Abstract
Mandibular trauma is a common problem seen by plastic surgeons. When fractures occur, they have the ability to affect the patient's occlusion significantly, cause infection, and lead to considerable pain. Interventions to prevent these sequelae require either closed or open forms of reduction and fixation. Physicians determining how to manage these injuries should take into consideration the nature of the injury, background information regarding the patient's health, and the patient's comorbidities. Whereas general principles guide the management of the majority of injuries, special consideration must be paid to the edentulous patient, complex and comminuted fractures, and pediatric patients. These topics are discussed in this article, with a special emphasis on pearls of mandibular trauma management.
Keywords: Mandible, occlusion, plating, closed reduction, IMF, MMF, lag screws, facial trauma, maxillofacial
Mandibular fractures play a significant role in craniofacial trauma and have accounted for nearly 50% of the facial fractures that we have encountered at the Texas Medical Center, thus making it the most commonly fractured facial bone at our center.1 At other centers, however, mandible fractures play less of a prominent role and have accounted for ∼20% of facial fractures. Treatment of these injuries is important to maintain proper speech, swallowing, and masticatory function of the lower jaw. To better understand how to do this, however, one needs a solid understanding of several key topics.
EPIDEMIOLOGY
Seventy percent to 85% of mandibular fractures occur in males, with the majority occurring in individuals in their twenties and thirties.2,3,4 The most common causes are aggravated assaults and motor vehicle collisions (MVCs) in males, and falls and MVCs in females.2,3,4,5 Other common causes include sporting activities and gunshot wounds. The mechanism of injury is important to take into consideration as it provides the physician with an index of suspicion for concomitant injuries, which may delay repair or necessitate a different treatment modality. MVCs and gunshot wounds, for example, because of the nature of the forces created, tend to be the most destructive to the craniofacial skeleton.2,6
Concomitant injuries are important in judging the gravity of the clinical scenario, because as one study showed, whereas the mortality of patients admitted for maxillofacial trauma with isolated mandibular fractures is fairly low (1.6%), when combined with fractures of regions of other areas of the face, the mortality is substantially higher (∼25%) (Table 1).7
Table 1.
Mortality Rates Associated with Various Mandibular Fracture Patterns Based on a 3-Year Retrospective Review of Facial Fractures That Resulted in Hospital Admission and Trauma Service Consult
| Fracture Pattern | Mortality Rate (%) |
|---|---|
| Isolated mandibular fracture | 1.60 |
| Mandible and midface | 28.20 |
| Mandible and upper facial skeleton (n = 1) | 100 |
| Mandible, midface, and upper facial skeleton | 25 |
Source: Based on data from Plaisier BR, Punjabi AP, Super DM, Haug RH. The relationship between facial fractures and death from neurologic injury. J Oral Maxillofac Surg 2000;58:708–712.
Other injuries frequently occur with mandibular fractures as well. Studies have reported that the incidence of C-spine injuries in patients presenting with facial fractures ranges from ∼2 to 10% (whereas there is an inverse relationship between mandibular fractures and intracranial pathology).8,9,10,11,12 Additionally, 32% of mandibular fractures are associated with abrasions or lacerations, 24% with neurologic injury, 20% with additional orthopedic injuries, and 12% with pulmonary, abdominal, or cardiac injury. Once again, though, the overall incidence of these accompanying injuries will differ based on the initial mechanism of injury.2,13
ANATOMY
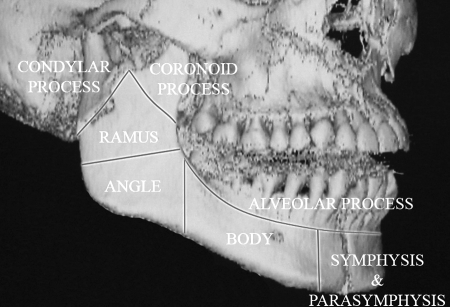
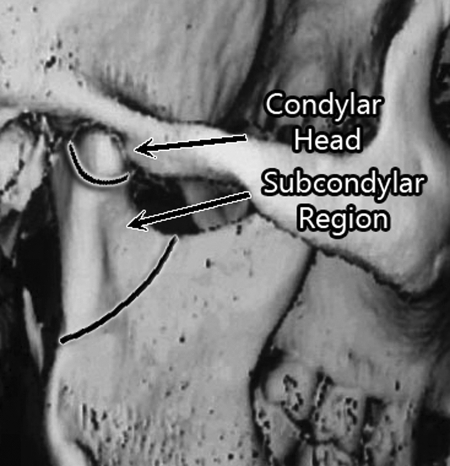
The mandible is a “U-shaped” bone that articulates with the cranial base at the temporomandibular joints (TMJs), and forms a functional interface with the maxilla via the dental occlusion. The symphysis, parasymphysis, and mandibular body can be differentiated from other regions of the mandible because of a ridge of compact cortical bone (alveolar ridge) located on its cranial aspect that allows for tooth-bearing (Fig. 1). This horizontally oriented tooth-bearing portion then becomes vertically oriented to form its articulation with the cranium. The change in orientation occurs at the mandibular angle, and subsequently the mandible continues as the mandibular body and condyle as it travels cranially to articulate with the cranial base and forms the TMJ. This condyle can further be divided into the condylar (intracapsular) and subcondylar regions (extracapsular) (Fig. 2).
Figure 1.
Regions of the mandible include symphysis, parasymphysis, body, angle, subcondylar and condylar regions, and alveolar ridge.
Figure 2.
The mandibular condyle can be divided into the condylar (intracapsular) and subcondylar (extracapsular) regions.
The entire mandibular structure is bicortical, with a thin medullary cavity that allows for passage of the inferior alveolar nerve and artery. The inferior alveolar neurovascular bundle courses from the mandibular foramen to the mental foramen and provides sensation and blood supply to the mandible and its dentition.
Along the entire course of the mandible are muscle attachments that place dynamic internal forces on the mandible. These muscles can be divided into two basic groups: muscles of mastication and suprahyoid muscles. The muscles of mastication include the medial and lateral pterygoids, the temporalis, and masseter muscles. Together these muscles aid in chewing by generating forces along the posterior aspects of the mandible (angle, ramus, coronoid process). Furthermore, two of the muscles of mastication, the medial pterygoid and masseter muscles, combine to form the pterygomasseteric sling, which attaches at the mandibular angle. Conversely, the suprahyoid group (digastric, stylohyoid, mylohyoid, and geniohyoid) functions, in part, to depress the anterior mandible by applying forces to the mandibular symphysis, parasymphysis, and a portion of the body. Together, these muscle attachments act to place dynamic vectors of force on the mandible that, when in continuity, allow for proper mandibular function, but when in discontinuity, as occurs with mandible fractures, can potentially disrupt appropriate fracture healing.
CLINICAL EVALUATION
The most important factor in deciding whether or not a mandible fracture requires a surgical intervention is the status of the occlusion, which can be abnormal in more than 80% of mandibular fractures.14 The occlusion can be evaluated by asking the patient if his or her bite has changed since the injury. If this basic information cannot be obtained, examination of wear facets or assessing old dental records can be helpful. Determining the type of occlusion prior to trauma is important, because the subsequent goal of any surgical intervention will be to restore the preinjury occlusion, even if the preinjury occlusion was abnormal.
The patient's occlusion can be systematically classified using the Angle classification system, the lingual-labial/buccal relationship, and the vertical relationship between the maxillary and mandibular teeth (Fig. 3; Table 2). The vertical height of each hemi-mandible can then be assessed for shortening or cant by placing a tongue depressor between the teeth when in occlusion and examining the horizontal orientation of the tongue depressor.
Figure 3.
Evaluation of the occlusion requires looking at several aspects.
Table 2.
The Occlusion Can Be Classified in a Systematic Manner Using the Angle Classification System, the Lingual-Labial/Buccal Relationship, and the Vertical Relationship between the Maxillary and Mandibular Teeth
| Classifying the Occlusion | |
|---|---|
| Angle classification | |
| Class 1 occlusion | Mesiobuccal cusp of 1st molar occludes into buccal groove |
| Class 2 occlusion | Mesiobuccal cusp of 1st molar lies mesial to the buccal groove |
| Class 3 occlusion | Mesiobuccal cusp of 1st molar lies distal to the buccal groove |
| Lingual-labial/buccal relationship | |
| Normal | Maxillary teeth are located slightly labial/buccal to mandibular teeth |
| Anterior crossbite | Anterior maxillary teeth located lingual to mandibular teeth |
| Posterior crossbite | Posterior maxillary teeth located lingual to mandibular teeth |
| Vertical relationship | |
| Normal | Incisal edges of the anterior maxillary teeth extend 2 to 3 mm below the incisal edges of the mandibular teeth |
| Open bite | Lack of occlusal contact between maxillary and mandibular dentition |
| Overbite | > 3 mm of vertical overlap |
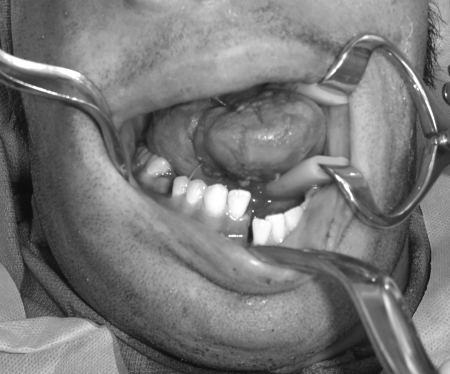
A complete physical examination, including inspection, palpation, sensation, and range of motion, should also be performed. Abnormal changes in dentition need to be noted, as well as any associated injury to the mental nerve. The latter is particularly important to differentiate trauma-related injury from iatrogenic injury postoperatively. Other associated injuries need to be evaluated as well, including intraoral soft tissue injuries (Fig. 4) and the common concomitant injuries mentioned previously.
Figure 4.
Intraoral soft tissue injuries and lacerations need to be evaluated for and addressed preoperatively, if possible.
Imaging of the mandible for fractures is best performed with high-resolution computed tomography (CT) images, whereas for dentition-related injuries, the Panorex is the best. Panorex imaging has the ability to image the tooth roots, which will ultimately help in plate positioning for fixation. For patients that are unable to stand and obtain Panorex imaging, use of the “Zonarc” may be an alternative option. This equipment uses the same principles behind panoramic imaging to create an adequate imaging study for patients that are unable to stand or sit in an upright position. This is extremely beneficial in unstable patients (as often seen in the trauma setting) who require imaging. Magnetic resonance imaging also has a role in mandibular trauma, as it is particularly useful for evaluation of the TMJs and condyles.
TIMING OF TREATMENT
Optimal treatment timing must take into consideration the type and severity of injury. Concomitant injuries that require attention for patient stabilization need to be addressed in an expeditious manner, prior to management of mandibular fractures.
Studies looking at the relationship between timing of surgery and subsequent outcomes have demonstrated no difference in infectious/nonunion complications between treatment within or after 3 days status postinjury but did find that complications because of technical errors increased after this time.15 As a result, the authors commented that if surgery was to commence 3 or more days after the injury, a technically accurate surgery by the surgeon is necessitated to overcome factors such as tissue edema and inflammation. In cases where a delay in treatment is necessary, consideration should be given for temporary closed fixation to reduce fracture mobility and patient pain.
TREATMENT TYPES
Treating mandibular fractures involves providing the optimal environment for bony healing to occur: adequate blood supply, immobilization, and proper alignment of fracture segments. As a result, most fractures require reduction and fixation to allow for primary or secondary bone healing. The one exception is the unilateral subcondylar fracture in the patient with a normal occlusion, which we shall discuss later.
Secondary bone healing occurs when fractured bone segments are placed in approximation, stabilized with allowance for some degree of micromotion, without significant devascularization of bone segments. Subsequently, bony healing occurs through a callous intermediate and ensuing ossification. This form of fixation can be performed with either intermaxillary fixation/maxillomandibular fixation (IMF/MMF) with arch bars, 4-point fixation, occlusal splints, or miniplates.
Primary bone healing with rigid fixation bypasses the callous intermediate by approximation and fixation, which inhibits micromotion of the fracture site. This is primarily performed via the application of plates (except for miniplates) and screws to the fracture site but ultimately results in a variable degree of periosteal undermining, which may compromise the vascularity of the injured bone segments.
There are advantages and disadvantages to both methods of fixation. Closed reduction does not traumatize the vascular envelope and is less expensive for the patient; however, it is associated with a significant period of immobilization and closure of the oral cavity, and requires intact dentition or some form of dental records. Open reduction and internal fixation (ORIF), in contrast, allows for direct visualization and reduction of fractured bone segments and restoration of the patient's preinjury occlusion without complete fixation of the mandible and maxilla. This allows for bony healing in a shorter period of time, which gives rise to the patient's earlier return to normal jaw function and better nutrition and oral hygiene. It is important to note, however, that potential foreign body infections are more likely with this technique.16 Additionally, studies that have examined the complications with both techniques have shown that ORIF is associated with increased morbidity, and although this can be explained by vascularity changes caused by the intervention, because there has not been a randomized study comparing the two. This could also be because ORIF is usually used in more severe injuries.17
Another important factor to take into consideration is patient compliance. One study noted that up to 60% of patients being treated for facial fractures can be noncompliant in some form.18 Determining those who are likely to be noncompliant is important when deciding between IMF/MMF or ORIF, as these patients are best treated with ORIF to reduce the risk of premature release of IMF/MMF and subsequent complications.
IMF/MMF is also a reasonable option for those at an increased risk for complications with ORIF (see the “Complications” section); however, there is considerable overlap between this at-risk group for complications and the at-risk group for noncompliance, and IMF/MMF may not be the best option for long-term outcomes. At this point, a thorough assessment should be made and a thorough discussion held with the patient to determine the best treatment method. The decision regarding compliance and choice of reconstruction is extremely important as the cause of many facial fractures (aggravated assault, fights, alcohol/drugs, etc.) already indicates a high likelihood of noncompliance.
Closed Reduction
IMF/MMF is a technique to immobilize the fractured segments of the mandible by externally locking the occlusion into place, using the dentition as a point of stability. The two terms refer to the same method of fixation, but the former is a vestige from a time when the mandible was considered the lower maxilla, and thus fixation occurred in an “intermaxillary” fashion.
Fixation with IMF/MMF can be performed in several ways. First, Kirschner wires can be used in either the Gilmer or Eyelet method to provide fixation. These methods differ in that the Eyelet method can allow for the removal of wires for inspection of the mandible without removing the intermaxillary ligatures. Erich arch bars provide the next level of IMF/MMF stability, alignment, and control and have become the standard of care for treatment with IMF/MMF, as they provide an additional structure for fixative support besides the dentition (Fig. 5). In cases where supplemental fixation is necessary, however, adjacent structures can be used to fixate the occlusion.
Figure 5.
The Gilmer method of IMF/MMF can be used along with Erich arch bars to provide additional stability, alignment, and control to the occlusion and fracture segments.
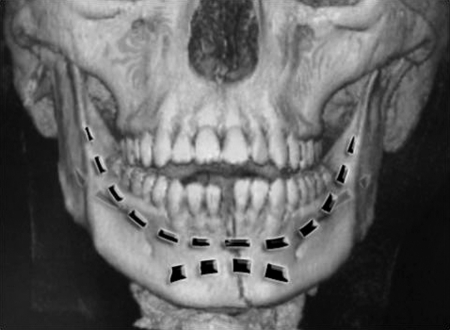
Additional stability of the occlusion can be obtained by placing wires that fixate the maxilla superiorly around the pyriform aperture and inferiorly around the mandibular border. Additionally, screws can be used to provide “4-point” fixation in these regions as well (Fig. 6). Screws can be placed into the maxilla and mandible in a bilateral fashion and wires subsequently used to fixate both the right and left hemi-mandibles using these fixation points. This technique is advantageous because it can be applied rapidly; however, it does not provide stabilization within the dental arch and also increases the risk of tooth injury. These additional forms of fixation are necessary, though, when inadequate stability is provided by the dentition, such as in the edentulous mandible in the elderly or the deciduous/transitioning dentition of the pediatric population.
Figure 6.
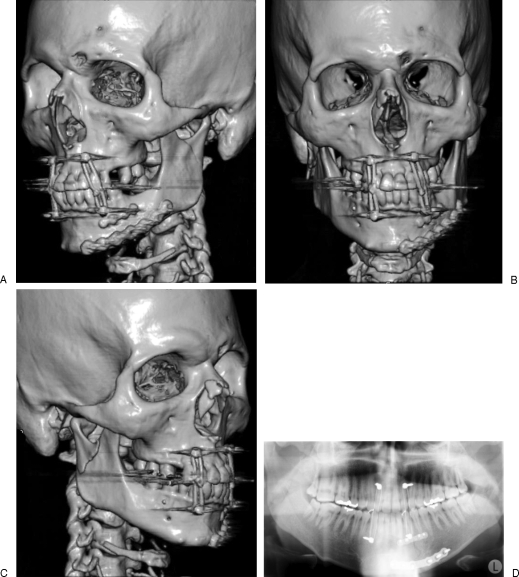
(A–D) Four-point screw fixation can also be used to stabilize the occlusion and maintain IMF/MMF.
Acrylic occlusal splints are also used to establish continuity of the dental arches in cases of discontinuity.19 Cases where these may be beneficial are when there are missing teeth or concomitant fractures of the alveolus that require stabilization within the maxillary or mandibular arch prior to IMF/MMF. These splints are wired into place and allow for accurate dental alignment while healing occurs.
A major downfall of any closed technique is the presence of soft tissue, bony fragments, or hematoma in the fracture site that prevents anatomic reduction. This may be less of an issue in the mandible as occlusion is the ultimate reduction measure, but if preinjury occlusion cannot be obtained with closed reduction, the fracture site may need to be cleaned of debris.
Open Reduction and Internal Fixation
Plates and screws function to rigidly fixate and prevent any motion of fracture segments by absorbing all or part of the functional load that is present at a fracture site. Subsequently, several principles underlie the decision-making process for mandibular fracture repair. Choices must be made regarding the proper plate length and thickness required, and what type and size of screws to use.
First, plate length is generally determined to allow for the placement of more than one screw on either side of the fracture to nullify the dynamic forces that act on the mandible. In ideal conditions, three screws are placed on either side of the fracture segments to allow for assurance against inadequate stabilization, with screws placed at least several millimeters from the fracture site.
Next, proper plate thickness is determined by the forces required to stabilize fractured bone segments. Options for stabilization can be divided into either load-sharing fixation (miniplates, 1.0-mm profile; universal fracture locking/nonlocking plates, 1.5-mm profile; lag screws) or load-bearing fixation (locking and nonlocking reconstruction (recon) plates, 1.5-, 2.0-, 2.5-, or 2.8-mm profile). These options differ in their internal screw diameter, thickness, surface area of in-contact bone (footprint), titanium grade, malleability, and in their ability to stabilize the bone segments against the intrinsic forces on the mandible. These characteristics, in general, increase as one progresses from miniplates, to normal fracture/locking plates, to recon plates.
Deciding between these forms of rigid fixation is based on both the bone quality of the fractured segments and the intrinsic forces on the mandible. If bone quality is poor, such as with significant comminution, defects, or atrophy, then load-bearing fixation will be needed for stabilization. For other situations, such as with young healthy male patients, stronger plates and extra screws will be necessary because of greater bite forces that are placed on the mandible. Miniplates, with decreased thickness, footprint, titanium grade, and increased malleability, are best used along areas of the mandible that are subjected to smaller degrees of forces. In 1978, Champy et al further defined these regions of the mandible that would only require monocortical plates to allow for stable fixation along the symphysis, parasymphysis, and angle of the mandible.20 These regions have subsequently been called Champy's lines of tension, with the superior portion of lines also referred to as the tension band of the mandible (Fig. 7).
Figure 7.
Champy's lines of tension correspond with biomechanically favorable regions of the mandible where less stability would be required to allow for fracture healing.
More recently, locking plates have been introduced that allow for the screw head to be “locked” into the plate, thus turning the plate and screw apparatus into an internal-external fixator. There are both theoretical and biomechanical advantages to this technique, including a lower risk of malocclusion secondary to inappropriate plate contouring, a lower frequency of screw loosening, ease of use, and reduced time for application.21 Additionally, studies have demonstrated its use and clinical safety22; however, a clear benefit over nonlocking plates and screws has not been definitively demonstrated.23 Although this technique of rigid fixation has become the status quo for fracture fixation, it is worth noting that one downside is that surgeons may get decreased sensory feedback regarding adequate bone purchase because of the design of the plate and screws.
As touched upon earlier, prior to ORIF complete cleaning of the fracture site is an essential and often overlooked first step. This can be accomplished by recreating the fracture after retracting the soft tissue and stripping the periosteum with elevators, synovial rongeurs, or a simple curved hemostat. A few minutes spent removing debris, soft tissue, hematoma, and fracture callous prevents frustration and problems obtaining occlusion/anatomic bony reduction, ultimately yielding a better outcome.
During plate placement, holding reduction, or more importantly occlusion, while drilling and placing screws, is of utmost importance. If the plan includes postoperative maintenance of IMF/MMF, then the arch bars should be placed prior to attempting ORIF and the IMF/MMF can hold occlusion while plating. However, one of the benefits of plate fixation is to absolve the need for IMF/MMF, as spending valuable operating room time placing arch bars only to remove them after plating can be tedious and time consuming. In these cases, where postoperative IMF/MMF is not indicated, it may be possible to use manual occlusal reduction, temporary 4- or 6-point IMF/MMF with screws, bone reduction forceps, or, most commonly, a combination of these. These techniques not only save time but also allow for rapid removal and checking of occlusion after placement of each screw to ensure sequential and incremental increases in alignment and stability. A potential pitfall can arise if the manual reduction or 4-point fixation is too close to the midline/focused on the inferior border of the parasymphyseal region, as this vector tends to open up the inferior border of the posterior body or mandibular angle fractures. This can be avoided with bilateral manual pressure distributed across the body and symphysis or properly spaced (between canine and bicuspid) 4-point IMF/MMF. However, placing the patient in IMF/MMF with arch bars and wires will always be the best way to guarantee occlusional integrity during fracture plating.
Screw choice will also require some thought. Screws can vary based on their amount of cortical bone purchase, and are termed monocortical and bicortical screws. Monocortical screws only travel through one of the bony cortices because of their decreased length. Subsequently, the screws are helpful in areas with important underlying structures, such as tooth roots, or the inferior alveolar neurovascular bundle; however, the limited bony purchase results in only functionally stable fixation, and thus must be placed along areas of less dynamic tension, such as Champy's lines.
Screws can also vary based on their diameter. In general, as the screw's diameter increases, so does the stability against the forces on the mandible. Subsequently, smaller screws (2.0 mm) are effective for simple fractures, and screws of larger diameters (2.3 mm) are better suited for comminuted or multiple fractures. The Stryker mandibular plating system has 2.0-, 2.3-, and 2.7-mm screws that can be used in any one of their plates (miniplates, recon plates, etc.). However, in general, the heavier the plate used, the thicker the screw should be.
When placing screws, it is important to work from the screw holes nearest the fracture outward to avoid splaying the fracture site, as can happen when working in the opposite direction. Using a threaded drill guide is important when using locking plates, as it ensures that you are within the angulation tolerances of the threading on the plate, and occlusion will not be altered when tightening that screw. If you freehand a hole that is angulated more than the plate can tolerate, the screw can be forced into conforming within the tolerances of the plate hole, and subsequently after the occlusion.
Screws can be also be applied without the use of plates. Lag screws are specialized screws that can stabilize simple fractures, and are placed at a 90-degree angle to the fracture in a plane that is parallel to the long axis of the bone. To prevent rotational and other forces from disrupting the rigid fixation of the fracture site, at least two screws are needed for stabilization. The proper use of lag screws, and the many other fixation methods mentioned previously, depends on the fracture site and type.
Fracture Management Based on Location
SYMPHYSIS/PARASYMPHYSIS
Fractures in this region can generally be managed in three ways. First, symphyseal and parasymphyseal fractures, even if displaced, do not need to be treated with internal fixation. Because this is a tooth-bearing region, MMF with arch bars can be used to reestablish and fixate the occlusion. Internal fixation can be used, however, and two methods for treatment exist, with both using an intraoral approach. One method is to place lag screws across the defect (Fig. 8). The other is to fixate the fractured segments using a plate placed monocortically at the superior border or tension band (to prevent damage to underlying tooth roots), and a second plate at the inferior border, placed bicortically (Fig. 9). In general, there is more room to work in this central region of the mandible as the tooth roots are vertically short, and the mental nerve can be mobilized and retracted to allow for appropriate visualization and fixation.
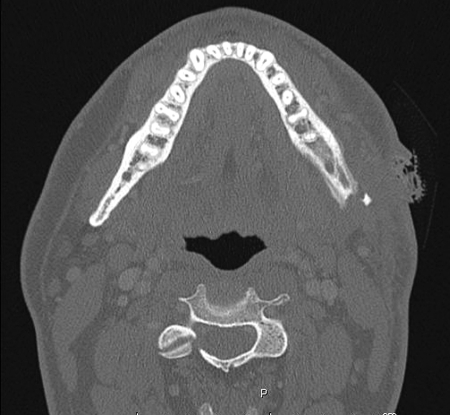
Figure 8.
(A–E) A young female patient suffered an oblique fracture through the symphysis/parasymphysis. This was subsequently treated with lag screws that were placed perpendicular to the fracture site. Postoperative reduction films demonstrate nearly perfect reduction.
Figure 9.
(A, B) An additional method to manage symphyseal/parasymphyseal fractures is through superior border monocortical and inferior border bicortical plating.
When fixating the region, it helps to temporarily fix the inferior border with bone clamps and then plate the superior border. The temporary fixation can then be released and the inferior border plated. The two points of fixation are necessary to prevent rotational forces from causing the superior border from splaying and disrupting the continuity of the alveolar arch. Arch bars or dental splints can also serve as the tension band for the region; however, it is important to use an arch bar that is strong enough to last for the period of fracture healing. After reduction and fixation, it is important to examine both the lingual and buccal aspects of the mandible, as inappropriate plate bending (with nonlocking plates) can cause gapping on the lingual aspect of the mandible, resulting in a cross-bite and an increase in mandibular width. Additionally, if multiple areas require fixation, it is important to check the occlusion after every plate is applied.
BODY
Fractures in the mandibular body are generally managed with a greater degree of caution because of the neighboring structures in the region. Like fractures in the symphyseal and parasymphyseal regions, these fractures within the tooth-bearing segments of the mandible can be treated with closed reduction and fixation. When internal fixation needs to be performed, these fractures are generally repaired using an intraoral approach. An extraoral approach may be required, however, for isolated fractures that are located along the posterior and inferior aspects of the mandibular body, as an intraoral incision does not provide enough visualization to rule out gapping after fracture reduction.
Treatment generally involves plating a monocortical miniplate along the superior border or tension band and a bicortical miniplate along the inferior border (Fig. 10). During the repair, several key anatomic features must be respected. The inferior alveolar nerve and artery must be identified, as well the smaller distance between the tooth roots and inferior mandibular border, because of the greater space taken up by the tooth buds.
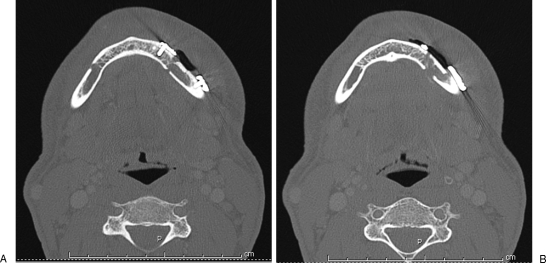
Figure 10.
(A, B) Body fractures can also be plated in accordance with Champy's lines of tension, with superior border monocortical plating and inferior border bicortical plating.
ANGLE
Angular fracture management is nuanced because of the inferior alveolar nerve and artery, and the variable presence of the third molar or wisdom tooth. Although removal criteria for impacted third molars are generally agreed upon (including infected, grossly mobile, or inhibiting fracture reduction), certain situations that do not meet these criteria need to be managed on a case-by-case basis. If a third molar is to be removed in mandibular angle fractures, these should generally be removed only after fracture reduction and fixation; however, in cases where the tooth is preventing fracture reduction, removal may be necessary prior to fixation.
The ideal surgical management involves using either an intraoral approach with or without transbuccal trochar instrumentation (for screw placement along the posterior and inferior aspects of the angle) or an extraoral approach (for comminuted and complex fractures). When combining an intraoral approach with a transbuccal trochar, placement of the trochar is essential. Frequently, a single access point will work for most but not every screw hole. Using the same incision to affix the entire plate will often work, as one can reposition the trochar by altering its course through the buccinator and buccal mucosa; however, struggling with a trochar that is severely angulated and that is placing extreme traction against the soft tissues simply increases surgeon frustration. This may also in fact do more damage to the soft tissue versus another tunnel, and makes subsequent successful screw placement difficult or impossible.
Fixation then requires either placing a miniplate along the oblique ridge of the mandible (Champy technique) with or without a miniplate along the inferior border, placing a strut plate (two miniplates buttressed with perpendicular strut bars) along the lateral aspect (Fig. 11), or placing a recon plate in cases of significant comminution or poor bone stock. Preference toward stabilization with a strut plate versus plating the oblique ridge should occur in situations of individuals that are able to generate significant bite forces, as stabilization along the oblique ridge does not provide fixation that is as rigid.
Figure 11.
(A–D) Strut plates (Stryker, Kalamazoo, MI) can be used for treating mandibular fractures when requiring more stability than that provided by a single plate along the oblique ridge.
RAMUS
Mandibular ramus fractures can be managed with either rigid fixation or functionally stable fixation. In cases of nondisplaced fractures, some individuals have advocated for treatment using IMF/MMF, albeit for a longer period of time (6 to 8 weeks); however, in our experience, we have found this to be an inadequate form of fixation as the stabilization affects the portions of the mandible involving the alveolar arches and fails to fully stabilize the posterior portions of the mandible against the intrinsic forces of the pterygomasseteric sling. Subsequently, consideration should be given toward ORIF, increasingly so as fractures descend along the ramus. Exposure of this region can involve either a preauricular or a submandibular approach (based on fracture location); however, both may be necessary in significantly comminuted fractures.
CORONOID
Coronoid fractures are generally stabilized by the insertion of the temporalis muscle. Subsequently, if the fracture is isolated, and the patient can open and close his or her mouth without difficulty, then conservative treatment is the best option. In the rare situation where a patient is unable to go through a range of motion or is limited by pain, ORIF is the best method for management.
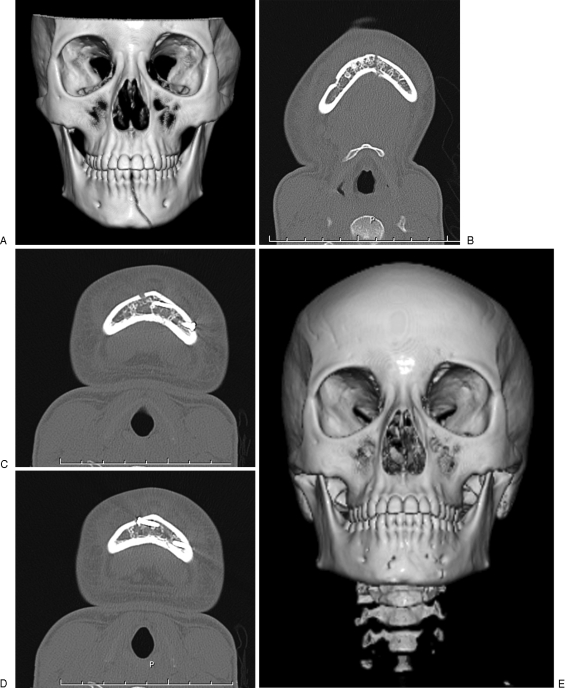
CONDYLE
The management of condylar fractures varies based on the specific location of the injury. Management options have historically been either an open approach, open with endoscopic approach, or closed approach, and investigators have made arguments for each modality.24 Generally speaking, though, the optimal management differs based on the location of the fracture. Condylar fractures involving the capsule of the TMJ (Fig. 12) are significant because of the associated risk of TMJ ankylosis, and it is generally understood that a conservative approach of IMF/MMF for 7 to 10 days with an early return to function is the best treatment option.25 This is probably due to a combination of the devascularization necessary to plate this distal segment and the difficulty associated with gaining stability of a small distal segment through ORIF.
Figure 12.
Intracapsular condylar fractures are usually managed with a conservative approach with IMF/MMF and an early return to function to reduce the risk of subsequent TMJ ankylosis.
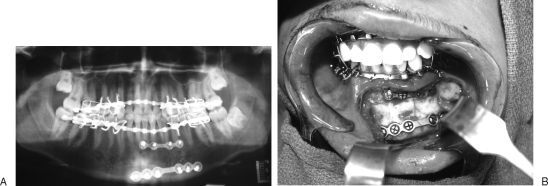
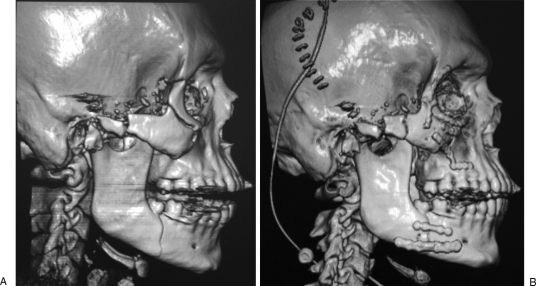
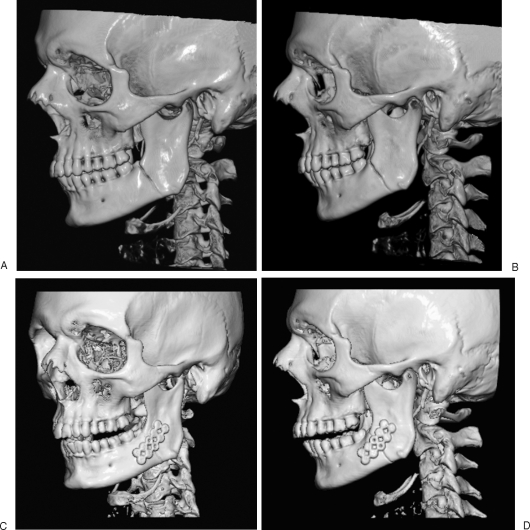
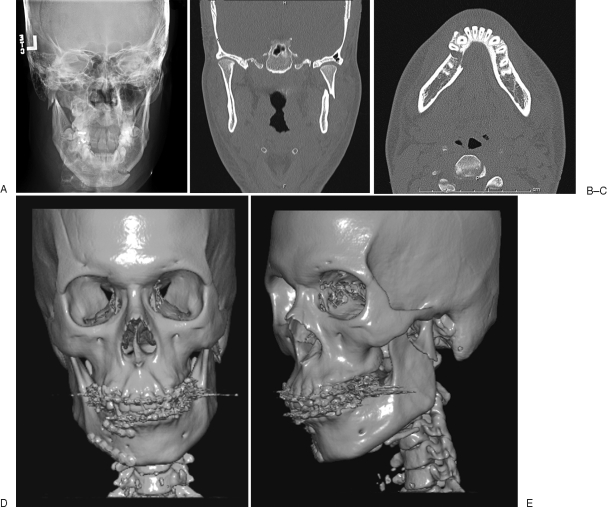
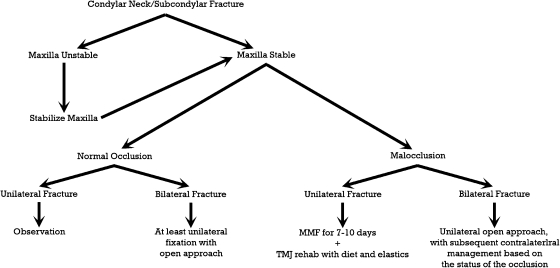
Subcondylar fractures are an area of greater contention. Both closed and ORIF methods of treatment have been described (Fig. 13), and although several studies have demonstrated superior results and fewer complications with ORIF,24,26,27,28,29,30,31 many other aspects must be considered. The open approach requires a significantly greater degree of expertise and carries a significant risk of facial nerve traction injury because of a required extraoral approach (Fig. 14). Though the injury is usually temporary, the uncertain period of time spent waiting for resolution can be stressful for both the physician and patient. Because of these concerns, we now use an algorithm for the management of these fractures, which takes into account the stability of the maxilla, the status of the occlusion, and the laterality of the injury (Fig. 15).
Figure 13.
(A–E) Subcondylar fracture and accompanying parasymphyseal fracture that were treated with IMF/MMF and superior and inferior border plating of the parasymphyseal fracture. Treating subcondylar fractures with a closed approach is often the best approach.
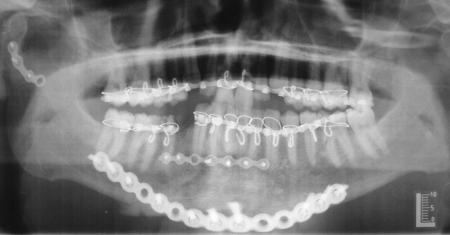
Figure 14.
Panorex demonstrating ORIF of a subcondylar fracture. The open approach requires a significantly greater degree of expertise, is technically more challenging, and carries a significant risk of a facial nerve traction injury.
Figure 15.
Algorithm for management of subcondylar fractures based on the stability of the maxilla, the status of the occlusion, and the laterality of the injury.
Maxillary stability is the most important issue when formulating a management plan. If the maxilla is stable, then management differs based on whether the fracture is unilateral (with or without malocclusion) or bilateral. In cases of unilateral subcondylar fractures with a normal/stable occlusion, the patient can be safely managed with observation. In cases of unilateral subcondylar/neck fractures with malocclusion, patients can be treated with IMF/MMF for 7 to 10 days, followed by TMJ rehabilitation with a soft diet and elastics. If the fracture is bilateral, at least one side needs to be fixated using an open approach. Subsequently, the contralateral side can be managed with an open approach or be treated in a similar manner to a unilateral fracture with management based on the status of the occlusion. In cases of unilateral or bilateral subcondylar/neck fractures where the maxilla is unstable, the management will be similar; however, the first step in management will be to stabilize the maxilla with plating techniques.
It is important to recognize that treatment of subcondylar fractures via a closed approach does not equal “closed reduction” as the majority of subcondylar fractures remain displaced after placement in IMF/MMF. However, with the patient maintained in occlusion by IMF/MMF and then likely elastics, the bone can begin callous formation, and subsequently the soft tissue envelope and musculature is trained to maintain a good occlusal relationship in the closed position.
ORIF of these fractures generally involves either a retromandibular and/or preauricular approach, but despite the combination of these incisions, visualization can still be difficult. Mobilization and adequate reduction of the fracture segments can be facilitated by placing bone clamps on the inferior fracture segment via the submandibular incision and by placing a small lag screw superficially through the superior segment outside of the TMJ capsule via the preauricular incision. The lag screw helps to manipulate the bone to achieve adequate reduction. Additionally, because of the issues with getting adequate visualization and access, there is usually only enough room to place one plate, and two screws on either side of the fracture.
Common Combinations
Mandibular fractures are rarely isolated and are commonly present at two or more fracture sites. Studies have shown that, because of the mandible's biomechanics, roughly half of all mandibular injuries involve more than one fracture, occurring in a coup-contrecoup fashion.4 Multiple fractures are significant as they have been associated with the highest risk for postsurgical sequelae, such as persistent pain, malocclusion, and facial contour deformity.32 One common example of this type of fracture injury is the combined body/symphyseal and contralateral subcondylar injury, often seen with direct blows (Fig. 13). In these cases, management uses principles similar to isolated mandibular fractures; however, larger stabilizing forces are required for at least one of the fracture sites because of biomechanical changes, and greater consideration should be given to recon plate placement.
Special Conditions
EDENTULOUS MANDIBLE
Recent studies have estimated that ∼8% of the adult population is edentulous in the United States, and this state is thought to be related to subsequent mandibular atrophy.33 This edentulous/atrophic population deserves special consideration for management of mandibular fractures for several reasons. First, these individuals tend to have other systemic comorbidities that need to be managed,34 as well as a poorer baseline nutritional status. Second, obtaining preinjury occlusion can be difficult, as the lack of dentition prevents individuals from noticing subtle changes in their teeth and prevents physicians from identifying wear facets; however, one trick is to use the patient's dentures, if available, to determine the preinjury occlusion.
There is also an inverse relationship between mandibular bone height and the rate of fibrous union/nonunion and infection after mandibular fracture.35 Subsequently, despite being generally poor operative candidates, because of the increased risk for fibrous union/nonunion, ORIF becomes a necessity. Furthermore, the poor bone stock associated with the mandibular atrophy often requires load-bearing fixation in the form of recon plates and usually requires an extraoral approach with or without an intraoral approach to be technically manageable, given the size of the plate and the generally limited visualization of the posterior aspects of the mandible via an intraoral approach.34 The underlying decrease in mandibular height in this population is important to be considered when treating this population, as there is often enough room for only one plate to be placed.
The edentulous mandible has one opportunity at being repaired. It is counterintuitive that a thinner, weaker bone without teeth requires the most aggressive ORIF, with the thickest and longest reconstruction plate possible, but any complication simply cannot be tolerated. With already weak bone stock, plates must be thicker to support the full load. Additionally, the plates must be longer and be able to hold an increased number of screws to distribute this force over a larger area to prevent secondary loosening or additional fractures postoperatively. Edentulous fractures are the only situation where fracture reduction and meticulous plate choice/placement is more important than occlusion.
COMPLEX FRACTURES
Complex injuries, such as comminuted fractures, blast injuries, or multiple fractures, deserve special consideration. Visualization of the fracture site becomes increasingly important, and whereas intraoral approaches are beneficial for improving aesthetic outcomes, extraoral approaches provide greater visualization and allow for the placement of larger plates in cases of extended areas with fracture involvement. Recon plates also play a larger role in management, and can be used in conjunction with miniplates for mandibular stabilization. Miniplates can also be used to stabilize the smaller bone fragments both to each other and to the larger bone fragments, while the recon plate serves as the major structural buttress of the mandible. With multiple fractures, the occlusion should be ideally checked after every plate has been placed because of the possibility of plate application creating torsional forces on the fracture segments causing malocclusion. Additionally, bone grafting plays a more significant role in these situations and should be used for significant defects of the mandible. In general, free bone grafts will survive if stabilization and soft tissue coverage is adequate36; however, in cases of large, irradiated, or anterior defects, vascularized bone grafts are preferred.37
External fixation is used for fractures with severe comminution, infections, nonunions, or significant bone or soft tissue defects and is used when the dentition is not sufficiently intact for stable IMF/MMF (Fig. 16). This method of fixation eliminates the need for significant soft tissue disruption, which may devascularize the bone fragments, and does not require the placement of an internal device.
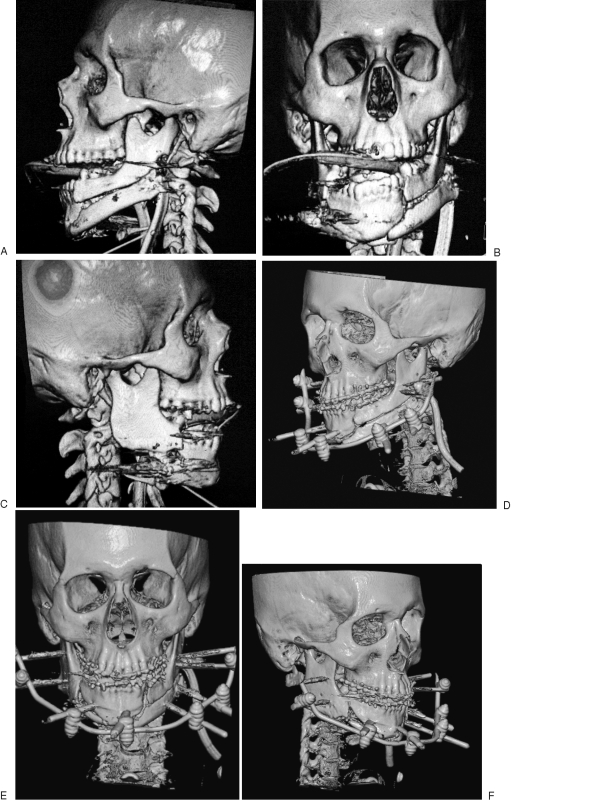
Figure 16.
(A–F) This is a complex and significantly comminuted mandibular fracture that was subsequently treated with external fixation to avoid significant soft tissue and vascularity disruption that would have occurred if internal fixation was attempted.
When external fixation is used for significant comminution, one should be prepared for a high risk of complications. One study found that greater than one third of mandibular fractures treated with external fixation had complications, which was double the rate for closed treatment and more than triple the rate versus ORIF.38 Additionally, the rate of malocclusion after the treatment of comminuted fractures with external fixation approaches 11.7%, almost triple the rate of complications seen with open reduction. This increased incidence of complications most likely is not a statement of the problematic nature of external fixation but reflects that although external fixation is appropriate for significant comminution, the significant comminution itself is associated with a significant risk of postoperative complications regardless of the fixation method used.38
Notably, when used for gunshot or shotgun blasts, external fixation can allow for remarkable healing and bridging of large bony defects. Therefore, external fixation can be used as a temporary damage control measure, to be followed by ORIF at a later date, if needed for stability or occlusion modification.
PEDIATRIC FRACTURES
Pediatric facial trauma accounts for less than 15% or less of all maxillofacial injuries; however, amongst this age group, the mandible was the most commonly fractured facial bone, occurring in 20 to 50% of all facial fractures.39,40,41 These patients are managed differently from adult patients for several reasons. First, the pediatric population tends to fracture less significantly, with most fractures being unicortical in nature (greenstick) and minimally displaced. This is thought to be secondary to increased elasticity of the thin cortical bone and the significant adipose tissue cushioning the bones. Additionally, options for immobilization may be limited in this population. The pediatric mandible can be a dynamic anatomic structure with missing and partially erupted teeth at times, as well as tooth surfaces that are not retentive for IMF/MMF wiring conversly, plate fixation of the mandible has the potential to disrupt tooth growth, as the mandible is filled with tooth buds during the dentitional transition period. Lastly, children have a thicker periosteal envelope with an increased capacity for bony remodeling. Subsequently, as a result of these factors, the majority of the fractures seen in the pediatric population are managed in a nonoperative or closed manner.
Other differences exist that make pediatric mandibular fractures a distinct breed of injury. Because these cases are largely caused by MVCs, a database survey of more than 600 U.S. trauma centers also revealed that these cases also differ in their overall morbidity and mortality compared with those of adult patients.40,42 About 32% of facial fractures in this age group were admitted to the intensive care unit, with a mean intensive care unit length of stay of 2.9 days and an associated 4% mortality rate. Additionally, the risk of having an associated facial soft tissue injury, brain injury, skull base fracture, or cervical fracture is also substantial.
One of the most common fractures seen in the pediatric population is the condylar fracture,6,39,43 which is significant because of its potential to disrupt growth of the mandible and its potential for ankylosis. Diagnosis can be difficult in the pediatric population because of age-related limitations in assessment, but certain presentations, such as bruising or a cut on the chin, should raise one's suspicion level. Although in the majority of these cases observation plays a prominent role in management, select cases will require fixation.
Closed methods of fixation can be difficult in pediatric patients in whom the permanent tooth roots have developed sufficiently,44 as the deciduous dentition is not able to support the hardware. Transitioning dentition is also troublesome for this end. Subsequently, circummandibular wiring, lingual splints, 4-point fixation with IMF screws, ORIF, and other forms of fixation are used as alternatives to achieve functional stability. Lingual splints achieve some degree of stability, without any internal hardware, but ultimately require multiple operations to be used appropriately. ORIF is not commonly performed until late mixed dentition, but may be indicated in the early or mixed dentition in severely dislocated and comminuted fractures, and in patients that are not able to handle IMF/MMF. Resorbable plates should be considered in young patients with deciduous teeth and mixed dentition, especially in the setting of displaced fractures. If titanium plates are used in the growing mandible (age < 18 years), they should be removed.
POSTOPERATIVE CARE
Postoperative management of mandibular fractures generally involves several key steps. At the outset, all patients who have undergone ORIF should be placed on a non-chew diet postoperatively. This will serve to reduce bite forces on the healing mandible and control fracture motion. Patients who are placed in IMF/MMF for long periods need to be counseled regarding the significant risk for nutritional issues. Patients need to be instructed to watch their weight and be given calorie supplementation as necessary. Patients also need to be instructed on oral hygiene, and the use of Peridex (3M, St. Paul, MN) oral rinse solution is invaluable for this end. Postoperative imaging should be performed to assess for callus formation and fracture healing, fracture segment alignment, and the status of the occlusion. This can be done with either a Panorex (can be performed in the clinic) or via CT scan (offers better visualization).
COMPLICATIONS
Complications after the management of mandibular fractures are not uncommon, with the most common forms being infectious and malunion/nonunion. Studies have demonstrated that factors such as patient age, sex, location, cause of fracture, associated facial injuries, time to repair, and length of hospitalization were unrelated to the development of complications.5 However, several other factors play significant roles. Smoking and substance abuse play a critical role in outcomes as studies have shown that complication rates increase significantly for these groups when using ORIF,5,45,46 with the majority of these (60–72%) being infectious in nature.45
Antibiotics play an important role in the management of the postoperative infections; however, the underlying cause in many of the cases is inadequate fixation, and if there is any concern, reoperation and either IMF/MMF, external fixation, or recon plates should be applied for rigid fixation. Infections that occur within 2 weeks (early infections) tend to be a soft tissue problem that can be treated with drainage, as long as the hardware in place is stable. If there is loose hardware present, however, it must be replaced. Infections occurring after 2 weeks (late infections) are more likely to be caused by inadequate fixation or dental pathology (Fig. 17 and Fig. 18). These require removal of hardware and larger fixation (bigger plates). The role of perioperative and postoperative antibiotics for preventing this complication is currently unclear, as there exist data to support both the benefits and the lack of benefits of their use5,17,47; however, given the degree of equipoise, the standard of care with antibiotics should be undertaken until more definitive evidence is available.
Figure 17.
Osteomyelitis associated with a mandibular angle fracture instability secondary to not receiving treatment.
Figure 18.
(A, B) Osteomyelitis of the mandibular body associated with fracture instability secondary to poor plate adaptation.
Another feared complication of mandibular fracture treatment is malunions/nonunions. Risk factors have been identified, as studies have shown that having complex fractures nearly doubles the risk of having a mandibular nonunion.48 Other factors affecting the risk of nonunion include poor fixation, osteomyelitis, and patient risk factors, among others. The most important complication to identify and treat, however, is malocclusion. This is generally managed by first evaluating the status of the fixation with either a Panorex or CT scan and subsequently re-plating or placing the patient in IMF/MMF.
CONCLUSION
Mandibular fractures are common craniofacial injuries. The proper approach depends on both fracture and patient characteristics. Whereas certain regions of the mandible have clear-cut options and solutions in case of injury, many injuries have intensely debated management plans, and even years of research have not been able to delineate a clear evidence-based answer, and in truth, there may not be a single right answer, but there is a personal answer: one that takes into consideration the skill set and ability of the surgeon along with the pros and cons associated with each management plan.
References
- Kelley P, Crawford M, Higuera S, Hollier L H. Two hundred ninety-four consecutive facial fractures in an urban trauma center: lessons learned. Plast Reconstr Surg. 2005;116:42e–49e. doi: 10.1097/01.prs.0000177687.83247.27. [DOI] [PubMed] [Google Scholar]
- Erdmann D, Follmar K E, Debruijn M, et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008;60:398–403. doi: 10.1097/SAP.0b013e318133a87b. [DOI] [PubMed] [Google Scholar]
- Sojot A J, Meisami T, Sandor G K, Clokie C M. The epidemiology of mandibular fractures treated at the Toronto general hospital: a review of 246 cases. J Can Dent Assoc. 2001;67:640–644. [PubMed] [Google Scholar]
- Ellis E, III, Moos K F, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59:120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- Furr A M, Schweinfurth J M, May W L. Factors associated with long-term complications after repair of mandibular fractures. Laryngoscope. 2006;116:427–430. doi: 10.1097/01.MLG.0000194844.87268.ED. [DOI] [PubMed] [Google Scholar]
- Haug R H, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:126–134. doi: 10.1067/moe.2000.107974. [DOI] [PubMed] [Google Scholar]
- Plaisier B R, Punjabi A P, Super D M, Haug R H. The relationship between facial fractures and death from neurologic injury. J Oral Maxillofac Surg. 2000;58:708–712. discussion 712–713. doi: 10.1053/joms.2000.7250. [DOI] [PubMed] [Google Scholar]
- Beirne J C, Butler P E, Brady F A. Cervical spine injuries in patients with facial fractures: a 1-year prospective study. Int J Oral Maxillofac Surg. 1995;24(1 Pt 1):26–29. doi: 10.1016/s0901-5027(05)80852-5. [DOI] [PubMed] [Google Scholar]
- Sinclair D, Schwartz M, Gruss J, McLellan B. A retrospective review of the relationship between facial fractures, head injuries, and cervical spine injuries. J Emerg Med. 1988;6:109–112. doi: 10.1016/0736-4679(88)90148-5. [DOI] [PubMed] [Google Scholar]
- Haug R H, Wible R T, Likavec M J, Conforti P J. Cervical spine fractures and maxillofacial trauma. J Oral Maxillofac Surg. 1991;49:725–729. doi: 10.1016/s0278-2391(10)80236-8. [DOI] [PubMed] [Google Scholar]
- Luce E A, Tubb T D, Moore A M. Review of 1,000 major facial fractures and associated injuries. Plast Reconstr Surg. 1979;63:26–30. doi: 10.1097/00006534-197901000-00005. [DOI] [PubMed] [Google Scholar]
- Baker A B, Mackenzie W. Facial and cervical injuries. Med J Aust. 1976;1:236–237. doi: 10.5694/j.1326-5377.1976.tb140555.x. [DOI] [PubMed] [Google Scholar]
- Haug R H, Prather J, Indresano A T. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932. doi: 10.1016/0278-2391(90)90004-l. [DOI] [PubMed] [Google Scholar]
- Piasecki J H, Gutowski K A, Lahvis G P, Moreno K I. An experimental model for improving fat graft viability and purity. Plast Reconstr Surg. 2007;119:1571–1583. doi: 10.1097/01.prs.0000256062.74324.1c. [DOI] [PubMed] [Google Scholar]
- Biller J A, Pletcher S D, Goldberg A N, Murr A H. Complications and the time to repair of mandible fractures. Laryngoscope. 2005;115:769–772. doi: 10.1097/01.MLG.0000157328.10583.A7. [DOI] [PubMed] [Google Scholar]
- Rehman J, Traktuev D, Li J, et al. Secretion of angiogenic and antiapoptotic factors by human adipose stromal cells. Circulation. 2004;109:1292–1298. doi: 10.1161/01.CIR.0000121425.42966.F1. [DOI] [PubMed] [Google Scholar]
- Andreasen J O, Storgård Jensen S, Kofod T, Schwartz O, Hillerup S. Open or closed repositioning of mandibular fractures: is there a difference in healing outcome? A systematic review. Dent Traumatol. 2008;24:17–21. doi: 10.1111/j.1600-9657.2006.00498.x. [DOI] [PubMed] [Google Scholar]
- Marciani R D, Haley J V, Kohn M W. Patient compliance—a factor in facial trauma repair. Oral Surg Oral Med Oral Pathol. 1990;70:428–430. doi: 10.1016/0030-4220(90)90203-5. [DOI] [PubMed] [Google Scholar]
- Cohen S R, Leonard D K, Markowitz B L, Manson P N. Acrylic splints for dental alignment in complex facial injuries. Ann Plast Surg. 1993;31:406–412. doi: 10.1097/00000637-199311000-00004. [DOI] [PubMed] [Google Scholar]
- Champy M, Loddé J P, Schmitt R, Jaeger J H, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978;6:14–21. doi: 10.1016/s0301-0503(78)80062-9. [DOI] [PubMed] [Google Scholar]
- Haug R H, Street C C, Goltz M. Does plate adaptation affect stability? A biomechanical comparison of locking and nonlocking plates. J Oral Maxillofac Surg. 2002;60:1319–1326. doi: 10.1053/joms.2002.35732. [DOI] [PubMed] [Google Scholar]
- Ellis E, III, Graham J. Use of a 2.0-mm locking plate/screw system for mandibular fracture surgery. J Oral Maxillofac Surg. 2002;60:642–645. discussion 645–646. doi: 10.1053/joms.2002.33110. [DOI] [PubMed] [Google Scholar]
- Collins C P, Pirinjian-Leonard G, Tolas A, Alcalde R. A prospective randomized clinical trial comparing 2.0-mm locking plates to 2.0-mm standard plates in treatment of mandible fractures. J Oral Maxillofac Surg. 2004;62:1392–1395. doi: 10.1016/j.joms.2004.04.020. [DOI] [PubMed] [Google Scholar]
- Eckelt U, Schneider M, Erasmus F, et al. Open versus closed treatment of fractures of the mandibular condylar process-a prospective randomized multi-centre study. J Craniomaxillofac Surg. 2006;34:306–314. doi: 10.1016/j.jcms.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Lee J W, Lee Y C, Kuo Y L. Reappraisal of the surgical strategy in treatment of mandibular condylar fractures. Plast Reconstr Surg. 2010;125:609–619. doi: 10.1097/PRS.0b013e3181c82ff0. [DOI] [PubMed] [Google Scholar]
- Ellis E, III, Simon P, Throckmorton G S. Occlusal results after open or closed treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2000;58:260–268. doi: 10.1016/s0278-2391(00)90047-8. [DOI] [PubMed] [Google Scholar]
- Palmieri C, Ellis E, III, Throckmorton G S. Mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. J Oral Maxillofac Surg. 1999;57:764–775. discussion 775–776. doi: 10.1016/s0278-2391(99)90810-8. [DOI] [PubMed] [Google Scholar]
- Ellis E, III, McFadden D, Simon P, Throckmorton G S. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000;58:950–958. doi: 10.1053/joms.2000.8734. [DOI] [PubMed] [Google Scholar]
- Ellis E, III, Throckmorton G S. Bite forces after open or closed treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2001;59:389–395. doi: 10.1053/joms.2001.21873. [DOI] [PubMed] [Google Scholar]
- Throckmorton G S, Ellis E., III Recovery of mandibular motion after closed and open treatment of unilateral mandibular condylar process fractures. Int J Oral Maxillofac Surg. 2000;29:421–427. [PubMed] [Google Scholar]
- Throckmorton G S, Ellis E, III, Hayasaki H. Masticatory motion after surgical or nonsurgical treatment for unilateral fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2004;62:127–138. doi: 10.1016/j.joms.2003.01.003. [DOI] [PubMed] [Google Scholar]
- Carinci F, Arduin L, Pagliaro F, Zollino I, Brunelli G, Cenzi R. Scoring mandibular fractures: a tool for staging diagnosis, planning treatment, and predicting prognosis. J Trauma. 2009;66:215–219. doi: 10.1097/TA.0b013e318194560b. [DOI] [PubMed] [Google Scholar]
- Beltrán-Aguilar E D, Barker L K, Canto M T, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis–United States, 1988–1994 and 1999–2002. MMWR Surveill Summ. 2005;54:1–43. [PubMed] [Google Scholar]
- Ellis E, III, Price C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. 2008;66:421–435. doi: 10.1016/j.joms.2007.08.042. [DOI] [PubMed] [Google Scholar]
- Luhr H G, Reidick T, Merten H A. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996;54:250–254. discussion 254–255. doi: 10.1016/s0278-2391(96)90733-8. [DOI] [PubMed] [Google Scholar]
- Hidalgo D A. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg. 1989;84:71–79. [PubMed] [Google Scholar]
- Foster R D, Anthony J P, Sharma A, Pogrel M A. Vascularized bone flaps versus nonvascularized bone grafts for mandibular reconstruction: an outcome analysis of primary bony union and endosseous implant success. Head Neck. 1999;21:66–71. doi: 10.1002/(sici)1097-0347(199901)21:1<66::aid-hed9>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Ellis E, III, Muniz O, Anand K. Treatment considerations for comminuted mandibular fractures. J Oral Maxillofac Surg. 2003;61:861–870. doi: 10.1016/s0278-2391(03)00249-0. [DOI] [PubMed] [Google Scholar]
- Ferreira P C, Amarante J M, Silva P N, et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005;115:1500–1508. doi: 10.1097/01.prs.0000160268.20294.fd. [DOI] [PubMed] [Google Scholar]
- Imahara S D, Hopper R A, Wang J, Rivara F P, Klein M B. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008;207:710–716. doi: 10.1016/j.jamcollsurg.2008.06.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaban L B. Diagnosis and treatment of fractures of the facial bones in children 1943-1993. J Oral Maxillofac Surg. 1993;51:722–729. doi: 10.1016/s0278-2391(10)80409-4. [DOI] [PubMed] [Google Scholar]
- Eskitascioglu T, Ozyazgan I, Coruh A, Gunay G K, Yuksel E. Retrospective analysis of two hundred thirty-five pediatric mandibular fracture cases. Ann Plast Surg. 2009;63:522–530. doi: 10.1097/SAP.0b013e318194fdab. [DOI] [PubMed] [Google Scholar]
- Thorén H, Iizuka T, Hallikainen D, Lindqvist C. Different patterns of mandibular fractures in children. An analysis of 220 fractures in 157 patients. J Craniomaxillofac Surg. 1992;20:292–296. doi: 10.1016/s1010-5182(05)80398-1. [DOI] [PubMed] [Google Scholar]
- Smartt J M, Jr, Low D W, Bartlett S P. The pediatric mandible: II. Management of traumatic injury or fracture. Plast Reconstr Surg. 2005;116:28e–41e. doi: 10.1097/01.prs.0000173445.10908.f8. [DOI] [PubMed] [Google Scholar]
- Serena-Gómez E, Passeri L A. Complications of mandible fractures related to substance abuse. J Oral Maxillofac Surg. 2008;66:2028–2034. doi: 10.1016/j.joms.2008.06.022. [DOI] [PubMed] [Google Scholar]
- Passeri L A, Ellis E, III, Sinn D P. Relationship of substance abuse to complications with mandibular fractures. J Oral Maxillofac Surg. 1993;51:22–25. doi: 10.1016/s0278-2391(10)80383-0. [DOI] [PubMed] [Google Scholar]
- Abubaker A O, Rollert M K. Postoperative antibiotic prophylaxis in mandibular fractures: a preliminary randomized, double-blind, and placebo-controlled clinical study. J Oral Maxillofac Surg. 2001;59:1415–1419. doi: 10.1053/joms.2001.28272. [DOI] [PubMed] [Google Scholar]
- Mathog R H, Toma V, Clayman L, Wolf S. Nonunion of the mandible: an analysis of contributing factors. J Oral Maxillofac Surg. 2000;58:746–752. discussion 752–753. doi: 10.1053/joms.2000.7258. [DOI] [PubMed] [Google Scholar]