JL, III, Geraldeli S, Rindal DB, Qvist V, Fellows JL, Kellum HP, Gilbert GH The DPBRN Collaborative Group. Repair or replacement of defective restorations by dentists in The Dental PBRN. Journal of the American Dental Association. :378–11. doi: 10.14219/jada.archive.2012.0238. DOI #. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sunnegårdh-Grönberg K, van Dijken JW, Funegård U, Lindberg A, Nilsson M. Selection of dental materials and longevity of replaced restorations in Public Dental Health clinics in northern Sweden. Journal of Dentistry. 2009;37:673–678. doi: 10.1016/j.jdent.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, Leitao J, DeRouen TA. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. Journal of the American Dental Association. 2007;138:775–783. doi: 10.14219/jada.archive.2007.0265. [DOI] [PubMed] [Google Scholar]
- 13.Mjör IA, Moorhead JE. Selections of restorative materials, reasons for replacement, and longevity of restorations in Florida. Journal of the American College of Dentists. 1998;65:27–33. [PubMed] [Google Scholar]
- 14.Smales RJ, Webster DA. Restoration deterioration related to later failure. Operative Dentistry. 1993;18:130–137. [PubMed] [Google Scholar]
- 15.Roulet JF, Salchow B, Wald M. Margin analysis of posterior composites in vivo. Dental Materials. 1991;7:44–49. doi: 10.1016/0109-5641(91)90026-u. [DOI] [PubMed] [Google Scholar]
- 16.Sundström A, Bergdahl J, Nyberg L, Bergdahl M, Nilsson LG. Cognitive status in persons with amalgam-related complaints. Journal of Dental Research. 2010;89:1236–1240. doi: 10.1177/0022034510376649. [DOI] [PubMed] [Google Scholar]
- 17.Weidenhammer W, Bornschein S, Zilker T, Eyer F, Melchart D, Hausteiner C. Predictors of treatment outcomes after removal of amalgam fillings: associations between subjective symptoms, psychometric variables and mercury levels. Community Dentistry and Oral Epidemiology. 2010;38:180–189. doi: 10.1111/j.1600-0528.2009.00523.x. [DOI] [PubMed] [Google Scholar]
- 18.Roberts HW, Charlton DG. The release of mercury from amalgam restorations and its health effects: a review. Operative Dentistry. 2009;34:605–614. doi: 10.2341/08-072-LIT. [DOI] [PubMed] [Google Scholar]
- 19.Bellinger DC, Trachtenberg F, Zhang A, Tavares M, Daniel D, McKinlay S. Dental amalgam and psychosocial status: the New England Children's Amalgam Trial. Journal of Dental Research. 2008;87:470–474. doi: 10.1177/154405910808700504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mutter J. Is dental amalgam safe for humans? The opinion of the scientific committee of the European Commission. Journal of Occupational Medicine and Toxicology. 2011;6:2. doi: 10.1186/1745-6673-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neghab M, Choobineh A, Hassan Zadeh J, Ghaderi E. Symptoms of intoxication in dentists associated with exposure to low levels of mercury. Industrial Health. 2011;49:249–254. doi: 10.2486/indhealth.ms1214. [DOI] [PubMed] [Google Scholar]
- 22.Lynch CD, Guillem SE, Nagrani B, Gilmour AS, Ericson D. Attitudes of some European dental undergraduate students to the placement of direct restorative materials in posterior teeth. Journal of Oral Rehabilitation. 2010;37:916–926. doi: 10.1111/j.1365-2842.2010.02119.x. [DOI] [PubMed] [Google Scholar]
- 23.Edlich RF, Cross CL, Wack CA, Long WB, 3rd, Newkirk AT. The food and drug administration agrees to classify mercury fillings. Journal of Environmental Pathology, Toxicology and Oncology. 2008;27:303–305. doi: 10.1615/jenvironpatholtoxicoloncol.v27.i4.70. [DOI] [PubMed] [Google Scholar]
- 24.Shenoy A. Is it the end of the road for dental amalgam? A critical review. Journal of Conservative Dentistry. 2008;11:99–107. doi: 10.4103/0972-0707.45247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kirkevang LL, Vaeth M, Wenzel A. Prevalence and incidence of caries lesions in relation to placement and replacement of fillings: a longitudinal observational radiographic study of an adult Danish population. Caries Research. 2009;43:286–293. doi: 10.1159/000217861. [DOI] [PubMed] [Google Scholar]
- 26.Gordan VV, Riley IIIJ, Blaser PK, Mjör IA. Two-year clinical evaluation of alternative treatments to replacement of defective amalgam restorations. Operative Dentistry. 2006;31:418–425. doi: 10.2341/05-112. [DOI] [PubMed] [Google Scholar]
- 27.Gordan VV, Riley JL, III, Blaser PK, Mondragon E, Garvan CW, Mjor IA. Alternative treatments to replacement of defective amalgam restorations: Results of a 7-year clinical study. Journal of the American Dental Association. 2011;142:842–849. doi: 10.14219/jada.archive.2011.0274. [DOI] [PubMed] [Google Scholar]
- 28.Fernandez EM, Martin J, Angel PA, Mjor IA, Gordan VV, Moncada G. Survival rate of sealed, refurbished and repaired defective restorations: 4-year follow-up. Brazilian Dental Journal. 2011;22:134–139. doi: 10.1590/s0103-64402011000200008. [DOI] [PubMed] [Google Scholar]
- 29.Roggenkamp CL, Berry FA, Lu H. In vitro bond strengths of amalgam added to existing amalgams. Operative Dentistry. 2010;35:314–323. doi: 10.2341/09-180-L. [DOI] [PubMed] [Google Scholar]
- 30.Ozcan M, Schoonbeek G, Gökçe B, Cömlekoglu E, Dündar M. Bond strength comparison of amalgam repair protocols using resin composite in situations with and without dentin exposure. Operative Dentistry. 2010;35:655–662. doi: 10.2341/10-091-L. [DOI] [PubMed] [Google Scholar]
- 31.Shen C, Mondragon E, Mjör IA. Effect of size of defect on the repair strength of amalgam. Quintessence International. 2007;38:464–469. [PubMed] [Google Scholar]
- 32.Gordan VV. In vitro evaluation of finishing margins in the replacement of resin based composite restorations. Journal of Esthetic Dentistry. 2000;12:209–215. doi: 10.1111/j.1708-8240.2000.tb00223.x. [DOI] [PubMed] [Google Scholar]
- 33.Gordan VV. Clinical evaluation of replacement of class v resin based composite restorations. Journal of Dentistry. 2001;29:485–488. doi: 10.1016/s0300-5712(01)00030-6. [DOI] [PubMed] [Google Scholar]
- 34.Gordan VV, Mondragon E, Shen C. Evaluation of the cavity design, cavity depth, and shade matching in the replacement of resin based composite restorations. Quintessence International. 2002;32:273–278. [PubMed] [Google Scholar]
- 35.Tezvergil A, Lassila LV, Yli-Urpo A, Vallittu PK. Repair bond strength of restorative resin composite applied to fiber-reinforced composite substrate. Acta Odontologica Scandinavica. 2004;62:51–60. doi: 10.1080/00016350310008210. [DOI] [PubMed] [Google Scholar]
- 36.Gordan VV, Shen C, Mjor IA. Marginal gap repair with flowable resin-based composites. General Dentistry. 2004;52:390–394. [PubMed] [Google Scholar]
- 37.Bonstein T, Garlapo D, Donarrummo J, Jr, Bush PJ. Evaluation of varied repair protocols applied to aged composite resin. Journal of Adhesive Dentistry. 2005;7:41–49. [PubMed] [Google Scholar]
- 38.Loomans BA, Cardoso MV, Roeters FJ, Opdam NJ, De Munck J, Huysmans MC, Van Meerbeek B. Is there one optimal repair technique for all composites? Dental Materials. 2011;27:701–709. doi: 10.1016/j.dental.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 39.Ozcan M, Koolman C, Aladag A, Dündar M. Effects of different surface conditioning methods on the bond strength of composite resin to amalgam. Operative Dentistry. 2011;36:318–325. doi: 10.2341/10-294-L. [DOI] [PubMed] [Google Scholar]
- 40.Hamano N, Chiang YC, Nyamaa I, Yamaguchi H, Ino S, Hickel R, Kunzelmann KH. Effect of different surface treatments on the repair strength of a nanofilled resin-based composite. Dental Materials J. 2011;30:537–545. doi: 10.4012/dmj.2010-202. [DOI] [PubMed] [Google Scholar]
- 41.Loomans BA, Cardoso MV, Opdam NJ, Roeters FJ, De Munck J, Huysmans MC, Van Meerbeek B. Surface roughness of etched composite resin in light of composite repair. Journal of Dentistry. 2011;39:499–505. doi: 10.1016/j.jdent.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 42.Gordan VV, Shen C, Riley IIIJL, Mjör IA. Two-year clinical evaluation of alternative treatments to replacement of defective composite restorations. Journal of Esthetic and Restorative Dentistry. 2006;18:144–154. doi: 10.1111/j.1708-8240.2006.00007.x. [DOI] [PubMed] [Google Scholar]
- 43.Gordan VV, Garvan CW, Blaser PK, Mondragon E, Mjor IA. A long-term evaluation of alternative treatments to replacement of resin-based composite restorations: Results of a seven-year study. Journal of the American Dental Association. 2009;140:1476–1484. doi: 10.14219/jada.archive.2009.0098. [DOI] [PubMed] [Google Scholar]
- 44.Moncada G, Martin J, Fernandez E, Hempel MC, Mjor IA, Gordan VV. Sealing, repair and refurbishment of class I and class II defective restorations: a three-year clinical trial. Journal of the American Dental Association. 2009;140:425–432. doi: 10.14219/jada.archive.2009.0191. [DOI] [PubMed] [Google Scholar]
- 45.Rosenstiel SF, Land MF, Rashid RG. Dentists' molar restoration choices and longevity: a web-based survey. Journal of Prosthetic Dentistry. 2004;91:363–367. doi: 10.1016/j.prosdent.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 46.Haj-Ali R, Walker MP, Williams K. Survey of general dentists regarding posterior restorations, selection criteria, and associated clinical problems. General Dentistry. 2005;53:369–375. [PubMed] [Google Scholar]
- 47.Magne P. Composite resins and bonded porcelain: the postamalgam era? Journal of the California Dental Association. 2006;34:135–147. [PubMed] [Google Scholar]
- 48.Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dental Materials. 2007;23:2–8. doi: 10.1016/j.dental.2005.11.036. [DOI] [PubMed] [Google Scholar]
- 49.Makhija S, Gordan VV, Gilbert GH, Litaker MS, Rindal DB, Pihlstrom DJ, Qvist V for The DPBRN Collaborative Group. Practitioner, patient, and caries lesion characteristics associated with type of restorative material: Findings from The Dental PBRN. Journal of the American Dental Association. 2011;142:622–632. doi: 10.14219/jada.archive.2011.0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Christensen GJ. Amalgam vs composite resin. Journal of the American Dental Association. 1998;129(12):1757–1759. doi: 10.14219/jada.archive.1998.0148. [DOI] [PubMed] [Google Scholar]
- 51.Ottenga ME, Mjor I. Amalgam and composite posterior restorations: curriculum versus practice in operative dentistry at a US dental school. Operative Dentistry. 2007;32(5):524–528. doi: 10.2341/06-134. [DOI] [PubMed] [Google Scholar]
- 52.Kikuchi M, Korioth TWP, Hannam AG. The association among occlusal contacts, clenching effort, and bite force distribution in man. Journal of Dental Research. 1997;76:1316–1325. doi: 10.1177/00220345970760061201. [DOI] [PubMed] [Google Scholar]
- 53.Hobson RS, McCabe JF, Hogg SD. Bond strength to surface enamel for different tooth types. Dental Materials. 2001;17:184–189. doi: 10.1016/s0109-5641(00)00068-3. [DOI] [PubMed] [Google Scholar]
- 54.Oztürk B, Malkoç S, Koyutürk AE, Catalbas B, Ozer F. Influence of different tooth types on the bond strength of two orthodontic adhesive systems. European Journal of Orthodontics. 2008;30:407–412. doi: 10.1093/ejo/cjn006. [DOI] [PMC free article] [PubMed] [Google Scholar]


