Abstract
Objectives
In this paper, we describe the first phase of a research project designed to quantify the role of race and cultural identity in HIV-related stigma. The ultimate purpose is to develop an intervention that could be implemented in Black and Colored communities in Cape Town, South Africa.
Design
The PEN-3 model provided the theoretical basis for this research. A total of 397 Black and Colored participants were recruited from two communities to complete a 16-item multi-part questionnaire that was developed based on focus groups and key informant interviews. A total of 196 questionnaires were administered in Mitchell’s Plain and 201 were administered in Gugulethu. Both communities are located approximately 20 km outside the city of Cape Town in an area known as the Cape Flats. Data were collected on individuals’ perceptions of stigma in the contexts of the family, healthcare settings, and the community. However, only the family context is explored here. Participants were also asked to identify what they felt should be the most important area of emphasis for researchers in eliminating stigma. Similarities and differences in perceptions between Black and Colored South Africans were examined.
Results
Data were compiled on the family support domain of stigma. Though most either disagreed or were neutral, nearly equal numbers of Blacks and Coloreds thought stigma occurred in families. Blacks were also more likely than Coloreds to report experiencing stigma in their families. Both Blacks and Coloreds felt the family should be the most important focus of interventions for eliminating HIV-related stigma.
Conclusion
Within the context of the family race, cultural values, and religious and spiritual values all contribute to HIV stigma in South Africa. Interventions should address the role of stigma within families in order to promote better HIV prevention, treatment, and care.
Keywords: HIV/AIDS, race, stigma, family, South Africa
Introduction
Though numerous efforts have been made over the last several years to address the HIV/AIDS epidemic through educational and policy changes (Herek 1999, Shisana et al. 2005, Simbayi et al. 2007), many countries and regions throughout the world have experienced little or no change in their infection rates, and subsequent deaths. South Africa has the highest prevalence of persons living with HIV or AIDS (PLWHA) in the world. An estimated 10.8% of all South Africans over 2 years old were living with HIV in 2005. Among those between 15 and 49 years, the prevalence was 16.2%. Females are much more likely than males to have HIV, and Black Africans and Coloreds make up the overwhelming majority of current HIV and AIDS cases (Shisana et al. 2005).
HIV/AIDS-related stigma is a key factor that contributes to the difficulties in controlling the pandemic. This pandemic has been reported to be a key factor in South Africa’s perceptions and attitudes toward AIDS. AIDS-related stigma is defined as ‘prejudice, discounting, discrediting, and discrimination directed at people perceived to have AIDS or HIV, and the individuals, groups, and communities with which they are associated’ (Herek 1999, p. 1107). This results in a number of negative health behaviors, such as not seeking voluntary testing, which in turn means that those who are positive, may not know to seek appropriate treatment, care, and support.
Stigma has had particular implications for South Africa given its history of racist apartheid and other stigmatizing practices (Skinner and Mfecane 2004). Apartheid was a system of segregationist laws based on policies of racial oppression against Black and Colored individuals. This system, promulgated by the White minority, not only led to strained race relations, but also to inequities in income, housing, education, and health (South Africa 2009).
A stigmatized person is often labeled as powerless, thus creating greater differences and diminishing that group or person’s social status and self worth (Link and Phelan 2002). According to Goffman (1963), stigma is an attribute that is deeply discrediting within a particular social interaction. He saw stigma as a discrepancy between social expectations and reality, which leads to a spoiled identity by preventing the stigmatized person from meeting the expectations of particular kinds of social interactions. However, Goffman (1963) stressed that stigma is not inherently an attribute. Rather, it is inherent in social interactions where the attribute is relevant to the participants’ expectations of the other person. In contemporary times, stigma has come to denote any sort of socially undesirable characteristic. For example, stigmatized individuals are members of social groups ‘about which others hold negative attitudes, stereotypes, and beliefs, or which, on average, receive disproportionately poor interpersonal or economic outcomes relative to members of the society at large because of discrimination against members of the social category’ (Crocker and Major 1989, p. 609). The devaluation of identity and discrimination associated with HIV-related stigma do not occur naturally. Rather, they are socially constructed by individuals and communities, who for the most part, generate stigma as a response to their own fears (Health Resources Services Administration [HRSA] 2003). It is hypothesized that eliminating stigma in the family is pivotal to eliminating stigma in general. However, the source of stigma in the family is important to uncover.
Defining the ‘family’ in HIV/AIDS research is difficult at best. The various contextual uses of the term make it clear that there is no consensus as to what constitutes the family. It is clear, however, that HIV affects social networks beyond the ‘nuclear family’ (usually comprised of two parents and their children in the same household; Bor et al. 1993). The social networks of African families (which often make up the ‘extended family’) are of particular interest to this research. According to Kayongo-Male and Onyango (1984), the extended family has important functions with regard to production, economic and social support, and socialization of new members. It may also be characterized by several key features: the extended family is a kinship-based group usually living in close proximity, it can identify a common household head, it recognizes reproduction as being central to the survival of the group, and it cooperates in economic matters, among other things. Overall, the family can often be thought of as a cohesive unit made up of members who share strong emotional ties that promote sharing and mutual dependence (Bharat and Aggleton 1999, Krishna et al. 2005).
Families function according to different sets of cultural values. For individual families these may include things such as specific customs to honor deceased family members, sharing food to show friendship and compassion, or participating in acts of charity. Families may also subscribe to a set of shared values that are part of the culture of society. These may include things like celebratory customs, work ethic, or the value placed on education and wealth. Religion and spirituality are important aspects of a given culture and often determine which values a family adheres to. They can be more or less influential than other cultural values. While cultural values are not necessarily exclusive of religion and spirituality, they can be employed differently within families when it comes to making decisions – for our purposes – relative to HIV/AIDS. For example, a family’s cultural values may dictate that the infected family member deserves the highest level of care and compassion from her relatives regardless of affliction simply because she is part of the family. However, if a family’s religious beliefs dictate that a lack of morality is the cause of HIV/AIDS, they may conflict with the notion of providing care and support and instead lead to stigmatization.
Race and stigma
It is not difficult to appreciate the fact that social conditions are important in determining exposure to disease (Packard 1990, Farmer 1999). Race, in contemporary society, is not only a social construction (Jones et al. 2008), but is also a means of social control that serves to perpetuate economic, social, and political inequality (Krieger 2000, Coates 2003). Thus, race can be thought of as ‘a process of structured events which over time demonstrate a system whereby groups and individuals are racialized’ (Coates 2006, p. 5). This lends credence to the socio-historical frame of reference with which race must be examined in relation to social conditions, including population health status. Historically, the concept of race in South Africa has played out in the form of hierarchical differentiation and discriminatory practices that were fueled by the political and economic environment of the country’s apartheid regime (Charasse-Pouele and Fournier 2006, Williams et al. 2008). The economic structures and political processes that foregrounded the country’s history make the reality of certain health disparities evident (Campbell and Williams 1999).
Fassin (2001) asserts that humans live within a social order characterized by hierarchies and inequalities, and that AIDS, therefore, can be viewed as a social condition that not only unites human beings in common suffering, but also divides them in terms of exposure to risk and access to treatment (Fassin 2003). Other factors leading to disparities among individuals include the distribution of wealth, the status of women, and health and social policies (Fassin 2003), all of which are frequently laced with racial undertones both in South Africa and in other countries. This racialization of certain health conditions, particularly HIV/AIDS, has created a prime breeding ground for HIV/AIDS-related stigma.
Stigma has been considered by numerous researchers (Herek 2002, Deacon et al. 2005, Airhihenbuwa 2007, Simbayi et al. 2007) to be a barrier to HIV/AIDS prevention and treatment. At the beginning of the pandemic, HIV/AIDS-related stigma was framed as an ‘African disease’ – one from which the rest of the world tries to distance itself (see for example, Patton 1990, Jungar and Oinas 2004). The resulting ‘blaming’ (Petros et al. 2006) that occurs is characteristic of how HIV/AIDS remains constructed as an illness of poor, Black communities, with women receiving much of the blame. This is particularly true in South Africa where racial wounds still fester in the wake of the violence, abandonment, and suffering that characterized the apartheid era. The sweeping representation of Africans as a diseased population, in overly sexualized bodies has led to such stigmatization, and has caused a profound resistance among many Africans to what they see as ‘racist’ AIDS prevention campaigns (Fassin 2003). In addition, a notion of conspiracy against South Africans that is believed to be instigated by the country’s White conservatives or from the pharmaceutical industry reinforced the notion that the AIDS epidemic and its treatments are part of a plot to eradicate the Black population (Fassin and Schneider 2003).
The current study aims to quantify the role of race and identity in HIV/AIDS-related stigma within the context of the family. The research was conducted with two specific aims in mind: (1) to examine the most salient individual and contextual factors that contribute to both non-stigmatizing and stigmatizing behaviors in South Africa; and (2) to recommend critical intervention points of entry (consistent with the PEN-3 model, which is described later under the subheading Theoretical Framework) based on results of the data in which participants were specifically asked to make such a recommendation.
Specifically, we focus on the family and how perceptions are either shared or different between Black African and Colored1 individuals. We also provide a discussion of participants’ thoughts about where they feel researchers should focus their interventions to eliminate the shame and rejection associated with HIV/AIDS.
Theoretical framework
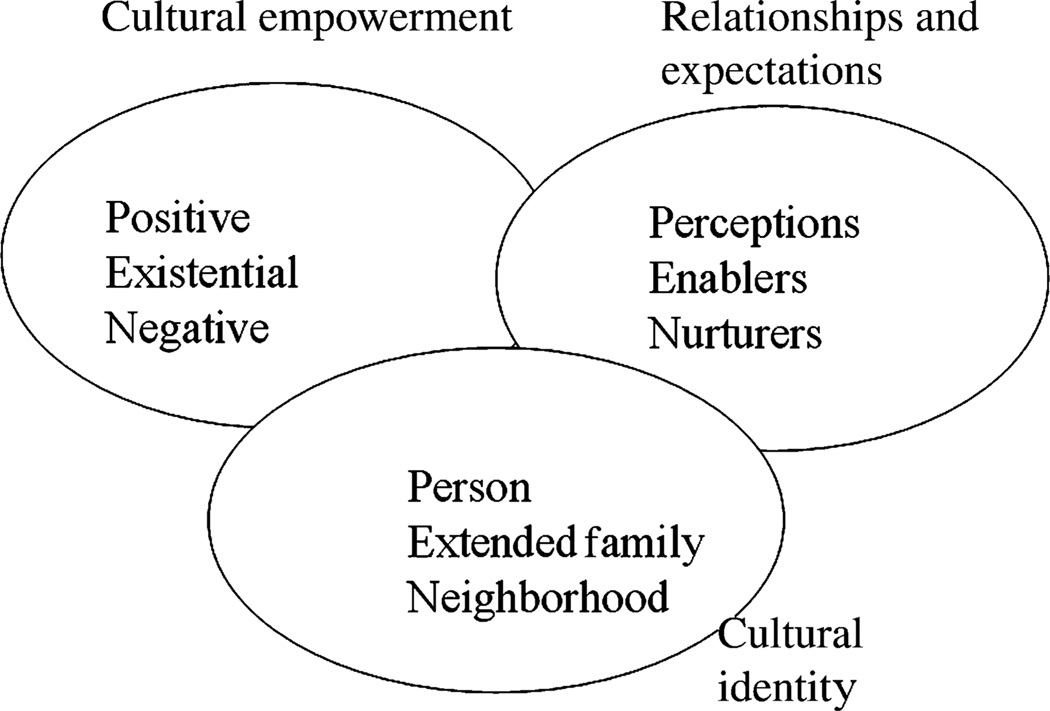
The PEN-3 cultural model provided the theoretical basis for this research. The model was developed by Airhihenbuwa in 1989 to establish a cultural approach to studying health behaviors and their sociocultural contexts with a focus on Africa (Airhihenbuwa 1989; Airhihenbuwa and Webster 2004). The model has been used by researchers to examine the health behaviors that are central to how people establish relationships and formulate their own expectations. PEN-3 is designed to guide the planning of community-based health research, as well as to assist in the analysis of the results of qualitative and quantitative research. It also serves to guide the planning, implementation, and evaluation of health interventions. At the level of research analysis and intervention, the model guides researchers and interventionists in examining cultures from a number of perspectives that range from positive to negative. This inclusion of positive aspects of culture avoids the trap of focusing solely on negative aspects, which typically leads to blaming the failure of programs on aspects of the culture that are misunderstood and ill-defined by the researchers and interventionists (Airhihenbuwa 1989, 1995, 2007). As seen in Figure 1, the model is made up of three interrelated and interdependent dimensions: relationships and expectations (RE); cultural empowerment (CE); and cultural identity (CI). In RE, there are three domains: perceptions (i.e., beliefs and values held by people about a condition); enablers (i.e., resources that either promote or hinder efforts at changing behavior); and nurturers (the role of friends and family in making positive or negative changes). In CE, there are three domains: positive (i.e., identifying positive attributes rather than focusing only on the negatives); existential (i.e., understanding the qualities that make the culture unique but that should not be blamed for program failure); and negative (i.e., values and behaviors that contribute to health problems). In CI, there are also three domains: person (i.e., focusing on the one person who may have the most impact on health decisions); extended family (i.e., the role of kinship in decisions that may affect one person); and neighborhood (i.e., the context of the community and values that shape health decisions).
Figure 1.
The PEN-3 model.
There are two phases involved in the application of PEN-3: the assessment phase and the intervention phase. In the assessment phase, the domains of the RE and CE dimensions are crossed to create nine cells. During the intervention phase, researchers present their findings and learn from the community before using the three domains of CI to decide on the intervention point of entry. Community engagement is critical to the application of PEN-3 (Airhihenbuwa et al. 2009).
Methods
Sample
Participants were recruited from two communities in Cape Town, Western Cape, South Africa – Gugulethu and Mitchell’s Plain – which lie in an area known as the Cape Flats. Gugulethu is one of the oldest predominantly Black townships in South Africa and is arguably one of the fastest developing. It lies approximately 20 km east of the city of Cape Town and has its roots in the migrant labor system of apartheid South Africa. Mitchell’s Plain, approximately 20 km southeast of Cape Town, is a sprawling, predominantly Colored township originally built to house Coloreds of the middle income group who were forcibly removed from their homes in the city during the apartheid era. It now houses a mixture of lower income residents (i.e., those who may not have enough money for basic goods, like food and clothing) and middle income residents (i.e., those who are mostly of working class and may have enough money for necessary goods like food and clothing, but very few luxury items).
Using a snowball sampling method, the researchers recruited a total of 400 participants to complete the survey in this study (200 from Gugulethu; 200 from Mitchell’s Plain). The participants in Gugulethu were recruited by canvassing the community. All potential participants met at a central location at a pre-determined time to reduce any influence of outside factors on questionnaire responses. In Mitchell’s Plain, participants were recruited by patient advocates who do weekly home visits with clinic patients. They were able to assist with participant recruitment because of their regular and easy access to community members. The participants from Mitchell’s Plain were drawn from a potentially larger area. Different patient advocates were assigned to various geographic areas, essentially providing services to patients in all corners of the township. None of the participants were pre-selected.
Measurement
A 16-item multi-part interview questionnaire was used. The items were based on data from focus groups and key informant interviews in the parent grant (Airhihenbuwa et al. 2009). The questionnaire examined the racial and cultural similarities and differences between Black African and Colored communities in Cape Town, South Africa. The questionnaire, therefore, drew on salient items from published research that locates HIV/AIDS stigma in its historical and cultural contexts in South Africa. We consulted the work of Krieger (2000), Jones (2000), Williams and Collins (2001), and others to develop a measure of the role of race and CI on stigma. The questionnaire included demographic items that measured stigma within the context of three domains of HIV/AIDS stigma: family support; healthcare institutions; and the general community. However, for this paper we only use the family support domain. The questions used for assessment of family support and stigma are:
Family support and stigma (all responses – Agree, Disagree, Neutral/Don’t Know)
The reason people shame their family members living with HIV/AIDS, is because of their cultural values.
The reason people shame their family members living with HIV/AIDS, is because of their religious and spiritual values.
The conceptual difference between these two levels of family support has been discussed in the introduction. Linear transformations were conducted to obtain a continuous domain score composed of both items. Transformed variables were averaged within the domain score. Both domain items were linearly transformed to represent a score from 0 to 100. Then the items were averaged. Internal consistency reliability for items in this domain was assessed using Chronbach’s α. A higher composite score indicates that individuals perceived more stigmatizing behavior with regard to the items related to family support.
Participants were also asked to rank three of six possible community entities on the basis of where they thought researchers should place more emphasis in eliminating shame and stigma with regard to HIV/AIDS. Of those three, participants ranked their selections from (highest importance = 1) to (lowest importance = 3). It should be noted that ranking percentages for each entity were not calculated with respect to the other entities. Only rankings within each entity were calculated.
Among the following, where should we place emphasis for eliminating shame and rejection associated with HIV/AIDS? Please rank your top 3 in order of importance
| (1) Family | 1 2 3 |
| (2) Community members | 1 2 3 |
| (3) Hospitals or clinics | 1 2 3 |
| (4) Provincial government | 1 2 3 |
| (5) National government | 1 2 3 |
| (6) Other, please specify | 1 2 3 |
The stigma domain, which we have termed family support, and the ranking of community responsibility for eliminating HIV/AIDS stigma item served as the dependent variables for this study. In this study, family support refers to the multiple levels at which the family directly or indirectly helps another member cope with HIV or AIDS.
Data collection
Participants in the Gugulethu community responded to the questionnaire in a group setting of approximately 20–25 persons at a time. The questionnaire was read aloud in both the English and Xhosa languages, and participants marked their answers using a paper and pencil method. In Mitchell’s Plain, the questionnaire was administered by a group of community patient health advocates. Each patient advocate randomly selected 10 patients with whom they were assigned to conduct regular home visits. If a patient declined to participate in the study, another one was selected. These participants also responded using a paper and pencil method. The questionnaires in Mitchell’s Plain were administered in English, Afrikaans, or Xhosa. All questionnaires were checked for completeness before being collected, and participants from Gugulethu were given a small monetary compensation for their time and to cover transportation costs. Participants in Mitchell’s Plain received compensation for their time as a gesture of fairness according to ethics review protocol. A total of 196 completed questionnaires were collected in Mitchell’s Plain and 201 were collected in Gugulethu. Due to a miscalculation in the recruitment procedure, one additional participant was allowed into the sample from Gugulethu and subsequently completed the questionnaire. Due to the time constraints of the study, the patient health advocates were only able to administer the questionnaire to 196 of 200 originally anticipated individuals in Mitchell’s Plain. None of the questions used for this research study asked participants directly for their HIV status.
Main effect
Race is the independent variable against which all the descriptive and behavioral variables are measured. The currently recognized racial classifications (White, Indian, Colored, and Black African) came out of the apartheid era. While some South Africans reject these classifications, it is understood that they are still important for the purpose of understanding differences in South Africa today and for the challenge of accounting for the historical basis for group relationships today. There is a degree of mixture of the races and certain historical factors that determine self-identity as either Black African or Colored. However, participants identified with a particular racial group in ways that allow us to examine feelings of mistrust, blame, and discrimination both within and between groups.
Other covariates
Dependent variables of interest that were analyzed against racial category include age, education level, location of residence (Gugulethu or Mitchell’s Plain), and language most often spoken at home. There are 11 officially recognized languages in South Africa. However, study participants primarily spoke one or more of the three prominent languages in the province – Afrikaans, Xhosa, or English.
Data analysis
All data were coded from individual surveys into a Microsoft Excel spreadsheet, with each item having an assigned variable name. The data were then imported into the SPSS 15.0 statistical software package. Descriptive statistics were run on the demographic variables, which were stratified by race group. Only the mean and standard deviation for the age of both race groups in the sample were calculated. Cross tabulations were done on each of the other variables in order to determine contextual differences in attitudes and beliefs between race groups, chi-square values were calculated for each cross tabulation. Linear regression models were employed to investigate the relationship between each of the first three stigma domains and the participants’ race, while controlling for age of the participants, gender, and educational level.
Results
A total of 397 participants completed the questionnaire. Basic demographics of the sample are shown in Table 1. All participants were adult men and women at least 18 years of age (mean age = 35.29 years). Among Black Africans in the sample, approximately 57% were female while 63% of Coloreds were female. Approximately 53% of the entire sample lived in Gugulethu, as did two-thirds of the Black Africans. Nearly all (98%) Coloreds in the sample lived in Mitchell’s Plain. A majority of both Black African (85%) and Colored (62%) participants were high school educated. Nearly all of the Black African (96%) participants indicated that Xhosa was the language they most often spoke at home, although English is widely spoken. Coloreds indicated that they spoke exclusively either Afrikaans (79%) or English (21%) at home. Although participants were not asked their HIV status during the study, the sample did include PLWHA, as well as other community members. According to the 2000 Income and Expenditure Survey, the average per capita income in 2000 in the Western Cape was R21,344 (US$2753) (Statistics South Africa 2002). This was due in large part to the economic toll the AIDS pandemic had taken on individuals and communities in South Africa. Therefore, participants from both communities were generally of a disadvantaged socioeconomic background.
Table 1.
Demographic characteristics of sample by race and language.
| Race | Language | ||||||
|---|---|---|---|---|---|---|---|
| Category | Black African, n (%) | Colored, n (%) | All, n (%) | Afrikaans, n (%) | English, n (%) | Xhosa, n (%) | |
| Age | |||||||
| p = 0.539 | Mean | 34.35 | 38.85 | 35.298 | |||
| Std. Deviation | 12.97 | 8.38 | 12.2 | ||||
| Gender | |||||||
| p = 0.230 | Male | 128 (43.2) | 30 (37.0) | 158 (41.9) | 29 (42.0) | 11 (33.3) | 124 (42.3) |
| Female | 168 (56.8) | 51 (63.0) | 219 (58.1) | 40 (58.0) | 22 (66.7) | 169 (57.7) | |
| Site | |||||||
| p = 0.001 | Mitchell’s Plain | 100 (33.7) | 79 (97.5) | 179 (47.4) | 66 (95.7) | 25 (75.8) | 104 (35.4) |
| Gugulethu | 197 (66.3) | 2 (2.5) | 199 (52.6) | 3 (4.3) | 8 (24.2) | 190 (64.6) | |
| Education | |||||||
| p = 0.128 | No formal education | 3 (1.0) | 3 (3.7) | 6 (1.6) | 2 (2.4) | 2 (6.1) | 2 (.7) |
| Primary school | 43 (14.5) | 28 (34.6) | 71 (18.8) | 25 (26.2) | 5 (15.2) | 44 (15.0) | |
| High school or greater | 251 (84.5) | 50 (61.7) | 301 (79.6) | 42 (60.9) | 26 (78.8) | 248 (84.4) | |
| Language most often spoken at home | |||||||
| p = 0.000 | Afrikaans | 1 (.3) | 64 (79.0) | 65 (17.2) | |||
| English | 2 (.7) | 17 (21.0) | 19 (5.0) | ||||
| Xhosa | 285 (96.3) | 0 (.0) | 285 (75.6) | ||||
| Other | 8 (2.7) | 0 (.0) | 8 (2.7) | ||||
Family support and stigma
Results of perceptions of stigma and family support are shown in Table 2. When asked whether they thought people shamed their family members living with HIV/AIDS because of cultural values, the majority of Black Africans disagreed (50%) or were neutral (35%) in their response to this statement. More Coloreds (61%) were neutral in their response, and about one-quarter of them also disagreed with this statement. Asked the same questions, but substituting religious or spiritual values for cultural values, 41% of Black Africans still disagreed compared to 24% who agreed with this statement. However, over half of Coloreds were neutral to this statement, while one-quarter of Coloreds either agreed or disagreed with the statement.
Table 2.
Family support by race and language.
| Race | Language | |||||||
|---|---|---|---|---|---|---|---|---|
| Reason for lack of family support | p-value | Black African, n (%) |
Colored, n (%) |
p-value | Afrikaans, n (%) |
English, n (%) |
Xhosa, n (%) |
|
| People shame their family members living with HIV/AIDS because of cultural values | Agree | 0.000 | 43 (15.4) | 11 (13.9) | 0.013 | 10 (14.8) | 7 (22.6) | 41 (14.9) |
| Disagree | 139 (49.8) | 20 (25.3) | 19 (28.4) | 7 (22.6) | 142 (51.4) | |||
| Neutral/don’t know | 97 (34.8) | 48 (60.8) | 38 (56.7) | 17 (54.8) | 93 (33.7) | |||
| People shame their family members living with HIV/AIDS because of religious/spiritual values | Agree | 0.004 | 66 (23.5) | 20 (25.3) | 0.109 | 18 (26.9) | 7 (21.2) | 64 (23.1) |
| Disagree | 115 (40.9) | 17 (21.5) | 17 (25.4) | 6 (18.2) | 119 (43.0) | |||
| Neutral/don’t know | 100 (35.6) | 42 (53.2) | 32 (47.8) | 20 (60.6) | 94 (33.9) | |||
The Chronbach’s α coefficient for Family support and stigma was α = 0.80. When linear regression was conducted, the calculations revealed that when controlling for age, gender, and education level, being of Black African or Colored race was associated with a greater likelihood (β = 11.712 [2.672, 20.752]) of perceptions of stigma within the family. Age (β = −0.122 [−0.419, 0.175]), gender (β = −0.128 [−7.34, 7.08]), and education level (β = −0.052 [−8.854, 8.750]), however, showed a decreased likelihood of perceived stigma under this domain.
Table 3 presents the sample means and standard deviations for the relationship between family support and stigma. With equal variability in stigmatizing attitudes between both racial groups, there is a significant difference (p = 0.0146, df = 363) between the number of Black Africans and Coloreds who feel that people shame their family members living with HIV/AIDS because of cultural and religious/spiritual values. The mean score of how strongly respondents agree that people shame their family members living with HIV/AIDS due to cultural values or religious/spiritual values is higher among Black Africans than among Coloreds. Therefore, according to the scale of measurement, Black Africans feel more strongly than Coloreds that family members shame PLWHA on the basis of cultural and religious/spiritual values.
Table 3.
Regression analysis of whether respondents agree that families stigmatize PLWHA based on cultural or religious/spiritual values by race, age, gender, and education.
| Race | N | M | Standard Deviation | df | t-value | p-value |
|---|---|---|---|---|---|---|
| Black African | 285 | 57.544 | 33.306 | 0.363 | −2.45 | 0.0146 |
| Colored | 80 | 68.125 | 36.668 | |||
| Independent variables | Whether respondents agree that families stigmatize PLWHA based on cultural or religious/spiritual values (Dependent variable) | |||||
| Beta (β) | p-value | |||||
| Constant | – | 0.000 | ||||
| Race | 0.143 | 0.011 | ||||
| Age | −0.045 | 0.419 | ||||
| Gender | −0.002 | 0.972 | ||||
| Education | −0.001 | 0.991 | ||||
| Model Summary | ||||||
| df | 4, 341 | |||||
| F | 1.806 | |||||
| p-value | 0.127 | |||||
| R2 | 0.021 | |||||
| Adjusted R2 | 0.009 | |||||
Eliminating shame and rejection associated with HIV/AIDS
Table 4 reveals that, given the choice to select where emphasis should be placed for future efforts targeted toward eliminating the shame and rejection associated with HIV/AIDS, both Black Africans and Coloreds ranked the exact same three choices the highest, but not in the exact same order of importance. The family was the top choice of both groups (88% of Black Africans, 64% of Coloreds); hospitals and clinics was the second choice of Black Africans (17.2%) and third choice for Coloreds (14.8%); and national government was the third choice for Black Africans (9.8%) and second choice for Coloreds (17.3%).
Table 4.
Rankings for future emphasis on elimination of stigma by race and language.
| Race | Language | ||||||
|---|---|---|---|---|---|---|---|
| Entity on which to place emphasis for eliminating shame and rejection associated with HIV/AIDS |
p-value |
N=297 Black African, n (% of all) |
N=81 Colored, n (% of all) |
p-value | Afrikaans, n (% of all) |
English, n (% of all) |
Xhosa, n (% of all) |
| Family | |||||||
| % that ranked Family | 0.000 | 286 (96.3) | 76 (93.8) | 0.000 | 65 (94.2) | 30 (90.9) | 284 (96.6) |
| % that ranked as #1 | 261 (87.9) | 52 (64.2) | 43 (62.3) | 27 (81.8) | 260 (88.4) | ||
| Community members | |||||||
| % that ranked Comm | 0.402 | 209 (70.4) | 49 (60.5) | 0.298 | 40 (58.0) | 25 (75.8) | 204 (69.4) |
| % that ranked as #1 | 27 (9.1) | 10 (12.3) | 10 (14.5) | 3 (9.1) | 26 (8.8) | ||
| Hospitals and clinics | |||||||
| % that ranked Hosp | 0.895 | 230 (77.4) | 52 (64.2) | 0.816 | 44 (63.8) | 22 (66.7) | 231 (78.6) |
| % that ranked as #1 | 51 (17.2) | 12 (14.8) | 14 (20.3) | 2 (6.1) | 54 (18.4) | ||
| Provincial government | |||||||
| % that ranked Prv gov | 0.110 | 73 (24.6) | 15 (18.5) | 0.882 | 14 (20.3) | 6 (18.2) | 73 (24.8) |
| % that ranked as #1 | 16 (5.4) | 1 (1.2) | 1 (1.4) | 2 (6.1) | 15 (5.1) | ||
| National government | |||||||
| % that ranked Natl gov | 0.201 | 115 (38.7) | 50 (61.7) | 0.229 | 43 (62.3) | 14 (42.4) | 119 (40.5) |
| % that ranked as #1 | 29 (9.8) | 14 (17.3) | 13 (18.8) | 3 (9.1) | 29 (9.9) | ||
Discussion
This study adds to the existing literature on perceptions of race and HIV-related stigma by examining both within the context of the family in South Africa. The data show that nearly one-quarter of the respondents felt that people shame their family members living with HIV/AIDS because of their religious or spiritual values. This corroborates previous research (Hamra et al. 2006, Neville Miller and Rubin 2007) on HIV/AIDS in the family context, as well as how religion has contributed to blaming others (Otolok-Tanga et al. 2007, Zou et al. 2009). The role that religion and spirituality play in the context of family and its influence on stigmatization of PLWHA requires further study. Cultural values seem to play a lesser role than religious values in family members’ stigmatizing attitudes toward PLWHA.
The family unit in South Africa is often a strong source of social support. It remains the strongest source of support for caring for those who are living with HIV or AIDS (Bor et al. 1993, Iwelunmor et al. 2008). Consistent with the PEN-3 model, we cross the RE and CE domains to determine the various levels at which family systems play a role in supporting members who may be dealing with the issue of HIV/AIDS. Families remain the strongest source of support when caring for members infected with HIV/AIDS. Positive perceptions of familial support are important when it comes to disclosure of one’s HIV status. Research has shown that disclosing one’s status can yield even greater social and emotional support for PLWHA and foster a sense of trust among family members (Bor et al. 1993, Krishna et al. 2005, Iwelunmor et al. 2008). This is an important part of coping with the stress of HIV/AIDS and maintaining trust and mutual respect within the family. Disclosing to family members can also provide another conduit through which information is shared. For example, family members can solicit medical advice and treatment options from doctors on behalf of the PLWHA. Counselors can provide referrals for various social services that may be able to assist PLWHA in a safe and confidential manner. These positive enablers can serve as excellent resources in assisting families affected by HIV/AIDS. Yet another level of support can come in the form of positive nurturers, where family members accompany the ill to clinic visits and support groups. These are ways in which families take positive actions to support HIV-infected relatives.
Despite the heavy toll HIV/AIDS can take, families develop different ways of coping. Their existential perceptions may dictate that family members must come together to discuss the issue before deciding on a course of action to support and care for the infected member. They counsel each other and educate themselves about its consequences (Iwelunmor et al. 2008). Existential enablers may be other community members who step in to fill the role of family member to provide an extra layer of support and security in case the family is unable to access a particular resource. Counselors and social workers may fulfill this role. Existential nurturers are often identified by the PLWHA. This could be someone like the mother or a sibling to whom the PLWHA first disclosed. As a matter of respect and trust, these nurturers would be the first line of support and perhaps the one who discloses the PLWHA’s status to the rest of the family (Iwelunmor et al. 2008).
However, family relations do not always embody the type of emotional support and physical care that PLWHA require. Stress can impact PLWHA through negative perceptions. For example, when families shun PLWHA or keep their status a secret from the rest of the community, this gives the perception that the family is ashamed. Such perceptions are reinforced by negative enablers that prevent a PLWHA from getting the help they need, and therefore, fuels stigmatization by the family. For example, in South Africa if a PLWHA cannot secure the government disability grant for people with HIV and AIDS, it creates a hardship on the family because the infected member is not contributing financially. Therefore, family members become upset, which can create a more stressful situation (Iwelunmor et al. 2008). Families may encounter negative nurturers based on their religious beliefs. Although they may want to be supportive, their values regarding immorality and HIV/AIDS may contradict their intentions, which can impose undue stress on the PLWHA. This is quite relevant to the study we have presented here.
Because the burden of the South African HIV/AIDS epidemic lies mostly within the Black African and Colored communities, exposure to disdainful and stigmatizing attitudes on the basis of one’s HIV status only reduces the likelihood of disclosure. Consequently, it increases the difficulty of finding proper care, treatment, and support in one’s community. A more pessimistic outcome can be argued, given the history of discrimination experienced by Black African and Colored South Africans. Feelings of inferiority, being shunned by family members, and enduring constant racial discrimination can create unbelievably difficult circumstances for PLWHA in South Africa. It is not surprising then, that the large majority of study participants (96% of Black Africans and 94% of Coloreds) felt emphasis needed to be placed on the family – among all possible contexts listed in the questionnaire – for future development of strategies to eliminate shame and rejection associated with HIV/AIDS. Of those, a majority (88% of Black Africans and 64% of Coloreds) felt that the family should be the highest priority when developing and implementing such strategies.
Given the high prevalence of HIV/AIDS in South Africa and the pervasiveness of stigma against PLWHA, there is a pressing need for social and structural interventions to change societal beliefs about PLWHA (Kalichman and Simbayi 2003). Thus far, much of the published research on stigma seems to suggest that interventions have been geared toward reduction of stigma in healthcare settings or in the general community (Brown et al. 2003). When interventions are attempted, they often utilize social marketing techniques like mass media campaigns to raise AIDS awareness and reduce stigma (Blankenship et al. 2000, Kalichman and Simbayi 2003). Many current stigma campaigns are also aimed at promoting antidiscrimination policies and protecting the human rights of PLWHA (Shriver et al. 2000, Kalichman and Simbayi 2003). However, none of them specifically target families of PLWHA in an effort to curb stigma at a level where perhaps the most intimate and familiar relationships occur.
Study limitations
Some important limitations of the study must be considered. First, this was a convenience sample gathered from two townships in Cape Town, South Africa. Geographically speaking, Cape Town is quite large and many of the other existing townships could have yielded an adequate sample. The townships also have varying levels of racial diversity, so generalizations to other geographic areas in Cape Town and throughout South Africa should be made cautiously. Furthermore, individuals from only two South African racial groups – which include many different ethnic groups – were included in this study. There are a number of ethnic groups within those two racial classifications that may not have been included in the study. This special population should, therefore, be considered when reflecting on the existence of HIV/AIDS-related stigma worldwide. While some results were gathered in a group setting and others were gathered individually, they all relied on self report.
The validity of some of the questionnaire items could be challenged because of the underlying assumption that ‘shame’ is imposed by the family. Although it was not the authors’ intent, forcing this assumption on the respondents could have led them to respond to the questionnaire in a certain way. Thus, the response to such items would have been less the honest opinion of the respondent and more a function of the respondent’s inability to indicate a ‘don’t know’ response or to abstain from responding all together. This sort of response bias is a fundamental shortcoming of the research methodology and must be taken into consideration when interpreting and generalizing the results. Additionally, the validity of the responses to the question regarding where researchers should place more emphasis in eliminating shame and stigma could be brought into question. It was the authors’ intent to gather data on the respondents’ top three choices. The instructions indicated that a ranking of ‘3’ meant the corresponding entity was of lowest importance. The respondents could have interpreted this to mean that ‘3’ was least important to them of the six possible choices. Alternatively, the respondents could have listed ‘3’ as their next most important entity for stigma elimination after ‘2’. This was the initial intent of the question. Due to the possible contradiction of responses, it might have been appropriate to exclude the number ‘3’ rankings from the analysis. Re-wording the question will be necessary in future studies utilizing this questionnaire.
Conclusion
Although caution should be used in generalizing to Black and Colored individuals in other areas of Cape Town and in South Africa in general, the results of the study are indicative of a major research gap in interventions on stigma in the family context. Results from the survey and focus groups suggest a strong desire for researchers to focus on family in order to reduce HIV-related stigma, particularly on the basis of their religious and spiritual values, as demonstrated by one-quarter of respondents. This will advance ongoing efforts to reduce the burden of stigma and lead to increased support and better health outcomes for PLWHA. Further study is necessary to fully grasp the social impact that family has on the stigmatization of PLWHA within the cultural contexts of Black and Colored South Africans. PEN-3 does provide a starting point for examining the positive, existential, and negative supporting structures within the family, as well as a point of entry (CI domain) for intervention development (i.e., the extended family). Further study might include more analysis at the spiritual and religious level (e.g., Christian, Muslim, and traditional African religions) to gain a clearer understanding of the source of stigma within families and to inform the type of community-based interventions that may be suitable for tackling spiritually based issues within the family. More specifically, future analysis might examine the way in which particular Christian denominational backgrounds influence the way family members stigmatize PLWHA. As it could be rather costly and time-consuming to launch an intervention directly to families, it might be more reasonable to involve religious and faith-based organizations, as well as adult education centers. These entities may be able to provide some of the community resources necessary to facilitate educational interventions in which families can participate as a collective unit.
Key messages.
The key messages that should be taken from this research are:
Stigma has particular implications for both the spread and reduction of HIV/AIDS in South Africa.
The family is an important context on which researchers should place emphasis for eliminating HIV/AIDS-related stigma.
Religious and spiritual values within the context of the family can be a starting point for developing interventions to reduce stigma.
Acknowledgements
This research was made possible through funding from the National Institute of Mental Health grant #MH 68180. We wish to extend our sincere gratitude to all those in the Guguletu and Mitchell’s Plain communities who helped make this research possible, including the community organizers, patient advocates, and especially the participants themselves.
Footnotes
Full terms and conditions of use: http://www.informaworld.com/terms-and-conditions-of-access.pdf
This article may be used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
Publisher's Disclaimer: The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
Black and Colored are two of the officially recognized race categories in South Africa, which were established during the Apartheid era. Blacks descend from one of several ethnic groups of what were formerly known as Bantus. Coloreds are generally of mixed race, including Bantu, Khoisan, Malay, and European ancestry. Coloreds were oppressed in much the same way as Blacks during Apartheid. While we do not endorse the historical apartheid classification system, these categories continue to be used by the South African
References
- Airhihenbuwa CO. Perspectives on AIDS in Africa: strategies for prevention and control. AIDS Education and Prevention. 1989;1(1):57–69. [PubMed] [Google Scholar]
- Airhihenbuwa CO. Health and culture: beyond the western paradigm. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Airhihenbuwa CO. Healing our differences: the global crisis of health and politics of identity. Lanham, MD: Rowman and Littlefield; 2007. [Google Scholar]
- Airhihenbuwa CO, Webster JD. Culture and African contexts of HIV/AIDS prevention, care and support. Journal of Social Aspects of HIV/AIDS Research Alliance. 2004;1(1):4–13. doi: 10.1080/17290376.2004.9724822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Airhihenbuwa CO, et al. Stigma, culture, and HIV and AIDS in the Western Cape, South Africa: an application of the PEN-3 cultural model for community based research. Journal of Black Psychology. 2009;35(4):407–432. doi: 10.1177/0095798408329941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bharat S, Aggleton P. Facing the challenge: household responses to HIV/AIDS in Mumbai, India. AIDS Care. 1999;11(1):31–44. doi: 10.1080/09540129948180. [DOI] [PubMed] [Google Scholar]
- Blankenship K, Bray S, Merson M. Structural interventions in public health. AIDS. 2000;14:S11–S21. doi: 10.1097/00002030-200006001-00003. [DOI] [PubMed] [Google Scholar]
- Bor R, Miller R, Goldman E. HIV/AIDS and the family: a review of research in the first decade. Journal of Family Therapy. 1993;15:187–204. [Google Scholar]
- Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Education and Prevention. 2003;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- Campbell C, Williams B. Beyond the biomedical and behavioral: towards an integrated approach to HIV prevention in the Southern African mining industry. Social Science and Medicine. 1999;48:1625–1639. doi: 10.1016/s0277-9536(98)00449-3. [DOI] [PubMed] [Google Scholar]
- Charasse-Pouele C, Fournier M. Health disparities between racial groups in South Africa: a decomposition analysis. Social Science and Medicine. 2006;62(11):2897–2914. doi: 10.1016/j.socscimed.2005.11.020. [DOI] [PubMed] [Google Scholar]
- Coates RD. Introduction: reproducing racialized systems of social control. American Behavioral Scientist. 2003;47:235–239. [Google Scholar]
- Coates RD. Introduction. In: Coates RD, editor. Race and ethnicity: across time, space and discipline. Leiden: Brill; 2006. pp. 1–18. [Google Scholar]
- Crocker J, Major B. Social stigma and self-esteem: the self-protective properties of stigma. Psychological Review. 1989;96:608–630. [Google Scholar]
- Deacon H, Stephney I, Prosalendis S. Understanding HIV/AIDS stigma: a theoretical and methodological analysis. Cape Town: HSRC Press; 2005. [Google Scholar]
- Farmer P. Infections and inequalities: the modern plagues. Berkeley, CA: University of California Press; 1999. [Google Scholar]
- Fassin D. Une double peine. La condition sociale des immigres malades du sida. Homme Revue Française d’Anthropologie. 2001;160:137–162. [Google Scholar]
- Fassin D. The embodiment of inequality: AIDS as a social condition and the historical experience in South Africa. EMBO reports. 2003;4(Special issue):S4–S9. doi: 10.1038/sj.embor.embor856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fassin D, Schneider H. The politics of AIDS in South Africa: beyond the controversies. BMJ. 2003;326:495–497. doi: 10.1136/bmj.326.7387.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. Stigma: notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall; 1963. [Google Scholar]
- Hamra M, et al. Relationship between expressed HIV/AIDS-related stigma and HIV-beliefs/knowledge and behaviour in families of HIV infected children in Kenya. Tropical Medicine International Health. 2006;11(4):513–527. doi: 10.1111/j.1365-3156.2006.01583.x. [DOI] [PubMed] [Google Scholar]
- Health Resources Services Administration (HRSA) [Accessed 27 January 2009];HRSA care action: providing HIV/AIDS care in a changing environment. 2003 Available from: http://hab.hrsa.gov/publications/august2003.htm#a1.
- Herek GM. AIDS and stigma. American Behavioral Scientist. 1999;42(7):1106–1116. [Google Scholar]
- Herek GM. Thinking about AIDS and stigma: a psychologist’s perspective. Journal of Law, Medicine and Ethics. 2002;30:594–607. doi: 10.1111/j.1748-720x.2002.tb00428.x. [DOI] [PubMed] [Google Scholar]
- Iwelunmor J, et al. Family systems and HIV/AIDS in South Africa. International Quarterly of Community Health Education. 2008;27(4):321–335. doi: 10.2190/IQ.27.4.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP. Levels of racism: a theoretic framework and a gardener’s tale. American Journal of Public Health. 2000;90:1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP, et al. Using ‘socially assigned race’ to probe White advantages in health status. Ethnicity & Disease. 2008;18:496–504. [PubMed] [Google Scholar]
- Jungar K, Oinas E. Preventing HIV? Medical discourses and invisible women. In: Arnfred S, editor. Re-thinking sexualities in Africa. Uppsala: The Nordic Africa Institute; 2004. pp. 97–114. [Google Scholar]
- Kalichman SC, Simbayi LC. HIV testing attitudes, AIDS stigma, and voluntary HIV counseling and testing in a black township in Cape Town, South Africa. Sexually Transmitted Infections. 2003;79:442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayongo-Male D, Onyango P. The sociology of the African family. London: Longman; 1984. [Google Scholar]
- Krieger N. Discrimination and health. In: Berkman L, Kawachi I, editors. Social epidemiology. Oxford: Oxford University Press; 2000. pp. 36–75. [Google Scholar]
- Krieger N, et al. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures – the public health disparities geocoding project. American Journal of Public Health. 2003;93(10):1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishna VS, et al. Unheard voices: experiences of families living with HIV/AIDS in India. Contemporary Family Therapy. 2005;27(4):483–506. [Google Scholar]
- Link B, Phelan J. [Accessed 11 February 2009];On stigma and its public health implications. 2002 Available from: http://www.stigmaconference.nih.gov/LinkPaper.htm.
- Neville Miller A, Rubin DL. Factors leading to self-disclosure of a positive HIV diagnosis in Nairobi, Kenya: people living with HIV/AIDS in the Sub-Sahara. Qualitative Health Research. 2007;17(5):586–598. doi: 10.1177/1049732307301498. [DOI] [PubMed] [Google Scholar]
- Otolok-Tanga E, et al. Examining the actions of faith-based organizations and their influence on HIV/AIDS-related stigma; a case study of Uganda. African Health Science. 2007;7(1):55–60. doi: 10.5555/afhs.2007.7.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packard R. White plague, black labour: tuberculosis and the political economy of health and disease in South Africa. Berkeley, CA: University of California Press; 1990. [Google Scholar]
- Patton C. Inventing AIDS. New York: Routledge; 1990. [Google Scholar]
- Petros G, et al. HIV/AIDS and ‘othering’ in South Africa: the blame goes on. Culture, Health & Sexuality. 2006;8(1):67–77. doi: 10.1080/13691050500391489. [DOI] [PubMed] [Google Scholar]
- Shisana O, et al. South African National HIV Prevalence, HIV Incidence, Behaviour and Communication Survey, 2005. Cape Town: HSRC Press; 2005. [Google Scholar]
- Shriver M, Everett C, Morin S. Structural interventions to encourage primary HIV prevention among people living with HIV. AIDS. 2000;14:S57–S62. doi: 10.1097/00002030-200006001-00009. [DOI] [PubMed] [Google Scholar]
- Simbayi LC, et al. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine. 2007;64:1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner D, Mfecane S. Stigma, discrimination and the implications for people living with HIV/AIDS in South Africa. Journal of Social Aspects of HIV/AIDS. 2004;1(3):157–164. doi: 10.1080/17290376.2004.9724838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South Africa. [27 March 2009];New world encyclopedia. 2009 Available from: http://www.newworldencyclopedia.org/entry/South_Africa.
- Statistics South Africa. Income and Expenditures Survey 2000. Pretoria: Statistics South Africa; 2002. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Report. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, et al. Perceived discrimination, race and health in South Africa. Social Science and Medicine. 2008;67(3):441–452. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou J, et al. Religion and HIV in Tanzania: influence of religious beliefs on HIV stigma, disclosure, and treatment attitudes. BMC Public Health. 2009;9:75–86. doi: 10.1186/1471-2458-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]