Abstract
OBJECTIVE
Short-term intensive insulin treatment in patients with newly diagnosed type 2 diabetes can improve β-cell function and insulin sensitivity, which results in long-term remission without need for further antidiabetes medication. Patient attitudes toward their disease were assessed using the Diabetes Care Profile (DCP) tool to evaluate the potential impact on maintaining long-term remission.
RESEARCH DESIGN AND METHODS
Newly diagnosed patients with type 2 diabetes were recruited and treated with continuous subcutaneous insulin infusion (CSII) for 2–3 weeks. They were also invited to participate in diabetes self-management intervention during hospitalization and complete a DCP questionnaire on attitudes toward diabetes at baseline and 3, 6, and 12 months after suspension of CSII.
RESULTS
Near normoglycemia was achieved by 118 patients after short-term CSII, with 65 remaining in drug-free remission for >1 year. They had significantly better glycemic control and greater restoration of acute insulin response after CSII as well as higher educational attainment compared with patients experiencing relapse. They also achieved higher scores in positive attitude, (belief in) importance of care, care ability, self-care adherence, and less negative attitude. Differences between the two groups became greater over time. Cox proportional hazards model analysis indicated that greater self-care adherence (hazard ratio 0.184, P < 0.001) and homeostasis model assessment of insulin resistance before treatment (0.854, P = 0.053) were independent predictors for long-term remission, whereas elevated 2-h postprandial plasma glucose after CSII (1.156, P = 0.015) was a risk factor for relapse.
CONCLUSIONS
Attitudes toward diabetes affect long-term drug-free remission in newly diagnosed patients with type 2 diabetes after short-term CSII.
Insulin is the most effective agent for lowering blood glucose. Although insulin therapy was once regarded as the “last straw” in a stepwise strategy, the current American Diabetes Association/European Association for the Study of Diabetes consensus statement recommends insulin therapy as part of a first-line combination regimen (1). However, long-term use of insulin is associated with hypoglycemia, weight gain, decreased patient adherence, and concerns about potential malignancy (2). During the past decade, many studies, including our own, have shown that short-term intensive treatment using continuous subcutaneous insulin infusion (CSII) in newly diagnosed patients with type 2 diabetes can substantially improve β-cell function by restoring part of the first-phase insulin secretion that results in long-term (>1 year) glycemic drug-free remission (3–6). A recent report from one of our study centers also shows that short-term intensive CSII greatly restored insulin sensitivity. A marked decrease of insulin resistance to a level of normal glucose tolerance after intensive treatment to that of impaired glucose tolerance at 1-year follow-up was observed in remission subjects (7).
The benefits of short-term intensive CSII for achieving drug-free remission in newly diagnosed patients with type 2 diabetes have gained more recognition and have become more appealing in recent years. However, efficacy varies considerably among study centers or even among patients in the same center. Therefore, identifying factors that are associated with long-term drug-free remission is crucial. Diet and exercise are major elements of diabetes care that also affect glycemic control after suspension of intensive treatment. Thus, diabetes self-management might be the major determinant for maintaining drug-free glycemic remission. Furthermore, in clinical practice, patients will have varying degrees of cognition, social and economic status, and activation as well as different attitudes toward their disease. We hypothesized that all these factors might influence self-management of diabetes and, thus, long-term clinical outcomes. Therefore, we followed longitudinally all the newly diagnosed type 2 diabetic patients who had received short-term CSII treatment to evaluate potential contributors that may affect subsequent diabetes self-management and maintenance of long-term (>1 year) drug-free glycemic remission.
RESEARCH DESIGN AND METHODS
Patient inclusion/exclusion criteria have been described in detail previously (3,4). In brief, newly diagnosed patients with type 2 diabetes were included if they were negative for urinary ketones and islet-cell antibodies and had never received antihyperglycemic therapy. Participants were aged between 25 and 70 years with a BMI of 21–35 kg/m2 and fasting plasma glucose (FPG) between 7.0 and 16.7 mmol/L. Patients were excluded if they had severe acute or chronic diabetes complications or intercurrent illnesses.
Rapid-acting insulin analogs (NovoRapid; Novo Nordisk, Bagsvaerd, Denmark; or HumaLog; Eli Lilly and Company, Indianapolis, IN) were administered with an insulin pump (MiniMed 712; Medtronic, Minneapolis, MN). Initial insulin doses were 0.5–0.6 IU/kg, with total daily doses divided 50/50 for basal and bolus infusion. Capillary blood glucose was monitored eight times per day (before and 2 h after each meal, bedtime, and 3 a.m.). Doses were titrated every day to achieve euglycemia within 3–5 days. Glycemic goals were capillary fasting blood glucose (FBG) <6.0 mmol/L and 2-h postprandial blood glucose (PBG) <8.0 mmol/L. CSII treatment was maintained for another 2 weeks and then suspended. Patients were discharged and then entered a follow-up period.
During hospitalization, all patients were invited to participate in a routine education program on diabetes self-management. This included advice on lifestyle, dietary counseling, physical exercise, self-monitoring of blood glucose (SMBG), the importance of controlling cholesterol and blood pressure, and prevention of acute and chronic complications. The study was approved by the medical research and ethics committee of the First Affiliated Hospital of Sun Yat-sen University, and written informed consent was obtained from each patient.
Follow-up procedure
Only patients achieving near-normoglycemic targets (FBG <7 mmol/L, PBG <10 mmol/L) after the suspension of short-term CSII and agreeing to be followed as outpatients were included in the study. They were scheduled for outpatient visits every month during the first 3 months and every 3 months thereafter.
During the follow-up period, patients were encouraged to record all SMBG results and maintain diet control and physical exercise as instructed. Whenever blood glucose exceeded an FBG >7.0 mmol/L or PBG >10.0 mmol/L, patients were asked to report for examination of venous plasma glucose, even if it was not a scheduled visit. Patients who maintained near-normoglycemic target for ≥12 months without medication were defined as being in remission. Those not meeting these criteria during the follow-up period, which was confirmed 1 week later with a repeated venous examination, were categorized as nonremission. Relapsed patients were treated with either oral hypoglycemic agents or insulin according to guidelines.
Measurements
Information about sociodemographic characteristics including age, sex, marital status, educational attainment, employment, insurance, and smoking status was obtained from all patients. During hospitalization, patients also completed the Diabetes Care Profile (DCP) questionnaire on attitudes toward diabetes. This was self-reported, with research nurses providing clarification as needed. Anthropometric and laboratory data, such as height, weight, FPG, 2-h postprandial plasma glucose (PPG), and HbA1c, as well as insulin and C-peptides during intravenous glucose tolerance test, were assessed before and after intensive CSII. β-Cell function was assessed using acute insulin response (AIR), which was calculated as the incremental trapezoidal area during the first 10 min of the intravenous glucose tolerance test. Homeostasis model assessment was used to estimate basal β-cell function (HOMA-B) and insulin resistance (HOMA-IR). All of these variables were assessed again at 3, 6, and 12 months after discharge.
The DCP questionnaire created by the University of Michigan Diabetes Research and Training Center is a well-recognized measure of social and psychological factors/outcomes related to diabetes treatment and self-management (8). It is suitable for both type 1 and type 2 diabetes (9) and also is valid and reliable in communities and hospitals. The Cronbach α of every subscale is >0.60, with the highest being 0.95. The Chinese translation version has been validated with good convergent and discriminated validity and high internal consistency (10), with a Cronbach α of 0.88 in this sample. The original profile consisted of 16 subscales and 234 items covering attitudes toward diabetes, diet, exercise, monitoring, foot care, and medication. It usually takes ∼1 h for a patient to complete the whole questionnaire, and only the attitudes toward diabetes scales section was measured and investigated in this study. Patients were questioned about five aspects, including positive attitude, negative attitude, ability to care for their diabetes, belief in importance of care, and self-care adherence. Each statement included a 5-point ranking scale, ranging from strongly disagree (never) to strongly agree (always), with 3 points as neutral. Items under the subscales of positive attitude, care ability, importance of care, and self-care adherence scoring ≥4 points and items of negative attitude scoring ≤2 points were designated as good performance, whereas the opposites were poor.
Statistical analyses
The SPSS program for Windows, version 16.0, was used for data analysis. Continuous and normally distributed variables were described as means ± SD, whereas categorical variables were described as proportions. Independent Student t test for normally distributed variables and Kruskal-Wallis H test for nonnormally distributed variables were used to compare differences between groups. A χ2 test was used to analyze the differences among HbA1c targeting rates. Changes over time in glycemic control, BMI, and DCP subscales in both groups were compared using repeated-measures ANCOVA with baseline values as covariates. Spearman rank correlation analysis was performed to investigate the correlation between attitudes toward diabetes and HbA1c at each visit. Cox proportional hazards modeling with forward conditional variable entry (P < 0.05) and removal (P > 0.10) was used to determine independent predictors of long-term remission. A two-sided value of P < 0.05 was considered statistically significant.
RESULTS
Between January 2008 and April 2011, 187 newly diagnosed patients with type 2 diabetes received short-term CSII treatment: 150 (80%) achieved near-normoglycemic targets after suspension of intensive treatment. A total of 20 patients relapsed within 1 month, whereas 12 dropped out because of migration to other provinces or refusal to follow-up and were excluded from further analyses. The remaining 118 patients were followed longitudinally and completed at least 12 months of follow-up. Remission for >1 year was maintained by 65 patients. For those who relapsed, 50 received oral hypoglycemic agents and 3 were treated with insulin.
Characteristics of patients at baseline
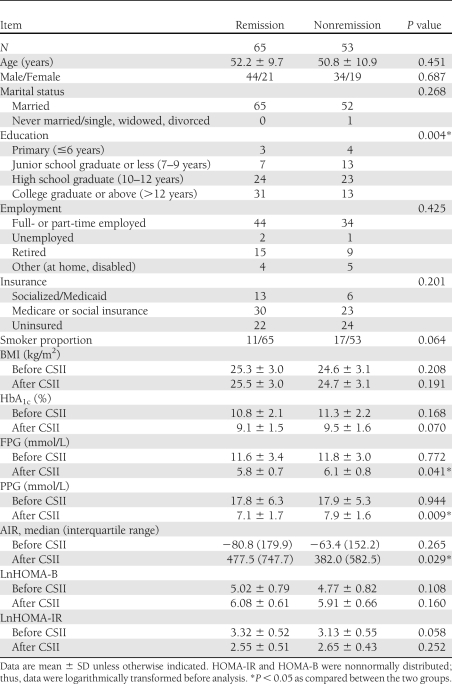
The demographic and clinical characteristics of the 118 patients grouped as remission versus nonremission before and after short-term CSII therapy are shown in Table 1. Significant reductions in HbA1c, FPG, PPG, and HOMA-IR were achieved in both groups after intensive treatment. AIR and HOMA-B increased markedly in both groups after short-term CSII. No significant differences in age, sex, marital status, employment, insurance, or smoking status were found between the two groups. BMI, HbA1c, and HOMA-B before and after short-term CSII were also similar in both groups. HOMA-IR in the remission group was higher, with marginal significance before treatment, but was not different from that of the nonremission group after CSII was suspended. However, after short-term CSII, significantly lower FPG and PPG levels as well as better AIR were found in the remission group; this group also had higher educational attainment (Table 1).
Table 1.
Clinical characteristics in remission and nonremission groups
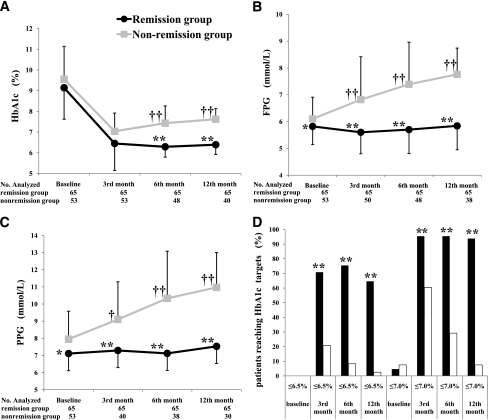
Changes in glycemic control and BMI
As shown in Fig. 1A, a dramatic decline in HbA1c occurred in both groups within the first 3 months. The level was stable during the following 9 months in the remission group, whereas a gradual ascending trend occurred in the nonremission group. Differences between the two groups were significant at follow-up visits after the 3rd month. Figure 1B shows that FPG levels after treatment in the remission group remained stable during the whole study period, whereas a steady increase occurred in the nonremission group. In a similar manner, elevation of PPG over time was observed in the nonremission group, although it remained stable in the remission group (Fig. 1C). Changes from baseline were significantly different between the two groups. Figure 1D shows the proportion of patients with HbA1c level ≤6.5 or ≤7.0% at each visit; the percentages of patients achieving the two HbA1c targets at 3, 6, and 12 months were significantly higher in the remission group.
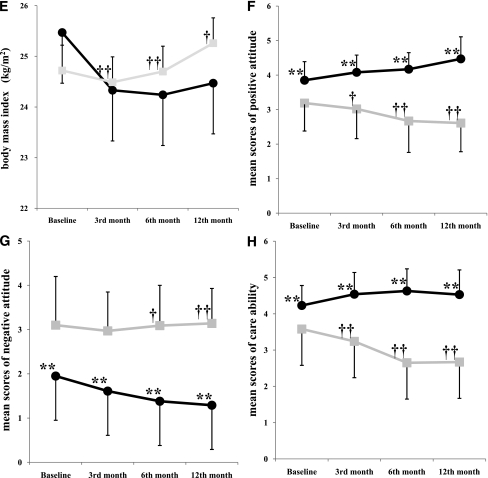
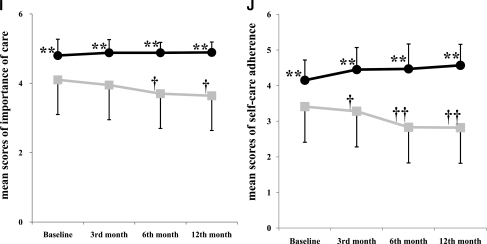
Figure 1.
Glycemic control, BMI, and attitudes toward diabetes during follow-up in remission (black circle) vs. nonremission (gray square) group. A: Changes in HbA1c. B: Changes in FPG. C: Changes in PPG. D: Percentages of patients achieving HbA1c targets ≤6.5 and ≤7.0%, respectively, in remission (black bar) vs. nonremission (white bar) group. E: Changes in BMI. F: Changes in mean scores of positive attitude. G: Changes in mean scores of negative attitude. H: Changes in mean scores of care ability. I: Changes in mean scores of importance of care. J: Changes in mean scores of self-care adherence. *P < 0.05, **P < 0.01 remission vs. nonremission group. †P < 0.05, ††P < 0.01 changes from baseline survey or glycemic level after short-term CSII, remission vs. nonremission group.
A small reduction in BMI occurred in the remission group within the first 3 months, followed by a stable maintenance; in contrast, nonremission patients gained weight during follow-up. Changes from baseline were significantly different between the two groups (Fig. 1E).
Attitudes toward diabetes
Mean scores between the two groups about patients’ attitudes toward diabetes, including positive attitude, negative attitude, care ability, importance of care, and self-care adherence, are shown in Fig. 1 E–J. For subscales of positive attitude, care ability, importance of care, and self-care adherence, significantly higher mean baseline scores were found in the remission group, whereas the nonremission group had more points for negative attitude. When compared with baseline, gradually decreasing trends were found in positive attitude, care ability, importance of care, and self-care adherence in the nonremission group, whereas these were stable or even improved in the remission group. Mean scores of negative attitude were consistently higher in the nonremission group but decreased significantly over time in the remission group.
The attitudes toward diabetes differed significantly between the two groups at the very beginning, and the differences remained, although varying, throughout the follow-up period. For example, for one item under the subscale of positive attitude listed as “Diabetes doesn’t affect my life at all,” 78.5% of patients in the remission group at baseline survey believed so, and this rose to 89.2, 92.6, and 87.7%, respectively, at the 3-, 6-, and 12-month follow-up visits, whereas 39.6% of patients in the nonremission group at baseline survey agreed, but the percentage decreased to only 11.1% by the 12th month. Similar changes were observed in importance of care, care ability, and self-care adherence. On the aspect of negative attitude, 12.3% of the remission patients at baseline survey felt that “I’m not as good as others because of my diabetes,” but the percentage fell to only 6.2% at the end visit, whereas the corresponding percentages in nonremission patients were 52.8 and 66.7%, respectively.
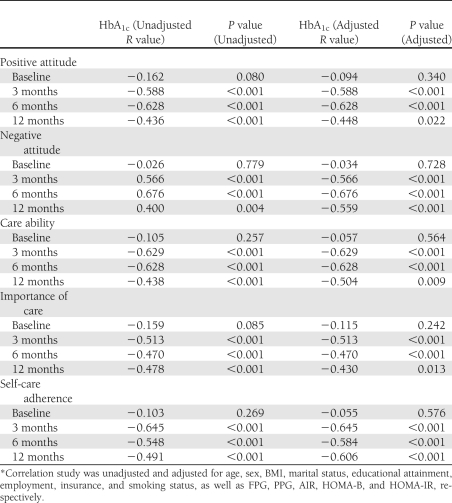
Relationship between HbA1c and attitudes toward diabetes
The relationships between HbA1c at every visit and attitudes toward diabetes were unadjusted for patients’ sociodemographic characteristics, including age, sex, marital status, educational attainment, employment, insurance, and smoking status, as well as laboratory data such as FPG, PPG, AIR, HOMA-B, and HOMA-IR. The attitudes toward diabetes at baseline did not correlate with HbA1c after CSII. However, HbA1c values were negatively correlated to positive attitude, care ability, importance of care, and self-care adherence at each follow-up visit (r = −0.44 to −0.65, P < 0.01), whereas they were positively correlated with negative attitude (r = 0.40 to 0.68, P < 0.01). When the analysis model was adjusted for all the above factors, the relationship remained significant (P < 0.05). This indicated that higher scores for positive attitude, care ability, importance of care, and self-care adherence and lower scores for negative attitude were associated with lower HbA1c levels (Table 2).
Table 2.
Relationship between HbA1c and attitudes toward diabetes categorized by visits*
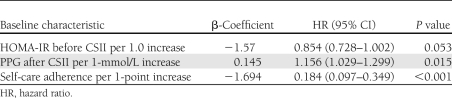
Baseline characteristics predictive of long-term remission
Univariate analysis of baseline characteristics identified that all the variables with a P value <0.2 were significant determinants for long-term remission. These included educational attainment; nonsmoker; lower FPG, PPG, and HbA1c; greater AIR after CSII; and all five aspects of attitudes toward diabetes. Multivariate Cox proportional hazards modeling showed that every 1-point increment achieved in self-care adherence decreased risk of relapse by 81.6%. Furthermore, HOMA-IR at baseline increased per 1.0 reduced the risk of relapse by 14.6% with borderline significance, and every 1 mmol/L increment of PPG after CSII increased relapse risk by 15.6% (Table 3).
Table 3.
Independent baseline predictors of long-term remission in multivariate Cox proportional hazards modeling
CONCLUSIONS
As shown previously (3–7), short-term intensive CSII was very effective for improving glycemic control, β-cell function, and insulin sensitivity, resulting in drug-free remission in patients with newly diagnosed type 2 diabetes. Our results indicate that patients with higher educational attainment, better glycemic control, and greater restoration of AIR after short-term CSII were more likely to maintain long-term remission. Investigation of individual attitudes toward diabetes showed that patients reporting increased positive attitude, greater belief in importance of care, better care ability, and self-care adherence maintained better and prolonged glycemic control. Correlation analysis also showed that positive attitude, importance of care, care ability, and self-care adherence were negatively correlated to HbA1c levels, whereas negative attitude was positively correlated to HbA1c levels. Self-care adherence and higher HOMA-IR before treatment were independent predictors for remaining in remission, and higher PPG after CSII was a risk factor for relapse.
Analysis of baseline characteristics provided some information as to which patients might benefit. Except for restoration of AIR after intensive treatment, which was also an indicator of improved β-cell function, other factors, including educational attainment, attitudes toward diabetes, and glycemic control after intensive treatment, were closely while indirectly related to each other, with diabetes self-management as the cord or bridge linking these factors. The Kidney Early Evaluation Program (KEEP), a recent large-scale observational cohort study, reported that higher educational attainment was independently associated with a lower prevalence of chronic diseases (including diabetes) and short-term mortality in all age and race/ethnic groups (11). Type 2 diabetes is a lifelong disease during which patients implement most of their own clinician-directed care. Diabetes self-management is physically and emotionally demanding and requires comprehensive knowledge and skills. Patients with more knowledge are more likely to be capable of and confident about managing their own healthcare and, thus, might have a more positive attitude, all of which can favor a better outcome. Likewise, patients with a positive attitude are usually more active and engaged in diabetes education and lifestyle intervention. In contrast, those with inadequate literacy may be less prepared and poorly supported; they may also find their diabetes self-care regimen overwhelming, thus leading to poorer glycemic control and clinical outcomes (12). Several studies support this view. In Chinese patients with type 2 diabetes living in urban community settings, Zhong et al. (13) found that best performances in self-management were achieved in those with a high degree of positive attitudes toward diabetes. In Jordanian patients with type 2 diabetes, a negative attitude toward diabetes and nonadherence to diabetes self-management behaviors were significantly associated with increased odds for poor glycemic control (14). Moreover, various independent studies indicate that patients with diabetes and depression (or in a depressive state) had poorer diabetes self-care and felt that they had less control over their disease (15–17). The clinical significance of assessing attitudes toward diabetes before implementing treatment may identify and predict patients who might be more likely to benefit from short-term intensive CSII as well as other treatments. This needs to be investigated in larger prospective studies.
The impact of attitudes toward diabetes on long-term remission not only manifested from the very beginning but also remained, with some variation, in both groups throughout the follow-up period. The effect stabilized or even optimized in the remission group but worsened over time with the increment of glycemic level in the nonremission group. Various cross-sectional and prospective studies evaluate the relationship between diabetes self-efficacy and glycemic control (18–22). Hibbard et al. (18) evaluated psychometric activation in chronic diseases, including diabetes, and found that the activation to disease was changeable, with a positive change being associated with benefits in self-management behaviors as well as clinical outcomes, including glycemic control. In a study of Croatian patients, Skocić et al. (19) suggested that psychopathological symptoms or stress contributed to poor glycemic control, whereas poor glycemic control increased psychological dysfunctions, or that both poor glycemic control and psychopathology occurred as a result of a third unknown underlying mechanism. A Japanese prospective study also shows that current glycemic control was important for psychological well-being and that psychosocial factors influenced future glycemic control independently of current glycemic control (20). Thus, from this perspective, short-term intensive treatment in newly diagnosed type 2 diabetic patients with greater self-efficacy not only results in immediate good glycemic control but also improves psychological well-being, both of which are favorable for a better clinical outcome. Therefore, for patients with suboptimal attitudes toward diabetes, the need for constant motivation and one-on-one level education at frequent intervals to ensure better adherence to intervention should be stressed.
Cox proportional hazards modeling showed that patients with higher self-care adherence were more likely to maintain long-term remission. Previous studies conclude that diabetes self-efficacy is the only factor that directly reinforces adherence and that adherence has a direct positive association with good glycemic control (20). Other studies show that better adherence to self-care regimens could reduce mortality and disability, improve quality of life, and reduce health care costs (21). Adherence to SMBG, one of the major contents of diabetes self-management, was significantly different as observed in the two groups in our study. More patients in the remission group reported SMBG at the 6th (73.8 vs. 45.3%, P < 0.001) and 12th month (63.1 vs. 30.2%, P < 0.001) as compared with the nonremission group, though the percentages were similar at baseline and the 3rd month. A study in adolescents with type 1 diabetes shows that lower frequency of blood glucose monitoring is associated with higher HbA1c, and that 38% of the link between depression and HbA1c level could be explained by blood glucose monitoring (23). In our study, those with higher PPG after short-term CSII were more likely to relapse sooner. Changes in PPG after CSII appear to be a sensitive marker that reflected the efficacy of short-term intensive treatment. The higher HOMA-IR before treatment being a protective factor is consistent with preliminary results from an ongoing study using combination therapies with CSII (A.C., Z.H., X.W., W.D., J.W., L.L., Q.C., H.X., and Y.L, unpublished data). On the basis of the results of these collective studies, we found that patients with newly diagnosed type 2 diabetes with more severe insulin resistance were usually those with higher BMI and better compensational insulin secretion. Therefore, they might also have a larger capacity for improvement of insulin sensitivity through intensive insulin treatment along with exercise and weight reduction. Further study is needed to address this hypothesis.
Limitations of our study include a small study cohort and use of a brief questionnaire. A much larger study with a more comprehensive patient reported–outcomes instrument may enable more definitive correlations to be identified. In addition, self-management behaviors, including adherence to diet, exercise, and SMBG frequencies, should be included in future studies. Furthermore, clinician attitudes, beliefs, and communication skills that can influence patients’ perception and attitudes toward diabetes (24,25) were not investigated but should be assessed in future studies.
Despite some limitations, we conclude that patient attitude toward diabetes affects the potential to remain in remission after short-term CSII. Furthermore, responses in PPG, AIR, and HOMA-IR also predicted positive outcomes. Our findings on positive attitude are consistent with studies on long-term self-management and adherence in patients requiring ongoing antidiabetes pharmacotherapy. Therefore, clinicians should continually assess attitude and motivate patients to adhere to the core components of diabetes care and self-management. This should be done in association with monitoring of PPG and HOMA indices of β-cell function in addition to standard measures of glycemic control when implementing intensive antidiabetes regimens. Patients achieving remission should also be seen at regular intervals to minimize risk of relapse.
Acknowledgments
This study was supported by the Natural Science Fund of China (81070659); the Key Science and Technique Research Project of Guangdong Province (9251008901000030); the Research Fund for the Doctoral Program of Higher Education of China (2009171110054); the Science and Technique Research Project of Guangzhou Municipality, Guangdong Province, China (2010J-E521); and the 5010 program of Sun Yat-sen University.
No potential conflicts of interest relevant to this article were reported.
A.C. and Z.H. analyzed data and wrote the manuscript. X.W., W.D., J.W., L.L., Q.C., and H.X. contributed to data collection. Y.L. designed and organized the study and reviewed the manuscript. Y.L. is the guarantor of this work and, as such, had full access to all data in the study and takes responsibility for the integrity of data and the accuracy of the data analysis.
Parts of this study were presented in abstract form at the 71st Scientific Sessions of the American Diabetes Association, San Diego, California, 24–28 June 2011.
The authors would like to extend their appreciation to Dr. James E. Foley, Global Medical Affairs at Novartis, and Xia Wang, MD, Advanced Rehabilitation Specialist, LLC, for editorial advice. They would also like to thank Professor Yuantao Hao, Department of Epidemiology and Biostatistics, School of Public Health, Sun Yat-sen University, for statistical support.
References
- 1.Nathan DM, Buse JB, Davidson MB, et al. ; American Diabetes Association; European Association for the Study of Diabetes Medical management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 2009;52:17–30 [DOI] [PubMed] [Google Scholar]
- 2.Schernthaner G, Barnett AH, Betteridge DJ, et al. Is the ADA/EASD algorithm for the management of type 2 diabetes (January 2009) based on evidence or opinion? A critical analysis. Diabetologia 2010;53:1258–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li YB, Xu W, Liao ZH, et al. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients is associated with improvement of β-cell function. Diabetes Care 2004;27:2597–2602 [DOI] [PubMed] [Google Scholar]
- 4.Weng JP, Li YB, Xu W, et al. Effect of intensive insulin therapy on β-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet 2008;371:1753–1760 [DOI] [PubMed] [Google Scholar]
- 5.Ilkova H, Glaser B, Tunçkale A, Bagriaçik N, Cerasi E. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients by transient intensive insulin treatment. Diabetes Care 1997;20:1353–1356 [DOI] [PubMed] [Google Scholar]
- 6.Ryan EA, Imes S, Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Diabetes Care 2004;27:1028–1032 [DOI] [PubMed] [Google Scholar]
- 7.Hu Y, Li L, Xu Y, et al. Short-term intensive therapy in newly diagnosed type 2 diabetes partially restores both insulin sensitivity and β-cell function in subjects with long-term remission. Diabetes Care 2011;34:1848–1853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the Diabetes Care Profile. Eval Health Prof 1996;19:208–230 [DOI] [PubMed] [Google Scholar]
- 9.Fitzgerald JT, Anderson RM, Gruppen LD, et al. The reliability of the Diabetes Care Profile for African Americans. Eval Health Prof 1998;21:52–65 [DOI] [PubMed] [Google Scholar]
- 10.Chen ZL, Zhang ZL, Liao ZH, et al. Self-management and quality of life in patients with diabetes mellitus. Chin J of Behavioral Med Sci 2006;15:434–436 [Google Scholar]
- 11.Choi AI, Weekley CC, Chen SC, et al. Association of educational attainment with chronic disease and mortality: the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 2011;58:228–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep 2006;121:245–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhong X, Tanasugarn C, Fisher EB, Krudsood S, Nityasuddhi D. Awareness and practices of self-management and influence factors among individuals with type 2 diabetes in urban community settings in Anhui Province, China. Southeast Asian J Trop Med Public Health 2011;42:185–186, 184, 187–196 [PubMed]
- 14.Khattab M, Khader YS, Al-Khawaldeh A, Ajlouni K. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complications 2010;24:84–89 [DOI] [PubMed] [Google Scholar]
- 15.Egede LE, Ellis C. The effects of depression on diabetes knowledge, diabetes self-management, and perceived control in indigent patients with type 2 diabetes. Diabetes Technol Ther 2008;10:213–219 [DOI] [PubMed] [Google Scholar]
- 16.Anderson RJ, Grigsby AB, Freedland KE, et al. Anxiety and poor glycemic control: a meta-analytic review of the literature. Int J Psychiatry Med 2002;32:235–247 [DOI] [PubMed] [Google Scholar]
- 17.Wagner JA, Tennen H, Osborn CY. Lifetime depression and diabetes self-management in women with type 2 diabetes: a case-control study. Diabet Med 2010;27:713–717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res 2007;42:1443–1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skocić M, Rudan V, Brajković L, Marcinko D. Relationship among psychopathological dimensions, coping mechanisms, and glycemic control in a Croatian sample of adolescents with diabetes mellitus type 1. Eur Child Adolesc Psychiatry 2010;19:525–533 [DOI] [PubMed] [Google Scholar]
- 20.Nakahara R, Yoshiuchi K, Kumano H, Hara Y, Suematsu H, Kuboki T. Prospective study on influence of psychosocial factors on glycemic control in Japanese patients with type 2 diabetes. Psychosomatics 2006;47:240–246 [DOI] [PubMed] [Google Scholar]
- 21.King DK, Glasgow RE, Toobert DJ, et al. Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care 2010;33:751–753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skelly AH, Marshall JR, Haughey BP, Davis PJ, Dunford RG. Self-efficacy and confidence in outcomes as determinants of self-care practices in inner-city, African-American women with non-insulin-dependent diabetes. Diabetes Educ 1995;21:38–46 [DOI] [PubMed] [Google Scholar]
- 23.Herzer M, Hood KK. Anxiety symptoms in adolescents with type 1 diabetes: association with blood glucose monitoring and glycemic control. J Pediatr Psychol 2010;35:415–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peyrot M, Rubin RR, Funnell MM, Siminerio LM. Access to diabetes self-management education: results of national surveys of patients, educators, and physicians. Diabetes Educ 2009;35:246–248, 252–256, 258–263 [DOI] [PubMed] [Google Scholar]
- 25.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract 2011;93:1–9 [DOI] [PubMed] [Google Scholar]