Abstract
The aim of the study was to examine longitudinal patterns of decision making based on risk and reward using a modified version of the Iowa Gambling Task (IGT) in children who had sustained traumatic brain injury (TBI) and children with orthopedic injury (OI). Participants were 135 children and adolescents with TBI (n=71) or OI (n=64) who were 7 to 17 years at the time of injury were enrolled and assessed prospectively at baseline and at follow-up intervals of 3, 12, 18, and 24 months after injury. Groups were similar in age, socioeconomic status, and gender. Participants chose from four decks of cards with the aim of maximizing earnings across 100 trials. Two of the decks offered relatively small rewards and relatively small losses, but were advantageous over the course of the experiment. The other two decks offered large rewards, but also introduced occasional large losses, and were considered disadvantageous over the course of the experiment. The variable of interest was the proportion of advantageous decks chosen across trials.
Longitudinal analysis of the pattern of change across two years revealed a three-way interaction among injury group, age, and the quadratic term of interval-since-injury,. In this interaction, the effect of age weakened in the TBI group across time, as compared to the OI group, which showed stronger quadratic patterns across the recovery intervals that differed by age. The OI group generally outperformed the TBI group.
In addition, analyses revealed a three-way interaction among group, gender and the cubic term of post-injury interval, such that overall, males improved a great deal with time, but females showed small gains, regardless of injury group.
1. Introduction
Children sustaining a traumatic brain injury (TBI) exhibit difficulties across neuropsychological domains (H. S. Levin & Hanten, 2005; Yeates, et al., 2002). Some of the most notable deficits involve working memory (H. S. Levin, et al., 2002; H. S. Levin, et al., 2004) cognitive/behavioral inhibition (Dennis, Guger, Roncadin, Barnes, & Schachar, 2001; Schachar, Levin, Max, Purvis, & Chen, 2004), and other higher-level executive skills (Hanten, et al., 2004; H. S. Levin & Hanten, 2005) including problem-solving and decision making (Catroppa & Anderson, 2006; Hanten, et al., 2006). Although significant recovery can occur (especially within the first year after injury), many children display persistent cognitive and behavioral deficits (Anderson, Catroppa, Morse, Haritou & Rosenfled, 2005; Chapman, et al., 2004; Fay, et al., 2009; Yeates, et al., 2002). These persistent executive deficits may create barriers to age-appropriate social interaction and dramatically increase the probability of impulsive, ill-advised decisions.
Although numerous investigations with TBI survivors clearly demonstrate a variety of executive deficits on laboratory measures, these kinds of tasks are limited in their ability to describe decision making deficits that may have implications for real-world functioning (H. S. Levin & Hanten, 2005). The Iowa Gambling Task (IGT) was designed to model naturalistic decision-making processes and has been used with neurologically compromised populations (A. Bechara, Damasio, Damasio, & Anderson, 1994; Antoine Bechara, Damasio, Tranel, & Damasio, 1997). In this task, individuals are asked to choose from four decks of cards. Two of these decks offer relatively small rewards and relatively small losses and are advantageous over the course of the experiment. Conversely, the other two decks offer larger rewards but significantly larger losses and are not advantageous over the course of the experiment. Individuals with orbitalfrontal cortex (OFC) or ventromedial damage are impaired on this procedure because they persist in choosing cards from the disadvantageous decks despite verbally providing insight into which decks are more profitable over time (Antoine Bechara, et al., 1997). Additional studies suggest that lesions in other brain areas such as the amygdala (AMG) and anterior cingulate cortex (ACC) result in deficits on the IGT (A. Bechara, Damasio, Damasio, & Lee, 1999).
A few studies have also used the IGT to demonstrate deficits in decision making following TBI (Hanten, et al., 2006; Levine, et al., 2005). Levine and colleagues (2005) found that, as a group, adults with severe TBI exhibited difficulties on the IGT although they suggested that the largest difference between groups was on the pattern of performance as opposed to the overall result. That is, individuals sustaining a TBI appeared to take longer to acquire the rules of the task although their performance near the end of the procedure was similar to the performance of control participants. In a preliminary investigation, Hanten and colleagues (Hanten, et al., 2006) used a modified IGT to investigate decision-making abilities in 11 children and adolescents who were at least one-year post TBI. Nine of the participants had amygdala (AMY) lesions whereas the other two participants had lesions in the ventral medial cortex (VMC). Results indicated that participants with AMY lesions exhibited significantly worse performance (i.e., greater selection from disadvantageous decks) when compared to participants with VMC lesions. Researchers cautioned their findings were based on a small number of participants, and they noted that injury severity differed markedly between the AMY and VMC lesion groups thereby complicating clear interpretation of the findings.
In addition to individuals with traumatic injuries and cortical lesions, the IGT and tasks analogous to the IGT have also been used to study the development of decision making in children and adolescents (Crone, Bunge, Latenstein, & van der Molen, 2005; Crone & van der Molen, 2004; Garon & Moore, 2004; C. J. Hooper, Luciana, Conklin, & Yarger, 2004; Catalina J. Hooper, Luciana, Wahlstrom, Conklin, & Yarger, 2008; Huizenga, Crone, & Jansen, 2007; Kerr & Zelazo, 2004; Overman, et al., 2004; van Leijenhorst, Crone, & Bunge, 2006; van Leijenhorst, Westenberg, & Crone, 2008). These studies typically demonstrate a linear positive relationship between decision making ability and age. That is, performance (as measured by overall gains) on the IGT generally increases with older age (Crone & van der Molen, 2004; C. J. Hooper, et al., 2004).
In the current investigation, we were interested in examining the trajectory of decision-making abilities in children and adolescents in the first two years following TBI as compared to children who sustained orthopedic injury (OI) not involving head trauma. We were also interested in examining the relationship between IGT performance and correlated variables such as age, gender, and socioeconomic status (SES). Behavioral data was obtained at five time points from a large cohort of children and adolescents between the ages of 6 and 17 years at the time of injury. Given the predominance of TBI injuries involving the frontal regions, including orbitofrontal and ventromedial areas, we expected the children with TBI to perform more poorly than children with OI. However, our prediction is tempered by the knowledge that risk factors predisposing to OI may relate to impulsivity. Based on current literature and given our age range, we also anticipated that males would outperform females as males within this age range tend to focus more on long-term outcomes on the IGT task (Overman, et al., 2004).
2. Methods
2.1 Participants
Children and adolescents with moderate or severe TBI or an OI between the ages of 7 to 17 years at the time of injury were recruited from consecutive admissions to medical centers in Dallas and Houston, Texas, and in Miami, Florida. An OI comparison group was included to control for risk factors predisposing children to injury and to equate for nonspecific factors such as maturation or stress resulting from hospitalization (Yeates, et al., 2004). Children and adolescents with TBI (n=71) or OI (n=64) were assessed on cognitive and neuropsychological tests at baseline, 3 months, 12 months, 18 months and 24 months. Baseline assessments all occurred within a month post-injury.
Inclusion criteria for the TBI group included a lowest post-resuscitation Glasgow Coma Scale (GCS; Teasdale & Jennett, 1974) score recorded at the emergency center consistent with moderate or severe TBI (mean GCS=7.9, SD=4.5, range=3 to 15). Moderate TBI was defined as a GCS score of 9 to 12, or 13 to 15 with brain lesions (contusions, hematomas) indicated by computed tomographic (CT) scans, following current methodology (Levin, et al., 2008), and severe TBI was defined by GCS scores of 3 to 8. The 64 hospitalized OI patients had mild to moderate orthopedic injuries as defined by the Abbreviated Injury Scale (AIS). All participants were English-speaking, had no previous hospitalization for head injury, and no diagnosis of mental retardation or a neurodevelopmental disorder (e.g., autism). Demographic and injury characterization data, including age at injury, race, gender, SES as measured by the Socioeconomic Composite Index (SCI; Yeates et al., 1997), GCS scores, presence or absence of preinjury ADHD, mechanism of injury and AIS scores are displayed in Table 1. The distribution of lesion location for the TBI participants is shown in Table 2. Note that not all participants were examined at each time point due to missed visits or computer failure, which were not injury-related. Twenty-four patients completed 5 visits, 44 patients completed 4 visits, 26 patients completed 3 visits, 17 patients completed 2 visits, and 24 patients only completed a single visit. The sample size for each interval was as follows: baseline, TBI=56, OI=55; 3 months, TBI=53, OI=53; 12 months, TBI=44, OI=41; 18 months TBI=36, OI=34; and 24 months TBI=33, OI=27. All procedures were approved by the institutional review boards of the participating organizations and were in compliance with the National Institute of Health policies on human subjects protection.
Table 1.
Demographics and injury characteristics of all subjects included in longitudinal analyses.
| OI (n=64) | TBI (n=71) | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | p-value | |
| Age at injury (yrs) | 11.89 | 2.5 | 7.05–17.21 | 13.38 | 2.81 | 7.10–16.55 | 0.0016 |
| SCI (z-score) | 0.103 | 0.83 | −1.52–1.89 | −0.0 | 0.82 | −1.86–1.75 | 0.4756 |
| GCS | 15 | 0 | 15–15 | 7.94 | 4.5 | 3–15 | |
| Gender | 18 female; 46 male | 25 female; 46 male | 0.3775 | ||||
| AIS score | 6.38 | 3.82 | 1–22 | 23.89 | 10.19 | 9–50 | <0.0001 |
| Pre injury ADHD | n=20 (31.75%) | n=13 (19.4%) | 0.1061 | ||||
| Race/Ethnicity | 22 AA; 20 Caucasian/Asian; 22 Hispanic | 9AA; 31 Caucasian/Asian; 30 Hispanic | 0.0105 | ||||
| Mechanism of Injury | * High Speed=11; Low Speed=53 | * High Speed=50; Low Speed=21 | <0.001 | ||||
TBI = Traumatic Brain Injury, OI = Orthopedic Injury, GCS = Glasgow Coma Scale, SCI = Socioeconomic Composite Index, AIS = Abbreviated Injury Scale
Table 2.
Frequency and percentage of sample of brain lesions by region (inclusive) for the TBI group.
| Total Freq. | Total % | Female Freq. | Female % | Male Freq. | Male % | |
|---|---|---|---|---|---|---|
| Lesion | Frequency | % sample | ||||
| Amygdala | 7 | 3.43 | 2 | 3.39 | 5 | 3.45 |
| Hippocampal | 16 | 7.84 | 4 | 6.78 | 12 | 8.28 |
| OFC_VM | 32 | 15.69 | 11 | 18.64 | 21 | 14.48 |
| Occipital | 9 | 4.41 | 1 | 1.69 | 8 | 5.52 |
| Other | 42 | 20.59 | 12 | 20.34 | 30 | 20.69 |
| OtherFrontal (excluding OFC_VM) | 52 | 25.49 | 15 | 25.42 | 37 | 25.52 |
| OtherTemporal (excluding amygdala, hippocampus) | 36 | 17.65 | 11 | 18.64 | 25 | 17.24 |
| Parietal | 10 | 4.90 | 3 | 5.08 | 7 | 4.83 |
OFC_VM = Orbitalfrontal/Ventromedial Cortex; OtherFrontal = all other frontal regions combined, excluding OFC_VM; OtherTemporal = all other temporal regions, excluding the amygdala and hippocampus.
2.2 Materials
Modified Iowa Gambling Task (Hanten, et al., 2006 after Bechara, et al., 1997). We modified the original IGT to be more appropriate for younger children and those with TBI in our study. The original task presented feedback separately for reward and penalty (e.g., “you have won $1500; but you have lost $110”), requiring a calculation to determine the net outcome of the trial (e.g., $1390). Younger children in our cohort (age 7 years) may have difficulty performing these calculations; therefore, we modified the task to give feedback on the net amount earned on each trial. Further, the high dollar amounts used in the original task ($1000+) were not meaningful to younger children so we modified the values by dividing the original task values by 400, which yielded amounts in dollars and cents, but preserved the original task’s schedule of increasing rewards/penalty contingencies. We also allowed the child to keep money earned during the task, which may have also increased the child’s incentive for performing the task. The decks were made more easily distinguishable and memorable to children by color labeling, which is different than the original IGT.
Each participant played a computer game with four card decks depicted on the screen. Each deck was a different color (red, yellow, blue, green). Consistently choosing two of the decks (e.g., red or yellow) resulted in a net loss (bad decks), whereas choosing the other decks resulted in a net gain (good decks). The participant was told to choose a deck to see how much money s/he won or lost, and that some decks were better than others. After each trial the computer displayed a graphic representation (a green or red bar) of the amount won or lost (this amount was also read aloud by the experimenter). Each participant was given $2.00 at the beginning of the test, and kept any money won. There were 100 trials in all, and four versions of the task in which the colors of good and bad decks were varied, and task version was counterbalanced across test intervals so that each subject received a different version of the task for the first 4 intervals (baseline, 3 months, 12 months and 18 months). At the 24 month interval, each subject was re-administered the same version as at baseline. The measure of interest was the number of good decks chosen as compared to the number of bad decks.
2.3 Statistics
Demographic statistics were compared using t-test for continuous variables, age at injury, and SCI. Chi-squared tests were used for categorical variables, such as gender, mechanism of injury, race and preinjury ADHD. For the gambling task, we divided the 100 trials into 5 blocks of 20 trials each. The outcome measure was a measure of the predominance of choices for good decks over bad decks, which was operationalized as good deck minus bad deck divided by total trials, for each of the 5 blocks. A growth curve analysis applying a linear mixed model was conducted to examine the recovery pattern. The advantage of the linear mixed model is that it can apply an appropriate variance-covariance structure for the correlated data and can accommodate subjects with missing data points therefore retain the largest sample size. The variances of the growth variables (intercept, linear, quadratic, and cubic functions of the interval -since -injury) were tested in the level 1 (unconditional) model. All were significant. Since there were repeated measurements on blocks of the performance at each time interval, in order to take into account the correlations among the measurements on blocks, blocks was entered into the level 1 model with the growth variables to indicate the nature of repeated measurements. Coefficients that did not vary randomly were then fixed for the level 2 model, in order to see their effects on those random parameters.
Other time-invariant variables, such as age at injury, gender, SCI and race, were entered into the level 2 model with group variable in order to examine their effects on the growth parameters. All possible 3-way interactions of group by growth variable by other variables were tested. In order to accurately capture the growth curve over time, we used the exact interval that had elapsed between time of injury and time of test (in months) for the ‘interval’ variable, instead of the designated time points for baseline, 3, 12, 18 and 24 months. Since age and group significantly affected the growth curve, the growth curves for both groups were compared at the grand mean of age, mean+1 standard deviation, and mean−1 standard deviation using least squares means to yield our three age points. This should not be interpreted as grouping patients into age groups. We examined group differences on ADHD, and whether an ADHD diagnosis modified group differences on the intercept and curvature. Although the groups different in the rate of ADHD, it was not significant, nor was the effect of ADHD on the outcome measure significant, therefore it was not included in the model.
Although the attrition rate was unexpectedly high analysis of the pattern of attrition revealed that it was not related to injury severity. As such, the missing data appeared to be at random and secondary to factors such as the patients’ unwillingness to visit, a recent move, or conflict of schedule. Mixed models are robust to significant missing data and can appropriately handle the within subject variance and covariance structure. Further, to examine whether demographic or other injury variables were affected by attrition, thus might create sampling bias, within the OI group, we grouped the patients with complete and without complete follow ups (11 verses 51), and compared the AIS score. There was no significant difference. Within TBI patients, we performed the same analysis with regard to GCS score. There were 12 TBI patients with all follow-up data verses 51 who were missing one or more follow-up sessions. Like in the OI group, there was no significant difference between these subgroups on GCS score. These findings suggest that despite our attrition rate, no obvious difference existed between participants completing all follow-ups and those with missing data. All figures used the fitted values at the corresponding follow-up time points.
3. Results
Demographics
There was a significant group difference in age, t(133)=3.22, p=0.0016. SES (measured via SCI) did not differ between groups, t(130)=0.72, p=0.4756. As expected, there was a significant group difference in mechanism of injury, χ2=38.51, p<0.0001, with children with TBI sustaining more high-speed injuries and fewer low speed injuries than children with OI. There was also a significant group difference in race, χ2 =9.1132, p=0.0105, with more African American children in the OI group than in the TBI group.
Growth Curve Analysis
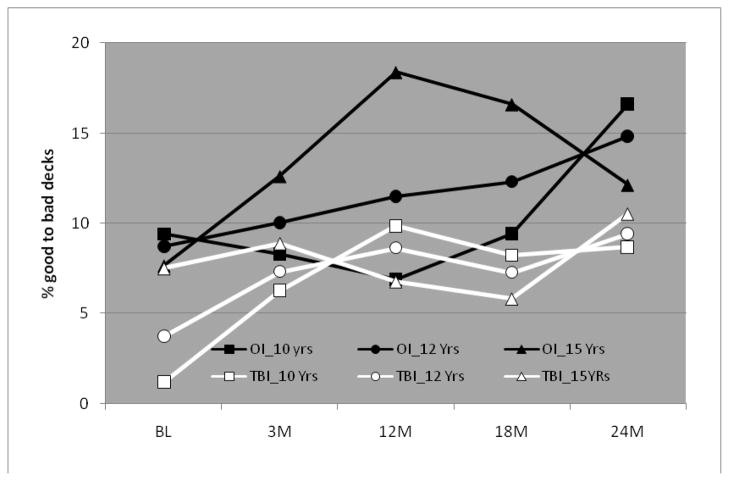
The growth curve analysis on performance over time revealed a three-way interaction among injury group, age, and the quadratic term of interval-since-injury, F(1,1898)= 8.01, p=0.0047, which indicated that age had a significant effect on the quadratic term of the recovery in OI patients, t(1899)=−2.47, p=0.0137, but not in the TBI patients, t(1898)= 1.44, p=0.1495. As can be seen in Figure 1, in children with TBI, the pattern across interval-since-injury is similar, with early gains from baseline, a slight falling off in the middle occasions, and improvement between 18–24 months post injury. All patients at the 3 age points improved over time in a curved pattern, with performance at 24 months better than at baseline, with the 2 youngest groups showing the greatest gains. Although effect sizes are not appropriate for this type of analysis, parameter estimates (in terms of change per unit value) are provided in Table 3 to facilitate understanding of the practical significance of effects. The group difference varied by age and interval-since-injury, indicating that at 12 month and 18 month, the group difference significantly increased with age-at-injury. The group difference gained significance at around age of 14 years, t(1896)=2.40, p=0.0166) and t(1896)=2.28, p=0.0227 at 12 month and 18 month respectively.
Figure 1.
Percentage good decks (good – bad/# of trials) on the modified IGT by group (OI or TBI), age and interval since injury.
Table 3.
Parameter estimates from the growth curve model
| Parameter | Estimates | t-value | p-value |
|---|---|---|---|
| Intercept | 9.8731 | 3.26 | .0014 |
| Group (OI vs. TBI) | .3547 | .10 | .9226 |
| Race (AA vs other) | 3.1634 | 1.37 | .1722 |
| Race (Caucasian vs other) | 4.6859 | 2.46 | .0138 |
| Block (1 vs 2) | −7.3611 | −4.49 | <.0001 |
| Block (2 vs 3) | −8.1944 | −5.00 | <.0001 |
| Block (3 vs 4) | 0.8796 | .54 | .5913 |
| Block (3 vs 5) | 3.2455 | 1.98 | .0478 |
| Block (4 vs 5) | 2.3658 | 1.44 | .1490 |
| Age | −.6901 | −1.09 | .2760 |
| Gender (F vs M) | −2.6698 | −.68 | .4942 |
| Group*Gender (OI & F vs other) | 4.3421 | .74 | .4617 |
| Age*Group (OI vs TBI) | 2.9932 | 2.82 | .0048 |
| Interval (slope) | −1.0503 | −2.27 | .0254 |
| Interval*age | −.04273 | −.89 | .3724 |
| Interval*Group (OI vs TBI) | 1.4844 | 2.34 | .0192 |
| Interval*Age*Group (OI vs TBI) | .02876 | .39 | .6996 |
| Interval*Gender (F vs M) | 1.7263 | 2.31 | .0209 |
| Interval*group*Gender (OI & F vs other) | −2.4097 | −2.25 | .0244 |
| Interval2 (quadratic) | −.0530 | −1.77 | .0770 |
| Interval2*Age | .0093 | 1.44 | .195 |
| Interval2*Group (OI vs TBI) | .0742 | 1.88 | .0606 |
| Interval2* Age*Group (OI vs TBI) | −.0294 | −2.83 | .0047 |
| Interval2*Gender (F vs M) | .08374 | 1.89 | .0583 |
| Interval2*Group*Gender (OI & F vs other) | −.1211 | −1.90 | .0577 |
| Interval3 (cubic) | .009988 | 2.75 | .0060 |
| Interval3 *Group (OI vs TBI) | −.01048 | −2.14 | .0328 |
| Interval3*Gender (F vs M) | −.01402 | −2.32 | .0205 |
| Interval3 Group*Gender (OI & F vs other) | .01732 | 2.05 | .0407 |
Children with OI showed an entirely different pattern due to the significant age effect, especially the 2 older groups. All patients performed similarly at baseline. At 10 years, OI children showed a clear quadratic pattern, with decreases from baseline until 12 months, then sharp increases at 18 and 24 months. At 15 years, OIs showed a quadratic pattern that is the precise mirror image of the 10 year-olds: sharp increases between baseline and 12 months, followed by declines at 18 and 24 months. At 12 years, patients showed an approximately linear progression with increases at each time point. Patients at all ages had gains in performance between baseline and 24 months.
There was a significant block effect, F(4,1898)= 30.76, p<0.0001, with best performance on block 3 and worst performance on block 1; the order from best performance to worst was block3>block4>block5>block2>block1. Contrasts between block3 and block 1, block2, block 4 and block 5 were tested at significance level of 0.05/4, which is 0.0125, showed block 3 was significantly better than block 1 and block 2, but not significantly differ from block 4 and block 5, p-values are <0.0001, <0.0001, 0.5913 and 0.0478 respectively, suggesting learning over the first three blocks. There was also a significant effect of race, with Caucasians (including Hispanic) showing an advantage with time over African Americans and others, F(2, 1898)= 3.12, p=0.0442. Neither the effect of block nor race interacted with group.
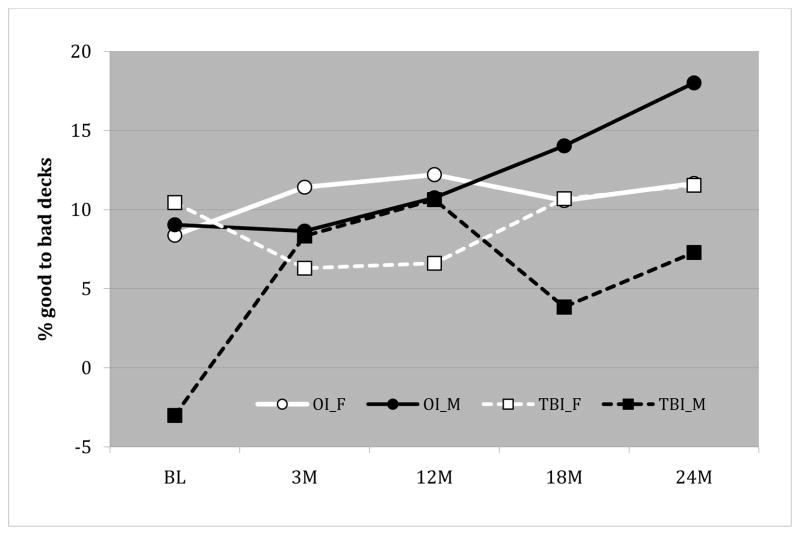
Finally, there was a three-way interaction among injury group, gender and the cubic term of interval-since injury, F(1,1898)= 4.20, p=0.0407, indicating that the gender effect on the growth curve differed by group. At the mean age-at-injury, the cubic term was only significant within TBI males, t(1898)= 2.75, p=0.0060; for TBI females, t(1898)= 0.84, p=0.4029; for OI males, t(1898)= −0.15, p=0.8814; for OI females, t(1898)= 0.55, p=0.5795. As shown in Figure 2, males improved a great deal over time, but females showed small gains, regardless of injury group. Males with OI out performed males with TBI at baseline, 18 months and 24 months, but females showed the opposite pattern: similar performance at baseline, 18 and 24 months, but female OIs outperformed female TBIs at 3 and 12 months. In the male OI group, performance improved in a linear fashion, with steady increases from 3 months to 24 months. In contrast, male TBIs, show a cubic pattern of performance across time, with a sharp increase from baseline to 3 months that flattened out at 12 months, then dropped at 18 months and recovered slightly at 24 months.
Figure 2.
Percentage good decks (good – bad/# of trials) on the modified IGT by group (OI or TBI), gender and interval since injury.
4. Discussion
The present investigation examined decision-making performance on the IGT over time in a group of children sustaining a moderate or severe TBI or OI. Results demonstrated interactions between group, interval-since-injury, and each of age and gender. In general, individuals in the OI group exhibited a dynamic pattern of performance across time. This was marked by significant gains in the oldest participants up to 12 months after injury, significant gains in the youngest OI participants after 12 months post-injury, and a relatively stable pattern of improvement in the middle childhood-aged OI group. Conversely, children sustaining a TBI exhibited generally less variability with age in performance, with linear increases in performance during the first months post-injury followed by a flattening out or slight diminishing of performance and a final upturn at the last assessment regardless of age.
This pattern of differences generally fits with other studies of the developmental progression in IGT performance (C. J. Hooper, et al., 2004). An interesting finding was the decrease in performance of the older OI participants at the 24-month time point. Although a specific reason for this decrease is not known, debriefing of participants in this age range in our pilot studies indicated that adolescents attempted to anticipate the task and ended up “over thinking” the procedure as they got older. Another possibility is that with repeated presentations of the tasks, the older participants became bored or inattentive to the task and therefore their performance was attenuated. As might be expected participants’ performance improved over blocks (of 20 trials each) within a session, with a pattern of gains in the first three blocks, but no further significant gains in blocks 4 and 5. That the pattern was not different for the two groups suggests although both the intercept (reflecting the impact of injury at baseline) and time affected each group differently, within a single session, subjects within each group showed a similar degree and pattern of learning, although the children with TBI, particularly the younger ones, started out with greater impairment, so ended up with impairment relative to the children without TBI.
The steady change in TBI participants is suggestive of at least partial recovery of function following their injuries; however, the less dynamic trajectory of their performance over time also suggests some attenuation of the expected developmental trajectory. This is in keeping with other studies following pediatric TBI on the same cohort of children in which changes in performance over time are observed, but these changes are either significantly less profound than would be expected throughout the course of development for brain structure (Wilde et al., This Issue) or, although showing an increase with time, fail to show recovery from initial baseline deficits (Hanten et al., 2008; Schmidt, Hanten, Li, Orsten & Levin, 2010). The hypothesis that TBI participants demonstrate recovery with a relative absence of subsequent development is bolstered by the lack of an association between age and performance over time emerging within the TBI group, and which may reflect altered development of circuitry connecting prefrontal regions and prefrontal-posterior cortical-subcortical regions.
Few studies have been conducted regarding the longitudinal pattern of performance on the IGT following damage to important brain structures, especially in children. Therefore, we have no means by which to compare our findings of a gradual improvement in performance in our TBI participants. However, structures implicated in decision-making processes such as the ventral-medial prefrontal cortex and insular cortex, and the prefrontal-ventral striatal connections that are important in motivation to guide decision making, are areas known to be vulnerable to TBI. Further, current knowledge suggests that some of the most significant structural remodeling secondary to recovery within these regions occurs within the first year following injury–a time course that loosely parallels our behavioral findings within the TBI group.
The impact of gender on post-injury IGT performance was not entirely unexpected, as other studies have also noted gender differences in IGT performance (van Leijenhorst, et al., 2008). In particular, females appear more risk adverse compared to males and demonstrate somewhat less optimal IGT performance with increasing age. The increase in the performance of males within the OI group over the two-year period combined with the attenuated rate of improvement after three months within males in the TBI group suggests a complex relationship between the development of decision making capacity and recovery from pediatric TBI. Conversely, the pattern of development and recovery appears more equitable among females regardless of injury group.
The significant difference in performance among male participants suggests the presence of another factor that may influence the performance of males in the TBI and OI groups. That is, it may be that a certain level of risk taking may be necessary for adequate performance on the IGT. For example, Hooper and colleagues (2008) demonstrated that increases in neuroticism were negatively correlated with IGT performance among males. Likewise, Suhr and Tsanadis (2007) demonstrated that increases in negative affect were associated with impairments on IGT performance in a group of young adults. This is a salient finding because neuroticism and negative affect are related constructs that have both been linked to various forms of internalizing and externalizing psychopathology (Krueger et al., 2002; Krueger & Markon, 2011; Mineka, Watson, & Clark, 1998). Other research has demonstrated a connection between externalizing psychopathology (e.g., conduct disorder and alcohol dependants) and impairments in IGT performance (Kim, Lee, & Kim, 2006).
One might argue that performance on the IGT depends on at least two factors: the ability to process information to analyze risks, and the personality characteristics necessary to take these risks when information suggests they are appropriate. If there are significant changes in either of these variables, performance on the IGT may be compromised. As such, males with TBI may be unable to sufficiently process all the information necessary to determine when risks should be pursued, leading to increases in selections from non-advantageous decks (i.e., those decks with high rewards but even higher costs). Conversely, females may be able to process all information necessary to make appropriate risk estimations, but be reluctant to engage in a sufficient level of risk to either maximize performance or demonstrate striking impairment. This observation dovetails with recent research suggesting that increased progesterone levels in females may serve a protective function following TBI (Stein, Wright, & Kellerman, 2008). Males within the OI group may be well positioned with the appropriate levels of information processing capacity and personality characteristics to outperform all other groups on this procedure.
4.1 Limitations
The current investigation has some limitations that need to be addressed. First, not all participants were assessed at each time point and some of the participants had data for only one or two sessions. This is a common problem for longitudinal studies, but the advantages of repeated measures and to the ability to observe changes over time outweigh the limitations inherent in accepting some missing data. Similarly, despite beginning with a large number of participants for this type of study and maintaining relatively good follow-up with participants, our two-year retention rate was somewhat lower than in previous studies, especially for OI participants. Thus, it is unclear how much of the slight drop off in performance of the older OI participants reflected a bias in our sample at the 24-month time point. Moreover, the OI participants in the current study presented with a pre-injury diagnosis of attention deficit hyperactivity disorder (ADHD) at a much higher base rate (32%) than individuals within the TBI group (19%) or within the general population (~ 5–8%). Therefore, the pattern of findings of these individuals may not generalize to a typically-developing population as aspects of an ADHD diagnosis (e.g., increased impulsivity) may influence performance on the IGT (I. P. Levin & Hart, 2003; Romer, et al., 2009). Finally, the performance of participants on the IGT appeared to differ by race with African American participants demonstrating slightly less advantageous performance compared to other groups. However, we do not believe this factor would significantly bias our findings of group differences, as African American participants were overrepresented within the OI group.
Although we collected debriefing data for strategies used in our pilot studies, we did not debrief subjects on this longitudinal study in order to avoid influencing performance across intervals. It would be interesting if future investigations attempted to discuss performance following task administration within both OI and TBI participants in order to evaluate if task strategy or insight differed between groups.
5.1 Conclusions
Children who have sustained moderate to severe TBI are likely to show impairments in decision making, but the nature of the effects and the trajectory of recovery appears to be influenced by both age and gender, which has implications for fully understanding the impact of childhood head injury and for intervention. Future studies should endeavor to examine performance on the IGT in relationship to changes in cortical structure (e.g., cortical volume, thickness, or surface area; as well as diffusion tensor imaging metrics).
Highlights.
We examined longitudinal patterns of decision-making based on risk and reward using a modified version of the Iowa Gambling Task (IGT) in children who had sustained traumatic brain injury (TBI) and children with orthopedic injury (OI).
Longitudinal analysis of the pattern of change across two years revealed a three-way interaction among injury group, age, and interval-since-injury, indicating weak effects of age in the TBI group across the intervals, as compared to the OI group, which showed strong quadratic patterns across intervals that differed by age.
Analyses also revealed a three-way interaction among injury group, gender and interval-since injury, such that overall, males improved a great deal with time, but females showed small gains, regardless of injury group.
Acknowledgments
This research was supported by Grant Number R01NS021889 from the National Institute of Neurological Disorders and Stroke. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bechara A, Damasio AR, Damasio H, Anderson SW. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994;50(1–3):7–15. doi: 10.1016/0010-0277(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Damasio AR, Lee GP. Different contributions of the human amygdala and ventromedial prefrontal cortex to decision-making. J Neurosci. 1999;19(13):5473–5481. doi: 10.1523/JNEUROSCI.19-13-05473.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechara A, Damasio H, Tranel D, Damasio AR. Deciding advantageously before knowing the advantageous strategy. Science. 1997;275(5304):1293–1295. doi: 10.1126/science.275.5304.1293. [DOI] [PubMed] [Google Scholar]
- Catroppa C, Anderson V. Planning, problem-solving and organizational abilities in children following traumatic brain injury: intervention techniques. Pediatric Rehab. 2006;9(2):89–97. doi: 10.1080/13638490500155458. [DOI] [PubMed] [Google Scholar]
- Chapman SB, Sparks G, Levin HS, Dennis M, Roncadin C, Zhang L, et al. Discourse macrolevel processing after severe pediatric traumatic brain injury. Dev Neuropsychol. 2004;25(1–2):37–60. doi: 10.1080/87565641.2004.9651921. [DOI] [PubMed] [Google Scholar]
- Crone EA, Bunge SA, Latenstein H, van der Molen MW. Characterization of children’s decision making: sensitivity to punishment frequency, not task complexity. Child Neuropsychol. 2005;11(3):245–263. doi: 10.1080/092970490911261. [DOI] [PubMed] [Google Scholar]
- Crone EA, van der Molen MW. Developmental changes in real life decision making: performance on a gambling task previously shown to depend on the ventromedial prefrontal cortex. Dev Neuropsychol. 2004;25(3):251–279. doi: 10.1207/s15326942dn2503_2. [DOI] [PubMed] [Google Scholar]
- Dennis M, Guger S, Roncadin C, Barnes M, Schachar R. Attentional-inhibitory control and social-behavioral regulation after childhood closed head injury: do biological, developmental, and recovery variables predict outcome? J Int Neuropsychol Soc. 2001;7(6):683–692. doi: 10.1017/s1355617701766040. [DOI] [PubMed] [Google Scholar]
- Fay TB, Yeates KO, Wade SL, Drotar D, Stancin T, Taylor HG. Predicting longitudinal patterns of functional deficits in children with traumatic brain injury. Neuropsychology. 2009;23(3):271–282. doi: 10.1037/a0014936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garon N, Moore C. Complex decision-making in early childhood. Brain Cogn. 2004;55(1):158–170. doi: 10.1016/S0278-2626(03)00272-0. [DOI] [PubMed] [Google Scholar]
- Hanten G, Dennis M, Zhang L, Barnes M, Roberson G, Archibald J, et al. Childhood head injury and metacognitive processes in language and memory. Dev Neuropsychol. 2004;25(1–2):85–106. doi: 10.1080/87565641.2004.9651923. [DOI] [PubMed] [Google Scholar]
- Hanten G, Scheibel RS, Li X, Oomer I, Stallings-Roberson G, Hunter JV, et al. Decision-making after traumatic brain injury in children: a preliminary study. Neurocase. 2006;12(4):247–251. doi: 10.1080/13554790600910490. [DOI] [PubMed] [Google Scholar]
- Hanten G, Wilde E, Menefee DS, Li X, Lane S, Vasquez C, Hunter JV, Levin HS. Correlates of social problem-solving during the first year after traumatic brain injury in children. Neuropsychology. 2008;22:357–370. doi: 10.1037/0894-4105.22.3.357. [DOI] [PubMed] [Google Scholar]
- Hooper CJ, Luciana M, Conklin HM, Yarger RS. Adolescents’ performance on the Iowa Gambling Task: implications for the development of decision making and ventromedial prefrontal cortex. Dev Psychol. 2004;40(6):1148–1158. doi: 10.1037/0012-1649.40.6.1148. [DOI] [PubMed] [Google Scholar]
- Hooper CJ, Luciana M, Wahlstrom D, Conklin HM, Yarger RS. Personality correlates of Iowa Gambling Task performance in healthy adolescents. Personality and Individual Differences. 2008;44(3):598–609. [Google Scholar]
- Huizenga HM, Crone EA, Jansen BJ. Decision-making in healthy children, adolescents and adults explained by the use of increasingly complex proportional reasoning rules. Dev Sci. 2007;10(6):814–825. doi: 10.1111/j.1467-7687.2007.00621.x. [DOI] [PubMed] [Google Scholar]
- Kerr A, Zelazo PD. Development of “hot” executive function: the children’s gambling task. Brain Cogn. 2004;55(1):148–157. doi: 10.1016/S0278-2626(03)00275-6. [DOI] [PubMed] [Google Scholar]
- Kim YT, Lee SJ, Kim SH. Effects of the history of conduct disorder on the Iowa Gambling Tasks. Alcohol Clin Exp Res. 2006;30(3):466–472. doi: 10.1111/j.1530-0277.2006.00051.x. [DOI] [PubMed] [Google Scholar]
- Levin HS, Hanten G. Executive functions after traumatic brain injury in children. Pediatr Neurol. 2005;33(2):79–93. doi: 10.1016/j.pediatrneurol.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Levin HS, Hanten G, Roberson G, Li X, Ewing-Cobbs L, Dennis M, et al. Prediction of cognitive sequelae based on abnormal compted tomography findings in children following mild traumatic brain injury. J Neurosurg Pediatrics. 2008;1:461–470. doi: 10.3171/PED/2008/1/6/461. [DOI] [PubMed] [Google Scholar]
- Levin HS, Hanten G, Chang CC, Zhang L, Schachar R, Ewing-Cobbs L, et al. Working memory after traumatic brain injury in children. Ann Neurol. 2002;52(1):82–88. doi: 10.1002/ana.10252. [DOI] [PubMed] [Google Scholar]
- Levin HS, Hanten G, Zhang L, Swank PR, Ewing-Cobbs L, Dennis M, et al. Changes in working memory after traumatic brain injury in children. Neuropsychology. 2004;18(2):240–247. doi: 10.1037/0894-4105.18.2.240. [DOI] [PubMed] [Google Scholar]
- Levin IP, Hart SS. Risk preferences in young children: early evidence of individual differences in reaction to potential gains and losses. Journal of Behavioral Decision Making. 2003;16(5):397–413. [Google Scholar]
- Levine B, Black SE, Cheung G, Campbell A, O’Toole C, Schwartz ML. Gambling task performance in traumatic brain injury: relationships to injury severity, atrophy, lesion location, and cognitive and psychosocial outcome. Cogn Behav Neurol. 2005;18(1):45–54. [PubMed] [Google Scholar]
- Overman WH, Frassrand K, Ansel S, Trawalter S, Bies B, Redmond A. Performance on the Iowa card task by adolescents and adults. Neuropsychologia. 2004;42(13):1838–1851. doi: 10.1016/j.neuropsychologia.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Romer D, Betancourt L, Giannetta JM, Brodsky NL, Farah M, Hurt H. Executive cognitive functions and impulsivity as correlates of risk taking and problem behavior in preadolescents. Neuropsychologia. 2009;47(13):2916–2926. doi: 10.1016/j.neuropsychologia.2009.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachar RJ, Levin HS, Max JE, Purvis KL, Chen S. Attention deficit hyperactivity disorder symptoms and response inhibition after closed head injury in children: do preinjury behavior and injury severity predict outcome? Developmental Neuropsychology. 2004;25:179–198. doi: 10.1080/87565641.2004.9651927. [DOI] [PubMed] [Google Scholar]
- Schmidt AT, Hanten G, Li X, Orsten KD, Levin HS. Emotion recognition following pediatric traumatic brain injury: Longitudinal analysis of emotional prosody and facial emotion recognition. Neuropsychologia. 2010;48:2869–2877. doi: 10.1016/j.neuropsychologia.2010.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein DG, Wright DW, Kellerman AL. Does progesterone have neuroprotective properties. Ann Emerg Med. 2008;51(2):164–172. doi: 10.1016/j.annemergmed.2007.05.001. [DOI] [PubMed] [Google Scholar]
- Suhr JA, Tsanadis J. Affect and personality correlates of the Iowa Gambling Task. Personality and Individual Differences. 2007;43(1):27–36. [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- van Leijenhorst L, Crone EA, Bunge SA. Neural correlates of developmental differences in risk estimation and feedback processing. Neuropsychologia. 2006;44(11):2158–2170. doi: 10.1016/j.neuropsychologia.2006.02.002. [DOI] [PubMed] [Google Scholar]
- van Leijenhorst L, Westenberg PM, Crone EA. A developmental study of risky decisions on the cake gambling task: age and gender analyses of probability estimation and reward evaluation. Dev Neuropsychol. 2008;33(2):179–196. doi: 10.1080/87565640701884287. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10(3):412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term neuropsychological outcomes after traumatic brain injury in children. Neuropsychology. 2002;16(4):514–523. doi: 10.1037//0894-4105.16.4.514. [DOI] [PubMed] [Google Scholar]