Abstract
OBJECTIVE
To evaluate the predictive role of increased corrected QT (QTc) and QT interval dispersion (QTd) on all-cause and cardiovascular mortality in a large, unselected type 2 diabetic population.
RESEARCH DESIGN AND METHODS
The prospective study included 1,357 type 2 diabetic patients from the Casale Monferrato Study. At baseline, QTc intervals >0.44 s and QTd intervals >0.08 s were considered abnormally prolonged. Both all-cause and cardiovascular mortality were assessed 15 years after the baseline examination.
RESULTS
During the follow-up period, 862 subjects per 12,450 person-years died. Multivariate analysis showed that the hazard ratio (HR) of cardiovascular mortality was significantly increased in subjects with prolonged QTd (1.26 [95% CI 1.02–1.55]) and was only slightly reduced after multiple adjustments. Conversely, prolonged QTc did not increase the HRs for all-cause or cardiovascular mortality.
CONCLUSIONS
Increased QTd predicts cardiovascular mortality after a long-term follow-up period in a large, unselected population of type 2 diabetic subjects.
Diabetes is a known cardiovascular risk factor, and there is much interest in the identification of factors that may improve cardiovascular risk stratification in diabetic subjects, possibly by using noninvasive low-cost approaches. In the general population, prolonged corrected QT (QTc) and increased QT interval dispersion (QTd), reflecting abnormalities of ventricular myocardial repolarization, are independent predictors of mortality (1). However, in type 2 diabetic subjects, the predictive role of QTc and QTd on all-cause and cardiovascular mortality remains controversial because studies addressing this issue were performed on small cohorts and/or had relatively short follow-up periods and/or focused on populations representative of specific ethnic groups (2–9). Therefore, we performed a prospective study to assess the predictive role of increased QTc and QTd on all-cause and cardiovascular mortality in an unselected, large population of type 2 diabetic subjects after a long-term follow-up period.
RESEARCH DESIGN AND METHODS
The study base included 1,540 type 2 diabetic subjects residing in Casale Monferrato (93,477 inhabitants) in 1991 who were identified through diabetes clinics, general practitioners, hospital discharges, prescriptions, and sales records of reagent strips/syringes (10,11). Electrocardiogram (ECG) records suitable for QTc/QTd evaluation were available for 1,359 (88%) patients (580 male and 779 female). R-R and QT intervals were measured blindly by two observers on the resting ECG tracing, using five consecutive beats on a lead V5. The QT interval corrected for the previous cardiac cycle length (QTc) was calculated according to the Bazett equation (12). A QTc >0.44 s was considered abnormally prolonged. R-R and QT intervals also were measured for three consecutive cardiac cycles on the six thoracic leads. QTc dispersion was calculated using the difference between the maximum and the minimum QTc in any thoracic leads. A QTd >0.080 s was considered abnormally increased (10).
The relevant time scale for the analysis was the time since diabetes diagnosis to death or to 31 December 2006 (11). During the follow-up period (1991–2006), patients were regularly evaluated (three to four times per year) at the diabetes clinic or by general practitioners. Information on both deaths and the causes of death was obtained from the demographic files of towns of residence, hospital discharges, and autopsy records. Causes of death were derived and coded according to the ICD-9 classification (11) by two independent observers.
The role of QTc and QTd as independent predictors of cardiovascular and all-cause mortality was assessed using multivariate Cox proportional hazards models. The test for nonproportional hazard was performed using Shoenfeld residuals. The P value was two-sided and considered statistically significant when <0.05.
RESULTS
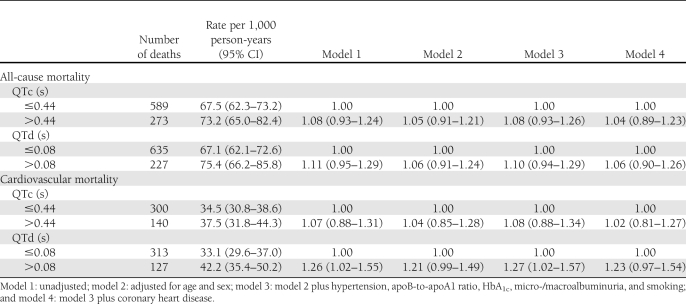
As previously reported (10), at the baseline examination subjects with increased QTc (n = 354) or QTd (n = 448) were older and had higher systolic and/or diastolic blood pressure. Patients with increased QTd also had greater creatinine and fibrinogen levels. Of 1,359 subjects recruited at baseline, information on vital status at follow-up was available for 1,357 patients (99.8%). During follow-up, 862 patients per 12,450 person-years died. Of these, 440 subjects died of cardiovascular disease. Relative to the reference category with QTd ≤0.08 s, the hazard ratio (HR) for cardiovascular mortality was 1.26 (95% CI 1.02–1.55) in patients with increased QTd and only was slightly reduced after multiple adjustment for age, sex, hypertension, smoking, apolipoprotein (apo)B-to-apoA1 ratio, HbA1c, coronary heart disease, and micro-/macroalbuminuria (Table 1). Conversely, prolonged QTc did not increase the HRs for all-cause or cardiovascular mortality. Tests for nonproportional hazard resulted as nonsignificant in all analyses.
Table 1.
Mortality rates and results of Cox regression analyses in the Casale Monferrato Study by QTc and QTd
CONCLUSIONS
This study provides evidence that, in a large population-based cohort of type 2 diabetic patients, increased QTd confers increased long-term cardiovascular mortality risk, independently of other cardiovascular risk factors. Previous reports have suggested a similar conclusion. However, they were performed on small clinic-based type 2 diabetic cohorts (2,8,9) and had a relatively short follow-up period (3).
A previous prospective study on an unselected type 2 diabetic population of American Indians showed the predictive value of ventricular repolarization abnormalities on cardiovascular mortality (4). Our results are in line with these findings and extend them to a European type 2 diabetic population.
Unlike previous reports (2–6,9,12), the current study did not identify QTc as a predictor of all-cause (4–6,12) and/or cardiovascular (2,3,9,12) mortality, possibly because of differences in the study design (2–6,9,12) and prolonged QTc cutoff values (4). Compared with population-based studies, clinic-based studies (2,3,5,6,9,12) notoriously have a potential for a selection bias, such as selecting patients with more severe illness. Nevertheless, findings from the current study are consistent with the view that QTd is a better cardiovascular risk predictor than QTc in type 2 diabetic subjects (3).
The prospective study design; the large population sample; the representativeness of the study base with regard to the Italian diabetic population; the high estimated completeness of ascertainment; the recruitment of subjects cared for by both general practitioners and diabetes clinics, thus limiting the effect of selection bias; and the centralized assessment of measurements are key strengths of our study.
The main limitation is represented by the manual assessment of the QT interval. However, ECGs potentially interfering with accurate QT interval measurements were excluded, and analyses were performed blindly. Furthermore, the QTc for each subject was considered as the mean of the readings of two observers to minimize interobserver variability (10).
The possibility that changes in QTc/QTd abnormalities occurred during follow-up cannot be excluded. However, QT abnormalities do not change significantly over time in type 2 diabetic patients (2). Furthermore, changes in repolarization later in time with respect to baseline would have resulted in an underestimation bias of HRs of QTc and QTd.
Finally, coronary heart disease, micro-/macroalbuminuria, HbA1c, and the apoB-to-apoA1 ratio (10,13–15) have been found to be associated with increased QTc or QTd and/or cardiovascular morbidity/mortality. Therefore, adjustment for these factors could result in an overadjustment bias that would ultimately reduce the statistical significance of the HRs in the fully adjusted model 4.
In conclusion, we found that increased QTd predicts cardiovascular mortality in type 2 diabetic subjects. This observation is of clinical relevance because it may help in identifying people at higher cardiovascular risk by using a noninvasive and low-cost tool.
Acknowledgments
The Casale Monferrato Study is supported by grants from the Piedmont Region (Ricerca Sanitaria Finalizzata 2009).
No potential conflicts of interest relevant to this article were reported.
S.G. and G.Gru. contributed to the study concept and design, participated in data analysis and interpretation, and wrote and reviewed the manuscript. P.F., F.B., C.A., and G.Ghe. researched data. P.C.-P. contributed to the study concept and design and reviewed the manuscript. G.B. contributed to the study concept and design, supervised the study, researched and analyzed the data, and wrote and reviewed the manuscript. G.B. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Okin PM, Devereux RB, Howard BV, Fabsitz RR, Lee ET, Welty TK. Assessment of QT interval and QT dispersion for prediction of all-cause and cardiovascular mortality in American Indians: the Strong Heart Study. Circulation 2000;101:61–66 [DOI] [PubMed] [Google Scholar]
- 2.Rana BS, Lim PO, Naas AA, et al. QT interval abnormalities are often present at diagnosis in diabetes and are better predictors of cardiac death than ankle brachial pressure index and autonomic function tests. Heart 2005;91:44–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cardoso CR, Salles GF, Deccache W. Prognostic value of QT interval parameters in type 2 diabetes mellitus: results of a long-term follow-up prospective study. J Diabetes Complications 2003;17:169–178 [DOI] [PubMed] [Google Scholar]
- 4.Okin PM, Devereux RB, Lee ET, Galloway JM, Howard BV; Strong Heart Study Electrocardiographic repolarization complexity and abnormality predict all-cause and cardiovascular mortality in diabetes: the Strong Heart Study. Diabetes 2004;53:434–440 [DOI] [PubMed] [Google Scholar]
- 5.Salles GF, Bloch KV, Cardoso CR. Mortality and predictors of mortality in a cohort of Brazilian type 2 diabetic patients. Diabetes Care 2004;27:1299–1305 [DOI] [PubMed] [Google Scholar]
- 6.Ziegler D, Zentai CP, Perz S, et al. ; KORA Study Group Prediction of mortality using measures of cardiac autonomic dysfunction in the diabetic and nondiabetic population: the MONICA/KORA Augsburg Cohort Study. Diabetes Care 2008;31:556–561 [DOI] [PubMed] [Google Scholar]
- 7.Stettler C, Bearth A, Allemann S, et al. QTc interval and resting heart rate as long-term predictors of mortality in type 1 and type 2 diabetes mellitus: a 23-year follow-up. Diabetologia 2007;50:186–194 [DOI] [PubMed] [Google Scholar]
- 8.Sawicki PT, Kiwitt S, Bender R, Berger M. The value of QT interval dispersion for identification of total mortality risk in non-insulin-dependent diabetes mellitus. J Intern Med 1998;243:49–56 [DOI] [PubMed] [Google Scholar]
- 9.Naas AA, Davidson NC, Thompson C, et al. QT and QTc dispersion are accurate predictors of cardiac death in newly diagnosed non-insulin dependent diabetes: cohort study. BMJ 1998;316:745–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Veglio M, Bruno G, Borra M, et al. Prevalence of increased QT interval duration and dispersion in type 2 diabetic patients and its relationship with coronary heart disease: a population-based cohort. J Intern Med 2002;251:317–324 [DOI] [PubMed] [Google Scholar]
- 11.Bruno G, Merletti F, Bargero G, et al. Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato Study. Diabetologia 2007;50:941–948 [DOI] [PubMed] [Google Scholar]
- 12.Christensen PK, Gall MA, Major-Pedersen A, et al. QTc interval length and QT dispersion as predictors of mortality in patients with non-insulin-dependent diabetes. Scand J Clin Lab Invest 2000;60:323–332 [DOI] [PubMed] [Google Scholar]
- 13.Psallas M, Tentolouris N, Papadogiannis D, et al. QT dispersion: comparison between participants with Type 1 and 2 diabetes and association with microalbuminuria in diabetes. J Diabetes Complications 2006;20:88–97 [DOI] [PubMed] [Google Scholar]
- 14.Veglio M, Borra M, Stevens LK, Fuller JH, Perin PC; The EURODIAB IDDM Complication Study Group The relation between QTc interval prolongation and diabetic complications. Diabetologia 1999;42:68–75 [DOI] [PubMed] [Google Scholar]
- 15.Szabó Z, Harangi M, Lörincz I, et al. Effect of hyperlipidemia on QT dispersion in patients without ischemic heart disease. Can J Cardiol 2005;21:847–850 [PubMed] [Google Scholar]