Abstract
Background
The Community Clinical Oncology Program (CCOP) plays an essential role in the National Cancer Institute’s (NCI) efforts to increase enrollment in clinical trials. There is currently little practical guidance in the literature to assist provider organizations in analyzing the return on investment (ROI), or business case, for establishing and operating a provider-based research network (PBRN) such as the CCOP. This paper presents a conceptual model of the business case for PBRN participation and provides a spreadsheet-based tool and advice for evaluating the business case for provider participation in a CCOP organization.
Methods
A comparative, case-study approach was used to identify key components of the business case for hospitals attempting to support a CCOP research infrastructure. Semi-structured interviews were conducted with providers and administrators. Key themes were identified and used to develop the financial analysis tool.
Results
Key components of the business case include CCOP start-up costs, direct revenue from the NCI CCOP grant, direct expenses required to maintain the CCOP research infrastructure, and incidental benefits, most notably downstream revenues from CCOP patients. The value of incidental benefits is recognized as an important contributor to the business case for CCOP participation, but is not currently calculated.
Conclusions
Providing a method for documenting the business case for CCOP or other PBRN involvement will contribute to the long-term sustainability and expansion of these programs by improving providers’ understanding of the financial implications of participation.
Keywords: Investments, Clinical Trials as a Topic, Community Networks, Research Support as Topic, Health Services Research, Financial Management, Financial Support, Organizational Decision Making, Cost Benefit Analysis, Cost and Cost Analysis
Background
Recent advances in clinical research and medicine require a new, more comprehensive research infrastructure to evaluate comparative effectiveness and translate basic science discoveries into evidence-based practice1–4. Federally-funded provider-based research networks (PBRNs) offer a promising mechanism for providing the type of large-scale, predictable research support needed to engage community clinicians in the research enterprise and accelerate scientific discovery and translation1, 3–7. By linking community practitioners to academic investigators and providing consistent research support, PBRNs have the potential to expand access to innovative treatment and prevention technologies, facilitate enrollment of more heterogeneous patients to clinical trials, and provide information to researchers about the acceptability of new interventions among community-based health care providers2, 8, 9.
Several Institutes within the National Institutes of Health, as well as other federal agencies, are developing and supporting PBRNs; however, their long-term success is dependent on the sustained engagement of community clinicians in research. As of 2004, only three percent of all clinicians had reportedly participated in research10. Studies have shown that economic barriers to research participation are substantial, and that community-based providers need support, methods and tools to evaluate the financial and resource implications of engaging in clinical research11. Yet, there is currently little practical guidance in the literature to assist provider organizations trying to analyze the return on investment (ROI), or business case, for establishing and operating a PBRN.
The National Cancer Institute’s (NCI) Community Clinical Oncology Program (CCOP) is a longstanding, federally-funded PBRN that supports cancer research. The CCOP has demonstrated success in engaging community clinicians in research, increasing enrollment to clinical trials and facilitating translation of evidence into practice12; therefore, the CCOP provides a unique opportunity to begin to identify the financial implications of PBRN participation. As part of a larger study to identify factors that motivate CCOP participation among hospital and physician practice leaders, we identified key components of the business case to provider organizations for participating in the CCOP in order to develop a tool to support future financial analyses.
To fill the existing knowledge gap, this paper presents a conceptual model of the business case for PBRN participation, a spreadsheet-based tool, and advice for evaluating the business case for provider participation in a CCOP organization. The tool can be employed by provider organizations using their own accounting data or financial estimates. Because of the CCOP’s similarity to other PBRNs, this tool has broad applicability to federally-funded clinical research networks.
The target users of this financial analysis tool include CCOP or PBRN administrators, principal investigators, and physicians or practice managers. Users must have some basic knowledge of research to develop estimates of resource requirements and unit costs and/or reimbursements associated with research activities. Expertise in finance and accounting is not required, but may be helpful in developing unit cost estimates. Completing the tool may require collaboration between individuals engaged in research and those responsible for budgeting and financial reporting for the organization.
The National Cancer Institute Community Clinical Oncology Program
The NCI CCOP was established in 1983 as a three-way partnership between the NCI’s Division of Cancer Prevention (NCI/DCP), selected cancer centers and clinical cooperative groups (CCOP research bases), and community-based networks of hospitals and physicians (CCOP organizations). NCI/DCP provides the overall direction and funding for the program; CCOP research bases design clinical trials; and CCOP organizations assist with patient accruals, data collection, and dissemination of study findings13, 14. The focus of the CCOP is Phase III clinical trials in community-practice settings in the areas of cancer prevention, control and treatment. In fiscal year 2010, the total CCOP budget was $93.6 million and supported 47 CCOP organizations in 28 states, 16 minority-based CCOP organizations in 12 states and Puerto Rico, and 12 research bases. The existing CCOP organizations include 400 hospitals and 3,520 community physicians (e.g., oncologists, surgeons, OB/GYNs).
NCI allows CCOP organizations great flexibility to organize and manage their operations in ways that meet the needs of the local patient population and physicians. Some are centralized, with a single office that houses all CCOP organization personnel, while others are more decentralized, coordinating dispersed research nurses from an administrative core2. The core of the CCOP organization is typically established within a local hospital. CCOP organization personnel coordinate with other local hospitals and physicians to form the clinical research network that provides care for cancer patients.
CCOP organizations are supported by peer-reviewed grant funding awarded by the NCI on the basis of productivity in accruing patients to clinical trials. In 2010, the average CCOP organization budget was $850,000 per year. The grant funding is intended to help support cancer research needs such as research staff, office space, and supplies by providing a consistent and reliable funding stream2. The CCOP grants are not, however, intended--nor are they typically sufficient--to cover the full cost of maintaining a research infrastructure. As a result, many provider organizations (e.g., hospitals and physician practices) subsidize CCOP organization operations, with the extent of the subsidy dependent on the size and structure of the local CCOP organization. Whether there is a business case for CCOP participation depends on the extent to which the benefits to the provider organization outweigh the costs of these subsidies. Like many programs, the CCOP faces challenges to its sustainability13, 15, 16. Thus, it is imperative that provider organizations understand the financial implications of investing in and operating PBRNs such as the CCOP in order to make informed decisions about participation.
Methods
Study Sample, Data, and Tool Development
The study sample used to develop the business case tool included five hospitals at different stages of maturity in terms of affiliation with CCOP organizations. Maturity was chosen as the primary selection criterion to allow identification of costs and benefits during all phases of establishing and operating a CCOP organization. One hospital in our sample was an applicant to the CCOP that had not yet been awarded a CCOP grant. This hospital provided information about the costs of preparing to apply to become and start-up a CCOP organization, as well as insights about projected benefits considered while making the decision to engage with the CCOP. Two other hospitals were part of relatively new CCOP organizations, in operation for less than 10 years. These hospitals provided information about the costs and benefits during the early years of growth as a CCOP organization. The final two hospitals were part of mature CCOP organizations, in operation for more than 10 years, chosen to provide information about costs and benefits given their multiple years of experience with the CCOP and clinical research. Selection based on maturity created variation in data sources and the financial data collected (e.g., estimates versus actual experience), and this allowed creation of a comprehensive tool applicable at all stages of PBRN participation.
Primary data were collected through semi-structured interviews with key personnel responsible for CCOP-related activities. At each study site, interviewees included the Principal Investigator of the CCOP grant or grant application, the CCOP organization Administrator (except at the applicant site), CCOP organization-affiliated physicians, research nurses, clinical research associates, and key hospital personnel responsible for financial operations. By including representatives from both the CCOP organization and the sponsoring hospital, we were able to collect information from diverse stakeholders to increase the generality of the model and incorporate potentially disparate objectives.
Interviews were transcribed and coded, using Atlas.ti to support the coding process17. Codes were reviewed and discussed among research team members and modified as new themes emerged related to costs and benefits of CCOP participation. From the coded interviews, key components of the business case (e.g., personnel, supply and laboratory costs; grant funds; philanthropic support; industry trial revenues) were identified and used to develop a conceptual model of the business case for PBRN participation. Because the goal was to create a model with maximum flexibility for users, we emphasized breadth and included financial flows that were mentioned by anyone during interviews.
Financial flows identified in the conceptual model were used to develop an EXCEL-based financial analysis tool to measure the ROI to a provider from investing in the CCOP organization18. Data collection fields are derived from costs and benefits identified by key informants, and based on data available from the internal, management accounting systems of three CCOP organizations. The business case tool was tested with financial managers and CCOP administrators from three study sites to determine usefulness and feasibility of data collection. Although the tool was designed primarily from the perspective of the hospital, its categories are broad and capture resources also relevant to physician practices interested in PBRN participation (e.g., supplies, provider and non-provider personnel time).
Results and Discussion
Conceptual Model
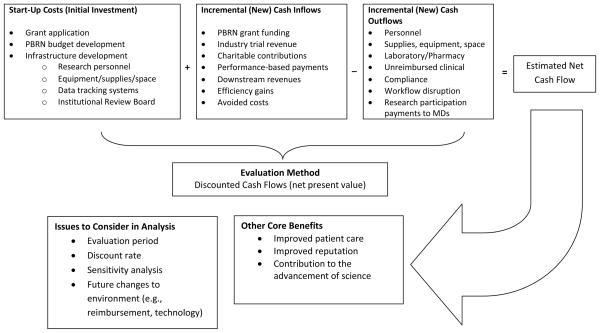
The conceptual model of the business case for PBRN participation is presented in Figure 1. The model shows the primary components of the business case, including the costs involved with developing and starting up a PBRN (the initial investment costs) and possible sources of cash inflow and outflow from participating in a PBRN. Cash inflows and outflows generally reflect cash flows new, or incremental, to the organization as a result of participating in the PBRN. By including incremental cash flows, the financial contribution of the PBRN to the organization’s bottom line can be estimated.
Figure 1. Conceptual Model of the Business Case for Hospital Participation in a PBRN.
Figure adapted from: Pink, GH and MS Thomas. (2005). The Business Case for Quality: Tracking the Cash Flows Progress Report. Unpublished report submitted to the Center for Health Management Research.
The net cash flow from PBRN participation reflects the difference between cash inflows and outflows in each year over the analysis timeframe. Because cash flows occur at various points in time, it is necessary to account for the opportunity cost of investing funds in the PBRN versus another alternative investment. This is accomplished by discounting future cash flows using a discount rate that reflects the return available on a similar alternative investment. An organization might start by assessing its overall cost of existing financing (i.e., its long-term borrowing and internally generated cash) to identify a discount rate. At a minimum, a rate that reflects general inflation should be chosen. The identified rate can then be adjusted up or down to reflect the uncertainty (or risk) of the PBRN cash flows versus cash flows obtained from other services provided by the organization. A higher discount rate would be used to reflect higher risk, and a lower discount rate to reflect lower risk.
Once future cash flows are discounted to the present, they can be summed and compared to the initial investment cost using the concept of net present value. If the discounted value of future net cash flows exceeds the cost of investing in the PBRN, then the PBRN investment has a positive business case (i.e., it creates value for the organization). If net present value is negative, the PBRN does not break even. The resulting net present value can be used by itself, or compared to similar analyses of other potential investments to provide information to guide an organization’s planning. For example, an organization choosing between two possible research collaboratives can identify the one with the greatest ROI.
Net present value is only one step in the overall analysis process. It provides information about the financial impacts of the PBRN; however, financial information should be used in combination with a qualitative assessment of the effects of PBRN participation on patient care, organizational reputation, and the contribution toward scientific discovery. It is often the qualitative benefits that make the business case for clinical interventions that may not be inherently profitable in a traditional sense19. Thus, the overall assessment of the business case should be collaborative, and involve stakeholders from multiple disciplines within the organization.
Structure of the Financial Analysis Tool
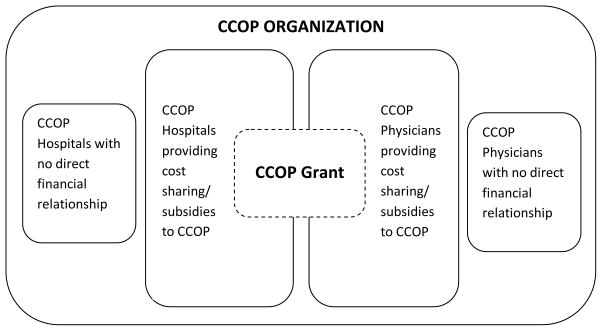
In the conceptual model and the business case tool, the primary unit of analysis is the provider affiliated with the CCOP organization (hospital/health system or physician practice). We use the term “provider organization” in this article to refer to either of these affiliated providers. Figure 2 describes two possible relationships between a provider organization and a CCOP organization – those that involve cost-sharing and those that do not.
Figure 2.
The Relationship of Provider Organizations to a CCOP Organization
The business case tool allows organizations to track direct, indirect and incidental financial flows from CCOP participation. Direct financial flows are transactions that involve actual cash transfers between parties that are directly attributable to the CCOP organization. Indirect financial flows represent the allocation of shared resources that support not only the CCOP organization, but also other divisions, units or activities within the provider organizations. Incidental financial flows are benefits and costs that accrue to provider organizations as a result of their affiliation with the CCOP organization, but that are less easy to monetize because they are not characterized by circumscribed cash transfers.
The tool is a series of spreadsheets, designed to be completed by extracting data from management accounting systems, and making estimates based on personnel reports of time and effort, unit costs of supplies and laboratory tests; and revenue generated specifically from research efforts. The tool allows users to collect all data potentially relevant to the business case including direct, indirect and incidental financial flows; however, users need only fill out the elements and worksheets relevant to their specific circumstances.
The tool is unique in that it extends the traditional boundaries of CCOP organization financial reporting beyond the CCOP grant to include costs and benefits accruing to participating provider organizations. Specifically, the tool allows for capture of: (1) costs included on the CCOP organization budget provided to NCI, and grant funding received from NCI to help support those costs, and (2) costs and benefits that accrue to individual provider organizations as a result of participating in the CCOP organization but that are not recognized directly in the CCOP grant.
The tool is designed to allow data collection during two important stages of CCOP organization engagement: (1) start-up, and (2) ongoing operations. For providers considering establishing a CCOP organization, there is a worksheet provided to collect start-up or initial investment costs. The remaining worksheets collect data related to the ongoing operation of a CCOP organization. Operating cost data may be collected for a single year or for up to five years to accommodate the timeframe of most CCOP grants and the planning horizon of many organizations. With this design, providers can use the tool to project the ROI to establish a CCOP organization, or the future returns anticipated from renewing a CCOP grant or continuing to support an existing CCOP organization. The tool can also be used retrospectively to analyze the actual return on an initial or continued investment in a CCOP organization.
The tool contains ten worksheets. The purpose and content of each is summarized in Table 1. The first worksheet (“Instructions”) provides instructions for use. The second worksheet (“Organizational Information”) collects name, location, type (hospital or physician practice), physician practice specialty (if applicable), CCOP organization age, and the provider’s cost of capital (discount rate). The discount rate is used as an input to the ROI analysis and allows providers to recognize the opportunity cost of using funds to support the CCOP organization. Providers may choose to calculate a CCOP-specific discount rate, or choose from a menu of possible discount rates that reflect an approximation of the rate of inflation, the average cost of long-term taxable or tax-exempt bonds, or other, higher discount rates to reflect greater risk. The discount rate is one of the most complex and uncertain estimates in the discounted cash flow analysis and can affect the outcome. Users should consider conducting the business case analysis using alternative discount rate assumptions to assess the effect of the discount rate on the net present value20.
Table 1.
Financial Analysis Tool: Purpose and Content of Worksheets
| Worksheet | Purpose | Content | User Input Required? |
|---|---|---|---|
| 1. Instructions | To describe the structure, content and purpose of the financial analysis tool | Instructions for use and description of color coding scheme | No |
| 2. Organizational Information | To identify the organization for which ROI is calculated, and to collect the cost of capital used to discount future cash flows | Organizational descriptors including:
|
Yes |
| 3. Initial Investment | To collect data about the costs of planning for and starting up a CCOP | Costs including:
|
Yes (if applicable) |
| 4. Outflows – CCOP | To collect data about the on-going costs of operating and maintaining a CCOP | Costs including:
|
Yes (if applicable) |
| 5. Outflows – Industry | To collect data about the on-going costs of participating in industry trials made possible through the CCOP research infrastructure or recognition | ||
| 6. Inflows – CCOP | To collect data about cash inflows to the provider as a direct result of the CCOP | Cash inflows including:
|
Yes (if applicable) |
| 7. Inflows – Industry | To collect data about cash inflows to the provider from industry trials made possible through the CCOP research infrastructure or recognition | Accrual based or lump sum payments | Yes (if applicable) |
| 8. Incidental Benefits & Costs | To collect data about financial benefits and costs that accrue to a provider participating in the CCOP, but that are not captured in the CCOP grant or are not easily quantified | Benefits including:
|
Yes (if applicable) |
| 9. Cash Flow Summary | To summarize all of the estimated financial inflows and outflows to the provider from CCOP participation | CCOP, industry and incidental inflows and outflows entered in worksheets 4–8 | No |
| 10. Return on Investment | To calculate the ROI, or business case, to the provider for participating in the CCOP | ROI calculated using discounted cash flow analysis under three scenarios:
|
No |
The main inputs to the business case analysis are collected in worksheets three through seven. Worksheet three (“Initial Investment”) collects the costs associated with investing in a CCOP organization, for example personnel time and renovation or recruitment costs. Worksheets four (“Outflows-CCOP”) through seven (“Inflows-Industry”) are designed to collect direct and indirect financial inflows and outflows associated with: (1) CCOP organization participation, and (2) industry trial participation made possible by the research infrastructure developed through the CCOP organization. Outflows are classified into major categories including: personnel; office supplies; laboratory, pharmacy or unreimbursed clinical costs; equipment; construction/renovation or recruitment; transfers of CCOP grant funds to participants; and direct cash subsidies from the provider to the CCOP organization.
Provider support of the CCOP organization through shared resources such as information technology, regulatory, or finance departments is an optional input accounted for through an allocation of indirect costs from the provider to the CCOP organization. The tool is designed to allocate indirect costs as a percentage of direct costs applying a user-provided allocation percentage; however, this field could be easily modified to accommodate other allocation methods.
Cash inflows include the CCOP grant funding if it is administered within a particular provider organization, any funds received from participation in commercial or industry trials that would not have been possible without CCOP affiliation, and any funds received by the provider from the CCOP grant (if the grant resides with a different provider).
Worksheet eight (“Incidental Benefits & Costs”) allows providers to consider costs and benefits that accrue incidental to CCOP participation. Although some incidental costs and benefits may be characterized by cash flows, quantifying and attributing those cash flows to CCOP participation can be challenging. Although no excess income is generated by the CCOP organization itself, clinical research provides an infrastructure that can be built upon by the provider organization in a way that could result in additional revenue beyond the CCOP activity. For example, study sites indicated that the most important incidental benefit is the ability to provide care to patients that remain in the health system while participating in the clinical research activity. By providing access to innovative treatment technologies, CCOP affiliation allows providers to treat patients locally who otherwise would be referred to major cancer centers. Further, these patients may require additional services outside the clinical trial protocol that could result in downstream revenue.
Although none of the study sites were tracking revenue from patients on clinical trials, downstream revenue was consistently recognized by informants as one of the primary components for making the business case for CCOP organization participation. Therefore, the tool provides a pragmatic method for estimating the contribution of downstream revenues. By looking at trends in the number of cancer patients over time, particularly those with cancers for which a study protocol is available, providers can enter an estimate of the increase in patients likely attributable to CCOP participation. Providers can also enter an estimate of average profit margin (revenue minus cost) for different types of patients. The tool multiplies the incremental number of cancer patients by the average profit margin to provide a pragmatic estimate of the financial contribution of keeping patients local.
Key informants identified several other incidental benefits of CCOP participation. Some felt the CCOP organization allowed the provider to attract charitable contributions; therefore, the tool provides a field for entering the value of charitable contributions received specifically to support CCOP organization operations, or more generally to support cancer research. The tool also allows for the entry of non-CCOP grant funds received to support cancer research, as well as performance-based payments received for improved cancer care quality attributable to CCOP participation.
Several key informants reported that CCOP participation may help recruit or retain staff, in particular, physicians. Offering clinical trials in a more rural practice setting, for example, might be used as a recruitment device to attract and retain higher-quality physicians. In worksheet eight, users of the financial analysis tool are able to enter an estimate of the number of nurses and/or physicians retained. Costs of turnover identified in the research literature are included to allow providers to estimate the value of avoided turnover costs. Pragmatic estimates of turnover rates could be developed by comparing turnover of CCOP organization-affiliated employees or physicians to turnover among employees and physicians in other parts of the organization. The value of physician recruitment is not included directly since practices would recruit physicians regardless of participation in a CCOP organization; however, users could modify the tool to include physician recruitment benefits if they were deemed substantial.
The tool also allows users to enter an estimate of avoided costs due to improved quality. It was noted, for example, that following a protocol-specified treatment regimen might lead to fewer medication errors. Providers could compare numbers of medical errors, avoidable complications, or patient-safety related events among cancer patients before and after CCOP participation to estimate avoided costs. Although none of the sites indicated productivity losses associated with provider participation in the CCOP organization, a field is included to allow users to enter an estimate if they feel that this would be an important incidental cost of participation. Estimates might come from comparisons of patient volume, relative value units, revenue generation or other measures of productivity among physicians participating and not participating in the CCOP organization, or among participating physicians before and after joining the CCOP organization. Although the pragmatic estimates described suffer from weaknesses, most importantly regression to the mean and the effects of non-CCOP related trends, they provide a point from which to begin to assess the value of CCOP participation beyond the grant funding received from NCI.
The final worksheets (“Cash Flow Summary” and “Return on Investment”) (nine and ten) provide a summary of the cash flows associated with CCOP participation and an estimate of the ROI. The cash flow summary allows organizations to quickly examine the largest financial flows associated with CCOP participation, and to consider areas where costs might be reduced or revenues increased. The ROI worksheet allows organizations to examine the business case under three scenarios. The most conservative scenario estimates the business case for CCOP participation including only cash flows directly and clearly attributable to the CCOP organization. The seconds cenario includes cash flows from the first scenario as well as cash flows from industry trials to allow for an estimate of the business case for participation in research facilitated by the existence of the CCOP organization. The most aggressive scenario includes all cash flows from the CCOP organization and industry trials as well as incidental costs and benefits to provide a comprehensive ROI estimate that considers all potential effects of CCOP participation on the organization. ROI is estimated using discounted cash flow analysis, where the net present value reflects the dollar impact of CCOP affiliation on the organization.
Because formulas are embedded in the model, users have the ability to vary assumptions throughout the model and conduct sensitivity analyses to assess the effects of uncertainty on the business case. Users are encouraged to change assumptions, e.g., discount rate and downstream revenue projections, to assess whether the net present value is particularly sensitive to certain estimates, and to identify the range of possible returns.
Discussion
The goal of this study was to identify and begin to systematize the elements of the business case to providers for participating in a PBRN. The conceptual model and financial tool were developed to provide an overview of the types of financial flows provider organizations can expect when engaging in a CCOP organization or other similar PBRN, and to introduce methods for developing pragmatic estimates of ROI. The lack of this type of pragmatic guidance has been noted as one barrier to expanding providers’ participation in clinical research11. As providers’ financial resources continue to be stressed by economic conditions, implementation of meaningful use regulations and health reform, program leaders will increasingly be required to justify their programs’ continued support. The tool described in this paper provides one way of demonstrating the value of PBRNs by allowing providers to identify and, to the extent possible, estimate the business case for participating in a PBRN.
The tool has several limitations that should be noted. First, developing scientific measures of components of the business case was beyond the scope of this study. Still, our tool provides a framework and systematic method to begin to assemble the data required to assess the business case, and provides a roadmap for data collection going forward. Applicants to PBRN programs can use the tool to inform decisions about whether to proceed, and to develop budgets, strengthen their applications by demonstrating an understanding of the costs associated with PBRN participation, and clarifying plans for cost sharing among the members of the proposed PBRN. Existing CCOP organizations or other PBRNs can use the tool in discussions with executive leaders and financial officers as they prepare budgets, negotiate funding levels, or make decisions about submitting PBRN renewal applications.
Second, the tool does not currently take into account potential changes to healthcare reimbursement such as bundling of payments or accountable care organizations; however, the tool could be easily modified by users to accommodate alternative payment strategies. Finally, although we achieved broad representation in the stakeholders interviewed to develop the model, it is possible we have omitted elements of the business case that were not mentioned by our stakeholders.
Perhaps the greatest strength of this financial tool is in helping provider organizations think through not only the resource commitment that is required to engage with a PBRN like the CCOP, but also the benefits that such engagement provides. Although the sites that we interviewed could not yet precisely measure incidental benefits, there was a strong belief that these benefits exist. In addition, sites routinely mentioned the value of intangible benefits, beyond those that provide a financial return. For example, the strong emphasis of the CCOP on providing novel treatment regimens keeps physicians current and allows both hospitals and physicians to offer the best options for care to their patients while they remain at home in a familiar environment. The financial tool allows organizations to assess, at a minimum, the value of incidental benefits that would be required in order for a positive business case to exist, with the understanding that significant intangible benefits are also likely to accompany CCOP participation.
Conclusion
PBRNs hold substantial promise for realizing a reengineered clinical research enterprise, including access to clinical trials in community-based provider organizations. The tool we developed in this study provides the first available approach for measuring the business case for a provider’s participation in a PBRN such as the CCOP. Although much work remains to be done, providing a systematic method for documenting the business case for PBRN participation will contribute to the long-term sustainability and expansion of community-engaged clinical research by improving providers’ understanding of the financial implications of participation.
Acknowledgments
Funding Source: The project described was supported by Award Number R01CA124402 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
We thank Erin Schaffer, Padmini Ekbote, Alexandra Moss, and J. Phil Harrop for their assistance in early work on this study.
Footnotes
Disclosures: The authors have no financial conflicts to disclose.
References
- 1.Zerhouni E. US biomedical research: basic, translational, and clinical sciences. Journal of the American Medical Association. 2005;294(11):1352–1358. doi: 10.1001/jama.294.11.1352. [DOI] [PubMed] [Google Scholar]
- 2.Minasian LM, Carpenter WR, Weiner BJ, et al. Translating research into evidence-based practice: The National Cancer Institute Community Clinical Oncology Program. Cancer. 2010;116(19):4440–4449. doi: 10.1002/cncr.25248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zerhouni E. Medicine. The NIH Roadmap. Science. 2003;302(5642):63–72. doi: 10.1126/science.1091867. [DOI] [PubMed] [Google Scholar]
- 4.Zerhouni E. Translational and clinical science -time for a new vision. New England Journal of Medicine. 2005;353(15):1621–1623. doi: 10.1056/NEJMsb053723. [DOI] [PubMed] [Google Scholar]
- 5.Lamb S, Greenlick MR, McCarty D, editors. Bridging the Gap Between Practice and Research. Washington, D.C: National Academy Press; 1998. [PubMed] [Google Scholar]
- 6.Lanier D. Practice-based research networks: laboratories for improving colorectal cancer screening in primary care practice. Medical Care. 2008;46(9 suppl 1):S147–S152. doi: 10.1097/MLR.0b013e31817f0d00. [DOI] [PubMed] [Google Scholar]
- 7.Ryan G, Berrebi C, Beckett M, et al. Reengineering the clinical research enterprise to involve more community clinicians. Implementation Science. 2011;6(36):1–7. doi: 10.1186/1748-5908-6-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sales A, Smith J, Curran G, Kochevar L. Models, strategies and tools. Theory in implementing evidence-based findings into health care practice. Journal of General Internal Medicine. 2006;21(suppl 2):S43–S49. doi: 10.1111/j.1525-1497.2006.00362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kiefe CI, Sales A. A state-of-the-art conference on implementing evidence in health care. Reasons and recommendations. Journal of General Internal Medicine. 2006;21(suppl 2):S67–S70. doi: 10.1111/j.1525-1497.2006.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahn K, Ryan G, Beckett M, et al. Bridging the gap between basic science and clinical practice: a role for community clinicians. Implementation Science. 2011;6(34):1–11. doi: 10.1186/1748-5908-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beckett M, Quiter E, Ryan G, et al. Bridging the gap between basic science and clinical practice: The role of organizations in addressing clinician barriers. Implementation Science. 2011;6(35):1–10. doi: 10.1186/1748-5908-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Cancer Institute. [accessed April 19, 2011];About the Community Clinical Oncology Program: History and Accomplishments. 2011 Available from: http://dcp.cancer.gov/programs-resources/programs/ccop/about/history.
- 13.McKinney M, Weiner BJ, Carpenter WR. Building community capacity to participate in cancer prevention research. Cancer Control. 2006;13(4):295–302. doi: 10.1177/107327480601300407. [DOI] [PubMed] [Google Scholar]
- 14.McKinney M, Weiner BJ, Wang B. Recruiting participants to cancer prevention and clinical trials: lessons from successful community oncology networks. Oncology Nursing Forum. 2006;33(5):951–959. doi: 10.1188/06.ONF.951-959. [DOI] [PubMed] [Google Scholar]
- 15.Sung NS, Crowley WFJ, Genel M, et al. Central challenges facing the national clinical research enterprise. Journal of the American Medical Association. 2003;289(10):1278–1287. doi: 10.1001/jama.289.10.1278. [DOI] [PubMed] [Google Scholar]
- 16.Institute of Medicine. Bridging the Gap Between Practice and Research: Forging Partnerships with Community-Based Drug and Alcohol Treatment. Washington, D.C: National Academy Press; 1998. [PubMed] [Google Scholar]
- 17.[computer program]. Version: ATLAS.ti. Scientific Software Development GmbH; 2010. [Google Scholar]
- 18.EXCEL [computer program]. Version 7.0. Seattle, WA: Microsoft Corporation; 2007. [Google Scholar]
- 19.Leatherman S, Berwick D, Iles D, et al. The business case for quality: case studies and an analysis. Health Affairs. 2003;22(2):17–30. doi: 10.1377/hlthaff.22.2.17. [DOI] [PubMed] [Google Scholar]
- 20.Gapenski LC. Healthcare Finance: An Introduction to Accounting and Financial Management. 4. Chicago, IL: Health Administration Press; 2008. [Google Scholar]