Abstract
Background
Recent studies suggest that surrogate decision makers may be too optimistic about their end-of-life decision making abilities for loved ones. We examined surrogates' decision making confidence with an emphasis on its linkages to their understandings of patients' values and goals for end-of-life care.
Methods
We used baseline data from a randomized trial with 58 dyads of African-American dialysis patients and their surrogates who separately completed the Values of Life-Sustaining Treatment Outcomes and the Goals of Care documents. Surrogates also completed a Surrogate Decision Making Confidence Scale.
Results
Overall, 60% of surrogates were unsure how their loved ones would feel about continuing life-sustaining treatment, including dialysis, in at least one of the four outcomes presented in the Values of Life-Sustaining Treatment Outcomes. For goals of care near end of life, 67.2% to 69.0% of patients preferred comfort care only, but only 20 (34.5%) surrogates were congruent with patients on Goals of Care. Nonetheless, surrogates' confidence was high (M=3.23 out of 4.0). Surrogates' confidence was positively associated with dyad congruence in values for life-sustaining treatment at only a small magnitude (Spearman's rho=.31, p=.02), but not with dyad congruence in goals of care (χ2=2.13, df=1, p=.19).
Conclusions
Surrogates' confidence had little association with their actual understanding of patients' values and goals. Interventions to prepare patients and surrogates for end-of-life decision making may need to address overconfidence and help surrogates recognize their limited understanding of patients' values and goals.
Introduction
The number of patients in the United States with end-stage kidney disease (ESKD) who require dialysis is increasing rapidly with the aging of the population and the epidemic of diabetes mellitus.1 Mortality in this population is high; over 80,000 patients with ESKD die every year primarily due to acute illnesses (e.g., infection and cardiovascular disease) associated with comorbidities.1 In the absence of patient competence to make decisions as to whether to continue or stop dialysis near end of life, family members or surrogate decision makers are asked to make those difficult decisions.2 This issue has been particularly challenging in the care of African Americans because they are thought to prefer aggressive treatment at the end of life and to be reluctant to stop life-sustaining treatment when its benefits are in doubt.3–7
Few African Americans make their wishes known to their surrogates, and discussions often remain too vague to guide surrogate decision makers.8, 9 Studies have shown that, without an effective communication intervention to improve surrogates' understanding of patients' wishes, surrogates' judgments are only modestly correlated with patients' preferences.10–14 Further, surrogates' judgments are more highly related to their own preferences than to dialysis patient's preferences.15
While the extent to which surrogate decision making is based on patients' actual preferences is uncertain at best, recent studies have suggested that surrogates may be too confident (too optimistic) about their ability to represent their loved one's wishes in end-of-life decisions.16–18 Understanding the relationship between surrogate confidence and their understanding of patients' wishes has clinical and research implications for how to better assist patients and their surrogates in end-of-life decision making. If both patients and their surrogates falsely believe that the surrogates have a good understanding of patients' wishes and that their surrogates would be able to make end-of-life decisions, such confidence may preclude them from engaging in end-of-life discussions.
The purpose of this paper was to examine surrogate decision making confidence, with an emphasis on its linkages to their understandings of patients' values and goals for end-of-life care. Data from 58 dyads of African-American dialysis patients and their surrogate decision makers were used. To address decision making confidence, we first determine if our data replicate previous work demonstrating lack of congruence between patients and surrogates on values and goals. The specific research questions were as follows. For African Americans with ESKD,
What values for life-sustaining treatment, based on likely outcomes, are held?
Is there congruence in values for life-sustaining treatment within the dyad? In other words, are surrogates' predictions of their loved ones' values congruent with patients' values?
What goals of care at the end of life are preferred?
Is there congruence in goals of care at the end of life within the dyad? In other words, are surrogates' predictions of their loved ones' preferences for goals of care congruent with patients' choices?
What is the level of decision making confidence in the surrogates?
Is there an association between surrogate decision making confidence and (a) dyad congruence in values for life-sustaining treatment and (b) dyad congruence in goals of care?
Methods
Design and sample
We used baseline data collected during a randomized controlled trial in which an end-of-life communication intervention was tested with 58 dyads of African-American dialysis patients and their surrogate decision makers.18 The original study, conducted from 2006 to 2009, included three measurement time points (baseline, one week post-intervention, and three months).
Patients were deemed eligible for the original study if they met the following criteria: self-identified African American, receiving dialysis for at least three months before enrollment, availability of a surrogate chosen by the patient who could be present during the intervention, over age 18, and able to speak English. Social workers at the dialysis clinics approached 125 potential patient participants from six outpatient dialysis clinics in western Pennsylvania to assess their eligibility. Subsequently, the research staff approached patients who indicated an interest in the study for informed consent and a cognitive function test, the 10-item Short Portable Mental Status Questionnaire (SPMSQ).19 Patients with >2 errors on the SPMSQ were deemed ineligible. Upon patients' consent, the research staff contacted their surrogates and invited them to join the study if they were over age 18, able to speak English, and willing to participate in the intervention with the patients. Of the 118 eligible patients, 87 (73.7%) consented; of those, 58 of the chosen surrogates (66.6%) agreed to participate. See Table 1 for patient and surrogate characteristics.
Table 1.
Sample Characteristics
| n (%) | |
|---|---|
| Patient | |
| Age, M±SD | 57.93±11.9 |
| Male | 33 (56.9) |
| Married or living with partner | 22 (37.9) |
| Completed high school | 50 (86.2) |
| Protestant, Religious affiliation | 43 (74.1) |
| Religious involvement | |
| Frequently or always | 36 (62.1) |
| Importance of spirituality in life | |
| Extremely important | 36 (62.1) |
| Annual household income | |
| <$13,000 | 24 (41.4) |
| $13,000 - $29,000 | 17 (29.3) |
| >$29,000 | 17 (29.3) |
| Medicare, Insurance | 46 (79.3) |
| Time on dialysis in year, median | 4.13 |
| Charlson Comorbidity Index, M±SD | 6.35±2.1 |
| Surrogate | |
| Age, M±SD | 49.52±12.7 |
| Male | 14 (24.1) |
| White | 3 (5.2) |
| Completed high school | 50 (86.2) |
| Relationship to patient | |
| Spouse or partner | 18 (31.0) |
| Parent | 11 (19.0) |
| Sibling | 14 (24.1) |
| Child | 4 (6.9) |
| Other relative or frienda | 11 (19.0) |
| Protestant, Religious affiliation | 42 (72.4) |
| Religious involvement | |
| Frequently or always | 41 (70.7) |
| Importance of spirituality in life | |
| Extremely important | 46 (79.3) |
Including ex-wives, in-laws, grandchildren, and nieces.
M, mean; SD, standard deviation.
Tools and data collection
Study procedures were approved by the institutional review board of the primary institution of the project. At baseline, each member of the dyad separately completed questionnaires at the dialysis clinic.
Values of life-sustaining treatment outcomes20
This tool assessed the patient's threshold for unacceptable outcomes of life-sustaining treatment. This tool asked patients to imagine that they developed cancer that has spread or that they have had a severe stroke or heart attack and became seriously ill at the hospital. Patients then were asked to think about conditions that for them would be worse than death and they would want their family member to make a decision to stop life-sustaining treatment, including dialysis, and focus on treatment to make them as comfortable as possible. Patients were presented with four outcomes and asked whether the outcome would be “acceptable,” “unacceptable,” or “unsure.” The four outcomes of life-sustaining treatment were: cannot recognize my family or friends, only respond to pain and yet in untreatable pain most of the time, can no longer control my bowels, and have to live in a nursing home until death. One-week test-retest reliability in 29 patients (assessed using probability of agreement with 95% confidence interval for each outcome) ranged 0.70 to 0.72 (95% CI=0.50 to 0.86) in a previous study.20
The surrogate version asked respondents whether the outcome would be acceptable or not acceptable to their loved ones or if they were unsure. For each of the four values, congruence was determined by whether the patient and surrogate both responded “acceptable” or both responded “unacceptable.” If both members of the dyad responded “unsure,” this was not considered congruent. In our analyses we report the percentage of dyads that were congruent on each value, the congruence score (a sum of the values [0 to 4] on which dyads were congruent), and the number of values on which surrogates were unsure of their loved one's values.
Goals of care document17,18
This document assessed patients' end-of-life treatment preferences using two scenarios describing medical conditions that commonly occur in patients with ESKD. The first scenario described a condition in which the patient develops cancer that spreads or has severe complications and cannot speak for himself/herself. The medical team believes that recovery is unlikely and that continuing life-sustaining treatment, including dialysis, is no longer beneficial. The second scenario described a condition in which the patient develops advanced dementia and he or she can no longer be him/herself. His/her dementia is no longer responding to treatment. For each scenario, patients were asked to choose one of three options: “the goals of care should be focused on delaying my death, and thus I want to continue life-sustaining treatment;” “the goals of care should be focused on my comfort and peace, and thus I do not want life-sustaining treatment, including dialysis;” and “I am not sure.” One-week test-retest reliability in 29 patients (the probability of agreement with 95% confidence interval) ranged 0.76 to 0.86 (95% CI=0.60 to 0.92) in a previous study.20
The surrogate version asked respondents to choose one of the two options that indicates best what their loved one's preference would be for each scenario or the option, “I am not sure,” if they were uncertain about their loved ones' preference. To determine congruence on goals of care, patients' and surrogates' responses were first stratified into delaying death in both scenarios, mixed (delaying death in one scenario and comfort care only in the other scenario), and comfort care only in both scenarios. Dyads were categorized as being congruent or incongruent as follows. A dyad was considered congruent if both the patient's and surrogate's responses were stratified into one of the three categories delaying death, mixed, and comfort care only. In the case when both members of the dyad chose “I am not sure,” the dyad was not considered congruent.
Decision making confidence scale17,18
This scale measured surrogates' confidence in end-of-life decision making for their loved ones. It consists of five items with response options from 0 (Not Confident At All) to 4 (Very Confident), reflecting level of comfort in the surrogate role (Cronbach's a=0.85). For example, one item was “I feel confident that I understand what my loved one's preferences are.” A total score is a mean of the five items.
Other descriptive data included sociodemographic information, such as age, gender, education, annual household income, health insurance status, the importance of religion or spirituality in life on a four-point scale from 1 (Not At All Important) to 4 (Extremely Important), and the extent of following religious customs on a four-point scale from 1 (Not At All) to 4 (Always). From medical record reviews we determined the duration of dialysis and the Charlson Comorbidity Index (CCI).21 The CCI includes 19 comorbid conditions, including myocardial infarction, congestive heart failure, AIDS, cerebrovascular disease, and liver disease. A higher score indicates a greater risk of mortality.21–23
Data analysis
Descriptive statistics (mean, SD, frequency, percent) were used to summarize sample characteristics, patients' values for life-sustaining treatment, dyad congruence on values, patients' goals of care, dyad congruence on goals of care, and surrogate decision making confidence. To examine the relationship of surrogate confidence to dyad congruence in values for life-sustaining treatment, a Spearman's rho was used. To examine the relationship between surrogate decision making confidence and dyad congruence in goals of care, a Fisher exact test was employed. The relationship between number of life-sustaining treatment outcomes on which the surrogate was unsure and surrogate confidence was determined using a Spearman's rho.
Results
Patients' values for life-sustaining treatment and dyad congruence
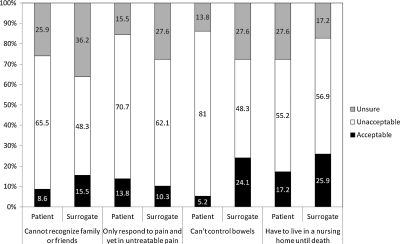
Figure 1 presents patients' values and surrogates' prediction of their loved ones' values for life-sustaining treatment. The outcome endorsed as unacceptable by the highest percentage of patients (81%) was a condition with the loss of bowel control, necessitating dependence on others for basic needs. Forty-one patients (70.7%) said that the outcome of untreatable pain would be unacceptable to them and they would want their family member to make a decision to stop all life-sustaining treatment, including dialysis. Nonetheless, a sizable number of patients were unsure about their own values, especially for the outcomes in which patients cannot recognize their family or friends (25.9%) or have to live in a nursing home until death (27.6%). Overall, 60% of surrogates were unsure how their loved ones would feel about continuing or stopping life-sustaining treatment, including dialysis, in at least one of the four outcomes.
FIG. 1.
Number (%) of patient preferences and surrogate predictions of values for life-sustaining treatment outcomes.
Dyad congruence on values is presented in Table 2. The outcome on which the largest number of dyads showed lack of congruence was the condition in which the patient cannot recognize his or her family or friends (69%). In other words, nearly 70% of surrogates predicted their loved ones' values for this outcome inconsistently with the patients' values or were unsure of the patients' values. Conversely, the outcome on which the largest number of dyads were congruent was only respond to pain…wherein 27 (46.6%) of the dyads were congruent. Overall, out of the four possible outcomes, the mean number of outcomes of life-sustaining treatment on which dyads showed congruence was 1.60 (SD=1.39).
Table 2.
Number (%) of Dyads Congruent in Values for Life-Sustaining Treatment Outcomes
| |
Congruent |
Incongruent |
|---|---|---|
| n (%) | n (%) | |
| Cannot recognize family or friends | 18 (31.0) | 40 (69.0) |
| Only respond to pain and yet in untreatable pain most of the time | 27 (46.6) | 31 (53.4) |
| Can no longer control bowels | 24 (41.4) | 34 (58.6) |
| Have to live in a nursing home until death | 24 (41.4) | 34 (58.6) |
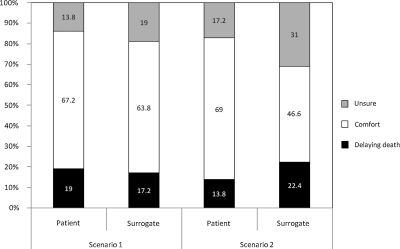
Patients' preferences for goals of care and dyad congruence
For goals of care near end of life, the majority of patients (67.2% in scenario 1 and 69.0% in scenario 2) said that they would want the focus to be on comfort care only and that life-sustaining treatment, including dialysis, should be withdrawn (Figure 2). For scenario 1, a large percentage of surrogates (63.8%) also selected focusing on comfort, but in scenario 2 only 46.6% of surrogates selected focusing on comfort. In addition, while quite a few patients were unsure of their own wishes (13.8% in scenario 1 and 17.2% in scenario 2), fully 31% of surrogates were unsure about what goals of care their loved ones would prefer in the condition of advanced dementia that is no longer responsive to treatment. Finally, in categorizing dyads as either congruent or not, only 20 (34.5%) dyads were congruent on both scenarios.
FIG. 2.
Number (%) of patients' preferences and surrogates' predictions of goals of care near end of life.
Surrogates' decision making confidence and its association with dyad values and goals congruence
Table 3 presents data regarding surrogates' decision making confidence. In general, decision making confidence was high (M=3.23), as were scores on each of the items in the scale. Another way to consider the data is that 46 surrogates (79.3%) scored between 3 (Confident) and 4 (Very Confident). Only one surrogate characteristic, i.e., the extent of following religious customs, was correlated (inversely) with decision making confidence (Spearman's rho=−0.30, n=58, p=0.03). Surrogate confidence was positively associated with dyad congruence in values for life-sustaining treatment, but the magnitude of the correlation was small (Spearman's rho=0.31, n=58, p=0.02). Alternatively, surrogate confidence was not associated with dyad congruence in goals of care (χ2=2.13, df=1, p=0.19; Table 4); in short, regardless of whether the surrogates' responses in the Goals of Care document were congruent with the patients' goals or not, surrogates felt confident in end-of-life decision making on behalf of their loved ones.
Table 3.
Mean (SD) Surrogate Decision-Making Confidence by Item and for Total Score
| Item | M±SD |
|---|---|
| I feel confident that … | |
| 1. I understand what my loved one's preferences are | 2.93±1.31 |
| 2. I can make a decision for my loved one as to what treatment he/she should have, even in a highly stressful situation | 3.12±1.09 |
| 3. I can ask questions to get the facts about the benefits or risks of each medical choice without feeling discouraged | 3.47±0.88 |
| 4. I can handle unwanted pressure from others, such as other family members or health care providers, in making decisions for my loved one | 3.26±0.91 |
| 5. I can communicate with doctors and nurses about my loved one's wishes | 3.38±0.95 |
| Total score | 3.23±0.82 |
Table 4.
Number (%) of Surrogates Who Were Confident or Not Confident by Dyad Goal Congruence
| |
Dyad congruent (n=20) |
Dyad incongruent (n=38) |
|---|---|---|
| n (%) | n (%) | |
| Surrogate scored 0–2 (Not Confident) | 2 (3.4) | 10 (17.2) |
| Surrogate scored 3–4 (Confident) | 18 (31.0) | 28 (48.3) |
To further explore surrogates' overconfidence in understanding patients' values, we examined the association between surrogate decision making confidence and the number of values for life-sustaining treatment on which they were unsure about their loved one's values. An inverse association (Spearman's rho=−0.51, n=58, p<0.001) was found. In other words, the more outcomes on which a surrogate was able to respond either “acceptable” or “unacceptable” to their loved ones – whether their answers were actually congruent with the patient's wishes or not – the more confident was the surrogate.
Discussion
Decisions to stop life-sustaining treatment, particularly dialysis, are extremely difficult to think about for patients whose lives have been dependent on dialysis.24,25 Understandably, discussions about end-of-life care are often avoided, and this may leave both patients and their family members and surrogates unprepared for those decisions.26,27 Although previous studies have demonstrated that congruence between patients and surrogates in end-of-life treatment preferences is low,10–13 our findings offer additional useful information to improve approaches to end-of-life communication.
For example, patients themselves may be unsure about their own values and care goals at the end of life. Therefore, they need opportunities to explore their own values in order to be able to provide instructions to their surrogates. We also found that end-of-life preferences in our sample differed from previous literature describing African Americans as preferring not to stop life-sustaining treatment.3–7 In this sample, a substantial number of African-American dialysis patients preferred comfort care over life-sustaining treatment, including dialysis. Although the patients expressed their preferences in response to hypothetical situations, these data challenge conventional beliefs about African Americans' end-of-life preferences. It is important for clinicians and researchers to be aware that there are diverse perspectives among African Americans about continuing life-sustaining treatment when the outcome is considered unacceptable.20
In our sample, surrogates tended to choose a response that reflects a focus on delaying death. Given the low congruence in both values for life-sustaining treatment and goals of care, these responses are likely to reflect their own values or difficulty choosing otherwise (and thus selecting a less distressing option).28 We also confirmed the results of previous studies16–18 that surrogates generally rated their decision making confidence high. Yet their confidence had little to no association with dyad congruence. This finding suggests that surrogates may be too optimistic about their ability to make end-of-life decisions for their loved ones because they may not have realized their lack of knowledge of patients' preferences, what roles a surrogate decision maker would need to play, and the burden associated with those roles. Much greater attention must be given to surrogates as opposed to focusing primarily on clarification and documentation of patients' wishes. To be effective, an intervention to prepare patients and their surrogates for end-of-life decision making will need to include components to provide patients enough opportunity to explore their own values and to help surrogates recognize the extent of their understanding of patients' values and potential difference between their own values and patients'.
This study has several limitations. Although the sample size of the original study was determined by the power needed to test an intervention, it still represents a small number of African-American dyads. Also, the sample was recruited from an urban area and vicinities and thus does not represent African Americans residing in a rural area where perspectives might be different. These limitations suggest the urgent need for further study examining what has become the conventional wisdom about African Americans' preferences for life-sustaining treatment as opposed to palliative care. That is, could it be the peculiarities of our sample that resulted in findings that differ from previous research, or is there in fact greater diversity in African-American preferences than is typically thought?
In summary, we found that congruence between African-American dialysis patients and their surrogates in end-of-life treatment preferences was low, but partly because some patients themselves were unsure about their own values and preferences. We also found that a substantial number of African Americans prefer comfort care over life-sustaining treatment, including dialysis. Surrogates were generally confident about their ability to make end-of-life decisions for their loved ones without fully recognizing their lack of understanding of patients' wishes. Our findings may be useful for clinicians and researchers in helping dialysis patients and their surrogates to prepare for end-of-life decision making.
Acknowledgments
This work was supported by the National Institute of Nursing Research (5R21NR009662, Song).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.U.S. Renal Data System. USRDS 2010 Annual Data Report: Atlas of End-Stage Renal Disease in the United States. Vol. 2007. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2010. [Google Scholar]
- 2.Braun UK. Beyth RJ. Ford ME. McCullough LB. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. J Gen Intern Med. 2008;23(3):267–274. doi: 10.1007/s11606-007-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torke AM. Garas NS. Sexson W. Branch WT. Medical care at the end of life: views of African American patients in an urban hospital. J Palliat Med. 2005;8(3):593–602. doi: 10.1089/jpm.2005.8.593. [DOI] [PubMed] [Google Scholar]
- 4.Mor V. Papandonatos G. Miller SC. End-of-life hospitalization for African American and non-Latino white nursing home residents: Variation by race and a facility's racial composition. J Palliat Med. 2005;8(1):58–68. doi: 10.1089/jpm.2005.8.58. [DOI] [PubMed] [Google Scholar]
- 5.Phipps E. True G. Harris D. Chong U. Tester W. Chavin SI. Braitman LE. Approaching the end of life: Attitudes, preferences, and behaviors of African-American and white patients and their family caregivers. J Clin Oncol. 2003;21(3):549–554. doi: 10.1200/JCO.2003.12.080. [DOI] [PubMed] [Google Scholar]
- 6.Hopp FP. Duffy SA. Racial variations in end-of-life care. J Am Geriatr Soc. 2000;48(6):658–663. doi: 10.1111/j.1532-5415.2000.tb04724.x. [DOI] [PubMed] [Google Scholar]
- 7.Owen JE. Goode KT. Haley WE. End of life care and reactions to death in African-American and white family caregivers of relatives with Alzheimer's disease. Omega (Westport) 2001;43(4):349–361. doi: 10.2190/YH2B-8VVE-LA5A-02R2. [DOI] [PubMed] [Google Scholar]
- 8.Hines SC. Glover JJ. Holley JL. Babrow AS. Badzek LA. Moss AH. Dialysis patients' preferences for family-based advance care planning. Ann Intern Med. 1999;130(10):825–828. doi: 10.7326/0003-4819-130-10-199905180-00016. [DOI] [PubMed] [Google Scholar]
- 9.Holley JL. Hines SC. Glover JJ. Babrow AS. Badzek LA. Moss AH. Failure of advance care planning to elicit patients' preferences for withdrawal from dialysis. Am J Kidney Dis. 1999;33(4):688–693. doi: 10.1016/s0272-6386(99)70220-9. [DOI] [PubMed] [Google Scholar]
- 10.Pruchno RA. Lemay EP., Jr. Feild L. Levinsky NG. Predictors of patient treatment preferences and spouse substituted judgments: The case of dialysis continuation. Med Decis Making. 2006;26(2):112–121. doi: 10.1177/0272989X06286482. [DOI] [PubMed] [Google Scholar]
- 11.Pruchno R. Cartwright FP. Wilson-Genderson M. The effects of race on patient preferences and spouse substituted judgments. Int J Aging Hum Dev. 2009;69(1):31–54. doi: 10.2190/AG.69.1.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fried TR. Bradley EH. Towle VR. Valuing the outcomes of treatment: Do patients and their caregivers agree? Arch Intern Med. 2003;163(17):2073–2078. doi: 10.1001/archinte.163.17.2073. [DOI] [PubMed] [Google Scholar]
- 13.Coppola KM. Ditto PH. Danks JH. Smucker WD. Accuracy of primary care and hospital-based physicians' predictions of elderly outpatients' treatment preferences with and without advance directives. Arch Intern Med. 2001;161(3):431–440. doi: 10.1001/archinte.161.3.431. [DOI] [PubMed] [Google Scholar]
- 14.Shalowitz DI. Garrett-Mayer E. Wendler D. The accuracy of surrogate decision makers: A systematic review. Arch Intern Med. 2006;166(5):493–497. doi: 10.1001/archinte.166.5.493. [DOI] [PubMed] [Google Scholar]
- 15.Pruchno RA. Lemay EP., Jr. Feild L. Levinsky NG. Spouse as health care proxy for dialysis patients: Whose preferences matter? Gerontologist. 2005;45(6):812–819. doi: 10.1093/geront/45.6.812. [DOI] [PubMed] [Google Scholar]
- 16.Nolan MT. Hughes MT. Kub J. Terry PB. Astrow A. Thompson RE. Clawson L. Texeira K. Sulmasy DP. Development and validation of the family decision-making self-efficacy scale. Palliat Support Care. 2009;7(3):315–321. doi: 10.1017/S1478951509990241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Song MK. Donovan HD. Piraino B. Choi J. Bernardini J. Verosky D. Ward SE. Effects of an intervention to improve communication about end-of-life care among African Americans with chronic kidney disease. Applied Nurs Res. 2010;23:65–72. doi: 10.1016/j.apnr.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Song MK. Ward SE. Happ MB. Piraino B. Donovan HS. Shields AM. Connolly MC. Randomized controlled trial of SPIRIT: An effective approach to preparing African American dialysis patients and families for end-of-life. Res Nurs Health. 2009;32:260–273. doi: 10.1002/nur.20320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 20.Song MK. Hanson LC. Relationships between psychosocial-spiritual well-being and end-of-life preferences and values in African American dialysis patients. J Pain Symptom Manage. 2009;38(3):372–380. doi: 10.1016/j.jpainsymman.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fried L. Bernardini J. Piraino B. Charlson comorbidity index as a predictor of outcomes in incident peritoneal dialysis patients. Am J Kidney Dis. 2001;37(2):337–342. doi: 10.1053/ajkd.2001.21300. [DOI] [PubMed] [Google Scholar]
- 22.Charlson M. Szatrowski TP. Peterson J. Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 23.Fried L. Bernardini J. Piraino B. Comparison of the Charlson Comorbidity Index and the Davies score as a predictor of outcomes in PD patients. Perit Dial Int. 2003;23(6):568–573. [PubMed] [Google Scholar]
- 24.Russ AJ. Shim JK. Kaufman SR. "Is there life on dialysis?": Time and aging in a clinically sustained existence. Med Anthropol. 2005;24(4):297–324. doi: 10.1080/01459740500330639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Russ AJ. Shim JK. Kaufman SR. The value of "life at any cost": Talk about stopping kidney dialysis. Soc Sci Med. 2007;64(11):2236–2247. doi: 10.1016/j.socscimed.2007.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davison SN. Simpson C. Hope and advance care planning in patients with end stage renal disease: Qualitative interview study. BMJ. 2006;333:886–890. doi: 10.1136/bmj.38965.626250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Davison SN. Torgunrud C. The creation of an advance care planning process for patients with ESRD. Am J Kidney Dis. 2007;49(1):27–36. doi: 10.1053/j.ajkd.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 28.Luce MF. Decision making as coping. Health Psychol. 2005;24(4 Suppl):S23–28. doi: 10.1037/0278-6133.24.4.S23. [DOI] [PubMed] [Google Scholar]