Abstract
Antibody therapies to prevent or limit filovirus infections have received modest interest in recent years, in part because of early negative experimental evidence. We have overcome the limitations of this approach, leveraging the use of antibody from nonhuman primates (NHPs) that survived challenge to filoviruses under controlled conditions. By using concentrated, polyclonal IgG antibody from these survivors, we treated filovirus-infected NHPs with multiple doses administered over the clinical phase of disease. In the first study, Marburg virus (MARV)-infected NHPs were treated 15 to 30 min postexposure with virus-specific IgG, with additional treatments on days 4 and 8 postexposure. The postexposure IgG treatment was completely protective, with no signs of disease or detectable viremia. MARV-specific IgM antibody responses were generated, and all macaques survived rechallenge with MARV, suggesting that they generated an immune response to virus replication. In the next set of studies, NHPs were infected with MARV or Ebola virus (EBOV), and treatments were delayed 48 h, with additional treatments on days 4 and 8 postexposure. The delayed treatments protected both MARV- and EBOV-challenged NHPs. In both studies, two of the three IgG-treated NHPs had no clinical signs of illness, with the third NHP developing mild and delayed signs of disease followed by full recovery. These studies clearly demonstrate that postexposure antibody treatments can protect NHPs and open avenues for filovirus therapies for human use using established Food and Drug Administration-approved polyclonal or monoclonal antibody technologies.
Keywords: passive antibody, polyclonal antibody, therapeutic agent, hemorrhagic fever virus
Marburg virus (MARV) and Ebola virus (EBOV), from the family Filoviridae, cause acute and frequently fatal hemorrhagic fever in humans and nonhuman primates (NHPs) and are considered among the deadliest infectious agents known to humans (1–3). Because of this high lethality and the increasing frequency of outbreaks, filoviruses pose significant emerging disease risks in sub-Saharan Africa and are considered important biological threats. Currently, there are no preventive vaccines or postexposure treatment options approved for use in humans, making the development of such products a high priority.
The use of antibodies as a postexposure treatment for hemorrhagic fever virus infection has met with mixed success. Passive transfer of serum collected from survivors of Junin virus or Lassa virus has proven effective provided treatments are initiated soon after infection (4–6). However, antibody passive transfer experiments have been largely unsuccessful in treating filovirus infections (7). During a 1995 outbreak of EBOV in Kikwit, Democratic Republic of the Congo, seven of eight patients who exhibited symptoms and detectable EBOV antigen in their blood survived disease after treatment with whole blood from convalescent EBOV survivors (8). The lethality rate (12.5%) from this treatment was significantly lower than the overall case fatality rate for the outbreak (80%); however, interpreting the role of antibodies in the achieved protection is complicated because the patients received whole blood, not just antibodies, in addition to supportive care in a hospital setting. After the 1995 outbreak, the World Health Organization procured a commercially available equine IgG product produced from horses hypervaccinated with EBOV for potential use in humans (9). Initial success was achieved by using similar IgG preparations in hamadryas baboons, in which the equine IgG was protective against lethal EBOV challenge (10–12). In contrast, cynomolgus macaques receiving the commercially available equine IgG product did not survive challenge with EBOV, although the onsets to clinical signs and viremia, and time to death, were delayed relative to controls (9, 13). From these studies, it appeared that the antibody was able to control viremia while present, but when the antibody had been depleted, presumably by complexing with virus or immune clearance because of its heterologous nature, the disease progressed unabated. A second line of research with a single human monoclonal antibody, KZ52, was found to be a potent in vitro neutralizing antibody and protective in guinea pigs (14, 15); however, KZ52 failed to protect NHPs against EBOV (16).
All these preceding studies suffered from one or more of the following limitations. In some cases, antibody treatments were not species-matched, which limited their duration in circulation and may have contributed to the lack of virus clearance. Supporting the notion that species-matched antibodies can control filovirus infections are studies demonstrating protection in mice against mouse-adapted EBOV with the use of homologous polyvalent immune serum (17) or monoclonal antibodies against Ebola glycoprotein (18). In the case of KZ52, all antibody was directed toward a single epitope, which was unable to slow viral replication in infected macaques. In addition, the antibody treatments were often delivered as a single bolus, limiting the quantity and duration of available antibody. For these reasons, we hypothesized that multiple administrations of concentrated, species-matched polyclonal IgG would protect NHPs against filovirus challenge. To test this, we performed a series of passive transfer experiments in rhesus macaques by using polyclonal, species-matched, virus-specific IgG obtained from a large quantity of convalescent serum from vaccinated rhesus macaques that subsequently survived challenge with a lethal dose of filovirus.
Results
Generation, Fractionation, and Characterization of Polyclonal IgG.
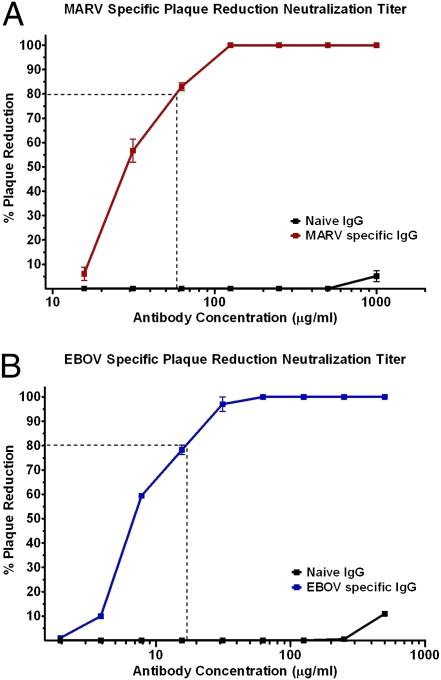
Polyclonal IgG was purified from a large preparation of convalescent serum pooled from vaccinated macaques that subsequently survived challenge with a lethal dose of filovirus. Serum was collected by exsanguinations of NHPs at the termination of successful vaccination and challenge studies. The serum was irradiated, safety-tested, and removed from the Biosafety Level 4 environment. The serum was then pooled and fractionated to separate and concentrate the IgG. The fractionated IgG was evaluated and shown to have virus-neutralizing activity (Fig. 1).
Fig. 1.
Filovirus-specific plaque-reduction neutralization titers of fractionated IgG. (A) MARV-specific or (B) EBOV-specific plaque-reduction neutralization titration of fractionated IgGs. Twofold serial dilutions of fractionated IgG was mixed with 100 pfu of (A) MARV or (B) EBOV at 37 °C for 1 h and used to infect Vero cells. Neutralization titers were determined, in duplicate, to be the last dilution of serum that reduced the number of plaques by 80% compared with control wells. Error bars indicate SEM in replicate experiments.
Polyclonal IgG Initiated 15 to 30 min Postexposure Provides Complete Protection of NHPs Challenged with MARV.
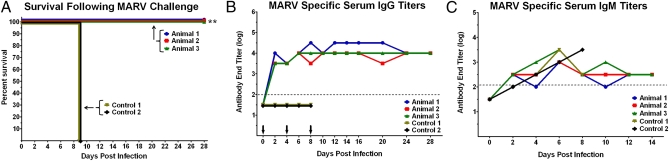
In the first study, five naive rhesus macaques were challenged by i.m. injection with a target dose of 1,000 pfu of MARV (Fig. 2). In the three experimental macaques, MARV-specific IgG treatment was initiated within 15 to 30 min. The other two macaques received nonspecific fractionated IgG (control 1) or PBS solution (control 2) as a treatment. Additional doses of treatment were given 4 and 8 d after challenge. The MARV-specific IgG provided 100% protection, with no observed clinical signs of disease or detectable viremia (Table 1, study 1; Fig. 2A; and Fig. S1), whereas the control macaques died with classical signs of filovirus hemorrhagic fever. To assess MARV-specific antibody levels and to determine if these NHPs were generating an adaptive immune response to the MARV infection, we performed ELISA on serum to measure MARV-specific IgM and IgG levels after infection. After IgG treatment, MARV-specific serum IgG levels were increased and remained so compared with their individual pretreatment titers (Fig. 2B). In addition, MARV-specific IgM responses were observed by day 4 and day 6 after challenge, which could only be attributed to the NHPs’ intrinsic immune response (Fig. 2C).
Fig. 2.
Percent survival and MARV specific antibody titers in NHPs treated 15 to 30 min after infection with MARV. (A) Percent survival following MARV challenge (**P < 0.01, Fisher exact test). MARV-specific (B) IgG and (C) IgM. Serum collected from NHPs at indicated days postinfection was analyzed by ELISA against whole irradiated MARV antigen. MARV-specific antibody end titers are reported. Dotted line indicates assay limit of detection. Arrows indicate IgG treatment days.
Table 1.
Rhesus macaques treated with 70–100 mg/kg of fractionated IgG after parenteral filovirus challenge
| Animal | Adverse events on days 1–28 after challenge | Status |
| Study 1: Macaques challenged with 1,000 pfu MARV; treatment initiated ∼15–30 min after challenge | ||
| Animal 1 | No clinical signs, no viremia | Survived |
| Animal 2 | Fever (day 8), no viremia | Survived |
| Animal 3 | No clinical signs, no viremia | Survived |
| Control 1* | Anorexia (day 8–9), depression (day 8–9), viremia (day 4, 6, 8), lymphopenia (day 4–6), >fivefold increase in ALT/AST (day 8) | Died, day 9 |
| Control 2† | Anorexia (day 8–9), depression (day 8–9), viremia (day 4, 6, 8, 9), lymphopenia (day 4–6), >fivefold increase in ALT/AST (day 8–9), hypothermia (day 9) | Died, day 9 |
| Control 3† | Fever (day 5), anorexia (day 8), depression (day 7–8), viremia (day 7, 8), lymphopenia (day 5, 7), more than fivefold increase in ALT/AST (day 7, 8), widespread rash (day 7–8), hypothermia (day 8) | Died, day 8 |
| Study 2: Macaques challenged with 1,000 pfu MARV; treatment initiated 48 h after challenge | ||
| Animal 4 | No clinical signs, no viremia | Survived |
| Animal 5 | No clinical signs, no viremia | Survived |
| Animal 6 | Fever (day 6, 10, 12), depression (day 10–12), lymphopenia (day 10), viremia (day 12, 14), >fivefold increase in ALT/AST (day 10, 12, 14, 16) | Survived |
| Control 4† | Fever (day 8), moderate rash (day 10), anorexia (day 9–10), depression (day 8–10), viremia (day 6, 8, 10), lymphopenia (day 6), more than fivefold increase in ALT/AST (day 8, 10) | Died, day 10 |
| Study 3: Macaques challenged with 1,000 pfu EBOV; treatment initiated 48 h after challenge | ||
| Animal 7 | Thrombocytopenia (day 6), no viremia | Survived |
| Animal 8 | Fever (day 6, 8, 10), thrombocytopenia (day 6), lymphopenia (day 12), no viremia, two- to threefold increase in AST (day 12, 14, 16) | Survived |
| Animal 9 | Thrombocytopenia (day 6), no viremia | Survived |
| Control 5† | Fever (day 4, 6), anorexia (day 6–8), depression (day 6–8), thrombocytopenia (day 6, 8) lymphopenia (day 6, 8), viremia (day 4, 6, 8), more than fivefold increase in ALT/AST (day 6, 8), mild rash (day 8) | Died, day 8 |
Fever was defined as a body temperature reading 1.5 °C greater than baseline. Depression and anorexia were subjectively assessed. Lymphopenia was defined as at least a 35% reduction in numbers of lymphocytes below a baseline of 3,000 cells/mL. Thrombocytopenia was defined as at least a 35% reduction in numbers of platelets. Rash was defined as mild (barely visible) or widespread petechia. Hypothermia was defined as a body temperature decrease of 4 °C below baseline. AST, aspartate aminotransferase; ALT, alanine aminotransferase.
*Given nonspecific IgG.
†Given PBS instead of EBOV-specific IgG.
To determine if these NHPs were infected to the extent that protective immune responses were generated, the survivors were rechallenged with MARV 77 d after the initial infection. These NHPs showed endogenous IgG responses to the challenge and displayed no clinical signs of disease or detectable viremia (Fig. S2). This indicates that, although the IgG treatment controlled and cleared the initial filovirus infection, sufficient virus was seen systemically to generate immune memory responses that were protective against subsequent rechallenge.
MARV-Infected NHPs Survive Infection When Administered Polyclonal IgG 48 h Postchallenge.
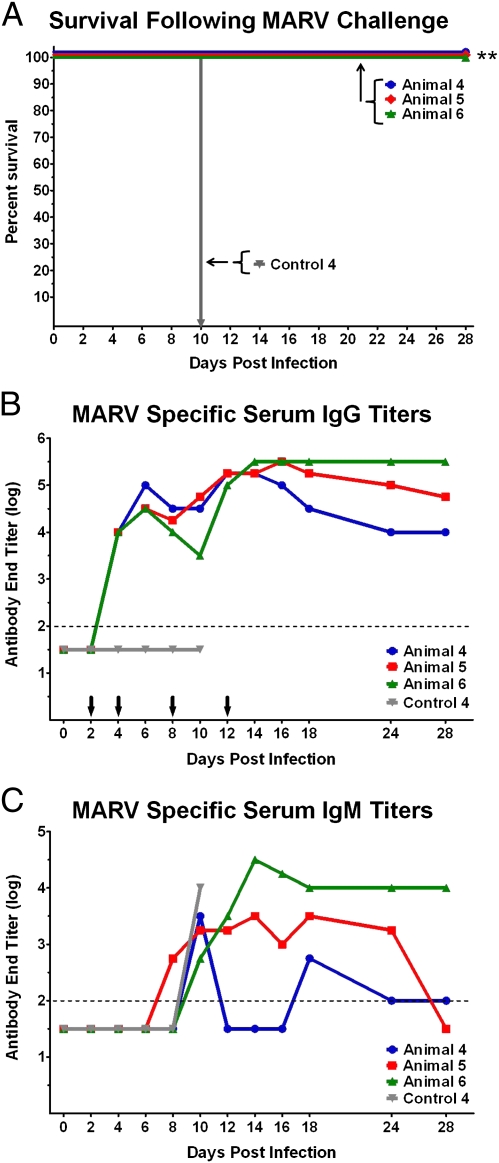
Given these encouraging results, we initiated a second NHP MARV study in which we expanded the therapeutic window. Four naive rhesus macaques were challenged as described earlier, but the initial IgG treatment was delayed for 48 h in the experimental macaques (Fig. 3). The one control macaque received PBS solution. All experimental NHPs received additional IgG doses on day 4 and 8 postinfection, with an additional dose delivered on day 12 to one NHP that displayed clinical signs of disease (Table 1, animal 6). Even with the delayed start of treatment, the NHPs were protected from lethal infection, with two of the three NHPs showing no clinical signs of disease (Table 1, study 2; and Fig. 3A). The one treated macaque that did develop clinical signs of disease differed from the control macaque in that the specific signs of MARV infection (increased liver enzyme levels and low level viremia) were delayed and much less severe (Fig. S3). This animal fully recovered from all signs of disease and was nonviremic by day 16 (Fig. S3D). In agreement with our initial experiment, MARV-specific serum IgG titers increased after IgG delivery (Fig. 3B). Of note, all NHPs developed MARV-specific IgM titers, again suggesting that an intrinsic immune response was generated (Fig. 3C).
Fig. 3.
Percent survival and MARV-specific antibody titers in NHPs treated 48 h postinfection with MARV. (A) Percent survival following MARV challenge (**P < 0.01, Fisher exact test). MARV-specific (B) IgG and (C) IgM. Serum collected from NHPs at indicated days postinfection was analyzed by ELISA against whole irradiated MARV antigen. MARV-specific antibody end titers are reported. Dotted line indicates assay limit of detection. Arrows indicate IgG treatment days.
Polyclonal IgG Given 48 h After EBOV Challenge Provides Complete Protection in NHP.
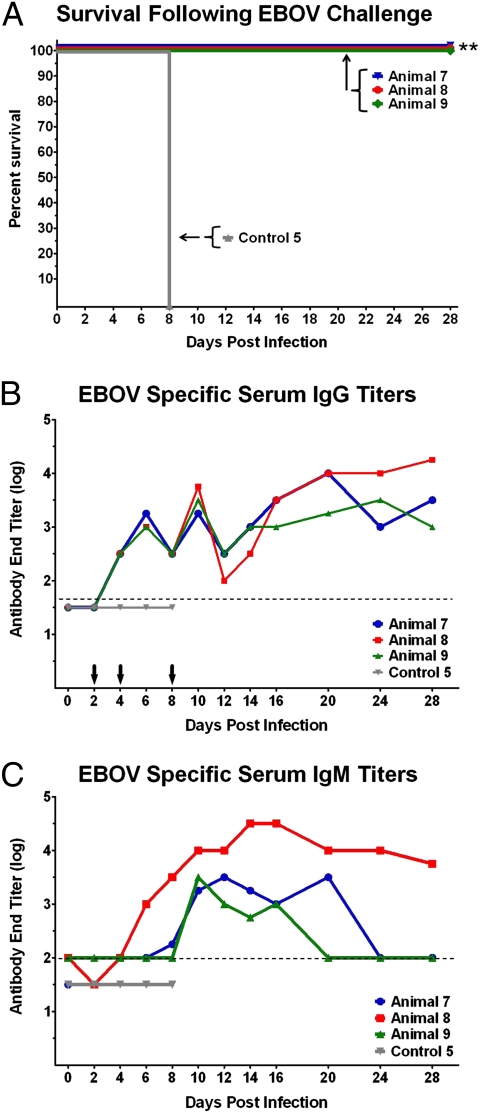
To assess the ability of antibody to protect NHPs against EBOV infection, we completed a final study in which four naive rhesus macaques were challenged i.m. with a target dose of 1,000 pfu of EBOV and IgG treatment was initiated 48 h after challenge in three of these macaques (Fig. 4). Additional IgG treatments were given on days 4 and 8 postexposure. The one control macaque received PBS solution. The IgG used for the third study was fractionated from serum collected from convalescent rhesus macaques that had been vaccinated with a multivalent filovirus vaccine (EBOV and MARV) and survived challenged with EBOV. This filovirus-specific IgG preparation had EBOV-specific and MARV-specific antibodies (Fig. 5A) and neutralization capacity against EBOV (Fig. 1B). The three macaques treated with IgG survived challenge, with two NHPs showing thrombocytopenia as the only sign of disease (Table 1, animals 7 and 9) and one macaque (Table 1, animal 8) showing mild to moderate signs of disease (fever, thrombocytopenia, lymphopenia, two- to threefold increase in aspartate aminotransferase level; Table 1, study 3; Fig. 4A; and Fig. S4). Although IgG serum titers in animal 8 decreased on day 12, the IgM responses seen at that time indicate an active immune response against infection (Fig. 4 B and C). As expected, the control macaque (control 5) died with classic signs of FHF on day 8 postexposure (Table 1, study 3).
Fig. 4.
Percent survival and EBOV specific antibody titers in NHPs treated 48 h postinfection with EBOV. (A) Percent survival following EBOV challenge (**P < 0.01, Fisher exact test). EBOV-specific (B) IgG and (C) IgM. Serum collected from NHPs at indicated days postinfection was analyzed by ELISA against whole irradiated EBOV antigen. EBOV-specific antibody end titers are reported. Dotted line indicates assay limit of detection. Arrows indicate IgG treatment days.
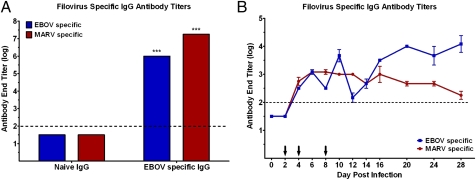
Fig. 5.
Filovirus-specific IgG antibody titers. (A) EBOV- and MARV-specific IgG antibody titers of IgGs. Fractionated naive IgG and EBOV-specific IgG was analyzed by ELISA against whole irradiated EBOV (blue) or MARV (red) antigen. Antibody end titers are reported. Error bars indicate SEM in replicate experiments (***P < 0.001, two-way ANOVA). (B) EBOV- and MARV-specific serum IgG antibody titers after EBOV infection. Serum collected from NHPs at indicated days after infection was analyzed by ELISA against whole irradiated EBOV (blue) or MARV (red) antigen. Filovirus specific antibody end titers are reported. Error bars indicate SEM of three experimental NHPs. Dotted line indicates assay limit of detection. Arrows indicate IgG treatment days.
Discussion
In the present studies, we have demonstrated that passively transferred species-matched, polyclonal IgG provided complete protection in filovirus-challenged NHPs. This protection was observed even when the IgG was initiated as late as 48 h after filovirus infection. The success with IgG treatments in our studies, compared with past studies with antibody-based efforts, may be attributed to two important factors–the polyclonal nature of the exogenous antibodies controlled virus infection and the multiple treatments maintained sufficiently high levels of IgG until the host's adaptive immune responses could be recruited to help clear the viral infection. This was not the case in studies that used the monoclonal anti-EBOV KZ52, in which virus infection progressed despite high levels of KZ52 in circulation (16), and in equine IgG studies in which EBOV-specific antibody levels in the blood could not be maintained beyond 7 to 8 d postexposure as a result of clearance of the heterologous equine IgG (9, 13).
Our use of IgG that contained EBOV-specific and MARV-specific antibodies in the EBOV challenge experiment provides some insight into antibody clearance, which appears to be in response to replicating virus. On closer examination of EBOV and MARV IgG levels from the IgG-treated EBOV-challenged NHPs, an interesting dynamic occurs between days 6 and 20 (Fig. 5B). As previously mentioned, the IgG used in this study was isolated from NHPs that were vaccinated against EBOV and MARV and contained antibody specific for both filoviruses. Analysis on day-6 and day-10 serum samples showed significant increases in EBOV-specific IgG titers that then decreased by the next sampling day (day 8 and day 12). Interestingly, the MARV-specific IgG titers remained relatively constant throughout the study, suggesting that the EBOV-specific IgG was perhaps being depleted by replicating EBOV. Analysis performed on later serum samples taken on days 14, 16, and 20 showed a different dynamic whereby EBOV-specific IgG titers increased without additional IgG treatments, whereas MARV-specific IgG titers gradually waned, suggesting IgG was being endogenously produced.
These results support the need to reconsider antibody therapeutic agents as an effective means of treating filovirus infections. In the recent past, experimental postexposure treatments for filovirus infections have included hyperimmune equine IgG (9), EBOV-specific human monoclonal IgG antibody (16), whole-blood transfusions from convalescent survivors (8), recombinant IFN (13), recombinant nematode anticoagulant protein C2 (19), recombinant human activated protein C (20, 21), recombinant vesicular stomatitis virus vectors (22–25), siRNAs (26), and phosphorodiamidate morpholino oligomers (27). A summary of these efforts is detailed in Table 2. The majority of these studies were completed in rhesus macaques and treatments were typically initiated within 30 to 60 min after parenteral filovirus challenge. Aside from the IgG treatment presented here, in only two of these studies were treatments initiated after the day of exposure, and only in the MARV recombinant vesicular stomatitis virus vector vaccine study was the treatment delayed as late as 48 h after exposure (22). These studies were partially successful, with survival rates of 33% in both studies. The results described in the present study are thus quite remarkable: 100% protection against MARV or EBOV infection was afforded in rhesus macaques even when treatment was delayed as late as 48 h postinfection.
Table 2.
Historic postexposure treatments for filoviruses and outcome
| Virus | Treatment1 | Macaque species | Initiation of treatment | Outcome, % survival | Source |
| EBOV | Equine IgG | Cynomolgus | Day 0 | 0, 0 | 9, 13 |
| EBOV | Whole-blood transfusions | Rhesus | Day 0 | 0 | 7 |
| EBOV | hMAb | Rhesus | Day −1 | 0 | 18 |
| EBOV | rIFN | Cynomolgus | Day 0 | 0 | 13 |
| EBOV | rNAPc2 | Rhesus | 10 min | 33 | 19 |
| 24 h | 33 | ||||
| EBOV | rVSV vaccine | Rhesus | 20–30 min | 50 | 22 |
| EBOV | rhAPC | Rhesus | 30–60 min | 18 | 20 |
| EBOV | siRNA-SNALPs | Rhesus | 30 min | 67–100 | 26 |
| EBOV | PMOplus | Rhesus | 30–60 min | 63 | 27 |
| EBOV | Rhesus IgG | Rhesus | 48 h | 100 | Present study |
| MARV | rNAPc2 | Rhesus | Day 0 | 18 | 21 |
| MARV | rVSV vaccine | Rhesus | 20–30 min | 100 | 23 |
| 24 h | 83 | 24 | |||
| 48 h | 33 | ||||
| MARV | PMOplus | Cynomolgus | 30–60 min | 100 | 27 |
| MARV | Rhesus IgG | Rhesus | 15–30 min | 100 | Present study |
| 48 h | 100 | ||||
| SUDV | rVSV vaccine | Rhesus | 20–30 min | 100 | 25 |
hMAb, EBOV-specific human monoclonal IgG1 monoclonal antibody vaccine; PMOplus, phosphorodiamidate morpholino oligomers; rhAPC, recombinant human activated protein C vaccine; rhesus IgG, fractionated IgG from convalescent serum from rhesus macaques; rIFN, recombinant IFN vaccine; rNAPc2, recombinant nematode anticoagulant protein C2 vaccine; rVSV, recombinant vesicular stomatitis virus vectored vaccine; siRNA-SNALPs, siRNAs in stable nucleic acid-lipid particles.
Polyclonal serum and monoclonal IgG are well established technologies of which multiple products have received Food and Drug Administration approval (28). The series of studies presented in this article provide a proof of concept that therapy based on antibodies can be used as an effective treatment for filovirus infections. This opens the prospect for development of human polyclonal antibody serum or a mixture of agent specific monoclonal antibodies.
Materials and Methods
Viruses.
The challenge viruses, EBOV (Zaire, Kikwit strain) (29) and MARV (Ci67) (30), were specific challenge stocks developed at the US Army Medical Research Institute of Infectious Diseases (USAMRIID).
Generation and Fractionation of Polyclonal IgG.
Polyclonal IgG used in all experiments was collected from macaques that were vaccinated with viral-vectored vaccine candidates and challenged 28 d later with filovirus. Surviving NHPs were exsanguinated before euthanasia. Serum was collected from blood and pooled into large batches determined by virus challenge, either MARV or EBOV. Serum was irradiated by gamma irradiation at approximately 6 million radiation units and safety tested by plaque assay on Vero cells to demonstrate no detectable live virus. Large batches of serum were shipped to AI Biotech (Richmond, VA) for fractionation. Polyclonal IgG was fractionated in protein G columns and suspended in PBS solution with final pH 7.4. For the first MARV study, the fractionated IgG contained an endotoxin level of 9.79 EU/mg of protein and was assessed to be 81% and 94% pure by nonreduced and reduced SDS-PAGE, respectively. The IgG used in the second MARV study contained an endotoxin level of 9.27 EU/mg of protein and was assessed to be 89% and 97% pure by nonreduced and reduced SDS-PAGE, respectively. For the EBOV study, the fractionated IgG contained an endotoxin level of 7.54 EU/mg of protein and was assessed to be 96% pure by nonreduced and reduced SDS-PAGE. Plaque-reduction neutralization assay was performed as previously described (31).
Animal Studies.
Fourteen (3–5 kg) rhesus macaques (Macaca mulatta) were used for these studies. In all animal challenge studies, the target dose of the virus was 1,000 pfu. The i.v. antibody treatments were administered to the macaques as a slow bolus via the saphenous vein.
For the first MARV study, experimental animals received three doses of 100 mg/kg given at 15 to 30 min, 4 d, and 8 d posexposure. The first dose was partitioned into three equal treatments and given by three different routes of administration (one third of the dose given i.m. 1 inch from infection site, one third of the dose given i.p., and one third of the dose given i.v.). The remaining two doses were given i.v. on 4 d and 8 d postinfection. For this study there were two control NHPs; one that received PBS solution and one that received IgG fractionated from naive NHP serum as sham treatments. The controls received equal volumes of sham treatment on an animal weight basis on the same treatment days as those doses given to the experimental animals. For the back challenge of the survivors from this MARV experiment, an additional filovirus-naive control was used. These NHPs were challenged i.m. with 1,000 pfu of MARV 77 d after the original challenge with MARV.
In the second MARV study (48 h postinfection), naive NHPs were challenged i.m. with 1,000 pfu of MARV. Experimental animals were provided a primary i.v. dose of 100 mg/kg of IgG at 48 h postinfection, with additional i.v. doses at 4 d and 8 d postinfection. One NHP received an additional i.v. treatment on day 12 after infection because it was showing signs of disease and had of lower levels of filovirus-specific IgG on day 10. The control animal received equal volumes of PBS solution as a sham treatment at the same treatment times as the experimental animals.
In the EBOV study (48 h postexposure), naive NHPs were challenged i.m. with 1,000 pfu of EBOV. Experimental animals were provided a primary i.v. dose of 80 mg/kg of IgG at 48 h postinfection, with additional i.v. doses at 4 d and 8 d postinfection. The control animal received equal volumes of PBS solution as a sham treatment at the same treatment times as the experimental animals.
All NHPs were monitored closely for 28 d following challenge. Because of ethical considerations stemming from the near-universal lethality of infection and as is standard practice for NHP studies with filoviruses, historical controls were sometimes used to limit the number of NHPs required. In these studies, all control animals died from filovirus challenge within the normal time to death. All challenge studies were conducted under maximum containment in an animal Biosafety Level 4 facility at USAMRIID and were approved by the USAMRIID Institutional Animal Care and Use Committee. Animal research was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals, and experiments involving animals and adhered to the principles stated in the Guide for the Care and Use of Laboratory Animals. The facility is fully accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care International.
Statistical Analysis.
Prism software (GraphPad) was used to graph and make statistical comparisons of all data.
Supplementary Material
Acknowledgments
The authors thank AI Biotech (Richmond, VA) for purification of IgG; Steven Bradfute (Arizona State University) and Kartik Chandran (Albert Einstein College of Medicine) for reviewing the manuscript; Gene Olinger [USAMRIID)] for providing the animal protocol for the initial MARV challenge; Jay Wells and Brian Hannah (USAMRIID), Keith Reimann (Harvard Medical School), and Alan Schmaljohn (University of Maryland) for helpful discussions on experimental design; and Josh Moore, Mike Winpigler, and Jimmy Fiallos (USAMRIID) for assisting with animal treatments. This work was supported by Defense Threat Reduction Agency Project CBM.THRV.01.RD.11.001. Opinions, conclusions, interpretations, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army.
Footnotes
The authors declare no conflict of interest.
*This Direct Submission article had a prearranged editor.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1200409109/-/DCSupplemental.
References
- 1.Kuhn JH, Jahrling PB. Clarification and guidance on the proper usage of virus and virus species names. Arch Virol. 2010;155:445–453. doi: 10.1007/s00705-010-0600-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anonymous Ebola haemorrhagic fever in Zaire, 1976. Bull World Health Organ. 1978;56:271–293. [PMC free article] [PubMed] [Google Scholar]
- 3.Anonymous Ebola haemorrhagic fever in Sudan, 1976. Report of a WHO/International Study Team. (Translated from eng) Bull World Health Organ. 1978;56:247–270. [PMC free article] [PubMed] [Google Scholar]
- 4.Enria DA, Briggiler AM, Fernandez NJ, Levis SC, Maiztegui JI. Importance of dose of neutralising antibodies in treatment of Argentine haemorrhagic fever with immune plasma. Lancet. 1984;2:255–256. doi: 10.1016/s0140-6736(84)90299-x. [DOI] [PubMed] [Google Scholar]
- 5.Jahrling PB, Peters CJ. Passive antibody therapy of Lassa fever in cynomolgus monkeys: importance of neutralizing antibody and Lassa virus strain. Infect Immun. 1984;44:528–533. doi: 10.1128/iai.44.2.528-533.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jahrling PB, Frame JD, Rhoderick JB, Monson MH. Endemic Lassa fever in Liberia. IV. Selection of optimally effective plasma for treatment by passive immunization. Trans R Soc Trop Med Hyg. 1985;79:380–384. doi: 10.1016/0035-9203(85)90388-8. [DOI] [PubMed] [Google Scholar]
- 7.Jahrling PB, Geisbert JB, Swearengen JR, Larsen T, Geisbert TW. Ebola hemorrhagic fever: Evaluation of passive immunotherapy in nonhuman primates. J Infect Dis. 2007;196(suppl 2):S400–S403. doi: 10.1086/520587. [DOI] [PubMed] [Google Scholar]
- 8.Mupapa K, et al. International Scientific and Technical Committee Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. J Infect Dis. 1999;179(suppl 1):S18–S23. doi: 10.1086/514298. [DOI] [PubMed] [Google Scholar]
- 9.Jahrling PB, et al. Passive immunization of Ebola virus-infected cynomolgus monkeys with immunoglobulin from hyperimmune horses. Arch Virol Suppl. 1996;11:135–140. doi: 10.1007/978-3-7091-7482-1_12. [DOI] [PubMed] [Google Scholar]
- 10.Krasnianskiĭ VP, et al. [The isolation of hyperimmune horse serum to the Ebola virus] Vopr Virusol. 1994;39:91–92. [PubMed] [Google Scholar]
- 11.Borisevich IV, et al. [Development and study of the properties of immunoglobulin against Ebola fever] Vopr Virusol. 1995;40:270–273. [PubMed] [Google Scholar]
- 12.Mikhaĭlov VV, Borisevich IV, Chernikova NK, Potryvaeva NV, Krasnianskiĭ VP. [The evaluation in hamadryas baboons of the possibility for the specific prevention of Ebola fever] Vopr Virusol. 1994;39:82–84. [PubMed] [Google Scholar]
- 13.Jahrling PB, et al. Evaluation of immune globulin and recombinant interferon-alpha2b for treatment of experimental Ebola virus infections. J Infect Dis. 1999;179(suppl 1):S224–S234. doi: 10.1086/514310. [DOI] [PubMed] [Google Scholar]
- 14.Maruyama T, et al. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol. 1999;73:6024–6030. doi: 10.1128/jvi.73.7.6024-6030.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parren PW, Geisbert TW, Maruyama T, Jahrling PB, Burton DR. Pre- and postexposure prophylaxis of Ebola virus infection in an animal model by passive transfer of a neutralizing human antibody. J Virol. 2002;76:6408–6412. doi: 10.1128/JVI.76.12.6408-6412.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oswald WB, et al. Neutralizing antibody fails to impact the course of Ebola virus infection in monkeys. PLoS Pathog. 2007;3:e9. doi: 10.1371/journal.ppat.0030009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta M, Mahanty S, Bray M, Ahmed R, Rollin PE. Passive transfer of antibodies protects immunocompetent and imunodeficient mice against lethal Ebola virus infection without complete inhibition of viral replication. J Virol. 2001;75:4649–4654. doi: 10.1128/JVI.75.10.4649-4654.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson JA, et al. Epitopes involved in antibody-mediated protection from Ebola virus. Science. 2000;287:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- 19.Geisbert TW, et al. Treatment of Ebola virus infection with a recombinant inhibitor of factor VIIa/tissue factor: A study in rhesus monkeys. Lancet. 2003;362:1953–1958. doi: 10.1016/S0140-6736(03)15012-X. [DOI] [PubMed] [Google Scholar]
- 20.Hensley LE, et al. Recombinant human activated protein C for the postexposure treatment of Ebola hemorrhagic fever. J Infect Dis. 2007;196(suppl 2):S390–S399. doi: 10.1086/520598. [DOI] [PubMed] [Google Scholar]
- 21.Geisbert TW, et al. Marburg virus Angola infection of rhesus macaques: Pathogenesis and treatment with recombinant nematode anticoagulant protein c2. J Infect Dis. 2007;196(suppl 2):S372–S381. doi: 10.1086/520608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feldmann H, et al. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 2007;3:e2. doi: 10.1371/journal.ppat.0030002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daddario-DiCaprio KM, et al. Postexposure protection against Marburg haemorrhagic fever with recombinant vesicular stomatitis virus vectors in non-human primates: an efficacy assessment. Lancet. 2006;367:1399–1404. doi: 10.1016/S0140-6736(06)68546-2. [DOI] [PubMed] [Google Scholar]
- 24.Geisbert TW, et al. Postexposure treatment of Marburg virus infection. Emerg Infect Dis. 2010;16:1119–1122. doi: 10.3201/eid1607.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Geisbert TW, et al. Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J Virol. 2008;82:5664–5668. doi: 10.1128/JVI.00456-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Geisbert TW, et al. Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: A proof-of-concept study. Lancet. 2010;375:1896–1905. doi: 10.1016/S0140-6736(10)60357-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Warren TK, et al. Advanced antisense therapies for postexposure protection against lethal filovirus infections. Nat Med. 2010;16:991–994. doi: 10.1038/nm.2202. [DOI] [PubMed] [Google Scholar]
- 28.Waldmann TA. Immunotherapy: Past, present and future. Nat Med. 2003;9:269–277. doi: 10.1038/nm0303-269. [DOI] [PubMed] [Google Scholar]
- 29.Geisbert TW, et al. Pathogenesis of Ebola hemorrhagic fever in cynomolgus macaques: Evidence that dendritic cells are early and sustained targets of infection. Am J Pathol. 2003;163:2347–2370. doi: 10.1016/S0002-9440(10)63591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Slenczka WG. The Marburg virus outbreak of 1967 and subsequent episodes. Curr Top Microbiol Immunol. 1999;235:49–75. doi: 10.1007/978-3-642-59949-1_4. [DOI] [PubMed] [Google Scholar]
- 31.Dias JM, et al. A shared structural solution for neutralizing ebolaviruses. Nat Struct Mol Biol. 2011;18:1424–1427. doi: 10.1038/nsmb.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.