Abstract
Nasal trauma plays a large and important role in the field of craniofacial trauma. The resulting aesthetic, structural, and functional sequelae associated with these injuries necessitate a thorough understanding of the topic. This includes an appreciation for the unique anatomic features of the region, the important aspects of the initial history and examination, nasal injury classification, and subsequent treatment timing and options. While a large body of literature has accumulated on the topic, the purpose of this article is to focus on both clinically relevant information and pearls of management. Additionally, age-specific concerns, secondary procedures, and nasal fracture grafting, will be addressed as well.
Keywords: Nasal trauma, nasal bone fractures, septal fracture, nasal airway, nasal airway obstruction, rhinoplasty, deviated nose, osteotomies, maxillofacial trauma, craniofacial trauma
Nasal fractures account for greater than 50% of all facial fractures in adults.1 The most common mechanism of injury is blunt trauma to the midface, usually the result of motor vehicle collisions, sports-related injury, or physical altercations. The natural projection and the fragility of distal structures in the nose contribute to its propensity for injury.2 The bones and cartilage of the nose provide both aesthetic and structural support for the midface and airway; therefore, proper evaluation and management is necessary to prevent nasal deformity and nasal airway compromise.
Problems with the classical approach are many. First, even to the skilled surgeon, most nasal fractures are not clearly delineated immediately secondary to edema. Second, though closed treatment for septal deformities and collapsed internal nasal structures (often seen in significant nasal injuries) is adequate to achieve temporary repositioning of structures, high recurrence rates and the need for reoperative rhinoplasty are common. Posttraumatic nasal deformities requiring reoperation have been reported to be as high as 50%.3,4,5,6 The current consensus is that secondary collapse is caused by failure of the severely comminuted nasal bones and the disrupted septum to provide adequate structural support against the contractile forces of scarring. The contemporary approach to nasal fractures now requires that these injuries be approached on an individual basis, as no one procedure or technique is satisfactory for all patients.
Injury to the bones and cartilage is less common in the pediatric population, especially in children under 5 years of age. This is largely due to the lack of exposure to facial trauma. However, fractures occur at an increasing frequency with age. The incidence of childhood nasal fractures is most common in boys between the ages of 16 and 20 years.7 Like adults, childhood fractures may commonly be caused by motor vehicle or sports-related trauma, but other causes such as falls and child abuse must also be considered.8,9,10,11
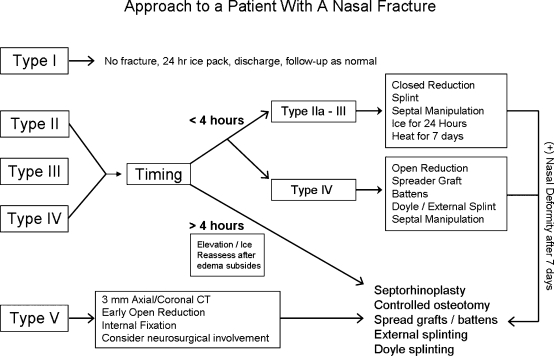
In all patients of any age, conservative selection is necessary to differentiate patients requiring acute treatment versus delayed treatment. Here we refine an algorithm (Fig. 1). Patients with significant septal and nasal shift present with nasal airway obstruction and require acute treatment with open reduction and visualization of the septum. In patients where a primary reduction is inappropriate or unavailable, a delayed reduction is adequate once swelling subsides. Treatment involves a traditional approach for complicated rhinoplasties, which involves correction of malposition, septal deflection, and airway obstruction. Spreader grafts may also be required for further correction. Ultimately, the goal of any reduction should be an aesthetic product and a functional repair of the nasal passages.
Figure 1.
The ideal management of nasal trauma differs based on the type of injury and timing of presentation.
ANATOMY
Detailed anatomic knowledge of the nose, including bony, cartilaginous, septal, and vascular supply, is necessary to understand the pathophysiology of injury, resultant deformity, and appropriate restoration. The bony components of the nose include the contributions from the maxilla, ethmoid, frontal, vomer, and nasal bones. Most commonly, fractures occur distally where the nasal bones become thinner and broader.12 Cases involving the proximal nasal bones, such as the frontal bone to the cribriform plate, are considered nasoorbitoethmoid (NOE) fractures, which represent more complicated injuries and pathology requiring additional attention.
Cartilaginous nasal structures include the paired upper and lower lateral cartilages, and the midline septum. The paired upper lateral cartilage functions to maintain the quadrangular cartilage in a midline position.13 The lower lateral portions contribute largely to the aesthetic contour of the nose. Cartilaginous fracture of these structures is generally an uncommon entity because it requires a much greater force to damage the distal deformable cartilage than to damage the nasal bone and septum.
The nasal septum is mostly derived from the quadrangular cartilage. The thicker posterior septal cartilage functions to support the upper two-thirds of the nose and the nasal dorsum much like a house with a central supporting wall. Proceeding caudally, however, the septum begins to thin.14 In children, the function of the septum is further magnified by its contribution to the face as a major growth center. Typically, growth of the nasal septum continues until ages 12 to 13 years, and septal trauma may disrupt midfacial development. In all age groups, this midline structure is supported laterally by the medial crura of the two lateral cartilages. Inferior support is provided by positioning within the vomerine groove, and superior and posterior support is provided by the perpendicular plate of the ethmoid bone.
Nasal blood supply derives from branches of both the internal and external carotid arteries; the majority stemming from the greater palatine, infraorbital, and sphenopalatine branches of the maxillary artery. The superior labial branch of the facial artery subsequently provides additional vasculature to the region. Blood supply to the inferior and middle turbinate is provided by branches off of the external carotid artery as well as the anterior and posterior ethmoidal branches off the internal carotid artery. Epistaxis after nasal injury is an indication of mucosal injury and commonly derives anteriorly from Kiesselbach's plexus in the anteroinferior septum. Posterior bleeding may result from both the sphenopalatine or anterior ethmoidal arteries. Anterior epistaxis is often effectively controlled through direct external pressure; posterior epistaxis will usually resolve spontaneously. Rarely, posterior bleeding may result in severe hemorrhage requiring further intervention (i.e., internal packing, balloon catheterization, interventional embolization).
Finally, the innervation of the nasal region is derived from both the ophthalmic and maxillary divisions of the trigeminal nerve. The infratrochlear nerve provides sensation to the skin of the upper nasal dorsum and sidewalls, and the anterior ethmoidal supplies the lower dorsum and tip.
INITIAL HISTORY AND EXAMINATION
The diagnosis of nasal trauma is based on clinical evaluation. A detailed patient history and examination is critical for proper patient selection and timing of repair. The mechanism of injury, time since injury, and patient age may all weigh heavily when differentiating patients needing acute reduction. Further, it is helpful to differentiate acute trauma–induced deformities from chronic or preexisting defects.
The precise mechanism of injury should be determined (i.e., motor vehicle, physical altercation with/without a weapon, fall, etc.). Different agents result in various types of trauma that mimics the direction and velocity of the force. Altercations resulting in assault-related nasal trauma typically generate low-energy lateral force transmission to the nose. These common injuries incur an in-fracture on the ipsilateral nasal bone, out-fracture on the contralateral side, and typically involve septal deformation. Frontal impact injuries are common in motor vehicle and projectile-induced trauma. These are typically high-energy insults resulting in greater nasal bone comminution and septal deformation. Crush injuries are also more common with frontal trauma.
The timing of injury is important as the optimal management differs if patients present within hours or weeks after injuries. In the initial hours after injury, prior to significant edema, it is possible to visualize new deformities fully. In these cases, a closed reduction is ideal. However, few patients present within this small window. After the onset of swelling, the physical details of the nose become obscured, and proper diagnosis becomes limited. In these instances, reduction should be delayed until the injury can be properly assessed (usually 3 to 5 days).15
Finally, history should address previous nasal trauma or procedures. It is important to compare the posttraumatic nose with a previous photograph (driver's license or wallet photo are useful in the acute setting). A further historical exploration of breathing difficulties, nasal congestion, snoring, sleep apnea, and nasal drainage will also allude to previous irregularities. Frequent use of over-the-counter allergy medications or inhalers may also be significant. Finally, the patient should be aware that any surgical treatment attempted will reflect only the best possible outcomes given previous deformities with the goal to minimize deformation and nasal airway obstruction.
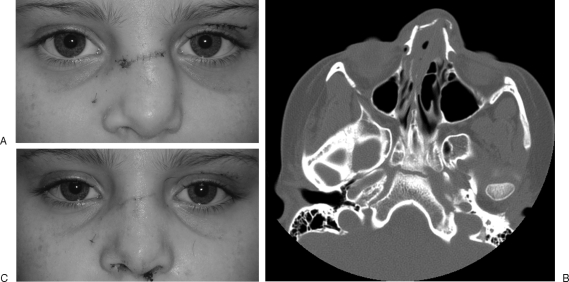
The physical examination should incorporate both internal and external components. External exam should focus on obvious nasal defects, malposition, and other apparent soft tissue injuries including lacerations, hemorrhage, or edema (Fig. 2). Palpation of the nose is critical. Physical findings of crepitus, tenderness, depression, step-offs, nasal shortening, or widening of the nasal base are indicative of fracture; however, any injury without some degree of bleeding is unlikely to be a severe fracture. Intercanthal measurements are useful in ruling out associated nasoorbital ethmoid fractures, especially in high-velocity frontal or inferior injuries.15 The finding of significant rhinorrhea should be evaluated for cerebrospinal fluid (CSF) leak by testing fluid levels of either glucose or β-transferrin.16 If a CSF leak is suspected, a neurosurgical consultation is advised. Patients should at the least be counseled on keeping the head elevated and avoiding supine positioning to allow healing. Leaks persisting longer than 2 weeks may necessitate lumbar drainage.
Figure 2.
Common findings associated with nasal bone fractures include loss of nasal dorsum projection, distortion of the dorsal aesthetic lines, and periorbital ecchymoses.
Internal examination of the nose requires minimal preparation and equipment. Patients are typically prepared with decongestant spray and/or topical vasoconstrictive medication. Frazier-tipped suction, a head lamp, a nasal speculum, and cotton-tipped applicators are necessary with or without rigid or flexed endoscope (3 mm, 30 degree) to facilitate complete internal visualization.15,17 Commonly used topical anesthetics include 4% lidocaine with oxymetazoline or phenylephrine hydrochloride. The method of examination is standard with the patient in the seated position, and if used, the endoscope is advanced beneath the inferior turbinate under direct vision. Attention should be made to the inferior meatus, turbinates, septum, and posteroinferior septal junction with the ethmoid plate. Inspect the septal mucosa for laceration or tearing. The presence of a septal hematoma should prompt immediate attention to prevent pressure necrosis of cartilage and further deformation.18,19 Hematomas may be treated by drainage followed by packing with local and systemic antibiotic coverage. Smaller hematomas may be aspirated with close follow-up. The examination of pediatric patients may present additional challenges. Though less likely to suffer nasal fractures, septal injuries are frequently missed in this population.20,21 Attention to trauma in children is critical in that septal necrosis may lead to problems with growth centers and predisposition to future deformities.22,23
Imaging is seldom necessary and has been found to be cost prohibitive as the diagnosis of nasal fracture is largely clinical.1,24 However, a computed tomography (CT) scan is indicated when NOE fracture is suspected to rule out intracranial injuries and other associated periorbital fractures. CT scans may also be helpful for characterization of septal deviation, especially of the posterior ethmoid.
Examination Pearls
Examination should start distally and move proximally, dividing the nasal examination into upper, middle, and lower thirds. Focus should be given to presence of ecchymosis, bruising, hemorrhage, and development of hematoma to determine if a structural injury is present. Crepitus or free air in soft tissue is indicative of more severe injury. Palpate for tenderness, irregularity, mobility, and fragmentation. Numbness indicates infraorbital nerve injury and suggests a more severe facial injury. Adjunctive studies, such as x-ray, are often unreliable and unnecessary. If imaging has been performed, attention to the septum and relative symmetry is warranted.
CLASSIFICATION OF NASAL FRACTURES
Categorization of nasal fractures is important for determining a treatment plan. Many groups have previously described classification systems for nasal fractures. Stranc and Robertson25 described a well-accepted classification stratagem based on the vector of force and clinical findings, whereas Murray et al19 described a classification of nasal fractures based on pathologic criteria. They also found that lateral nasal deviation of more than half the nasal width was a good predictor of septal involvement. The senior author (S.S.) has previously reported a modified Murray classification system that relies heavily on clinical findings as opposed to the pathologic patterning of injury (Table 1).16
Table 1.
Nasal Trauma Classification
| Type I | Injury restricted to soft tissue |
| Type IIa | Simple, unilateral nondisplaced fracture |
| Type IIb | Simple, bilateral nondisplaced fracture |
| Type III | Simple, displaced fracture |
| Type IV | Closed comminuted fracture |
| Type V | Open comminuted fracture or complicated fracture* |
Type II to IV fracture with CSF rhinorrhea, airway obstruction, septal hematoma, crush injury, numbness, severe displacement, or NOE midface involvement.
PREOPERATIVE MANAGEMENT OF NASAL FRACTURES
Management of a nasal trauma is dependent upon multiple factors including (1) age of the patient, (2) time since injury, (3) necessity for acute versus delayed reduction, (4) choice of anesthesia, and (5) approach (open vs. closed reduction). It should be noted, however, that the fracture should be carefully classified and diagnosed prior to any management attempt.
Age-Specific Concerns
Nasal surgery in the very young or very old may pose additional difficulties. The elderly may present with brittle, short nasal bones, and subsequently conservative reduction and osteotomy with use of spreader grafts is prudent. However, the patient should be preoperatively counseled to remain realistic about the final appearance. Rhinoplasty in children should be approached with special care, as age-specific variations in anatomy, interference with facial growth centers, and age-related effects on wound healing may apply.26 Children cannot simply be regarded as “small adults,” as a safe and effective surgery in adults is not necessarily wise in children.22 The best timing for septal surgery in children is after 13 to 14 years of age when growth in this region is complete. Surgery may be prudent in patients if the septum is completely malpositioned and will prevent normal growth without intervention. Simple nasal surgeries are often approached with careful reduction of fractured segments, with postoperative nasal packing. Younger children tend to be obligate nasal breathers and should be carefully observed.
Considerations for Anesthesia
Many studies have examined the use of local versus general anesthesia for the reduction of nasal fractures.5,27,28 Overriding concerns for patient safety and cooperativeness should be assessed preoperatively. Other considerations include differences in cost, variation in outcomes, and patient overall health. Pediatric patients pose additional challenges and should typically be reduced under general anesthesia, whereas most adults with type IIa through type IV fractures can be reduced with a combination of topical and infiltrative local anesthetic if properly selected.29 Infiltrative anesthesia may be used externally to the nasal dorsum and can be better tolerated over bilateral internal blocks.30
ADMINISTRATION OF TOPICAL AND INFILTRATIVE ANESTHESIA
Local anesthesia is typically divided into topical and infiltrative. In general, 4% lidocaine and either oxymetazoline (Afrin, Schering-Plough Healthcare Products, Inc., Berkeley Heights, NJ) or phenylephrine hydrochloride (Neo-Synephrine, Pittsburgh, PA) can be used and applied via pledgets.15,16 Administration of three pledgets per nostril for 8 to 10 minutes is usually sufficient. Specific focus areas should be along the dorsal septum near the anterior ethmoid nerve and artery, the middle turbinate proximal to the pterygopalatine ganglion, and the nasal floor adjacent to the nasopalatine nerve and sphenopalatine artery.16 Infiltrative anesthesia is administered with epinephrine both internally and externally. The volume of infiltrative anesthesia should be minimized to prevent obscuring nasal anatomy and interfering with the planned reduction. The septal submucosa should be infiltrated bilaterally, as well as the undersurface of nasal bones. If necessary, infiltrative blocks may also be applied at the level of the dorsal nasal and infraorbital nerves.
CLOSED REDUCTION
Closed reduction is usually reserved for simple, noncomminuted nasal fractures, although exceptions can be made (Fig. 3). The key principal is to apply a force opposite to the vector of trauma to achieve fracture reduction. After anesthesia, attention should be paid to the bony nasal pyramid. A Goldman elevator can be inserted to aid in manual repositioning of bones. Care should be used with this technique over the cribriform plate if injury is suspected. The Goldman elevator is applied with upward/outward force with bimanual manipulation of the external nasal bones.
Figure 3.
The patient is a young female who suffered a blow to the nasal dorsum. (A) The patient was noted to have both widening and flattening of the nasal dorsum. (B) CT scan findings demonstrated a severely comminuted and depressed nasal bone fracture. The patient underwent closed reduction and treatment of nasal bone fractures. (C) The patient's postoperative appearance, with return of nasal bone position and dorsal projection and width.
Attention to the nasal septum is particularly important as nasal bone deformities will typically recur if a septal injury is missed. Straightening of the septum is accomplished by blunt pressure from the Goldman elevator opposite to the direction of deviation with concurrent elevation of the nasal pyramid.1,6,17 A Boies elevator may alternatively be used for blunt septal repositioning.15 Ultimately, the septal base should be repositioned into the vomerian groove if possible.
Closed reduction can be an effective tool in the appropriately selected patient. However, the closed approach may necessitate further postoperative attention in certain areas. Partial nasal fractures may require osteotomy for mobilization and appropriate reduction.1,14,17 Again, preoperative discussion with the patient should be realistic. It is unlikely that the patient will have a “perfect” result, and the primary goal is to minimize deformity and functional impairment. Further, patients should be prepared for the possibility that a future open septorhinoplasty may be necessary as reoperation rates range between 9 and 17% for closed reductions.15,27
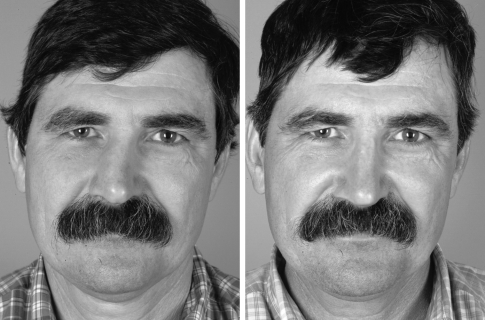
OPEN REDUCTION
A key point of rhinosurgery is that certain nasal injuries cannot be sufficiently managed with a closed reduction. Comminuted fractures with severe loss of nasal support, severe septal injuries, and injuries with considerable soft tissue damage should be addressed with full exposure as the advantages of open reduction are many (Fig. 4). The greater exposure allows for direct visualization and precise reapproximation of dislocated structures, especially in cases of nasal tip distortion. Also, the traditional transfixion or hemitransfixion incision in the membranous septum allows for drastically improved caudal, inferior, and posterior septal visualization.31,32 Surgery should occur early enough that secondary healing and remodeling has not drastically distorted the preinjury form. However, it is critical that edema be allowed to subside prior to any procedure, usually after 5 to 7 days if proper postinjury care is used.
Figure 4.
Preoperative and 6-month postoperative photos of a 47-year-old man with a history of multiple nasal fractures. The patient underwent open reduction and internal fixation of nasal bone fractures and septoplasty. Postoperatively, the dorsal aesthetic lines have significantly improved from their preoperative position and contour.
CONSIDERATIONS FOR SEPTAL REPAIR
There are multiple approaches for elevation of the mucoperichondrium and periosteum at the junction of the anterior maxillary septum. In our experience, we recommend a single superior mucopericoperiosteal tunnel brought inferiorly from posterior to anterior. This approach minimizes the risk of perforation and provides excellent exposure of the vomerian crest and the floor of the cartilaginous septum. Careful dissection of the extramucosal tissue at the dorsal septum allows for separation of the internal and external nose while maintaining support. In the event that a perforation is made, mobilization and closure should be attempted. Additionally, without permanent and appropriate fixation, the septum will tend to deform. Thus, it is important to ensure septal alignment with other key structures such as the quadrangular cartilage and vomerian groove.
Quadrangular Cartilage
Manipulation of the quadrangular cartilage is essential to reconstructing the nasal midline and permanent repositioning of the septum. A dorsal and caudal strut of cartilage of least 10 to 15 mm in width should always be maintained. Removal of the inferior horizontal segment of septum assists in midline septal alignment. If necessary, it is acceptable to remove portions of the perpendicular plate of the ethmoid bone to maintain attachment to the underlying mucoperichondrium.16
Bony Septum
Bony septal deformities contribute to airway obstruction and mechanical midline malposition; however, because little nasal support is derived from this structure, malposition of the bony septum is an indication for greenstick fracture or resection to prevent airway obstruction. A 2-mm osteotome can be used to reposition the bony septum into the midline, but careful attention should be made to spurs or malformed bone as these may play a role in obstruction. If malposition of the premaxillary crest or nasal spine is apparent, resection of a 3- to 4-mm inferior strip of septal cartilage may allow midline repositioning. Fixation of the caudal septum to the premaxillary periosteum can be accomplished with a 4-0 nylon suture.
Caudal Septum
Weakening or destruction of the caudal septum may result in loss of nasal tip maintenance, and subsequent repair of this structure represents a difficult surgical challenge. Structural support can be reestablished with autogenous cartilage fixed in place with a 4-0 clear nylon or PDS (Ethicon Inc., Somerville, NJ) suture.
Dorsal Septum
The cartilaginous dorsum should be approached once all other septal abnormalities have been addressed. If the septum remains crooked despite caudal, inferior, and posterior cartilage reconstruction, incision of the dorsal cartilage may be attempted. Vertical incisions in the intact dorsal cartilage should be made up to 2 to 3 mm of total transection. If continuity is interrupted, care must be taken to ensure that mobilized septal components do not displace posteriorly. Reconstituting support is critical with a spreader type graft to keep distortion to a minimum. A successful dorsal septum dissection should be preceded by (1) trans-septal mattress sutures under the dorsum buttress of cartilage or bone to prevent posterior displacement, (2) stabilization of the caudal cartilage strut and septum by internal splinting, and (3) skeletal repositioning by lateral osteotomies. Finally, if a hump resection is not used, the upper lateral cartilages must be released from the septum through submucosal tunnels for exposure and access.
HUMP REMOVAL
After septal repair and fixation, hump removal should be attempted and can be simplified by use of previously created submucosal tunnels. Any cartilaginous asymmetry should be assessed visually as well as digitally with a wet gloved finger. Any resection should be approached conservatively. A chisel or rasp can be used to remove cartilage carefully in an incremental fashion. Extra care should be taken in a deviated nose due to the frequent occurrence of skeletal asymmetry. Cases involving wide nasal bridges are at risk to develop open-roof deformity. Such can be prevented with the use of osteotomies or onlay cartilage grafts.
OSTEOTOMIES
Nasal osteotomies can be performed to modify the nasal dorsum and bony vault, but should be used in addition to successful septal realignment and repair of nasal support. Without proper repositioning of the dorsal septum, the dorsum will remain displaced laterally with upper lateral cartilage deviation.33 Repair and mobilization by osteotomy alone will often result in only temporary correction of deviation and eventual recurrence.16 Nasal bones may present with unexpected intraoperative challenges due to asymmetry and irregularity of natural bone shape. Additionally, bowing may be present in both the nasal bones and the nasal process of the maxilla. In the severely deviated nose, paramedian or double osteotomies may aid in creating comminution and appropriate repositioning. If the nasal bone is severely comminuted, consider using large cephalad cartilage grafts to maintain the bone from collapsing.
SECONDARY PROCEDURES
Occasionally, additional support or aesthetic symmetry refinement is needed when completing the open reduction. Dorsum and midvault defects can be filled with diced cartilage or bone. Additional support can be provided to the middle and lower nose with larger septal spreader grafts applied to the keystone area. If inferior turbinate hypertrophy is compounding nasal airway obstruction, bony resection or greensticking with microfracture may be undertaken on the nasal turbinates. If the true midline becomes obscured, the incisors can serve as a reference point during nasal bone mobilization. Finally, alar base narrowing may be indicated in cases of nostril asymmetry.
FINAL CONSIDERATIONS IN OPEN NASAL FRACTURE REDUCTION
A successful open reduction should be planned extensively and approached in a stepwise manner. In severely comminuted open fractures, it may be necessary to fix the nasal bones internally with plating or wires. The frontal bone and maxilla may be used in these cases as anchor points. Nasal plating should be used judicially as patients may suffer skin erosion, especially if they wear glasses. Typically, 26- to 30-gauge wiring can be used without risk of palpability. An acceptable result may be made by using thick, absorbable suture in “figure-of-eight” patterns to lock nasal bones in place.1 Of added note, care should be taken to maintain bony vascularization; therefore, rasping should be used sparingly near fracture fragments.
CONSIDERATIONS AFTER SUCCESSFUL REDUCTION
General Considerations
After successful repair of nasal fractures, it is important to reevaluate the patient prior to splinting or packing. A primary concern is adequate patency of the airway. The nasal airway can easily be assessed by passing a Goldman bar or other blunt instrument along the floor to the nasopharynx. Any narrowing or obstruction should be fixed at this time. The external contour and aesthetics of the nose should be evaluated both visually and physically. Physical examination of the nose can be accomplished manually with a moistened, gloved finger to detect subtle irregularities. Should dorsal hump problems persist after manipulation, a rasp may be used through an intercartilaginous incision. Conversely, if contour deformities exist, onlay cartilage grafting or AlloDerm (Lifecell Corp., Branchburg, NJ) placement should be considered.
Splinting and Packing
All reduced fractures, whether open or closed, should be splinted postoperatively. This may include internal as well as external splinting. Intranasal Doyle splints are recommended because they provide internal septal stabilization, aid in airway maintenance, and prevent synechiae after substantial manipulation. They are typically tolerated by most patients.34 Intranasal splinting should generally be maintained for 2 to 3 weeks postoperatively.15 Extranasal splinting provides support and limited protection to the reduced bones and cartilage and may aid in skin adherence to underlying structures of the nose, especially after an open procedure.
Packing is now used less frequently than in the past. Since its inception, surgeons have documented that packing may pose a risk to patients, and its use has become polarized. Packing has been justified by the belief that it decreases postoperative complications, such as bleeding, adhesion formation, and septal hematomas. However, research has suggested that not only can packing fail to prevent complications, but also it may actually precipitate them.35 Packing has been shown to be directly associated with postoperative pain, discomfort, soft palate laceration, septal perforation, nasopulmonary reflex (a life-threatening vagal response that can lead to hypoxia and bradycardia), and even toxic shock.36,37 We recommend packing in cases of extreme comminution of nasal bones, such that packing is necessary to maintain their position. Packing should be placed directly under areas of severely comminuted bone and maintained no longer than 72 hours.
SURGICAL PEARLS FOR NASAL FRACTURE GRAFTING
Patients should be counseled preoperatively that restoration of the pretraumatic nasal appearance may not be a realistic outcome. Follow-up should extend to 6 to 12 weeks postoperatively, at which time structural integrity of the nose should be assessed. If midvault nasal collapse has occurred, the surgeon should realize that support has been lost and a future septorhinoplasty may be necessary. In these cases, a large, cartilaginous spreader graft may be sensible. Large grafts in the form of cadaveric or autologous rib, placed medial to the nasal bones and just lateral to the septum, can be used to maintain comminuted nasal fracture reduction. Similarly, if tip support has been lost, the rib graft can function as a stronger columellar strut graft to improve and maintain projection. Thinner cartilaginous grafts may be used to fix a deviated septum after appropriate release and fixed with multiple sutures. The body of the septum may be harvested in adults without dire consequences to be used as grafting material, whereas ear cartilage is often not appropriate in this region due to its natural curve. Batten grafts, centered at the point of maximal weakness and concavity of the alar sidewall, can be used to straighten the septum as opposed to simple reduction and dissection. Bilateral batten grafts are becoming more common in contemporary repair and may be valuable for maintaining nasal straightness.
FINAL THOUGHTS
Nasal fractures can be treated with good outcomes in the majority of patients. Obvious outliers to simple procedures include the elderly, adolescents, and children. Further, the classification and timing of any nasal injury will greatly influence the approach and outcome of the intervention.
Many surgeons miss valuable opportunities in nasal repair, and posttraumatic nasal reduction may be handled inappropriately. Proper treatment of any nasal injury begins with excellent preoperative screening and appropriate diagnosis. Surgeons expect long-term aesthetic and functional results but may fail to support damaged septal and cartilaginous structures adequately. Considering the frequency and difficulty of these reconstructions, surgeons must begin considering these injuries as seriously as other severe entities in facial trauma.
References
- Renner G J. Management of nasal fractures. Otolaryngol Clin North Am. 1991;24:195–213. [PubMed] [Google Scholar]
- Dingman R O, Natvig P. The nose. In: Natvig P, editor. Surgery of Facial Fractures. Philadelphia, PA: Saunders; 1969. p. 267. [Google Scholar]
- Murray J A, Maran A G. The treatment of nasal injuries by manipulation. J Laryngol Otol. 1980;94:1405–1410. doi: 10.1017/s0022215100090241. [DOI] [PubMed] [Google Scholar]
- Crowther J A, O'Donoghue G M. The broken nose: does familiarity breed neglect? Ann R Coll Surg Engl. 1987;69:259–260. [PMC free article] [PubMed] [Google Scholar]
- Waldron J, Mitchell D B, Ford G. Reduction of fractured nasal bones; local versus general anaesthesia. Clin Otolaryngol Allied Sci. 1989;14:357–359. doi: 10.1111/j.1365-2273.1989.tb00384.x. [DOI] [PubMed] [Google Scholar]
- Bailey B J, Tan L KS. Nasal and frontal sinus fractures. In: Bailey B J, editor. Head and Neck Surgery–Otolaryngology. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1998. pp. 1007–1031. [Google Scholar]
- Azevedo A B, Trent R B, Ellis A. Population-based analysis of 10,766 hospitalizations for mandibular fractures in California, 1991 to 1993. J Trauma. 1998;45:1084–1087. doi: 10.1097/00005373-199812000-00020. [DOI] [PubMed] [Google Scholar]
- Anderson P J. Fractures of the facial skeleton in children. Injury. 1995;26:47–50. doi: 10.1016/0020-1383(95)90552-9. [DOI] [PubMed] [Google Scholar]
- Türegün M C, Zins J E. Maxillofacial fractures in weightlifters: a report of two cases. J Oral Maxillofac Surg. 1999;57:626–628. doi: 10.1016/s0278-2391(99)90090-3. [DOI] [PubMed] [Google Scholar]
- Perkins S W, Dayan S H, Sklarew E C, Hamilton M, Bussell G S. The incidence of sports-related facial trauma in children. Ear Nose Throat J. 2000;79:632–634, 636, 638. [PubMed] [Google Scholar]
- Canty P A, Berkowitz R G. Hematoma and abscess of the nasal septum in children. Arch Otolaryngol Head Neck Surg. 1996;122:1373–1376. doi: 10.1001/archotol.1996.01890240079017. [DOI] [PubMed] [Google Scholar]
- Fry H. Nasal skeletal trauma and the interlocked stresses of the nasal septal cartilage. Br J Plast Surg. 1967;20:146–158. doi: 10.1016/s0007-1226(67)80031-6. [DOI] [PubMed] [Google Scholar]
- Vora N M, Fedok F G. Management of the central nasal support complex in naso-orbital ethmoid fractures. Facial Plast Surg. 2000;16:181–191. doi: 10.1055/s-2000-12578. [DOI] [PubMed] [Google Scholar]
- Verwoerd C D. Present day treatment of nasal fractures: closed versus open reduction. Facial Plast Surg. 1992;8:220–223. doi: 10.1055/s-2008-1064653. [DOI] [PubMed] [Google Scholar]
- Rohrich R J, Adams W P., Jr Nasal fracture management: minimizing secondary nasal deformities. Plast Reconstr Surg. 2000;106:266–273. doi: 10.1097/00006534-200008000-00003. [DOI] [PubMed] [Google Scholar]
- Higuera S, Lee E I, Cole P, Hollier L H, Jr, Stal S. Nasal trauma and the deviated nose. Plast Reconstr Surg. 2007;120(7, Suppl 2):64S–75S. doi: 10.1097/01.prs.0000260722.91183.50. [DOI] [PubMed] [Google Scholar]
- Cox A J., III Nasal fractures—the details. Facial Plast Surg. 2000;16:87–94. [PubMed] [Google Scholar]
- Murray J A. Management of septal deviation with nasal fractures. Facial Plast Surg. 1989;6:88–94. doi: 10.1055/s-2008-1064714. [DOI] [PubMed] [Google Scholar]
- Murray J A, Maran A G, Busuttil A, Vaughan G. A pathological classification of nasal fractures. Injury. 1986;17:338–344. doi: 10.1016/0020-1383(86)90159-2. [DOI] [PubMed] [Google Scholar]
- Olsen K D, Carpenter R J, III, Kern E B. Nasal septal injury in children. Diagnosis and management. Arch Otolaryngol. 1980;106:317–320. doi: 10.1001/archotol.1980.00790300005002. [DOI] [PubMed] [Google Scholar]
- Hinderer K H. Nasal problems in children. Pediatr Ann. 1976;5:499–509. [PubMed] [Google Scholar]
- Hatef D A, Cole P D, Hollier L H., Jr Contemporary management of pediatric facial trauma. Curr Opin Otolaryngol Head Neck Surg. 2009;17:308–314. doi: 10.1097/MOO.0b013e32832d95a0. [DOI] [PubMed] [Google Scholar]
- Stal S. Septal deviation and correction of the crooked nose. In: Daniel R K, editor. Aesthetic Plastic Surgery Rhinoplasty. Boston, MA: Little, Brown; 1993. pp. 723–737. [Google Scholar]
- Logan M, O'Driscoll K, Masterson J. The utility of nasal bone radiographs in nasal trauma. Clin Radiol. 1994;49:192–194. doi: 10.1016/s0009-9260(05)81775-1. [DOI] [PubMed] [Google Scholar]
- Stranc M F, Robertson G A. A classification of injuries of the nasal skeleton. Ann Plast Surg. 1979;2:468–474. doi: 10.1097/00000637-197906000-00004. [DOI] [PubMed] [Google Scholar]
- Verwoerd C D, Verwoerd-Verhoef H L. Rhinosurgery in children: basic concepts. Facial Plast Surg. 2007;23:219–230. doi: 10.1055/s-2007-995814. [DOI] [PubMed] [Google Scholar]
- Cook J A, McRae R D, Irving R M, Dowie L N. A randomized comparison of manipulation of the fractured nose under local and general anaesthesia. Clin Otolaryngol Allied Sci. 1990;15:343–346. doi: 10.1111/j.1365-2273.1990.tb00480.x. [DOI] [PubMed] [Google Scholar]
- Watson D J, Parker A J, Slack R W, Griffiths M V. Local versus general anaesthetic in the management of the fractured nose. Clin Otolaryngol Allied Sci. 1988;13:491–494. doi: 10.1111/j.1365-2273.1988.tb00323.x. [DOI] [PubMed] [Google Scholar]
- Wang T D, Facer G W, Kern E B. Nasal fractures. In: Gates G A, editor. Current Therapy in Otolaryngology: Head and Neck Surgery. Philadelphia, PA: B. C. Decker; 1990. pp. 105–109. [Google Scholar]
- Cook J A, Murrant N J, Evans K, Lavelle R J. Manipulation of the fractured nose under local anaesthesia. Clin Otolaryngol Allied Sci. 1992;17:337–340. doi: 10.1111/j.1365-2273.1992.tb01008.x. [DOI] [PubMed] [Google Scholar]
- Anderson J R. A personal technique of rhinoplasty. Otolaryngol Clin North Am. 1975;8:559–562. [PubMed] [Google Scholar]
- Converse J M. Corrective surgery of nasal deviations. AMA Arch Otolaryngol. 1950;52:671–708. doi: 10.1001/archotol.1950.00700030697001. [DOI] [PubMed] [Google Scholar]
- Goodman W S. External approach to rhinoplasty. Can J Otolaryngol. 1973;2:207–210. [PubMed] [Google Scholar]
- Doyle D E, House L F, Hall W P. Description of a new device: an intranasal airway/splint. Laryngoscope. 1977;87(4 Pt 1):608–612. doi: 10.1288/00005537-197704000-00013. [DOI] [PubMed] [Google Scholar]
- Repanos C, McDonald S E, Sadr A H. A survey of postoperative nasal packing among UK ENT surgeons. Eur Arch Otorhinolaryngol. 2009;266:1575–1577. doi: 10.1007/s00405-009-0978-8. [DOI] [PubMed] [Google Scholar]
- Fairbanks D N. Complications of nasal packing. Otolaryngol Head Neck Surg. 1986;94:412–415. doi: 10.1177/019459988609400337. [DOI] [PubMed] [Google Scholar]
- Stucker F J, Ansel D G. A case against nasal packing. Laryngoscope. 1978;88(8 Pt 1):1314–1317. doi: 10.1288/00005537-197808000-00013. [DOI] [PubMed] [Google Scholar]