Introduction
Emergency Department (ED) use represents an important indicator of asthma morbidity because it is associated with frequent asthma exacerbations. The frequency of ED visits may reflect inadequate disease management skills by the family, or long-term asthma management that deviates from guideline-based care.1 National epidemiological data indicate significant disparities in ED use for asthma, with Latinos and Blacks in the Northeastern US demonstrating particularly high rates of ED use, even when key socio-demographic indicators, such as poverty and insurance status are controlled.2, 3 However, few studies have investigated the factors that may account for these disparities. A number of general factors have been associated with higher rates of overall ED use among children with asthma, including poverty,4, 5 young age,6 asthma severity,2, 5 low inhaled corticosteroid (ICS) use5, 7 and poor environmental control.8 Frequent ED use has also been associated with health system factors such as lack of a usual source of care,5 lack of access to a specialist, poor continuity with a primary care provider,9 and having public insurance.10 Many of these factors traditionally associated with lower socioeconomic and minority status may explain the disparities in ED use observed among Latino and Black children with asthma.
In previously reported data from the Rhode Island Puerto Rico Asthma Center (RIPRAC) we showed that island Puerto Ricans had significantly higher rates of ED use than non Latino whites (NLWs) and Latinos (Puerto Ricans and Dominicans) living in Rhode Island (RI). This difference was striking, because island Puerto Ricans had similar asthma control to NLWs and milder severity than RI, Dominicans, Puerto Ricans and NLWs, while no differences in severity between these three groups were observed in RI.11 We speculated that these findings could be due in part due to differences across sites in the health care system, but did not present empirical evidence to evaluate this hypothesis. However, in this study, we did not focus on ED use or health care context factors, such as insurance status and source of care.
In this paper, we build on our previous results11 to empirically examine the extent to which differences in individual/family factors (i.e. asthma control, parental perception of asthma severity, medication concerns) and health system factors (public vs. private insurance, usual source of care) among Latinos and non-Latino whites (NLWs) are related to frequent ED use for asthma in our RIPRAC sample. Our main hypothesis is that health care system variables will account for disparities in ED use for asthma between Puerto Rico and Rhode Island while individual/family variables may account for disparities in ED use between Latinos and NLW families in both sites.
Methods
Study Design and Sampling
The methods of our study have been described in detail elsewhere.12 The study design was the same in both sites: a cross-sectional, observational approach with repeated measurements of selected variables. The Latino sub sample from RI included Dominican children in addition to mainland Puerto Rican children (but no other Latino groups). Dominicans represent an understudied group who also show high rates of parent-reported asthma and ED use.5, 13 Similar to Puerto Rican children; Dominican children are of Caribbean descent and may face socioeconomic challenges related to ED use.
Participants in RI came primarily from convenience samples recruited at a hospital-based ambulatory pediatric clinic and community primary care clinics. In PR, children were recruited primarily from four independent provider organizations, two hospital-based ambulatory pediatric clinics that served mostly medically indigent patients, and from 26 private practice offices. Written parent consent and child assent were obtained in accordance with institutional review board guidelines at both sites.
Measures
All the measures used in the study were translated and back-translated in Spanish, and reviewed for linguistic and cultural appropriateness for the Latino participants (see12).
Poverty Threshold
We derived a ratio of income-to needs for each family by dividing yearly household family income by the poverty threshold for that family size.14, 15 A family was considered below the poverty line if the ratio was less than or equal to 1.0 during the year of study participation.
Health Care System Measures
Access Measures
This measure, based on previous studies16, inquired about usual source of health care for asthma, continuity of care and insurance coverage.
Current Controller Medication Use
Parents were asked to bring all of their child's asthma medications and were queried regarding currently prescribed medications, delivery system and color so they could be identified by research staff. Controller medications were classified as 1) Inhaled Corticosteroids (ICS), including combination ICS/Long-acting β-agonist medications, or 2) other controller medication.
Individual/Family Variables
Asthma Control
Data were gathered from a standardized questionnaire administered to parents asking about nocturnal symptoms, daytime symptoms, limitation of activity, and need for quick-relief medication17 and from a pre-bronchodilator FEV1 measured by a USB spirometer (Koko pneumotachometer, nSpire Health, Inc., Longmont, CO) following American Thoracic Society criteria.18 A computer algorithm was subsequently constructed for the study from asthma guidelines to determine asthma control level for each subject,19 as detailed in Esteban et al.11 The three resulting levels of asthma control were “Controlled”, “Partly Controlled”, and “Uncontrolled”.
Parent Perception of Asthma Severity
Parents rated their child's asthma severity as very mild, mild, moderate, severe, or very severe.
Medication Concerns and Necessity
Was assessed using the Beliefs about Medicine Questionnaire20 that quantifies parental beliefs about asthma medications.
Environmental Tobacco Smoke Exposure (ETS)
Was assessed by asking the parent if anyone smoked in the home.
Environmental Measures
Neighborhood Risk Index
This index was derived by geocoding each participant's address to identify the census block group (defined by the 2000 census) of the residence. A score of 1 was assigned for each of the following characteristics of the block groups: (1) family income less than 1/3 national average; (2) more than 29% of adults did not complete high school; (3) more than 9% of adults unemployed; (4) more than 27% of adults non-English speaking; (5) less than 50% non Latino whites (NLWs); (6) more than 10% vacant housing; (7) more than 22% small housing units; (8) more than 15% of families living below poverty threshold. Each of these cut points represents the 25% poorest block groups on the specified indicator. The participant's neighborhood risk index was the sum of each factor.
ED Use
Infrequent ED use was defined as zero or one ED visit in the preceding 12 months and frequent ED use as two or more visits to an ED within the preceding 12 months.
Statistical Analysis
We examined multiple factors, some of which corresponded to those associated in previous studies with elevated ED use in Latino children (compared with NLW children), and compared these factors among our three demographic groups.11 We then examined the contributions of individual/family factors and health system factors on ED use (frequent vs. infrequent use) using the entire sample (Chi-square and T-tests). Interactions of site/ethnic group with other variables in predicting ED use were also examined in order to evaluate if these associations differed between ethnic groups. Multiple logistic regressions were used to examine the relative contribution of 1) site/ethnicity, and 2) key variables identified in the bivariate analyses in predicting ED use. Lastly, a regression model that excluded RI non Latino whites (NLW) was used to allow for a more direct comparison of the RI Latino and PR groups in key factors predicting ED use.
Results
The sample was composed of 804 children (ages 7 to 15 years), with 405 from PR and 399 from RI. Among the RI children, 151 were NLW, 112 were of Puerto Rican descent, and 136 were of Dominican descent. To evaluate whether it was acceptable to combine the Puerto Ricans and Dominicans into one RI Latino sample, we compared key demographic indicators between these groups. There were no significant differences regarding asthma indicators (severity, control, frequency of ED visits for asthma, hospitalization for asthma in the past year), or demographic variables (child age and gender, maternal level of education, or poverty threshold). Hence, the Puerto Rican and Dominican samples were combined to create one RI Latino sample for all subsequent analyses.
The characteristics of the participants are summarized in Table 1. Island Puerto Ricans had the highest number of participants with at least one ED visit and the highest number of frequent ED users, followed by RI Latinos, and NLWs. The differences in frequent ED visits were significant across all ethnic groups and across ethnic groups within RI. There were significant differences across ethnic groups in all independent variables measured except for age.
Table 1.
Characteristics of study participants based on ethnic groups
| Island PR n=405 | RI Latino n=249 | RI NLW n=151 | |
|---|---|---|---|
| At least one ED visit for asthma** | 62% | 38% | 26% |
| Two or more ED visits for asthma** | 44% | 23% | 13% |
| Child age, mean, (SD) | 10.7 (2.5) | 10.6 (2.5) | 10.5 (2.6) |
| Female, %* | 44% | 48% | 35% |
| Lack a usual source of care for breathing problems,%** | 21% | 3% | 1% |
| Public Insurance, %** | 52% | 77% | 30% |
| ICS User, %** | 20% | 46% | 59% |
| Controller Medication use (any, including ICS), %** | 41% | 72% | 79% |
| Below poverty threshold, %** | 65% | 59% | 15% |
| Environmental Tobacco Smoke Exposure, %** | 34% | 17% | 32% |
| Parent Perception of Asthma Severity, mean, (SD)** | 3.1 (0.8) | 2.9 (0.9) | 2.4 (0.8) |
| Asthma control, mean (SD)* | 1.1 (0.7) | 1.3 (0.7) | 1.1 (0.7) |
| Concerns about Medications, mean (SD)** | 3.1 (0.8) | 3.0 (0.8) | 2.6 (0.7) |
| Neighborhood Risk, mean (SD)** | 0.51 (0.09) | 0.35 (0.12) | 0.13 (0.10) |
p<0.05
p<0.001
The characteristics of children with frequent ED use compared to children with infrequent ED use for the entire study sample are compared in Table 2. Children with frequent ED use were more likely to lack a usual source of care for breathing problems, have public insurance, be below the poverty threshold, be exposed to environmental tobacco smoke (ETS), and be perceived by their parent as having moderate or severe asthma. In addition, children with frequent ED use had worse asthma control, greater parental concerns about asthma medications, and greater neighborhood risk.
Table 2.
Characteristics of study participants based on frequent versus infrequent ED use
| Infrequent ED use n = 549 | Frequent ED use n = 255 | |
|---|---|---|
| Child age, mean, (SD) | 10.7 (2.6) | 10.5 (2.4) |
| Female, % | 43% | 44% |
| Lack a usual source of care for breathing problems,%* | 8% | 20% |
| Public Insurance, %* | 51% | 66% |
| ICS User, % | 31% | 26% |
| Controller Medication use (any, including ICS), % | 50% | 45% |
| Below poverty threshold, %* | 49% | 64% |
| Environmental Tobacco Smoke Exposure, %* | 24% | 38% |
| Parent Perception of Asthma Severity, mean, (SD)* | 2.7 (0.9) | 3.4 (0.7) |
| Asthma control* (scale 0–2; higher score = worse control) | 1.1 (0.7) | 1.3 (0.7) |
| Concerns about Medications, mean (SD)* | 2.8 (0.8) | 3.1 (0.8) |
| Neighborhood Risk, mean (SD)* | 4.8 (2.8) | 6.1 (2.0) |
p<0.001
Independent variables that were associated with frequent ED use were public insurance (F=10.3 p≤0.05), poverty (F=4.9; p≤0.05), higher parent perception of asthma severity (F=42; p≤0.001), increased ETS (F=3.9; p≤0.05), decreasing asthma control (F=26; p≤0.001), and greater concerns about medications (F=4.9; p≤0.05) (Table not shown). Interaction terms between ethnic groups and independent variables were examined to determine if associations between independent variables and frequency of ED use differed between ethnic groups. The public insurance by ethnic group status interaction was significant (F=6.2, p<0.005). When examined graphically public insurance appeared to be associated with frequency of ED use for both RI NLW and PR groups, but not for the RI Latino group (see Figure 1). No other interaction terms were statistically significant.
Figure 1.
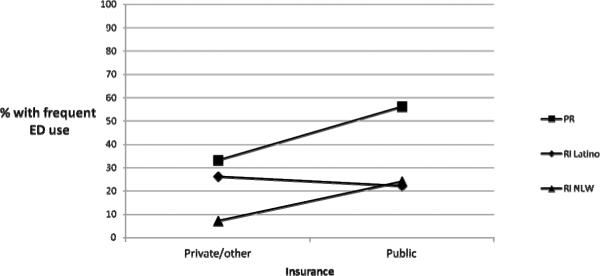
Association between public insurance and frequent ED utilization beetween ethnic groups
A logistic regression model, which included the significant predictors identified in earlier analyses, was constructed to evaluate the relative contributions of each of the key variables in predicting ED use across the entire study sample. (Poverty was not included in this model due to its redundancy with public insurance status). In this regression model that included the entire study sample, living in Puerto Rico (AOR 2.9; 95% CI 1.3–6.6), having public insurance (AOR 2.0; 95% CI 1.4–2.9), having worse asthma control (AOR 1.3; 95% CI 1.0–2.7), and parents perceiving asthma as more severe (AOR 2.3; 95% CI 1.9–2.8) were significantly associated with frequent ED use (Table not shown).
In a sub-analysis, a separate regression model was derived that excluded RI NLWs to allow for a direct comparison of the PR sample and RI Latinos. In this model, living in PR (AOR 3.1; 95% CI 2.0–4.9), having public insurance (AOR 1.9; 95% CI 1.3–2.8), and parents perceiving asthma as more severe (AOR 2.2; 95% CI 1.8–2.8) were significantly associated with frequent ED use (Table not shown).
Discussion
In our previous work11 we had hypothesized that the apparent paradox (higher rates of ED use with milder asthma among island Puerto Ricans) could be related to public insurance policies on the island. Our current findings provide support for this hypothesis, as public insurance was one of the important variables in predicting ED utilization. Public insurance status was also associated with increased ED use in NLWs. Public insurance has been found to be a predictor of frequent hospitalizations and ED use among studies of young children with various illnesses including asthma.10, 21 Medicaid and other public managed care insurance policies are characterized by higher per capita resource constraints, stricter limits on covered services, and restricted provider networks, including limited access to specialists.22, 23 Children with public insurance often lack a primary care physician,10 and less frequently use primary care physicians for preventive care.24 The access and quality barriers linked to public insurance and decreased use of primary care have been associated with the lower reimbursement rates typical of public insurance10 and with a lower quality of care.22 All these factors present in public Medicaid and managed care public insurance policies are also present in the Puerto Rico's managed care public insurance and may be related to the high rates of ED use observed in the island. Furthermore, the public health policy in Puerto Rico required managed care organizations (MCOs) and the Independent Provider Associations (IPAs) with whom they sub-contracted to be directly responsible financially for medication costs and referrals to specialists. Private insurance companies do not capitate medication costs and thus providers bear no financial risks in prescribing medications. This public health policy was in great part responsible for the fact that only 12.3% of children with asthma that had public insurance versus 48.3% in the private sector were dispensed controller asthma medication within a given year.25 After controlling for severity, children with public health plans who were not receiving controller medications compared to those that were dispensed the medication, were also significantly more likely to use the ED use and to have their asthma be poorly controlled.25 Since October of 2010 the public health policy has changed in Puerto Rico and insurance companies instead of providers are directly responsible for medication costs. Changes in public policy so that reimbursement to providers are increased, or the risk for medication costs and referrals is eliminated, have the potential of eliminating barriers of access to specialists and prescription of controller medications previously associated with public insurance.22, 23, 25
Among the RI Latino population, no association was found between public insurance and ED use. In RI, public insurance (RIte Care) is also run through a managed care model, in which three private insurance companies also administer a public plan. Functionally, these plans operate very similar to private insurance options, but with many more benefits (e.g., limited or no co-pay for medications). Hence in RI the “public insurance” designation may be reflective of the income requirements needed to obtain public insurance coverage, rather than pronounced disparities in benefits and care received. Furthermore, in the RI sample, the majority of Latinos (77.3%) have this type of public insurance, providing little variability for the statistical analyses performed.
We also found that parents' perception of their children's asthma severity was important in predicting frequent ED visits, a finding that has been replicated in another sample of mainland Latinos, and in our previous findings in which parental perception of acute need was one of the strongest predictors of ED use.13, 26
Although the existing literature indicates that lack of a usual source of care may predict more frequent ED use5 in our data lack of a usual source of care was not associated with frequent ED use. One potential explanation is that the finding is artifactual. Our item regarding this construct allowed the respondent to endorse any of a list of potential locations for use of care, including the ED. Analyses from a related report27 indicate a fair proportion (35.3%) of our PR group reported the ED as a usual source of care, a rate substantially higher than the RI Latino (4.5%) and NLW (2.7%) groups. The high rate of a “usual source of care” in the RI population (approximately 98%) may also have resulted in little variability in the statistical analyses.
Use of inhaled corticosteroids (ICS) was not associated with ED use. Prior studies that have found an association between ICS use and ED use have not simultaneously controlled for severity, frequent night time symptoms, and other factors related to ED use.5, 7 ICS use may not have a direct association with ED use for a few reasons. ED use may be decreased when children with persistent-level asthma use ICS medications properly. Several studies have found lower frequency of ED use to be associated with better adherence to ICS.28, 29 Yet, because children with increasing asthma severity are more likely to use ICS, there is an association between ED use and ICS use due to this higher baseline asthma severity. Our results also showed differences between the NLW and Latinos in parental medication concerns, neighborhood risk, and lack of asthma control (Table 1). Yet, for all ethnic groups these variables were significantly related to ED use as evidenced by the lack of interaction between ethnicity and any of the variables in frequent ED use.
Several limitations of this study should be noted. First, ED utilization was based on self report and not on more objective methods such as claims data; however, a recent report showed moderate agreement (k=.60) between claims data and report of ED visits over a one year period.30 Second, our study was based on convenience samples, and we may not have accessed children who were not receiving any care at all for their asthma, which limits the generalizability of our findings. Further, our study was cross-sectional and therefore we cannot make causal inferences regarding the relationship between ED use with the factors examined in the study. Disparities in asthma morbidity are related to multiple complex and inter-related factors.31
Factors not measured, such as difficulties contacting the provider, number of unscheduled visits, difficulties in obtaining medication, and continuity of providers32 may have exerted important effects. Further research should address these and other modifiable factors related to ED use including health literacy, health care system variables (i.e. existing health care policies and reimbursement practices), and provider-specific variables (i.e. provider's preventive care and prescription practices).
Conclusions and Recommendations
The high rates of ED utilization particularly among island Puerto Ricans are troubling because ED treatment is associated with lack of continuity of care, and little or no preventive care, factors that are necessary for achieving good control of asthma.10 Our results suggest the need for the development of interventions that are geared towards educating families on how best to use the ED, enhance continuity with providers, and motivate families to attend follow up visits. Revisions of public policies driving public insurance, such as low provider reimbursement and provider risk for referral and medication costs to assure better access to specialists, and evidence based treatment are needed.
Acknowledgments
Financial Support: This study was supported by Grants # U01-Hl072438-01 and HL 072519-05 (G. Fritz and G. Canino, P.I.s) from the National Heart Lung and Blood Institute and from NIH Grant # 5P60 MD002261-02 funded by the National Center for Minority Health and Health Disparities (NCMHD-NH). In addition it was supported for technical assistance by the UPR School of Medicine Endowed Health Services Research Center, Grants 5S21MD000242 and 5S21MD000138, from NCMHD-NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosure Statement: “No competing financial interests exist.”
References
- 1.National Institutes of Health NH, Lung, and Blood Institute. National Asthma Education and Prevention Program . Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health; Bethesda, MD: 2007. [Google Scholar]
- 2.Boudreaux ED, Emond SD, Clark S, Camargo CA., Jr. Acute asthma among adults presenting to the emergency department: the role of race/ethnicity and socioeconomic status. Chest. 2003;124:803–812. doi: 10.1378/chest.124.3.803. [DOI] [PubMed] [Google Scholar]
- 3.Ginde AA, Espinola JA, Camargo CA., Jr. Improved overall trends but persistent racial disparities in emergency department visits for acute asthma, 1993–2005. J Allergy Clin Immunol. 2008;122:313–318. doi: 10.1016/j.jaci.2008.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller JE. The effects of race/ethnicity and income on early childhood asthma prevalence and health care use. Am J Public Health. 2000;90:428–430. doi: 10.2105/ajph.90.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stingone JA, Claudio L. Disparities in the use of urgent health care services among asthmatic children. Ann Allergy Asthma Immunol. 2006;97:244–250. doi: 10.1016/S1081-1206(10)60021-X. [DOI] [PubMed] [Google Scholar]
- 6.Lieu TA, Lozano P, Finkelstein JA, et al. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. Pediatrics. 2002;109:857–865. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 7.Cohen RT, Celedon JC, Hinckson VJ, et al. Health-care use among Puerto Rican and African-American children with asthma. Chest. 2006;130:463–471. doi: 10.1378/chest.130.2.463. [DOI] [PubMed] [Google Scholar]
- 8.Rand CS, Butz AM, Kolodner K, Huss K, Eggleston P, Malveaux F. Emergency department visits by urban African American children with asthma. J Allergy Clin Immunol. 2000;105(1 Pt 1):83–90. doi: 10.1016/s0091-6749(00)90182-9. [DOI] [PubMed] [Google Scholar]
- 9.Oster A, Bindman AB. Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med Care. 2003;41:198–207. doi: 10.1097/01.MLR.0000045021.70297.9F. [DOI] [PubMed] [Google Scholar]
- 10.Todd J, Armon C, Griggs A, Poole S, Berman S. Increased rates of morbidity, mortality, and charges for hospitalized children with public or no health insurance as compared with children with private insurance in Colorado and the United States. Pediatrics. 2006;118:577–585. doi: 10.1542/peds.2006-0162. [DOI] [PubMed] [Google Scholar]
- 11.Esteban CA, Klein RB, McQuaid EL, et al. Conundrums in childhood asthma severity, control, and health care use: Puerto Rico versus Rhode Island. J Allergy Clin Immunol. 2009;124:238–44. 44 e1–5. doi: 10.1016/j.jaci.2009.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canino G, McQuaid EL, Alvarez M, et al. Issues and methods in disparities research: the Rhode Island-Puerto Rico asthma center. Pediatric Pulmonol. 2009;44:899–908. doi: 10.1002/ppul.21075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lara M, Duan N, Sherbourne C, Halfon N, Leibowitz A, Brook RH. Children's use of emergency departments for asthma: persistent barriers or acute need? J Asthma. 2003;40:289–299. doi: 10.1081/jas-120018331. [DOI] [PubMed] [Google Scholar]
- 14.Duncan TE, Duncan SC, Hops H, Alpert A. Multi-level covariance structure analysis of intra-familial substance use. Drug and Alc Depend. 1997;46:167–180. doi: 10.1016/s0376-8716(97)00057-4. [DOI] [PubMed] [Google Scholar]
- 15.U.S. Department of Health and Human Services Federal Register. The 2005 HHS poverty guidelines. 2005 Feb 18;70(33):8373–8375. [Google Scholar]
- 16.Ortega AN, Gergen PJ, Paltiel AD, Bauchner H, Belanger KD, Leaderer BP. Impact of site of care, race, and Hispanic ethnicity on medication use for childhood asthma. Pediatrics. 2002;109:E1. doi: 10.1542/peds.109.1.e1. [DOI] [PubMed] [Google Scholar]
- 17.Rosier MJ, Bishop J, Nolan T, Robertson CF, Carlin JB, Phelan PD. Measurement of functional severity of asthma in children. Am Jo Respir Crit Care Med. 1994;149:1434–1441. doi: 10.1164/ajrccm.149.6.8004295. [DOI] [PubMed] [Google Scholar]
- 18.American Thoracic Society Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med. 1995;1523:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 19.GINA Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2006 Available from: http://www.ginasthma.org.
- 20.Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy S, Stone A, Rachelefsky G. Factors associated with emergency department use in asthma: acute care interventions improving chronic disease outcomes. Ann Allergy Asthma Immunol. 2003;90:45–50. doi: 10.1016/S1081-1206(10)63613-7. [DOI] [PubMed] [Google Scholar]
- 22.Smedley BDSA, Nelson AR. Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Board of Health Sciencies Policy, Institute of Medicine; Washington, D.C.: 2002. Unequal treatment confronting racial and ethnic disparities in health care. [Google Scholar]
- 23.Tai-Seale M, Freund D, LoSasso A. Racial disparities in service use among Medicaid beneficiaries after mandatory enrollment in managed care: a difference-in-differences approach. Inquiry. 2001;38:49–59. doi: 10.5034/inquiryjrnl_38.1.49. [DOI] [PubMed] [Google Scholar]
- 24.Berman S, Armon C, Todd J. Impact of a decline in Colorado Medicaid managed care enrollment on access and quality of preventive primary care services. Pediatrics. 2005;116:1474–1479. doi: 10.1542/peds.2005-0923. [DOI] [PubMed] [Google Scholar]
- 25.Vila D, Rand CS, Cabana MD, et al. Disparities in asthma medication dispensing patterns: the case of pediatric asthma in Puerto Rico. J Asthma. 2010;47:1136–1141. doi: 10.3109/02770903.2010.517338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fritz GK, McQuaid EL, Kopel SJ, et al. Ethnic differences in perception of lung function: a factor in pediatric asthma disparities? Am J Respir Crit Care Med. 2010;182:12–18. doi: 10.1164/rccm.200906-0836OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jandasek B, Ortega AN, McQuaid EL, et al. Access to and use of asthma health services among Latino children: The Rhode Island-Puerto Rico Asthma Center Study. Med Care Res Rev. doi: 10.1177/1077558711404434. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bender B, Zhang L. Negative affect, medication adherence, and asthma control in children. J Allergy Clin Immunol. 2008;22:490–495. doi: 10.1016/j.jaci.2008.05.041. [DOI] [PubMed] [Google Scholar]
- 29.Cochrane GM, Horne R, Chanez P. Compliance in asthma. Respir Med. 1999;93:763–769. doi: 10.1016/s0954-6111(99)90260-3. [DOI] [PubMed] [Google Scholar]
- 30.Ungar WJ, Davidson-Grimwood SR, Cousins M. Parents were accurate proxy reporters of urgent pediatric asthma health services: a retrospective agreement analysis. J Clin Epidemiol. 2007;60:1176. doi: 10.1016/j.jclinepi.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol. 2009;123:1209–17. doi: 10.1016/j.jaci.2009.02.043. quiz 18–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fredrickson DD, Molgaard CA, Dismuke SE, Schukman JS, Walling A. Understanding frequent emergency room use by Medicaid-insured children with asthma: a combined quantitative and qualitative study. J Am Board Fam Pract. 2004;17:96–100. doi: 10.3122/jabfm.17.2.96. [DOI] [PubMed] [Google Scholar]


