Abstract
Validated measures that can be administered to school populations are needed to advance knowledge of help-seeking processes and to evaluate suicide prevention programs that target help-seeking. With 6,370 students from 22 high schools, we assessed the psychometric properties of three brief measures: Help-Seeking Acceptability at School, Adult Help for Suicidal Youth, and Reject Codes of Silence. Internal consistency coefficients ranged from 0.64 – 0.84. In support of construct validity, lower scores on each scale were associated with more maladaptive coping norms; and for each one unit increase on each scale, students were one-third to one-half as likely to report suicidal ideation, suicide attempts and elevated depression.
Suicide is the third leading cause of death among 10–24 year olds in the U.S., and 5–8% of adolescents attempt suicide each year (Xu, Kochaneck, Murphy, & Tejada-Vera, 2010). A diagnosable mental, emotional or behavioral disorder is present in 80–90% of youth who die by suicide (Brent et al., 1993; Gould, Greenberg, Velting, & Shaffer, 2003). However, fewer than one-third of adolescent suicide decedents (Brent, et al., 1993; Shaffer, Gould, Fisher, Trautman, & et al., 1996) or attempters (Wu, Katic, Liu, Fan, & Fuller, 2010) were receiving treatment at the time of their death/attempt. Most suicidal adolescents do not bring their distress to the attention of an adult (Brenton, Tousignant, Bergeron, & Berthiaume, 2002; Garrison, Jackson, Addy, McKeown, & Waller, 1991; Kashani, Goddard, & Reid, 1989; Kerr, Owen, Pears, & Capaldi, 2008; Klaus, Mobilio, & King, 2009; Sourander, Helstelä, Haavisto, & Bergroth, 2001), and only a small portion of suicidal youth are recognized by adults, including adults such as school personnel or parents who presumably have the most opportunity to respond with help (Brown, Wyman, Brinales, & Gibbons, 2007)..
The inability of adults to identify young people at risk for suicide is at least partially due to adolescents’ reluctance to seek help from adults (Wyman et al., 2008). Among adolescents with emotional problems, those who experience suicidal ideation or behaviors are particularly unlikely to seek and accept help from parents, other family members (Groholt, Ekeberg, Wichstrom, & Haldorsen, 2005) or from mental health and other medical professionals (Wilson, Deane, Marshall, & Dalley, 2010). Depression in adolescents is likewise associated with a disinclination to seek help (Wilson, Rickwood, & Deane, 2007).
In recognition that suicidal youths’ reluctance to seek help from adults is a major barrier to reducing suicide deaths, an increasing number of school-based suicide prevention approaches are aimed at enhancing help-seeking among groups of youth at high-risk for suicide (Aseltine Jr & DeMartino, 2004; Aseltine, James, Schilling, & Glanovsky, 2007; Freedenthal, 2010) and among the total population of students in schools (Wyman et al., 2010). However, developing and evaluating theoretically-informed interventions designed to promote help-seeking is currently limited by: (1) minimal scientific progress toward understanding the facilitating and inhibiting factors related to help-seeking among suicidal youth, and (2) a lack of validated measures of pertinent constructs that can be administered across a large social system, such as a school. To date, most research on norms of suicidal youth has focused on their views about the acceptability of suicide (e.g., Joe & Romer, 2007), and on other indicators of maladaptive coping, such as poor interpersonal problem solving (Asarnow, Carlson, & Guthrie, 1987; Rotheram-Borus, Trautman, Dopkins, & Shrout, 1990), use of illegal substances to manage problems, and unhealthy self-reliance (Gould et al., 2004).
In this article, we report on the development and psychometric properties of scales designed to assess three dimensions of students’ attitudes pertaining to help-seeking. Congruent with a substantial body of research on youth help-seeking, we focused on measuring three constructs that, based on empirical and conceptual evidence, are likely to be critical for understanding help-seeking behavior of suicidal youth and for evaluating suicide prevention programs that target help-seeking: the acceptability of seeking help from adults for distress; perceptions about the availability of adults who can help suicidal youth; and the willingness to involve adults to help a suicidal peer despite requests for secrecy. These constructs comprise attitudes, intentions, and perceived norms, which are widely accepted predictors of health behaviors (Ajzen, 1991; Fishbein, 2008; Rosenstock, Strecher, & Becker, 1988) and mental health service utilization (Costello, Pescosolido, Angold, & Burns, 1998; Olafsdottir & Pescosolido, 2009; Pescosolido, 1992; Stiffman, Pescosolido, & Cabassa, 2004).
The acceptability of seeking help brings together theory and evidence that point to the importance of norms, expectations, and intentions in shaping help-seeking decisions and actions. Perceived norms influence an array of teen risk behaviors (Bauermeister, Elkington, Brackis-Cott, Dolezal, & Mellins, 2009; Borsari & Carey, 2003; Buhi & Goodson, 2007; Carter, Orr, & Dittus, 2009; DeJong et al., 2006; O’Donnell, Myint, O’Donnell, & Stueve, 2003; Rimal & Real, 2003) and prosocial behaviors (Barry & Wentzel, 2006; Ellis & Zarbatany, 2007). Similarly, research has begun to show that adolescents’ propensity to seek help from adults at school for emotional distress may also be influenced by their perceptions of peers’ behaviors and whether members of their social networks (e.g., friends, family members) would approve of asking for help (Wyman, et al., 2008). Likewise, knowing someone who has sought professional mental health care, which increases the likelihood of seeing it at normative, is associated with adolescents’ willingness to seek help (Rickwood & Braithwaite, 1994). Attitudes that are contrary to getting help, including the belief that people should resolve emotional problems on their own, are also related to lower intentions to seek and accept professional help for emotional problems in general (Rickwood, Deane, & Wilson, 2007; Wilson & Deane, 2010a), and for suicide concerns in particular(Gould, et al., 2004; Wilson, Deane, & Ciarrochi, 2005).
In addition to help-seeking acceptance, the research literature on mental health services suggests that adolescents’ help-seeking decisions are influenced by their perceptions of adults’ capability to respond to their needs (Sullivan, Marshall, & Schonert-Reichl, 2002). For example, adolescents who have ties to adults who they perceive as trustworthy and capable are more likely to indicate they need help for mental health problems when needed (Rickwood, Deane, Wilson, & Ciarrochi, 2005). Youth perceptions of adults in their social sphere are critical because the most frequent pathway to receiving help for adolescents is through a process involving ‘lay’ adults, such as teachers, parents or coaches, who are not mental health professionals (Costello, et al., 1998; Logan & King, 2002; Logan & King, 2001). Accordingly, adolescents’ decisions to seek help for suicide concerns for themselves or friends are likely to be influenced by their appraisals of adults’ availability and capability to respond to their suicide problems.
The willingness to overcome requests for secrecy about suicide ideation is a common target of clinical and preventive interventions, but has only recently been examined in empirical research (Wyman, et al., 2010). Across the age-span, individuals who disclose suicidal thoughts or behaviors to others frequently request that their confidante keep secret his or her suicide concerns (Quinnett, 1995; Shaffer et al., 1990). Shame about having suicidal thoughts or behaviors, fears about the consequences of disclosure, and lack of trust that others will understand may contribute to secrecy requests. Although the precise frequency of secrecy requests is unknown, ‘codes of silence’ are posited as particularly common in adolescent-to-adolescent communication about suicide. Accordingly, adolescents’ norms regarding how they and others in their peer group respond to secrecy requests may be highly influential in determining if young people will engage adults for help.
Three proposed scales, measuring conceptually distinct dimensions of help seeking were the focus of this present study. The first scale pertains to the acceptability of seeking help for emotional distress at school. This scale, developed for a prior school-based study evaluating a gatekeeper suicide prevention program (Wyman, et al., 2008), assesses students’ views on the acceptability of seeking help from adults at school for emotional distress including perceptions of peer and family support for getting help. This study extends that prior work by reporting on the psychometric properties of this measure of help-seeking norms. In this current study, we also report the psychometric properties of two scales that pertain to engaging adults to help specifically with suicide concerns, either inside or outside school. These scales assess two additional dimensions of students’ attitudes related to help-seeking for suicide concerns: adolescents’ perceptions regarding the availability of capable adults in their school to help suicidal youth, and attitudes about overcoming suicidal peers’ secrecy requests and reluctance to seek help. We examined associations with an established measure of coping norms (Gould, et al., 2004), and also examined “known-groups” validity (Carmines & Zeller, 1979; DeVellis, 2003) by evaluating associations between the scales and being a member of three groups characterized by well-established disinclination to seek help: adolescents reporting separately suicidal ideation, suicide attempts or elevated depression symptoms.
METHODS
Participants
Participants were 6,370 students from 22 high schools participating in a series of randomized trials of a universal suicide prevention program (Sources of Strength; Wyman et al., 2010). Data for this study were drawn from surveys with representative samples of students in each school conducted at baseline before any intervention occurred.
Schools enrolled in three cohorts over three consecutive school years: 2007–08, 2008–09, and 2009–10 (Table 1). Cohort 1 consisted of 2,419 racially diverse 9th–10th grade students from six high schools in a large metropolitan school district in Georgia. School size ranged from 1594 – 2654 students. Approximately one-half of 9th–10th grade classrooms were randomly selected; of students invited, 86% participated. Cohort 2 consisted of 2,737 9th–12th grade students from 12 predominantly rural high schools in New York State and North Dakota. School size ranged from 67 – 1007 students. In the six smallest schools, all students were invited to participate; in the larger schools, one-half of all classrooms were selected to participate through stratified (by grade) random sampling. Of all students invited to participate, 81% completed the survey. Cohort 3 consisted of 1,214 9th–12th grade students from 4 high schools in New York State, two rural and two urban. School size ranged from 260 – 2417 students. Approximately 1/3rd of the student body was invited to participate through stratified (by grade) random sampling. Of students invited, 76.9% completed the survey. Cohort 1 had more race/ethnic minority students compared to Cohorts 2 and 3.
Table 1.
Schools and participants
| Cohort 1 | Cohort 2 | Cohort 3 | |
|---|---|---|---|
| Schools | 6 | 12 | 4 |
| Students (N) | 2419 | 2737 | 1214 |
| Grades Participating | 9–10 | 9–12 | 9–12 |
| Age (%) | |||
| ≤14 | 31.0 | 23.8 | 12.8 |
| 15 | 44.1 | 27.2 | 27.3 |
| 16 | 18.1 | 24.5 | 23.9 |
| 17 | 3.6 | 18.7 | 25.0 |
| ≥18 | .7 | 5.7 | 4.8 |
| % Male | 47.2 | 48.0 | 47.8 |
| Race/Ethnicity (%) | |||
| White | 40.4 | 78.4 | 71.8 |
| Black | 26.8 | 3.3 | 1.7 |
| Hispanic/Latino | 17.7 | 11.3 | 14.9 |
| Other | 12.3 | 5.1 | 6.7 |
Procedures
Recruitment and survey procedures were identical in each cohort. All students or students in selected classrooms were invited to participate in an anonymous survey. Students assented to participation (waiver of parent permission); however, letters were sent to parents providing them an opportunity to decline their child’s participation (fewer than 1% declined). Surveys were administered to the entire classroom during the regular school day. Students were informed that participation was voluntary, and collection procedures assured that surveys were kept anonymous. The protocol was approved by the University of Rochester IRB.
Measures for Psychometric Evaluation
Help Seeking Acceptability at School (Wyman, et al., 2008) consists of four questions beginning with the stem, “If I was really upset and needed help…” Students respond to questions covering intentions to seek help (“I would talk to a counselor or other adult at school”), expectations of receiving help (“I believe a counselor or other adult at school could help me”) and perceived support from their friends and family for seeking help, i.e., injunctive norms (Cialdini, Reno, & Kallgren, 1990; Lapinski & Rimal, 2005; Rimal & Real, 2003) (”My friends would want me to talk to a counselor or other adult at school”; ”My family would want me to talk to a counselor or other adult at school”). Items were selected by the authors and reviewed for face validity by experts in youth suicide prevention: PhD level clinicians, and masters level professionals with long history of implementing suicide prevention programs with adolescents. These experts were invited by the authors and none declined. Drafted items were retained that were nominated as best reflecting the intended construct. Students responded to each question using a four-point Likert scale: Strongly Disagree (1), Disagree (2), Agree (3), and Strongly Agree (4). Higher sum scores (item average) reflect more positive intentions and norms about seeking help for distress from an adult at school.
Adult Help for Suicidal Youth and Reject Codes of Silence are the two additional domains of items created to assess students’ attitudes. Items were selected by the authors and reviewed for face validity by experts in youth suicide prevention as above; those items were retained that were nominated as best reflecting the intended construct. Three questions covered appraisals of Adult Help for Suicidal Youth: “I know adults who could help a friend thinking of suicide; My school has people who can help students going through hard times; I can think of an adult who I trust enough to help a suicidal friend.” Three questions measured norms regarding overcoming requests for secrecy about suicide concerns, i.e., Reject Codes of Silence: “A suicidal teen should be left alone if he/she doesn’t want help (reverse keyed); I would tell an adult I trusted if I knew that a friend was suicidal; I would tell an adult about a suicidal friend, even if that friend asked me to keep it secret.” Students answered each question using the four-point Likert scale described above, with higher scores indicating more positive perceptions that adults are available to help suicidal friends and intentions to get help for suicidal friends and resist requests for secrecy.
Measures for Testing Construct Validity
Maladaptive Coping Attitudes were measured using a 4-item scale developed by Gould and colleagues to evaluate differences in coping attitudes and practices between suicidal and non-suicidal youth (Gould, et al., 2004). The scale includes questions about the acceptability of getting help for problems (“People should be able to handle their own problems without outside help.”), endorsement of drugs and alcohol as ways to solve problems, and endorsement of suicide (“Suicide is a possible solution to problems”). Higher endorsement of overall maladaptive norms on this scale differentiated adolescents who had made suicide attempts from those who had not (Gould, et al., 2004).
Suicidal Ideation was ascertained using an item from the Youth Risk Behavior Survey (YRBS; Centers for Disease Control and Prevention, 2008) “During the past 12 months, did you ever seriously consider attempting suicide?” (answered YES or NO).
Suicide Attempts were ascertained in two ways. In Cohort 2, students answered the question, “I have attempted suicide in the last year” (answered YES or NO). In Cohort 3, attempts were assessed using the item from the YRBS (Centers for Disease Control and Prevention, 2008) “During the past 12 months, how many times did you actually attempt suicide?” (0 to six or more times). For this study, responses to both items about suicide attempts were collapsed into either “none” or “1 or more.”
We chose YRBS items because they were specifically developed for population-based assessments, and studies support their reliability and validity (e.g. Brener, Krug, & Simon, 2000; Centers for Disease Control and Prevention, 2004; Eaton, Lowry, Brener, Galuska, & Crosby, 2005; Shaughnessy, Doshi, & Jones, 2004). In nationwide surveys of high school students conducted in 2007, 7.5% of high school students answered that they had attempted suicide one or more times during the 12 months before taking the YRBS survey(Eaton, 2008).
Depression was measured using the 13-item Short Mood and Feelings Questionnaire (Angold et al., 1996). The SMFQ was designed specifically to assess core symptoms of depression in preadolescent and adolescent children and has demonstrated content and criterion-related validity with longer diagnostic assessments of depression in clinical and non-clinical youth (Angold, Erkanli, Silberg, Eaves, & Costello, 2002; Kuo, Vander Stoep, & Stewart, 2005; Rhew et al., 2010; Sharp, Goodyer, & Croudace, 2006). Scores range from 0–26, with higher scores indicating greater severity of depressive symptoms. To indicate significant depressive symptoms, we used the recommended cut-off (≥ eight on total score); the cut-off scores have a high sensitivity and specificity in identifying youth with depressive disorders (Angold, et al., 1996) .
Measures of suicidal ideation, suicide attempts and depression were completed by students in Cohorts 2 and 3. Maladaptive Coping Norms was included in the survey administered to students in Cohort 3 only.
Analyses
We first examined rates of suicidal ideation and suicide attempts, elevated depression and maladaptive coping norms among students in the 16 schools in Cohorts 2 and 3, which were used for analyses evaluating construct validity. Next, we conducted three stages of analyses, step-wise across the three cohorts of schools. (1) Item response distributions were examined in Cohort 1, along with the internal structure of items within Help Seeking Acceptability at School (HSA: Wyman et al., 2008) and the two new proposed scales, Adult Help for Suicidal Youth (AHSY) and Reject Codes of Silence (RCS). Next, an exploratory factor analysis (EFA) was conducted using a principal axis factoring method with promax oblique rotation to allow for correlation among the factors (also Cohort 1). The EFA was conducted with all ten items under review. Both eigenvalues and scree plots were examined to determine the number of factors to extract, following the recommendation that the scree test can be more accurate than the common criterion of eigenvalues > 1.0 (Floyd & Widaman, 1995). We combined information from eigenvalues and scree test to select the most interpretable solution. (2) A confirmatory factor analysis (CFA) was conducted on the solution obtained from the EFA with students from the 12 high schools in Cohort 2 using the maximum likelihood method to analyze variance/covariance matrices. To further ascertain the suitability of retaining AHSY and RCS as distinct factors, CFAs were run with both a 2- and 3-factor solution. To determine fit of the CFA models, we used the Comparative Fit Index (CFI), with values > .90 indicating acceptable fit and values >0.95 indicating close fit and Root Mean Square Error of Approximation (RMSEA) with values < 0.05 indicating good fit and values >0.1 indicating poor fit (Browne & Cudeck, 1993; Hu & Bentler, 1999; Tabachnick & Fidell, 2007) (3) Last, two types of construct validity were examined, concurrent validity known-groups validity (Carmines & Zeller, 1979; DeVellis, 2003). Concurrent validity was tested by estimating models assessing associations between the scales and Maladaptive Coping Norms scores in Cohort 3. To test known-groups validity, models were estimated comparing scores on each scale between students who did versus did not report suicide ideation, suicide attempts and elevated depression symptoms in Cohort 2 and independently with Cohort 3 as a replication. Linear multivariate regression and logistic regression analyses were used for continuous (Maladaptive Coping Norms) and dichotomous data (suicide ideation, suicide attempts and elevated depression), respectively. All models entered age, sex and race/ethnicity (categorical variable: White, African American, Hispanic/Latino, Other) as covariates. Prior to validity analyses, we tested for clustering effects of school on associations between the HSA, AHSY, and RCS scales and each of the dichotomous validity measures. Minimal school-level clustering was found (ICCs < 0.02), indicating that the use of multi-level analyses accounting for school clustering was not necessary.
All analyses except the CFA were conducted in SPSS versions 16 and 19. CFAs were run in AMOS v19.
RESULTS
Sample Characteristics
Rates of suicidal ideation (SI) were 13.9% among students in the 12 schools in Cohort 2 (381/2737) and 11.6% in the four schools in Cohort 3 (141/1214). Rates of suicide attempts (SA) were 5.0% (137/2737) and 7.0 (85/1214), respectively, in Cohorts 2 and 3. Depression symptoms were comparable in Cohort 2 (Mean=5.45, SD=5.86) and Cohort 3 (Mean=5.51, SD=5.81); scores above the clinically-significant cut-off (Angold, et al., 1996) were reported by 25.5% of students in Cohort 2 (699/2737) and 27.8% in Cohort 3 (337/1214). The Maladaptive Coping Norms measure was administered to students in the third cohort (Mean = 1.73, SD=0.64).
Item Distributions and Scale Properties
Item distributions and scale properties are summarized in Table 2. For each scale, the total score consisted of the item average, with higher scores indicating more positive norms. All items had acceptable skewness and kurtosis values (< 1.5, > −1.5) (Kline, 2005). However, responses were weighted towards the ‘positive’ end of the 4-point response scale, as shown by negative skewness values, with the exception of one item on the HSA scale (“I would talk to a counselor or other adult at school”) that had a skewness value of 0. The four items on the HSA scale had high internal consistency (Cronbach’s alpha= 0.84), and high item-total correlations (range 0.81 – 0.85) and squared multiple correlations (SMC) (range 0.35 – 0.61). Cronbach’s alphas for the AHSY and RCS scales were 0.67 and 0.64, respectively. Although Cronbach’s alpha ≥ 0.7 is a commonly-used threshold to indicate acceptable reliability, having only a three-item scale underpowers the calculation of alpha (Cortina, 1993; Schmitt, 1996). To further ascertain internal consistency, we examined mean inter-item correlation for both AHSY and RCS scales. Both were greater than 0.3 (RCS = .38; AHSY = .40), suggesting good internal consistency/reliability (Cortina, 1993). Of the ten items, two had squared multiple correlations (SMC) below the generally accepted threshold of 0.2: the reverse-keyed item on RCS, “A suicidal teen should be left alone if he/she doesn’t want help” (0.08) and on AHSY “My school has people who can help students going through hard times” (0.18).
Table 2.
Items and psychometric properties for three scales pertaining to help seeking norms (Cohort 1, n=2419)
| Scale Item | Mean (SD) | % agree (≥ 3) | Skew | Item- total R | SMCs | SCALE ALPHA |
|---|---|---|---|---|---|---|
|
HELP SEEKING ACCEPTABILITY AT SCHOOL If I was really upset and needed help… |
||||||
| I believe a counselor or other adult at school could help me | 2.60 (0.94) | 58.8 | −0.25 | 0.83 | 0.58 | |
| I would talk to a counselor or other adult at school | 2.43 (0.93) | 48.8 | 0.00 | 0.85 | 0.61 | |
| My friends would want me to talk to a counselor or other adult at school | 2.61 (0.92) | 56.6 | −0.18 | 0.81 | 0.45 | |
| My family would want me to talk to a counselor or other adult at school | 2.64 (0.97) | 57.7 | −0.21 | 0.76 | 0.35 | |
| Scale | 2.56 (0.76) | 0.84 | ||||
| ADULT HELP FOR SUICIDAL YOUTH | ||||||
| I know adults who could help a friend thinking of suicide | 2.80 (0.94) | 68.5 | −0.49 | 0.74 | 0.25 | |
| My school has people who can help students going through hard times | 2.88 (0.86) | 73.6 | −0.61 | 0.70 | 0.18 | |
| I can think of an adult who I trust enough to help a suicidal friend | 3.02 (0.90) | 76.6 | −0.72 | 0.75 | 0.29 | |
| Scale | 2.86 (0.63) | 0.67 | ||||
| REJECT CODES OF SILENCE | ||||||
| A suicidal teen should be left alone if he/she doesn’t want help (reverse keyed) | 3.19 (0.91) | 79.8 | −0.90 | 0.67 | 0.08 | |
| I would tell an adult I trusted if I knew that a friend was suicidal | 3.17 (0.86) | 83.1 | −0.95 | 0.77 | 0.42 | |
| I would tell an adult about a suicidal friend, even if that friend asked me to keep it secret | 2.98 (0.91) | 75.3 | −0.65 | 0.79 | 0.43 | |
| Scale | 3.25 (1.05) | 0.64 |
Note: All items have range of 1(Strongly Disagree) – 4(Strongly Agree); % agree column is percent respondents with scores of 3 or 4 (Agree or Strongly Agree); SMC=Squared Multiple Correlation.
To further assess the internal consistency of the scales, Cronbach’s alpha was calculated for all three scales for students in Cohorts 2 and 3. HSA alpha was consistently high across cohorts with values of 0.86 and 0.88 for Cohort 2 and 3, respectively. AHSY alphas were 0.69 and 0.63; however, the mean inter-item correlation for this scale increased from 0.40 in Cohort 1 to 0.42 and 0.59 in Cohorts 2 and 3, respectively, suggesting a cohesive scale. In cohorts 2 and 3, Cronbach’s alpha for RCS was 0.71 and 0.73. The satisfactory alpha for RCS in cohorts 2 and 3 suggested that retaining the one RCS item with low SMC value yielded acceptable internal consistency in the subsequent cohorts.
Exploratory Factor Analyses
The sample for the EFA consisted of 2,419 9th–10th grade students (Cohort 1). The EFA with all ten items identified two factors with eigenvalues > 1. The first factor had an eigenvalue of 4.21 (42.1% of the variance); the second factor had an eigenvalue of 1.44 (14.4% of the variance). Examination of the scree plot (Floyd & Widaman, 1995) suggested a third factor, which had an eigenvalue of 0.90 and accounted for an additional 9.0% of the variance. After this third factor, the eigenvalues dropped substantially, a pattern congruent with retaining the 3-factor solution (Floyd & Widaman, 1995). The three factors were as follows: on factor 1, all HSA items loaded together (factor loadings 0.67 – 0.84); factor 2 consisted of the three RCS items, with two high item loadings (0.86 and 0.64) and the third item (“A suicidal teen should be left alone if he/she doesn’t want help”-reversed) loading at 0.32; factor 3 consisted of the three AHSY items, with two high loadings (0.74 and 0.62) and third item (“My school has people who can help students going through hard times”) loading at 0.39. The 3-factor solution was retained as the best representation of the factor structure.
Confirmatory Factor Analysis
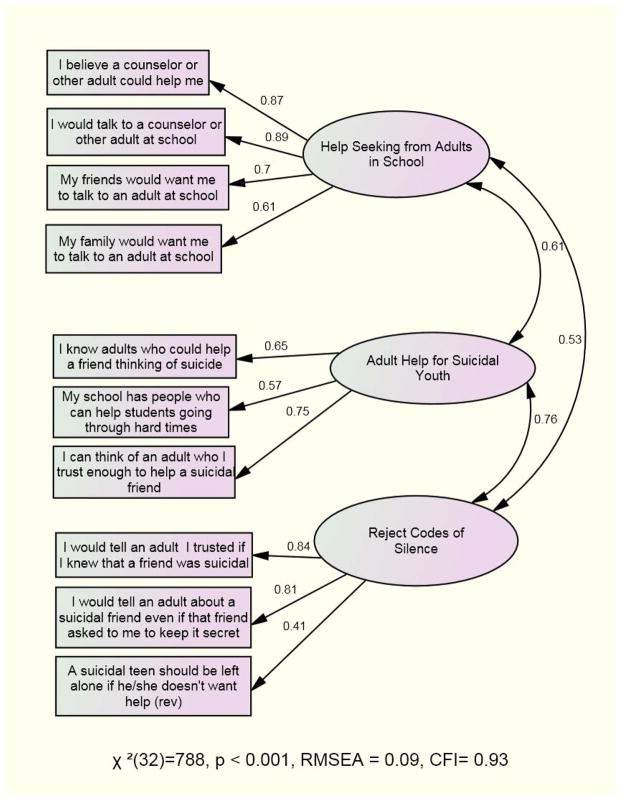
The results of the CFA testing the proposed solution of three separate scales with students from 12 high schools in Cohort 2 (n=2,737) showed an acceptable fit to the data (χ2(32) = 788, p < 0.001, RMSEA = 0.09, CFI= 0.93). In terms of RMSEA, this model may only be considered marginal (Browne & Cudeck, 1993), but a CFI greater than .90 is acceptable (Bentler, 1980; Hu & Bentler, 1999; Tabachnick & Fidell, 2007). The model is summarized in Figure 1. All items loaded acceptably high (> 0.40) on their respective factors. On the HSA factor, factor loadings for the two items pertaining to personal attitudes about help seeking (0.87 and 0.89) were higher than for the two items pertaining to perceived family and peer acceptance of help seeking (0.70 and 0.61). HSA was moderately correlated with AHSY and RCS (r = 0.61 and r = 0.53, respectively), and AHSY and RCS were more highly correlated (r = 0.76).
Figure 1.
Results from confirmatory factor analysis for 3-scale solution (standardized loadings).
Due to the high correlation of the AHSY and RCS scales and relatively low factor loading for one RCS item (0.41), we further evaluated the appropriateness of the 3-factor solution by comparing the fit of alternative CFAs. Specifically, we conducted a 2-factor CFA, with factor 1 consisting of the HSA items and factor 2 consisting of all six AHSY and RCS items. The overall fit (χ2(34) = 1159.0, p=.000; RMSEA = 0.11, CFI = 0.89) was lower than the fit for the 3-factor model, with a significant increase in χ2 (χ2 difference = χ2 (2)=370.82, p<.001). In addition, the item loadings were lower on the 2-factor model, suggesting that the 3-factor solution provided the superior fit to the data. In addition, we contrasted the fit from our 3-factor CFA with several alternative CFAs - a single factor combining all 10 items; and two or three factor solutions dropping the lowest loading items (“A suicidal teen should be left alone if he/she doesn’t want help”; and “school has people who can help students going through hard times”) – which all showed inferior fits to the 3-factor model with all items included.
Last, we ran the 3-factor CFA with students from the 4 schools in cohort 3 (n=1,214) and replicated our cohort 2 findings. With cohort 3, the model fit was again within an acceptable range (χ2(32) = 389, p < 0.001, RMSEA = 0.09, CFI= 0.94). Factor loadings for HSA and RCS were comparable to the cohort 2 model (HSA 0.67 – 0.89; RCS 0.38 – 0.86) and improved for AHSY (0.71 – 0.82). HSA was moderately correlated with AHSY and RCS (r = 0.55 and r = 0.43, respectively), and AHSY and RCS were more highly correlated (r = 0.75).
Construct Validity
Students who reported lower acceptability of seeking help for problems and higher endorsement of drugs, alcohol, and suicide as acceptable strategies for solving problems (i.e., reported higher scores on Maladaptive Coping Norms; Gould et al., 1996), also reported less adaptive perceptions and appraisals on HSA (β = −0.11, CI (−0.13, −0.04), ES= 0.15), AHSY (β = −0.31, CI (−0.36, −0.23), ES = 0.54) and RCS (β = −0.07, CI (−0.13, −0.01), ES=0.12).
Students who reported suicidal ideation, attempts, or elevated depression symptoms reported: (a) lower help-seeking acceptability for distress from an adult at school (HSA), (b) less favorable perceptions that capable adults are available to help suicidal youth (AHSY) and (c) less willingness to overcome resistance of suicidal peers to get help from adults (RCS) (Table 3). Single-scale models included one scale as a predictor, along with age, sex and race/ethnicity as covariates. Within these single-scale models, all odds ratios (ORs) demonstrated strong relationships between our scales and the outcomes (p< 0.001) and were comparable for students in the two independent cohorts of schools. For each point increase on each scale, students were one-third to one-half as likely to be in a group reporting suicidal ideation (OR=0.36 – 0.53), attempted suicide (OR=0.34 – 0.48) or elevated depression symptoms (OR=0.41 – 0.49).
Table 3.
Associations between help-seeking scales and membership in three groups in cohorts 2 and 3.
| Suicidal Ideation | Suicide Attempts | Depression | |||||
|---|---|---|---|---|---|---|---|
| Cohort | Scales | OR (CI) Single- scale | OR (CI) Multiple- scale | OR (CI) Single- scale | OR (CI) Multiple- scale | OR (CI) Single- scale | OR (CI) Multiple- scale |
| 2 | Help Seeking Acceptability at School | 0.44*** (0.38, 0.51) | 0.65*** (0.54, 0.78) | 0.43*** (0.34, 0.54) | 0.61*** (0.47, 0.80) | 0.48*** (0.42, 0.54) | 0.65*** (0.57, 0.75) |
| Reject Codes of Silence | 0.37*** (0.31, 0.45) | 0.65*** (0.52, 0.81) | 0.36*** (0.28, 0.46) | 0.66* (0.48, 0.92) | 0.41*** (0.35, 0.48) | 0.66*** (0.55, 0.79) | |
| Adult Help for Suicidal Youth | 0.35*** (0.30, 0.42) | 0.52*** (0.42, 0.64) | 0.39*** (0.31, 0.49) | 0.59** (0.44, 0.80) | 0.42*** (0.36, 0.48) | 0.63*** (0.53, 0.74) | |
| 3 | Help Seeking Acceptability at School | 0.52*** (0.41, 0.66) | 0.71* (0.54, 0.93) | 0.50*** (0.37, 0.67) | 0.74+ (0.52, 1.04) | 0.50*** (0.42, 0.60) | 0.64*** (0.52, 0.78) |
| Reject Codes of Silence | 0.44*** (0.34, 0.57) | 0.68* (0.48, 0.95) | 0.39*** (0.28, 0.53) | 0.59* (0.39, 0.89) | 0.42*** (0.34, 0.52) | 0.65** (0.50, 0.85) | |
| Adult Help for Suicidal Youth | 0.40*** (0.30, 0.53) | 0.58** (0.41,0 .83) | 0.36*** (0.26, 0.51) | 0.55** (0.36, 0.84) | 0.45*** (0.36, 0.56) | 0.69** (0.53, 0.90) | |
Note: All models include sex, age and race/ethnicity;
p <.001;
p<.01,
p<.05,
p<.10.
To determine unique associations between each scale and group status (SI, SA, elevated depression), multiple-scale models were estimated including all three scales (also summarized in Table 3), which also included age, sex and race/ethnicity as covariates. In both cohorts, each of the three scales (HSA, RCS, AHSY) was independently associated with students’ status as with and without: suicidal ideation, suicide attempts, and depression, with the exception of the association between HSA and suicide attempts in cohort 3 (p<0.10).
DISCUSSION
We developed brief scales to assess, within a school population, three dimensions of adolescents’ self-perceptions and appraisals: (a) acceptability of seeking help from adults at school for emotional distress; (b) availability of capable adults who help suicidal adolescents; and (c) intentions to obtain adult help for suicidal peers despite requests for secrecy and reluctance to get help. Confirmatory factor analyses supported retaining all three scales in order to measure related but distinct aspects of students’ perceptions about seeking help for distress and engaging adult help for suicidal peers.
The Help-Seeking Acceptability at School (HSA) scale (Wyman, et al., 2008) emerged as a clear one-factor scale. Items measuring youth’s attitudes toward personal help-seeking had the highest factor loadings, indicating the importance of those attitudes in help-seeking acceptance. Factor loadings on this scale from two items pertaining to perceived family and peer support for help-seeking were lower but acceptably high. The strong interrelationships among items on the HSA scale showed that students’ intentions to get help for their own distress were, as hypothesized, positively related to perceptions that their friends and family members would support their help seeking efforts. This finding is congruent with a large body of literature showing that perceived norms, which reflect appraisals of how widespread and socially sanctioned behavior is within an affiliation group (Cialdini, et al., 1990; Lapinski & Rimal, 2005; Rimal & Real, 2003), are robust predictors of adolescents’ own expectations and behavioral intentions (Valente, 2010).
Students’ scores on the HSA scale were correlated with scores on Adult Help for Suicidal Youth (AHSY) and Reject Codes of Silence (RCS). The latter two scales were more substantially correlated, suggesting that students’ intentions to get help for suicidal peers who are reluctant to get help themselves, are linked to perceiving adults as trustworthy and capable of helping suicidal youth. In addition, each of the three scales demonstrated acceptable variability of scores. Students’ responses were weighted toward the positive end of the 4-point Likert scales; however, the items on all three scales had skew and kurtosis values within acceptable limits and showed no evidence of ceiling effects. Internal consistency was high for HSA (0.84) and lower for AHSY (0.67) and RCS (0.64), suggesting that additional work on these latter two scales may lead to improved internal consistency by adding additional items.
Construct validity of our new scales was supported by associations with (a) a widely-used scale that assesses adolescents’ maladaptive coping attitudes (concurrent validity), and (b) students’ placement in three high risk groups defined by self-rated symptoms, suicidal ideations and behaviors (known-groups validity). First, higher scores on all three of our help-seeking scales–HSA, AHSY, and RCS—were associated with more maladaptive coping attitudes, a scale that includes acceptability of seeking help for problems, use of illicit substances to manage problems, and endorsement of suicide as an acceptable response to distress. Maladaptive Coping Attitudes has been shown to differentiate suicidal from non-suicidal adolescents (Gould, et al., 2004). Second, adolescents and young adults with suicidal ideation, suicidal behavior and depression are known to eschew adult help (Groholt, et al., 2005; Saunders, Resnick, Hoberman, & Blum, 1994; Wilson & Deane, 2010b; Wilson, et al., 2010). All three scales independently and robustly differentiated these ‘known’ groups (Carmines & Zeller, 1979; DeVellis, 2003), which provided useful anchor points, relative to others youths in the school population. Students were between one-third and one -half as likely to be in the group reporting suicidal ideation (OR=0.35 – 0.53), attempted suicide (OR=0.34 – 0.48) or elevated depression symptoms (OR=0.41 – 0.49) for each one-point increase in scores across the three scales. These findings, which were consistent across two independent cohorts comprised of 16 high schools with approximately 4,000 students, are important specifically because these new scales were designed to differentiate the propensity to seek and receive help for emotional distress generally and suicide concerns specifically.
Evidence supporting the construct validity of the scales is compelling, in part, because it was generated using a population-based survey design, in which either all students in a high school were invited to participate, or all students within randomly selected classrooms, as well as the independent replication with two separate cohorts of schools. Nevertheless, conclusive support for construct validity will need to come from future studies demonstrating a relationship between these scales and actual help-seeking behavior.
Our selection of constructs to measure in the new scales was influenced by a social-ecological perspective due to evidence that risk and protective influence for suicide accrues from the relationship systems in which adolescents interact, including their communication ties with adults at school and perceptions of help available from adults (Wyman, et al., 2010). However, we found minimal school-level clustering of scores on these new measures. In other words, there was minimal shared variation in students’ perceived norms as a function of attending the same school. This finding suggests that school may not be the most relevant unit of analysis for evaluating peer-to-peer influences on the aforementioned norms for help-seeking and trusting adults to help suicidal friends. Consistent with other literature showing that peer affiliation groups exert a substantial and increasing influence on adolescents’ norms and practices (Valente, 2010) particularly norms pertaining to suicidal behavior (Insel & Gould, 2008), future interventions and investigations relating to norms about suicide and help-seeking may profitably focus on clustering of attitudes among smaller social units, particularly friendship groups. The measures examined in the present study, which can be efficiently administered to an entire school population, can provide data for social network analysis to detect such clustering, as well as the spread of new norms and attitudes through networks.
Several limitations of this study should be noted. First, with regard to the psychometric properties of the scales, one reverse-keyed item on the Reject Codes of Silence scale (“A suicidal teen should be left alone if he/she doesn’t want help”) showed minimally acceptable associations with the other scale items in the first cohort used for scale development. Although the internal consistency of the scale was acceptable, and increased modestly in the second and third cohorts, this item continued to have lower association with the other items. Additional studies are needed to determine how this item coheres with the rest of the items in the Reject Codes of Silence scale in other samples and to identify alternative, better performing items. Second, students in the schools in both cohorts used to evaluate construct validity (Cohorts 2 and 3) were from primarily rural communities with limited ethnic/racial diversity. Future studies are needed to demonstrate the reliability and validity of these scales in a broader range of youth populations, particularly populations that are high priority for suicide prevention such as American Indians.
The present study also does not link students’ help-seeking norms, as measured by these new scales, with actual help-seeking behaviors. For further scale validation as well as for the field of youth suicide prevention in general, we suggest that future research include studies to increase knowledge of (1) which interventions promote enduring changes in adolescents’ help-seeking norms for suicide, particularly among young people within peer groups holding maladaptive norms, and (2) the specific mechanisms linking changes in help-seeking norms to actual help-seeking behaviors among those at high risk for suicide. In considering the second of the aforementioned research steps, we note that a sole focus on increasing help-seeking norms may not be sufficient to substantially increase the proportion of suicidal youth in a school population who seek and receive help from adults, or the proportion of students who engage adults to help suicidal friends. Our findings showed that most students reported relatively high scores on all three of our scales, that is, a large proportion of agreed or strongly agreed with statements such as they would get help for a suicidal friend even though that friend did not seek help. Yet, the evidence is compelling that only a small proportion of suicidal youth in a school come to the attention of adults (Brown, et al., 2007). In addition to help-seeking acceptability and perception that help is available, adolescents’ quality of communication and ongoing relationships with adults, as well as psychological factors such as having strategies for persisting in efforts to get help in the presence of strong emotions, may be key in determining whether help-seeking intentions are translated into actions (Wyman, et al., 2010).
In conclusion, Help Seeking from Adults, Adult Help for Suicidal Youth, and Reject Codes of Silence provide researchers and program evaluators with psychometrically sound scales for measuring, within a school population, student norms and attitudes about help-seeking for suicide concerns. In addition, the constructs measured by these scales have theoretical utility for understanding how the social environment influences how young people behave when they face emotional distress and suicidal thinking. These new scales can contribute to building needed models for understanding help seeking processes among suicidal youth.
Acknowledgments
We gratefully acknowledge support from the Center for Mental Health Services, SAMHSA (SM-05-019), New York State-Office of Mental Health, and National Institute of Mental Health (P20MH071897 and T32MH20061), and the NIH National Center for Research Resources (2 KL2 RR024136-06). Thanks also to Erin Walsh and Emily Hurley for contributions to the study.
References
- Ajzen I. The theory of planned behavior. Organizational behavior and human decision processes. 1991;50(2):179–211. [Google Scholar]
- Angold A, Costello EJ, Messer S, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1996;5:237–249. [Google Scholar]
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: Effects of age and gender. Journal of Child Psychology and Psychiatry. 2002;43(8):1052–1063. doi: 10.1111/1469-7610.00232. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Carlson GA, Guthrie D. Coping strategies, self-perceptions, hopelessness, and perceived family environments in depressed and suicidal children. Journal of Consulting and Clinical Psychology. 1987;55(3):361–366. doi: 10.1037//0022-006x.55.3.361. [DOI] [PubMed] [Google Scholar]
- Aseltine R, Jr, DeMartino R. An outcome evaluation of the sos suicide prevention program. American Journal of Public Health. 2004;94(3):446. doi: 10.2105/ajph.94.3.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aseltine RH, Jr, James A, Schilling EA, Glanovsky J. Evaluating the sos suicide prevention program: A replication and extension. [Randomized Controlled Trial] BMC Public Health. 2007;7:161. doi: 10.1186/1471-2458-7-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry CM, Wentzel KR. Friend influence on prosocial behavior: The role of motivational factors and friendship characteristics. Developmental Psychology. 2006;42(1):153–163. doi: 10.1037/0012-1649.42.1.15. [DOI] [PubMed] [Google Scholar]
- Bauermeister J, Elkington K, Brackis-Cott E, Dolezal C, Mellins C. Sexual behavior and perceived peer norms: Comparing perinatally HIV-infected and HIV-affected youth. Journal of youth and adolescence. 2009;38(8):1110–1122. doi: 10.1007/s10964-008-9315-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Borsari B, Carey KB. Descriptive and injunctive norms in college drinking: A meta-analytic integration. Journal of Studies on Alcohol and Drugs. 2003;64(3):331–341. doi: 10.15288/jsa.2003.64.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Krug EG, Simon TR. Trends in suicide ideation and suicidal behavior among high school students in the United States, 1991–1997. Suicide and Life-Threatening Behavior. 2000;30(4):304–312. [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, Baugher M. Psychiatric risk factors for adolescent suicide: A case-control study. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(3):521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- Brenton JJ, Tousignant M, Bergeron L, Berthiaume C. Informant-specific correlates of suicidal behavior in a community survey of 12- to 14-year-olds. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(6):723–730. doi: 10.1097/00004583-200206000-00012. [DOI] [PubMed] [Google Scholar]
- Brown CH, Wyman PA, Brinales JM, Gibbons RD. The role of randomized trials in testing interventions for the prevention of youth suicide. International Review of Psychiatry. 2007;19(6):617–631. doi: 10.1080/09540260701797779. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural models. Newbury Park, CA: Sage Publications; 1993. [Google Scholar]
- Buhi E, Goodson P. Predictors of adolescent sexual behavior and intention: A theory-guided systematic review. Journal of Adolescent Health. 2007;40(1):4–21. doi: 10.1016/j.jadohealth.2006.09.027. [DOI] [PubMed] [Google Scholar]
- Carmines E, Zeller R. Reliability and validity assessment. Beverly Hills, CA: Sage Publications; 1979. [Google Scholar]
- Carter M, Orr M, Dittus P. Trends in sexual risk behaviors, by nonsexual risk behavior involvement, U.S. High school students, 1991–2007. Journal of Adolescent Health. 2009;44(4):372–379. doi: 10.1016/j.jadohealth.2008.08.020. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Suicide among hispanics - United States, 1997–2001. MMWR Recommendations and Reports. 2004;53(22) [Google Scholar]
- Centers for Disease Control and Prevention. 2007 youth risk behavior survey. Surveillance summaries. MMWR Recommendations and Reports. 2008;57:1–131. [Google Scholar]
- Cialdini RB, Reno RR, Kallgren CA. A focus theory of normative conduct: Recycling the concept of norms to reduce littering in public places. Journal of Personality and Social Psychology. 1990;58(6):1015–1026. [Google Scholar]
- Cortina JM. What is coefficient alpha? An examination of theory and applications. Journal of Applied Psychology. 1993;78:98–104. [Google Scholar]
- Costello EJ, Pescosolido B, Angold A, Burns BJ. A family network-based model of access to child mental health services. In: Morrissey JP, editor. Research in community and mental health: Social networks and mental illness. Vol. 9. Stamford, CT: JAI Press; 1998. pp. 165–190. [Google Scholar]
- DeJong W, Schneider SK, Towvim LG, Murphy MJ, Doerr EE, Simonsen NR, Scribner RA. A multisite randomized trial of social norms marketing campaigns to reduce college student drinking. Journal of Studies on Alcohol and Drugs. 2006;67(6):868–879. doi: 10.15288/jsa.2006.67.868. [DOI] [PubMed] [Google Scholar]
- DeVellis R. Scale development: Theory and applications. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R. Youth risk behavior surveillance—United States, 2007. MMWR Recommendations and Reports. 2008;57(SS-4):1–131. [PubMed] [Google Scholar]
- Eaton DK, Lowry R, Brener ND, Galuska DA, Crosby AE. Associations of body mass index and perceived weight with suicide ideation and suicide attempts among us high school students. Archives of Pediatric and Adolescent Medicine. 2005;159(6):513–519. doi: 10.1001/archpedi.159.6.513. 159/6/513 [pii] [DOI] [PubMed] [Google Scholar]
- Ellis WE, Zarbatany L. Peer group status as a moderator of group influence on children’s deviant, aggressive, and prosocial behavior. Child Development. 2007;78(4):1240–1254. doi: 10.1111/j.1467-8624.2007.01063.x. [DOI] [PubMed] [Google Scholar]
- Fishbein M. A reasoned action approach to health promotion. Medical Decision Making. 2008;28(6):834. doi: 10.1177/0272989X08326092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd F, Widaman K. Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment. 1995;7(3):286–299. [Google Scholar]
- Freedenthal S. Adolescent help-seeking and the yellow ribbon suicide prevention program: An evaluation. Suicide and Life-Threatening Behavior. 2010;40(6):628–639. doi: 10.1521/suli.2010.40.6.628. [DOI] [PubMed] [Google Scholar]
- Garrison C, Jackson K, Addy C, McKeown R, Waller J. Suicidal behaviors in young adolescents. American Journal of Epidemiology. 1991;133(10):1005. doi: 10.1093/oxfordjournals.aje.a115809. [DOI] [PubMed] [Google Scholar]
- Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(4):386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- Gould MS, Velting D, Kleinman M, Lucas C, Thomas JG, Chung M. Teenagers’ attitudes about coping strategies and help-seeking behavior for suicidality. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(9):1124–1133. doi: 10.1097/01.chi.0000132811.06547.31. [DOI] [PubMed] [Google Scholar]
- Groholt B, Ekeberg O, Wichstrom L, Haldorsen T. Suicidal and nonsuicidal adolescents: Different factors contribute to self-esteem. Suicide and Life-Threatening Behavior. 2005;35(5):525–535. doi: 10.1521/suli.2005.35.5.525. http://dx.doi.org/10.1521/suli.2005.35.5.525. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariate structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Insel BJ, Gould MS. Impact of modeling on adolescent suicidal behavior. Psychiatr Clin North Am. 2008;31(2):293–316. doi: 10.1016/j.psc.2008.01.007. [DOI] [PubMed] [Google Scholar]
- Joe S, Romer D. Suicide acceptability is related to suicide planning in us adolescents and young adults. Suicide and Life-Threatening Behavior. 2007;37(2):165–178. doi: 10.1521/suli.2007.37.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashani JH, Goddard P, Reid JC. Correlates of suicidal ideation in a community sample of children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1989;28(6):912–917. doi: 10.1097/00004583-198911000-00016. [DOI] [PubMed] [Google Scholar]
- Kerr D, Owen L, Pears K, Capaldi D. Prevalence of suicidal ideation among boys and men assessed annually from ages 9 to 29 years. Suicide and Life-Threatening Behavior. 2008;38(4):390. doi: 10.1521/suli.2008.38.4.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaus N, Mobilio A, King C. Parent–adolescent agreement concerning adolescents’ suicidal thoughts and behaviors. Journal of Clinical Child & Adolescent Psychology. 2009;38(2):245–255. doi: 10.1080/15374410802698412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. 2. New York: Guilford; 2005. [Google Scholar]
- Kuo ES, Vander Stoep A, Stewart DG. Using the Short Mood and Feelings Questionnaire to detect depression in detained adolescents. Assessment. 2005;12:374–383. doi: 10.1177/1073191105279984. [DOI] [PubMed] [Google Scholar]
- Lapinski MK, Rimal RN. An explication of social norms. Communication Theory. 2005;15(2):127–147. [Google Scholar]
- Logan D, King C. Parental identification of depression and mental health service use among depressed adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41(3):296. doi: 10.1097/00004583-200203000-00009. [DOI] [PubMed] [Google Scholar]
- Logan DE, King CA. Parental facilitation of adolescent mental health services utilization: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2001;8(3):319–333. http://dx.doi.org/10.1093/clipsy/8.3.319. [Google Scholar]
- O’Donnell L, Myint U, O’Donnell C, Stueve A. Long - term influence of sexual norms and attitudes on timing of sexual initiation among urban minority youth. Journal of School Health. 2003;73(2):68–75. doi: 10.1111/j.1746-1561.2003.tb03575.x. [DOI] [PubMed] [Google Scholar]
- Olafsdottir S, Pescosolido BA. Drawing the line: The cultural cartography of utilization recommendations for mental health problems. Journal of Health and Social Behavior. 2009;50(2):228–244. doi: 10.1177/002214650905000208. [DOI] [PubMed] [Google Scholar]
- Pescosolido B. Beyond rational choice: The social dynamics of how people seek help. American Journal of Sociology. 1992:1096–1138. [Google Scholar]
- Quinnett P. QPR: Ask a question, save a life. Spokane, WA: QPR Institute and Suicide Awareness/Voices of Education; 1995. [Google Scholar]
- Rhew I, Simpson K, Tracy M, Lymp J, McCauley E, Tsuang D, Vander Stoep A. Criterion validity of the Short Mood and Feelings Questionnaire and one-and two-item depression screens in young adolescents. Child and Adolescent Psychiatry and Mental Health. 2010;4(8):1–11. doi: 10.1186/1753-2000-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickwood DJ, Braithwaite VA. Social-psychological factors affecting help-seeking for emotional problems. [doi: DOI: 10.1016/0277-9536(94)90099-X] Social Science & Medicine. 1994;39(4):563–572. doi: 10.1016/0277-9536(94)90099-x. [DOI] [PubMed] [Google Scholar]
- Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? Medical Journal of Australia. 2007;187(7 Suppl):S35–39. doi: 10.5694/j.1326-5377.2007.tb01334.x. [DOI] [PubMed] [Google Scholar]
- Rickwood DJ, Deane FP, Wilson CJ, Ciarrochi AJ. Young people’s help-seeking for mental health problems. Australian e-Journal for the Advancement of Mental Health. 2005;4(3):1–34. [Google Scholar]
- Rimal RN, Real K. Understanding the influence of perceived norms on behaviors. Communication Theory. 2003;13(2):184–203. [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Trautman PD, Dopkins SC, Shrout PE. Cognitive style and pleasant activities among female adolescent suicide attempters. Journal of Consulting and Clinical Psychology. 1990;58(5):554–561. doi: 10.1037//0022-006x.58.5.554. [DOI] [PubMed] [Google Scholar]
- Saunders SM, Resnick MD, Hoberman HM, Blum RW. Formal help-seeking behavior of adolescents identifying themselves as having mental health problems. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33(5):718–728. doi: 10.1097/00004583-199406000-00013. [DOI] [PubMed] [Google Scholar]
- Schmitt N. Uses and abuses of coefficient alpha. Psychological Assessment. 1996;8:350–353. [Google Scholar]
- Shaffer D, Gould MS, Fisher P, Trautman P, et al. Psychiatric diagnosis in child and adolescent suicide. Archives of General Psychiatry. 1996;53(4):339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Vieland V, Garland A, Rojas M, Underwood M, Busner C. Adolescent suicide attempters. Response to suicide-prevention programs. JAMA. 1990;264(24):3151–3155. [PubMed] [Google Scholar]
- Sharp C, Goodyer IM, Croudace TJ. The Short Mood and Feelings Questionnaire (SMFQ): A unidimensional item response theory and categorical data factor analysis of self-report ratings from a community sample of 7- through 11-year-old children. Journal of Abnormal Child Psychology. 2006;34(3):379–391. doi: 10.1007/s10802-006-9027-x. [DOI] [PubMed] [Google Scholar]
- Shaughnessy L, Doshi SR, Jones SE. Attempted suicide and associated health risk behaviors among Native American high school students. Journal of School Health. 2004;74(5):177–182. doi: 10.1111/j.1746-1561.2004.tb08217.x. [DOI] [PubMed] [Google Scholar]
- Sourander A, Helstelä L, Haavisto A, Bergroth L. Suicidal thoughts and attempts among adolescents: A longitudinal 8-year follow-up study. J Affect Disord. 2001;63(1–3):59–66. doi: 10.1016/s0165-0327(00)00158-0. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Pescosolido B, Cabassa LJ. Building a model to understand youth service access: The gateway provider model. Ment Health Serv Res. 2004;6(4):189–198. doi: 10.1023/b:mhsr.0000044745.09952.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan K, Marshall S, Schonert-Reichl K. Do expectancies influence choice of help-giver?: Adolescents’ criteria for selecting an informal helper. Journal of Adolescent Research. 2002;17(5):509. [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. Vol. 5. Boston, MA: Pearson Education, Inc; 2007. [Google Scholar]
- Valente TW. Social networks and health: Models, methods, and applications. New York: Oxford University press USA; 2010. [Google Scholar]
- Wilson C, Deane FP, Ciarrochi J. Can hopelessness and adolescents’ beliefs and attitudes about seeking help account for help negation? Journal of Clinical Psychology. 2005;61(12):1525–1540. doi: 10.1002/jclp.20206. [DOI] [PubMed] [Google Scholar]
- Wilson CJ, Deane FP. Brief report: Need for autonomy and other perceived barriers relating to adolescents’ intentions to seek professional mental health care. Journal of Adolescence. 2010a:1–5. doi: 10.1016/j.adolescence.2010.06.011. [DOI] [PubMed] [Google Scholar]
- Wilson CJ, Deane FP. Help-negation and suicidal ideation: The role of depression, anxiety and hopelessness. Journal of Youth and Adolescence. 2010b;39(3):291–305. doi: 10.1007/s10964-009-9487-8. [DOI] [PubMed] [Google Scholar]
- Wilson CJ, Deane FP, Marshall KL, Dalley A. Adolescents’ suicidal thinking and reluctance to consult general medical practitioners. Journal of Youth and Adolescence. 2010;39(4):343–356. doi: 10.1007/s10964-009-9436-6. [DOI] [PubMed] [Google Scholar]
- Wilson CJ, Rickwood D, Deane FP. Depressive symptoms and help-seeking intentions in young people. Clinical Psychologist. 2007;11(3):98–107. http://dx.doi.org/10.1080/13284200701870954. [Google Scholar]
- Wu P, Katic B, Liu X, Fan B, Fuller C. Mental health service use among suicidal adolescents: Findings from a us national community survey. Psychiatric Services. 2010;61(1):17. doi: 10.1176/ps.2010.61.1.17. [DOI] [PubMed] [Google Scholar]
- Wyman PA, Brown CH, Inman J, Cross W, Schmeelk-Cone K, Guo J, Pena JB. Randomized trial of a gatekeeper program for suicide prevention: 1-year impact on secondary school staff. Journal of Consulting and Clinical Psychology. 2008;76(1):104–115. doi: 10.1037/0022-006X.76.1.104. 2008-00950-013 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyman PA, Brown CH, LoMurray M, Schmeelk-Cone K, Petrova M, Yu Q, Wang W. An outcome evaluation of the Sources of Strength suicide prevention program delivered by adolescent peer leaders in high schools. American Journal of Public Health. 2010;100(9):1653–1661. doi: 10.2105/AJPH.2009.190025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J, Kochaneck K, Murphy S, Tejada-Vera B. Deaths: Final data for 2007. National Vital Statistics Reports. 2010;58(19):1–73. [PubMed] [Google Scholar]