Abstract
Background
A better understanding of the nature and etiology of conduct disorder (CD) can inform nosology and vice-versa. We posit that any prevalent form of psychopathology, including CD, can be best understood if it is studied in the context of other correlated forms of child and adolescent psychopathology using formal models to guide inquiry.
Methods
Review of both cross-sectional and longitudinal studies of the place of CD in the phenotypic and causal structure of prevalent psychopathology, with an emphasis on similarities and differences between CD and oppositional defiant disorder (ODD). Papers were located using Web of Science by topic searches with no restriction on year of publication.
Results
Although some important nosologic questions remain unanswered, the dimensional phenotype of CD is well defined. CD differs from other disorders in its correlates, associated impairment, and course. Nonetheless, it is robustly correlated with many other prevalent dimensions of psychopathology both concurrently and predictively, including both other “externalizing” disorders and some “internalizing” disorders. Based on emerging evidence, we hypothesize that these concurrent and predictive correlations result primarily from widespread genetic pleiotropy, with some genetic factors nonspecifically influencing risk for multiple correlated dimensions of psychopathology. In contrast, environmental influences mostly act to differentiate dimensions of psychopathology from one another both concurrently and over time. CD and ODD share half of their genetic influences, but their genetic etiologies are distinct in other ways. Unlike most other dimensions of psychopathology, half of the genetic influences on CD appear to be unique to CD. In contrast, ODD broadly shares nearly all of its genetic influences with other disorders and has little unique genetic variance.
Conclusions
CD is a relatively distinct syndrome at both phenotypic and etiologic levels, but much is revealed by studying CD in the context of its causal and phenotypic associations with other disorders over time. Advancing and refining formal causal models that specify the common and unique causes and biological mechanisms underlying each correlated dimension of psychopathology should facilitate research on the fundamental nature and nosology of CD.
Keywords: Conduct disorder, oppositional defiant disorder, taxonomy, etiology, homotypic and heterotypic continuity
Conduct disorder (CD) is a prevalent syndrome, recognized in both DSM-IV and ICD-10, which is defined by a relatively persistent pattern of multiple antisocial behaviors during childhood and adolescence, including fighting, bullying, stealing, vandalism, and lying for personal gain. These and other CD behaviors harm victims in physical and psychological ways. Furthermore, children and adolescents who meet diagnostic criteria for CD are themselves at substantially increased risk for incarceration, depression, substance use disorders, and suicide (Lahey, 2008; Loeber, Farrington, Stouthamer-Loeber, & Van Kammen, 1998). Although more remains to be learned, the associations between these forms of impairment and the number of CD behaviors are predominantly linear (Lahey et al., 1994), suggesting that CD is a dimensional phenomenon that should be dichotomized only to aid clinicians in making the inherently dichotomous diagnostic decision to treat or not treat. In this article, we review evidence on CD as both a dimensional and a dichotomous diagnostic construct to make full use of the available evidence. Regardless of whether CD is treated as a dimension or a category, however, it is a serious public health problem that must be understood, treated, and prevented far better than at present.
In this paper, we first discuss open questions regarding the nosology of CD and related disorders. Next, we review emerging evidence on the etiology of CD in the context of other prevalent forms of psychopathology. We do so because studies of etiology and nosology are mutually informative and, indeed, inseparable. To guide future research on the etiology and nature of CD and other correlated forms of psychopathology, we offer a set of disconfirmable hypotheses based on the phenotypic and causal structural model of prevalent forms of psychopathology. Regardless of how these specific hypotheses fare in the scientific arena, the process of testing, confirming or refuting, and revising these hypotheses will significantly advance our understanding of the nature and classification of CD.
NOSOLOGY OF CD
Although many studies have advanced understanding of the nosology of CD, a number of critical questions remain unanswered. For each of these questions, we highlight both what we already know and what needs to be learned. In this discussion, we rely heavily on the results of both factor analysis and univariate and multivariate behavior genetic analyses to address key questions and frame the types of future studies that are needed to help advance our understanding of CD.
Is ODD Distinguishable from CD?
ODD is defined by symptoms of irritability and defiance of adult authorities, whereas CD symptoms refer to specific antisocial behaviors. For many years, there have been three views in the literature on the structure of ODD and CD symptoms. The first view, embodied in the ICD-10 approach to diagnostic classification, is that ODD is part of a CD diagnostic spectrum, characterizes a less severe form of CD, and is often a developmental precursor to CD (WHO, 1992). The second perspective, which is represented in DSM-IV, is that although ODD frequently overlaps with CD and their symptoms are highly correlated (Angold & Costello, 2009; Angold, Costello, & Erkanli, 1999; Lahey, Rathouz, et al., 2008), ODD and CD are relatively distinct dimensions of psychopathology with at least some distinct correlates and sequelae (Boden, Fergusson, & Horwood, 2010; Burke, Waldman, & Lahey, 2010; Petty et al., 2009; Rowe, Costello, Angold, Copeland, & Maughan, 2010). The third model underlies the Child Behavioral Checklist (CBCL) (Achenbach, 1978). In the CBCL, aggressive CD symptoms are on the same dimension as ODD symptoms and nonaggressive CD symptoms (and other symptoms) are on a separate factor.
A number of published studies are relevant to these three alternative hypotheses regarding ODD and CD. The DSM-IV field trials for the disruptive behavior disorders identified two non-overlapping sets of symptoms with greater diagnostic utility for ODD or CD, respectively (Frick et al., 1994). Many studies have subsequently supported the distinction between the DSM-IV symptom lists for ODD and CD using factor analysis, although some ODD symptoms (intentionally bothers others and spiteful and vindictive) may poorly discriminate ODD and CD (Lahey, Applegate, et al., 2004; Lahey, Rathouz, et al., 2008). A meta-analysis was conducted of 60 exploratory factor analyses of a range of childhood conduct problem behaviors from 44 separate studies using multidimensional scaling (Frick et al., 1993). This meta-analysis supported four symptom dimensions of oppositionality, aggression, property violations, and status offenses. These four dimensions were found to differ in terms of their retrospectively reported ages-of-onset, with oppositionality having the earliest onset (median age = 6.0 years), followed by aggression (median age = 6.75 years), property violations (median age = 7.25 years), and status offenses (median age = 9.0 years) (Frick, et al., 1993).
A direct comparison has been made between the DSM-IV model and a model inspired by the structure of the CBCL, in which aggressive CD symptoms are on the same dimension as ODD symptoms and nonaggressive CD symptoms are on a separate factor (Lahey, Rathouz, et al., 2008). Because the specific CBCL items were not used in this analysis, it is not certain that the CBCL itself achieves a less good fit to the data than does the DSM-IV model. Nonetheless, when DSM-IV symptoms were used in the comparison of these alternative models, a model of ODD and CD based on DSM-IV achieved a closer fit than a model inspired by the CBCL (Lahey, Rathouz, et al., 2008). In the same study, the DSM-IV model achieved a significantly better fit than a model based on ICD-10, in which the ODD and CD symptoms loaded together on a single dimension (Lahey, Rathouz, et al., 2008). Taken together, these findings suggest that ODD and CD are best considered as distinguishable if highly correlated dimensions of psychopathology at the phenotypic level.
Although ODD and CD have similar background correlates, CD is more strongly related to parental antisocial behavior and psychopathology and with atypical maternal parenting (Frick et al., 1992). Similarly, CD predicts adult antisocial outcomes more strongly than ODD (Lahey, 2008). Both ODD and CD predict later depression, but although ODD appears to be directly related to later depression, CD appears to indirectly increase risk for depression by causing stressful life events—such as expulsion from school, peer rejection, and incarceration—that in turn precipitate depression (Burke, Loeber, & Birmaher, 2002; Burke, Loeber, Lahey, & Rathouz, 2005; Patterson & Capaldi, 1990). Thus, although they are highly correlated, ODD and CD are different enough to distinguish as dimensions of psychopathology.
Nonetheless, there is an important practical issue that strongly argues that the ICD-10 approach to ODD and CD is preferable when it is necessary to make categorical diagnoses. Valid diagnostic taxonomies must be comprehensive in the sense of identifying all impaired individuals. In the ICD-10 Research Diagnostic Criteria (WHO, 1992), oppositional defiant disorder is defined by 4 or more symptoms from the combined list of both ODD and CD symptoms, but only if the individual does not meet criteria for CD. This means that children and adolescents with a combination of 2 (or 3) symptoms of ODD and 2 (or 1) symptoms of CD are given the diagnosis of ODD according to ICD-10. Under DSM-IV rules, these children would not receive a diagnosis of either ODD or CD, although they could be given the diagnosis of “disruptive behavior disorder not otherwise specified.” In either case, these children tend to be ignored by researchers who use categorical DSM-IV diagnoses; furthermore, their families may be less able to receive third-party reimbursement for clinical services.
The key question, therefore, is whether the children and adolescents who receive an ICD-10 diagnosis of ODD, but do not qualify for a DSM-IV diagnosis of ODD are significantly impaired and should be diagnosed. A large population-based study found that the substantial number of children and adolescents who received an ICD-10 diagnosis of ODD but not a DSM-IV diagnosis of ODD were as impaired as youth who received a DSM-IV diagnosis of ODD (Rowe, Maughan, Costello, & Angold, 2005). This important finding has been replicated in both clinic- and population-based samples (Burke, et al., 2010), suggesting that there is a “hole” in the DSM-IV nomenclature that lets seriously impaired children with a mixture of some ODD and some CD symptoms go undiagnosed. Therefore, the current evidence indicates that ODD and CD are independent, if highly correlated forms of psychopathology that should be distinguished when these constructs are treated as dimensions. Nonetheless, the ICD-10 approach of combining ODD and CD when nominal diagnostic decisions are made has important clinical advantages.
Would a Nosological Distinction between Aggressive and Nonaggressive CD Symptoms be Useful?
It is possible that the dimension of CD behaviors should be subdivided further for some purposes. For example, although aggressive (e.g., fighting, bullying, and threat with confrontation of the victim) and nonaggressive CD behaviors (e.g., lying to con, truancy, and theft without confrontation of the victim) are highly correlated, enough may be gained to make a nosological distinction between these dimensions to make it worthwhile. There is a small but informative literature in which factor analysis has been used to examine the hypothesis that aggressive and non-aggressive dimensions of CD symptoms should be distinguished. Such analyses have found that a model in which aggressive and nonaggressive CD symptoms load on two separate factors fits the data better than a model in which these load on a single CD symptom dimension (Dekovic, 2003; Tackett, Krueger, Iacono, & McGue, 2005).
There is also evidence of differences between aggressive and nonaggressive CD behavior dimensions in terms of their external correlates. For example, there is replicated evidence that cognitive ability measures (executive functioning and verbal intelligence) are significantly (inversely) associated with physical aggression but not with theft (Barker et al., 2007; Barker et al., 2011). Similarly, there also are differences between aggressive and nonaggressive conduct problems in their correlations with personality traits. In two non-referred samples of undergraduate students, Burt and Donnelan (2008) found that several measures of aggression were uniquely correlated with higher levels on the Stress Reaction scale of the Multidimensional Personality Questionnaire (Patrick, Curtin, & Tellegen, 2002), whereas nonaggressive conduct problems were uniquely correlated with lower levels on the Control scale of this personality measure.
Taken together, these results suggest that the distinction between aggressive and nonaggressive CD symptoms could be important for some purposes. A further important issue for future research, however, is whether aggressive and nonaggressive CD behaviors are themselves homogenous in nature or there are actually multiple syndromes within them that should be distinguished. There is reason to believe that there are important differences between two types of nonaggressive CD behaviors: property violations (e.g., theft without confrontation and vandalism) and status offenses (e.g., truancy and stay out late without parental permission) (Frick, et al., 1993; Lahey et al., 2000). Little research has addressed this issue, but it should not be ignored in the future. Considerably more research has addressed the question of whether distinctions should be made between different forms of aggression, however.
Proactive and reactive aggression
Several factor analytic studies of reactive and proactive aggression have been conducted (Dodge & Coie, 1987; Raine et al., 2006) and have suggested that these represent two distinct yet correlated dimensions. Although this distinction has been challenged (Bushman & Anderson, 2001), several studies have demonstrated different correlates of proactive and reactive aggression. For example, proactive aggression has been uniquely associated with delinquency, poor school motivation, poor peer relationships, single-parent status, psychosocial adversity, substance-abusing parents, and hyperactivity during childhood and with psychopathic personality, blunted affect, delinquency, and serious violent offending in adolescence (Kempes, Matthys, de Vries, & van Engeland, 2005; Raine, et al., 2006). In contrast, reactive aggression has been associated with impulsivity, hostility, social anxiety, problems encoding and interpreting social cues, lower peer status, and lack of close friends in adolescence (Kempes, et al., 2005; Raine, et al., 2006).
There are two strong arguments against including separate dimensions of proactive and reactive aggression in DSM-V and ICD-11, however. First, because many of the items defining reactive aggression are very similar to ODD items, any distinction between reactive and proactive aggression may overlap substantially with the distinction between ODD and CD. Second, when items defining proactive and reactive aggression were included with symptoms of psychopathology in the assessment of a large represent sample, exploratory factor analyses (EFAs) supported DSM-IV-like symptom dimensions of ODD and CD. Some reactive and proactive aggression items did not load on any psychopathology factor, but the ones that did loaded on either the ODD or the CD factors, not on their own factors (Lahey, Applegate, et al., 2004). Thus, although it would be important to consider some reactive and proactive aggression items as possible new symptoms of ODD or CD in DSM-V and ICD-11, there is not currently evidence that independent dimensions of proactive or reactive antisocial behavior exist.
Relational aggression
This term refers to behaviors that are intended to hurt others by damaging their social relationships or self-esteem, but that do not involve physical contact or harm (Archer & Coyne, 2005; Crick & Zahn-Waxler, 2003). Consideration has been given to the possibility that relational aggression should be included in DSM-V and ICD-11, either as part of the definition of CD or as a new form of psychopathology (Keenan, Coyne, & Lahey, 2008; Keenan, Wroblewski, Hipwell, Loeber, & Stouthamer-Loeber, 2011; Moffitt et al., 2008).
As with proactive and reactive aggression, the ultimate question is whether there is an incremental contribution of relation aggression in identifying children with impairing antisocial behavior. Two analyses of data from a large representative sample of children and adolescents are relevant to this question. First, measuring symptoms of relational aggression adds very little to the identification of children and adolescents with impairing antisocial behavior after symptoms of ODD and CD have been assessed (Keenan, et al., 2008; Keenan, et al., 2011). Second, when items defining relational aggression were included with DSM-IV symptoms in EFA, a relational aggression factor distinct from ODD and CD did not emerge (Lahey, Applegate, et al., 2004). Nonetheless, some relationally aggressive behaviors loaded strongly on CD, suggesting that they should be considered for inclusion as symptoms that broaden our description of CD in DSM-V and ICD-11.
Later in this paper we address the distinction between aggressive and nonaggressive CD behaviors again from the perspective of similarities and differences in their etiologic influences. We also review evidence on the etiology of reactive, proactive, and relational aggression that may be relevant to their nosology.
Is There Sufficient Evidence to Distinguish Subtypes of CD?
There is widespread agreement that the diagnosis of CD is highly heterogeneous, but there is no consensus on the best way to reduce that heterogeneity by subtyping the diagnosis. Thus, an important issue is whether subtypes of CD should be distinguished in DSM-V and ICD-11 and, if so, which subtypes are most diagnostically meaningful. Previous subtyping schemas for DSM-IV distinguished between “socialized” and “undersocialized” CD and between “aggressive” and “nonaggressive CD.” These were abandoned and replaced in DSM-IV because no clear operational definition of the socialized/undersocialized distinction had been proposed and studied and because inspection of data from a longitudinal study of prepubertal children with CD (Lahey et al., 1995b) found that all children who met diagnostic criteria for CD displayed aggression in at least one wave of the study (Lahey, Loeber, et al., 1998). In DSM-IV, a distinction was made instead between childhood and adolescent age-of-onset subtypes based on the presence of at least one CD symptom prior to age 10 years. In this section we consider whether this or any other subtyping scheme has been demonstrated to be sufficiently valid to be incorporated into the nosology of CD.
Validity of subtypes based on age of onset
Considerable research has documented important differences between childhood-onset (life-course persistent) and adolescent-onset (adolescence-limited) forms of antisocial behavior (Moffitt, 1993, 2003, 2006). Although the prevalence of antisocial behavior in these studies, which was based on behaviors that ranged from very mild to very serious, was far higher than the diagnosis of CD, this research could be relevant to the taxonomy of CD. Childhood-onset adolescent antisocial behavior is associated with parental antisocial behavior, serious family dysfunction, perinatal complications, lower IQ and neuropsychological deficits, higher levels of concurrent and earlier symptoms of attention-deficit/hyperactivity (ADHD) and ODD, possibly greater aggression, and difficulties in school performance and peer relations, whereas adolescence-limited antisocial behavior is associated with greater affiliation with deviant peers and less severe maladjustment and negative outcomes in adulthood (Hinshaw, Lahey, & Hart, 1993; Lahey et al., 2006; Moffitt, 1993, 2003, 2006; Odgers et al., 2008). The correlates of childhood-onset and adolescent-onset antisocial behavior also are quite different (Lahey, et al., 2006; Lahey & Waldman, 2003; Odgers, et al., 2008) and, therefore, their causes and mechanisms could differ.
Thus, there is strong evidence that trajectories of broadly defined antisocial behavior differ considerably as a function of their age of onset and persistence. A rather different question is whether subtypes of CD based on age of onset should be distinguished as in DSM-IV. Challenges have been raised regarding its validity and utility, but evidence both for and against the DSM-IV subtypes of CD based on age of onset are thin (Moffitt, et al., 2008). The primary difficulty is that in the years since the publication of DSM-IV no longitudinal study has been published to our knowledge that prospectively distinguished between children who met criteria for CD according to DSM-IV criteria and exhibited childhood- and adolescent-onset CD types. This would be by far the strongest kind of study of developmental trajectories, but it would require large population-based samples that began in childhood and compared children who met criteria for childhood-onset CD to children who met criteria for adolescent-onset CD in later years of the study. Although there is support for the DSM-IV age of onset subtypes from studies that used the specific DSM-IV diagnostic criteria, the only data we have on the distinction are from studies that used potentially biased retrospective ages of onset of symptoms (Lahey, Loeber, et al., 1998; McCabe, Hough, Wood, & Yeh, 2001). These studies support the DSM-IV subtypes, particularly by finding greater aggression and ADHD in the childhood-onset group, but constitute weak evidence given their retrospective nature. Given the lack of stronger evidence, it is impossible to evaluate the DSM-IV subtypes of CD at this time.
Validity of subtypes based on callous-unemotional traits
Among the alternatives for subtyping CD that has received the most attention is the use of callous-unemotional traits (CU), a central aspect of psychopathic traits in youth, to subtype CD (Frick, 2009; Frick & White, 2008). In one proposal (Moffitt, et al., 2008), children who meet diagnostic criteria for CD would be subtyped based on their levels of CU traits.
There is now consistent evidence that among heterogeneous groups of children and adolescents with conduct problems (i.e., with diagnoses of either ODD or CD, but not all with CD) the children who are most elevated on CU traits tend to show more persistent CD symptoms, higher levels of proactive aggression (Frick & Viding, 2009; Frick & White, 2008), more serious antisocial outcomes (McMahon, Witkiewitz, & Kotler, 2010), and appear to have greater deficits in processing facial emotional expressions of fear and distress (Dadds, El Masry, Wimalaweera, & Guastella, 2008; De Brito et al., 2009; Marsh et al., 2008). These findings strongly imply that CU traits represent an important aspect of antisocial behavior and therefore might be a useful means of subtyping the disorder. Nonetheless, more evidence is needed to determine if there would be incremental value in using CU traits to subtype CD. In particular, the difficulty is that few data are available that compare children who actually meet DSM-IV criteria for CD and differ in their level of CU traits. One recent longitudinal study that compared children and adolescents with CD who differed in CU traits did not find differences in their antisocial outcomes (Burke, et al., 2010). This suggests that CU traits may be so high in children who meet criteria for CD that it does not work well as a subtyping variable for CD, but far more data are needed before this subtyping schema for CD can be fully evaluated.
Should Sex Differences be Reflected in the Nosology of Conduct Disorder?
It is clear that there are sex differences the rates of engagement in broadly defined antisocial behavior (i.e., not limited to CD symptoms) during childhood and adolescence (Moffitt, Caspi, Rutter, & Silva, 2001). Furthermore, when antisocial behavior is defined broadly it is clear that far more boys than girls exhibit high levels of adult-reported antisocial behavior during childhood that persists in the sense of high levels of self-reported antisocial behavior during adolescence. In contrast, the numbers of girls and boys who exhibit normative childhood behavior but engage in high levels of self-reported antisocial behavior during adolescence is nearly equal (Lahey, et al., 2006; Moffitt, et al., 2001).
It is also clear that boys engage in higher mean numbers of the specific DSM CD symptoms during childhood and adolescence as well, with this sex difference emerging somewhere between ages 4-7 years (Keenan, Loeber, & Green, 1999; Keenan & Shaw, 2003; Maughan, Rowe, Messer, Goodman, & Meltzer, 2004). There is currently conflicting evidence on whether the magnitude of the sex difference in mean CD symptoms increases in magnitude during adolescence (Lahey, et al., 2006) or remains relatively constant over age (Maughan, et al., 2004). Additional evidence is critically needed on this because sex-differentiated etiologic factors may be operating in adolescence if the sex ratio increases during this period.
The large sex difference in the prevalence of CD has prompted the question of whether CD should be diagnosed using different thresholds and different symptoms to equate the prevalence in the sexes. The key issue is whether different diagnostic criteria would identify equally impaired youth or whether lowering the threshold for girls would result in the overdiagnosis of unimpaired girls. A recent review of the literature and new analyses of a large representative longitudinal sample of girls suggested that there is not currently strong evidence for sex-specific diagnostic criteria for CD in girls (Keenan, et al., 2011). This is an important issue, however, and should be examined further in samples in which girls and boys are sampled and assessed in the same ways and can be directly compared.
CONDUCT DISORDER AND THE PHENOTYPIC AND CAUSAL STRUCTURE OF PSYCHOPATHOLOGY
We now turn to a review of evidence on the etiology of CD both because of its inherent importance and because of what it can tell us about the nosology of CD. One must be able to define disorder X to study its etiology, but studies of the etiology of X then become a rich source of evidence for refining the nosologic definition of X.
Our review of evidence on the etiology of CD takes a broad perspective. We believe that a sea change is needed in how data on the nature and causes of CD and other prevalent forms of psychopathology (i.e., ODD, ADHD, and the anxiety and depressive disorders) are conceived. Our views are similar to and strongly influenced by those of others (Angold & Costello, 2009; Krueger & Markon, 2006a, 2006b). Rather than considering each dimension of psychopathology to be a distinct entity whose nature and etiology should be studied in isolation, we believe that it is time to fully come to grips with the implications of the well-documented empirical fact that all prevalent mental disorders are highly correlated, particularly within broad higher-order domains (Lahey, Rathouz, et al., 2008; Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011).
The phenotypic correlations among prevalent forms of psychopathology are well known, but their fundamental importance largely has been ignored. It is probable that psychopathology phenotypes are correlated largely because they share common causes. Thus, the substantial correlations between CD and other forms of psychopathology argue that it is unlikely that any of these correlated dimensions of psychopathology have entirely unique genetic and environmental causes or distinct neurobiological risk mechanisms that instantiate these causal processes. If this view is correct, far more will be learned by studying each form of psychopathology in the context of the multiple other prevalent forms of psychopathology in model-driven studies than by continuing to study one mental disorder at a time.
We propose a novel perspective on the nosology, etiology, and nature of CD. We posit that it will not be possible to fully understand the fundament nature of CD until we understand why it is highly comorbid with a broad spectrum of other prevalent forms of psychopathology. Indeed, we believe that examining CD in this context will reveal important information about CD that has heretofore gone unnoticed. Specifically, we posit that CD shares a great deal of its genetic etiology and neurobiology with other prevalent mental disorders of children and adolescence. It is differentiated from other mental disorders partly by unique genetic influences and partly because varying environmental influences shape a general predisposition to psychopathology into more or less distinct symptom constellations in different individuals over time (Lahey, Van Hulle, et al., 2011).
Concurrent Comorbidity and Phenotypic Correlations among Dimensions of Prevalent Psychopathology
The empirical starting point for this new perspective is the robust pattern of comorbidity and correlations among CD and other forms of psychopathology at both diagnostic and dimensional levels. We believe that these correlations need to be understood in a new way—in a new Gestalt—to advance research on CD and other prevalent forms of psychopathology. It is well known that children who meet criteria for the categorical diagnosis of CD frequently also meet criteria for diagnoses of the other externalizing disorders at the same time, namely ADHD and ODD (Beauchaine, Hinshaw, & Pang, 2010; Biederman, Newcorn, & Sprich, 1991; Button et al., 2007; Hinshaw, et al., 1993; Lahey, 2008). What is less well appreciated is that there is also substantial concurrent overlap between diagnoses of CD and the internalizing disorders (Lahey, 2008; Maughan, et al., 2004), particularly major depressive disorder, dysthymia, and generalized anxiety disorder, which are often referred to collectively as ‘distress’ disorders (Watson, O'Hara, & Stuart, 2008). When child and adolescent psychopathology is treated dimensionally, there similarly is extensive evidence of robust correlations between CD symptoms and the symptoms of other prevalent forms of psychopathology (Achenbach, Conners, Quay, Verhulst, & Howell, 1989; Lahey, 2008).
The symptoms of prevalent forms of psychopathology have been the subject of many multivariate correlational studies. These were conducted primarily to determine which items (symptoms) were correlated with one another sufficiently to constitute dimensional syndromes and to determine the optimal number of syndromes necessary to comprehensively describe and classify the common dimensions of psychopathology.
Exploratory factor analyses
Many EFAs of items describing child and adolescent psychopathology have been conducted since the seminal studies of Quay, Peterson, and Achenbach (Achenbach, 1978; Quay & Peterson, 1967). In recent years, many studies have used items based on DSM-IV/ICD-10 symptoms in their EFAs. Nearly all of these studies of the symptoms used in DSM-IV and ICD-10 examined only subsets, such as all “externalizing” symptoms, as reviewed by Lahey et al. (2004, 2008), but an EFA has been conducted of all DSM-IV/ICD-10 symptoms of prevalent mental disorders in childhood and adolescence and other items resembling those included in widely-used rating scales (Lahey, Applegate, et al., 2004). Given the limited empirical evidence that went into the development of DSM-IV, it is remarkable that at the dimensional level the results of these EFAs consistently supported the decisions behind the assignment of symptoms to syndromes and the number of syndromes to distinguish in DSM-IV. Although little attention has been paid to this fact, these EFA-based studies have consistently shown that the dimensions of psychopathology in these ages are correlated to varying extents, often quite strongly. This consistent finding figures prominently in the argument that we develop in this paper.
Confirmatory factor analyses
Based on the results of the many EFAs of symptoms of child and adolescent psychopathology, a substantial number of confirmatory factor analyses (CFAs) have now been conducted to test alternative hypotheses regarding the correlational structure of both internalizing and externalizing symptoms (Bauermeister, Canino, Polanczyk, & Rohde, 2010; Gomez, Burns, Walsh, & de Moura, 2003; Higa-McMillan, Smith, Chorpita, & Hayashi, 2008) and of the full set of DSM-IV/ICD-10 symptoms of prevalent mental disorders (Hartman et al., 2001; Lahey, Rathouz, et al., 2008). In CFA, all parameters of the hypothesized model must be specified in advanced. This allows tests of significant differences in fit between alternative models to be made with a strong statistical basis regarding the number of dimensions, the items that load on those dimensions, and the correlational structure of the dimensions. These CFA studies have consistently supported the implicit hypotheses regarding the dimensional structure of symptoms underlying DSM-IV (Hartman, et al., 2001; Lahey, Rathouz, et al., 2008).
Of interest, a CFA study of DSM-IV symptoms of only the attention-deficit and disruptive disorders (DBDs) based on 309 clinic-referred children and adolescents and 230 healthy comparison children found that the DSM-IV three-dimensional model of the DBDs (inattention, hyperactivity-impulsivity, ODD, and CD) fit the data well. Nonetheless, the fit improved when a general bifactor was added on which all DBD symptoms loaded (Martel, Gremillion, Roberts, von Eye, & Nigg, 2010). We will have much more to say about the importance of this general bifactor as we develop our argument.
Thus, whether viewed in terms of the co-occurrence of diagnoses or concurrent correlations among symptom dimensions, CD and the other dimensions of prevalent forms of psychopathology are robustly correlated, but there is a structure to those correlations with some being stronger than others. In particular, in a CFA of a comprehensive list of DSM-IV and ICD-10 symptoms in a large and representative sample (Lahey, Rathouz, et al., 2008), the latent dimension of CD symptoms was significantly correlated with every other latent dimension of psychopathology. As shown in Figure 1, most of these correlations were in the r = .42 to .90 range, with the strongest correlations being between CD and the other externalizing disorders, but there also were moderately strong correlations with a dimension reflecting the symptoms of the distress disorders of major depression and generalized anxiety disorder and some other anxiety disorders. These patterns of concurrent phenotypic correlations are the first clear indication that the CD and other prevalent mental disorders have too much in common to study separately.
Figure 1.
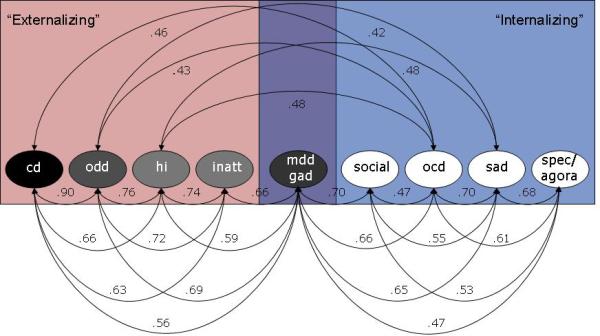
Correlations among latent factors in the best fitting phenotypic model of caretaker-reported dimensions of common dimensions of child and adolescent psychopathology. The best-fitting model included broad “internalizing” and “externalizing” factors of dimensions. Only correlations > .40 among dimensions are shown. Reprinted by permission from Lahey et al. (2008), Figure 5, page 196.
Genetic and Environmental Structure of CD and Other Prevalent Forms of Psychopathology
We have reviewed evidence showing that, like other prevalent forms of psychopathology, CD is robustly related to a wide range of other mental disorders. The fundamental question is why these disorders are correlated. The concurrent and predictive comorbidities and correlations among CD and other prevalent forms of psychopathology must be caused by something. We argue that understanding the causes of these correlations among dimensions of psychopathology will provide important new directions for future studies of CD and other prevalent mental disorders.
One possibility is that CD and other mental disorders are correlated both concurrently and longitudinally because they partly share the same causal influences (Kessler et al., 2011; Krueger & Markon, 2001, 2006b; Lahey, D'Onofrio, & Waldman, 2009; Rutter, Kim-Cohen, & Maughan, 2006). In this section, we review evidence on the genetic and environmental etiologic factors that underlie the correlated phenotypic structure of psychopathology and offer a testable model of the origins of these forms of psychopathology. This model warrants rigorous testing less because it may be accurate (i.e., supported by future studies) than because it addresses fundamental issues that cannot be ignored. Whether or not the current hypotheses are partly or wholly supported in the future, a well validated explanation for the phenomena that our model attempts to explain must be developed to guide further research and theory.
Univariate studies of genetic and environmental influences
Many biometric studies of one mental disorder at a time using genetically informative samples of siblings, twins, and adoptees have indicated that CD and other prevalent dimensions of psychopathology have moderate to substantial genetic influences (Ehringer, Rhee, Young, Corley, & Hewitt, 2006; Franic, Middeldorp, Dolan, Ligthart, & Boomsma, 2010; Lahey, Van Hulle, et al., 2011; Rhee & Waldman, 2002). These biometric studies partition the etiologic influences on psychopathology into additive genetic influences (A), shared environmental influences (C, which are shared by siblings and contribute to their similarity on a phenotype), and nonshared environmental influences (E, which are experienced uniquely by siblings and them make different on a phenotype) (Neale & Cardon, 1992). A, C, and E must be interpreted as composite categories, as A comprises genetic main effects, genetic selection into particular environments (gene-environment correlation), and interactions between genes and shared environmental influences (A × C). Similarly, E comprises the impact of environments not shared by the twins, interactions between genes and environments not shared by the twins (A × E), and measurement error (Rijsdijk & Sham, 2002). This means that the results of twin studies must be interpreted with these complexities in mind.
Bivariate studies of genetic and environmental influences
Of central importance to this paper, a large number of bivariate biometric studies have been conducted using models that can determine the extent to which one dimension of psychopathology shares some of its partitioned A, C, or E influences with another form of psychopathology (Neale & Cardon, 1992). These studies consistently have found that CD shares a considerable proportion of its genetic influences (A) with both ADHD and ODD (Dick, Viken, Kaprio, Pulkkinen, & Rose, 2005; Nadder, Rutter, Silberg, Maes, & Eaves, 2002; Tuvblad, Zheng, Raine, & Baker, 2009; Waldman, Rhee, Levy, & Hay, 2001) and with depression (Subbarao et al., 2008), but no bivariate biometric studies have examined the causes of the less robust comorbidity of CD with anxiety. Thus, although more remains to be learned, these bivariate studies suggest that CD shares genetic influences in common with a broad range of other dimensions of prevalent psychopathology. The next step is to study these broadly shared genetic influences among multiple forms of psychopathology in the same sample in multivariate biometric studies.
Multivariate studies of genetic and environmental influences in children and adolescents
We recently conducted a study of the genetic and environmental causes of correlations among multiple dimensions of prevalent forms of psychopathology using data from structured diagnostic assessments of a study of a representative sample of 1,571 pairs of 9-17 year old twins (Lahey, Van Hulle, et al., 2011). Phenotypic correlations among dimensional scores for 11 prevalent forms of psychopathology were partitioned into a covariance matrix (i.e., correlations expressed in nonstandardized form) among the psychopathology dimensions that could be attributed to shared A, C, and E using standard biometric twin models (Neale & Cardon, 1992). There was relatively little influence of C on most of the psychopathology dimensions, but we subjected the variance/covariance matrices for A and E to CFAs to test alternative hypotheses regarding the extent to which the 11 disorders were correlated due to shared A and/or shared E. The genetic covariances among the 11 mental disorders were high, reflecting a great deal of sharing of genetic influences (A). A two-factor CFA model for genetic covariances revealed that most genetic factors nonspecifically influenced risk for either all disorders within the “externalizing” domain or for all disorders within the “internalizing” domains. However, in this model the correlation between the externalizing and internalizing genetic factors was very high (r = .89). This suggests that the genetic influences on externalizing disorders and those on internalizing disorders were largely the same. Therefore, as shown in Figure 2, we compared the two-factor model to a model that also included a general bifactor (Gibbons & Hedeker, 1992) on which all 11 dimensions loaded. This bifactor reflects globally shared genetic risk among all 11 dimensions of psychopathology. This model fit significantly better and explained nearly all of the genetic correlation between the externalizing and internalizing genetic factors.
Figure 2.
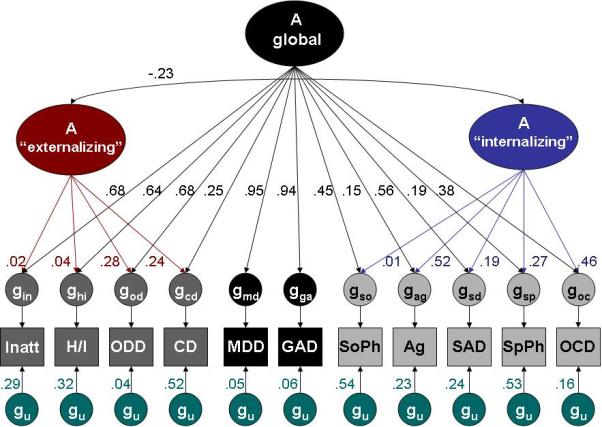
Proportions of genetic variance in combined caretaker- and youth-reported dimensions of child and adolescent psychopathology associated with three latent genetic factors and genetic influences unique to each specific dimension of psychopathology (gu). Inatt = inattention; H/I = hyperactivity-impulsivity; ODD = oppositional defiant disorder; CD = conduct disorder; MDD = major depression; GAD = generalized anxiety disorder; SoPh = social phobia; Ag = agoraphobia; SAD = separation anxiety disorder; SpPh = specific phobia; OCD = obsessive-compulsive disorder. Reprinted by permission from Lahey et al. (2011), Figure 1, page 185.
With some notable exceptions, Figure 2 also shows that dimension-specific genetic influences accounted for only modest amounts of the genetic variance in each individual dimension of psychopathology. It is very informative that CD is one of those notable exceptions. The proportion of genetic variance that is unique to CD (“gu” for CD in Figure 2) is greater at .52 than any other externalizing disorder. Similarly, the proportion of the genetic variance in CD that is shared with all other mental disorders (the .25 path from “A global” to gcd) is lower than the proportion for the other externalizing disorder dimensions. This figure also reveals differences in the genetic influences on ODD and CD. In sharp contrast to CD, ODD has only 4% unique genetic variance and shares nearly 96% of its genetic variance with other disorders (Lahey et al., 2011).
The results of the CFA of nonshared environmental influences were quite different. As shown in Figure 3, the best-fitting model for the nonshared environmental covariances also included a general bifactor and internalizing and externalizing factors as in the model of genetic covariances. Nevertheless, the degree of sharing of the nonshared environmental influences1 was minimal. Rather, most of the nonshared environmental influences were unique to each psychopathology dimension. This suggests that the vast majority of the phenotypic correlations among these common dimensions of psychopathology is due to genetic influences that are common to all of these dimensions.
Figure 3.
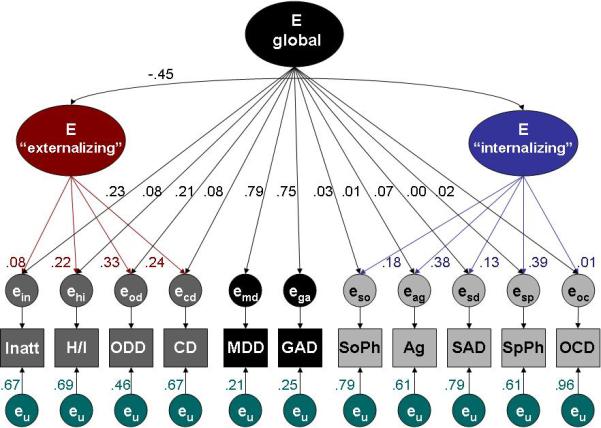
Proportions of nonshared environmental variance in combined caretaker- and youth-reported dimensions of child and adolescent psychopathology associated with three higher-order latent nonshared environmental factors and nonshared environmental influences unique to each specific dimension of psychopathology (eu). Inatt = inattention; H/I = hyperactivity-impulsivity; ODD = oppositional defiant disorder; CD = conduct disorder; MDD = major depression; GAD = generalized anxiety disorder; SoPh = social phobia; Ag = agoraphobia; SAD = separation anxiety disorder; SpPh = specific phobia; OCD = obsessive-compulsive disorder. Reprinted by permission from Lahey et al. (2011), Figure 2, page 186.
Published nearly simultaneously, the results of a study of 1162 twin pairs and 426 siblings (Cosgrove et al., 2011) also revealed that the genetic influences on higher-order internalizing and externalizing factors of child and adolescent psychopathology are strongly correlated (r = .74). A general genetic bifactor on which all disorders directly loaded was not estimated in this study, but the high degree of sharing of genetic influences on internalizing and externalizing disorders suggests that it might have improved the fit of their model. Also like the findings of the Lahey et al. (2011) study, CD was found to have substantial unique genetic influences, in spite of considerable sharing of genetic influences with other disorders. In addition, like Lahey et al. (2011), this study found that there were substantial disorder-specific nonshared environmental influences on each mental disorder. Thus, the results of these two studies (Cosgrove, et al., 2011; Lahey, Van Hulle, et al., 2011) converge, even though they used different modeling strategies.
Hypothesis 1: Generalist genes and specialist environments
Consistent with a causal model of cognitive abilities and disabilities (Kovas & Plomin, 2007), we offer a generalist genes/specialist environments hypothesis for all of the prevalent dimensions of child and adolescent psychopathology, including CD:
Generalist genetic influences
We hypothesize that the correlations between CD and other prevalent dimensions of child and adolescent psychopathology are primarily the result of two forms of pleiotropic genetic influences. One set of genetic factors nonspecifically increases risk for all prevalent forms of psychopathology (Cosgrove, et al., 2011; Lahey, Van Hulle, et al., 2011), whereas an apparently distinct second set of genetic influences further increases risk for all externalizing dimensions. In the case of CD, approximately half of the genetic influences on CD are shared with other disorder, but half is unique to CD (Cosgrove, et al., 2011; Lahey, Van Hulle, et al., 2011).
Specialist environmental influences
We further hypothesize that nonshared environmental influences mostly serve to differentiate all of the prevalent dimensions of psychopathology from one another. In particular, like other symptom dimensions, CD is differentiated from other mental disorders in large part by unique nonshared environmental influences that influence siblings in different ways.
Generalist genes and specialist environments in adults
It is important that analyses of a large multivariate twin study of common genetic and environmental influences on 10 prevalent mental disorders in a representative sample of adults also support the generalist genes/specialist environments hypothesis (Kendler et al., 2011; Kendler, Prescott, Myers, & Neale, 2003). As these investigators put it, “The pattern of lifetime comorbidity of common psychiatric and substance use disorders results largely from the effects of genetic risk factors.” (Kendler, et al., 2003) (p. 292). In their studies, there was widespread sharing of genetic influences among externalizing disorders and among internalizing disorders, but very little sharing of environmental influences by these disorders. Thus, as in children and adolescents (Lahey, Van Hulle, et al., 2011), the correlations among mental disorders was found to be almost exclusively due to shared genetic influences. A general psychopathology bifactor was not fit in either set of analyses, but the correlation between genetic influences on externalizing and internalizing disorders was large enough (Kendler, et al., 2011) that the addition of such a factor may have resulted in a better fit to the data.
Etiologic Differences between Aggressive and Nonaggressive CD
Earlier we reviewed evidence that models distinguishing aggressive and nonaggressive dimensions of CD symptoms fit better than a unidimensional model of CD and that aggressive and nonaggressive CD have different correlates. We turn now to etiologic studies that may inform the decision on potentially distinguishing between aggressive and nonaggressive CD behaviors. If aggressive and nonaggressive CD behaviors have substantially different etiologies, it would be useful to distinguish them both in etiologic research and in the development of effective preventive and treatment interventions based on their etiologies.
Studies using the CBCL
Several bivariate biometric studies examined common and unique genetic and environmental influences on aggressive and nonaggressive conduct problems using the CBCL (Edelbrock, Rende, Plomin, & Thompson, 1995; Eley, Lichtenstein, & Moffitt, 2003; Eley, Lichtenstein, & Stevenson, 1999). It is notable that ODD symptoms are included on the scale measuring aggressive conduct problems and the measure of nonaggressive conduct problems is broader than in DSM and ICD definitions, including early substance use and affiliation with peers who get into trouble. These CBCL-based studies yielded three consistent findings: First, there were substantial genetic influences on both aggressive and nonaggressive conduct problems, although these were of greater magnitude for ODD+aggressive conduct problems. Second, shared environmental influences were either only present for nonaggressive conduct problems or were of greater magnitude for nonaggressive conduct problems than for aggression. Third, although there were substantial common genetic influences on aggression and nonaggressive conduct problems, each dimension of conduct problems showed additional unique genetic influences.
Studies using DSM and ICD symptoms
In spite of differences in the definitions of the dimensions, the results of more recent biometric studies of aggressive and nonaggressive conduct problems using DSM and ICD CD symptoms have largely supported findings based on the CBCL. A meta-analysis of these studies (Burt, 2009) found that genetic influences are more substantial on aggressive conduct problems than on nonaggressive conduct problems (heritabilities = 65% and 48%, respectively), and that only the latter showed significant shared environmental influences (accounting for 18% of the variance).
Taken together, these findings suggest that it could be very useful to distinguish between aggressive and nonaggressive CD behaviors in future etiologic studies. It is important to note, however, that there is evidence that the substantial correlation between aggressive and nonaggressive CD is primarily due to common genetic influences on both forms of CD (Barker et al., 2009; Gelhorn et al., 2006; Tackett, et al., 2005). Thus, there may be both overlapping and distinct causal influences on aggressive and nonaggressive CD.
Studies of the etiology of reactive and proactive aggression
It is also important to look at etiologic studies to see if they support distinctions between subtypes of aggression. Two biometric studies of reactive and proactive aggression have been conducted. A study of 172 6-year-old twin pairs (Brendgen, Vitaro, Boivin, Dionne, & Perusse, 2006), found very similar magnitudes of genetic and nonshared environmental influences on proactive (h2 = .41, e2 = .59) and reactive aggression (h2 = .39, e2 = .61), with a high correlation between the genetic influences on each dimension of aggression (r = .87). A study of 1219 9- to 10-year-old twins (Baker, Raine, Liu, & Jacobson, 2008) yielded considerably more complex results. Baker and colleagues found a significant sex difference in the magnitude of genetic and environmental influences on aggression, in which moderate genetic influences were found for boys but not girls, whereas moderate shared environmental influences were found for girls but not boys (boys; h2 = .38 and e2 = .62 for reactive aggression and h2 = .50 and e2 = .50 for proactive aggression; girls: c2 = .36 and e2 = .64 for reactive aggression and c2 = .14 and e2 = .86 for proactive aggression). In contrast, no sex differences were found for mother or teacher reports. As in the Brendgen et al. study, however, common genetic and environmental influences were both responsible for the correlation between proactive and reactive aggression, with the former being moderate-to-high and the latter being small-to-moderate in magnitude. Thus, there is currently not consistent evidence that proactive and reactive aggression differ substantially in their etiologies, but more research is needed.
Studies of the etiology of relational aggression
A study of 172 6-year-old twin pairs (Brendgen et al., 2005) examined the association between physical and relational aggression and found that genetic influences were greater in magnitude for physical than for relational aggression (h2 = .54 - .63 versus h2 = .20 - .23, respectively). It is noteworthy that there were shared environmental influences on relational but not physical aggression, and that these were equal in magnitude to the genetic influences underlying relational aggression. Phenotypic overlap between the two forms of aggression was mainly due to common genetic influences. In a sample of 7449 7-year-old twin pairs (Ligthart, Bartels, Hoekstra, Hudziak, & Boomsma, 2005), however, similar genetic, shared environmental, and nonshared environmental influences were found on both relational and direct aggression (h2 = .53 - .66, c2 = .13 - .23, e2 = .18 - .27) . The phenotypic correlation between relational and direct aggression was due mainly to common genetic influences and to a lesser extent to common environmental influences. Thus, there is not currently sufficient evidence to distinguish relational and physical aggression on etiologic grounds.
Issues in Understanding the Causal Structure of Child and Adolescent Psychopathology
In order to move forward our understanding of the nosology and etiology of CD, some issues regarding current evidence on the causal structure of child and adolescent psychopathology, and their implications for future research, need to be considered.
Note on the “fear” and “distress” dimensions of psychopathology
Several studies of the correlational structures of mental disorders using large and representative samples of adults have found that models of phenotypic correlations fit better when the higher-order internalizing factor is divided into factors corresponding to fears (phobias and panic) and distress (major depression, dysthymia, generalized anxiety disorder, and post-traumatic stress disorders) (Krueger & Markon, 2006a). We did not test such a model in the study of the causal structure of psychopathology in children and adolescents (Lahey, Van Hulle, et al., 2011) because we did not assess post-traumatic stress disorder and our dimensional measure of psychopathology did not allow a distinction between major depression and dysthymia. Nonetheless, it is clear that depression and generalized anxiety disorder are (a) more strongly correlated at the phenotypic level with CD than are the fear dimensions (Figure 1) (Lahey, Rathouz, et al., 2008), and (b) share genetic influences with CD to a greater extent than do the fear dimensions (Figure 2). Thus, it is likely that the distinction between fear and distress dimensions of psychopathology is relevant to CD, even though the fear and distress dimensions are themselves highly correlated.
Potential confounding role of global rater bias in multivariate studies
It is important to consider the possibility that the correlations among dimensions of psychopathology are partly due to global rater biases in which the presence of some symptomatic behaviors increase the likelihood of inflated reports of symptoms of other disorders. This issue has not been studied extensively, but there is replicated evidence from controlled experiments that adults tend to rate children who engage in only oppositional behaviors as exhibiting symptoms of attention-deficit/hyperactivity disorder, and perhaps vice versa (Abikoff, Courtney, Pelham, & Koplewicz, 1993; Hartung et al., 2010). Because assessments of psychopathology are almost exclusively conducted using self- and other-reports of symptoms, rater bias could inflate comorbidity at every level of analysis, from the studies of the bivariate comorbidity of any pair of mental disorders to the general psychopathology factor identified by Lahey et al. (2011).
It is essential to note, therefore, that two kinds of empirical findings argue that it is unlikely that reports of symptoms of psychopathology are fatally obscured by rater biases. First and foremost, there is clearly an adequate and useful degree of specificity in reports of symptoms of child and adolescent psychopathology. That is, in clinic-based samples, parent and teacher ratings of each dimension of externalizing psychopathology are uniquely associated with measures of functional impairment, even when all other dimensions are controlled (Lahey, Pelham, et al., 2004; Lahey, Pelham, et al., 1998). Moreover, both parent and youth reports of every prevalent dimension of psychopathology accounted for unique variance in appropriate aspects of functional impairment when all other dimensions were controlled in a population-based sample (Lahey, Applegate, et al., 2004). This could not be the case if comorbidity was solely the result of specious reporting of symptoms that are not actually present due to negative halos created by the perception of those symptoms that are actually present.
Second, the correlational structure of child and adolescent psychopathology is substantially differentiated at both the phenotypic (Lahey, Rathouz, et al., 2008) and etiologic levels (Lahey, Van Hulle, et al., 2011). For example, although all dimensions are positively correlated (at statistically significant levels in large samples), some correlations are very high (e.g., CD and ODD), some are moderate (e.g., CD and depression), and some are small (e.g., CD and specific phobias). Thus, the correlations among dimensions of psychopathology are differentiated rather than nonspecific. Informants do not simply report all kinds of symptoms when they perceive the presence of one form of symptoms.
It is clearly important to continue to study the likely role of rater bias in influencing the correlational structure of psychopathology. The real test of structural models based on the correlations among dimensions of psychopathology, however, is whether they help us understand the etiology of psychopathology and the role of biopsychological processes in psychopathology. We suspect that rater bias contaminates the correlational structure of psychopathology to some extent, but we posit that models based on those correlations will be of considerable scientific and clinical utility.
LONGITUDINAL COMORBIDITY AND CORRELATIONS AMONG DISORDERS
The cross-sectional factor analytic and biometric studies just reviewed reveal strong concurrent correlations among dimensions of psychopathology and robustly shared genetic influences among these prevalent disorders, but they provide only a “snap shot” of correlational patterns in the concurrent symptoms at a single point in time. It is of great importance, therefore, that longitudinal studies of the same individuals over time provide striking evidence that cross-sectional studies considerably underestimate the extent to which nominally different forms of psychopathology are correlated (Rutter, et al., 2006). In reviewing this evidence, we distinguish between two types of “longitudinal” comorbitiy over time: heterotypic continuity and dynamic comorbidity.
Longitudinal Comorbidity: Heterotypic Continuity
Although many children with CD and other forms of psychopathology improve over time, many others show a course that reflects short-term variability superimposed over relatively high stability in symptoms over time (homotypic continuity) (Ferdinand, Dieleman, Ormel, & Verhulst, 2007; Keenan, Feng, Hipwell, & Klostermann, 2009; Lahey et al., 1995a; Lahey, Pelham, et al., 2004). Furthermore, longitudinal studies also reveal the robust predictive relations between childhood CD and other forms of psychopathology over time (heterotypic continuity) (Copeland, Shanahan, Costello, & Angold, 2009; Reef, van Meurs, Verhulst, & van der Ende, 2010). Although data from longitudinal studies have not been extensively analyzed to directly address this issue, the strongest heterotypic continuity appears to be within the “externalizing” and “internalizing” disorders. In the case of CD, childhood and adolescent CD robustly predicts the future emergence of other eternalizing disorders, including both antisocial personality disorder (Burke, et al., 2010; Copeland, et al., 2009; Lahey, Loeber, Burke, & Applegate, 2005; Odgers, et al., 2008) and substance use disorders (Fergusson, Horwood, & Ridder, 2007). Nonetheless, children with CD also are at substantially increased risk for developing internalizing disorders in adolescence and adulthood, including both depression and some anxiety disorders (Burke, et al., 2005; Capaldi, 1992; Fergusson, Horwood, & Ridder, 2005; Odgers, et al., 2008). Notably, both robust homotypic (Lahey, et al., 1995a) and heterotypic (Burke, et al., 2005; Lahey, Loeber, Burke, Rathouz, & McBurnett, 2002) continuity of CD have been observed in the same samples. This suggests that both forms of continuity appear to be common features of the developmental course of CD. It should be noted that not all studies of the heterotypic continuity of CD have controlled for concurrent ODD and other mental disorders at time 1 when assessing the extent to which CD predicts other mental disorders. When this has been done, however, CD has often, although not always, emerged as a significant independent predictor of other forms of psychopathology (Copeland, et al., 2009; Reef, et al., 2010).
Thus, CD and other prevalent dimensions of psychopathology are not only concurrently correlated at any single point in time, they are also are prospectively correlated—both within and across the broad externalizing and internalizing domains—from one point in time to the next. That is, prevalent forms of psychopathology have the properties of mythic “shape shifters.” The particular symptoms of psychopathology exhibited often shift enough over time to lead to the addition of another diagnosis or a change from one diagnosis to another. The consistent findings of robust heterotypic continuity of CD are at least as important to the thesis of this paper as are the high levels of concurrent correlations among CD and other dimensions of psychopathology at a single point in time.
Causal models of heterotypic continuity
To fully understand the nature of CD, or any prevalent mental disorder, it will be essential to develop and test causal models of heterotypic continuity. In our view, both concurrent comorbidity and heterotypic continuity are the results of shared etiologic influences. There are many different ways in which causal influences could be shared across mental disorders (Krueger & Markon, 2006a). At least two possible models, which are not mutually exclusive, seem particularly worth careful consideration, however.
Heterotypic continuity may reflect psychopathological progressions that are a special case of “developmental cascades” (Masten et al., 2005). This term refers to the processes through which behavioral functioning at one point in time influences the environment in ways that influence another form of behavior at a later point in time. For example, there is replicated evidence consistent with the hypothesis that childhood CD increases the likelihood of adverse life events (e.g., school failure, peer rejection, and incarceration) which increase the likelihood of subsequent adolescent depression (Burke, et al., 2005; Patterson, 1993; Patterson & Stoolmiller, 1991).
It is possible that a common set of pleiotropic genetic variants (or ‘pleiotropic’ environments) directly increases the risk for different mental disorders at different times in life. The genetic predisposition may be manifested as different mental disorders at different times due to interactions with physical development (e.g., increased myelination of neural networks or body strength), changes in social environments (e.g., increased unsupervised time or the emergence of dating), or due to other environmental conditions that vary over time that are not brought about by the individual's behavior as in developmental cascades.
It is important to note that these two models both involve the same causes giving rise to different syndromes at different points in time. That is, in both models, the common causal risk factors for psychopathology have a constant impact on risk for maladaptive behavior in general, but the particular symptoms of psychopathology that are manifested over successive points in time would vary in the ways that are referred to as heterotypic continuity. Again, this argues for a new emphasis on the common underlying causes of psychopathology that result in their correlations and a move away from only studying mental disorders one at a time as if they were completely distinct and unrelated.
Note that these models are consistent with the fact that heterotypic continuity is sequenced and not symmetrical. That, some transitions from one disorder at time 1 to another at time 2 are more likely than others. For example, children who meet criteria for CD are more likely to meet criteria for major depression for the first time in adolescence than vice-versa (Burke, et al., 2002; Burke, et al., 2005; Patterson & Capaldi, 1990). This non-random sequencing of heterotypic continuity likely reflects interactions between pleiotropic genetic influences and developmental factors.
Hypothesis 2: Heterotypic continuity of CD
We hypothesize that the matrix of etiologic factors that give rise to concurrent correlations among dimensions of CD and other prevalent forms of psychopathology are the same factors that give rise to their heterotypic continuity. In particular, we hypothesize that enduring pleiotropic genetic liabilities contribute to the persistence over time of psychopathology in general whereas nonshared environmental factors shape and reshape the specific symptoms of psychopathology that are exhibited over time. This is likely to occur both through age-related changes in expression of genetic influences due to interactions with developmental factors and through developmental cascades. We further hypothesize that the role of nonshared environmental factors in these longitudinal patterns is critical, but remains to be worked out (Rutter, 2011).
Dynamic Comorbidity: Concurrent Waxing and Waning Over Time
Loeber and collaborators followed a sample of clinic-referred boys with CD over 7 years (Loeber, Green, Keenan, & Lahey, 1995). They found a dramatic dynamic association from year to year between levels of CD symptoms and those of ODD, ADHD, depression, and anxiety disorders. In youth whose CD behaviors improved (or worsened), their levels of all other symptoms also significantly improved (or worsened) in a clear time-locked pattern. In youth whose CD behaviors remained relatively constant over time, their other symptoms also remained constant (Lahey, et al., 2002). Other longitudinal studies have replicated this theoretically important pattern of dynamic comorbidity of CD with a range of other mental disorders (Barker, Oliver, & Maughan, 2010; Beyers & Loeber, 2003).
This pattern of dynamic comorbidity is a highly revealing complement to the heterotypic continuity seen in CD over time. In both cases, CD is more strongly related to other forms of psychopathology over time than it is distinct from them. Sometimes the interplay of fixed and time-varying causal factors result in shifts from symptoms of CD to the symptoms of other disorders, or the addition of symptoms of other disorders (heterotypic continuity). At other times, as yet unidentified time-varying causal factors cause CD and other correlated dimensions of symptoms to increase or decrease in time-locked synchrony. These time-varying causal influences that influence the course of symptoms over time—in patterns of either heterotypic continuity or dynamic comorbidity—are very likely to be environmental, but remain to be identified.
Hypothesis 3: Dynamic comorbidity of CD
We hypothesize that dynamic comorbidity over time—the tendency for many forms of psychopathology to wax and wane in time-locked fashion over time—is caused by time-varying environmental factors that are able to robustly influence multiple dimensions of psychopathology simultaneously. One potential candidate for the time-varying environmental factors that could change the course of multiple forms of psychopathology over time is stressful life events (Timmermans, van Lier, & Koot, 2010), but much remains to be learned about such crucially important environmental influences and their interactions with genetic risk processes. Because of the important implications for both theory and the design of psychosocial treatments, these hypothesized environmental influences should be a topic of future research.
Are There Sex Differences in the Etiology of CD?
There is consistent evidence from twin and sibling studies that the same genetic and environmental factors influence broadly defined antisocial behavior in both girls and boys (Cosgrove, et al., 2011; Ehringer, et al., 2006; Van Hulle, Rodgers, D'Onofrio, Waldman, & Lahey, 2007). Nonetheless, it is possible but by no means clear that females have a higher “threshold” for these genetic influences than boys and require a higher level of etiologic influences for the expression of antisocial behavior (Van Hulle, et al., 2007). Additional research is needed on this vital issue in genetically informative samples in which DSM-IV symptoms were measured. It will be necessary to identify the factors that cause the robust sex difference in the prevalence of CD to have a fully complete understanding of the etiology of CD. Furthermore, if females have a different threshold for etiologic influences on CD, identifying its components may inform prevention science. That is, in theory at least, it may be possible to manipulate factors in boys to increase their thresholds, as well. In this context, a review of biological factors that may contribute to the sex differences in childhood-onset CD is of interest (Eme, 2007).
IMPLICATIONS OF ETIOLOGIC RESEARCH FOR THE NOSOLOGY OF CD
The research on the causes of CD reviewed here has some important implications for nosology. First, the distinction between ODD and CD in DSM-IV is supported by studies of their shared and unique causal influences. CD differs from ODD in having greater disorder-specific genetic influences and less common genetic influences that are shared with other disorders. That said, CD and ODD still share about half of their genetic influences with each other (Figure 2) and some of their nonshared environmental influences (Figure 3) (Lahey, Van Hulle, et al., 2011). Second, additional etiologic research could provide a strong basis for distinguishing between aggressive and nonaggressive CD on etiologic grounds. Such research would need to take the potentially important confound between aggression and developmental trajectories into consideration. If longitudinal studies find that childhood-onset CD is characterized by greater aggression than adolescent-onset CD as cross-sectional studies suggest (Lahey et al., 1999; Lahey, Loeber, et al., 1998), then what appears to be an etiologic difference between aggressive and nonaggressive CD might be better explained by differences in developmental trajectory. At this point, there is insufficient etiologic evidence to support the proposed distinctions between proactive and reactive aggression and between physical and relational aggression. These issues deserve further study, but for the reasons summarized above, there is not clear evidence at the phenotypic level that these distinctions should be made in DSM-V and ICD-11.
Third, until now, nosologic research has focused on the validity of distinguishing among syndromes of maladaptive behavior. Although that has been necessary, we posit that a full understanding of psychopathology will equally require an understanding of the correlations among syndromes and the causal factors underlying those correlations. Current evidence strongly suggests that, like every other prevalent mental disorder, CD is far from distinct from other mental disorders in etiology. CD is correlated with other syndromes both concurrently and predictively and it shares about half of its genetic influences, and some of its environmental influences, with other syndromes. Keeping the unresolved issues and caveats noted above, it appears this sharing of etiologic influences is the basis for the high correlations between CD and other mental disorders.
If we expand our understanding of the causal relations among prevalent mental disorders, we should be able to greatly improve prognosis and prevention. That is, it should be possible to predict both comorbidity and the heterotypic continuity from childhood CD to other mental disorders during adolescence by tracing the paths that connect disorders in models like that illustrated in Figure 2. In this sense, it is not surprising that CD often co-occurs in the same individuals (concurrently and at different times) with other disruptive behavior disorders because it shares half of its genetic influences with them. Similarly, consistent with the empirical evidence reviewed above, CD would be expected to co-occur with major depression and generalized anxiety disorder (distress disorders) more often than with the other (fear-based) internalizing disorders because, as shown in Figure 2, fear disorders share a smaller proportion of their genetic influences with CD through the global genetic factor than do the distress disorders.
To the extent that heterotypic continuity reflects different environmentally influenced manifestations of the same pleiotropic genetic influences, disorders that share more genetic influences with CD should be more likely to be comorbid or to occur in the same individual at different points in time (heterotypic continuity). As our understanding of the nonshared environmental influences that differentiate and change mental disorders improves, we will further improve our predictions and should be able use this knowledge to promote recovery and reduce the likelihood of heterotypic continuity.
IMPLICATIONS FOR FUTURE RESEARCH
The evidence reviewed here on the causal structure of CD and other prevalent mental disorders has potentially important implications for future research.
Refining the phenotype of CD
It is critically important to determine if the unidimensional definition of CD in DSM-IV provides an adequate phenotype for all research purposes or, perhaps more likely, a distinction should be made between aggressive and nonaggressive dimensions of CD for some purposes. At this point, it appears unlikely that a distinction between reactive and proactive aggression or between relational and physical aggression should be made in DSM-V and ICD-11, but the evidence reviewed above suggests that some of the behaviors that define these constructs should be considered as new symptoms of CD. Until these fundamental nosologic questions are answered, etiologic research may be misleading because it is not using the best possible phenotypes.
At the level of the diagnosis of CD, it is equally important to resolve open questions regarding the possible subtypes of CD. This can be accomplished especially well using longitudinal studies that are designed to shed light on etiology. This is because it is possible that dividing youth with CD into subgroups based on levels of aggression, “undersocialization,” or CU traits, or distinguishing subgroups based on childhood- versus adolescent-onset trajectories, would largely identify the same subgroups of individuals with CD (Lahey, et al., 2006; Moffitt, Caspi, Dickson, Silva, & Stanton, 1996; Odgers, et al., 2008). Only longitudinal studies that can address developmental trajectories can determine which, if any of these potential subtyping variables is valid.
Strategies for molecular genetic studies
If the generalist genes/specialist environments hypothesis is supported in future studies, designing studies for finding molecular genetic risk factors for CD and related disorders with this model in mind should facilitate the identification of both pleiotropic and CD-specific genetic variants. Such studies would need to differ from recent studies in two ways. First, they would have to assess most if not all of the prevalent mental disorders and model the higher-order phenotypes shown in Figure 2 rather than assessing only one mental disorder. Second, they could not be based on case-controls design, because selecting the cases for the sample based on only CD would bias associations between gene variants and the other prevalent forms of psychopathology. Thus, population-based studies in which all prevalent mental disorders are measured and associations between genetic variants and both specific dimensions of psychopathology and higher-order phenotypes are modeled might greatly increase the power to identify the highly important pleiotropic genetic variants that influence CD and other prevalent mental disorders.
Indeed, failing to recognize the possibility of both pleiotropic and disorder-specific genetic influences on any mental disorder could seriously interfere with molecular genetic research. For example, consider the situation in which polymorphism X is pleiotropically associated with general risk for all prevalent forms of psychopathology, but was examined in a study that only measured CD. For children who have the risk allele and exhibit ODD instead of CD at time of the study, the lack of association between the genetic variant and CD would be a highly misleading false negative. This is because it would underestimate the importance of the genetic variant to risk for psychopathology in general, thereby failing to identify a genetic variant that is related to CD because it is related to all forms of psychology in general, which appears to be one of major classes of genetic influence on CD.
Strategies for studies of nonshared environmental influences
If the generalist genes/specialist environments model is supported, it would mean that studies of aspects of the environment that are not shared by siblings and tend to make them different would be of great importance. The model states that these environmental variables help differentiate one form of psychopathology from another (along with disorder-specific genetic influences). Furthermore, according to the model, these environments are strong enough to cause both heterotypic continuity and dynamic comorbidity. That is, in theory, these environments have the power to robustly change behavior. If this is correct, they must be identified. Harnessing such powerful variables may well give us the ability to intentionally change maladaptive behavior for the better.
Because of the great potential importance of the nonshared environmental variables, our future studies of them should not just test for correlations, but should test causal environmental hypotheses. In some cases, it will be possible to randomly assign individuals to different exposures to the putatively causal environments to conduct strong tests of the causal hypothesis. The assumptions of randomized experiments cannot always be met and they are not always feasible, however (West, 2009). For such cases, quasi-experimental designs have been devised to test causal hypotheses by ruling out plausible alternative explanations (Lahey & D'Onofrio, 2010; Shadish, Cook, & Campbell, 2002). Quasi-experiments support causal inferences in the same way as randomized experiments—by controlling genetic and environmental variables that are confounded with the hypothesized causal environment. They do so by adding design elements to observational studies that allow the researcher to compare the obtained results to both (a) the results expected if the environmental variable has a true causal effect, and (b) the results expected under alternative hypotheses of confounding of the environment with other causal influences (Shadish, et al., 2002; West & Thoemmes, 2010). Quasi-experimental designs rarely, if ever, control all potential confounds, but well-designed quasi-experiments substantially reduce the number of alternative explanations for apparent causal effects. Crucially, when different quasi-experiments with different flaws support the same conclusion, the causal inference is strengthened considerably.
Strategies for studying the neurobiology of CD
The present model also has important implications for the way in which studies of the neurobiological mechanisms underlying CD and other forms of psychopathology are designed. Currently, the neural bases of mental disorders are studied one disorder at a time as if each disorder has a unique neural basis. That would make sense if prevalent mental disorders were not correlated with one another, but as this review makes clear, that is decidedly not the case. Because genes influence behavior by coding for the synthesis of proteins that underlie various aspects of nervous system structure and function, as well as many other potentially relevant biological structures and systems, the pervasive sharing of genetic influences across multiple forms of psychopathology suggested by this review means that the neurobiological basis of CD is almost certainly shared with other prevalent mental disorders. This means that studies of the neurobiology of psychopathology should focus on both the common and disorder-specific neurobiological mechanisms underlying psychopathology using a structural model of shared and specific etiology to guide research. In the case of CD, because half of the genetic etiology of CD appears to be unique to CD, identifying both the common and disorder-specific neurobiology of CD will likely require studies including large numbers of children and adolescents with CD.
Importance of studying sex differences
It is essential that future research continue to seek an explanation of sex differences in the prevalence of CD. The magnitude of these sex differences is so large that a theory of the origins of CD that does not explain sex differences would be incomplete (Moffitt, et al., 2001; Rutter, Caspi, & Moffitt, 2003). Conversely, understanding sex differences would greatly facilitate understanding of the causes of CD in general. In particular, it will be important to determine if CD has fundamentally different causes in the two sexes or, as currently appears more likely, boys and girls are influenced by the same etiological factors but has different thresholds for the manifestation of CD (Van Hulle, et al., 2007).
A future direction for research: Dispositional dimensions and risk for psychopathology
We previously presented (Lahey & Waldman, 2003, 2005) and subsequently supported the hypothesis (Lahey, Applegate, et al., 2008; Lahey, Rathouz, Applegate, Tackett, & Waldman, 2010) that CD is most common among children and adolescents who exhibit low cognitive abilities and high levels of one or more socioemotional dispositions: (1) a tendency to respond excessively with negative emotions to threat and frustration; (2) low levels of prosocial/sympathetic concern for others and guilt over misdeeds, conceived as synonymous with the core of CU traits (Frick & White, 2008); and (3) high levels of daring and fearless sensation seeking (Lahey, Applegate, et al., 2008; Lahey, et al., 2010). Also consistent with this hypothesis, we have shown in two samples that a substantial proportion of the genetic variance in CD and other externalizing disorders is shared in common with these three dispositions, particularly prosociality and negative emotionality (Singh & Waldman, 2010; Waldman et al., 2011). This is important because biometric studies have suggested that CU traits are moderately heritable (Forsman, Lichtenstein, Andershed, & Larsson, 2008; Viding, Blair, Moffitt, & Plomin, 2005; Viding, Jones, Frick, Moffitt, & Plomin, 2008), that they substantially share common genetic influences with CD (Viding, Frick, & Plomin, 2007), and that CD is more heritable when accompanied by high levels of CU (Forsman, et al., 2008; Viding, et al., 2005; Viding, et al., 2008).
Based on recent evidence (Barker, et al., 2007; Barker, et al., 2011) we now hypothesize that cognitive abilities are specifically related to aggressive CD and not nonaggressive CD. We further hypothesize that the global genetic risk factor in Figure 2 is strongly related to the genetic influences on negative emotionality. An influential review of current evidence on adult psychopathology (Krueger & Markon, 2006a) suggested that individuals with internalizing disorders are high on the trait of negative emotionality and persons with externalizing disorders are high on both negative emotionality and disinhibition. If that is correct, then negative emotionality should be closely linked to general liability to psychopathology (Lahey, Van Hulle, et al., 2011). Furthermore, it seems likely that the externalizing genetic risk factor is also associated with both low levels of constraint and low levels of prosociality and the internalizing genetic risk factor is associated with high levels of constraint (Krueger & Markon, 2006a, 2006b; Lahey, Applegate, et al., 2008; Lahey, et al., 2010).
Another potential reason for studying negative emotionality is its possible role in dynamic comorbidity. One possible explanation for time-locked changes in levels of multiple dimensions of psychopathology over time would be stressful events that impact negative emotionality, which is robustly associated with risk for multiple forms of psychopathology (Krueger & Markon, 2006b; Lahey, Applegate, et al., 2008; Lahey, et al., 2010).
Key Points.
Although some nosologic questions remain unanswered, CD is a well-described and relatively independent dimension of psychopathology that is relatively distinct from ODD and associated with specific forms serious impairment and harm to victims.
The robust correlations of CD with many other prevalent dimensions of psychopathology, both concurrently and longitudinally are highly informative when viewed from the perspective of the etiologic factors that cause those correlations.
Recent multivariate biometric studies of twins suggest that the robust concurrent and longitudinal correlations among prevalent forms of psychopathology result primarily from widespread genetic pleiotropy that nonspecifically influences risk for all prevalent forms of psychopathology to varying degrees; unlike ODD and most other dimensions of psychopathology, however, about half of the genetic influences on CD appear to be unique to CD.
Environmental influences mostly act to differentiate dimensions of psychopathology from one another and to shape and reshape symptoms over time.
Because genes influence behavior by coding for protein structures of neurons and other organs, recent findings on the role of highly pleiotropic genetic influences suggest that CD will be found to share much of its neurobiological mechanisms with other prevalent forms of psychopathology, but probably has some unique underlying mechanisms as well.
Acknowledgement
This review article was invited by the journal, for which the principal author has been offered a small honorarium payment towards personal expenses.
This manuscript is based on material funded by the NIH.
Abbreviations
- CD
conduct disorder
- ODD
oppositional defiant disorder
- EFA
exploratory factor analysis
- CFA
confirmatory factor analysis
- A
additive genetic influences
- C
shared environmental influences
- E
nonshared environmental influences
Footnotes
This is neither an oxymoron nor a truism that is true by definition. Nonshared environmental influences influence siblings differently and make them less similar. In theory, however, the same nonshared environmental influences could influence more than one dimension of psychopathology in the same way, making them correlated.
The author(s) has/ve declared that they have no competing or potential conflicts of interest.
References
- Abikoff H, Courtney M, Pelham WE, Koplewicz HS. Teachers ratings of disruptive behaviors: The Influence of halo effects. Journal of Abnormal Child Psychology. 1993;21:519–533. doi: 10.1007/BF00916317. [DOI] [PubMed] [Google Scholar]
- Achenbach TM. The Child Behavior Profile: I. Boys aged 6-11. [Journal; Peer Reviewed Journal]. Journal of Consulting and Clinical Psychology. 1978;46:478–488. doi: 10.1037//0022-006x.46.3.478. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Conners CK, Quay HC, Verhulst FC, Howell CT. Replication of empirically derived syndromes as a basis for taxonomy of child and adolescent psychopathology. [Article]. Journal of Abnormal Child Psychology. 1989;17:299–323. doi: 10.1007/BF00917401. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ. Nosology and measurement in child and adolescent psychiatry. [Article]. Journal of Child Psychology and Psychiatry. 2009;50:9–15. doi: 10.1111/j.1469-7610.2008.01981.x. doi: 10.1111/j.1469-7610.2008.01981.x. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40:57–87. [PubMed] [Google Scholar]
- Archer J, Coyne SM. An integrated review of indirect, relational, and social aggression. Personality and Social Psychology Review. 2005;9:212–230. doi: 10.1207/s15327957pspr0903_2. [DOI] [PubMed] [Google Scholar]
- Baker LA, Raine A, Liu JH, Jacobson KC. Differential genetic and environmental influences on reactive and proactive aggression in children. Journal of Abnormal Child Psychology. 2008;36:1265–1278. doi: 10.1007/s10802-008-9249-1. doi: 10.1007/s10802-008-9249-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker ED, Larsson H, Viding E, Maughan B, Rijsdijk F, Fontaine N, Plomin R. Common genetic but specific environmental influences for aggressive and deceitful behaviors in preadolescent males. Journal of Psychopathology and Behavioral Assessment. 2009;31:299–308. doi: 10.1007/s10862-009-9132-6. [Google Scholar]
- Barker ED, Oliver BR, Maughan B. Co-occurring problems of early onset persistent, childhood limited, and adolescent onset conduct problem youth. [Article]. Journal of Child Psychology and Psychiatry. 2010;51:1217–1226. doi: 10.1111/j.1469-7610.2010.02240.x. doi: 10.1111/j.1469-7610.2010.02240.x. [DOI] [PubMed] [Google Scholar]
- Barker ED, Seguin JR, White HR, Bates ME, Lacourse E, Carbonneau R, Tremblay RE. Developmental trajectories of male physical violence and theft - Relations to neurocognitive performance. Archives of General Psychiatry. 2007;64:592–599. doi: 10.1001/archpsyc.64.5.592. doi: 10.1001/archpsyc.64.5.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker ED, Tremblay RE, van Lier PAC, Vitaro F, Nagin DS, Assaad JM, Seguin JR. The neurocognition of conduct disorder behaviors: Specificity to physical aggression and theft after controlling for ADHD symptoms. Aggressive Behavior. 2011;37:63–72. doi: 10.1002/ab.20373. doi: 10.1002/ab.20373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JJ, Canino G, Polanczyk G, Rohde LA. ADHD across cultures: Is there evidence for a bidimensional organization of symptoms? Journal of Clinical Child and Adolescent Psychology. 2010;39:362–372. doi: 10.1080/15374411003691743. doi: 10.1080/15374411003691743. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Hinshaw SP, Pang KL. Comorbidity of attention-deficit/hyperactivity disorder and early-onset conduct disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology-Science and Practice. 2010;17:327–336. doi: 10.1111/j.1468-2850.2010.01224.x. [Google Scholar]
- Beyers JM, Loeber R. Untangling developmental relations between depressed mood and delinquency in male adolescents. [Article]. Journal of Abnormal Child Psychology. 2003;31:247–266. doi: 10.1023/a:1023225428957. [DOI] [PubMed] [Google Scholar]
- Biederman J, Newcorn J, Sprich S. Comorbidity of attention-deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. American Journal of Psychiatry. 1991;148:564–577. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Risk factors for conduct disorder and oppositional/defiant disorder: Evidence from a New Zealand birth cohort. [Article]. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1125–1133. doi: 10.1016/j.jaac.2010.08.005. doi: 10.1016/j.jaac.2010.08.005. [DOI] [PubMed] [Google Scholar]
- Brendgen M, Dionne G, Girard A, Boivin M, Vitaro F, Perusse D. Examining genetic and environmental effects on social aggression: A study of 6-year-old twins. Child Development. 2005;76:930–946. doi: 10.1111/j.1467-8624.2005.00887.x. [DOI] [PubMed] [Google Scholar]
- Brendgen M, Vitaro F, Boivin M, Dionne G, Perusse D. Examining genetic and environmental effects on reactive versus proactive aggression. Developmental Psychology. 2006;42:1299–1312. doi: 10.1037/0012-1649.42.6.1299. doi: 10.1037/0012-1649.42.6.1299. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Birmaher B. Oppositional defiant disorder and conduct disorder: A review of the past 10 years, part II. [Review]. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1275–1293. doi: 10.1097/00004583-200211000-00009. doi: 10.1097/01.chi.0000024839.60748.e8. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. [Article]. Journal of Child Psychology and Psychiatry. 2005;46:1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Burke JD, Waldman I, Lahey BB. Predictive validity of childhood oppositional defiant disorder and conduct disorder: Implications for the DSM-V. Journal of Abnormal Psychology. 2010;119:739–751. doi: 10.1037/a0019708. doi: 10.1037/a0019708. [DOI] [PubMed] [Google Scholar]
- Burt SA. Are there meaningful etiological differences within antisocial behavior? Results of a meta-analysis. [Article]. Clinical Psychology Review. 2009;29:163–178. doi: 10.1016/j.cpr.2008.12.004. doi: 10.1016/j.cpr.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Bushman BJ, Anderson CA. Is it time to pull the plug on the hostile versus instrumental aggression dichotomy? Psychological Review. 2001;108(1):273–279. doi: 10.1037/0033-295x.108.1.273. doi: 10.1037//0033-295x.108.1.273. [DOI] [PubMed] [Google Scholar]
- Button TMM, Rhee SH, Hewitt JK, Young SE, Corley RP, Stallings MC. The role of conduct disorder in explaining the comorbidity between alcohol and illicit drug dependence in adolescence. Drug and Alcohol Dependence. 2007;87:46–53. doi: 10.1016/j.drugalcdep.2006.07.012. [DOI] [PubMed] [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys .2. A 2-year follow-up at grade 8. [Article]. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of General Psychiatry. 2009;66:764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosgrove VE, Rhee SH, Gelhorn HL, Boeldt D, Corley RC, Ehringer MA, Hewitt JK. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. [Article]. Journal of Abnormal Child Psychology. 2011;39:109–123. doi: 10.1007/s10802-010-9444-8. doi: 10.1007/s10802-010-9444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crick NR, Zahn-Waxler C. The development of psychopathology in females and males: Current progress and future challenges. [Journal; Peer Reviewed Journal]. Development and Psychopathology. 2003;15:719–742. [PubMed] [Google Scholar]
- Dadds MR, El Masry Y, Wimalaweera S, Guastella AJ. Reduced eye gaze explains “Fear Blindness” in childhood psychopathic traits. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:455–463. doi: 10.1097/CHI.0b013e31816407f1. doi: 10.1097/CHI.0b013e31816407f1. [DOI] [PubMed] [Google Scholar]
- De Brito SA, Hodgins S, McCrory EJP, Mechelli A, Wilke M, Jones AP, Viding E. Structural neuroimaging and the antisocial brain: Main finding and methodological challenges. Criminal Justice and Behavior. 2009;36:1173–1186. doi: 10.1177/0093854809342883. [Google Scholar]
- Dekovic M. Aggressive and nonaggressive antisocial behavior in adolescence. [Article]. Psychological Reports. 2003;93:610–616. doi: 10.2466/pr0.2003.93.2.610. doi: 10.2466/pr0.93.6.610-616. [DOI] [PubMed] [Google Scholar]
- Dick DM, Viken RJ, Kaprio J, Pulkkinen L, Rose RJ. Understanding the covariation among childhood externalizing symptoms: Genetic and environmental influences on conduct disorder, attention deficit hyperactivity disorder, and oppositional defiant disorder symptoms. [Article]. Journal of Abnormal Child Psychology. 2005;33:219–229. doi: 10.1007/s10802-005-1829-8. doi: 10.1007/s10802-005-1829-8. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Coie JD. Social-information-processing factors in reactive and proactive aggression in children's peer groups. Journal of Personality and Social Psychology. 1987;53:1146–1158. doi: 10.1037//0022-3514.53.6.1146. [DOI] [PubMed] [Google Scholar]
- Edelbrock C, Rende R, Plomin R, Thompson LA. A twin study of competence and problem behavior in childhood and early adolescence. [Article]. Journal of Child Psychology and Psychiatry. 1995;36:775–785. doi: 10.1111/j.1469-7610.1995.tb01328.x. doi: 10.1111/j.1469-7610.1995.tb01328.x. [DOI] [PubMed] [Google Scholar]
- Ehringer MA, Rhee SH, Young S, Corley R, Hewitt JK. Genetic and environmental contributions to common psychopathologies of childhood and adolescence: A study of twins and their siblings. [Journal; Peer Reviewed Journal]. Journal of Abnormal Child Psychology. 2006;34:1–17. doi: 10.1007/s10802-005-9000-0. [DOI] [PubMed] [Google Scholar]
- Eley TC, Lichtenstein P, Moffitt TE. A longitudinal behavioral genetic analysis of the etiology of aggressive and nonaggressive antisocial behavior. Development and Psychopathology. 2003;15:383–402. doi: 10.1017/s095457940300021x. [DOI] [PubMed] [Google Scholar]
- Eley TC, Lichtenstein P, Stevenson J. Sex differences in the etiology of aggressive and nonaggressive antisocial behavior: Results from two twin studies. Child Development. 1999;70:155–168. doi: 10.1111/1467-8624.00012. doi: 10.1111/1467-8624.00012. [DOI] [PubMed] [Google Scholar]
- Eme RF. Sex differences in child-onset, life-course-persistent conduct disorder. A review of biological influences. Clinical Psychology Review. 2007;27:607–627. doi: 10.1016/j.cpr.2007.02.001. doi: 10.1016/j.cpr.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Ferdinand RF, Dieleman G, Ormel J, Verhulst FC. Homotypic versus heterotypic continuity of anxiety symptoms in young adolescents: Evidence for distinctions between DSM-IV subtypes. Journal of Abnormal Child Psychology. 2007;35:325–333. doi: 10.1007/s10802-006-9093-0. doi: 10.1007/s10802-006-9093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. [Article]. Journal of Child Psychology and Psychiatry. 2005;46:837–849. doi: 10.1111/j.1469-7610.2004.00387.x. doi: 10.1111/j.1469-7610.2004.00387.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence and later substance use, abuse and dependence: Results of a 25-year longitudinal study. [Article]. Drug and Alcohol Dependence. 2007;88:S14–S26. doi: 10.1016/j.drugalcdep.2006.12.011. doi: 10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- Forsman M, Lichtenstein P, Andershed H, Larsson H. Genetic effects explain the stability of psychopathic personality from mid- to late adolescence. [Article]. Journal of Abnormal Psychology. 2008;117:606–617. doi: 10.1037/0021-843X.117.3.606. doi: 10.1037/0021-843x.117.3.606. [DOI] [PubMed] [Google Scholar]
- Franic S, Middeldorp CM, Dolan CV, Ligthart L, Boomsma DI. Childhood and adolescent anxiety and depression: Beyond heritability. [Review]. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:820–829. doi: 10.1016/j.jaac.2010.05.013. doi: 10.1016/j.jaac.2010.05.013. [DOI] [PubMed] [Google Scholar]
- Frick PJ. Extending the construct of psychopathy to youth: Implications for understanding, diagnosing, and treating antisocial children and adolescents. Canadian Journal of Psychiatry-Revue Canadienne De Psychiatrie. 2009;54(12):803–812. doi: 10.1177/070674370905401203. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Lahey BB, Applegate B, Kerdyck L, Ollendick T, Hynd GW, Waldman I. DSM-IV field trials for the disruptive behavior disorders: Symptom utility estimates. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:529–539. doi: 10.1097/00004583-199405000-00011. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Lahey BB, Loeber R, Stouthamer-Loeber M, Christ MAG, Hanson K. Familial risk factors to oppositional defiant disorder and conduct disorder: Parental psychopathology and maternal parenting. [Article]. Journal of Consulting and Clinical Psychology. 1992;60:49–55. doi: 10.1037//0022-006x.60.1.49. doi: 10.1037/0022-006x.60.1.49. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Lahey BB, Loeber R, Tannenbaum L, Vanhorn Y, Christ MAG, Hanson K. Oppositional defiant disorder and conduct disorder: A meta-analytic review of factor analyses and cross-validation in a clinic sample. Clinical Psychology Review. 1993;13:319–340. [Google Scholar]
- Frick PJ, Viding E. Antisocial behavior from a developmental psychopathology perspective. Development and Psychopathology. 2009;21:1111–1131. doi: 10.1017/S0954579409990071. doi: 10.1017/s0954579409990071. [DOI] [PubMed] [Google Scholar]
- Frick PJ, White SF. Research Review: The importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. Journal of Child Psychology and Psychiatry. 2008;49:359–375. doi: 10.1111/j.1469-7610.2007.01862.x. doi: 10.1111/j.1469-7610.2007.01862.x. [DOI] [PubMed] [Google Scholar]
- Gelhorn H, Stallings M, Young S, Corley R, Rhee SH, Hopfer C, Hewitt J. Common and specific genetic influences on aggressive and nonaggressive conduct disorder domains. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:570–577. doi: 10.1097/01.chi.0000198596.76443.b0. doi: 10.1097/01.chi.0000198596.76443.b0. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Hedeker DR. Full-Information Item bifactor analysis. [Article]. Psychometrika. 1992;57:423–436. [Google Scholar]
- Gomez R, Burns GL, Walsh JA, de Moura MA. A multitrait-multisource confirmatory factor analytic approach to the construct validity of ADHD rating scales. Psychological Assessment. 2003;15:3–16. doi: 10.1037/1040-3590.15.1.3. doi: 10.1037/1040-3590.15.1.3. [DOI] [PubMed] [Google Scholar]
- Hartman CA, Hox J, Mellenbergh GJ, Boyle MH, Offord DR, Racine Y, Sergeant JA. DSM-IV internal construct validity: When a taxonomy meets data. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2001;42:817–836. doi: 10.1111/1469-7610.00778. [DOI] [PubMed] [Google Scholar]
- Hartung CM, Lefler EK, Tempel AB, Armendariz ML, Sigel BA, Little CS. Halo effects in ratings of ADHD and ODD: Identification of susceptible symptoms. [Article]. Journal of Psychopathology and Behavioral Assessment. 2010;32:128–137. doi: 10.1007/s10862-009-9135-3. [Google Scholar]
- Higa-McMillan CK, Smith RL, Chorpita BF, Hayashi K. Common and unique factors associated with DSM-IV-TR internalizing disorders in children. Journal of Abnormal Child Psychology. 2008;36:1279–1288. doi: 10.1007/s10802-008-9250-8. doi: 10.1007/s10802-008-9250-8. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Lahey BB, Hart EL. Issues of taxonomy and comorbidity in the development of conduct disorder. Development and Psychopathology. 1993;5:31–50. [Google Scholar]
- Keenan K, Coyne C, Lahey BB. Should relational aggression be included in DSM-V? [Article]. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:86–93. doi: 10.1097/chi.0b013e31815a56b8. doi: 10.1097/chi.0b013e31815a56b8. [DOI] [PubMed] [Google Scholar]
- Keenan K, Feng X, Hipwell A, Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry. 2009;50:1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Loeber R, Green S. Conduct disorder in girls: A review of the literature. [Journal; Peer Reviewed Journal]. Clinical Child and Family Psychology Review. 1999;2:3–19. doi: 10.1023/a:1021811307364. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw DS. Starting at the beginning: Exploring the etiology of antisocial behavior in the first years of life. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of conduct disorder and juvenile delinquency. Guilford Press Guilford Press; New York, NY: 2003. pp. 153–181. [Google Scholar]
- Keenan K, Wroblewski K, Hipwell A, Loeber R, Stouthamer-Loeber M. Age of onset, symptom threshold, and expansion of the nosology of conduct disorder for girls. [Article]. Journal of Abnormal Psychology. 2011;119:689–698. doi: 10.1037/a0019346. doi: 10.1037/a0019346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempes M, Matthys W, de Vries H, van Engeland H. Reactive and proactive aggression in children - A review of theory, findings and the relevance for child and adolescent psychiatry. European Child & Adolescent Psychiatry. 2005;14:11–19. doi: 10.1007/s00787-005-0432-4. doi: 10.1007/s00787-005-0432-4. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GU, Roysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and axis II disorders. American Journal of Psychiatry. 2011;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Ustun TB. Development of lifetime comorbidity in the World Health Organization world mental health surveys. [Article]. Archives of General Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovas Y, Plomin R. Learning abilities and disabilities: Generalist genes, specialist environments. Current Directions in Psychological Science. 2007;16:284–288. doi: 10.1111/j.1467-8721.2007.00521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. The higher-order structure of common DSM mental disorders: internalization, externalization, and their connections to personality. Personality and Individual Differences. 2001;30:1245–1259. [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology. 2006a;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Understanding psychopathology: Melding behavior genetics, personality, and quantitative psychology to develop an empirically based model. Current Directions in Psychological Science. 2006b;15:113–117. doi: 10.1111/j.0963-7214.2006.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB. Oppositional defiant disorder, conduct disorder, and juvenile delinquency. In: Beauchaine T, Hinshaw SP, editors. Child and adolescent psychopathology. Wiley; New York: 2008. pp. 335–369. [Google Scholar]
- Lahey BB, Applegate B, Barkley RA, Garfinkel B, McBurnett K, Kerdyk L, Shaffer D. DSM-IV field trials for oppositional defiant disorder and conduct disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1163–1171. doi: 10.1176/ajp.151.8.1163. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Chronis AM, Jones HA, Williams SH, Loney J, Waldman ID. Psychometric characteristics of a measure of emotional dispositions developed to test a developmental propensity model of conduct disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:794–807. doi: 10.1080/15374410802359635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Applegate B, Hakes JK, Zald DH, Hariri AR, Rathouz PJ. A general factor of liability to prevalent forms of psychopathology during adulthood. 2011. Unpublished manuscript. [DOI] [PMC free article] [PubMed]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lahey BB, D'Onofrio BM. All in the family: Comparing siblings to test causal hypotheses regarding environmental influences on behavior. Current Directions in Psychological Science. 2010;19:319–323. doi: 10.1177/0963721410383977. doi: 10.1177/0963721410383977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, D'Onofrio BM, Waldman ID. Using epidemiologic methods to test hypotheses regarding causal influences on child and adolescent mental disorders. Journal of Child Psychology and Psychiatry. 2009;50:53–62. doi: 10.1111/j.1469-7610.2008.01980.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Goodman SH, Waldman ID, Bird H, Canino G, Jensen P, Applegate B. Relation of age of onset to the type and severity of child and adolescent conduct problems. Journal of Abnormal Child Psychology. 1999;27:247–260. doi: 10.1023/a:1022661224769. doi: 10.1023/a:1022661224769. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke J, Rathouz PJ, McBurnett K. Waxing and waning in concert: Dynamic comorbidity of conduct disorder with other disruptive and emotional problems over 17 years among clinic-referred boys. [Journal; Peer Reviewed Journal]. Journal of Abnormal Psychology. 2002;111(4):556–567. doi: 10.1037//0021-843x.111.4.556. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke JD, Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. Journal of Consulting and Clinical Psychology. 2005;73:389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Hart EL, Frick PJ, Applegate B, Zhang QW, Russo MF. 4-Year longitudinal study of conduct disorder in boys: Patterns and predictors of persistence. [Article]. Journal of Abnormal Psychology. 1995a;104:83–93. doi: 10.1037/0021-843X.104.1.83. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Hart EL, Frick PJ, Applegate B, Zhang QW, Russo MF. Four-year longitudinal study of conduct disorder in boys: Patterns and predictors of persistence. Journal of Abnormal Psychology. 1995b;104:83–93. doi: 10.1037/0021-843X.104.1.83. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Quay HC, Applegate B, Shaffer D, Waldman I, Bird HR. Validity of DSM-IV subtypes of conduct disorder based on age of onset. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:435–442. doi: 10.1097/00004583-199804000-00022. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Kipp H, Ehrhardt A, Lee SS, Massetti G. Three-year predictive validity of DSM-IV attention deficit/hyperactivity disorder in children diagnosed at 4-6 years of age. American Journal of Psychiatry. 2004;161:2014–2020. doi: 10.1176/appi.ajp.161.11.2014. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Stein MA, Loney J, Trapani C, Nugent K, Baumann B. Validity of DSM-IV attention-deficit/hyperactivity disorder for younger children. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:695–702. doi: 10.1097/00004583-199807000-00008. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Hulle CV, Garriock HA, Urbano RC, Waldman ID. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Applegate B, Tackett JL, Waldman ID. Psychometrics of a self-report version of the child and adolescent dispositions scale. Journal of Clinical Child and Adolescent Psychology. 2010;39:351–361. doi: 10.1080/15374411003691784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Schwab-Stone M, Goodman SH, Waldman ID, Canino G, Rathouz PJ, Jensen PS. Age and gender differences in oppositional behavior and conduct problems: A cross-sectional household study of middle childhood and adolescence. Journal of Abnormal Psychology. 2000;109:488–503. [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68:181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Waldman ID, Rodgers JL, D'Onofrio BM, Pedlow S, Keenan K. Testing descriptive hypotheses regarding sex differences in the development of conduct problems and delinquency. Journal of Abnormal Child Psychology. 2006;34:737–755. doi: 10.1007/s10802-006-9064-5. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID. A developmental propensity model of the origins of conduct problems during childhood and adolescence. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of conduct disorder and juvenile delinquency. Guilford Press Guilford Press; New York, NY: 2003. pp. 76–117. [Google Scholar]
- Lahey BB, Waldman ID. A developmental model of the propensity to offend during childhood and adolescence. In: Farrington DP, editor. Advances in criminological theory. Vol. 13. Transaction Publishers; Piscataway, NJ: 2005. pp. 15–50. [Google Scholar]
- Ligthart L, Bartels M, Hoekstra RA, Hudziak JJ, Boomsma DI. Genetic contributions to subtypes of aggression. Twin Research and Human Genetics. 2005;8:483–491. doi: 10.1375/183242705774310169. [DOI] [PubMed] [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behavior and mental health problems: Explanatory factors in childhood and adolescence. Lawrence Erlbaum Associates Publishers Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 1998. [Google Scholar]
- Loeber R, Green SM, Keenan K, Lahey BB. Which boys will fare worse? Early predictors of the onset of conduct disorder in a six-year longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:499–509. [PubMed] [Google Scholar]
- Marsh AA, Finger EC, Mitchell DGV, Reid ME, Sims C, Kosson DS, Blair RJR. Reduced amygdala response to fearful expressions in children and adolescents with callous-unemotional traits and disruptive behavior disorders. American Journal of Psychiatry. 2008;165:712–720. doi: 10.1176/appi.ajp.2007.07071145. doi: 10.1176/appi.ajp.2007.07071145. [DOI] [PubMed] [Google Scholar]
- Martel MM, Gremillion M, Roberts B, von Eye A, Nigg JT. The structure of childhood disruptive behaviors. [Article]. Psychological Assessment. 2010;22:816–826. doi: 10.1037/a0020975. doi: 10.1037/a0020975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Roisman GI, Long JD, Burt KB, Obradovic J, Riley JR, Tellegen A. Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. [Article]. Developmental Psychology. 2005;41:733–746. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: Developmental epidemiology. [Article]. Journal of Child Psychology and Psychiatry. 2004;45:609–621. doi: 10.1111/j.1469-7610.2004.00250.x. [DOI] [PubMed] [Google Scholar]
- McCabe KM, Hough R, Wood PA, Yeh M. Childhood and adolescent onset conduct disorder: A test of the developmental taxonomy. Journal of Abnormal Child Psychology. 2001;29:305–316. doi: 10.1023/a:1010357812278. [DOI] [PubMed] [Google Scholar]
- McMahon RJ, Witkiewitz K, Kotler JS. Predictive validity of callous-unemotional traits measured in early adolescence with respect to multiple antisocial outcomes. [Article]. Journal of Abnormal Psychology. 2010;119:752–763. doi: 10.1037/a0020796. doi: 10.1037/a0020796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: A developmental taxonomy. [Journal; Peer Reviewed Journal]. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moffitt TE. Life-course-persistent and adolescence-limited antisocial behavior: A 10-year research review and a research agenda. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of conduct disorder and juvenile delinquency. Guilford Press Guilford Press; New York, NY: 2003. pp. 49–75. [Google Scholar]
- Moffitt TE. Life-course persistent and adolescence-limited antisocial behavior. In: Cicchetti D, Cohen D, editors. Developmental Psychopathology. 2nd Edition Wiley; New York: 2006. pp. 570–598. [Google Scholar]
- Moffitt TE, Arseneault L, Jaffee SR, Kim-Cohen J, Koenen KC, Odgers CL, Viding E. Research Review: DSM-V conduct disorder: research needs for an evidence base. [Review]. Journal of Child Psychology and Psychiatry. 2008;49:3–33. doi: 10.1111/j.1469-7610.2007.01823.x. doi: 10.1111/j.1469-7610.2007.01823.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Dickson N, Silva PA, Stanton W. Childhood-onset versus adolescent-onset antisocial conduct problems in males: Natural history from ages 3 to 18 years. [Journal; Peer Reviewed Journal]. Development and Psychopathology. 1996;8:399–424. [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva PA. Sex differences in antisocial behaviour: Conduct disorder, delinquency, and violence in the Dunedin Longitudinal Study. Cambridge University Press; New York: 2001. [Google Scholar]
- Nadder TS, Rutter M, Silberg JL, Maes HH, Eaves LJ. Genetic effects on the variation and covariation of attention deficit-hyperactivity disorder (ADHD) and oppositional-defiant disorder/conduct disorder (ODD/CD) symptomatologies across informant and occasion of measurement. [Article]. Psychological Medicine. 2002;32:39–53. doi: 10.1017/s0033291701004792. [DOI] [PubMed] [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Kluwer Academic; Boston: 1992. [Google Scholar]
- Odgers CL, Moffitt TE, Broadbent JM, Dickson N, Hancox RJ, Harrington H, Caspi A. Female and male antisocial trajectories: From childhood origins to adult outcomes. Development and Psychopathology. 2008;20:673–716. doi: 10.1017/S0954579408000333. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14:150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Orderly change in a stable world: The antisocial trait as a chimera. [Article]. Journal of Consulting and Clinical Psychology. 1993;61:911–919. doi: 10.1037//0022-006x.61.6.911. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Capaldi DM. A mediational model for boys’ depressed mood. In: Rolf JE, editor. Risk and protective factors in the development of psychopathology. Cambridge University Press; New York: 1990. pp. 141–163. [Google Scholar]
- Patterson GR, Stoolmiller M. Replications of a dual failure model for boys depressed mood. [Article]. Journal of Consulting and Clinical Psychology. 1991;59:491–498. doi: 10.1037//0022-006x.59.4.491. [DOI] [PubMed] [Google Scholar]
- Petty CR, Monuteaux MC, Mick E, Hughes S, Small J, Faraone SV, Biederman J. Parsing the familiality of oppositional defiant disorder from that of conduct disorder: A familial risk analysis. [Article]. Journal of Psychiatric Research. 2009;43:345–352. doi: 10.1016/j.jpsychires.2008.03.010. doi: 10.1016/j.jpsychires.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quay HC, Peterson DR. Behavior problem checklist. University of Illinois; Champaign, IL: 1967. [Google Scholar]
- Raine A, Dodge K, Loeber R, Gatzke-Kopp L, Lynam D, Reynolds C, Liu JH. The reactive-proactive aggression questionnaire: Differential correlates of reactive and proactive aggression in adolescent boys. Aggressive Behavior. 2006;32:159–171. doi: 10.1002/ab.20115. doi: 10.1002/ab.20115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reef J, van Meurs I, Verhulst FC, van der Ende J. Children's problems predict adults’ DSM-IV disorders across 24 years. [Article]. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1117–1124. doi: 10.1016/j.jaac.2010.08.002. doi: 10.1016/j.jaac.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Rhee SH, Waldman ID. Genetic and environmental influences on antisocial behavior: A meta-analysis of twin and adoption studies. [Journal; Peer Reviewed Journal]. Psychological Bulletin. 2002;128:490–529. [PubMed] [Google Scholar]
- Rijsdijk FV, Sham PC. Analytic approaches to twin data using structural equation models. Briefings in Bioinformatics. 2002;3:119–133. doi: 10.1093/bib/3.2.119. [DOI] [PubMed] [Google Scholar]
- Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. [Article]. Journal of Abnormal Psychology. 2010;119:726–738. doi: 10.1037/a0020798. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe R, Maughan B, Costello EJ, Angold A. Defining oppositional defiant disorder. [Article]. Journal of Child Psychology and Psychiatry. 2005;46:1309–1316. doi: 10.1111/j.1469-7610.2005.01420.x. doi: 10.1111/j.1469-7610.2005.01420.x. [DOI] [PubMed] [Google Scholar]
- Rutter M. Commentary: Revisiting the dismissal of shared environmental influences as argued by Burt et al. (2011). Journal of Child Psychology and Psychiatry. 2011 doi: 10.1111/j.1469-7610.2011.02402.x. Published online 25 March 2011. [DOI] [PubMed] [Google Scholar]
- Rutter M, Caspi A, Moffitt TE. Using sex differences in psychopathology to study causal mechanisms: Unifying issues and research strategies. Journal of Child Psychology and Psychiatry. 2003;44:1092–1115. doi: 10.1111/1469-7610.00194. [DOI] [PubMed] [Google Scholar]
- Rutter M, Kim-Cohen J, Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry. 2006;47:276–295. doi: 10.1111/j.1469-7610.2006.01614.x. [DOI] [PubMed] [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Houghton Mifflin; Boston: 2002. [Google Scholar]
- Singh AL, Waldman ID. The etiology of associations between negative emotionality and childhood externalizing disorders. Journal of Abnormal Psychology. 2010;119:376–388. doi: 10.1037/a0019342. doi: 10.1037/a0019342. [DOI] [PubMed] [Google Scholar]
- Subbarao A, Rhee SH, Young SE, Ehringer MA, Corley RP, Hewitt JK. Common genetic and environmental influences on major depressive disorder and conduct disorder. Journal of Abnormal Child Psychology. 2008;36:433–444. doi: 10.1007/s10802-007-9189-1. doi: 10.1007/s10802-007-9189-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett JL, Krueger RF, Iacono WG, McGue M. Symptom-based subfactors of DSM-defined conduct disorder: Evidence for etiologic distinctions. Journal of Abnormal Psychology. 2005;114:483–487. doi: 10.1037/0021-843X.114.3.483. doi: 10.1037/0021-843x.114.3.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timmermans M, van Lier PAC, Koot HM. The role of stressful events in the development of behavioural and emotional problems from early childhood to late adolescence. Psychological Medicine. 2010;40:1659–1668. doi: 10.1017/S0033291709992091. doi: 10.1017/s0033291709992091. [DOI] [PubMed] [Google Scholar]
- Tuvblad C, Zheng M, Raine A, Baker LA. A common genetic factor explains the covariation among ADHD ODD and CD symptoms in 9-10 year oldboys and girls. [Article]. Journal of Abnormal Child Psychology. 2009;37:153–167. doi: 10.1007/s10802-008-9278-9. doi: 10.1007/s10802-008-9278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hulle CA, Rodgers JL, D'Onofrio BM, Waldman ID, Lahey BB. Sex differences in the causes of self-reported adolescent delinquency. Journal of Abnormal Psychology. 2007;116:236–248. doi: 10.1037/0021-843X.116.2.236. [DOI] [PubMed] [Google Scholar]
- Viding E, Blair RJR, Moffitt TE, Plomin R. Evidence for substantial genetic risk for psychopathy in 7-year-olds. [Article]. Journal of Child Psychology and Psychiatry. 2005;46:592–597. doi: 10.1111/j.1469-7610.2004.00393.x. doi: 10.1111/j.1469-7610.2004.00393.x. [DOI] [PubMed] [Google Scholar]
- Viding E, Frick PJ, Plomin R. Aetiology of the relationship between callous-unemotional traits and conduct problems in childhood. British Journal of Psychiatry. 2007;190:S33–S38. doi: 10.1192/bjp.190.5.s33. doi: 10.1192/bjp.190.5.s33. [DOI] [PubMed] [Google Scholar]
- Viding E, Jones AP, Frick PJ, Moffitt TE, Plomin R. Heritability of antisocial behaviour at 9: do callous-unemotional traits matter? Developmental Science. 2008;11:17–22. doi: 10.1111/j.1467-7687.2007.00648.x. doi: 10.1111/j.1467-7687.2007.00648.x. [DOI] [PubMed] [Google Scholar]
- Waldman ID, Rhee SH, Levy F, Hay DA. Causes of the overlap among symptoms of ADHD, oppositional defiant disorder, and conduct disorder. In: Levy F, Hay DA, editors. Attention, genes, and ADHD. Brunner-Routledge; New York: 2001. pp. 115–138. [Google Scholar]
- Waldman ID, Tackett JL, Van Hulle CA, Applegate B, Pardini D, Frick PJ, Lahey BB. Child and adolescent conduct disorder substantially shares genetic influences with three socioemotional dispositions. Journal of Abnormal Psychology. 2011;120:57–70. doi: 10.1037/a0021351. doi: 10.1037/a0021351. [DOI] [PubMed] [Google Scholar]
- Watson D, O'Hara MW, Stuart S. Hierarchical structures of affect and psychopathology and their implications for the classification of emotional disorders. [Article]. Depression and Anxiety. 2008;25:282–288. doi: 10.1002/da.20496. doi: 10.1002/da.20496. [DOI] [PubMed] [Google Scholar]
- West SG. Alternatives to randomized experiments. [Article]. Current Directions in Psychological Science. 2009;18:299–304. [Google Scholar]
- West SG, Thoemmes F. Campbell's and Rubin's perspectives on causal inference. [Article]. Psychological Methods. 2010;15:18–37. doi: 10.1037/a0015917. doi: 10.1037/a0015917. [DOI] [PubMed] [Google Scholar]
- WHO . Classification of Mental and Behavioural Disorders: Research Diagnostic Criteria. 10th ed. World Health Organization; Genva: 1992. [Google Scholar]


