Abstract
Background
Given the general population prevalence rates of obsessive compulsive disorder (OCD) and the affective disorders, one would expect the co-occurrence of these syndromes to be rare. Yet findings by our group and others have revealed extremely high rates of comorbidity in OCD with both depressive disorders (DD; 50%) and bipolar disorder (BPD; 10%). The current investigation sought to further clarify the role affective disorder comorbidity—particularly that with BPD—may play in the clinical expression of OCD.
Method
A total of 605 individuals with OCD were evaluated with the Structured Clinical Interview for DSM-IV. The sample included three groups: BPD (bipolar I or II; N=79, 13.1%), DD (major depression or dysthymia; N=388, 64.1%), and NAD (no affective disorder comorbidity; N=138, 22.8%). Group-wise comparisons were conducted on comorbidity patterns, impairment measures, and clinical features of OCD. Results: Analyses revealed a graded severity pattern, with the BPD group as the most severe, followed by the DD group, and lastly the NAD group. Severity was reflected by the total number of Axis I disorders (p<0.01), the number of psychiatric hospitalizations (p<0.001), impairment measures (p’s<.05), and OCD symptoms (p<0.01). Of note, the impairment and OCD symptom severity findings were not attributable to the higher level of non-mood disorder comorbidities in the BPD and DD groups.
Conclusion
Those individuals with comorbid affective disorders, particularly BPD, represent a clinically severe group compared to those without such comorbidity. Clarifying the phenomenological features of OCD-affective disorder comorbidity has important etiological and treatment implications.
Keywords: obsessive-compulsive disorder, comorbidity, bipolar disorder, depression, anxiety disorders
Introduction
Obsessive compulsive disorder (OCD) is an anxiety syndrome marked by intrusive and aversive thoughts that are accompanied by repetitive actions or rituals. The symptoms of OCD are distributed continuously on a spectrum from mild to severe [1], and approximately 2% of the population meets diagnostic criteria [2; 3]. OCD is associated with a wide range of psychosocial and occupational impairments and is often extremely distressing to the individuals and their families [4]. Along with a marked heterogeneous symptom profile, substantial comorbidity represents a hallmark feature of OCD. The presence of additional comorbid disorders has been associated with further impairment in functioning [5], greater OCD symptom severity [6], and lower treatment response [7; 8]. Comorbidity with specific disorders also raises important etiological and classification questions [9]. By definitively documenting different comorbidity patterns, researchers can begin to investigate the underlying causes of co-occurrence and subsequently refine the conceptualization of the psychopathology in question [10]. In addition, clarifying comorbidity patterns will allow researchers to examine constellations of common traits, which may, in turn, lead to the identification of common etiological factors [11]. This is particularly germane for detecting clusters of genes that may contribute to comorbid disorders.
Patients with OCD experience elevated comorbidity levels over a wide range of affective, anxiety, and other Axis I disorders, as compared to the general population [12]. In fact, only a small proportion of individuals with OCD, approximately 8%, do not appear to have any comorbid disorders [13]. Considering specifically the affective disorders, one would expect—based on chance alone—relatively low rates of comorbidity: with major depressive disorder (MDD) in only .3% of cases and with bipolar disorder (BPD) in only .04% of cases. In reality the rates are much higher—across the different diagnostic categories, affective syndromes stand out as the most commonly comorbid in samples of OCD. Lifetime major depressive disorder (MDD) affects between 41% and 70% of individuals with OCD [6; 13–16], as compared to 17% of the general population [17]. Bipolar disorder (BPD), which is prevalent in 1.6% of the general population, is also commonly comorbid and affects a reported range of 1–23% of clinical OCD samples [6; 13–16]. The large discrepancy between what would be true based on chance and the actual co-occurrence of these disorders points to the need to further understand the intricate relationships between OCD and the mood disorders.
The most commonly comorbid disorder with OCD is MDD [6; 13; 16], and it has been noted that the two disorders share certain phenomenological features in common, including frequent agitation, indecision, guilt, and other cognitive factors [18; 19]. Although both MDD and OCD respond to similar antidepressants [7], a diagnosis of comorbid MDD with OCD contributes significantly to increased severity of illness [20] and greater rates of additional comorbidity [21]. OCD patients with comorbid MDD have been found to endorse an earlier age of onset of OCD [21], and a recent OCD family study found support for elevated levels of familiality for depressive disorders [22]—two factors that might underlie a genetic predisposition for MDD and OCD.
The potential link between BPD and OCD is also noteworthy. A recent epidemiological investigation of the 12-month prevalence of obsessive compulsive symptoms in Germany found that a diagnosis of OCD was associated with significantly increased chances (OR = 22.6) of also being diagnosed with probable BPD [23]. Likewise, rates of OCD in samples of BPD reveal high comorbidity ranging from 7–21% [24–26]. Past research on OCD-BPD comorbidity has illustrated that patients with OCD and BPD are at elevated risk for high levels of comorbidity with other disorders, including generalized anxiety disorder, social phobia, panic disorder, agoraphobia, and alcohol and substance use disorders [27–31]. From the clinical perspective, there is also an acknowledgement that individuals with OCD and BPD are among the most treatment resistant. Collectively, there is suggestive evidence that patients with OCD-BPD represent a unique group in terms of symptom presentation and impairment [32], and examining this comorbidity may help to elucidate a psychopathological link between the two disorders.
The current report attempts to further clarify the role that affective disorder comorbidity—particularly that with BPD—may play in the clinical expression of OCD. Our primary aim was to consider the clinical impact of affective disorder comorbidity on the phenomenology and clinical features of OCD. A previous investigation by Perugi and colleagues [29] conducted a similar analysis; however, the current report sought to extend that examination by addressing a number of sampling and methodological limitations. In addition to relying on a substantially larger N, our investigation examined a non-treatment seeking OCD population and contrasted three OCD participant groups: (1) those with BPD, (2) those with DD, (3) and those with no affective disorder comorbidity. Factors considered included demographic and treatment variables, comorbidity patterns, measures of impairment and functioning, and clinical features of OCD. Importantly, we controlled for overall (non-mood disorder) comorbidity levels in our group comparisons on impairment and the clinical features of OCD. We hypothesized that BPD group status would be associated with the greatest levels of severity, and that the DD group would be more severe than the NAD group.
Methods
Participants
Subjects for this study included 605 individuals with OCD who were participating in an ongoing family study of OCD genetics conducted by the National Institute of Mental Health (NIMH) Intramural Research Program. All participants were over the age of 18 years and had a lifetime diagnosis of OCD. Participants were excluded if they had active psychosis, severe mental retardation, or OCD symptoms that were only present during episodes of depression. Participants were recruited through the NIMH website, referrals, and newspaper advertisements, and included 363 (60%) women and 242 (40%) men. Most participants were Caucasian (87.8%), but included small groups of Hispanic (2.6%), African American (2%), Asian-American (2.3%), and other participants (3.5%), with a subset of the sample not reporting ethnicity (1.8%). More than half of the sample was college-educated (54.4%), with 7% having earned a graduate degree.
Comorbid Affective Disorder Group Classification
The sample was divided into three groups based on affective disorder comorbidity. The Bipolar Disorder (BPD) group consisted of those individuals with a comorbid diagnosis of either bipolar I (BPI) or bipolar II (BPII). The Depressive Disorder (DD) group was comprised of individuals with comorbid major depressive disorder (MDD) or dysthymia, and the No Affective Disorder (NAD) group included OCD participants with no comorbid affective disorder.
Measures
Demographics
A semi-structured intake interview, conducted either in person or over the phone by a clinically trained interviewer, ascertained participants’ demographic characteristics, including: age, sex, race, education, and marital status.
Treatment Variables
Participants completed a form, on which they indicated past and current usage of medications. The following categories were assessed: benzodiazepines, serotonin reuptake inhibitors (SRIs), tyricyclics, mood stabilizers, and neuroleptics. In addition, as part of the semi-structured intake interview, participants were asked if they had ever received cognitive behavioral therapy (CBT). All indices were coded as yes (1) or no (0).
Structured clinical interview for DSM-IV Axis I Disorders Patient Edition (SCID-P)
Lifetime diagnoses for OCD and other major DSM-IV Axis I disorders were evaluated using the SCID-P [33]. The interview was conducted by a clinically trained interviewer, and two independent reviewers evaluated each SCID in a blind diagnostic procedure to ensure reliability. Past research has found the SCID-P to be a highly reliable diagnostic tool for most Axis I disorders [34]. For the present report, we grouped alcohol abuse and dependence together as alcohol use disorders and combined substance abuse and dependence into substance use disorders. SCID diagnoses demonstrated excellent reliability between interviewers (e.g., kappa for major depression = .93; kappa for anorexia nervosa = .86). OCD diagnoses were also highly reliable with 98% agreement and a kappa of .96.
Additional variables derived from the SCID included: total number of Axis I disorders, which represents a sum of all comorbid disorders, excluding affective disorders; total number of anxiety disorders, which is a sum of all comorbid anxiety disorders; and 3 or more Axis I disorders, a dichotomous (yes=1, no=0) variable that categorizes individuals into a high or low comorbidity group.
Global Assessment of Functioning (GAF)
The GAF scale evaluates an individual’s overall functioning in terms of psychological, occupational, and social domains. The scale is rated from 0 to 100 and has been found to be a reliable and valid measure of psychiatric well-being and disturbance [35–37]. Lifetime worst GAF ratings of 0–100 were determined by clinically trained interviewers based on information gathered during the intake interview and SCID-P.
Impairment Measures
To supplement the GAF impairment ratings, additional questions were asked regarding the following proxy measures for impairment: (1) Income, defined by income above or below $15,000; (2) Disability, defined by not being able to work for a year or more and currently (i.e., at the time of the interview) receiving Social Security Disability Insurance (SSDI); (3) Employment Status, defined as being currently unemployed; and (4) lifetime hospitalization for psychiatric reasons. Indices were coded as yes (1) or no (0).
Yale-Brown Obsessive-Compulsive Scale (YBOCS)
The YBOCS scale consists of 10 items to evaluate the severity of OCD symptoms [38]. The accompanying YBOCS symptom checklist (YBOCS-SC) includes 71 items to evaluate current and lifetime obsessions and compulsions and is divided into 15 clinically derived categories. The current study used the self-report version of the YBOCS, which correlates highly with the clinical interview version [39]. The YBOCS is internally consistent, has high inter-rater reliability, and demonstrates concurrent validity with other measures of OCD symptom severity [38; 40].
Data Analysis
Analyses were conducted using the SPSS 18.0 software package. A two-tailed significance level of p<.05 was set a priori for all tests. For the demographic, treatment, and comorbidity analyses, chi-square and one-way ANOVA tests with Tukey’s post hoc comparison were used to compare categorical and continuous variables, respectively. Odds-ratios (OR) and 95% confidence intervals were used to examine associations with the categorical comorbidity variables. Specifically, we examined the OR for one patient group being associated with a particular comorbidity, with respect to the other two groups, combined. To examine impairment and the clinical features of OCD, we first conducted chi-square and one-way ANOVA tests, followed by analyses that controlled for the total number of non-mood disorder comorbidities. We selected ANCOVA analyses for the continuous outcome variables, and logistic regressions for the categorical outcome variables. Group-wise follow-up comparisons were conducted using dummy coding (BPD=2 vs DD=1; BPD=2 vs NAD=0; DD=1 vs NAD=0).
Results
Prevalence of Affective Comorbidity along with Demographic and Treatment Differences
Of the total sample, 79 participants (13.1%; 51 with BPI and 28 with BPII) were classified in the BPD group, 388 (64.1%; 299 with MDD, 16 with dysthymia, and 73 with both) in the DD group, and 138 (22.8%) in the NAD group. Analysis of demographic variables revealed no significant differences among the three patient groups for sex, race, marital status, and education (Table 1). The DD group was significantly older than the NAD group by 3.6 years (p<.05).
Table 1.
General descriptive characteristics and impairment indices of the sample.
| Total Sample | BPD | DD | NAD | Statistic | |
|---|---|---|---|---|---|
| N (%) | 605 | 79 (13.1%) | 388 (64.1%) | 138 (22.8%) | - |
| Socio-demographic variables | |||||
| Age: Mean [Range]a | 39.2 [17–92] | 39.5 [20–81] | 38.3 [17–76] | 41.9 [18–92] | F = 3.44* |
| Sex, female: n (%) | 363 (60.0%) | 51 (64.6%) | 236 (60.8%) | 76 (55.1%) | χ2 = 2.19 |
| Caucasian: n (%) | 531 (89.4%) | 71 (92.2%) | 341 (88.8%) | 119 (89.5%) | χ2 = .786 |
| Married: n (%) | 236 (40.8%) | 26 (33.8%) | 148 (39.7%) | 62 (48.1%) | χ2 = 4.59 |
| College graduate: n (%) | 328 (54.2%) | 47 (59.5%) | 203 (52.3%) | 78 (56.5%) | χ2 = 1.74 |
| Treatment variables n (%) | |||||
| Any treatment | 521 (86.1%) | 71 (89.9%) | 346 (89.2%) | 104 (75.4%) | χ2 = 17.32*** |
| CBT | 169 (27.9%) | 19 (24.1%) | 120 (30.9%) | 30 (22.7%) | χ2 = 4.95 |
| Benzo’s | 291 (48.1%) | 47 (59.5%) | 204 (52.6%) | 40 (29.0%) | χ2 = 27.42*** |
| SRI’s | 482 (79.7%) | 67 (84.8%) | 325 (83.8%) | 90 (65.2%) | χ2 = 23.10*** |
| Tricyclics | 133 (22.0%) | 24 (30.4%) | 97 (25.0%) | 12 (8.7%) | χ2 = 19.51*** |
| Mood Stabilizers | 178 (29.4%) | 49 (62.0%) | 107 (27.6%) | 22 (15.9%) | χ2 = 53.15*** |
| Neuroleptics | 193 (31.9%) | 44 (55.7%) | 129 (33.2%) | 20 (14.5%) | χ2 = 40.17*** |
p < .001
p < .05
DD group significantly different than the NAD group (p<.05)
With respect to treatments, 85.8% of the total sample reported receiving either CBT or medications during their lifetime, though only 28.4% endorsed CBT (Table 1). The BPD and DD groups did not differ significantly on endorsement rates for any of the pharmacological agents, with the exception that a greater proportion of the BPD group reported use of mood stabilizers and neuroleptics (all p’s < .001). Both the DD and BPD groups were more likely than the NAD group to endorse any of the medications (all p’s < .001). With respect to CBT, the BPD group did not differ in endorsement rates from either the DD or the NAD group; however, the DD group was significantly more likely to report having received CBT than the NAD group (p < .05).
Differences in Comorbidity
Significant differences among the groups were found for both the total number of anxiety disorders (F=13.94, p <.001) and the total number of comorbid disorders (excluding the affective disorders; F=20.67, p <.001). Post hoc comparisons for both analyses revealed a stepwise severity pattern, wherein the BPD group had a greater number of comorbid disorders than the DD group (p’s < .01), and the DD group had a greater number of comorbid disorders than the NAD group (p’s <.001).
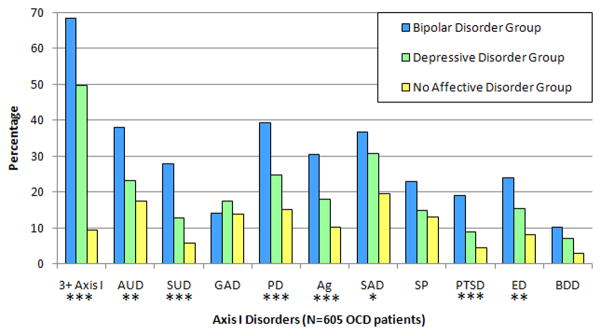
We next examined group differences in comorbidity rates for the separate disorders (see Figure 1). The omnibus chi-square test was significant for alcohol use disorders, substance use disorders, panic disorder, agoraphobia, social anxiety disorder, post-traumatic stress disorder (PTSD), and eating disorders. Table 2 summarizes both the group-by-group chi-square comparisons for these disorders, and the OR’s for one group being associated with a particular comorbidity in contrast to the other two groups. Across analyses, BPD group membership was associated with greater odds of having any given comorbidity than either the DD or the NAD group, with exception of generalized anxiety disorder (GAD). Of particular note, individuals with BPD were over two times as likely to be also diagnosed with substance use disorders (OR = 3.2) and PTSD (OR = 2.9).
Figure 1.
Lifetime comorbidity in OCD/affective disorder subgroups. 3+ Axis I= diagnosis of 3 or more Axis I disorders, excluding affective disorders; AUD = alcohol use disorders; SUD = substance use disorders; GAD= generalized anxiety disorder; PD= panic disorder; Ag= agoraphobia; SAD= social anxiety disorder; SP= specific phobia; PTSD= post traumatic stress disorder; ED= eating disorder; BDD= body dysmorphic disorder. Omnibus chi-square test, ** p < .01, *** p < .001.
Table 2.
Group comparisons of comorbidity.
| Axis I Disorders | OR [95% CI] | χ2 | ||||
|---|---|---|---|---|---|---|
| BPD | DD | NAD | BPD vs DD | BPD vs NAD | DD vs NAD | |
| 3+ comorbid disorders | 2.97 [1.83–4.82] | 1.06 [.073–1.54] | .36 [0.22–0.60] | 13.34*** | 30.87*** | 10.51*** |
| AUD | 2.21 [1.34–3.65] | .91 [0.62–1.34] | .61 [0.37–0.99] | 7.51** | 11.39** | 2.02 |
| SUD | 3.18 [1.81–5.58] | .90 [0.55–1.47] | .34 [0.16–0.73] | 11.79*** | 20.51*** | 4.92* |
| PD | 2.26 [1.38–3.71] | 1.04 [0.71–1.54] | .48 [0.29–0.80] | 6.97** | 15.91*** | 5.34* |
| Ag | 2.30 [1.35–3.91] | 1.04 [0.67–1.60] | .45 [0.25–0.81] | 6.22* | 14.24*** | 4.73* |
| SAD | 1.51 [0.92–2.48] | 1.27 [0.88–1.85] | .52 [0.33–0.83] | 1.11 | 7.71** | 6.26* |
| PTSD | 2.85 [1.49–5.45] | .90 [0.51–1.59] | .39 [0.16–0.93] | 7.31** | 12.32*** | 2.82 |
| ED | 2.03 [1.14–3.60] | 1.14 [0.71–1.83] | .43 [0.22–0.83] | 3.44 | 10.90*** | 4.90* |
p < .05
p < .01
p < .001
Note. AUD = alcohol use disorders; SUD= substance use disorders; GAD= generalized anxiety disorder; PD= panic disorder; Ag= agoraphobia; SAD= social anxiety disorder; SP= specific phobia; PTSD= post traumatic stress disorder; ED= eating disorder; BDD= body dysmorphic disorder
Differences on Impairment Measures
Initial chi-square analyses revealed that the BPD group was overall more impaired than either the DD or the NAD group (Table 3). After taking into account the total number of non-mood disorder comorbidites, significant differences remained for GAF, unemployment, income, and hospitalization. Closer inspection revealed a step-wise severity relationship for GAF lifetime worst functioning, with the BPD group having significantly lower GAF scores than the DD group (p<.01) and the DD group having lower scores than the NAD group (p<.01). The BPD group was more likely to report an income of less than $15,000 and be unemployed than either the DD (all p’s<.05) or the NAD (all p’s<.05) groups. The DD and NAD groups did not significantly differ from one another on income or unemployment. The final impairment measure considered was endorsement of hospitalization for psychiatric reasons. Over half of BPD participants reported hospitalization, and as with the GAF comparisons, a step-wise severity relationship was noted, even after taking into account comorbidity levels. Specifically, the BPD group was significantly more likely to have been hospitalized than the DD group (p<.001), which in turn was more likely to have been hospitalized than the NAD group (p<.001).
Table 3.
Group means and rates for impairment measure and features of OCD, along with test statistic for group comparisons controlling for non-mood disorder comorbidity levels.
| Rates and Means
|
Group Comparisons
|
|||||
|---|---|---|---|---|---|---|
| BPD | DD | NAD | Initial | Controlling for Comorbidity | ||
| Test statistic | Test statistic | Group-wise differences (p < .05) | ||||
| Impairment Features | ||||||
| GAF worst: M(SD) | 39.4 (19.4) | 46.1 (17.0) | 57.0 (12.4) | F = 24.0*** | F = 21.0*** | NAD > DD > BPD |
| Income, ≤15K: n (%) | 21 (26.6%) | 59 (15.2%) | 17 (12.3%) | χ2 = 8.1* | OR= 1.6* | BPD > DD = NAD |
| Disability: n (%) | 11 (13.9%) | 18 (4.6%) | 6 (4.3%) | χ2 = 11.1** | OR=1.8 | |
| Unemployed: n (%) | 27 (34.2%) | 67 (17.3%) | 17 (12.3%) | χ2 = 16.9*** | OR= 1.8*** | BPD > DD = NAD |
| Psych Hosp: n (%) | 46 (58.2%) | 120 (30.9%) | 19 (13.8%) | χ2 = 46.8*** | OR= 2.9*** | BPD > DD > NAD |
| OCD Features | ||||||
| OCD age at onset | 12.7 (8.0) | 13.9 (8.8) | 13.8 (10.1) | F = .7 | F = .8 | |
| YBOCS: M (SD) | 22.7 (9.8) | 21.7 (8.6) | 18.2 (8.5) | F = 8.3*** | F = 4.9** | BPD = DD > NAD |
| YBOCS-obs: M (SD) | 11.3 (5.5) | 11.6 (4.7) | 9.4 (4.8) | F = 7.7*** | F = 5.3** | BPD = DD > NAD |
| YBOCS-comp: M (SD) | 11.6 (5.0) | 10.7 (4.6) | 9.4 (4.4) | F = 5.2** | F = 3.5* | BPD = DD > NAD |
p < .05
p < .01
p < .001
Note. GAF worst = Lifetime worst score on the Global Assessment of Functioning scale (DSM-IV); Psych Hosp = Hospitalization for a psychiatric problem; Disability = Receiving Social Security Disability Insurance (SSDI), as defined by not being able to work for one year or more; YBOCS=Yale-Brown Obsessive Compulsive Scale, total score; YBOCS-obs=total obsession severity; YBOCS-comp=total compulsion severity.
Differences in the Clinical Features of OCD
There was no significant difference in OCD age of onset between groups. OCD severity was analyzed using the YBOCS total, obsessions, and compulsions scores (Table 3). After taking into account comorbidity levels, post hoc analyses revealed that the BPD and DD groups did not differ significantly from one another on any of these indices (p>.05); however, both groups had significantly greater YBOCS total, obsessions, and compulsions scores than the NAD group (all p’s<.05).
We next conducted a series of exploratory analyses to determine whether obsessions or compulsions might be differentially associated with group membership. Three separate logistic regression analyses were built with comorbidity as a covariate, and YBOCS obsessions and compulsions scores entered simultaneously as the primary predictors. We then created three dummy-coded variables that reflected group membership in the BPD, DD, or NAD group (0=no, 1=yes); these variables served as the respective dependent variables for the three regression analyses. Results revealed that YBOCS compulsions significantly predicted BPD group membership (OR = 1.1, p < .05, 95% CI = 1.0–1.2), and YBOCS obsessions significantly predicted DD group membership (OR = 1.1, p < .01, 95% CI = 1.0–1.2).
Differentiating between BPI and BPII
In a series of follow-up analyses, we compared potential differences between BPI and II. Specifically, we compared the DD group to the BPII subset of the BPD group; the two groups did not differ on comorbidity levels of any Axis I disorders, impairment measures, and OCD features. Results indicate that BPI comorbidity was driving the associations reported above.1
Discussion
This investigation focused on the significant ways in which affective disorder comorbidity can influence the expression of OCD, associated features, and additional comorbidity patterns. Our results also speak to the ubiquitous relationship between OCD and affective disorders, as only a quarter of the sample fell in the NAD group. Across analyses, the BPD group emerged as the most severe, as reflected in the increased comorbidity rates with other disorders and greater overall impairment. Results also pointed to a graded pattern, with the DD group being less severe than the BPD group, but more severe than the NAD group. The large sample size of our investigation, along with the relatively high comorbidity with BPD, and the non-treatment seeking nature of our sample, allowed for a more comprehensive investigation that corroborated and extended past reports [27; 29; 31].
Considering the clinical expression of OCD, we found that both the BPD and DD groups had significantly higher YBOCS total, obsessions, and compulsions scores than the NAD group, even after controlling for overall comorbidity levels. This finding suggests that OCD symptom severity increases with the co-occurrence of either BPD or MDD/dysthymia, but that no specific affective disorder is uniquely associated with greater OCD severity. This supports past research that considered each mood disorder separately, and found that BPD and depression in OCD are important factors linked with greater severity [6; 20]. An interesting pattern emerged when we examined the relationships between the three groups and the YBOCS obsessions and compulsions subscale scores. While the DD group was significantly associated with the obsessions scale, the BPD group was linked with the compulsions scale. In line with these findings, previous research found that symptoms of depression are uniquely associated with obsessions, in contrast to compulsions [41]. Future research should consider the potential relationship between compulsions and BPD.
In examining the comorbidity patterns, several noteworthy findings emerged. First, a graded-severity relationship emerged wherein those with BPD represented the most comorbid group, followed by the DD group. This finding corroborates extant research with both adult and pediatric samples [24; 27; 29]. Second, the BPD group was over twice as likely to also be comorbid with panic disorder, agoraphobia and PTSD compared to the DD and NAD groups. The greater incidence of panic disorder among those with both OCD and BPD is mirrored in other investigations [24; 29; 32; 42], and speaks to the intriguing possibility of a tri-disorder relationship. Although less work has been conducted on the association between PTSD, OCD, and affective disorders, studies suggest that patients with BPD may be at increased risk for PTSD, especially due to the increased likelihood of experiencing trauma [43–45]. Third, with respect to alcohol and substance use disorders, the BPD group was substantially more likely to meet criteria than either the DD or the NAD group. These results correspond to past research on the high frequency of alcohol and substance use disorders among BPD [46; 47] and OCD with BPD [29] patients.
Our findings suggest that it was comorbidity with BPI that primarily accounted for the association with severity, in contrast to comorbidity with BPII. When individuals with BPII were considered separately from those with BPI, they displayed similar severity and comorbidity patterns as those in the DD group. However, these results may be due to the relatively smaller number of participants in our sample who had BPII (n=28), as compared to those with BPI (n=51). The one other study that conducted a similar comparison based on affective comorbidity, relied on a sample with primarily BPII and found comparable comorbidity patterns as in our investigation [29]. Given that the latter report did not directly compare BPI to BPII patients, and furthermore did not examine symptom severity between those with BPD and depression, we cannot speak further to the potential lack of concordance between investigations. What does emerge from these findings is that future research is needed to clarify the relationship of OCD with BPI, BPII, and MDD.
The implications of this research are limited by the cross-sectional design employed. Longitudinal investigations could provide valuable information regarding the onsets of each disorder, which would help clarify the relationship between them. A longitudinal design would also be informative for elucidating the role BPD comorbidity may have on the course of OCD. Some research has suggested that BPD may contribute to a more episodic course for OCD, sometimes referred to as cyclothymic OCD [25; 28; 48]. A second limitation is that we did not examine specific factors that could account for the comorbidity patterns noted. Future research should be well aimed at exploring potential psychological or biological factors, along with specific comorbidity models [10], that could provide a more nuanced understanding of the relationship between OCD, BPD, and depression.
In addition to etiological implications, a number of treatment and intervention research considerations emerge. Although efficacious psychological and pharmacological treatments have been developed for both OCD and the affective disorders, little research has considered outcomes when these disorders are comorbid. Our findings point to the relatively high frequency with which individuals with OCD have either BPD or MDD/dysthymia, and it would therefore be advantageous to develop more specific treatment guidelines. For example, in the treatment of OCD and BPD, treatment providers may consider combining medications for BPD with cognitive behavioral interventions for OCD [49; 50]. This is particularly poignant given our findings that less than 30% of the sample endorsed having had CBT during their lifetime, and those with depression were more likely to have received it.
In conclusion, the current report underscores the significant ways in which the presence of a comorbid affective disorder may hinder the general functioning and well-being of individuals with OCD. The relationships noted in this study raise a number of intriguing etiological and treatment implications that should be considered further. For example, although our data are suggestive that it was mood disorder comorbidity that was responsible for the increased clinical severity noted, it is also possible that the relationship is indirect and the result of additional factors, such as potential related endophenotypes. Genetic investigations focused on this OCD-affective disorder relationship—particularly that with BPD—may also be warranted and of interest. It should be noted that while there exists some data reporting incidence of OCD in patients with BPD [e.g. 47] and MDD [20], there does not seem to be as detailed of an evaluation of the influence of comorbid OCD in the affective disorders.
Acknowledgments
This research was supported by the Intramural Research Program of the NIMH, NIH. We thank F. J. McMahon for helpful discussions, as well as T. DeGuzman, B. L. Justement and D. Kazuba for their contributions to this research.
Footnotes
If desired, readers can request additional information on these analyses from the first author.
References
- 1.Olatunji BO, Williams BJ, Haslam N, et al. The latent structure of obsessive-compulsive symptoms: a taxometric study. Depress Anxiety. 2008;25(11):956–68. doi: 10.1002/da.20387. [DOI] [PubMed] [Google Scholar]
- 2.Angst J, Gamma A, Endrass J, et al. Obsessive-compulsive severity spectrum in the community: prevalence, comorbidity, and course. European Archives of Psychiatry and Clinical Neuroscience. 2004;254(3):156–64. doi: 10.1007/s00406-004-0459-4. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey. Replication Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 4.Lopez AD, Murray CC. The global burden of disease, 1990–2020. Nat Med. 1998;4(11):1241–3. doi: 10.1038/3218. [DOI] [PubMed] [Google Scholar]
- 5.Angst J, Gamma A, Endrass J, et al. Obsessive-compulsive syndromes and disorders: significance of comorbidity with bipolar and anxiety syndromes. Eur Arch Psychiatry Clin Neurosci. 2005;255(1):65–71. doi: 10.1007/s00406-005-0576-8. [DOI] [PubMed] [Google Scholar]
- 6.Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(1):53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan A, Hollander E. A review of pharmacologic treatments for obsessive-compulsive disorder. Psychiatr Serv. 2003;54(8):1111–8. doi: 10.1176/appi.ps.54.8.1111. [DOI] [PubMed] [Google Scholar]
- 8.Steketee G, Chambless DL, Tran GQ. Effects of axis I and II comorbidity on behavior therapy outcome for obsessive-compulsive disorder and agoraphobia. Compr Psychiatry. 2001;42(1):76–86. doi: 10.1053/comp.2001.19746. [DOI] [PubMed] [Google Scholar]
- 9.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- 10.Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–33. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grados MA, Walkup J, Walford S. Genetics of obsessive-compulsive disorders: new findings and challenges. Brain and development. 2003;25 (Suppl 1):S55–61. doi: 10.1016/s0387-7604(03)90010-6. [DOI] [PubMed] [Google Scholar]
- 12.Murphy DL, Timpano KR, Wheaton MG, et al. Obsessive-compulsive disorder and its related disorders: a reappraisal of obsessive-compulsive spectrum concepts. Dialogues Clin Neurosci. 2010;12(2):131–48. doi: 10.31887/DCNS.2010.12.2/dmurphy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LaSalle VH, Cromer KR, Nelson KN, et al. Diagnostic interview assessed neuropsychiatric disorder comorbidity in 334 individuals with obsessive-compulsive disorder. Depress Anxiety. 2004;19(3):163–73. doi: 10.1002/da.20009. [DOI] [PubMed] [Google Scholar]
- 14.Nestadt G, Samuels J, Riddle MA, et al. The relationship between obsessive-compulsive disorder and anxiety and affective disorders: results from the Johns Hopkins OCD Family Study. Psychol Med. 2001;31(3):481–7. doi: 10.1017/s0033291701003579. [DOI] [PubMed] [Google Scholar]
- 15.Nestadt G, Di CZ, Riddle MA, et al. Obsessive-compulsive disorder: subclassification based on co-morbidity. Psychol Med. 2009;39(9):1491–501. doi: 10.1017/S0033291708004753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miguel EC, Ferrao YA, Rosario MC, et al. The Brazilian Research Consortium on Obsessive-Compulsive Spectrum Disorders: recruitment, assessment instruments, methods for the development of multicenter collaborative studies and preliminary results. Rev Bras Psiquiatr. 2008;30(3):185–96. doi: 10.1590/s1516-44462008000300003. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 18.Insel TR. Obsessive compulsive disorder-five clinical questions and a suggested approach. Compr Psychiatry. 1982;23(3):241–51. doi: 10.1016/0010-440x(82)90072-4. [DOI] [PubMed] [Google Scholar]
- 19.Abramowitz JS, Storch EA, Keeley M, Cordell E. Obsessive-compulsive disorder with comorbid major depression: what is the role of cognitive factors? Behav Res Ther. 2007;45(10):2257–67. doi: 10.1016/j.brat.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Quarantini LC, Torres AR, Sampaio AS, et al. Comorbid major depression in obsessive-compulsive disorder patients. Compr Psychiatry. 2010 doi: 10.1016/j.comppsych.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Hong JP, Samuels J, Bienvenu OJ, 3rd, et al. Clinical correlates of recurrent major depression in obsessive-compulsive disorder. Depress Anxiety. 2004;20(2):86–91. doi: 10.1002/da.20024. [DOI] [PubMed] [Google Scholar]
- 22.Bienvenu O, Samuels J, Wuyek L, et al. Is obsessive-compulsive disorder an anxiety disorder, and what, if any, are spectrum conditions? A family study perspective. Psychological Medicine. doi: 10.1017/S0033291711000742. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adam Y, Meinlschmidt G, Gloster AT, Lieb R. Obsessive-compulsive disorder in the community: 12-month prevalence, comorbidity and impairment. Soc Psychiatry Psychiatr Epidemiol. 2011 doi: 10.1007/s00127-010-0337-5. [DOI] [PubMed] [Google Scholar]
- 24.Chen YW, Dilsaver SC. Comorbidity for obsessive-compulsive disorder in bipolar and unipolar disorders. Psychiatry Res. 1995;59(1–2):57–64. doi: 10.1016/0165-1781(95)02752-1. [DOI] [PubMed] [Google Scholar]
- 25.D’Ambrosio V, Albert U, Bogetto F, Maina G. Obsessive-compulsive disorder and cyclothymic temperament: an exploration of clinical features. J Affect Disord. 2010;127(1–3):295–9. doi: 10.1016/j.jad.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 26.Kruger S, Braunig P, Cooke RG. Comorbidity of obsessive-compulsive disorder in recovered inpatients with bipolar disorder. Bipolar Disord. 2000;2(1):71–4. doi: 10.1034/j.1399-5618.2000.020111.x. [DOI] [PubMed] [Google Scholar]
- 27.Joshi G, Wozniak J, Petty C, et al. Clinical characteristics of comorbid obsessive-compulsive disorder and bipolar disorder in children and adolescents. Bipolar Disord. 2010;12(2):185–95. doi: 10.1111/j.1399-5618.2010.00795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Magalhaes PV, Kapczinski NS, Kapczinski F. Correlates and impact of obsessive-compulsive comorbidity in bipolar disorder. Compr Psychiatry. 2010;51(4):353–6. doi: 10.1016/j.comppsych.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Perugi G, Akiskal HS, Pfanner C, et al. The clinical impact of bipolar and unipolar affective comorbidity on obsessive-compulsive disorder. J Affect Disord. 1997;46(1):15–23. doi: 10.1016/s0165-0327(97)00075-x. [DOI] [PubMed] [Google Scholar]
- 30.Perugi G, Toni C, Frare F, et al. Obsessive-compulsive-bipolar comorbidity: a systematic exploration of clinical features and treatment outcome. J Clin Psychiatry. 2002;63(12):1129–34. [PubMed] [Google Scholar]
- 31.Tukel R, Meteris H, Koyuncu A, et al. The clinical impact of mood disorder comorbidity on obsessive-compulsive disorder. Eur Arch Psychiatry Clin Neurosci. 2006;256(4):240–5. doi: 10.1007/s00406-006-0632-z. [DOI] [PubMed] [Google Scholar]
- 32.Koyuncu A, Tukel R, Ozyildirim I, et al. Impact of obsessive-compulsive disorder comorbidity on the sociodemographic and clinical features of patients with bipolar disorder. Compr Psychiatry. 2010;51(3):293–7. doi: 10.1016/j.comppsych.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 33.First MB, Spitzer RL, Gibbon M, Williams JBW. Sturctured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- 34.Segal DL, Hersen M, Van Hasselt VB. Reliability of the Structured Clinical Interview for DSM-III-R: an evaluative review. Compr Psychiatry. 1994;35(4):316–27. doi: 10.1016/0010-440x(94)90025-6. [DOI] [PubMed] [Google Scholar]
- 35.Jones SH, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF) Br J Psychiatry. 1995;166(5):654–9. doi: 10.1192/bjp.166.5.654. [DOI] [PubMed] [Google Scholar]
- 36.Piersma HL, Boes JL. The GAF and psychiatric outcome: a descriptive report. Community Ment Health J. 1997;33(1):35–41. doi: 10.1023/a:1022413110345. [DOI] [PubMed] [Google Scholar]
- 37.Sohlberg S. There’s more in a number than you think: new validity data for the Global Assessment Scale. Psychol Rep. 1989;64(2):455–61. doi: 10.2466/pr0.1989.64.2.455. [DOI] [PubMed] [Google Scholar]
- 38.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46(11):1006–11. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 39.Steketee G, Frost R, Bogart K. The Yale-Brown Obsessive Compulsive Scale: interview versus self-report. Behav Res Ther. 1996;34(8):675–84. doi: 10.1016/0005-7967(96)00036-8. [DOI] [PubMed] [Google Scholar]
- 40.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989;46(11):1012–6. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- 41.Ricciardi J, McNally R. Depressed Mood is Related to Obsessions, But Not to Compulsions, in Obsessive-Compulsive Disorder. J Anxiety Disord. 1995;9(3):249–256. [Google Scholar]
- 42.Zutshi A, Kamath P, Reddy YC. Bipolar and nonbipolar obsessive-compulsive disorder: a clinical exploration. Compr Psychiatry. 2007;48(3):245–51. doi: 10.1016/j.comppsych.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 43.Assion HJ, Brune N, Schmidt N, et al. Trauma exposure and post-traumatic stress disorder in bipolar disorder. Social Psychiatry and Psychiatric Epidemiology. 2009;44(12):1041–1049. doi: 10.1007/s00127-009-0029-1. [DOI] [PubMed] [Google Scholar]
- 44.Dilsaver SC, Benazzi F, Akiskal HS, Akiskal KK. Post-traumatic stress disorder among adolescents with bipolar disorder and its relationship to suicidality. Bipolar Disord. 2007;9(6):649–55. doi: 10.1111/j.1399-5618.2007.00396.x. [DOI] [PubMed] [Google Scholar]
- 45.Pollack MH, Simon NM, Fagiolini A, et al. Persistent posttraumatic stress disorder following September 11 in patients with bipolar disorder. J Clin Psychiatry. 2006;67(3):394–9. doi: 10.4088/jcp.v67n0309. [DOI] [PubMed] [Google Scholar]
- 46.Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Archives of General Psychiatry. 2007;64(5):543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Potash JB, Toolan J, Steele J, et al. The bipolar disorder phenome database: A resource for genetic studies. American Journal of Psychiatry. 2007;164(8):1229–1237. doi: 10.1176/appi.ajp.2007.06122045. [DOI] [PubMed] [Google Scholar]
- 48.Hantouche EG, Angst J, Demonfaucon C, et al. Cyclothymic OCD: a distinct form? J Affect Disord. 2003;75(1):1–10. doi: 10.1016/s0165-0327(02)00461-5. [DOI] [PubMed] [Google Scholar]
- 49.Foa EB. Cognitive behavioral therapy of obsessive-compulsive disorder. Dialogues Clin Neurosci. 2010;12(2):199–207. doi: 10.31887/DCNS.2010.12.2/efoa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Provencher MD, Hawke LD, Thienot E. Psychotherapies for comorbid anxiety in bipolar spectrum disorders. J Affect Disord. 2010 doi: 10.1016/j.jad.2010.10.040. [DOI] [PubMed] [Google Scholar]