Abstract
Objective
To determine how often patients diagnosed with bulimia nervosa (BN) surpass their highest pre-morbid weight during the course of their disorder.
Method
The weight histories of individuals with BN were determined using retrospective weight data (Study 1) and combined retrospective/prospective data (Study 2).
Results
Retrospective analyses indicated that 59.0% (n = 46) and 61.8% (n = 110), respectively, reported that their highest weight was reached after developing BN. In Study 2, 35.3% of participants superseded their highest pre-enrollment weights during 8 years of follow-up, and 71.6% reached a post-morbid highest weight before remission. Across studies, the primary difference between patients who did and did not reach their highest weight post-morbidly was that those who did had an earlier age of onset and longer duration of BN.
Discussion
Findings are discussed in terms of possible links between BN and weight-gain proneness, weight fluctuation across the course of BN, and implications for treating BN.
Keywords: bulimia nervosa, weight gain, weight suppression
In Russell’s initial characterization of bulimia nervosa (BN), he suggested that while the body weights of patients with this eating disorder are typically “unremarkable” when they present for treatment, they are usually significantly below their highest pre-morbid weights (1). Indeed, those with BN have usually lost so much weight in the past that about one-third to one-half have a history of anorexia nervosa (2). Aside from this distinction, most researchers and clinicians have paid little attention to the fact that at presentation most BN individuals are further below their highest previous body weights than are non-eating disordered individuals of the same age (3). This may be because these patients’ weights are usually neither low enough to create the physiological or psychological consequences associated with an abnormally low body weight nor high enough to elicit concerns about the possible medical and psychological consequences of overweight.
Similarly, in the effort to explain why only a small fraction of young women concerned about their bodies develop problems related to BN (4), potential weight-related predispositions have been overlooked relative to psychological predispositions (e.g., low self-esteem, poor body image, etc.). However, it is possible that a susceptibility toward excessive weight gain puts certain young women at greater risk for developing BN. Evidence suggests that women who develop BN have higher relative weights pre-morbidly than their same aged peers and are more likely to have one or both parents who are obese (5). Studies examining appetitive indicators in patients with bulimia have also shown an exaggerated appetitive response to food stimuli relative to healthy controls (i.e. 6, 7,8).
The fact that individuals with BN are often in the normal weight range but have a history of overweight indicates that at presentation they weigh considerably less than their highest weight (9,10). Lowe (11) called the discrepancy between one’s highest ever and current weight “weight suppression” and research indicates that those with BN have elevated weight suppression relative to their non-bulimic peers (3). Recent research has shown that weight suppression level in those with BN predicts frequency of binge eating and purging (3,12), amount of weight gain over a period of several months (13,14) and over 5 years (15), and poorer outcome in CBT (3). Furthermore, recent research (16) found that weight suppression level predicted the probability of developing a BN-spectrum disorder over 10 years among young women initially without this disorder.
Our research on weight suppression has always assumed that the historical highest weights of those with BN were reached before their eating disorder began (e.g. 13). Bulimic patients typically lose a significant amount of weight in the process of developing their disorder (9,10) and then engage in extreme weight control behaviors to avoid weight gain. Nonetheless, as we began to ask individuals with BN about their weight history, we were surprised to learn that some individuals reported reaching their highest weight after their disorder developed. Because there is evidence that the pre-morbid body weights of those with BN are already elevated (9), such evidence would suggest that BN individuals are even more prone toward weight gain than current models of BN generally assume. In this regard it is interesting to note that the eating disorder of BN was first identified (1)at about the same time the prevalence of obesity in the United States started accelerating (around 1980; 17).
Determining the percent of individuals with BN who reached their highest past weight pre-versus post-morbidly is important for several reasons. First, because those with BN already have higher relative weights than their same-age peers before developing their disorder (5), if some reach even higher weights following onset it would strengthen the possibility that individuals with BN have a predisposition toward overweight or obesity. Second, since most of those with BN reach very low body weights during their disorder, such a finding would indicate that the degree of weight fluctuation experienced by those with BN is even larger than previously suspected. Third, if during their disorder some patients with BN reach a higher weight than their highest pre-morbid weight, it would suggest that bulimic behavior patterns (i.e., restricting, bingeing, purging) might contribute to post-morbid weight gains. Fourth, the notion that individual BN patients have the potential to not only lose but to gain a great deal of weight could suggest a reinterpretation of a core feature of BN which has variously been referred to as a “morbid fear of fatness,” and a“ persistent over-concern with body shape and weight,” (see 18). If many patients with BN have a history of being overweight at some point during (not just prior to) the development of their disorder, then patients’ persistent fears of weight gain might be viewed in part as a realistic concern based on their own weight history. Finally, and perhaps most significantly, if the weight fluctuations experienced by individuals with BN are larger than previously suspected, this information may be important in shaping the goals of treatment. In particular, a patient’s body weight, both in absolute terms and in relation to their highest previous body weight, could influence the interpretation of a patient’s weight and shape concerns and also suggest that weight changes during and after treatment should become an explicit topic of discussion in therapy.
The purpose of this paper was therefore to determine what percentage of individuals with BN report their highest weight after as opposed to before the onset of their disorder, as well as to determine how much weight those who supersede their previous highest weight gain during their disorder. Additionally, we attempted to confirm whether previous evidence indicating elevated pre-morbid weights relative to same-aged peers (5) could be replicated in our samples. Finally we compared sub-groups of individuals with BN who reported reaching their highest previous weight before or after onset of their disorder on various measures of eating disorder psychopathology to determine if the timing of reaching one’s highest weight is related to severity of eating disorder symptoms.
We analyzed two data sets to explore these questions. One was derived from a treatment study conducted among patients with BN enrolled in an intensive outpatient program. The other was derived from a longitudinal study of BN that has followed a group of individuals with that disorder over a 10-year period (19). This latter data set allowed us to explore these questions not only retrospectively (i.e., looking backward from the time participants enrolled in the study) but also prospectively to determine what percentage of individuals with BN subsequently gained enough weight to supersede their pre-enrollment highest body weight.
Study 1
Method
Data used for this study were collected as part of a two-year treatment outcome study that compared the results of cognitive-behavioral therapy to treatment as usual at a local eating disorder clinic. This study was approved by the Drexel University Institutional Research board, and its main results will be published separately.
Participants
Women seeking intensive outpatient treatment at the Renfrew Center for eating disorders were eligible for this study if they completed an intake assessment for the parent study (n = 210) and received a bulimia spectrum diagnosis (37.1%, n = 78), defined as meeting full criteria for BN according to DSM-IV or meeting all criteria except that the binge eating and compensatory behavior occurred only once a week or for a duration of less than three months. Average age for the bulimic sample was 21.9 years (SD = 5.6) and the majority (95%) were Caucasian.
Measures
Participants were interviewed at intake by researchers trained in the SCID to determine diagnostic status and completed self-report measures. The main variables reported in this study were current and highest historical weight since reaching adult height. Age of onset for BN was also obtained using the SCID. To try to determine if differences in weight history were related to eating disorder specific psychopathology, we examined the Eating Disorder Examination (EDE, 20), the Bulimia, Body Dissatisfaction and Drive for Thinness subscales from the Eating Disorder Inventory (2nd Edition, EDI, 21), Eating Attitudes Test (EAT, 22), Cognitive Restraint Scale of the Three Factor Eating Questionnaire (TFEQ, 23), and Goldfarb Fear of Fat Scale (GFFS, 24).
Dieting and weight history
Participants were interviewed regarding their weight and dieting histories. They were asked to report both the age at which they reached their lowest and highest weights and what they weighed at each of those points. The validity of recalled past weights was supported by a study that found a correlation of .85 between measured body weight at age 25 and recalled weights collected an average of about 20 years later (25).
Current weight and height
Participants weight and height were measured by Renfrew staff using a physician’s scale with a stadiometer. Self-report weight and height were substituted in cases where measured weights could not be obtained (11.5% of cases). Self-report and measured weights were found to be highly correlated (r = .99, p < .001), and the mean difference between these weights was small (M = 1.25 lb, SD = 3.64 or M = 0.57 kg, SD = 1.65), indicating that this substitution was unlikely to affect the validity of our findings.
Eating Pathology
The Eating Disorder Examination (EDE, 20) is a semi-structured interview that assesses the severity of specific eating-related pathology over the 28 days before assessment. It contains a Global scale which is the average of the four subscales: Shape Concern, Weight Concern, Eating Concern, and Restraint. This measure has demonstrated acceptable reliability and validity (26,27). The EDE also was used to measure the number of objective and subjective bulimic episodes, self-induced vomiting episodes, and laxative and diuretic use that participants reported in the previous 28 days.
The Eating Disorder Inventory (2nd Edition, EDI, 21) is a 91-item self-report measure composed of 3 eating disorder symptom related and 8 personality related subscales. This study only administered the three eating disorder scales (Drive for Thinness, Bulimia, and Body Dissatisfaction). Reliability and validity of these subscales have been previously demonstrated (28,29).
The Eating Attitudes Test-26 (EAT, 22) is a 26-item self-report inventory and is a reliable and valid measure of anorexic symptoms and dimensions relevant to BN (30).
The Three Factor Eating Questionnaire (TFEQ, 23) is a psychometrically established self-report measure with three subscales, including Cognitive Restraint (TFEQ-CR). The TFEQ-CR consists of 21 items scored on a 2-point scale (0 or 1). Higher scores on this scale reflect more restrained eating patterns.
The Goldfarb Fear of Fat Scale (GFFS, 24) is a 10-item self-report measure that assesses an individual’s fear of weight gain and becoming fat. The GFFS has good test retest reliability and discriminantvalidity (24).
Statistical methods
Participants were categorized into groups based on whether they reported reaching their highest weight before or after onset of their disorder. These groups were then compared to determine if differences in eating psychopathology could help explain why some participants surpassed their previous highest weight during the course of their disorder while others did not. Across all analyses included in this paper, two-tailed independent samples t-tests were used to compare weight history groups. Adjusted t values were reported for all analyses in which the assumption of homogeneity of variance was violated due to the discrepancy in the sample sizes of these weight history groups (Current BMI, age at highest weight, subjective binges).
Results
The majority of participants (59.0%, n=46) reported reaching their highest weight after onset of BN (High Follows group); 20.5% (n=16) reported reaching their highest weight before onset (High Precedes group). The remaining 20.5% (n=16) reported reaching their highest weight and the onset of their disorder at the same age. Because ages were recorded in whole years, the order of events that occurred at the same age could not be determined. Therefore, these individuals were not assigned to either of the two groups and were excluded from additional analyses.
We next examined the highest pre-morbid BMIs of the High Precedes group relative to norms for non-eating disordered peers of the same average age. The average highest pre-morbid BMI of the High Precedes group was 25.7, and these participants reached this weight at an average of 17.1 years old. By comparison, the average BMI of girls at the 50th percentile of the CDC’s height/weight tables (31) at this age is 20.0, a much lower figure. The difference between these two BMI figures is 5.7 BMI units or about 34 lbs.
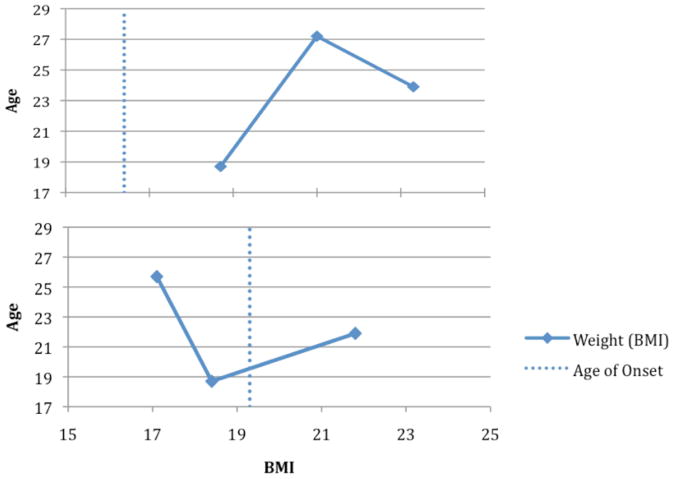
Participants in the High Follows group reported reaching their highest weight 2.9 years later than the High Precedes group (t (60) = 4.07, p < .001), and their age of onset as three years earlier than the High Precedes group (t (60) = 2.86, p = .006). Their average disorder duration was also significantly longer than the High Precedes group (t(57) = 3.95, p < .001). Other differences between the two groups were minimal (see Table 1). Figure 1 illustrates the BMI patterns of the High Follows and High Precedes groups, including age of onset for both groups.
Table 1.
Comparisons Between High Precedes and High Follows Groups
| High Precedes | High Follows | |
|---|---|---|
| Age at onset | 19.4 (2.4) | 16.4 (4.0)** |
| Age at highest weight | 17.1 (1.9) | 21.0 (5.6)** |
| Age at lowest weight | 18.4 (3.2) | 18.7 (3.1) |
| Current age | 21.8 (2.9) | 23.3 (6.7) |
| Duration of disorder | 2.4 (2.2) | 6.9 (6.3)** |
| Highest BMI | 25.7 (2.5) | 27.2 (7.3) |
| Current BMI | 22.0 (1.9) | 23.9 (4.5)* |
| Lowest BMI | 18.7 (2.9) | 18.7 (3.1) |
| Weight suppression (lb) | 22.7 (14.1) | 22.0 (35.5) |
| Weight suppression (kg) | 10.3 (6.4) | 10.0 (16.1) |
p<.05
p<.005
Figure 1.
Weight history in study 1: High Precedes Group (bottom) and High Post Group (top)
No significant group differences were found in the frequency of compensatory behaviors or objective bulimic episodes reported in the past 28 days. Subjective bulimic episodes were significantly more frequent in the High Precedes group (M = 23.9, SD = 31.25) in comparison to the High Follows group (M = 6.6, SD = 11.1, t (58) = 2.10, p = .05). No significant differences were found on any other measures of eating disorder psychopathology, including the EDE global and subscale scores, EAT26, EDI, GFFS, PFS or TFEQ-CR (ps > .16). The largest effect size (using Cohen’s d) for these analyses was .42, indicating that this lack of significant findings was not likely due to the relatively small sample size in the High Precedes group.
Study I Discussion
Through historic weight data reported by participants with BN, we were able to identify two different weight history patterns based on timing of highest weight. The High Precedes group follows the pattern that most weight suppression research has assumed to be universal-that participants reach their highest weight ever pre-morbidly, then undergo a period of significant weight loss, and that while their weight rebounds from this point, it does not surpass their previous highest weight. Surprisingly, however, this pattern only describes a minority of participants (20.5%) in this sample.
In the more common High Follows pattern, participants reached their lowest weight an average of 2.4 years after onset of BN, followed by an average period of 1.6 years during which their BMI rose sharply to reach their highest ever weight1. The average weight gain between these two points was very large (M = 49.6 lb, SD = 36.3 or M = 22.5 kg, SD = 16.5) before participants’ weights begin to decline again into the normal range.
We also found evidence that the High Precedes group’s pre-morbid weights were elevated relative to their same aged peers based on national norms. We did not have data that would allow us to determine what the highest pre-morbid weight was in the High Follows group. Because the lowest weight for this group was objectively quite low (a BMI of about 19) and occurred post-morbidly, it is likely that this group also lost considerable weight in the process of developing their disorder. If this assumption is true, then both the High Precedes and High Follows group would have experienced substantial weight loss while developing their disorder and their weight histories would only differ in whether they superseded their previous highest weight post-morbidly.
Because the High Precedes group was similar in age to the High Follows group yet reported a later age of onset, it is possible that the two groups represent the same pattern at different time points. The High Follows group reached their highest weight an average of 4.6 years after onset, while the High Precedes group only had the disorder for an average of 2.6 years. Thus it is possible that the High Precedes group will also eventually supersede their pre-morbid highest weight. The few differences in eating psychopathology found between the two groups may lend further support to this hypothesis. The availability of a second data set that has followed individuals with BN for over 8 years allowed us to test the replicability of the results of Study I as well as the hypothesis that the most individuals in the High Precedes group will also supersede their highest pre-morbid body weights.
Study 2
Method
Participants
Between 1987 and 1991, the Massachusetts General Hospital Longitudinal Study of Anorexia and Bulimia Nervosa recruited participants from MGH and other Boston-area treatment centers. A sample of 246 participants meeting Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (32)criteria for AN or BN were recruited for the parent study. Participants’ entry eating disorder diagnoses were reclassified according to the new criteria established in the fourth edition of the DSM so that the sample was comprised of 51 women with AN restricting subtype, 85 women with AN binge/purge subtype, and 110 women with BN. Detailed descriptions of the exclusion criteria and sample characteristics have been reported previously (19,33). All participants who received a BN diagnosis at study entry were included in this report.
Procedure
This study was approved by the MGH Institutional Review Board and written informed consent was obtained from all participants. Participants were interviewed in person at intake by trained research assistants. Intake interviewers assessed current and lifetime Axis I disorders, collected data on current and past eating disorder symptomatology, and measured height and weight. During follow-up, participants were interviewed every six months in person when possible, or by telephone. During follow-up, body weights were collected via self-report. See Study 1 for a discussion of the correlation between measured and self-report weights. Remuneration was provided for all interview assessments.
Measures
At intake, a modified version of the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (34), which included a section from the Diagnostic Interview Schedule (35)with criteria for AN and BN, was used to assess current and lifetime diagnoses. The Eating Disorder Inventory (EDI; 21), assessed self-reported current weight, height, highest past weight (phrased to exclude pregnancy), and lowest past weight. Age of onset (month and year) was determined during the intake interview using the EAT-SADS-L. A calibrated stadiometer and balance beam scale were used to obtain current height and weight measurements at intake. See Herzog et al. (19) for a complete description of all measures completed during the intake interview.
During follow-up, participants were interviewed every 6 months with the Longitudinal Interval Follow-up Evaluation—Eating Disorders Version (LIFE-EAT II), a modified version of the LIFE II interview (36). This instrument yielded retrospective weekly psychiatric status rating (PSR) scores for both anorexia nervosa and bulimia nervosa for all participants. Scores range from 0 to 6 based on symptom severity, where 0 – 1 represent no current symptoms, 2 represents residual symptoms (minor eating disorder cognitions without behavioral symptoms), 3–4 represent subthreshold behavioral symptoms, and 5–6 represent meeting full criteria for BN. The PSR scores were used in the present study to determine when subjects reached full remission from BN. Full recovery is defined as the absence of symptoms or the presence of only residual symptoms for at least 8 consecutive weeks (PSR of 1 or 2).
Statistical methods
As described in Study 1, across all analyses two-tailed independent samples t-tests were used to compare weight history groups. Adjusted t values were reported for all analyses in which the assumption of homogeneity of variance was violated (In retrospective analyses: Highest reported BMI; in prospective analyses: Intake BMI, weight suppression).
Results
Retrospective Data
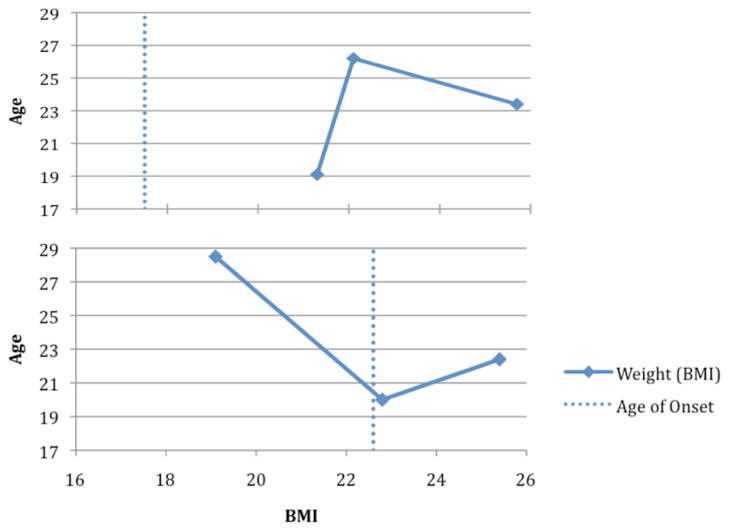
Analyses of intake data were conducted to determine if the retrospective results of Study 1 could be replicated. Participants were categorized into groups at intake based on whether they reported reaching their highest weight before or after onset of their disorder. Similar to study 1, at intake the majority of participants (61.8%, n = 68) reported reaching their highest weight after onset of BN (High Follows group), while 38.2% (n=42) reported reaching their highest weight before onset (High Precedes group). The weight history patterns of these two groups were similar to those reported in study 1. Participants in the High Follows group reported reaching their highest weight three years later than the High Precedes group (t (108) = 2.94, p = .004), and their age of onset as 5.1 years earlier than the High Precedes group (t (108) = 4.89, p < .001). Average duration of disorder for this group was 5.3 years longer than the High Precedes group (t(108) = 5.40, p <.001). Other differences between the two groups were minimal (see Table 2). Figure 2 demonstrates the relative weight patterns of the High Follows and High Precedes groups in study 2, including age of onset for both groups.
Table 2.
Comparisons Between High Precedes and High Follows Groups at Intake
| High Precedes | High Follows | |
|---|---|---|
| Age at onset | 22.6 (5.5) | 17.5 (5.1)** |
| Age at highest weight | 19.1 (4.0) | 22.1 (5.8)** |
| Age at lowest weight | 22.8 (5.3) | 21.3 (5.8) |
| Current age | 25.4 (6.0) | 25.7 (6.8) |
| Duration of disorder | 2.8 (3.4) | 8.2 (6.9)** |
| Highest BMI | 28.5 (7.1) | 26.2 (3.8) |
| Current BMI | 22.4 (2.9) | 23.4 (3.5) |
| Lowest BMI | 20.0 (1.7) | 19.1 (2.0)* |
| Weight suppression (lb) | 37.4 (36.5) | 16.7 (16.4)** |
| Weight suppression (kg) | 17.0 (16.6) | 7.6 (7.4)** |
p<.05
p<.005
Figure 2.
Weight history at intake in study 2: High Precedes Group (bottom) and High Post Group (top)
As we did for Study 1, we also compared the average pre-morbid highest BMI of the High Precedes group (28.5 at the average age of 19.1) with the BMI of 19-year-old girls at the 50th percentile of the CDC height-for-weight charts, which was 20.8 (31). The difference between these two figures was 7.7 BMI units or about 46 lbs.
Prospective data
Because comparisons between participants grouped by weight history again seemed to support the hypothesis that reaching a post-morbid high weight was related to disorder duration, a second set of analyses examined prospectively the percentage of participants who surpassed their previous highest weight during the eight-year follow-up period. A small number of participants (n = 8) had not yet completed follow-up visits through year eight and these individuals were therefore excluded from this analysis. All analyses were repeated including all 110 participants’ highest weights up to year eight or their last recorded follow-up visit, and the pattern of results was similar.
During the eight-year follow-up period, 45.1% (N=46) of the overall sample surpassed their previously recorded highest weight, with an additional 4.9% matching their previous high weight. There were no significant differences between the High Precedes and High Follows groups (as defined by their weight history at intake) in the percentage of participants who surpassed their previous highest weight (χ2 (2, N=102) = 1.61, p = .45) during the follow-up period. In the High Precedes group specifically, 39.5% (n = 15) surpassed their previous high weight with an additional 7.9% matching their previous high weight. When combined with intake data, this indicates that only 19.6% of the overall sample had not equaled or surpassed their previous highest weight at any point after onset of their disorder by the eighth follow-up year. Included in the 80.4% who equaled or surpassed their previous highest weight at some point after onset were some participants who both reported a post-onset highest weight at intake and reached a new highest weight during eight year follow-up period (30.4% of the overall sample).
Because some participants experienced remission from their eating disorder during the eight-year follow-up period, it is possible that some of the highest weights reached during this period occurred after remission from BN. We therefore re-examined these percentages excluding all weights reported after a participant first met study criteria for remission (M = 3.50 years, SD = 3.62). Pregnancy was also considered as a potential confound, however in this data set all pregnancies occurred at least nine months after remission. When post-remission weights are excluded, 36 participants (35.3%) match or exceed their previous high weight during the eight-year follow-up period (regardless of their weight history status at intake). The percentage of participants who do not equal or surpass their previous highest weights at any point before remitting is 28.4% at year eight. The remaining prospective results reported below exclude weights occurring after remission and any differences in analyses with all weights included are reported as footnotes. Table 3 includes information regarding how these different weight history categorizations were obtained.
Table 3.
Flowchart of participants included in Study 2 analyses
| High Before Onset | High After Onset | |||||
|---|---|---|---|---|---|---|
| n (%) | n (%) | |||||
| Categorization at Intake | 42 (38.2%)* | 68 (61.8%)* | ||||
| Surpassed previous HW during follow-up? (All follow-up weights included) | Yes | Match | No | Yes | Match | No |
| 15 (39.5%) | 3 (7.9%) | 20 (52.6%) | 31 (48.4%) | 3 (7.9%) | 31 (48.4%) | |
| Categorization after Follow-up (All follow-up weights included) | 20 (19.6%) | 82 (80.4%) | ||||
| Surpassed previous HW during follow-up? (Pre-remission weights ONLY) | Yes | Match | No | Yes | Match | No |
| 12 (31.6%) | 3 (7.9%) | 23 (60.5%) | 38 (59.4%) | 3 (7.9%) | 38 (59.4%) | |
| Categorization after Follow-up (Pre-remission weights ONLY) | 23 (22.5%)** | 79 (77.5%)** | ||||
Compared in Part 1 of Study 2 analyses.
Compared in Part 2 of Study 2 analyses.
Participants who exceeded a previous highest weight during the course of the eight-year follow-up period weighed an average of 22.5 pounds (SD = 24.3 or M = 10.2 kg, SD = 11.0) more at their new high weight in comparison to their pre-intake highest weight (Median = 12.0 lb or 5.4 kg). This new highest weight represents an average weight gain of 38.2 pounds (SD = 37.5 or M = 17.3 kg, SD = 17.0) from their weight at the time of the intake assessment (Median = 25.0 lb or 11.3 kg). Average weight gain from all participants during the follow-up period (relative to intake weight) was 12.0 pounds (SD = 22.6 or M = 5.4 kg, SD = 10.3; Median = 5.0 lb or 2.3 kg) at their highest reported weight during that period.
We next sought to examine differences between individuals who never reach a post-onset highest weight and those that do (either prior to intake or during the follow-up period). Participants were categorized based on whether or not they reached a post-onset high weight at any point and were compared on intake variables to those who never exceeded their pre-morbid highest weight. Participants who never reach a post-onset highest weight (n = 29) had a significantly lower intake BMI (M = 21.8, SD = 2.0) than the group with a post-onset highest weight (n = 73, M = 23.5, SD = 3.7, t(100) = 2.98, p = .004). These participants showed greater levels of weight suppression at intake (M = 42.2 lb, SD = 39.6 or M = 19.1 kg, SD = 17.9) than the group with a post-onset high weight (M = 17.8 lb, SD = 18.3 or M = 8.1 kg, SD = 8.3, t(100) = 3.18, p = .003). There were no significant differences between these groups in lowest or highest relative weights reported at intake. Age of onset was later in the group with a pre-onset high weight (M = 23.1, SD = 5.2) in comparison to the rest of the sample (M = 18.0, SD = 5.5, t(100) = 4.26, p < .001) and average duration of their disorder was 3.8 years shorter (t(100) = 2.37, p = .02). The majority of participants (79.1%) recovered within the eight year follow-up period. There were no significant differences in highest weight reached during the follow-up period or amount of weight gained during this period between these two groups2.
Study II Discussion
Data from this study replicated findings from study 1 suggesting that the majority of individuals with bulimia nervosa reach their highest weight after onset of their disorder, and extended that finding by examining both retrospective and prospective data. We also replicated the finding from study 1 that participants in the High Precedes group were on average overweight relative to their peers before developing their disorder.
Similarly to Study 1 the High Precedes group underwent a period of weight loss resulting in reaching both their lowest weight and the onset of BN about 3.5 years later. This was followed by a gradual weight regain resulting in the typically normal weights seen when individuals with BN present for treatment or participate in research studies. However, the majority of the sample (61.8%) followed a heretofore unanticipated pattern in which participants reached their lowest weight 3.8 years after onset of BN, followed by a period of less than a year during which their BMI rose sharply to reach its highest point before it again began to decline into the normal range1.
Analyses of the prospective data indicated that nearly half of all participants (45.1%) surpassed their pre-intake highest weight during the eight-year follow-up period (regardless of whether their highest weight at intake occurred before or after onset of BN) and 35.5% did so prior to remission. Only a minority of the sample (28.4%when excluding post-remission) did not reach a post-onset high weight at any point.
However, this does still leave a minority of participants that did not reach a post-onset high weight at any point between onset and the end of the eight-year follow-up. This group was both lower in BMI and higher in weight suppression at intake than those who eventually reached a post-onset high weight. These participants also had a significantly shorter duration of disorder and later age of onset than those who did reach a post-onset high weight.
General Discussion
The results of both of the current studies were consistent with findings suggesting that individuals with BN were higher in body mass than their same-agednon-bulimic peers before developing their disorder. Bulimic individuals in the High Precedes group reported much higher relative weights (an average BMI of about 27 across the two studies) relative to the average BMI level of individuals of the same age (about 20 across studies) and gender. This difference of roughly 7 BMI units translates into a weight difference of about 40 pounds. This difference is not only quite large in physical terms, but is likely to be highly distressing to young women in the late teenage years, when body weight and shape are often emotionally charged issues because of perceived peer and media pressure to be thin as well as concerns about dating and physical attractiveness (37–39). These results suggest that the radical dieting and weight loss that is usually seen early in the development of bulimia occurs not just because susceptible women over-value their weight and shape but because they are significantly heavier than other women their age.
Because individuals with BN typically lose a significant amount of weight in the process of developing their disorder, are phobic about gaining weight, and engage in extreme compensatory behaviors to prevent weight gain from binge eating (40), it stands to reason that bulimic individuals would rarely gain so much weight during their disorder that they would supersede their already-elevated highest pre-morbid body weight. This seems particularly reasonable since most women with BN also reach substantially reduced weights during the course of their disorder and are typically weight suppressed even while in the normal weight range as seen across both of these studies. Yet post-onset highest weights were found in a majority of bulimic women in both data sets we examined.
Retrospective analyses in Study 1 and 2 found that 58.0%to 61.8% of participants experienced their highest weight after onset of BN, while a minority reached their highest weight before the onset of their disorder. The most notable distinction between these two groups was that those who had not surpassed their premorbid highest weight reported a later age of onset (2.9 years and 5.1 years later, respectively), and a shorter disorder duration (4.4 years and 5.3 years, respectively)than those who reached their highest weight during the course of BN.
Because these differences in disorder duration leave open the possibility that those who had not reached a post-onset high weight would also rebound in weight as their disorder progressed, prospective weight data were examined in study 2. These analyses indicated that about half of participants surpass their previous highest weight during the 8-year follow-up period. Nonetheless, a minority (28.4% when post-remission weights are excluded) never surpass their pre-morbid highest weights during the course of their disorder. This group was found to have a later age of onset and shorter duration of disorder than the rest of the sample.
Although we are not able to determine definitively whether these groups represent two distinct courses of weight change across BN, comparisons between the groups seem to indicate more similarities than differences. The groups were not found to differ on any measures of eating pathology other than subjective binge eating in Study 1, and were shown to experience similar amounts of weight fluctuation across the follow-up period in Study 2. The different timing of highest weights in these groups may instead be explained by differences in disorder duration, age of onset, or level of premorbid weight gain (which could not be examined in the current study).
Because the average age of onset in the High Follows group is 16.4.–17.5 years old, it is possible that this group surpasses their premorbid highest weight due to normal post-pubescent weight gain unrelated to the course of the disorder. To examine this possible confound, we used age of onset and disorder duration to predict highest BMI achieved within those who had reached a post-onset high weight using linear regression. In both data sets, disorder duration was significantly predictive of highest weight achieved after controlling for age of onset (Study 1: F = 11.58, p = .002, Study 2: F = 17.20, p < .001). In the Study 1 data set, age of onset was not significantly predictive of highest weight (F = .73, p = .40) however it was predictive in Study 2 (F = 4.04, p = .05). These findings indicate that the length of time that a person experiences BN symptoms is related to weight gain independently of their age when the disorder first began, and thus may provide further evidence that bulimia is related to weight gain beyond that which would be considered age-appropriate.
Although most women without an eating disorder will reach new highest weights as they age (41), there are several reasons why this pattern is striking when seen in individuals with BN. The amount of time and effort that women with BN devote to weight control as well as the extremity of weight control behaviors they engage in exceeds that of most healthy women. Additionally, these individuals are, on average, highly weight suppressed (11.0 kg or 24.2 lb across our studies) and most were even more weight suppressed at the lowest weight they reached during their disorder. Therefore the amount of weight gain bulimic individuals experience during their disorder is much greater than commonly supposed, and is far greater than the typically gradual weight gain pattern seen in most non-bulimic women.
One of the more striking features of the weight history pattern in those who report a post-onset high weight at intake is the relatively short time frame (3.9 years in Study 1 and 3.6 years in Study 2)3 during which these participants experienced a massive weight gain following their lowest weight (41.7 lb or 18.9 kg in Study 1 and 44.8 lb or 20.3 kg in Study 2) which led them to reach their highest reported weight. This represents a weight gain of 15.0 pounds (6.8 kg) per year in Study 1 and 15.6 pounds (7.1 kg) per year in Study 2. On the other hand, the average Caucasian woman gains weight at a rate of 1.2 pounds (.6 kg) per year (41). While weight suppression at patients’ lowest weights may partially account for the speed of post-morbid weight gain, this relationship would not account for why participants would also go on to surpass their highest premorbid weight or for the relationship observed between disorder duration and highest weight achieved. It would be of interest in future research to examine whether there is a higher rate of weight gain per year from participants’ onset weight (not available in the current data set) rather than lowest weight in comparison to healthy controls, and to examine whether the rate of weight change stabilizes after recovery from BN.
The rapid post-morbid weight rebound experienced by these participants after reaching their lowest weight could be due to increased metabolic efficiency resulting from weight loss, to resulting increases in binge eating, or to both influences. This rapid weight regain may also indicate a stronger bio-behavioral predisposition towards overweight in the majority of individuals with BN, which manifests itself in spite of their continual engagement in extreme weight control behaviors. Thus in terms of both the observed elevation of pre-morbid weights in the High Precedes group and observed rates of post-onset weight rebound, the results of this study are consistent with the hypothesis that bulimia nervosa may be linked to a predisposition towards overweight or obesity. Also consistent with this conclusion is a recent study by Thomas et al. (42), who showed that both large weight losses and large weight gains were associated with the onset of a bulimic-spectrum disorder. Of greater relevance to the current results was the finding that both those who underwent a major weight loss and those who underwent a major weight gain were significantly higher in body mass than a weight stable comparison group one and two years following the year in which they lost or gained at least 10% of their body weight.
There are, however, alternate hypotheses that should be considered to explain the post-onset high weights experienced by most patients with bulimia. The post-onset weight gains experienced by these participants could be due to a progressive disregulation of homeostatic appetitive mechanisms as a result of repeated dieting and binging behaviors, or more directly to the ineffectiveness of most purging methods at eliminating the calories consumed during a typical binge. This could potentially indicate that the highest post-morbid weights reported by these participants may not represent a susceptibility to becoming overweight, but rather an artificially inflated weight that these participants might not have reached without engaging in disorder-related behaviors.
In addition to providing further evidence regarding a possible link between BN and weight-gain proneness, these findings have several possible applications for the conceptualization and treatment of BN. The patterns displayed here indicate that the extreme fear of weight gain endorsed by most patients with bulimia may in part be product of their actual past experience with rapid weight gain and/or prior elevations in their weight. This may impact the ability to dispel this fear with techniques such as cognitive restructuring. Clinically, these results may also help identify a subset of patients who are more likely to gain large amounts of weight during the course of their disorder. Namely, those who experience the onset of BN at a younger age may be more likely to reach a post-morbid highest weight. This information and information regarding the correlation between disorder duration and highest weight achieved could be used to educate patients regarding the likelihood of weight gain in spite of (or because of) their continual engagement in bulimic behaviors, which may help weaken their conviction that maintaining these behaviors will provide the intended protective effects. Similarly, these findings could be incorporated into weight gain prevention programs. It is possible that fewer girls would choose to begin engaging in extreme behaviors such as purging if it were widely known that these behaviors did not prevent – and might even contribute to -weight gain. Although further replication as well as the collection of additional data regarding bulimic patients’ pre-morbid weight histories is necessary to further test these hypotheses, the strikingly similar weight patterns found in these two studies provide strong initial evidence that the course of BN is characterized not only by large weight losses, but also by large weight gains as the disorder progresses.
It is also important to consider the implications of these findings to the meaning of weight suppression. Weight suppression could result from either a steady decline in weight or from fluctuations between repeated weight losses and weight gains. It is also possible that weight suppression may have differential predictive power depending on whether one calculates it as the difference from a pre-morbid or post-morbid highest weight. Data are currently being collected to examine these possibilities.
The present study has several limitations that should be considered. The historical weights examined in both studies and the prospective weights used in Study 2 were collected via self-report. Though the validity of past weights has been supported in other studies (e.g. 25), the accuracy of the weights reported by our samples is unknown. A second limitation is that neither study collected information regarding the pre-morbid weights of those who report a post-onset highest weight at intake. This information would help us to better determine both whether the majority of patients with bulimia report elevated pre-morbid weights as seen in a subset of our participants, and whether the two weight history patterns described represent two different weight trajectories or the same weight trajectory captured at different time points. Data are currently being collected which will help us to examine this question. Finally, these results are limited to individuals seeking treatment (Study 1) or willing to participate in a research study (Study 2), and may not generalize to individuals with bulimia nervosa who are not seeking or receiving treatment.
In spite of these limitations, this study also had several strengths. One is that it sought to describe a phenomenon that has rarely been investigated – the weight trajectories of individuals with BN. A second strength is the use of two distinct data sets to replicate retrospective results. Finally, this study was able to establish a pattern using retrospective data and confirm it using prospective data. Future research is needed to more clearly describe the typical weight history patterns of individuals with BN and to establish how these weight trajectories may relate to a predisposition towards overweight. Research is also needed to determine whether discussing historic and future weight gain more explicitly in therapy would be beneficial in the treatment of BN.
Acknowledgments
This work was supported by the National Institute of Mental Health grants R34 MH 071691 (MRL) and 5R01 MH 38333 05 (DBH).
Footnotes
Note that the average amount of time between participants’ lowest and highest weights described here and displayed in Figure 1 is shorter than the actual difference between these two events because participants who reach their lowest weight after their highest weight have been included (60% of participants across both studies). When only participants who report reaching their lowest weight prior to their highest weight are included, this period of weight gain is still quite rapid (see General Discussion).
Results including all follow-up weights were similar except in that duration of disorder no longer differed significantly.
These figures only include participants who report reaching their lowest weight before reaching their highest weight.
Financial Disclosure and Conflict of Interest
Jena A. Shaw has no competing financial interests or conflict of interest with the contents of this manuscript. David B. Herzog has no competing financial interests or conflict of interest with the contents of this manuscript.
Vicki L. Clark has no competing financial interests or conflict of interest with the contents of this manuscript.
Laura A. Berner has no competing financial interests or conflict of interest with the contents of this manuscript.
Kamryn T. Eddy has no competing financial interests or conflict of interest with the contents of this manuscript.
Debra L. Franko has no competing financial interests or conflict of interest with the contents of this manuscript.
Michael R. Lowe is a Research Consultant for the Renfrew Center for Eating Disorders.
References
- 1.Russell G. Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med. 1979;9(3):429–448. doi: 10.1017/s0033291700031974. [DOI] [PubMed] [Google Scholar]
- 2.Eddy KT, Dorer DJ, Franko DL, Tahilani KK, Thompson-Brenner H, Herzog DB. Should bulimia nervosa be subtyped by history of anorexia nervosa? A longitudinal validation. Int J Eat Disord. 2007;40 (Suppl):S67–71. doi: 10.1002/eat.20422. [DOI] [PubMed] [Google Scholar]
- 3.Butryn ML, Lowe MR, Safer DL, Agras WS. Weight suppression is a robust predictor of outcome in the cognitive-behavioral treatment of bulimia nervosa. J Abnorm Psychol. 2006 Feb;115(1):62–67. doi: 10.1037/0021-843X.115.1.62. [DOI] [PubMed] [Google Scholar]
- 4.Wilson GT. The Controversy Over Dieting. In: Fairburn CG, Brownell KD, editors. Eating Disorders and Obesity: A Comprehensive Handbook. New York: Guilford Press; 2002. [Google Scholar]
- 5.Fairburn CG, Welch SL, Doll HA, Davies B, O’Connor ME. Risk factors for bulimia nervosa: A community-based case-control study. Archives of General Psychiatry. 1997;54:509–517. doi: 10.1001/archpsyc.1997.01830180015003. [DOI] [PubMed] [Google Scholar]
- 6.Monteleone P, Serritella C, Scognamiglio P, Maj M. Enhanced ghrelin secretion in the cephalic phase of food ingestion in women with bulimia nervosa. Psychoneuroendocrinology. 2010 Feb;35(2):284–288. doi: 10.1016/j.psyneuen.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 7.Legenbauer T, Vogele C, Ruddel H. Anticipatory effects of food exposure in women diagnosed with bulimia nervosa. Appetite. 2004 Feb;42(1):33–40. doi: 10.1016/S0195-6663(03)00114-4. [DOI] [PubMed] [Google Scholar]
- 8.Wisniewski L, Epstein LH, Marcus MD, Kaye W. Differences in salivary habituation to palatable foods in bulimia nervosa patients and controls. Psychosom Med. 1997 Jul-Aug;59(4):427–433. doi: 10.1097/00006842-199707000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Garner DM, Fairburn CG. Relationship between anorexia nervosa and bulimia nervosa: diagnostic implications. In: Garner DM, Garfinkel PE, editors. Diagnostic Issues in Anorexia Nervosa and Bulimia Nervosa. New York: Brunner/Mazel; 1988. p. 56. [Google Scholar]
- 10.Polivy J, Herman CP. Dieting and binging: A casual analysis. Am Psychol. 1985;40:193–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- 11.Lowe MR. The effects of dieting on eating behavior: a three-factor model. Psychol Bull. 1993;114:100–121. doi: 10.1037/0033-2909.114.1.100. [DOI] [PubMed] [Google Scholar]
- 12.Lowe MR, Thomas JG, Safer DL, Butryn ML. The relationship of weight suppression and dietary restraint to binge eating in bulimia nervosa. Int J Eat Disord. 2007 Nov;40(7):640–644. doi: 10.1002/eat.20405. [DOI] [PubMed] [Google Scholar]
- 13.Lowe MR, Davis W, Lucks D, Annunziato R, Butryn M. Weight suppression predicts weight gain during inpatient treatment of bulimia nervosa. Physiol Behav. 2006 Mar 30;87(3):487–492. doi: 10.1016/j.physbeh.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 14.Carter FA, McIntosh VW, Joyce PR, Bulik CM. Weight suppression predicts weight gain over treatment but not treatment completion or outcome in bulimia nervosa. Journal of Abnormal Psychology. 2008;117(4):936–940. doi: 10.1037/a0013942. [DOI] [PubMed] [Google Scholar]
- 15.Herzog DB, Thomas JG, Kass AE, Eddy KT, Franko DL, Lowe MR. Weight suppression predicts weight change over 5 years in bulimia nervosa. Psychiatry Res. 2010 May;177(3):330–334. doi: 10.1016/j.psychres.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keel PK, Heatherton TF. Weight suppression predicts maintenance and onset of bulimic syndromes at 10-year follow-up. J Abnorm Psychol. 2010 May;119(2):268–275. doi: 10.1037/a0019190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogden CL, Carroll MD. Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults: United States, Trends 1976–1980 Through 2007–2008. National Center for Health Statistics. Vital Health Stat. 2010 [Google Scholar]
- 18.Fairburn CG, Cooper Z. Binge eating: Nature, assessment, and treatment. New York, NY: Guildford Press; 1993. [Google Scholar]
- 19.Herzog DB, Keller MB, Sacks NR, Yeh CJ. Psychiatric comorbidity in treatment-seeking anorexics and bulimics. Journal of the American Academy of Child& Adolescent Psychiatry. 1992 Sep;31(5):810–818. doi: 10.1097/00004583-199209000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Fairburn CG, Cooper ZC. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment, and treatment. 12. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 21.Garner DM. Eating Disorders Inventory-2. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- 22.Garner DM, Garfinkel PE. The eating attitudes test: An index of the symptoms of anorexia nervosa. Psychol Med. 1979 May;9(2):273–279. doi: 10.1017/s0033291700030762. [DOI] [PubMed] [Google Scholar]
- 23.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 24.Goldfarb LA, Dykens EM, Gerrard M. The Goldfarb Fear of Fat Scale. Journal of Personality Assessment. 1985;49(3):329–332. doi: 10.1207/s15327752jpa4903_21. [DOI] [PubMed] [Google Scholar]
- 25.Tamakoshi K, Yatsuya H, Kondo T, Hirano T, Hori Y, Yoshida T, et al. The accuracy of long-term recall of past body weight in Japanese adult men. Int J Obes. 2003;27:247–252. doi: 10.1038/sj.ijo.802195. [DOI] [PubMed] [Google Scholar]
- 26.Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. British Journal of Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 27.Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the eating disorder examination. Int J Eat Disord. 2000 Nov;28(3):311–316. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 28.Garner DM, Olmsted MP, Polivy J. Development and validation of a multidimensional Eating Disorder Inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2:15–34. [Google Scholar]
- 29.Garner DM. EDI-3 Eating Disorder Inventory-3 Professional Manual. Odessa, FL: Psychological Assessment Resource, Inc; 2004. [Google Scholar]
- 30.Koslowsky M, Scheinberg Z, Bleich A, Mark M. The factor structure and criterion validity of the short form of the Eating Attitudes Test. J Pers Assess. 1992 Feb;58(1):27–35. doi: 10.1207/s15327752jpa5801_3. [DOI] [PubMed] [Google Scholar]
- 31.Center for Disease Control and Prevention. 2000 CDC Growth Charts for the United States: Methods and Development. National Center for Health Statistics. Vital Health Stat. 2000;11(246) [PubMed] [Google Scholar]
- 32.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, D.C: American Psychiatric Association; 1987. [Google Scholar]
- 33.Herzog DB, Dorer DJ, Keel PK, Selwyn SE, Ekeblad ER, Flores AT, et al. Recovery and relapse in anorexia and bulimia nervosa: A 7. 5-year follow-up study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999 Jul;38(7):829–837. doi: 10.1097/00004583-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Endicott J, Spitzer RL. Use of the Research Diagnostic Criteria and the Schedule for Affective Disorders and Schizophrenia to study affective disorders. Am J Psychiatry. 1979 Jan;136(1):52–56. doi: 10.1176/ajp.136.1.52. [DOI] [PubMed] [Google Scholar]
- 35.Robins LN, Helzer JE, Croughan JL, Ratcliff KS. National Institute of Mental Health diagnostic interview schedule: Its history, characteristics, and validity. Arch Gen Psychiatry. 1981 Apr;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 36.Keller MB, Lavori PW, Friedman B, Nielsen E. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987 Jun;44(6):540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 37.Striegel-Moore RH, Cachelin FM. Body image concerns and disordered eating in adolescent girls: Risk and protective factors. In: Johnson NG, Roberts MC, Worell J, editors. Beyond appearance: A new look at adolescent girls. Washington, DC, US: American Psychological Association; 1999. pp. 85–108. [Google Scholar]
- 38.Jones DC. Social comparison and body image: Attractiveness comparisons to models and peers among adolescent girls and boys. Sex Roles. 2001 Nov;45(9–10):645–664. [Google Scholar]
- 39.McCabe MP, Ricciardelli LA. Parent, peer, and media influences on body image and strategies to both increase and decrease body size among adolescent boys and girls. Adolescence. 2001 Sum;36(142):225–240. [PubMed] [Google Scholar]
- 40.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; 2000. text revision ed. [Google Scholar]
- 41.Lewis CE, Jacobs DR, McCreath H, Kiefe CI, Schreiner PJ, Smith DE, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Am J Epidemiol. 2000;151(12):1172–81. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 42.Thomas JG, Butryn ML, Stice E, Lowe MR. A Prospective Test of the Relation Between Weight Change and Risk for Bulimia Nervosa. Internation Journal of Eating Disorders. doi: 10.1002/eat.20832. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]