Abstract
Objectives
We sought to examine whether there are patterns of evolving depression symptoms among older primary care patients that are related to prognostic factors and long-term clinical outcomes.
Method
Primary care practices were randomly assigned to Usual Care or to an intervention consisting of a depression care manager offering algorithm-based depression care. In all, 599 adults 60 years and older meeting criteria for major depression or clinically-significant minor depression were randomly selected. Longitudinal analysis via growth curve mixture modeling was carried out to classify patients according to the patterns of depression symptoms across 12 months. Depression diagnosis determined after a structured interview at 24 months was the long-term clinical outcome.
Results
Three patterns of change in depression symptoms over 12 months were identified: high persistent course (19.1% of the sample), high declining course (14.4% of the sample), low declining course (66.5% of the sample). Being in the intervention condition was more likely to be associated with a course of high and declining depression symptoms than high and persistent depression symptoms (OR = 2.53, 95% CI [1.01, 6.37]). Patients with a course of high and persistent depression symptoms were much more likely to have a diagnosis of major depression at 24 months compared with patients with a course of low and declining depression symptoms (adjusted OR = 16.46, 95% CI [7.75, 34.95]).
Conclusion
Identification of patients at particularly high risk of persistent depression symptoms and poor long-term clinical outcomes is important for the development and delivery of interventions.
Trial Registration
clinicaltrials.gov registration number: NCT00000367.
Keywords: Aged, Primary health care, Geriatric depression
INTRODUCTION
The diagnosis and management of depression is challenging: a focus on syndromes such as major depression is balanced by the realization that major depression describes a clinically diverse set of people. While some elderly patients may respond quickly to treatment, other elderly patients may have a slower road to recovery (Alexopoulos et al., 2005). The basis for individual differences in response and course relates to many factors (Hardeveld, Spijker, De Graaf, Nolen, & Beekman, 2009), including genetic factors (Caspi, Hariri, Holmes, Uher, & Moffitt, 2010), but clinicians must rely on the venerable disease characteristics of course, prognostic factors, and outcomes to make decisions about treatment.
Course of depressive illness might help identify who with major or minor depression is most at risk for persistent depression much as the use of prognostic factors and course has changed medicine in recent decades. For example, the use of prostate-specific antigen for screening has evolved from reliance on a single measurement at one point in time to examine the rate of change in prostate-specific antigen level over time as a guide to treatment (Carter et al., 1992; Eastham et al., 2003), and developmental patterns of alcohol use have been found to predict risk for alcohol dependence (Muthen & Muthen, 2000a; Muthen, 2001; Muthen & Muthen, 2000b; Muthen & Shedden, 1999). The strategy of delineating subtypes based on the course of illness assumes we can relate the rate or nature of change or course of change to outcomes such as disease progression that would signal a need to intervene and interrupt the course of the disease. Experienced clinicians often follow and use course to guide the next steps in therapy.
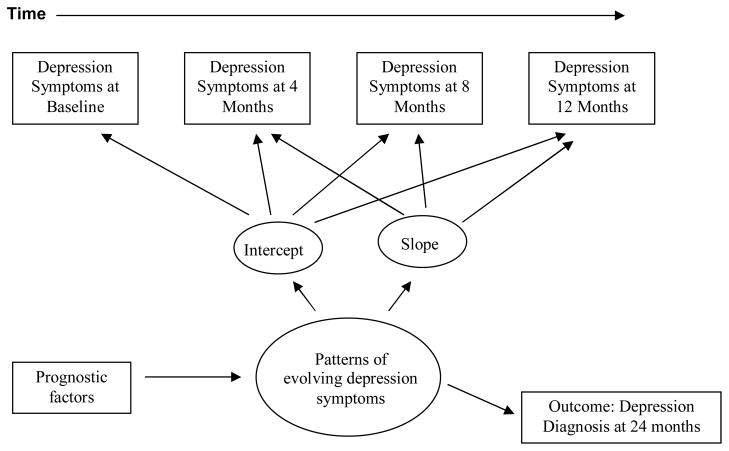
Our investigation uses longitudinal depression symptom data to identify subgroups of older patients at risk for persistent depression symptoms over 12 months and a diagnosis of major depression at 24 months. Our purpose was to further understand (1) course of depression symptoms through the examination of patterns of depression symptoms over 12 months among older adults, (2) whether such patterns are related to baseline prognostic factors of course; and, (3) whether patterns predict the long-term outcome of depression at 24 months (Figure 1). We used an innovative technique for longitudinal data analysis, the growth curve mixture model (GCMM), which is well suited to the study of individual differences in development and change over time. This technique identifies different subgroups of patients based on their underlying trends and whether membership in the subgroups is associated with baseline prognostic factors of course and subsequent long-term clinical outcomes. We employed data from the multi-site, randomized trial, PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial). The study intervention was implemented at the practice level and involved a depression care manager working with physicians to provide algorithm-based care (Bruce et al., 2004). We hypothesized that some patients will have a course of depression symptoms consistent with delayed or little recovery and persistence of depression symptoms across 12 months. We also hypothesized based on the literature that patients who were cognitively impaired (Alexopoulos et al., 1996; Farmer et al., 1990), were not married (Voils, Steffens, Flint, & Bosworth, 2005), or had a greater medical burden (Rosenstock, 1988) would be more likely than others to have a course of persistent depression symptoms. We hypothesized that patients in usual care would be more likely to have persistent depression symptoms compared to patients in the intervention condition. Finally, we hypothesized that patients with a course of persistent depression symptoms across 12 months will be at increased risk for meeting criteria for major depression at 24 months. Identifying patterns of depression over 12 months linked to the long-term outcome of depression diagnosis at 24 months will set the stage for interventions targeting resources to the persons most at risk for persistent depression.
Figure 1.
Conceptual framework consistent with prognostic factors, course, and long-term clinical outcome of depression.
Note: Data gathered from the PROSPECT study. Depression symptoms over time based on the Hamilton Depression Rating Scale (HDRS). Depression diagnosis at 24 months based on the Structured Clinical Interview for Axis I DSM-IV Diagnoses (SCID).
Prior work has focused on the chronic course of Major Depression and has sought to identify clinical factors related to patients’ history of depression that may account for a differential response to treatment. Our work fills a gap in the literature and differs from prior work in the following ways. First, many of the prior studies on course of depression focus on specialty mental health settings (Andreescu et al., 2008; Dew et al., 1997; Gildengers et al., 2005; Hybels, Blazer, Pieper, Landerman, & Steffens, 2009; Hybels, Pieper, Blazer, & Steffens, 2008; Mulder, Joyce, Frampton, Luty, & Sullivan, 2006; Stulz, Thase, Klein, Manber, & Crits-Christoph, 2010) or community settings (Beard, Tracy, Vlahov, & Galea, 2008; Colman, Ploubidis, Wadsworth, Jones, & Croudace, 2007; Patten & Schopflocher, 2009; Sullivan, Kessler, & Kendler, 1998). However, primary care is an important part of the pathway to mental health care in community settings (Bogner, de Vries, Maulik, & Unutzer, 2009) and enhancing primary care depression management for patients most at risk of poor outcomes would be a promising use of health care resources (Rost, Pyne, Dickinson, & LoSasso, 2005). Second, we are specifically interested in older adults, while most studies include age ranges encompassing younger samples (Aikens, Kroenke, Nease, Klinkman, & Sen, 2008). The undertreatment of mental disorders remains the greatest among vulnerable groups, including older adults (Wang et al., 2005). Third, other studies have focused only on major depression (Licht-Strunk et al., 2009) or not incorporated treatment into the analyses (Cui, Lyness, Tang, Tu, & Conwell, 2008). Thus, to our knowledge, no study has examined prognostic factors, pattern of time-varying depression, and outcome in a primary care trial of depression management among older adults with the ultimate goal of translating the knowledge into reducing the persistence of depression symptoms. Accurate differentiation of a high risk group of older adults for depression should not only lead to intensive treatment but also reduction of factors leading to relapse or recurrence. The American Psychiatric Association has posted a draft of Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) on a special website, www.dsm5.org, to obtain feedback. One substantial innovation they are proposing is using dimensional assessments to account for severity of symptoms. The National Institute of Mental Health Strategic Plan states the “developmental trajectory of illnesses opens the possibility that we could intervene and alter trajectories” and stresses the importance of identifying “malleable and robust risk factors for different phases of the disease trajectory” (United States Department of Health and Human Services, 2008). A further understanding of the patterns of evolving depression symptoms and whether such patterns are related to baseline prognostic factors of course and long-term clinical outcomes among elderly primary care patients would be a key step in intervening to improve recognition and treatment of late life depression.
METHODS
The PROSPECT Study
The PROSPECT Study was a multisite, collaborative study designed to assess whether depression treatment in primary care settings can reduce the risk of suicide in elderly patients. A total of 20 primary care practices participated, including practices from greater New York, New York, and Philadelphia and Pittsburgh, Pennsylvania in the United States. Practices were paired within each region (New York, Philadelphia, Pittsburgh) by setting (urban, suburban, rural), academic affiliation (university vs. community based), size, and the ethnicity distribution of their patient populations. Within pairs, practices were randomly assigned to either enhanced care or intervention. The study used a two-stage sampling design to generate a representative sample of primary care patients with the DSM-IV diagnosis of major depression or clinically-significant minor depression. All patients in our study sample met criteria for major depression or clinically-significant minor depression. An age-stratified (60–74 years, over 75 years), random sample was obtained of patients with an appointment with their primary care physician within 2 weeks. Patients were interviewed in person at the primary care practices. Eligibility criteria included: (a) age 60 years and older; (b) community dwelling (i.e., not living in a nursing home or other institution); (c) English speaking; and (d) attending a scheduled visit with a primary care physician (i.e., a non-emergency visit). Exclusion criteria included: (a) inability to give informed consent; (b) severe cognitive impairment as indicated by a MMSE score of 17/30 or less; and (c) severe aphasia interfering with communication. First, patients who gave oral consent were screened for depression symptoms using the Centers for Epidemiologic Studies Depression scale (CES-D) (Radloff, 1977). All patients with CES-D above 20 as well as a 5% random sample of patients with lower scores were invited to enter the study. The purpose of the 5% sample was to assess for “false negative” cases of screened depression. To increase the sensitivity of the screening procedure, patients with CES-D <20 and not selected for the 5% random sample were also recruited if they reported history of depression or antidepressant treatment. From the resulting sample, depression diagnoses were determined by the Structured Clinical Interview for Axis I DSM-IV Diagnoses (SCID) (Spitzer, Gibbon, & Williams, 1995). Clinically-significant minor depression was defined by the study as a depression meeting at least three DSM-IV criteria, having a 24-item Hamilton Depression Rating Scale (HDRS) score of 10 or higher, and persisting for at least one month. Details of the study design of the PROSPECT Study are available elsewhere (Bruce, et al., 2004). The study protocols were approved by the Institutional Review Boards of the Cornell University, University of Pittsburgh, and University of Pennsylvania Schools of Medicine.
PROSPECT Intervention
The intervention was implemented by 15 depression care managers, who used the Agency for Health Care Policy and Research (AHCPR) Guidelines (after operationalization and adaptation for older patients) to provide appropriately timed and targeted recommendations to primary care physicians. The depression care managers were nurses, social workers, or psychologists trained and supervised weekly by geriatric psychiatrist investigators and functioned as collaborators to primary care physicians. The depression care managers monitored psychopathology, treatment adherence, treatment response and side effects and provided follow-up in-person or by telephone at predetermined intervals or when clinically necessary. However, the primary care physicians remained responsible for the clinical care of their patients. The intervention and the algorithm derived from the AHCPR Guidelines has been described in detail elsewhere (Bruce, et al., 2004).
Measurement strategy: Depression diagnoses
Trained research assistants (Ph.D., M.A. or experienced B.A. level) assigned clinical depression diagnoses to patients using the SCID (Spitzer, Gibbon, & Williams, 1995) at baseline and 24 months. Study psychiatrists reviewed all the SCID ratings. Severity of depression was assessed using the 24-item Hamilton Depression Rating Scale (HDRS) (Hamilton, 1960) at baseline, 4 months, 8 months, and 12 months. HDRS scores were analyzed as a continuous variable. We used the Scale for Suicidal Ideation (SSI) (Beck, Brown, & Steer, 1997) to measurepresence and intensity of current suicidal ideation at baseline. Scores of 0 indicated no suicidal ideation, while scores >1 on items 1–3 indicated passive suicidal ideation. These items reflect lack of desire to live, desire to die, and the belief that reasons for dying outweigh reasons for living.
Measurement strategy: Covariates
We used standard questions to obtain information from the patients on baseline age, gender, self-reported ethnicity, marital status, and education. Persons were classified as having a medical comorbidity by self-report at baseline. The questionnaire used was based on the Charlson Comorbidity Index, supplemented by questions about the common disabling conditions of late life (Charlson, Pompei, Ales, & MacKenzie, 1987). Patients were asked about myocardial infarction, heart failure, angina, angioplasty or coronary artery bypass surgery, atrial fibrillation, stroke, peripheral vascular disease, high blood pressure, diabetes, cancer, chronic pulmonary disease, peptic ulcer disease, and joint disease. Total medical burden was calculated by adding up the number of medical conditions. The median number of medical conditions in our sample was 3, and persons with 3 or more conditions were considered to have high medical burden.
Baseline cognitive status was assessed with the Mini-Mental State Examination (MMSE) which is a short standardized mental status examination that has been widely employed for clinical and research purposes (Folstein, Folstein, & McHugh, 1975). The MMSE has been extensively studied, as reviewed by Tombaugh and McIntyre (Tombaugh & McIntyre, 1992). The MMSE assesses orientation to time and place, registration, memory, attention and concentration, praxis, and constructional and language capacity. Based on prior work, MMSE scores were analyzed as a dichotomous variable with scores less than 24 representing cognitive impairment (Bogner et al., 2005; Crum, Anthony, Bassett, & Folstein, 1993)
Analytic strategy
In the first phase we used the growth curve mixture model (GCMM) to create latent classes corresponding to subtypes of depression based on course of depression symptoms (measured by HDRS) across the first 12 months of the study (baseline, 4, 8, and 12 months). The model for the course subtype of longitudinal depression symptom outcomes included random intercepts and slopes to account for within-subject correlations and separate fixed effect intercepts and fixed effects slopes for time within each latent class or pattern of evolving depression symptoms. We compared the results of this longitudinal linear model to models that accommodated nonlinear changes in depression across time. The classifications into different patterns of evolving depression symptoms were similar across the different models, so we base our results on the simpler linear model. For longitudinal depression symptom outcomes, clustering by practice and pairs of practice was negligible and did not affect the analysis. The choice of the number of classes was determined through examination of fit indices as well as for clinically interpretable results. The Rubin-Lo-Mendell test (Lo, Mendell, & Rubin, 2001) was used to determine if additional classes added further information to the model.
In the second phase the GCMM also included a multinomial logistic regression of the latent classes on the baseline covariates to find predictors of class membership. Accordingly, the relationship between these baseline covariates and the latent classes or patterns of evolving depression symptoms was simultaneously assessed with the odds ratio and confidence intervals. The baseline covariates were selected on the basis of previous literature on prognostic factors for depression.
In the third phase each respondent was assigned to their most likely class under the GCMM as indicated by the posterior probabilities of class membership. We related the assigned classes or patterns of evolving depression symptoms based on 12 months of depression symptoms to the diagnosis of clinical major, minor, or no depression at 24 months using multinomial logistic regression. The results are presented in the form of odds ratios and 95% confidence intervals. The model included terms to adjust for baseline differences in age, gender, ethnicity, marital status, baseline depression diagnosis, medical comorbidity, suicidal ideation, and intervention condition. We set α at 0.05, recognizing that tests of statistical significance are approximations that serve as aids to interpretation and inference. The GCMM was fitted using Mplus version 5.1 and other analyses were conducted in SAS version 9.2.
RESULTS
Study sample
The CONSORT flow diagram for the PROSPECT trial has been published elsewhere (Bruce, et al., 2004). In brief, the study screened 9,072 older persons, and 1,888 persons were invited to participate. Out of the 1,888 persons invited to participate, 1,238 (65.8%) agreed to a baseline interview. Our study sample included 599 depressed patients, of whom 396 (66.1%) met DSM-IV criteria for major depression and 203 (33.9%) met criteria for clinically-significant minor depression. Two respondents were missing values on a baseline covariate leaving 597 for analysis. The mean age of our sample was 70.2 years (standard deviation (s.d.) 7.9 years, range 60 to 94 years). Four hundred and twenty-seven (71.5%) of the patients were women. The self-identified ethnicity of patients was 419 white (70.2%), 162 African-American (27.1%), and 16 American Indian or Asian (2.7%). In all, 220 persons (36.9%) were married and 260 persons (43.6%) had 3 or more medical conditions. The mean education was 12.8 years (s.d. 4.2 years) and the mean MMSE score was 27.4 (s.d. 2.7). In the last part of our analysis involving the outcome of depression diagnosis, 206 patients were excluded due to missing data on depression diagnosis at 24 months, leaving a sample size of 391 for this part of the analysis. Out of the 206 patients with missing data, 37 patients had died. The remaining 169 patients with missing data did not differ significantly in age, gender, ethnicity, education, marital status, medical comorbidity, suicidal ideation, baseline depression diagnosis, and cognitive status compared to the 391 patients without missing data on depression diagnosis at 24 months. However, persons with missing data were more likely to be in the intervention group than usual care. We will examine the implications in the discussion of the study results.
Patterns of depression symptoms
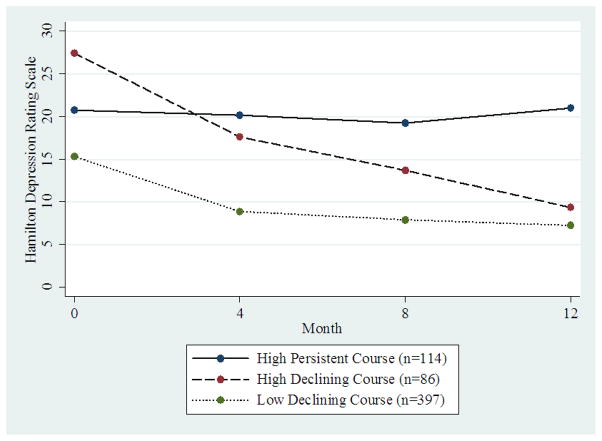
Figure 2 shows the patterns of evolving depression symptoms represented by the mean observed HDRS scores at each of four time points over the 12-month follow-up interval. The first pattern represents persons who report a high level of depression symptoms at baseline and have a persistent course (“high persistent course”; n = 114, 19.1% of the sample). Patients with a high persistent course had a mean HDRS at baseline of 20.2 and a flat slope of −0.03 (95% confidence interval (CI) [−0.22, 0.17]). The slope was not statistically significant indicating persistently high depression symptoms. The second pattern represents persons who report a high level of depression symptoms at baseline and improve (“high declining course”; n = 86, 14.4% of the sample). Patients with a high declining course had a mean HDRS score of 25.8 at baseline with a statistically significant decline in depression symptoms (slope = −1.43, 95% CI [−1.67, −1.19]). This slope represents a reduction of depression symptom score of 1.43 per month over the 12-month follow-up. Patients in the third pattern had a baseline HDRS score of 14.6 with a statistically significant decline in depression symptoms (slope = −0.67, 95% CI [−0.84, −0.51]). We designated these patients as having a “low declining course”; n=397, 66.5% of the sample). The Rubin-Lo-Mendell test indicated that the three-class model of longitudinal depression trajectories improved the model fit over the two-class model (p = 0.03), with the four-class model providing no additional improvement in fit (p = 0.21). The three-class model was also clinically most relevant. For the three-class model the average posterior probability of class 1 membership “high persistent course” for those assigned to class 1 was 79.5%. Similarly, the average posterior probability of class 2 “high declining course”; and class 3 “low declining course” for those assigned to class 2 and class 3 were 78.8% and 90.8%, respectively.
Figure 2.
Mean Hamilton Depression Rating Scales across time stratified on the three patterns of evolving depression symptoms (n=597).
Note: Data gathered from the PROSPECT study.
Prognostic factors for patterns of depression symptoms: Depression diagnosis
Table 1 shows the relationship between baseline depression diagnosis (meets criteria for major depression or for clinically-significant minor depression) and patterns of evolving depression symptoms (χ2 (2)= 88.8, p<.001). Among patients who met criteria for major depression at baseline, 99 (25.1%) had a course of depression symptoms consistent with the high persistent course, 84 (21.3%) with the high declining course, and 212 (53.7%) with the low declining course. Among patients who met criteria for clinically-significant minor depression at baseline, 185 (91.5%) had a course of depression symptoms consistent with the low declining course. In all, 17 (8.4%) patients with clinically-significant minor depression had a course of depression symptoms consistent with the high declining course or the high persistent course.
Table 1.
Baseline Structured Clinical Interview for Axis I DSM-IV Diagnoses (SCID) by the three patterns of evolving depression symptoms (n=597).
| N, % | |||
|---|---|---|---|
| Patterns of depression symptoms | High persistent course (n=114) | High declining course (n=86) | Low declining course (n=397) |
| Baseline major depressive disorder | 99 (25.1%) | 84 (21.3%) | 212 (53.7%) |
| Baseline clinically-significant minor depression | 15 (7.4%) | 2 (1%) | 185 (91.5%) |
Note: Data gathered from the PROSPECT study. Percents are row percents.
Chi-Square test on the table: (χ2 (2)= 88.8, p<.001).
Prognostic factors for patterns of depression symptoms: Patient characteristics
Patient characteristics associated with patterns of evolving depression symptoms are shown in Table 2. Education and cognitive status were not statistically significantly associated with patterns of depression symptoms and were dropped from further consideration. The column of Table 2 labeled High persistent vs. Low declining course provides odds ratios estimating the association of baseline prognostic factors with pattern of depression symptoms, comparing the high persistent course to the low declining course. Age less than 70 years, not being married, reporting 3 or more medical conditions, and suicidal ideation at baseline were associated with a high persistent course. The column of Table 2 labeled High declining vs. Low declining course comparing the high declining course to the low declining course shows similar results. Overall, relative to patients with low and declining depression symptoms, patients with high and persistent depression symptoms and high and declining depression symptoms were more likely to be less than 70 years with higher levels of baseline suicidal ideation and medical comorbidity. To highlight differences in prognostic factors between the high declining course and high persistent course, we provide the estimates in the column of Table 2 labeled High declining vs. High persistent course. Being married was more likely to be associated with a course of high and declining depression symptoms than high and persistent depression symptoms (odds ratio (OR) = 3.56, 95% confidence interval (CI) [1.18, 10.71]). Being in the intervention condition was also more likely to be associated with a course of high and declining depression symptoms than high and persistent depression symptoms (OR = 2.53, 95% CI [1.01, 6.37]).
Table 2.
Multivariate logistic regression of baseline patient characteristics among the three patterns of evolving depression symptoms generated from the growth curve mixture model (GCMM) (n= 597).
| Patient characteristics | High persistent vs. Low declining course OR [95% CI] | High declining vs. Low declining course OR [95% CI] | High declining vs. High persistent course OR [95% CI] |
|---|---|---|---|
| Age (reference: less than 70 years) | 0.42* [0.22, 0.79] | 0.21* [0.09, 0.50] | 0.50 [0.16, 1.55] |
| Gender (reference: male) | 1.45 [0.70, 3.00] | 1.33 [0.45, 3.98] | 0.92 [0.20, 4.13] |
| Ethnicity (reference: minority) | 0.76 [0.44, 1.31] | 1.04 [0.57, 1.88] | 1.37 [0.71, 2.64] |
| Marital status (reference: not married) | 0.45* [0.20, 0.99] | 1.60 [0.49, 5.24] | 3.56* [1.18, 10.71] |
| Medical comorbidity (reference: less than 3 conditions) | 1.99* [1.11, 3.56] | 3.61* [1.96, 6.65] | 1.81 [0.84, 3.91] |
| Suicidal ideation (reference: no suicidal ideation) | 3.16* [1.78, 5.61] | 6.51* [3.17, 13.37] | 2.06 [0.86, 4.95] |
| Intervention (reference: usual care) | 0.75 [0.32, 1.76] | 1.91 [0.94, 3.88] | 2.53* [1.01, 6.37] |
Note: Data gathered from the PROSPECT study.
OR = odds ratio; CI = confidence interval.
p< .05
Long-term clinical outcome of patterns of depression symptoms: Depression diagnosis at 24 months
Having presented the results related to prognostic factors assessed at baseline, we now turn our attention to the outcome of depression diagnosis at 24 months in relation to the three patterns of evolving depression symptoms (Table 3). Clinical depression diagnosis at 24 months using the SCID was strongly related to the patterns of depression symptoms (χ2 (4)= 94.7, p<.001). Patients with a course of high and persistent depression symptoms were much more likely to have a diagnosis of major depression at 24 months compared with patients with a course of low and declining depression symptoms (adjusted OR = 16.46, 95% CI [7.75, 34.95]). Patients with a course of high and persistent depression symptoms were also more likely to have a diagnosis of clinically-significant minor depression at 24 months compared with patients with a course of low and declining depression symptoms (adjusted OR = 5.53, 95% CI [2.34, 13.06]). Patients with a course of high and declining depression symptoms were at increased risk for meeting criteria for major depression at 24 months (adjusted OR = 3.38, 95% CI [1.37, 8.37]), but not for clinically-significant minor depression, compared to patients with a course of low and declining depression symptoms. The model included terms to adjust for baseline differences in age, gender, ethnicity, marital status, baseline depression diagnosis, medical comorbidity, suicidal ideation, and intervention condition.
Table 3.
Outcome Structured Clinical Interview for Axis I DSM-IV Diagnoses (SCID) at 24 months for the three patterns of evolving depression symptoms (n=391).
| Adjusted OR** [95% CI] | ||
|---|---|---|
| Patterns of depression symptoms (0–12 months) | Major depressive disorder vs. non-depressed at 24 months | Clinically-significant minor depression vs. non-depressed at 24 months |
| High persistent course (n=70) | 16.46* [7.75, 34.95] | 5.53* [2.34, 13.06] |
| High declining course (n=52) | 3.38* [1.37, 8.37] | 1.48 [0.47, 4.61] |
| Low declining course n=269) | 1.00 | 1.00 |
Note: Data gathered from the PROSPECT study.
OR = odds ratio; CI = confidence interval;
The total sample is 391 for the outcome depression diagnosis due to missing values at 24 months on the Structured Clinical Interview for Axis I DSM-IV Diagnoses (SCID).
p< .05
adjusted for baseline age, gender, ethnicity, marital status, medical comorbidity, baseline depression diagnosis, suicidal ideation, and intervention condition.
DISCUSSION
Examination of course of depression symptoms over 12 months revealed three patterns of evolving depression symptoms (high persistent course, high declining course, and low declining course). Overall, relative to patients with low and declining depression symptoms, patients with high and persistent depression symptoms and high and declining depression symptoms were more likely to be less than 70 years consistent with the literature that depressed patients in late life may not acknowledge sadness (Gallo, Anthony, & Muthen, 1994). In addition, patients with high and persistent depression symptoms and high and declining depression symptoms were more likely to have higher levels of baseline suicidal ideation and medical comorbidity compared to patients with low and declining depression symptoms. However, patients with high and persistent depression symptoms were less likely to be married and less likely to be in the intervention condition compared to patients with high and declining depression symptoms. Major depression at baseline did not identify a single set of patients with a distinct course. Patients with a course of high and persistent depression symptoms were also much more likely to have a diagnosis of major depression at 24 months compared with patients with a course of low and declining depression symptoms. Prognostic factors and course of depression identified older adults at high risk of poor clinical outcomes.
Before discussing our findings, the results must first be considered in the context of some potential study limitations. First, we obtained our results only from primary care sites in greater New York City, Philadelphia, and Pittsburgh whose patients may not be representative of other primary care practices in the United States. However, these practices were both community-based and academically affiliated and are therefore probably similar to the range of other practices in that region. Second, although more frequent follow-up would have been desirable, concerns about participant burden and cost led us to select few, yet clinically meaningful, follow-up times. If there was a group with increasing depression symptoms, we did not have enough variability in the data to identify such a group. Third, our measure of medical comorbidity determined by adding up the number of conditions the patient reported is a common method for dealing with comorbidity, but assumes that all conditions are weighted equally. Other authors have found a simple count of chronic conditions performed at least as well as the more complex measures (Perkins et al., 2004). Fourth, we had to exclude patients with missing data on depression diagnosis at 24 months from the analysis involving the outcome of depression diagnosis. However, our model under the missing at random assumption adjusts for any bias due to missing data rates that differ between covariates in the study including intervention condition (Little & Rubin, 2002). Therefore, the results are not biased by differential attrition between the intervention and usual care groups. Finally, we cannot rule out the possibility, despite the randomized nature of the study design, that the course of depression symptoms we observed among depressed patients in intervention practices may be due to factors other than the specific effects of a depression management program.
Our results were not wholly consistent with our initial hypotheses. Age, suicidal ideation, number of medical conditions, and marital status were found to be associated with the patterns of evolving depression symptoms. We did not find as we had hypothesized an association of cognitive status with the patterns of evolving depression symptoms. In the examination of cognition more careful assessment of executive function, memory, and attention may be necessary to find a clear association with cognitive measures (Bogner et al., 2007). The lack of significant associations of gender, ethnicity, education, or cognitive status suggests that the effects of these patient-level variables did not appear to influence the patterns of evolving depression symptoms.
Nonetheless, despite limitations our results deserve attention because we attempted to characterize patterns of evolving depression symptoms over 12 months and the association of prognostic factors and outcomes with the patterns of depression symptoms. One point in time is not good enough to understand the heterogeneity of depression, and major depression might only be one identifier of risk of persistent depression. The three patterns of evolving depression symptoms we observed suggest a possible need for more intensive interventions for certain individuals. For patients with a high declining course or a low declining course, the rapid improvements in depression symptoms are maintained after four months. However, for the high persistent course, patients reported a high level of depression symptoms over the twelve month time period. Our results suggest that the PROSPECT intervention increased the number of patients with a high declining course who might have otherwise have had a high persistent course. Identifying patients who will benefit most from a more intensive intervention such as PROSPECT may be key to improving outcomes for depression in primary care.
Married patients were less likely to have a high persistent course compared to a high declining course. Seeking care is often a social process managed by social relationships (e.g., the network-episode model of the pathway to mental health services (Pescosolido & Boyer, 1999)), not a one-time personal cost-benefit analysis. Depressed persons with more extensive and supportive relationships improve more quickly than those who are socially isolated or in conflictful relationships (Alexopoulos, et al., 1996; George, Blazer, Hughes, & Fowler, 1989; Lara, Leader, & Klein, 1997). Patients who are not married patients are at risk for a high persistent course and may need more special attention for improvement of depression symptoms.
Our findings hold particular clinical importance by demonstrating an increased risk of major depression at 24 months among patients with high and persistent depression symptoms. As more is discovered regarding the genetic and neurobiological determinants of major depression, we may be able to more accurately identify predictors of patterns of evolving depression symptoms. In the future, such models may be used to link individual prognostic factors and course of depression symptoms to risk in order to guide treatment. Nevertheless, more intensive or tailored interventions for certain subgroups of patients with high and persistent depression symptoms after four months might potentially have substantial public health impact through reduction of long-term major depression. Identification of older persons at risk for long-term major depression is a crucial step before proposing a dynamic, real-time intervention. Previously we referred to the example of prostate specific antigen in which trajectory of increasing prostate specific antigen is a clinical marker of risk. Knowledge of prognostic factors has changed the use of prostate-specific antigen in clinical practice. Physicians could follow depression symptoms and make better predictions in real time about which patients are most at risk for poor long-term clinical outcomes based on prognostic factors and course of depression. Computerized assessments at routine doctor visits incorporating prescription and electronic medical records could allow estimates of individual risk analogous to the use of prostate-specific antigen for screening and the early deployment of interventions. Identifying vulnerable older primary care patients with delayed or little recovery in depressive symptoms who may lack the resilience of persons with declining depressive symptoms is important in order to identify patients who may be in need of more intensive treatments and referral.
Acknowledgments
FUNDING
This work was supported by the National Institute of Mental Health at the National Institute of Health (grant numbers MH082799, MH047447). Dr. Bogner was supported by the American Diabetes Association (grant number 1-09-CR-07) and the American Heart Association (grant number 0855448D). Dr. Morales was supported by the National Institute of Mental Health at the National Institute of Health (grant number MH073903).
References
- Aikens JE, Kroenke K, Nease DE, Jr, Klinkman MS, Sen A. Trajectories of improvement for six depression-related outcomes. Gen Hosp Psychiatry. 2008;30(1):26–31. doi: 10.1016/j.genhosppsych.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Katz IR, Bruce ML, Heo M, Ten Have T, Raue P, Reynolds CF., 3rd Remission in depressed geriatric primary care patients: a report from the PROSPECT study. Am J Psychiatry. 2005;162(4):718–724. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Feder M, Einhorn A, Rosendahl E. Recovery in geriatric depression. Archives of General Psychiatry. 1996;53:305–312. doi: 10.1001/archpsyc.1996.01830040039008. [DOI] [PubMed] [Google Scholar]
- Andreescu C, Mulsant BH, Houck PR, Whyte EM, Mazumdar S, Dombrovski AY, Reynolds CF., 3rd Empirically derived decision trees for the treatment of late-life depression. Am J Psychiatry. 2008;165(7):855–862. doi: 10.1176/appi.ajp.2008.07081340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard JR, Tracy M, Vlahov D, Galea S. Trajectory and socioeconomic predictors of depression in a prospective study of residents of New York City. Ann Epidemiol. 2008;18(3):235–243. doi: 10.1016/j.annepidem.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Beck A, Brown G, Steer R. Psychometric characteristics of the scale for suicide. Ideation with psychiatric outpatients. Behavior Research and Therapy. 1997;35:1039–1046. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- Bogner HR, Bruce ML, Reynolds CF, 3rd, Mulsant BH, Cary MS, Morales K, Alexopoulos GS. The effects of memory, attention, and executive dysfunction on outcomes of depression in a primary care intervention trial: The PROSPECT study. Int J Geriatr Psychiatry. 2007;22(9):922–929. doi: 10.1002/gps.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogner HR, Cary M, Bruce ML, Reynolds CF, III, Mulsant BH, Ten Have TR, Alexopoulos GS. The role of medical comorbidity in outcome of major depression in primary care: the PROSPECT study. American Journal of Geriatric Psychiatry. 2005;13(10):861–868. doi: 10.1176/appi.ajgp.13.10.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogner HR, de Vries HF, Maulik PK, Unutzer J. Mental health services use: Baltimore epidemiologic catchment area follow-up. Am J Geriatr Psychiatry. 2009;17(8):706–715. doi: 10.1097/JGP.0b013e3181aad5c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce ML, TenHave TR, Reynolds CF, Katz II, Schulberg HC, Mulsant BH, Alexopoulos GS. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. Jama. 2004;291(9):1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- Carter HB, Pearson JD, Metter EJ, Brant LJ, Chan DW, Andres R, Walsh PC. Longitudinal evaluation of prostate-specific antigen levels in men with and without prostate disease. Jama. 1992;267(16):2215–2220. [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE. Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry. 2010;167(5):509–527. doi: 10.1176/appi.ajp.2010.09101452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Disease. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Colman I, Ploubidis GB, Wadsworth ME, Jones PB, Croudace TJ. A longitudinal typology of symptoms of depression and anxiety over the life course. Biol Psychiatry. 2007;62(11):1265–1271. doi: 10.1016/j.biopsych.2007.05.012. [DOI] [PubMed] [Google Scholar]
- Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993;269:2386–2391. [PubMed] [Google Scholar]
- Cui X, Lyness JM, Tang W, Tu X, Conwell Y. Outcomes and predictors of late-life depression trajectories in older primary care patients. Am J Geriatr Psychiatry. 2008;16(5):406–415. doi: 10.1097/JGP.0b013e3181693264. [DOI] [PubMed] [Google Scholar]
- Dew MA, Reynolds CF, 3rd, Houck PR, Hall M, Buysse DJ, Frank E, Kupfer DJ. Temporal profiles of the course of depression during treatment. Predictors of pathways toward recovery in the elderly. Arch Gen Psychiatry. 1997;54(11):1016–1024. doi: 10.1001/archpsyc.1997.01830230050007. [DOI] [PubMed] [Google Scholar]
- Eastham JA, Riedel E, Scardino PT, Shike M, Fleisher M, Schatzkin A, Begg CB. Variation of serum prostate-specific antigen levels: an evaluation of year-to-year fluctuations. Jama. 2003;289(20):2695–2700. doi: 10.1001/jama.289.20.2695. [DOI] [PubMed] [Google Scholar]
- Farmer ME, Kittner SJ, Abbott RD, Wolz MM, Wolf PA, White LR. Longitudinally measured blood pressure, antihypertensive medication use, and cognitive performance: the Framingham Study. Journal of Clinical Epidemiology. 1990;43:475–480. doi: 10.1016/0895-4356(90)90136-d. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gallo JJ, Anthony JC, Muthen BO. Age differences in the symptoms of depression: a latent trait analysis. J Gerontol. 1994;49(6):251–264. doi: 10.1093/geronj/49.6.p251. [DOI] [PubMed] [Google Scholar]
- George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. British Journal of Psychiatry. 1989;154:478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- Gildengers AG, Houck PR, Mulsant BH, Dew MA, Aizenstein HJ, Jones BL, Reynolds CF., 3rd Trajectories of treatment response in late-life depression: psychosocial and clinical correlates. J Clin Psychopharmacol. 2005;25(4 Suppl 1):S8–13. doi: 10.1097/01.jcp.0000161498.81137.12. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology and Neurosurgical Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2009 doi: 10.1111/j.1600-0447.2009.01519.x. [DOI] [PubMed] [Google Scholar]
- Hybels CF, Blazer DG, Pieper CF, Landerman LR, Steffens DC. Profiles of depressive symptoms in older adults diagnosed with major depression: latent cluster analysis. Am J Geriatr Psychiatry. 2009;17(5):387–396. doi: 10.1097/JGP.0b013e31819431ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hybels CF, Pieper CF, Blazer DG, Steffens DC. The course of depressive symptoms in older adults with comorbid major depression and dysthymia. Am J Geriatr Psychiatry. 2008;16(4):300–309. doi: 10.1097/JGP.0b013e318162f15f. [DOI] [PubMed] [Google Scholar]
- Lara ME, Leader J, Klein DN. The association between social support and course of depression: Is it confounded with personality? Journal of Abnormal Personality. 1997;106:478–482. doi: 10.1037//0021-843x.106.3.478. [DOI] [PubMed] [Google Scholar]
- Licht-Strunk E, Van Marwijk HW, Hoekstra T, Twisk JW, De Haan M, Beekman AT. Outcome of depression in later life in primary care: longitudinal cohort study with three years’ follow-up. Bmj. 2009;338:a3079. doi: 10.1136/bmj.a3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little R, Rubin D. Statistical Analysis with Missing Data. 2. New York: John Wiley & Sons; 2002. [Google Scholar]
- Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. [Google Scholar]
- Mulder RT, Joyce PR, Frampton CM, Luty SE, Sullivan PF. Six months of treatment for depression: outcome and predictors of the course of illness. Am J Psychiatry. 2006;163(1):95–100. doi: 10.1176/appi.ajp.163.1.95. [DOI] [PubMed] [Google Scholar]
- Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000a;24(6):882–891. [PubMed] [Google Scholar]
- Muthen BO. Latent variable mixture modeling. In: Marcoulides GA, Schumacker RE, editors. New Developments and Techniques in Structural Equation Modeling. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2001. pp. 1–33. [Google Scholar]
- Muthen BO, Muthen LK. The development of heavy drinking and alcohol-related problems from ages 18 to 37 in a U.S. national sample. J Stud Alcohol. 2000b;61(2):290–300. doi: 10.15288/jsa.2000.61.290. [DOI] [PubMed] [Google Scholar]
- Muthen BO, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Patten SB, Schopflocher D. Longitudinal epidemiology of major depression as assessed by the Brief Patient Health Questionnaire (PHQ-9) Compr Psychiatry. 2009;50(1):26–33. doi: 10.1016/j.comppsych.2008.05.012. [DOI] [PubMed] [Google Scholar]
- Perkins AJ, Kroenke K, Unutzer J, Katon W, Williams JW, Hope C, Callahan CM. Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol. 2004;57(10):1040–1048. doi: 10.1016/j.jclinepi.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Boyer CA. How do people come to use mental health services? Current knowledge and changing perspectives. In: Horwitz AV, Scheid TL, editors. A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. New York, New York: Cambridge University Press; 1999. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rosenstock IM. Enhancing patient compliance with health recommendations. Journal of Pediatric Health Care. 1988;2:67–72. doi: 10.1016/0891-5245(88)90169-1. [DOI] [PubMed] [Google Scholar]
- Rost K, Pyne JM, Dickinson LM, LoSasso AT. Cost-effectiveness of enhancing primary care depression management on an ongoing basis. Ann Fam Med. 2005;3(1):7–14. doi: 10.1370/afm.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for Axis I DSM-IV Disorders (SCID) Washington, D.C: American Association Press, Inc; 1995. [Google Scholar]
- Stulz N, Thase ME, Klein DN, Manber R, Crits-Christoph P. Differential effects of treatments for chronic depression: a latent growth model reanalysis. J Consult Clin Psychol. 2010;78(3):409–419. doi: 10.1037/a0019267. [DOI] [PubMed] [Google Scholar]
- Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the national comorbidity survey. Am J Psychiatry. 1998;155(10):1398–1406. doi: 10.1176/ajp.155.10.1398. [DOI] [PubMed] [Google Scholar]
- Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40(9):922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. The National Institute of Mental Health Strategic Plan (Publication No. 08-6368) Washington, D.C: Government Printing Office; 2008. [Google Scholar]
- Voils CI, Steffens DC, Flint EP, Bosworth HB. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. Am J Geriatr Psychiatry. 2005;13(2):157–165. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]