Abstract
Zygomaticomaxillary complex (ZMC) fractures are a group of fractures that can significantly alter the structure, function, and appearance of the midface, including the globe. Like other facial fractures, the optimal management of operative ZMC fractures requires anatomic reduction of all fractures followed by rigid internal fixation. However, surgical treatment of these fractures can be quite challenging with the potential for high rates of complications. The goal of this article is to provide an overview of ZMC fractures and discuss treatment options, with an emphasis on providing surgical pearls to optimize outcomes.
Keywords: Zygomaticomaxillary complex, zygomatic arch, zygoma, facial trauma, enophthalmos, tetrapod, facial fractures
The zygomatic arch and complex play a significant role in the structure and function of the face. Although studies differ regarding the incidence of these fractures, our experience in the adult population has demonstrated that ∼17% of facial trauma cases involve fractures of the zygoma,1 and fracture of the zygoma continues to be one of the three most common types of facial fractures.2 The two primary causes of these injuries in the United States have been identified as assault and motor vehicle accident.1,3 Although facial fractures are less common in the pediatric population, a similar incidence of these fractures (i.e., 22%) occurs among all cases of facial fractures.4 In this population, however, they are more commonly due to falls, motor vehicle accidents, and sports-related blunt trauma. Although the widespread use of seat belts and airbags has decreased the prevalence of injuries resulting from motor vehicle accidents,5 orbitozygomatic malar fractures still comprise a substantial portion of the facial trauma seen by plastic surgeons.
ANATOMY
The zygomaticomaxillary complex (ZMC) functions as a buttress for the face and is the cornerstone to a person's aesthetic appearance, by both setting midfacial width and providing prominence to the cheek. It can best be anatomically described as a “tetrapod” as it maintains four points of articulation with the frontal bone, temporal bone, maxilla, and greater wing of the sphenoid, at the zygomaticofrontal (ZF) suture, zygomaticotemporal (ZT) suture, zygomaticomaxillary buttress (ZMB), and zygomaticosphenoid (ZS) suture, respectively (Fig. 1). This tetrapod configuration then lends itself to complex fractures, as fractures here rarely occur in isolation. Additionally, the zygoma serves as the attachment point for muscles of both mastication and facial animation, but among these, it is the masseter that provides the most significant intrinsic deforming force on the zygomatic body and arch, albeit a small one. As apparent in Fig. 1, the zygoma plays an integral role with the orbit, as it buttresses the orbit and forms the majority of the lateral orbital wall and floor. In fact, the term orbitozygomatic fracture is perhaps more accurate, as isolated fractures of the zygoma without orbital involvement present rarely.
Figure 1.

Anatomy. The normal anatomic boundaries of the ZMC are outlined. On the opposite side is a ZMC fracture involving the ZF suture, ZMB, and ZS suture.
DIAGNOSIS
Physical Exam
Perhaps the most important aspect of the physical exam is to obtain a thorough, prompt ophthalmologic exam, as ZMC fractures are frequently complicated by blindness or a serious eye injury. ZMC fractures have a high incidence of ocular injury (10%) and a higher incidence of visual sequelae (41%) than most other forms of midfacial injury (15%).6,7 Moreover, individuals who suffer a zygoma fracture or other adjacent fracture after facial trauma are seven times more likely to sustain an eye injury compared with individuals with facial trauma without a bony fracture.6 Although a full eye exam is beyond the scope of a plastic surgeon's role in patient management, there are several basic tests that should be performed by all surgeons evaluating these patients.
First, gross vision should be assessed. Whereas a visual acuity exam is a very sensitive test for ocular injury, it is not very specific in the acute setting. Patients may or may not be wearing their glasses or contact lenses, vision may be obscured by ointment or tears in the eye, or soft tissue swelling may significantly alter the exam findings.
After evaluating for defects of gross vision, tests can be performed to assess for the presence of traumatic optic neuropathy, which can be as high as 6% in patients with ZMC fractures.8 An afferent pupillary defect (i.e., Marcus Gunn pupil), which is a pupil that exhibits no direct light constriction but constricts in a consensual response, is worrisome for traumatic optic neuropathy. Red color desaturation is also an important test as red color perception is first to be lost in optic nerve compromise. This can be easily examined by holding a penlight against the back of the finger, and having the patient identify its color. Any difference in the appearance of color in both eyes is worrisome for optic nerve injury.
Extraocular movement should also be tested, as should visual fields. Restriction in the movement of the extraocular muscles, especially on upward gaze, should raise the physician's concern for muscle entrapment. When in doubt, either a forced duction test can be performed with local anesthetic or computed tomography (CT) scans can be performed to examine for extraocular muscle entrapment. The exception to this, though, is the patient who presents with facial trauma, suspected orbital floor fracture, who also has nausea, vomiting, and bradycardia (oculocardiac reflex), which is pathognomonic for extraocular muscle entrapment.
During a standard visual field exam, a gross discrepancy between the surgeon and patient's range of vision indicates a problem with visual fields and potential ocular nerve compromise. The management of optic neuropathy is beyond the scope of this article; however, many surgeons initiate a steroid protocol to minimize swelling and further damage to the optic nerve. In addition, surgery is delayed until vision has stabilized or improved.9,10,11
Lastly, sensation in the V2 distribution should be tested and noted as sensation in this area is almost always diminished in malar fractures. Therefore, it is important to make note of this finding to avoid postoperative concerns of iatrogenic nerve dysfunction. Sensation often resolves postoperatively without specific treatment. Other physical exam findings are obscured by swelling encountered in the majority of these patients and are not helpful in the acute setting.
IMAGING
Over the years, CT scanning has supplanted plain radiography as the imaging modality of choice. Almost all malar fractures require direct CT scanning in both the axial and coronal planes (< 3-mm slice thickness) to categorize the pattern of injury clearly and direct subsequent management. If direct coronal images cannot be obtained, as in the case when neck extension is precluded by possible cervical spine injury, then thin-section axial helical scans can be reformatted to obtain coronal sections.12,13 Although these reformatted images are lower in resolution and less clear than directly obtained coronal images, they still provide significant information regarding the extent of the injury, especially to the orbital floor. In the most complex injuries and those involving multiple planes, three-dimensional CT imaging can be used to help the surgeon better visualize fracture fragments.
TREATMENT ALGORITHM
The decision to intervene surgically in these patients should be based primarily on whether there is displacement of the malar complex. As a general rule, nondisplaced fractures can usually be treated expectantly by first allowing for the edema to subside. These patients can be discharged home on a soft non-chew diet for 6 weeks with protection of the malar eminence. Antibiotics are not indicated, and follow-up should be in 2 weeks to assess for displacement and enophthalmos, which, if present, are indications for delayed intervention.
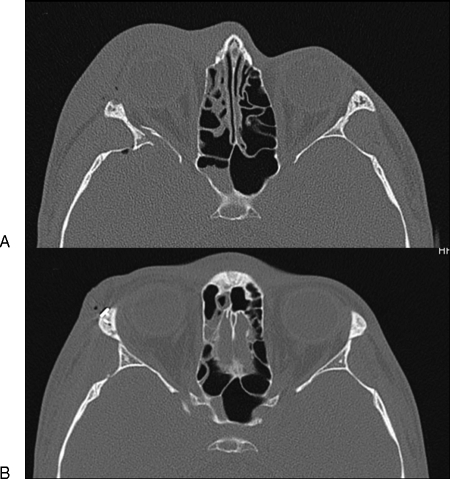
In contrast, displaced fractures should be surgically reduced and stabilized. The degree of displacement can be easily checked by assessing the status of the normal articulations of the ZMC with the craniofacial skeleton on CT scan. In particular, the lateral orbital wall (i.e., the articulation of the zygoma with the greater wing of the sphenoid) should be examined, as there must be a fracture through the lateral orbital wall to be classified as a true orbitozygomatic complex fracture (Fig. 2). This ZS articulation also gives an excellent indication of the direction and degree of displacement of the fracture complex.
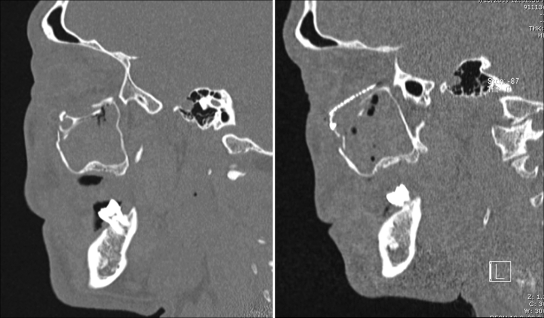
Figure 2.
ZS articulation. Fractures through the ZS suture should be noted (A) as accurate reduction here is of utmost importance to prevent inadequate reduction (B). Often, the infraorbital rim and ZMB can appear relatively well aligned despite inadequate reduction at the ZS suture.
Surgical indications for concomitant orbital fractures include significant fractures of the inferior orbital rim, orbital floor defects greater than 2 cm2, and significant posterior displacement (> 1 cm2) of the ZMC body.14 Posterior displacement of the ZMC can cause the orbital floor to buckle as it is also displaced posteriorly. Subsequently, as the ZMC is anatomically reduced, it can unearth a significant orbital floor defect that requires reconstruction. Recently, Tahernia et al reported that 1 cm of posterior displacement would subsequently correlate with ∼3 mm of enophthalmos.14
Finally, one should carefully evaluate the integrity of the zygomatic arch. Although an isolated zygomatic arch fracture does not need to be repaired, significant displacement here can decrease midface projection by up to 8 mm and, at the same time, increase facial width.14 Occasionally, isolated zygomatic arch fractures can be reduced with an elevator under the arch via a simple intraoral or temporal incision. The closed approach, however, is only successful if comminution does not exist and if there is an intact periosteum to maintain the reduction.
More recently, endoscopic technique has been used successfully at various centers in the management of zygomatic arch fractures.15,16,17 This minimally invasive approach negates the need for coronal incisions and appears to be a promising tool that augments, rather than replaces, the time-tested principles of adequate skeletal exposure, accurate fracture reduction, and appropriate internal fixation.16 However, endoscopic technique requires a steep learning curve and special equipment. Moreover, the long-term data on outcomes is lacking.
TREATMENT
Exposure and Reduction
Accurate reduction and fixation of displaced zygomatic fractures are necessary to ensure proper healing and prevent postoperative complications, such as enophthalmos and malar asymmetry. The number of surgical approaches and sites of fixation necessary to ensure this will vary based on the type of injury and the experience of the operating surgeon. Not every articulation needs to be addressed to achieve an acceptable reduction. However, at least three of four articulations must be addressed intraoperatively to reduce these fractures accurately.
The first step is accurate reduction of the fracture body. In the majority of cases, an incision in the gingivobuccal sulcus can be the first and only incision necessary as it allows for exposure of the ZMB, which is also the most commonly affected buttress of the ZMC.18 A blunt elevator is inserted laterally beneath the zygomatic arch and an attempt at reduction is made here. In rare cases, this will achieve anatomic reduction, and a single 2-mm L-plate along the ZMB laterally is sufficient.19 In addition, fractures of the zygomatic arch when present can easily be reduced with an elevator through the gingivobuccal sulcus incision. The fracture fragment is disimpacted to a more anatomic position, and subsequent fixation can be applied if needed.
When indicated, the inferior orbital rim can be approached with either a transcutaneous or transconjuctival lower-eyelid incision. It must also be noted, however, that the lower-lid approach is not without significant risks, such as the possibility of lower-lid malposition and external lid scarring. For this reason, the subciliary incision should be avoided in facial trauma in favor of subtarsal incision, especially in older patients with multiple facial rhytides, should a transcutaneous approach be chosen for access.20,21 In most patients, however, a tranconjunctival approach is preferred.22,23 As a general rule, the gingivobuccal incision should be made prior to the lower-eyelid incision. If one were to perform the lower-eyelid incision first, dissection is frequently more difficult because the fracture fragment is not in an anatomic location and results in the surgeon having to dissect through the lower lid much more extensively than is necessary if the fracture had already been grossly reduced.
One tool that is particularly useful for three-dimensional manipulation of the ZMC is the Carol-Gerard screw. This tool can be placed through the lower-eyelid incision into the substance of the malar eminence and used to manipulate the fracture fragment into the correct position.
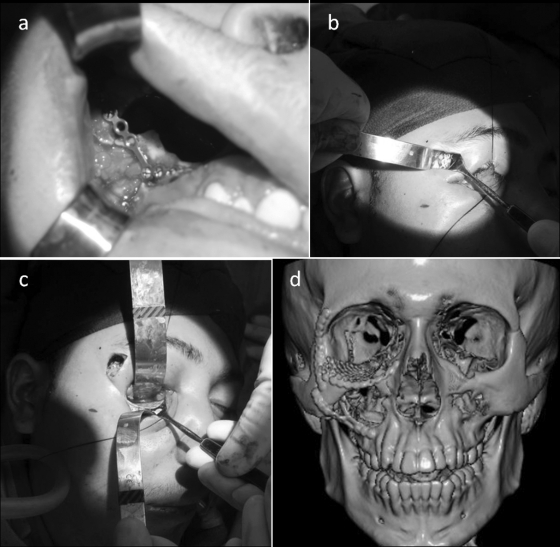
In most cases, these will be the only two incisions necessary for treatment, given the relative strength of the ZF pillar, which typically makes it the last buttress to be displaced. If indeed this displacement is seen on the preoperative CT scan, then consideration can be given to making a lateral eyebrow or upper-lid incision to visualize this buttress (Fig. 3).
Figure 3.
Operative incisions. (A, B) Often, the gingivobuccal sulcus and lower-eyelid incisions are the only two incisions necessary for treatment. (C) Reduction and fixation of ZF fracture may require lateral eyebrow or upper-eyelid incision. (D) Plates are placed along ZMB, infraorbital rim, and, if needed, ZF suture.
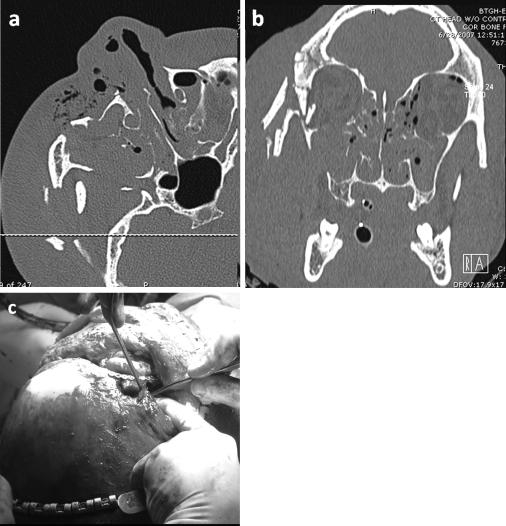
Although fraught with complications, the coronal incision should be considered in complex fractures with severe comminution, difficult reductions, or cases where the arch is laterally displaced (Fig. 4). This is a more significant exposure but is incredibly useful in appropriately positioning the fracture fragment when it is necessary and does not require a subsequent inferior orbital incision. Such an access is also crucial in an inferiorly displaced fracture where accurate alignment and stabilization at this level can reestablish the vertical position of the fracture fragment.
Figure 4.
Coronal incision. A coronal incision can be incredibly helpful in complex fractures with severe comminution (A, B), difficult reductions, or severely displaced arch. Note the amount of exposure afforded by this incision (C).
INTERNAL FIXATION
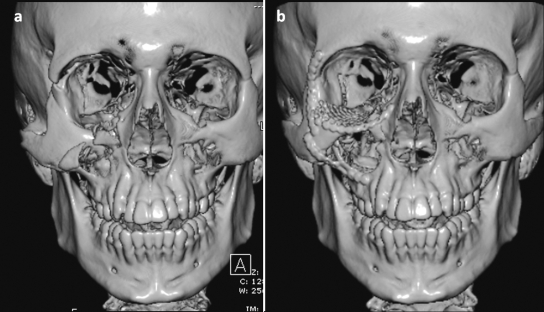
As a general rule, one large plate (2 mm) along the ZMB probably provides enough stability in most cases. The reason that many patients end up with plates at the other buttresses is that this helps the surgeon sequentially align the fracture fragments. However, it is very difficult to hold the malar complex in optimal reduction with just one plate in the ZMB holding reduction. Therefore, in most cases, the ZF suture is secured first with a wire or a small plate (1 to 1.5 mm). With this vertical position of the fracture established, attention is then turned to the infraorbital rim and ZMB. When these are relatively aligned, a small plate (1.5 mm) is placed along the infraorbital rim, taking care to place the plate superiorly rather than anteriorly to avoid palpability. Lastly, a 2-mm L-plate is placed along the ZMB (Fig. 5). If the arch is to be plated, then it must be remembered that the arch is essentially a straight structure.13,24,25 Plating as a true arch will result in recession of the malar eminence and expansion of the orbital volume. If exposed and reduced, then the arch should always be plated first.13
Figure 5.
Preoperative (A) and postoperative (B) images. Postoperative scans can be helpful in assessing the adequacy of reduction and fixation of ZMC fractures.
Once the zygomaticomaxillary fractures have been plated, attention is typically turned to the orbital component of the injury. Although detailed review of the management of orbital floor fractures is beyond the scope of this article, it is worth discussing the appropriate type and proper placement of orbital floor implants. Most surgeons today use alloplastic material such as titanium meshes, high-density polyethylene (MedPor; Porex Surgical, Newnan, GA), or a combination of the two.13 An implant that combines titanium mesh within the polyethylene combines support and pliability of titanium mesh with the ease of use afforded by the polyethlene. Bone grafting is also acceptable, although it is not typically necessary in these cases. The classic mistake when inserting the implant is to place it straight back into the maxillary antrum. As the orbital floor inclines superiorly, the implant must be placed up on the stable posterior ledge (Fig. 6).26
Figure 6.
Orbital floor reconstruction. Care must be taken to ensure that the orbital floor implant is placed up on the stable posterior ledge. The classic mistake here is to place the implant straight back into the maxillary antrum.
Assessing for the accuracy of reduction at the completion of the case can be difficult. In general, the most accurate area to check for adequacy of reduction and prevent future complications is the ZS suture along the lateral orbital wall. Rather deceivingly, the infraorbital rim and ZMB can appear relatively well aligned while there is still significant lateral rotation of the malar complex in its posterior component. If one examines the lateral wall or slides an elevator here, misalignment will easily be made known by a step-off in this region. Every effort should be made to overrotate the posterior aspect of the fragment in cases of uncertain fragment position to cause relative compression of the orbital contents.
At the end of the procedure, one should also closely evaluate the anteroposterior position of the globes. When accounting for the swelling on the operative side, the globe should be more anteriorly projected than on the normal side. If the globes are symmetric or if the operated side is posteriorly displaced, one should assume that the orbital volume is still too large and further correction is required. If repositioning the malar complex at this point does not seem to help, then one option is to add more volume to the orbital cone. One potential solution is to place a high-density porous polyethylene into the posterolateral aspect of the lateral cone and subsequently shape these wedges to an appropriate size.26 When placed posteriorly and laterally in the orbit, these implants can increase the projection of the globe without altering the vertical dimension and causing hyperglobus.
Upon completion of fixation and adequate globe positioning, a consideration for soft tissue midface suspension to the infraorbital rim plate or to the lateral orbital rim periosteum should be given. Although not absolutely necessary in all patients, resuspension helps to support the lower-eyelid closure and minimize the risk of ectropion. In thin patients, resuspension can prevent the appearance of malar ptosis. In some cases in which the tear trough or an implant appears to be too pronounced, a small sheet of acellular dermal matrix may be useful in smoothing this area and covering the hardware at the level of the infraorbital rim.26 A forced duction test must be performed prior to skin closure to ensure that the implant has not entrapped the intraocular contents.13
PEDIATRIC ZMC FRACTURES
The treatment of ZMC fractures in the pediatric population deserves special attention. Treatment is complicated by the pediatric skeleton's capacity for remodeling as well as growth.27 Many of the operative fracture patterns seen in adults can be managed conservatively in children as clinical evidence suggests that many fractures in children remodel with little or no intervention.28 This statement holds true at our institution where most ZMC fractures are managed conservatively, at least initially, despite having variable degrees of displacement.
When indicated, open reduction and plate-and-screw fixation for the pediatric population is well tolerated.29 However, there are a few basic tenets that are important to note for this treatment population. First, the exposure of the fracture site should be minimized as evidence suggests that soft tissue undermining during surgery can adversely affect growth.30,31 Next, the use of resorbable plates is an increasingly attractive option and is well tolerated in children. Permanent implants have the potential to migrate in addition to having deleterious effect on growth. However, the strength of equally sized resorbable and metallic plates is not equivalent due to the biomechanics of the resorbable plates themselves. Therefore, either larger resorbable plates will need to be used or they will need to be augmented with additional methods (wires or splints) to achieve desired fixation.
COMPLICATIONS
Potential complications associated with ZMC fractures include malar malposition, enophthalmos, visual disturbances, and persistent sensory disturbances of the cheek. The most troubling of these complications are postoperative diplopia and enophthalmos, and both tend to be related to fracture severity and failure to accurately reduce and reconstruct the orbital walls. The best method of managing enophthalmos remains prevention of the complication itself because no effective solution exists to truly manage the complication postoperatively. If enophthalmos is noted in the early postoperative period, the best solution is to return the patient to the operating room for revision reduction and fixation. Early diagnosis of the complication is greatly facilitated if the surgeon routinely obtains immediate postoperative CT scans of the patient, which allows detection of gross malreductions while the patient is still in the hospital. Another option is to scan the patient intraoperatively with a portable CT scanner. The use of these scanners is increasingly practiced, especially in the neurosurgical intensive care units for those critically ill patients who require frequent CT scans.32 More data are needed before recommending routine use of this new technology.
One of the most common complaints after surgical management of ZMC fracture is paresthesia along the infraorbital nerve distribution.33 These cases are mostly secondary to compression of the nerve, but the degree of compression can vary widely. More importantly, neurapraxia and nerve injuries seen in the setting of facial fracture repair are also often the result of undue traction on the nerve by the surgical assistant. Every attempt should be made to carefully identify and protect the nerves during surgical exposure and manipulation to avoid any iatrogenic traction injuries. The benefit of surgery, though, to improve upon these sensory disturbances is variable. One study found that half of individuals on long-term follow-up believed that paresthesias had either not improved or worsened after attempted corrective procedure.33,34
Various complications can result from metallic plate fixation. Although the rates and reasons for plate removal vary widely among study groups, the main indications for plate removal are infection, plate exposure, patients' request, cold intolerance, and/or plates being palpable.35,36 However, surgical access for plate retrieval is oftentimes difficult and tedious, which must be weighed against the possibility of symptomatic relief with plate removal.
Surprisingly, postoperative infections are uncommon after isolated zygomatic fractures. In general, the potential risk will vary based on mechanism of injury, degree of contamination, prosthetic insertion, duration of surgery, and patient comorbidities, but this is still extremely low. In fact, a systematic review concluded that infection rates were so low in isolated zygomatic fractures that prophylactic antibiotics were not recommended.37 Likewise, other complications, excluding those related to the lower eyelid, are relatively uncommon and rarely require intervention.
CONCLUSION
Optimal management of ZMC fractures begins with accurate and expedient diagnosis followed by formulation of a treatment plan that accounts for proper reduction of fractured segments to restore facial balance. Finally, surgical expertise is needed to allow for appropriate execution of treatment plan as well as to manage complications should they arise.
References
- Kelley P, Crawford M, Higuera S, Hollier L H. Two hundred ninety-four consecutive facial fractures in an urban trauma center: lessons learned. Plast Reconstr Surg. 2005;116:42e–49e. doi: 10.1097/01.prs.0000177687.83247.27. [DOI] [PubMed] [Google Scholar]
- Erdmann D, Follmar K E, Debruijn M, et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008;60:398–403. doi: 10.1097/SAP.0b013e318133a87b. [DOI] [PubMed] [Google Scholar]
- Bogusiak K, Arkuszewski P. Characteristics and epidemiology of zygomaticomaxillary complex fractures. J Craniofac Surg. 2010;21:1018–1023. doi: 10.1097/scs.0b013e3181e62e47. [DOI] [PubMed] [Google Scholar]
- Chapman V M, Fenton L Z, Gao D, Strain J D. Facial fractures in children: unique patterns of injury observed by computed tomography. J Comput Assist Tomogr. 2009;33:70–72. doi: 10.1097/RCT.0b013e318169bfdc. [DOI] [PubMed] [Google Scholar]
- Murphy R X, Jr, Birmingham K L, Okunski W J, Wasser T. The influence of airbag and restraining devices on the patterns of facial trauma in motor vehicle collisions. Plast Reconstr Surg. 2000;105:516–520. doi: 10.1097/00006534-200002000-00005. [DOI] [PubMed] [Google Scholar]
- Guly C M, Guly H R, Bouamra O, Gray R H, Lecky F E. Ocular injuries in patients with major trauma. Emerg Med J. 2006;23:915–917. doi: 10.1136/emj.2006.038562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- al-Qurainy I A, Stassen L FA, Dutton G N, Moos K F, el-Attar A. The characteristics of midfacial fractures and the association with ocular injury: a prospective study. Br J Oral Maxillofac Surg. 1991;29:291–301. doi: 10.1016/0266-4356(91)90114-k. [DOI] [PubMed] [Google Scholar]
- Jamal B T, Pfahler S M, Lane K A, et al. Ophthalmic injuries in patients with zygomaticomaxillary complex fractures requiring surgical repair. J Oral Maxillofac Surg. 2009;67:986–989. doi: 10.1016/j.joms.2008.12.035. [DOI] [PubMed] [Google Scholar]
- Levin L A, Beck R W, Joseph M P, Seiff S, Kraker R. The treatment of traumatic optic neuropathy: the International Optic Nerve Trauma Study. Ophthalmology. 1999;106:1268–1277. doi: 10.1016/s0161-6420(99)00707-1. [DOI] [PubMed] [Google Scholar]
- Wang B H, Robertson B C, Girotto J A, et al. Traumatic optic neuropathy: a review of 61 patients. Plast Reconstr Surg. 2001;107:1655–1664. doi: 10.1097/00006534-200106000-00003. [DOI] [PubMed] [Google Scholar]
- Warner J EA, Lessell S. Traumatic optic neuropathy. Int Ophthalmol Clin. 1995;35:57–62. doi: 10.1097/00004397-199503510-00007. [DOI] [PubMed] [Google Scholar]
- Bacelar M T, Rao V M. Facial and other head and neck trauma: Imaging patterns and their significance. Appl Radiol. 2002;31:20–27. [Google Scholar]
- Hollier L H, Thornton J, Pazmino P, Stal S. The management of orbitozygomatic fractures. Plast Reconstr Surg. 2003;111:2386–2392; quiz 2393. doi: 10.1097/01.PRS.0000061010.42215.23. [DOI] [PubMed] [Google Scholar]
- Tahernia A, Erdmann D, Follmar K, Mukundan S, Grimes J, Marcus J R. Clinical implications of orbital volume change in the management of isolated and zygomaticomaxillary complex-associated orbital floor injuries. Plast Reconstr Surg. 2009;123:968–975. doi: 10.1097/PRS.0b013e318199f486. [DOI] [PubMed] [Google Scholar]
- Czerwinski M, Izadpanah A, Ma S, Chankowsky J, Williams H B. Quantitative analysis of the orbital floor defect after zygoma fracture repair. J Oral Maxillofac Surg. 2008;66:1869–1874. doi: 10.1016/j.joms.2007.11.014. [DOI] [PubMed] [Google Scholar]
- Schubert W, Jenabzadeh K. Endoscopic approach to maxillofacial trauma. J Craniofac Surg. 2009;20:154–156. doi: 10.1097/SCS.0b013e318191cfb8. [DOI] [PubMed] [Google Scholar]
- Xie L, Shao Y, Hu Y, Li H, Gao L, Hu H. Modification of surgical technique in isolated zygomatic arch fracture repair: seven case studies. Int J Oral Maxillofac Surg. 2009;38:1096–1100. doi: 10.1016/j.ijom.2009.05.004. [DOI] [PubMed] [Google Scholar]
- Olate S, Lima S M, Jr, Sawazaki R, Moreira R WF, de Moraes M. Surgical approaches and fixation patterns in zygomatic complex fractures. J Craniofac Surg. 2010;21:1213–1217. doi: 10.1097/SCS.0b013e3181e1b2b7. [DOI] [PubMed] [Google Scholar]
- Manson P N, Markowitz B, Mirvis S, Dunham M, Yaremchuk M. Toward CT-based facial fracture treatment. Plast Reconstr Surg. 1990;85:202–212. discussion 213–214. [PubMed] [Google Scholar]
- Appling W D, Patrinely J R, Salzer T A. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg. 1993;119:1000–1007. doi: 10.1001/archotol.1993.01880210090012. [DOI] [PubMed] [Google Scholar]
- Werther J R. Cutaneous approaches to the lower lid and orbit. J Oral Maxillofac Surg. 1998;56:60–65. doi: 10.1016/s0278-2391(98)90917-x. [DOI] [PubMed] [Google Scholar]
- Baumann A, Ewers R. Use of the preseptal transconjunctival approach in orbit reconstruction surgery. J Oral Maxillofac Surg. 2001;59:287–291. discussion 291–292. doi: 10.1053/joms.2001.20997. [DOI] [PubMed] [Google Scholar]
- Mullins J B, Holds J B, Branham G H, Thomas J R. Complications of the transconjunctival approach. A review of 400 cases. Arch Otolaryngol Head Neck Surg. 1997;123:385–388. doi: 10.1001/archoto.123.4.385. [DOI] [PubMed] [Google Scholar]
- Covington D S, Wainwright D J, Teichgraeber J F, Parks D H. Changing patterns in the epidemiology and treatment of zygoma fractures: 10-year review. J Trauma. 1994;37:243–248. doi: 10.1097/00005373-199408000-00016. [DOI] [PubMed] [Google Scholar]
- Zingg M, Laedrach K, Chen J, et al. Classification and treatment of zygomatic fractures: a review of 1,025 cases. J Oral Maxillofac Surg. 1992;50:778–790. doi: 10.1016/0278-2391(92)90266-3. [DOI] [PubMed] [Google Scholar]
- Kaufman Y, Stal D, Cole P, Hollier L., Jr Orbitozygomatic fracture management. Plast Reconstr Surg. 2008;121:1370–1374. doi: 10.1097/01.prs.0000308390.64117.95. [DOI] [PubMed] [Google Scholar]
- Smartt J M, Jr, Low D W, Bartlett S P. The pediatric mandible: I. A primer on growth and development. Plast Reconstr Surg. 2005;116:14e–23e. doi: 10.1097/01.prs.0000169940.69315.9c. [DOI] [PubMed] [Google Scholar]
- Leake D, Doykos J, III, Habal M B, Murray J E. Long-term follow-up of fractures of the mandibular condyle in children. Plast Reconstr Surg. 1971;47:127–131. doi: 10.1097/00006534-197102000-00005. [DOI] [PubMed] [Google Scholar]
- Koltai P J, Rabkin D, Hoehn J. Rigid fixation of facial fractures in children. J Craniomaxillofac Trauma. 1995;1:32–42. [PubMed] [Google Scholar]
- Bardach J, Kelly K M. Does interference with mucoperiosteum and palatal bone affect craniofacial growth? An experimental study in beagles. Plast Reconstr Surg. 1990;86:1093–1100. discussion 1101–1102. [PubMed] [Google Scholar]
- Bardach J, Kelly K M, Salyer K E. The effects of lip repair with and without soft-tissue undermining and delayed palate repair on maxillary growth: an experimental study in beagles. Plast Reconstr Surg. 1994;94:343–351. doi: 10.1097/00006534-199408000-00020. [DOI] [PubMed] [Google Scholar]
- Demianczuk A NA, Antonyshyn O M. Application of a three-dimensional intraoperative navigational system in craniofacial surgery. J Craniofac Surg. 1997;8:290–297. doi: 10.1097/00001665-199707000-00012. [DOI] [PubMed] [Google Scholar]
- Kurita M, Okazaki M, Ozaki M, et al. Patient satisfaction after open reduction and internal fixation of zygomatic bone fractures. J Craniofac Surg. 2010;21:45–49. doi: 10.1097/SCS.0b013e3181c36304. [DOI] [PubMed] [Google Scholar]
- Pedemonte C, Basili A. Predictive factors in infraorbital sensitivity disturbances following zygomaticomaxillary fractures. Int J Oral Maxillofac Surg. 2005;34:503–506. doi: 10.1016/j.ijom.2004.10.026. [DOI] [PubMed] [Google Scholar]
- Rallis G, Mourouzis C, Papakosta V, Papanastasiou G, Zachariades N. Reasons for miniplate removal following maxillofacial trauma: a 4-year study. J Craniomaxillofac Surg. 2006;34:435–439. doi: 10.1016/j.jcms.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Thorén H, Snäll J, Kormi E, Lindqvist C, Suominen-Taipale L, Törnwall J. Symptomatic plate removal after treatment of facial fractures. J Craniomaxillofac Surg. 2010;38:505–510. doi: 10.1016/j.jcms.2010.01.005. [DOI] [PubMed] [Google Scholar]
- Andreasen J O, Jensen S S, Schwartz O, Hillerup Y. A systematic review of prophylactic antibiotics in the surgical treatment of maxillofacial fractures. J Oral Maxillofac Surg. 2006;64:1664–1668. doi: 10.1016/j.joms.2006.02.032. [DOI] [PubMed] [Google Scholar]