Abstract
Orbital fractures account for a significant portion of traumatic facial injuries. Although plastic surgery literature is helpful, additional pearls and insights are provided in this article from the experience of an oculoplastic surgeon. The fundamentals remain the same, but the perceptions differ and provide a healthy perspective on a long-standing issue. The most important thing to remember is that the optimal management plan is often variable, and the proper choice regarding which plan to choose rests upon the clinical scenario and the surgeon having an honest perception of his or her level of expertise and comfort level.
Keywords: Orbital fractures, orbital floor, orbital roof, medial orbital wall, lateral orbital wall, orbitozygomatic fractures, enophthalmos, ectropion, lower, facial trauma, entrapment
A comprehensive understanding of orbital fractures is necessary for the treating physician due to the functional and aesthetic deformities that often result. Studies have estimated that orbital fractures account for roughly 10 to 25% of all cases of facial fractures,1,2,3 and, similar to all facial trauma, are most commonly seen in conjunction with assaults and motor vehicle accidents (MVAs). MVA-related orbital fractures, in particular, tend to be more destructive and are associated with more concomitant organ injuries, zygoma fractures, and multiple orbital wall fractures than the other common causes of assault, sports-related, falls, and so forth.4 Penetrating orbital injuries occur less frequently but are associated with a greater than 10% incidence of death or subsequent vegetative state, mostly due to adjacent intracranial injuries.5 Additionally, damage to the globe, optic nerve, and extraocular muscles are always a concern.
An understanding of the essential subtleties of orbital injuries requires an appreciation for the orbital examination, appropriate management, and potential complications.
INITIAL ASSESSMENT
As with all maxillofacial trauma, appropriate assessment begins with Advanced Trauma Life Support guidelines. After patient stabilization, orbital fractures should be suspected based on clinical signs and the mechanism of injury.
The most common clinical signs seen with adult orbital fractures are periorbital ecchymoses and subconjunctival hemorrhages (Fig. 1); however, the absence of such signs do not rule out an orbital floor fracture, particularly in the pediatric population. In a 2007 study by Lane et al, 43% of pediatric orbital floor fractures were not associated with grossly visible signs, resulting in a “white-eyed blowout fracture” that often only a careful ophthalmic motility examination will uncover.6 Furthermore, ∼5% of adults with head trauma have occult orbital fractures, and approximately half of these require surgical intervention.7
Figure 1.
Physical findings that should increase suspicion for an underlying orbital fracture include periorbital ecchymoses and subconjunctival hemorrhages.
Even in the absence of appreciated physical signs, several patient complaints should illicit strong suspicion of an occult orbital fracture, including mild proptosis, eyelid swelling; orbital or eyelid pressure; chemosis after nose blowing; a “crackling” sound upon eyelid pressure or eye movement; numbness of the cheek, side of the nose, or ipsilateral front two teeth; pain or nausea in a particular gaze direction; and an unexplained desire to keep an eye closed after trauma.
Any of the above-mentioned findings as well as consistent mechanisms of injury should prompt a suspicion for an orbital fracture. However, we are often consulted to see patients after an orbital fracture has already been diagnosed with the aid of computed tomography (CT). When this occurs, the essential questions to answer become the following: (1) Are there associated neurologic or ophthalmologic injuries that require management, potentially altering the approach and timing of orbital reconstruction? (2) Does the fracture merit repair?
OPHTHALMOLOGIC EVALUATION
Eleven to 15% of orbital fractures are associated with ophthalmological emergencies, the majority of which will present with diminished visual acuity or other visual changes.8,9 However, it is important to note that although decreased vision in the setting of trauma is common, such a finding is neither 100% sensitive nor specific for ophthalmologic emergencies. For example, testing vision with a near vision card in the absence of reading glasses or with eyelid swelling causing temporary, but significant, astigmatism may result in spuriously poor vision, whereas a self-sealing anterior scleral laceration or a peripheral retinal injury may not significantly alter grossly tested vision. The most time-critical ophthalmic emergency related to orbital trauma is ophthalmic infarction secondary to orbital compartment syndrome. This syndrome may occur from acute hemorrhage (most commonly involving lacerations of the infraorbital artery or the anterior or posterior ethmoid arteries), soft tissue swelling, severe implosion of the orbit by inwardly rotated bone fragments causing tissue impaction, or even orbital emphysema. Sneezing or nose blowing in patients with orbital fractures may suddenly introduce large air volumes into the orbit from the adjacent sinuses and nose, and the orbital fat can act as a ball valve, creating sudden orbital pressure and compartment syndrome with attendant vascular compromise and ocular or optic nerve stroke. Importantly, primate studies have shown irreversible vision loss after roughly 90 minutes of tissue hypoxia. Every minute may count, and if a facial reconstructive surgeon is the first to recognize and attend a patient with such an injury, awaiting input from an ophthalmology consultation before intervening may not be prudent.
Orbital compartment syndrome with evidence of optic nerve infarct mandates emergent orbital decompression via open technique, CT-guided needle aspiration, or lateral cantholysis. If lateral cantholysis is chosen, be aware that profound orbital pressure from continued, brisk hemorrhage may lead to progressive exophthalmos no longer held in check by the eyelids, and in rare cases stretch optic neuropathy or even optic nerve avulsion may result.
Other significant ocular injuries that may require urgent, but less emergent, intervention include a ruptured globe, retinal tears or detachment, vitreous hemorrhage, hyphema, extraocular muscle injury, bone fragments impinging on the globe, orbital cellulitis, and traumatic optic neuropathy.9
Traumatic optic neuropathy, is seen in ∼0.5 to 5% of orbital trauma patients.10 Traumatic optic neuropathy may result from direct injury to the nerve by a penetrating object, fractured bone fragments impinging on the nerve, vibrational transmission of forces to the optic nerve from the craniofacial skeleton, shearing force at the optic foramen, or nerve compression from extrinsic (hematoma) or intrinsic (hematoma or edema) sources. A high index of suspicion for this type of injury should be present in any patient who presents with periorbital trauma, lacerations or contusions at the occiput, glabella, or over the lateral superior orbital rim; altered visual acuity; diminished visual field; abnormal pupillary response; or change in bright light or red color perception; and it may occur in the absence of facial fractures. Testing for red color desaturation in the setting of orbital trauma is a sensitive indication of optic nerve injury and can help in determining the cause of a vision change. This test is performed by showing the patient a bright red object and having them assess the hue and color intensity (not image clarity) with one eye at a time. The color should appear the same with each eye. A similar white-light intensity test, although less sensitive than the red color test, may be more useful in patients with blood within the eye or unwillingness to open their eyelids.
In the emergency department, in the face of life- or limb-threatening injuries, the consequences of an eye that is unable to close from an eyelid laceration or proptosis is often forgotten. However, frank corneal exposure can quickly lead to serious microbial keratitis in an intensive care setting where patients may be unable to express ocular pain. An exposed eye can be managed acutely with thick, lubricating ophthalmic ointment, petroleum jelly, or a clear adhesive dressing (will not stick to a wet eye), to create an effective moisture chamber.
Given the significant risk for intraorbital injuries, it is reasonable for all patients with suspected orbital fracture to undergo a formal, comprehensive ophthalmology consultation to rule out interventions that might supersede orbital fracture repair. However, it is also incumbent upon all facial surgeons who perform orbital surgeries to conduct their own independent ocular and periocular assessments, as they are ultimately responsible for the patient's outcome. Equally important is a basic understanding of ocular anatomy for both correct diagnosis and effective communication. With a penlight, nobody should confuse an opacified cornea with a cataract; the former blocks and scatters light on the surface of the eye, whereas the latter does so within the eye. In a trauma setting, the implications may be profoundly different.
The key components to the physical examination are gross and focused penlight inspection of the eye and ocular adnexa; palpation for areas of step-off, point tenderness, and crepitus from subcutaneous emphysema; examination of extraocular muscle function; gross or Tono-Pen (Reichert, Inc., Buffalo, NY) evaluation of intraocular pressure; visual acuity and fields; pupillary evaluation; fundus exam with a direct ophthalmoscope; and a cranial nerve exam.
The penlight examination of the eye and ocular adnexa should be performed to look for conjunctival hyperemia, chemosis, and flattening of the anterior chamber. Hyperemia suggests focal irritation, and a cause, such as a superficial laceration or retained foreign body, should be excluded. Chemosis may herald a hidden globe rupture or simply a bruise indicating significant local trauma. Irregularities of the cornea may indicate a self-sealing corneal laceration. Flattening of the anterior chamber suggests ocular perforation. A “sunsetting,” subluxed lens, half visible in the pupil, may lead to serious ocular complications if not addressed. A layering of blood or purulence in the anterior chamber portends potentially serious ocular disease.
A rough and dirty assessment of orbital pressure may be made by asking the patient to open their eyes. Easy and full eyelid opening generally belies severe orbital pressure. In the absence of the patient's ability or cooperation, gently separating the upper and lower eyelids with one's fingers provides a fair assessment of pressure pushing the eye forward. In the presence of high orbital pressure, the globe is pressed tightly against the eyelids, creating resistance to eyelid opening.
Other signs may lead to an increased suspicion for concomitant injuries. For example, cutaneous lacerations and contusions may point toward underlying corneal, globe, canthal tendon (telecanthus), lacrimal apparatus, or optic nerve injuries.11 Fat protruding from a periocular laceration means orbital penetration. An upper-eyelid laceration should prompt an examination of the eye both above and below the cornea, because with forced eyelid closure, as may precede injury, the Bell phenomenon causes the eye to rotate upward, and an upper-eyelid laceration may penetrate the globe below the cornea. An irregularly-shaped pupil (corectopia), particularly a teardrop shape, is indicative of anterior penetrating injury tract with the point of the teardrop pointing toward the globe laceration. Relative afferent pupillary defects are elicited with the swinging-flashlight test, and a positive test results from unilateral injury to the retina, optic nerve, optic chiasm, or optic tract.
ORBITAL ANATOMY, IMAGING, AND IDENTIFYING OPERATIVE CANDIDATES
The structural integrity of the orbital floor, medial and lateral walls, and roof function to maintain the volume of the orbit, prevent displacement of orbital contents, and separate the orbital contents from surrounding structures. The most anterior portion of these walls, the orbital rim, is formed by thick cortical bone that provides a stable buttress for the craniofacial skeleton. The middle-third of the orbital walls is significantly thinner and more prone to fracture. Each wall varies in thickness, and accordingly, those with the thinnest walls—the medial wall (lamina papyracea) and orbital floor—are the most susceptible to fracture. Although the medial wall has the thinnest bone, a buttressing effect of the ethmoid sinus laminas makes the orbital floor more readily fractured. Together, fractures in the region of the medial wall and orbital floor account for 81% of all orbital fractures when the predominant mechanism of injury is assault.1 The thick lateral wall, in contrast, is further supported by the temporalis muscle, which helps protect it from both medial and lateral displacement, making lateral wall fractures less common unless associated with zygomatic arch and maxillary fractures. Although the orbital rim at the roof is the most forward-projecting portion of the rim, in adults, orbital roof fractures are the least common, due in part to the thicker bone and in part to the proximity of the frontal sinus, which may preferentially collapse.
Imaging
The most useful imaging modality in trauma patients is CT. Axial, coronal, and sagittal images may be obtained through the orbital region. In general, 3-mm sections will suffice, but in situations where fine detail is required, 1.25-mm thin slices or less may be desirable. Axial images and three-dimensional re-formations can be used to evaluate the orbital rims, as well as fractures involving the zygomaticofrontal suture and zygomaticomaxillary buttress. In general, however, three-dimensional reformations of the orbit are not very helpful for isolated orbital fractures. Coronal images are particularly useful to identify orbital roof, floor, or extraocular muscle involvement, as well as the degree of enophthalmos, whereas medial and lateral wall fractures are often more easily conceptualized when viewing axial images. Lastly, sagittal images may be helpful in assessing orbital floor and roof fractures, but the real power of sagittal sections is as a self-assessing tool postoperatively for novice orbital surgeons who wish to understand how well they were able to approximate the normal contour of the orbital floor.
ORBITAL FLOOR
The most common indication for emergent repair of an orbital floor fracture is extraocular muscle entrapment. This injury is common in the pediatric patient whose orbital floor is more apt to greenstick rather than down-fracture, and then bounce back, entrapping the inferior rectus muscle. In adults, rectus muscle entrapment may also occur with the inferior, medial, lateral, and superior recti incarcerated with decreasing frequencies, mirroring the frequency of associated orbital walls. Although midposterior muscle entrapments are more common, because the muscles are in closest apposition to their respective orbital walls at that point, muscle entrapments may occur anteriorly or posteriorly in the orbit. In general, anterior entrapments are more likely to restrict globe movement away from the entrapped muscle, whereas posterior entrapments more often cause decreased movement in the direction of the entrapped muscle.
Diplopia, or double vision, does not in itself mean entrapment of an extraocular muscle, as global orbital edema may diminish eye movement. Back et al have shown that ∼80% of cases that initially present with decreased eye excursion resolve within a short period of time.12 This is attributed to the fact that trauma to the soft tissue can cause nerve paresis, inferior rectus contusion, and local edema, all of which may mimic inferior rectus entrapment. However, decreased eye movement in one gaze meridian or axis is highly suggestive of extraocular muscle dysfunction, especially if the movement deficit is vertical. Forced duction testing, CT imaging, and pain on eye movement can all be helpful, but none are 100% sensitive or specific. Muscle and neurovascular compromise may accompany muscle entrapment, especially with the inferior rectus.
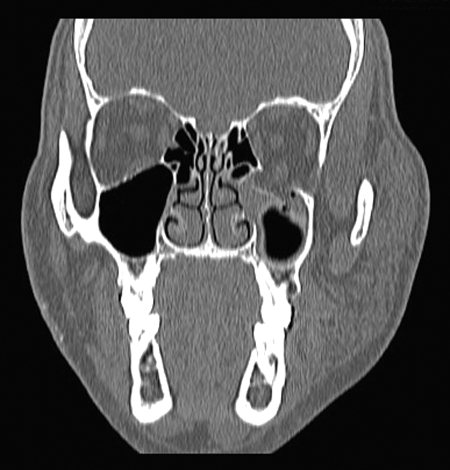
In children, determination of restricted gaze excursion may be difficult, as children are frightened to report diplopia, and may poorly cooperate due to pain associated with muscle entrapment and subsequently keep their eye closed. A higher degree of suspicion should be had in the pediatric population when the child presents with an orbital fracture, nausea and vomiting, as this clinical triad carries a greater than 80% positive predictive value for entrapment, which necessitates a more urgent intervention.13 Diagnosis of inferior rectus entrapment within the orbital floor fracture may be confirmed by CT scan. However, it should be noted that CT imaging does not always correlate well with the clinical findings. Some “entrapments” on CT scan may present without clinical dysmotility, and some muscle sheath or frank muscle belly entrapments can be missed by radiologists. Figure 2 shows an inferior rectus muscle in the plane of the usual position of the orbital floor. The wide space around the muscle suggests no entrapment at this section of imaging, but with tremendous local inflammation and swelling, the muscle might behave as though it is entrapped (Fig. 2). Figure 3 demonstrates tissue incarceration by a fracture of the orbital floor. The otherwise normal shape and size of the inferior rectus muscle belies muscle injury or entrapment, but the clinical examination may tell a different story (Fig. 3).
Figure 2.
Orbital floor fracture that involves greater than 50% of the orbital floor with enophthalmos greater than 2 mm. These cases may not present clinically with enophthalmos in the acute setting because of significant soft tissue edema, which is why CT scans play a major role in diagnosing operative candidates in the acute stages.
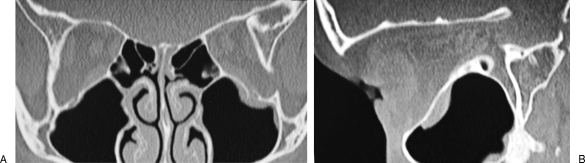
Figure 3.
(A, B) CT scans of a pediatric patient who presented with nausea and vomiting after facial trauma. Emergent operative intervention of this trapdoor orbital floor fracture with muscle entrapment is indicated to prevent prolonged muscle ischemia.
Nonemergent operative indications for the orbital floor include (1) fractures that involve greater than 50% of the floor (Fig. 2), (2) fractures greater than 1 cm2, and (3) hypoglobus or enophthalmos > 2 mm. Additionally, zygomaticomaxillary complex (ZMC) fractures, when posteriorly displaced, will cause the orbital floor to buckle posteriorly. When the ZMC is reduced into anatomic position, a significant orbital floor defect may be created, requiring surgical reconstruction. Surgical exploration of the orbital floor is necessary in patients with 1 cm or more of posterior displacement.14 Orbital exploration may also be considered whenever significant rotation of the ZMC segment is repaired to ensure that orbital contents were not incarcerated during the rotation.
MEDIAL WALL
The medial orbital wall has four primary structural and functional features. First, this portion of the orbit separates the orbital contents from the ethmoid air cells. Small medial orbital wall fractures often present with orbital emphysema due to fracture and involvement of the adjacent nares and ethmoid air cells. As previously discussed, air that is subsequently trapped within the orbit has the potential to cause vascular compromise to the intraorbital contents if significant, although true vision-threatening orbital compartment syndrome under these circumstances is rare. Second, the medial wall and rim provide a site of insertion for the medial canthal tendon, and fractures of the medial wall may lead to telecanthus. Third, the anterior and posterior limbs of the medial canthal tendon encase the nasolacrimal sac, and severe damage in this area may lead to tear outflow obstruction. Finally, the anterior and posterior ethmoidal arteries traverse the medial wall at its junction with the orbital roof, carrying blood from the ophthalmic artery to the nasal cavity. Although the ethmoidal arteries are small, usually less than 1 mm in diameter,15 injury to these vessels can cause significant intraorbital hemorrhage and even orbital compartment syndrome. Fractures of the medial wall must accordingly be evaluated for potential effects on these associated structures.
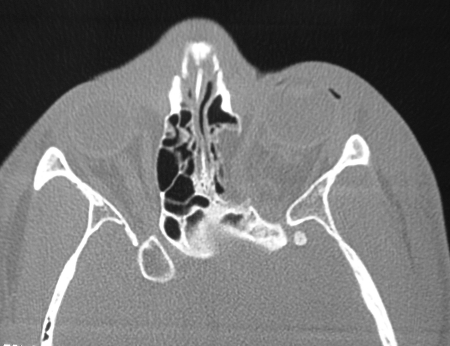
Indications for repair of medial wall fractures are analogous to those for the orbital floor. These include medial rectus muscle entrapment and significant defects of the medial wall, which can result in enophthalmos, especially when associated with large orbital floor fractures or loss of bone support at the junction of the orbital floor and medial wall in the anterior orbit (Fig. 4). Enophthalmos from isolated medial wall fractures occurs less frequently than it does with isolated orbital floor fractures, as the force of gravity does not usually displace intraorbital contents sideways into the adjacent nose and ethmoid sinuses.16
Figure 4.
Medial wall fractures of the orbit have the potential risk of medial rectus entrapment and enophthalmos. The risk of enophthalmos, though, is not necessarily the same as with similarly sized orbital floor fractures. This is because the force of gravity is not displacing orbital contents into the areas of the adjacent sinus, as with orbital floor fractures.
LATERAL WALL
The lateral orbital wall functions to contain the lateral orbital contents and provides the upper-third of the face with its width. Additionally, the lateral wall is the site of insertion for the lateral canthal tendon onto Whitnall's tubercle. Lateral orbital fractures that require surgical intervention are commonly linked to fractures of the zygomatic bone, also known as orbitozygomatic, ZMC, or tripod fractures, and most often result from a lateral blow on the cheek. If the bone fragments are not reduced, a flattening and widening of the side of the face persists, the lateral canthal tendon may be displaced, and the globe may be malpositioned, either exophthalmic if the orbital volume is decreased or enophthalmic if the orbital volume is increased.
ORBITAL ROOF
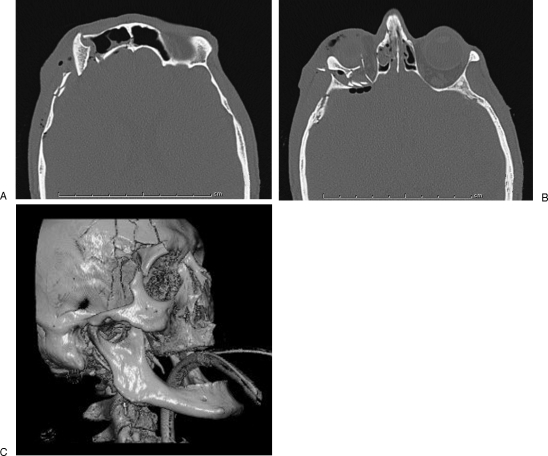
Orbital roof injuries appear more commonly in the pediatric population, prior to the pneumatization of the pediatric craniofacial skeleton.17 In adults, however, orbital roof fractures are significantly less common injuries and tend to occur during high-impact craniofacial trauma, with roughly half occurring during MVAs.18,19 Consequently, there is a high association of orbital roof fractures with neurologic injury (57 to 90%), ocular damage (14 to 38%), and additional orbital (76%) and facial fractures (33%) (Fig. 5).18,19 Also, due to the proximity of the superior rectus and superior oblique muscles to the roof, there is a risk of entrapment associated with these injuries as well as potential damage to the trochlea, the pivot point of the superior oblique muscle. As with all orbital fractures, there is a risk of exophthalmos and enophthalmos, depending on the direction of displacement of the fractured bone fragments.
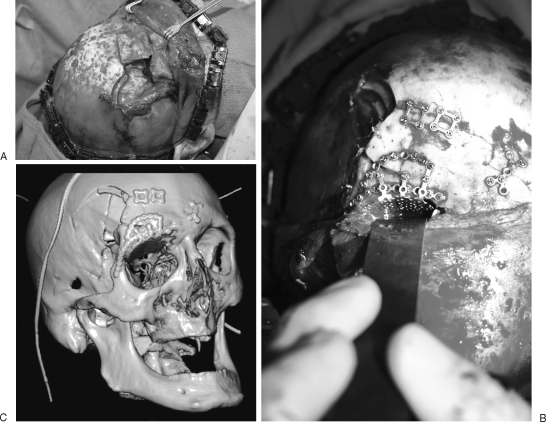
Figure 5.
(A–C) Orbital roof fracture with adjacent damage to the frontal bone and sinus, and lateral orbital wall.
Damage to cranial contents occurs often as well, including dural tears and pneumocephalus. Such injuries carry an increased risk of meningitis and should probably trigger a neurosurgical consultation, although 80% of these injuries resolve spontaneously and can be managed by intravenous antibiotics alone.20
Nondisplaced orbital roof fractures often may be managed conservatively. Superiorly displaced fractures may require intracranial pressure monitoring. However, if there is an associated neurologic injury that requires intervention, the fracture can be repaired concurrently via an intracranial approach. Inferiorly displaced fractures may result in proptosis, hypoglobus, and/or exophthalmos and should be treated surgically.18 Other indications for surgical intervention include diplopia, gaze restriction, and lagophthalmos, which may be caused by injury to the cranial nerves or entrapment of the superior oblique, superior rectus, and levator palpebrae superioris muscles.
Surgical Timing
As previously mentioned, certain orbital injuries require emergent surgical intervention. The timing for nonemergent injuries, however, is an area of contention and often treated in a semi-delayed fashion around 7 to 14 days, before soft tissue scarring develops, but after resolution of posttraumatic edema.21,22 After 2 weeks, soft tissue fibrosis can become significant, especially in young males, and require sharp dissection for reduction of orbital tissues. Sharp dissection techniques are often required at the orbital apex and to separate the infraorbital neurovascular bundle from the inferior rectus muscle and should not be undertaken by the casual or novice orbital surgeon.
Surgical Technique
Intravenous corticosteroids should be administered preoperatively to decrease intraoperative edema, which may distort estimations of globe position and increase the risk of postsurgical orbital congestion and vision loss. The literature, however, does not provide a consensus for specific corticosteroid dosage or type, and usage is generally based on arbitrary practice patterns, which change over time.
ORBITAL FLOOR
As with most orbital surgeries, approaches to the orbital floor can be divided into transcutaneous and transconjunctival approaches, and both have their proponents. The transcutaneous approaches (subciliary, subtarsal, inferior orbital) are better for a wider exposure of the orbital floor, but risk an external scar. The subciliary approach seems to be falling out of general favor, as an extensive review of the plastic surgery literature has revealed a significantly increased risk of postoperative ectropion and other adverse outcomes compared with both transconjunctival and transcutaneous approaches.23 Nevertheless, this remains the approach of choice for many already accomplished in this technique. Among the remaining transcutaneous approaches, the subtarsal has then been preferred over the inferior orbital approach for aesthetic outcomes, particularly in older patients with well-defined subtarsal rhytides. The transconjunctival approach allows for exposure of the orbital floor without external scarring and also limits postoperative ectropion when performed retroseptally; however, when greater exposure is desired, this approach is often supplemented by a lateral canthotomy to gain more visualization and carries a small but real risk of postoperative canthal dystopia.
As with most surgical techniques, there are strong opinions by accomplished orbital surgeons regarding the “best” approach. Undoubtedly the difference in choice is most likely related to training, experience, anatomic comfort, and a sprinkling of anecdotal complications. The retroseptal transconjunctival and subtarsal approaches may be the safest to avoid postoperative complications, but when performed in experienced hands, both the subciliary and preseptal transconjunctival approaches remain just as favored.
It is important with all lower-eyelid approaches to avoid disturbing the orbicularis muscle adjacent to the orbital rim. An infrequent but important complication of infraorbital surgery can be the postoperative adhesion of the eyelid to the inferior orbital rim and is often secondary to orbicularis muscle injury adjacent to this area. If this occurs, massage over weeks to months generally resolves the problem. Corticosteroid injections are rarely required, and reoperation even less so.
A transantral endoscopic approach, such as the Caldwell-Luc, for orbital floor fractures has been advocated by some, because of the decreased risk of lower-eyelid scarring and postoperative malposition, as well as the degree of soft tissue dissection and postoperative edema. Although this technique offers a clear view of any tissues entrapped by the repair, placement of orbital floor implants is more challenging, and there is less direct visualization and protection of the orbital apex. Late fractures are particularly difficult, if not impossible, with this approach. Some surgeons prefer a combined transorbital and transmaxillary, endoscopic approach.
MEDIAL WALL
Approaches to the medial wall include: transcutaneous, transconjunctival, and transnasal incisions. The Lynch incision was the transcutaneous incision of choice at one time for approaching this region and entails an incision extending from the inferomedial portion of the brow to the nasojugal junction. However, excessive scarring in this region has caused most surgeons to modify this classic description to include z-plasties or other ancillary techniques to reduce the incidence of webbing.
Different regions of the conjunctiva can be used as a starting point to access the medial wall. The transcaruncular or retrocaruncular incision provides access to the region via an incision through or posterior to the caruncle and anterior to the semilunar fold. This eliminates an external scar. However, the access provided by this approach does have a learning curve and may be challenging for larger, more complex fractures. Care must also be taken to avoid scarring attachments between the globe and eyelids if overexuberant retraction or excessive wound manipulation occurs. An inferior orbital transconjunctival approach can also be used with or without upward medial extension, but care must be taken to avoid damaging the lacrimal drainage system and the insertion of the inferior oblique.
Intranasal approaches have been described to aid in fracture reduction and augmentation; however, the limited visualization, risk of optic nerve injury with posterior fractures, and technical difficulty associated with this approach are considerable. With more extensive fracture patterns, such as with accompanying nasoorbitoethmoid fractures and orbital roof fractures, access may be achieved via a bicoronal and/or lower-eyelid/intraoral approach.
LATERAL WALL
The lateral wall of the orbit can be exposed through several approaches. A lateral brow or upper blepharoplasty incision can be used as a transcutaneous approach to the lateral orbital rim. A transconjunctival approach may be used to access the superolateral orbital wall, via an incision superior to the lateral canthal tendon, with caution to avoid the medially-situated levator palpebrae superioris, and a ptotic lacrimal gland.
Another method to gain exposure is a direct horizontal incision at the lateral canthus of ∼5 mm with temporary disinsertion of the superior and inferior crus of the lateral canthal tendon. This provides excellent exposure to the entire lateral orbital rim, from suture line to suture line. Coronal, hairline, and lower-eyelid approaches may also be used.
ORBITAL ROOF
Orbital roof fractures can be approached via an upper blepharoplasty incision, but this is mostly for bone fragment removal. The best fixation of orbital roof implants always comes from above, via a coronal incision and transcranial approach (Fig. 6).
Figure 6.
(A–C) Surgical management of the orbital roof fracture from Fig. 5 required management of the frontal sinus fracture, reconstruction of the orbital roof, and fixation of the lateral orbital wall at the zygomaticofrontal suture.
RECONSTRUCTION
Reconstruction and augmentation of the orbital walls is often necessary. Two main options for volume augmentation are autologous grafts and alloplastic implants. Bone grafts may be harvested from the calvarium, iliac crest, rib, or fibula. However, these autologous options are associated with potential donor site morbidity, difficult contouring, and graft resorption. Titanium, high-density porous polyethylene, and many other materials have been used as bone substitutes. They are relatively inert, provide reliable support without donor site morbidity, and are easily adapted to the contour of the orbit. Additionally, most non-smooth-surfaced orbital floor implants do not require fixation due to the nature of the surrounding structures and their relative immobilization. In many cases, the use of alloplastic materials is less expensive than the increased operative time required to harvest bone. However, in very complex craniofacial reconstructions, many highly experienced craniofacial surgeons prefer to avoid a surfeit of foreign material.
Pediatric orbital trauma has distinct nuances pertaining to its reconstruction. Small fractures may be treated with absorbable bioprosthetics, such as polylactic and polyglycolic acid polymer implants, which provide temporary support to the orbital floor and resorb over a period of a year.21 Such materials do not appear to restrict skeletal growth as has been reported with rigid fixation in pediatric patients.22,24 It is important to note, however, that prospective studies to evaluate the loss of support or other complications have not yet been performed, and the use of absorbable implants has not been sufficiently evaluated for orbital fracture defects in excess of 2 cm2.25
After the orbital fracture has been reduced and reconstructed, a forced duction test should be performed to ensure full range of motion. Additionally, it is sometimes desirable to overcorrect the enophthalmos relative to the contralateral globe by a millimeter or so, as resolution of the operative soft tissue swelling of the orbit may recede and result in enophthalmos.
Perhaps the single most important issue during reconstruction is avoidance of optic nerve impingement by implanted materials improperly fixated or too far posteriorly positioned. Extraocular muscle impingement is also problematic, but far less devastating, should it occur.
Regarding hemostasis, two useful points are worth remembering. Adrenaline-soaked gauze can be useful to control sinus mucosal bleeding, but thrombin and adrenaline should be avoided in the posterior orbit, as both together have been associated with optic nerve infarct. Bleeding within the orbit should be meticulously controlled with bipolar cautery under direct visualization. Polyanhydroglucuronic acid packs should never be used in the orbit. These are highly acidic and will form rock-hard masses, both of which may have catastrophic impacts on the optic nerve.
Postoperative
Postoperatively, two issues predominate the management of orbital surgical patients: (1) corneal protection and (2) avoidance of optic nerve compression.
As mentioned previously, orbital swelling can be significant after surgeries, and corneal coverage may be compromised with a severely proptotic globe and chemosis. Several options exist for management, including thick, lubricating ophthalmic ointments, petroleum jelly, clear adhesive dressings, and the use of Frost sutures.26 Frost sutures should be used with extreme caution, however, because closing the eyelids removes the important cue of diminishing vision and no longer allows the orbit to decompress itself through proptosis in the face of increasing orbital swelling, providing a set up for orbital compartment syndrome. Using lubricating ointment or a clear adhesive dressing reduces this risk and is easy to apply. In situations where it is difficult to ensure adequate postoperative care or materials, however, suture techniques may be the only suitable option.
Pain and nausea control are essential to diminish the chance of increased orbital venous pressure and resultant hemorrhage within the newly enclosed orbit. That said, administering as little pain medication as is needed is advised, because the onset of significantly greater pain from sudden orbital swelling or hemorrhage may herald serious danger and should be reported to and evaluated by the surgical team.
We routinely ask patients to perform red saturation tests every 2 hours after orbital surgery for 48 hours. Although imperfect, this seems a reasonable compromise between what patients can accomplish and the knowledge that irreversible vision loss may accompany vascular compromise of greater than 90 minutes.
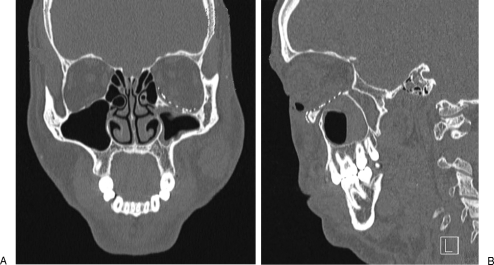
Adequate positioning of materials used in orbital reconstruction can always be a postoperative concern. Placement too far posteriorly can impinge upon the optic nerve and lead to traumatic optic neuropathy. Many orbital surgeons routinely perform postoperative CT scans to ensure adequate reconstructive positioning, but as personal surgical experience with orbital reconstructions increases, such practices often diminish. Nevertheless, if there is ever any question of implant positioning, or when an individual is gaining experience in orbital surgery, a postoperative CT scan is a good idea (Fig. 7).
Figure 7.
(A, B) Surgical management of the orbital floor fracture from Fig. 3 required a lower-eyelid incision and orbital floor reconstruction. Care should be taken not to place implants too far posteriorly, as this may impinge on the optic nerve; however, it is important to make sure that the posterior portion of the implant does not rest within the maxillary sinus, increasing the risk of postoperative enophthalmos.
Complications
As we have discussed, the most important complication for which we must be vigilant is optic neuropathy secondary to implant impingement, hemorrhage, or orbital edema. Extraocular muscle impingement is the second most important complication, as it may not be easily managed secondarily, even with strabismus surgery.
Yet, the most common complications are enophthalmos and ectropion. Increased intraorbital volume is commensurate with the degree of out-fracture of bone fragments into the adjacent sinuses, and when occurring acutely after orbital reconstruction is almost always secondary to inadequate intraorbital volume restoration with implant position or inaccurate fracture reduction. Late-presenting enophthalmos, in contrast, is often due to global orbital fat atrophy from severe concussive injury. In either case, a CT scan should be performed to evaluate the orbital volume and ensure that implant malposition has not occurred. The likelihood of imperfect orbital reconstruction is significantly increased in patients with concomitant areas of trauma and who have more than one orbital wall affected.4 If malpositioned, correction is performed by re-placing the implant into anatomic position. With late-presenting enophthalmos related to fat atrophy, orbital volume can be re-established with onlay alloplastic or autogenous bone grafts. In general, fat atrophy creates both enophthalmos and hypoglobus, and a posterior orbital implant with anterior extension below the globe may be used. If the problem is mostly direct enophthalmos, then an implant positioned in a posterolateral location within the orbit is required.
ORBITAL FLOOR
Lower-eyelid malposition and/or ectropion after lower-eyelid approaches may occur due to scarring of the middle lamella, disruption or laxity of the lateral canthal tendon, and/or tension on the repair caused by excessive anterior lamellar tissue resection or dissection without resuspension. Methods to prevent this complication include meticulous surgical approach, Frost sutures, canthopexy or canthoplasty, and cheek resuspension. The majority of cases resolve with lower-eyelid massage and forced eye closure exercises. In fact, surgical intervention should be reserved for patients with corneal exposure, which is more common in entropion than ectropion. When diplopia is present postoperatively, a CT scan may be performed to rule out entrapment posteriorly by the reconstruction. Delayed release of muscle entrapment is associated with an increased risk of ischemia and fibrosis of the affected rectus muscle and subsequent extraocular gaze restrictions/diplopia. Even in cases where an entrapped inferior rectus muscle was released appropriately, a patient may have diplopia in primary gaze and hypertropia postoperatively, as the weakened inferior rectus muscle is released from its incarceration. In children, this often spontaneously resolves within 9 months. In adults, strabismus surgery is more often required.
Late-presenting proptosis is an uncommon postoperative complication. When it occurs, it has been reported to be caused by either peri-implant inflammation, implant infection, capsular hemorrhage around the implanted material, development of a gelatin film cyst, sinoorbital fistula, intraorbital sinus mucocele, or carotid-cavernous fistula.27
Orbital cellulitis is also a rare complication associated with orbital floor trauma and occurs in ∼0.8% of patients.28 Risk factors include paranasal sinusitis at the time of trauma and nose blowing. However, prophylactic antibiotics have not been shown to decrease the incidence of orbital cellulitis in the immediate posttraumatic period and are generally reserved for clearly identified cases of coexistent sinusitis, especially if corticosteroids are administered.29,30
MEDIAL WALL
Again, the most important complications to watch for are optic nerve and medial rectus muscle impingement by the reconstruction. Other, potential complications after medial wall fracture treatment include failure to recognize and manage telecanthus, tear outflow system disruption, and diplopia or gaze restriction. Small degrees of horizontal dysmotility are often far better tolerated by patients than vertical dysmotilities for two reasons. First, downgaze is far more important for reading, stepping over curbs, and descending stairs than horizontal gaze. If we need to look to the sides, we routinely turn our heads. Second, our fusional amplitude (ability to keep our eyes working together) is far greater in the horizontal axis than in the vertical. We are always bringing our eyes together and apart when we horizontally converge to read and diverge to look at something far in the distance. We don't perform similar tasks in the vertical axis.
LATERAL WALL
Complications associated with lateral wall fractures may occur from inadequate fracture reduction and fixation. Adequate repositioning of the lateral wall is very important in orbital volume determination, as these fractures tend to displace the entire orbitozygomatic complex, resulting in large increases in orbital volume with small changes in positioning. Also, as the fractured segment is truly a tetrapod, inaccurate repositioning along just one axis or meridian is enough to cause a significant increase in orbital volume. Ectropion is also a concern if the lateral canthal tendon is injured and not accurately repaired.
ORBITAL ROOF
As always, the most important postoperative ocular complication of orbital surgery is blindness, which can occur as a result of very high pressures on the globe or optic nerve. Late complications of orbital roof fractures are primarily associated with its proximity to the intracranial cavity and frontal sinus and include the risk of encephalocele, growing skull fractures, mucocele formation, and cerebrospinal fluid leak.31 Other complications associated with orbital roof repair include hematoma, infection, incision- and dissection-related damage to the supraorbital or supratrochlear nerves, injury to the levator palpebrae superioris causing blepharoptosis, and disruption of the trochlea.
Repair of orbital roof fractures sometimes requires detachment of the trochlea, prompting some to attempt to repair the trochlea back to its anatomic position. However, the structure of the trochlea is sufficiently complex, and attempts at primary repair can easily do more harm than good, leading to both vertical and torsional diplopia. Haug et al demonstrated that if trochlea detachment during orbital surgery was required, adequate gaze excursions could be seen postoperatively if the trochlea and periosteum were simply reapproximated without fixation.32
CONCLUSION
Proper management of orbital fractures can be complex, mainly due to the variability of injuries, the proximity of eyes and brain, and the position that the eyes and thus the orbits occupy as the focal point in the middle of the face. Most of the potential important adverse sequelae associated with orbital trauma reconstruction occur as a result of optic neuropathy, ocular dysmotility, ocular injury, or undesirable appearance. Careful attention to a thorough preoperative assessment, individualized surgical plan, honest appreciation of one's own limitations, meticulous attention to surgical technique with a clear understanding of the relevant anatomy, and a thoughtful respect for the local essential structures will, as in most surgery, steer us clear of most complications.
References
- Erdmann D, Follmar K E, Debruijn M, et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008;60:398–403. doi: 10.1097/SAP.0b013e318133a87b. [DOI] [PubMed] [Google Scholar]
- Scherer M, Sullivan W G, Smith D J, Jr, Phillips L G, Robson M C. An analysis of 1,423 facial fractures in 788 patients at an urban trauma center. J Trauma. 1989;29:388–390. doi: 10.1097/00005373-198903000-00020. [DOI] [PubMed] [Google Scholar]
- Kelley P, Crawford M, Higuera S, Hollier L H. Two hundred ninety-four consecutive facial fractures in an urban trauma center: lessons learned. Plast Reconstr Surg. 2005;116:42e–49e. doi: 10.1097/01.prs.0000177687.83247.27. [DOI] [PubMed] [Google Scholar]
- Seider N, Gilboa M, Miller B, Hadar R S, Beiran I. Orbital fractures complicated by late enophthalmos: higher prevalence in patients with multiple trauma. Ophthal Plast Reconstr Surg. 2007;23:115–118. doi: 10.1097/IOP.0b013e318032b30e. [DOI] [PubMed] [Google Scholar]
- Gönül E, Erdoğan E, Taşar M, et al. Penetrating orbitocranial gunshot injuries. Surg Neurol. 2005;63:24–30. discussion 31. doi: 10.1016/j.surneu.2004.05.043. [DOI] [PubMed] [Google Scholar]
- Lane K, Penne R B, Bilyk J R. Evaluation and management of pediatric orbital fractures in a primary care setting. Orbit. 2007;26:183–191. doi: 10.1080/01676830701519374. [DOI] [PubMed] [Google Scholar]
- Exadaktylos A K, Sclabas G M, Smolka K, et al. The value of computed tomographic scanning in the diagnosis and management of orbital fractures associated with head trauma: a prospective, consecutive study at a level I trauma center. J Trauma. 2005;58:336–341. doi: 10.1097/01.ta.0000141874.73520.a6. [DOI] [PubMed] [Google Scholar]
- Lee H J, Jilani M, Frohman L, Baker S. CT of orbital trauma. Emerg Radiol. 2004;10:168–172. doi: 10.1007/s10140-003-0282-7. [DOI] [PubMed] [Google Scholar]
- Mellema P A, Dewan M A, Lee M S, Smith S D, Harrison A R. Incidence of ocular injury in visually asymptomatic orbital fractures. Ophthal Plast Reconstr Surg. 2009;25:306–308. doi: 10.1097/IOP.0b013e3181aa9a73. [DOI] [PubMed] [Google Scholar]
- Steinsapir K D, Goldberg R A. Traumatic optic neuropathy. Surv Ophthalmol. 1994;38:487–518. doi: 10.1016/0039-6257(94)90145-7. [DOI] [PubMed] [Google Scholar]
- Soparkar C NS, Patrinely J R. The eye examination in facial trauma for the plastic surgeon. Plast Reconstr Surg. 2007;120(7, Suppl 2):49S–56S. doi: 10.1097/01.prs.0000260733.61389.0b. [DOI] [PubMed] [Google Scholar]
- Back C PN, McLean N R, Anderson P J, David D J. The conservative management of facial fractures: indications and outcomes. J Plast Reconstr Aesthet Surg. 2007;60:146–151. doi: 10.1016/j.bjps.2006.01.032. [DOI] [PubMed] [Google Scholar]
- Cohen S M, Garrett C G. Pediatric orbital floor fractures: nausea/vomiting as signs of entrapment. Otolaryngol Head Neck Surg. 2003;129:43–47. doi: 10.1016/S0194-59980300487-X. [DOI] [PubMed] [Google Scholar]
- Tahernia A, Erdmann D, Follmar K, Mukundan S, Grimes J, Marcus J R. Clinical implications of orbital volume change in the management of isolated and zygomaticomaxillary complex-associated orbital floor injuries. Plast Reconstr Surg. 2009;123:968–975. doi: 10.1097/PRS.0b013e318199f486. [DOI] [PubMed] [Google Scholar]
- Erdogmus S, Govsa F. The anatomic landmarks of ethmoidal arteries for the surgical approaches. J Craniofac Surg. 2006;17:280–285. doi: 10.1097/00001665-200603000-00014. [DOI] [PubMed] [Google Scholar]
- Kim K S, Kim E S, Hwang J H. Combined transcutaneous transethmoidal/transorbital approach for the treatment of medial orbital blowout fractures. Plast Reconstr Surg. 2006;117:1947–1955. doi: 10.1097/01.prs.0000218330.55731.2d. [DOI] [PubMed] [Google Scholar]
- Chapman V M, Fenton L Z, Gao D, Strain J D. Facial fractures in children: unique patterns of injury observed by computed tomography. J Comput Assist Tomogr. 2009;33:70–72. doi: 10.1097/RCT.0b013e318169bfdc. [DOI] [PubMed] [Google Scholar]
- Haug R H, Sickels J E Van, Jenkins W S. Demographics and treatment options for orbital roof fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:238–246. doi: 10.1067/moe.2002.120975. [DOI] [PubMed] [Google Scholar]
- Fulcher T P, Sullivan T J. Orbital roof fractures: management of ophthalmic complications. Ophthal Plast Reconstr Surg. 2003;19:359–363. doi: 10.1097/01.IOP.0000083646.20672.6B. [DOI] [PubMed] [Google Scholar]
- Raaf J. Posttraumatic cerebrospinal fluid leaks. Arch Surg. 1967;95:648–651. doi: 10.1001/archsurg.1967.01330160118017. [DOI] [PubMed] [Google Scholar]
- Hollier L H, Rogers N, Berzin E, Stal S. Resorbable mesh in the treatment of orbital floor fractures. J Craniofac Surg. 2001;12:242–246. doi: 10.1097/00001665-200105000-00009. [DOI] [PubMed] [Google Scholar]
- Fearon J A, Munro I R, Bruce D A. Observations on the use of rigid fixation for craniofacial deformities in infants and young children. Plast Reconstr Surg. 1995;95:634–637. discussion 638. [PubMed] [Google Scholar]
- Ridgway E B, Chen C, Colakoglu S, Gautam S, Lee B T. The incidence of lower eyelid malposition after facial fracture repair: a retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast Reconstr Surg. 2009;124:1578–1586. doi: 10.1097/PRS.0b013e3181babb3d. [DOI] [PubMed] [Google Scholar]
- Berryhill W E, Rimell F L, Ness J, Marentette L, Haines S J. Fate of rigid fixation in pediatric craniofacial surgery. Otolaryngol Head Neck Surg. 1999;121:269–273. doi: 10.1016/S0194-5998(99)70183-X. [DOI] [PubMed] [Google Scholar]
- Tabrizi R, Ozkan T B, Mohammadinejad C, Minaee N. Orbital floor reconstruction. J Craniofac Surg. 2010;21:1142–1146. doi: 10.1097/SCS.0b013e3181e57241. [DOI] [PubMed] [Google Scholar]
- Sharabi S E, Hatef D A, Hollier L H, Jr, Izaddoost S. Opening eyes to the Frost suture. J Oral Maxillofac Surg. 2010;68:1430–1431. doi: 10.1016/j.joms.2009.06.028. [DOI] [PubMed] [Google Scholar]
- Stewart M G, Patrinely J R, Appling W D, Jordan D R. Late proptosis following orbital floor fracture repair. Arch Otolaryngol Head Neck Surg. 1995;121:649–652. doi: 10.1001/archotol.1995.01890060047009. [DOI] [PubMed] [Google Scholar]
- Ben Simon G J, Bush S, Selva D, McNab A A. Orbital cellulitis: a rare complication after orbital blowout fracture. Ophthalmology. 2005;112:2030–2034. doi: 10.1016/j.ophtha.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Goldfarb M S, Hoffman D S, Rosenberg S. Orbital cellulitis and orbital fractures. Ann Ophthalmol. 1987;19:97–99, 115. [PubMed] [Google Scholar]
- Westfall C T, Shore J W. Isolated fractures of the orbital floor: risk of infection and the role of antibiotic prophylaxis. Ophthalmic Surg. 1991;22:409–411. [PubMed] [Google Scholar]
- Cruz A A, Eichenberger G C. Epidemiology and management of orbital fractures. Curr Opin Ophthalmol. 2004;15:416–421. doi: 10.1097/01.icu.0000136113.56288.87. [DOI] [PubMed] [Google Scholar]
- Haug R H. Management of the trochlea of the superior oblique muscle in the repair of orbital roof trauma. J Oral Maxillofac Surg. 2000;58:602–606. doi: 10.1016/s0278-2391(00)90148-4. [DOI] [PubMed] [Google Scholar]