Abstract
Choosing a pedicled flap to reconstruct an intraoral defect depends on the size and the anatomic position of the tissue defect. The goals are to restore form and function and minimize donor site morbidity. Regional pedicled flaps available for intraoral reconstruction are the buccal fat pad flap, facial artery musculomucosal flap, platysma, pectoralis major, temporalis muscle flap, and trapezius flaps. We give a concise illustration of anatomy, our harvesting technique, indications, and eventual pitfalls for each of the six flaps.
Keywords: Buccal fat pad flap, facial artery musculomucosal flap, intraoral reconstruction, pectoralis major flap, platysma flap, temporalis muscle flap, trapezius flap
The choice of the appropriate regional pedicled flap to reconstruct an intraoral defect is determined by the size and anatomic position of the defect. The aim is to restore form and function, avoiding donor site morbidity as much as possible.
When using a pedicled flap, it is necessary to consider the amount of flap tissue available, and particularly the pivot point of the arc of rotation; in fact, it is the pedicle rotation that influences the final position of the flap. We follow the classification of Mathes and Nahai1 to categorize the different types of vascular anatomy, and we evaluate the extent of the defect as follows:
Small: up to 4 cm maximum diameter.
Medium: up to 7 cm.
Large: more than 7 cm.
The flaps that can be considered for the various anatomic positions are listed in Table 1. We briefly describe the anatomy of the flaps listed, focusing on our harvesting technique, the indications, and the eventual pitfalls. First, we describe the flaps that are already within the oral cavity or close to it, such as the buccal fat pad flap and facial artery musculomucosal flap; these flaps can be used for limited intraoral defects. We then describe the four flaps that are external to the oral cavity: platysma flap, temporalis muscle flap, pectoralis major flap, and the various types of trapezius flaps.
Table 1.
Regional Flap Options Based on Anatomic Position of the Defect
| Anatomic Position | Possible Flap(s) |
|---|---|
| Anterior defects | |
| Lip and anterior vestibulum, upper and/or lower | FAMM, platysma |
| Anterior mandibular arch, between canine teeth | Platysma, FAMM, PM |
| Anterior mouth floor | Platysma, FAMM, PM |
| Lateral defects, upper and/or lower | |
| Lateral vestibulum and lateral alveolar ridge | BFP, FAMM, trapezius |
| Lateral mouth floor | FAMM, PM, lower vertical trapezius |
| Area behind the trigone (retrotrigone) | BFP, TMF, FAMM |
| Hard palate defects | |
| Premaxillae | FAMM, TMF |
| Posterior hard palate | BFP, FAMM, TMF |
| Soft palate defects | |
| Half soft palate | BFP, FAMM, TMF |
| Whole soft palate | TMF |
BFP, buccal fat pad; FAMM, facial artery musculomucosal; PM, pectoralis major; TMF, temporalis muscle flap.
BUCCAL (BICHAT) FAT PAD FLAP2,3,4,5
The buccal fat pad (BFP) is a specialized type of tissue that is distinct from subcutaneous fat. In infants it prevents in-drawing of the cheek during sucking; in adults the BFP enhances intermuscular motion. The BFP lies in the masticatory space between the buccinator muscle medially and the masseter muscle laterally. It separates the muscles of mastication from one another, from the zygomatic arch, and from the ramus of the mandible and is wrapped within a thin fascial envelope. It is thought to serve as a rich venous net, with valve-like structures, possibly involved in exo-/endocranial blood flow through the pterygoid plexus. The landmarks to identify the BFP are the superior buccal sulcus in the molar region and the anterior border of the mandibular ramus.
The BFP consists of a central body and four extensions: buccal, pterygoid, superficial, and deep temporal. The main body is situated deep along the posterior maxilla and upper fibers of the buccinator. The buccal extension lies superficially within the inner side of the cheek. The pterygoid extension lies deep to the medial aspect of the mandibular ramus, located between the origins of the medial and lateral pterygoid muscles and the ramus of the mandible. The deep and superficial temporal extensions reside within the temporal region although they are actually two separate fat pads that are not in continuity. The deep temporal fat pad is in continuity with the buccal fat, passing beneath the zygomatic arch to lie directly on the temporalis and its tendon, separating this muscle from the zygomatic arch. Above the arch, it also passes medially behind the lateral orbital wall and body of the zygoma to rest along the greater wing of the sphenoid. The superficial temporal fat pad is completely enveloped by two layers of the deep temporal fascia and lies between them from the superior orbital rim to their respective insertions along the lateral and medial surfaces of the zygomatic arch. This fat is isolated from the deep temporal extension of the BFP by the interposition of the deep layer of the temporal fascia.
The advantages of this flap are as follows: quick, simple, and easy dissection; can be used under local anesthesia; there are no visible scars; low rate of morbidity; very low failure rate; and it can be associated with other pedicled flaps.
The disadvantages are as follows: it can cover only small-to-medium defects; because of its thinness, it is only suitable for covering, providing no bulk.
The blood supply to the BFP (it has partly an axial pattern) comes from three sources:
Buccal and deep temporal branches (from the maxillary artery).
Transverse facial branch (from the superficial temporal artery).
Small branches from the facial artery.
The average weight of each fat pad is 9.3 g, and its average volume is 9.6 mL. When properly dissected and mobilized, the BFP provides a 6 × 4 × 3 cm pedicled graft. Because much of the BFP does not have a clear pedicle, a clear arc of rotation cannot be defined, thus utmost care is required during insetting of a BFP flap.
Harvesting
The body and the buccal extension (about half the volume of the BFP) are accessible through the mouth. There are three different approaches to the BFP, the choice depending on the defect that has to be closed:
Through a vertical incision slightly lateral to the anterior border of the mandibular ascending ramus.
Through the elevation of a lateral mucoperiosteal flap in the upper molar region and a lateral incision of the periosteum at the level of the vestibular sulcus.
Through a horizontal mucosal incision along the superior vestibular sulcus.
We prefer the horizontal approach:
A horizontal mucosal incision is made along the superior vestibular sulcus in the upper molar region, 5 mm above the second molar, halfway between the gingivobuccal sulcus and Stensen's duct papilla, spreading through the buccinator muscle, and extending 2 cm posteriorly.
Once the loose fascia surrounding the BFP is incised, the BFP becomes immediately visible (Fig. 1).
Gentle pressure on the cheek helps express the fat intraorally.
After the BFP is separated from the surrounding tissues, it is gently pulled out from its bed and positioned in the site of the defect, either by direct rotation or by tunneling under the mucosa.
Finally, the BFP is sutured in place and left uncovered.
To provide immobilization and protection of the flap and pedicle, it is mandatory to use a splint or a bite block for 12 days.
The BFP epithelializes completely in 3 to 4 weeks and by 3 months is covered with healthy mucosa.
Figure 1.
Buccal fat pad (BFP). After a mucosal incision is made along the superior vestibular sulcus in the upper molar region, spreading through the buccinator muscle and loose fascia surrounding the BFP, the BFP becomes immediately visible.
For intraoral malignant defects:
Very often the resection itself exposes the BFP in the mouth. After the incision, the second step is to perform a very careful blunt dissection through the periosteum layer just to allow the BFP to exit from its usual location.
Avoid any kind of suction on the flap because the blood supply can be compromised.
Use gentle traction to get the flap in the right position to cover the defect.
Branches from the internal maxillary artery and superficial temporal artery run into the BFP in a posterior and superior direction and are likely to be preserved. However, the facial artery comes from below and is vulnerable to damage during the resection.
Indications
The BFP flap is capable of covering small to medium defects ∼5 cm in diameter.
Oro-antral fistula.
Palatal cleft defect.
Covering exposed bony or mucosal defects within the alveolar crest and maxilla, soft and hard palate, retromolar region of the mandible, anterior tonsillar pilar, superior buccal sulcus.
Pitfalls
Because the blood supply is precarious and there is no signal pedicle, the arc of rotation of the BFP must be minimized, and the inset must be without any tension.
It is very important to preserve the thin capsule overlying the BFP so that the small blood vessels are not damaged.
Avoid suction on the BFP.
Minimal trismus is possible due to intraoral scarring.
In patients who have undergone neck dissection or extensive radiation therapy to the head and neck, take care to assess the blood supply and viability of the BFP intraoperatively.
Cheek contour and aesthetic malar projection may be altered when using this flap.
To immobilize and protect the flap, a splint or bite block should be used for 12 days.
Make it clear to the patient that she or he will need a nasogastric tube for feeding during that period.
FACIAL ARTERY MUSCULOMUCOSAL FLAP6,7,8
In 1992, Pribaz described an axial musculomucosal flap based on the facial artery, combining the principles of the nasolabial and buccal mucosal flaps. He designated the flap the facial artery musculomucosal (FAMM) flap.
The FAMM flap is designed just anterior to Stenson's duct and consists of mucosa, submucosa, a small amount of buccinator muscle, the facial artery, and a rich venous plexus. The feeding vessel of FAMM donor area is the facial artery as it courses through the cheek, lateral to the buccinator muscle, but medial to most of the muscles of facial expression. The facial artery, a branch of the external carotid artery, enters the face by hooking around the lower border of the mandible at the anterior edge of the masseter muscle. It follows a tortuous course, giving off several branches to the buccinator muscle at the superior border of the mandible, before giving off the inferior labial artery. The facial artery crosses the superior border of the mandible at a mean distance of 6.5 cm from the midline and then passes upwards and forward to a point 1.38 cm (range, 1 to 1.6 cm) lateral to the commissure of the mouth, where it lies deep to the risorius zygomaticus major muscle and superficial lamina of the orbicularis oris. The facial artery lies superficial to the buccinator, the levator anguli oris muscle, and the lateral edge of the deep lamina of the orbicularis oris muscle. It has a variable relationship to the levator labii superioris alaeque nasi muscle. At this point, the facial artery gives off several perforators to the cheek, the superior labial artery, and continues as the angular artery, reaching the medial canthus. The FAMM flap has an excellent venous outflow based on a rich venous submucosal plexus that allows the mobility of the flap without venous congestion.
Harvesting
The FAMM flap can be based superiorly (retrograde flow) or inferiorly (anterograde flow). Its average size is 2.5 × 7 cm. The pivot point of the arc of rotation of the FAMM flap pedicle is at the lower retromolar trigone if it is inferiorly based (anterograde flow) or at the level of the upper gingival sulcus, close to the level of the alar margin of the nose if it is superiorly based (retrograde flow).
The design of the flap must be centered over the facial artery in a boomerang design—an oblique orientation—from the retromolar trigone to the level of the ipsilateral gingival sulcus at the level of the alar margin. It is positioned anterior to Stenson's duct.
Retraction stitches (2-0) are placed along the ipsilateral upper and lower lips and commissure to gain better access to the FAMM donor area.
The course of the facial artery is outlined intraorally using Doppler ultrasound.
The dissection starts at the distal end of the flap, with an incision through the mucosa and buccinator muscle.
The most distal end of the facial artery is identified, ligated, and cut, and the rest of the flap is incised.
The dissection proceeds just deep to the facial vessels, taking only a minimum of the overlying buccinator and orbicularis muscles near the oral commissure.
It is mandatory that the facial artery be raised with the flap so that the entire flap is axial. However, the facial vein is never taken with the flap. Venous drainage depends on the buccinator venous plexus.
The pivot point of the pedicle depends on the orientation of the pedicle itself: anterograde or retrograde.
The FAMM flap can be rotated 180 degrees and transposed across the retromolar area, passed over the mandibular/maxillary alveolus through edentulous spaces, or tunneled through the gingivobuccal sulcus to reach the nasal antra.
A two-layered closure of the donor defect is performed, approximating the buccinator muscle and mucosa, taking care to avoid the opening of Stenson's duct.
The patient is immobilized with a bite block for 10 days to protect the flap.
Indications
The FAMM flap can repair defects up to 3 cm wide.
When based superiorly (retrograde flow), the FAMM flap can be used to close mucosal defects in the anterior hard palate, alveolus, maxillary antrum, nasal floor and septum, upper lip, sulcus, and vermilion.
When based inferiorly (anterograde flow), the flap can close defects in the posterior hard palate, soft palate, tonsil fossa, alveolus, floor of the mouth, cheek, and lower lip.
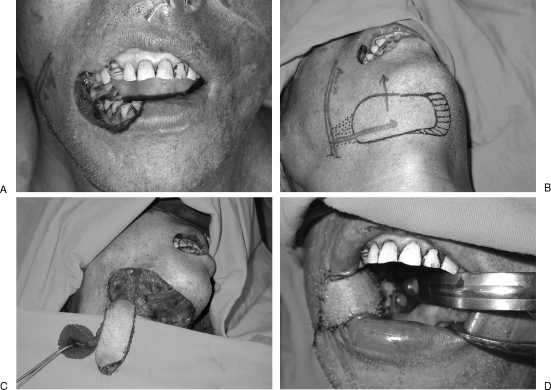
Figure 2 illustrates the use of a FAMM flap for oral lining in the reconstruction of an oro-antral fistula using a local rotation flap for antral lining.
Figure 2.
Oro-antral fistula reconstructed with local rotation flap for antral lining and facial artery musculomucosal (FAMM) flap for oral lining. The patient is a 43-year-old woman who had previously undergone a right partial maxillectomy and reconstruction. Attempted closure had been performed on three occasions without success. (A) View from below demonstrating the presence of an oro-antral fistula. The FAMM flap has been elevated. (B) After marking the course of the facial artery with a hand-held Doppler, the FAMM flap is marked, with the facial artery in the center of the flap. As the FAMM flap in this case is used to reconstruct a defect in the maxillary region, the flap is pedicled on the blood supply coming from the superior aspect of the flap. The inferior incision is performed first, and the facial artery and vein are located and ligated. After gentle tugging on the vessels, the surgeon can confirm the location of the vessels and re-mark if necessary. The flap is elevated from distal to proximal below the plane of the vessels. (C) FAMM flap after complete isolation of the pedicle and elevation. (D) Local random pattern flaps were used to line the antral side of the defect. The FAMM flap is inset into the defect and used to obliterate the dead space and line the oral side of the fistula.
Pitfalls
This flap is an axial flap and must follow the serpiginous course of the facial artery.
Resist the temptation to make the pedicle longer and inset the FAMM flap without any tension.
The facial artery has a tortuous course with serpentine coils, which may be carefully released to gain additional pedicle length (∼4 cm).
The rich vascularity of the FAMM flap supports a length:width ratio of 5:1; however, flaps >3 cm will create cheek tethering, which will likely require a Z-plasty to release cheek contracture.
A bite block should be used for 10 days to prevent injury to the pedicle if it crosses over molar teeth.
When suturing the donor site, pay attention to Stenson's duct.
PLATYSMA FLAP9,10,11,12
The platysma is a bilateral, thin, broad muscle investing the anteromedial aspects of the neck. It drapes the neck just under the subcutaneous layer. It is enclosed by the superficial cervical fascia, which splits into a superficial layer and a deep layer. It has a broad origin from the fascia over the upper parts of the pectoralis major and deltoid muscles; its fibers course diagonally, upwards and medially, along the sides of the neck, to insert in the lower face skin and subcutaneous tissue. The platysma adheres to the anterior neck skin. In the submental region, the platysma fibers from each side of the neck interweave. Above the mandible, the platysma joins the superficial muscular aponeurotic system.
The pattern of circulation of platysma muscle is type II. The dominant pedicle is represented by the submental artery with venae comitantes. The submental artery is a branch of the facial artery that gives off the submental branch at the level of the insertion of the posterior belly of the digastric muscle to the hyoid bone. The submental artery runs over the mylohyoid muscle just below the angle of the mandible, then passes the medial aspect of the submandibular gland. The submental artery is deep to the anterior belly of the digastric muscle in 70% of cases.
The minor blood supply is a branch of the suprasternal artery, which receives its blood supply from the suprascapular artery and vein. The motor nerve supply is by a cervical branch of the facial nerve that enters in contact with the muscle fibers from below. The sensory innervation is by the transverse cervical nerve.
There are two kinds of flap based on the platysma muscle: the submental flap and the island platysma flap.
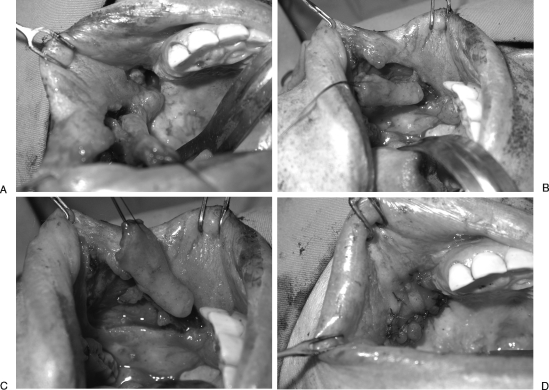
Submental Flap (Fig. 3)
Figure 3.
Submental flap used for reconstruction of lower lip and buccal defect. The patient underwent resection of an oral cancer involving the lower lip and buccal mucosa. Reconstruction was performed with a submental island flap. (A) Marking of the submental flap. (B) Marking of the submental flap and the course of the axial blood supply to the flap. The artery is marked after locating its course using a hand-held Doppler. (C) Submental flap after elevation. The instrument is pointing to the contralateral vein, which can be anastomosed at the recipient site if venous congestion is apparent. (D) Submental flap after inset for reconstruction of lower lip and buccal defect. Part of the flap can be excised in future procedures by advancing an upper and lower lip vermilion flap. (Parts B and C from Yazar S, Chen H-C, Mardini S. Augmentation of venous drainage by a venous anastomosis for pedicled flaps. Journal of Reconstructive Microsurgery 2008;24:369–376. Reprinted by permission.)
The submental flap is designed across the midline over the submental area: the upper limit is just under the mandibular arch in the midline; the lateral limits are marked below the mandibular angles, bilaterally. The inferior limits depend on the redundant tissue available to allow primary closure. The area of a submental flap is between 5 cm × 5 cm minimum, even in younger patients, and 7 cm wide × 12 cm long maximum. The arc of rotation of the submental flap pedicle has its pivot point at the level of the angle of the mandible.
Island Platysma Flap
The island platysma flap is placed over the distal insertion of the sternocleidomastoid muscle, in a hairless area. The size of an island platysma flap can be 5 cm wide × 7 cm long maximum. The arc of rotation of the island platysma flap pedicle has its pivot point at the level of the inferior border of the mandible.
Indications
Platysma-based flaps can be used as muscle or as musculocutaneous flaps. Based on the dominant pedicle, the entire muscle can be elevated.
The submental flap can easily reach the chin and lower lip area, the commissure, and even the posterior part of the oral cavity. It can be used to reconstruct through-and-through defects of the cheek.
The main indications for use of an island platysma flap are defects of the alveolar ridge, floor of the mouth, cheek, retromolar trigone, commissure, and lining of the lower lip.
Harvesting
KEY POINTS FOR HARVESTING BOTH TYPES OF PLATYSMA FLAPS
The pedicle is based on the submental artery and release of the muscle from the surrounding tissues. The first step is to identify the limits of the platysma in the anterolateral part of the neck: the anterior and posterior borders of the muscle are identified in the awake, grimacing patient. The mandible and clavicle represent the upper and lower extent of the muscle, respectively.
SUBMENTAL FLAP
The inferior border of the skin paddle is incised, with the platysma muscle included.
Once the submandibular gland is reached, the dissection must be close to the gland, ligating each branch coming from the submental artery. It is necessary to proceed up to the upper-third of the gland. It is then possible to see the facial vessels clearly.
Care must be paid to identify the marginal branch of the facial nerve in the subplatysma fatty layer before proceeding to dissect. Staying close to the posterior (deep) aspect of the platysma prevents any injury to the nerve.
The upper incision is made through the platysma muscle. The flap is raised from the contralateral side to the ipsilateral pedicled side. The contralateral anterior belly of the digastric muscle is left deep, but the platysma muscle is taken with the flap. At this point, the contralateral submental artery and submental vein are ligated.
Depending on the arc of rotation required, the ipsilateral anterior belly of the digastric muscle may be detached from the hyoid bone and included in the flap.
Dissection of the vessels is then completed to obtain the maximal pedicle length: The facial artery and the submandibular and facial veins are identified and dissected to their origin. Further pedicle length can be obtained according to Martin's description.10
Primary closure of the donor site is made with the patient's neck in extension to avoid hypertrophic scarring. The cervical area is undermined, mainly on the midline, and sutured to the hyoid bone to reconstruct an appropriate cervicomental angle. The scar is hidden behind and below the mandibular arch, without any eversion of the lower lip; skin undermining is allowed only on the neck side to obtain this latter aesthetic and functional goal.
Drains are placed in the neck.
Figure 3 illustrates the use of a submental flap to reconstruct a lower lip and buccal defect.
ISLAND PLATYSMA FLAP
An elliptical island, measuring 5 × 7 cm maximum, is planned over the distal insertion of the sternocleidomastoid muscle, in a hairless area.
Flap harvesting should be performed before tumor resection and neck dissection to avoid injury to the blood supply to the flap.
The platysma and sternocleidomastoid fascia are entered just below the lower margin of the skin ellipse. The muscle attachments to the clavicle must be detached.
The dissection starts at the clavicle level and continues in a subplatysmal plane.
Proximally, the incision is made through the skin only, and the dissection continues over the platysma.
Care must be taken to preserve the external jugular vein and to include that vein in the flap. Sensory nerves are identified and cut.
The upper border of the platysma has to be elevated very carefully, close to the mandible, at the level of the facial artery; the facial vessels and the marginal branch of the facial nerve must be preserved.
At this point, the neck dissection and the tumor excision are performed, saving the facial vessels.
The flap is passed superiorly in a subcutaneous tunnel between the mandible and the cervical skin; through this tunnel the flap can reach the oral cavity or the inner aspect of the cheek. The tunnel has to be large enough to avoid any compression of the pedicle.
Pitfalls
Although there are many cases reported in the literature of the use of platysma flaps in the setting of cancer, we typically use this flap for traumatic cases and benign tumors because the blood supply to the flap is within a lymph node area.
The marginal branch of the facial nerve must always be identified and saved.
In cases of malignant tumors, the contraindications are preoperative radiation, prior neck dissection, ligation of the facial artery, and ipsilateral facial nerve paralysis.
Venous drainage is a key variable; in fact, the facial veins are more prone than the artery to be damaged, even by minor trauma.
The tunnel for the vascular pedicle has to be large enough to prevent any compression.
SUBMENTAL FLAP
Care should be taken not to injure the marginal branch of the mandibular nerve, especially when the dissection starts by incision of the upper part of the skin paddle.
Patients should be aware of intraoral hair.
Take care during the dissection to include the ipsilateral anterior belly of the digastric muscle to improve the blood supply to the contralateral side.
ISLAND PLATYSMA FLAP
For floor of mouth: Only a small defect can be reconstructed using the island platysma flap; preserve the mylohyoid muscle.
For cheek reconstruction: Large through-and-through defects require the use of a different, thicker flap. The island platysma flap is a good option if the resection involves only the mucosa.
For lip reconstruction: The island platysma flap can be used in combination with a pedicled or free flap to provide the inner lining of the lip.
Flap elevation should be performed before tumor ablation and neck dissection to avoid injuries to the pedicle. This requirement is an important limitation because the skin paddle must be designed before tumor removal, not after. Thus, as a result, the flap might not be large enough.
Venous congestion often occurs and can cause marginal necrosis of the flap.
TEMPORALIS MUSCLE FLAP13,14
The temporalis muscle is a fan-shaped muscle on the lateral skull, filling the entire temporal fossa. It passes under the zygomatic arch to insert onto the coronoid process and the anterior aspect of the ramus of the mandible.
The temporalis muscle flap (TMF) has a type III pattern of circulation. The dominant pedicles are the anterior deep and posterior deep temporal arteries and venae comitantes. Both arteries arise from the internal maxillary artery, which is a branch of the external carotid artery. The artery enters the muscle at its undersurface, deep to the zygomatic arch. It should be kept in mind that the internal maxillary artery courses deep and close to the coronoid process of the mandible.
An additional minor pedicle comes from the superficial temporal vessel, through the middle temporal artery and venae comitantes. This additional pedicle has to be cut.
The TMF is mainly elevated as a muscle flap because the musculocutaneous flap leaves an unacceptable donor area in the hair-bearing scalp. Its size averages 10 × 20 cm. The maximum arc of rotation of the TMF pedicle has its pivot point at the level of the origin of the deep temporal vessels (considered as one pedicle) from the internal maxillary artery.
Harvesting
A coronal or hemicoronal incision is made through the scalp from the midportion of the superior auricular helix to ∼2 cm above the superior temporal line. The dissection is carefully maintained in the subgaleal layer to expose the superficial temporalis fascia.
The superficial temporalis fascia in incised, maintaining the dissection just above the deep temporalis fascia.
The skin and superficial facial incision can be extended into the preauricular crease to expose the superficial temporal vessels. Preservation of the vascular pedicle to the temporoparietal fascia allows this fascia to be elevated as a separate pedicled flap.
The deep temporal fascia is exposed by elevating scalp flaps ∼6 cm anteriorly and posteriorly.
To mobilize the TMF, an incision is made into the deep temporalis fascia, starting from its outer margin and proceeding along the superior border of the zygomatic arch.
Incisions are then made in the attachments of the temporalis muscle at the inferior temporal line, at the lateral margin of the orbit, and at the superior temporal crest.
Subperiosteal elevation of the TMF is mandatory to avoid damaging the blood supply.
At this point, the TMF, supplied by the deep temporal vessels, is free and can be moved to the recipient site.
The zygomatic arch is not an obstacle: Osteotomy of the zygomatic arch can be avoided in almost all cases. The muscle is pulled under an intact arch by means of three sutures passed through the anterior, cranial, and middle parts of the muscle. The surgeon gently pulls the sutures one by one in a clockwise movement: The anterior suture is the first to pass under the zygomatic arch while a gentle pressure is maintained on the muscle.
To obtain the greatest arc of rotation, an osteotomy of the mandible at the base of the coronoid process can be performed, paying careful attention to the fact that the TMF pedicle lies just medial to the coronoid process.
The TMF is transposed via a tunnel in the infratemporal fossa, with the fascia facing the oral cavity.
At the donor site, we reconstruct the temporal fossa with an alloplastic material (porous polyethylene; MEDPOR; Porex Surgical, Inc., College Park, GA) with a suction drain. This porous polyethylene is available in temporal fossa–shaped sheets, in various sizes, which readily fit the donor site.
If just the anterior part of the TMF is transposed, the remaining muscle will be moved forward, producing a good cosmetic camouflage.
Indications
Defects of the ipsilateral maxilla and palate; the lateral oropharyngeal wall; anterior to the pharyngeal tonsil; the retromolar area.
In cases of total maxillectomy, a free flap is the best choice; however, in an elderly patient with poor health status, a double TMF can close this large defect.
A TMF can be used to fill a residual clef palate defect; however, it is difficult to pass the bulky muscle through the posterior maxillary wall.
Pitfalls
It must be checked that previous surgery has not jeopardized the vascular supply. The pedicle is on the undersurface of the TMF, arising from the internal maxillary artery, behind the coronoid process of the mandible. Thus, the surgeon has to be careful during coronoid osteotomy.
To avoid injury to the facial nerve, keep in mind that the frontal branch is located deep to the superficial temporal fascia, so keep the dissection plane close to the deep temporal fascia, and also keep in mind that the frontal branch crosses from above the zygomatic arch, around 2 cm lateral to the external eyelid canthus, so keep the dissection plane deep to the periosteum of the arch.
Use TMF for only one area of defect (e.g., for filling an orbit after exenteration or for maxillae after maxillectomy). If it is used for both orbit and maxilla, it may fill the space initially, but postoperative retraction will give a terrible sunken effect to the reconstructed parts.
Fibrosis can occur, especially in reconstruction of the retromolar area, which may lead to trismus. Adequate physiotherapy can prevent this complication.
When TMF is used in skull-base surgery, eventual cerebral fluid leakage is of concern; thus, we insert a no-suction drain such as a Penrose type or a closed drain without any suction force.
PECTORALIS MAJOR MUSCLE FLAP15,16,17
The pectoralis major (PM) is a fan-shaped unipennate muscle located on the superficial chest wall, where it lies beneath the subcutaneous fat layer. The muscle can be separated into a clavicular portion and a sternocostal portion. The clavicular portion originates from the medial half of the clavicle. The sternocostal portion originates from the anterior surface of the sternum, at the second to sixth costal cartilages, and at the aponeurosis of the external oblique muscle. The PM inserts, with one tendon, into the crest of the great tuberosity of the humerus. The clavicular, superior fibers are horizontal, whereas the inferior, sternocostal fibers are oblique. Hence, the inferior fibers can be split, whereas the superior fibers, particularly those attached to the humerus, require transection.
The pattern of circulation1 is type V. The dominant blood supply is the pectoral branch of the thoracoacromial artery and its venae comitantes. Minor pedicles are from the lateral thoracic artery, and perforators are from the internal mammary artery and from the fifth to seventh intercostal arteries. The pectoral branch runs a cephalocaudal course on the deep surface of the PM.
The motor nerve supply consists of a lateral and a medial pectoral nerve from the brachial plexus. These nerves enter the muscle near the axilla under the horizontal fibers of the muscle and can be visualized between the pectoralis minor and PM muscles. The size of the PM flap averages 15 × 23 cm. The arc of rotation of the pedicle has its pivot point at the level just below the clavicle.
Harvesting
Mark the clavicle, the lateral border of sternum, and the approximate course of the dominant vascular pedicle (line connecting the acromion to the xiphoid process). The parasternal perforators to the deltopectoral flap should also be marked. The skin paddle is marked over the caudal medial portion of the chest wall.
Make an incision down to the muscle fascia, at the lateral border of the skin paddle. Wide undermining of the skin of the lateral chest wall is performed. This allows the dimensions of the muscle to be evaluated. A sterile Doppler probe may be of help in verifying the position of the main pedicle. If the incision is close to the lateral margin of the PM, this lateral margin is elevated deep to a plane along the anterior surface of the pectoralis minor muscle. Otherwise, the PM is split along its fibers, with the certainty that the pectoral artery is medial to this line of separation. It is mandatory to identify the vascular pedicle on the undersurface of the PM.
Completion of the circumferential incision around the skin paddle, down to the muscle, allows complete exposure of whole PM. The skin edges are tacked to the immediate underlying PM to prevent separation of the skin from the muscle.
The PM is elevated off the chest wall by blunt and sharp dissection. The deep plane of dissection is above the pectoralis minor and intercostal muscles. The plane between the PM and the pectoralis minor is avascular. The intercostal perforators, which enter the deep surface of the PM, should be clipped or tied. The main pedicle of the PM is kept in view during the entire dissection, taking care to preserve the fascia on the deep side with the muscle. The pectoral artery lies within this fascia.
The attachments of the PM to the rectus fascia and the sternum are then divided up to the level of the clavicle. Save the large perforators from the internal mammary artery in the second and third intercostal spaces in case there is a need for an ipsilateral deltopectoral flap. The reflected PM flap shows the pectoral artery and vein.
One of the pectoral nerves lateral to the pedicle can be transected to achieve additional mobilization of the muscle.
The horizontal fibers of the PM, which are attached to the humerus and form the anterior fold of the axilla, can be transected, if deemed possible. Otherwise, the PM is transected more medially, closer to the pectoral artery. Good hemostasis is mandatory while the lateral portion of the PM is transected as this is the most common location for postoperative bleeding.
A tunnel is created for passage of the PM into the neck, over the clavicle. Adequate undermining must be obtained to prevent compression of the vascular pedicle. The tunnel should easily fit four fingers breadth.
If additional length is required, the medial half of the clavicle can be resected; this minimizes compression of the vascular pedicle on the clavicle.
Donor site closure is obtained by wide undermining of the chest wall skin. Suction drains are used to prevent seroma and hematoma.
Indications
This flap can be used as a muscle flap or a musculocutaneous flap.
It is ideally suited to reconstruct or serve as a replacement for pathology surrounding the tracheostoma.
For intraoral defects, it can be considered for large defects at the anterior and lateral floor of the mouth, tongue, or cheek area. In the latter case, the defect should not extend more cephalad than the maxillary teeth line. We consider first a free flap and then switch to a PM flap in the case of real poor health status of the patient or after the failure of a free flap.
Soft tissue defect of the neck resulting from previous radical dissection, with the subsequent danger of exposure of the great vessels.
Pitfalls
Do not resurface defects more cephalad than the oral floor, or the cheek area. A more cephalad defect requires that the skin paddle of the PM is extended caudally, over the rectus muscle sheath, but the blood circulation over the rectus sheath is not reliable, resulting in high rates of partial flap failure.
To avoid any compression or twisting of the pedicle, it must be remembered that the pivot point of the vascular pedicle is below the clavicle.
Excessive bulk may be troublesome in terms of functionality and wound healing. Avoid a PM flap in obese patients, especially a myocutaneous PM flap.
Pedicle compression can result from external causes, such as tracheostomy tapes or circumferential dressing; the veins are especially vulnerable.
Postoperative neck contracture and scarring can be problematic.
TRAPEZIUS FLAP18,19,20
The trapezius is a large, flat muscle located at the superior aspect of the posterior trunk, lying just underneath the skin and subcutaneous fat. It has a triangular shape with attachments to the base of the skull, lateral shoulder, and inferior thoracic vertebral column. The trapezius flap (TF) has a superficial relationship to the levator scapulae at its superior edge and the rhomboid minor and major muscles in its midportion. Inferiorly, the TF extends over the superior edge of the latissimus dorsi muscle. It is medial to the latissimus dorsi muscle and lateral to the spine.
The function of the TF is to raise the lateral angle of the scapula, which is important for adduction of the arm. It originates from the external occipital protuberance, the medial third of the superior nuchal line of the occipital bone, the ligamentum nuchae, the spinous processes of the seventh cervical vertebra, and all 12 thoracic vertebrae.
The trapezius has three separate portions in terms of insertion and function:
Superior portion: inserts onto the lateral third of the clavicle.
Middle portion: inserts onto the spine of the scapula.
Inferior portion: inserts onto the acromion.
The vascular pattern of the trapezius is generally classified as type II (dominant pedicle: the transverse cervical artery [TCA] and vein); however, the blood supply is confusing because of variations in the origin of the TCA and the dorsal scapular artery (DSA). Of note, Haas19 proposed to include the TF among the type V muscle flaps.
According to Mathes and Nahai's classification,1 the dominant pedicle is the TCA and vein (the transverse cervical vessels), which exit the posterior triangle superficial to the levator scapulae, and mostly arise from the thyrocervical trunk (80%) or from the subclavian artery and vein (20%).
The minor pedicles, according to type II classification, are several:
The DSA, which is usually a branch of the subclavian artery or, occasionally, a deep branch of the TCA. The DSA supplies the caudal portion of the trapezius muscle, emerging between the major and minor rhomboid muscles or, less commonly, between the rhomboid minor and the levator scapulae.
The branches from the occipital artery and vein, from the external carotid artery and vein. These vessels are close to the origin of the trapezius at the external occipital protuberance.
The perforating posterior intercostals arteries and veins, so-called paraspinous perforators, coming from the descending aorta and vena cava. These vessels enter the trapezius along the posterior midline, adjacent to the cervical and thoracic vertebral bodies.
The nerve supply is provided by the spinal accessory nerve (11th cranial nerve); sensory branches come from the third and fourth cervical nerves and the posterior cutaneous branches of intercostal nerves.
The TF can be based on:
The paraspinous perforators of the lower cervical region: the superior trapezius flap.
The TCA: the lateral island trapezius flap.
The DSA: the vertical trapezius flap.
Thus, it is possible to harvest three different flaps, which have different sizes and different arcs of rotation of their pedicles. The size of the entire trapezius muscle is 34 × 18 cm. The superior TF has its arc of rotation at the lower cervical region of the spine. The flap is designed on the trapezius, but the distal portion of the skin paddle may safely extend 8 to 10 cm beyond the acromion process. To achieve direct closure of the donor site, the flap width depends upon the redundancy of the tissue. The donor site is often closed with a skin graft.
The lateral island TF has its arc of rotation at the posterior border of the sternocleidomastoid muscle, which is the anterior border of the posterior triangle of the neck. The flap is usually ∼4 × 6 cm, but the dimensions are typically limited by the redundancy of the tissue that would permit primary closure of the defect.
The vertical TF has the largest arc of rotation. In fact, the DSA and vein can be followed beneath the rhomboid minor muscle up to the levator scapulae muscle at the posterior neck. The flap can have a size of up to 8 × 15 cm.
Indications
SUPERIOR TF
The superior TF is unique among the TFs in that its blood supply is unaffected by a prior radical neck dissection with transection of the transverse cervical (TC) vessels. Moreover, the superior TF is superiorly based; thus the gravity force does not pull the flap away from the recipient site as readily as when other regional flaps are used.
This flap is a reliable source of coverage for defects of the posterolateral portion of the neck that extend no further medially than the midline. For oral reconstruction, it can reach the posterior part of the mouth floor or the posterior part of the cheek.
For difficult wounds, the flap can be inserted along its entire path to the site of the defect, and the intervening skin can be excised. The poor aesthetic result of wrapping this flap around the neck is compensated by the increased chances of successful wound healing.
LATERAL ISLAND TF
The lateral island TF is the least reliable of the three musculocutaneous flaps because its arc of rotation is dependent on favorable anatomy and meticulous mobilization of the TC vessels. The lateral island flap can reconstruct defects of the pharynx and of the lateral part of the oral cavity, although its primary use is for external defects of the lateral and anterior neck.
VERTICAL TF
The vertical TF is a thin pliable musculocutaneous flap, with a very long constant pedicle and minor donor site morbidity, permitting a safe flap elevation and also the possibility of free tissue transfer.
The tremendous arc of rotation of the pedicle of the vertical TF makes it the most versatile of the three trapezius musculocutaneous flaps; it can reach the lateral skull.
For intraoral reconstruction, the vertical TF can be used for tumors in the retrotrigone or oropharynx region.
Harvesting
SUPERIOR TF
The flap is outlined over the upper portion of the trapezius muscle with the anterior incision of the flap made along the anterior border of the trapezius muscle. The posterior border of the flap is a transverse incision parallel to the anterior incision (the width of the flap is determined in part by the width of the defect and by the necessity of incorporating several perforators).
The posterior incision is made through the skin and the trapezius muscle. The firm attachments of the trapezius to the spine of the scapula must be incised to maintain the proper depth of dissection. Ligate and transect the TCA and vein. The correct plane of dissection is between the trapezius and the supraspinatus muscle.
In the medial aspect of dissection, the trapezius is elevated off the levator scapulae and the rhomboid minor.
The distal portion of the skin paddle may extend several centimeters beyond the acromion process. It is elevated along a plane just superficial to the deltoid fascia.
Reaching the lateral aspect of the trapezius muscle, the plane of the dissection is deepened to incorporate that muscle.
The flap is then rotated. Closure of the donor site is achieved by wide undermining. In most cases, a skin graft is needed to cover the wound.
Usually, a “dog-ear” deformity is present, below the auricle.
The second-stage transection of the muscle can be performed in ∼3 weeks. It is at this time that correction of the “dog-ear” deformity can be addressed.
LATERAL ISLAND TF
Outline an island of skin overlying the lateral aspect of the cephalad portion of the trapezius muscle, where it inserts into the clavicle and the acromion process of the scapula.
The anterior border of the trapezius muscle is marked at its insertion on the distal third of the clavicle.
The dimensions of the flap are limited by the redundancy of the tissue in this region, which permits primary closure of the defect.
Incising through the anterior skin incision displays the inferior aspect of the posterior triangle. The supraclavicular fossa is carefully dissected to identify the TC vessels.
The anterior border of the trapezius is identified as well as the posterior belly of the omohyoid muscle. The TCA runs along the floor of the posterior triangle.
The incisions are made around the skin paddle, after the anatomy of these vessels has been determined and it is certain that TC vessels are not intertwined with the roots of the brachial plexus.
After the skin paddle is outlined, the incisions are made circumferentially through the skin, subcutaneous tissue, and trapezius muscle.
Distal ligation of the TCA and vein, as they descend along the caudal aspect of the muscle, must be accomplished when the distal incision through the flap is made.
Complete the transposition of the flap to the recipient site. Greater mobilization of the flap can be achieved by dissection along the vessels in the medial aspect of the posterior triangle.
Wide undermining followed by layered closure is required to manage the donor site defect.
VERTICAL TF
With the patient sitting, identify the margins of latissimus dorsi and trapezius muscles and medial border of the scapula. It is difficult to mark the DSA preoperatively using Doppler because of the partial overlying scapula and because the DSA could be confused with the superficial branch of the TCA.
Design the skin island between the medial border of the scapula and the spine: One third of the skin island must be over the trapezius closer to the spine and should not extend more than 7 cm distal to the inferior angle of the scapula.
Place the patient in the lateral decubitus position.
An incision is made from the posterior base of the neck to the cephalad margin of the skin island. The incision is carried down to the level of the trapezius muscle.
The incision is then made along the lateral edges of the skin paddle. The superficial surface of the trapezius muscle is identified all around the skin paddle.
The lateral border of the muscle is elevated off the rhomboid muscles. Then, the muscle attachments to the midline vertebrae are transected to mobilize the muscle distally to proximally.
The paraspinous perforators must be ligated.
The trapezius muscle is elevated when the course of the DSA can be seen.
An incision is then made along the medial border of the scapula, and the flap is elevated by cutting the muscle fibers and following straight along the pedicle vessels.
At the junction of the rhomboid major and minor, the dorsal scapular (DS) vessels are identified as they enter the undersurface of the trapezius muscle. The descending branch of the DSA, which runs deep to the major rhomboid muscle, has to be divided.
The minor rhomboid muscle is divided, preserving a cuff of this muscle around the pedicle.
From this point the pedicle, which consists of the artery and always two veins, can be prepared under the superior angle of the scapula.
The flap could be transferred through a subcutaneous tunnel to the recipient site, or the dissection can continue under the levator scapulae muscle to the lateral neck region. In so doing, the arc of rotation of the pedicle is ∼5 to 7 cm wider.
With more proximal dissection, the TC vessels are identified on the undersurface of the trapezius muscle (Fig. 4). Preservation of both pedicle and DS and TC vessels can be accomplished to ensure maximal nourishment to the flap, depending on the location of the recipient defect. The arc of rotation can be improved even further by transecting the DSA. Before doing this, a temporary microvascular clamp must be applied to the DSA, and this maneuver should demonstrate that the nourishment from the TCA is enough for the muscle and the skin paddle.
The second-stage transection of the muscle should be performed in ∼3 weeks.
Figure 4.
Vertical trapezius flap (TF). Raised skin island between the medial border of the scapula and the spine. One third of the skin island must be over the trapezius closer to the spine and should not be extended more than 7 cm distal to the inferior angle of the scapula. The TC vessels are identified on the undersurface of the trapezius muscle.
Pitfalls
SUPERIOR TF
Its limited arc of rotation has to be respected: The rotation can be improved only slightly by extending the incision across the midline in a cephalad direction.
The extent of the defect does not cross the midline anteriorly.
LATERAL ISLAND TF
Preliminary exploration of the posterior triangle of the neck is essential to assess the suitability of these TC vessels.
The likelihood of the TC vessels being present after radical neck dissection is small, but this flap should not be selected in such patients.
Careful exploration of the posterior triangle should ensure that the anatomy of the TC vessels is favorable. Failure to identify and isolate both artery and vein will lead to failure.
Particular attention should be paid to preserving the TC vein, which may be in jeopardy because of its course superficial to the posterior belly of the omohyoid muscle and its entry into the external jugular vein.
VERTICAL TF
Previous radical neck dissection or radiation therapy could have divided or injured the branches of the TCA, as well as the DSA. Some authors therefore advocate preoperative arteriography to confirm the patency of the DSA. In any case, we believe that it is prudent to harvest the vertical TF contralateral to the side of a prior neck dissection.
One third of the skin island must be over the trapezius muscle closer to the vertebral spine to ensure musculocutaneous blood supply and should not be extended more than 7 cm distal to the inferior angle of the scapula.
The most common error in harvesting the vertical TF is failure to raise the trapezius muscle in the plane superficial to the rhomboid major and minor muscles. This is best accomplished by identifying the lateral border of the caudal portion of the trapezius muscle. Meticulous dissection in the plane deep to the trapezius muscle allows identification of the fibers of the rhomboid major muscle that run in a more transverse orientation and insert into the medial border of the scapula.
After the incision along the lateral border of the trapezius muscle (the medial border of the scapula), the flap is elevated by cutting the muscle fibers and following straight along the pedicle vessels. Because of the size and course of the vessels at this level, magnification is really helpful.
When dissecting the upper part of trapezius off the rhomboid minor muscle, utmost care must be taken to avoid injury to the accompanying DS nerve, and the dissection must not affect the accessory nerve.
CONCLUSION
While free tissue transfer is the mainstay of complex intraoral reconstructions, knowledge of pedicled regional flaps is very useful for smaller defects or salvage of partially failed reconstructions. The BFP flap, FAMM flap, platysma, PM flap, TMF, and TFs offer a plethora of options for local/regional flap reconstruction for intraoral pathology.
References
- Mathes S J, Nahai F. Classification of the vascular anatomy of muscles: experimental and clinical correlation. Plast Reconstr Surg. 1981;67:177–187. [PubMed] [Google Scholar]
- Dean A, Alamillos F, García-López A, Sánchez J, Peñalba M. The buccal fat pad flap in oral reconstruction. Head Neck. 2001;23:383–388. doi: 10.1002/hed.1048. [DOI] [PubMed] [Google Scholar]
- Chien C Y, Hwang C F, Chuang H C, Jeng S F, Su C Y. Comparison of radial forearm free flap, pedicled buccal fat pad flap and split-thickness skin graft in reconstruction of buccal mucosal defect. Oral Oncol. 2005;41:694–697. doi: 10.1016/j.oraloncology.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Amin M A, Bailey B M, Swinson B, Witherow H. Use of the buccal fat pad in the reconstruction and prosthetic rehabilitation of oncological maxillary defects. Br J Oral Maxillofac Surg. 2005;43:148–154. doi: 10.1016/j.bjoms.2004.10.014. [DOI] [PubMed] [Google Scholar]
- Poeschl P W, Baumann A, Russmueller G, Poeschl E, Klug C, Ewers R. Closure of oroantral communications with Bichat's buccal fat pad. J Oral Maxillofac Surg. 2009;67:1460–1466. doi: 10.1016/j.joms.2009.03.049. [DOI] [PubMed] [Google Scholar]
- Pribaz J J, Stephens W, Crespo L, Gifford G. A new intraoral flap: facial artery musculomucosal (FAMM) flap. Plast Reconstr Surg. 1992;90:421–429. doi: 10.1097/00006534-199209000-00009. [DOI] [PubMed] [Google Scholar]
- Ashtiani A K, Emami S A, Rasti M. Closure of complicated palatal fistula with facial artery musculomucosal flap. Plast Reconstr Surg. 2005;116:381–386. discussion 387–388. doi: 10.1097/01.prs.0000142475.63276.87. [DOI] [PubMed] [Google Scholar]
- Ayad T, Kolb F, De Monés E, Mamelle G, Temam S. Reconstruction of floor of mouth defects by the facial artery musculo-mucosal flap following cancer ablation. Head Neck. 2008;30:437–445. doi: 10.1002/hed.20722. [DOI] [PubMed] [Google Scholar]
- Martin D, Pascal J F, Baudet J, et al. The submental island flap: a new donor site. Anatomy and clinical applications as a free or pedicled flap. Plast Reconstr Surg. 1993;92:867–873. [PubMed] [Google Scholar]
- Martin D, Legaillard Ph, Bakhach J, Hu W, Baudet J. [Reverse flow YV pedicle extension: a method of doubling the arc of rotation of a flap under certain conditions] Ann Chir Plast Esthet. 1994;39:403–414. [PubMed] [Google Scholar]
- Szudek J, Taylor S M. Systematic review of the platysma myocutaneous flap for head and neck reconstruction. Arch Otolaryngol Head Neck Surg. 2007;133:655–661. doi: 10.1001/archotol.133.7.655. [DOI] [PubMed] [Google Scholar]
- Chen W L, Li J S, Yang Z H, Huang Z Q, Wang J U, Zhang B. Two submental island flaps for reconstructing oral and maxillofacial defects following cancer ablation. J Oral Maxillofac Surg. 2008;66:1145–1156. doi: 10.1016/j.joms.2007.09.023. [DOI] [PubMed] [Google Scholar]
- Clauser L, Curioni C, Spanio S. The use of the temporalis muscle flap in facial and craniofacial reconstructive surgery. A review of 182 cases. J Craniomaxillofac Surg. 1995;23:203–214. doi: 10.1016/s1010-5182(05)80209-4. [DOI] [PubMed] [Google Scholar]
- Pinto F R, de Magalhães R P, Capelli F de A, Brandão L G, Kanda J L. Pedicled temporoparietal galeal flap for reconstruction of intraoral defects. Ann Otol Rhinol Laryngol. 2008;117:581–586. doi: 10.1177/000348940811700805. [DOI] [PubMed] [Google Scholar]
- Urken M L, Biller H F. Pectoralis major. In: In: Urken ML, Cheney ML, Sullivan MJ, Biller HF, editor. Atlas of Regional and Free Flaps for Head and Neck Reconstruction. New York, NY: Raven Press; 1995. pp. 3–28. [Google Scholar]
- Milenović A, Virag M, Uglesić V, Aljinović-Ratković N. The pectoralis major flap in head and neck reconstruction: first 500 patients. J Craniomaxillofac Surg. 2006;34:340–343. doi: 10.1016/j.jcms.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Vartanian J G, Carvalho A L, Carvalho S MT, Mizobe L, Magrin J, Kowalski L P. Pectoralis major and other myofascial/myocutaneous flaps in head and neck cancer reconstruction: experience with 437 cases at a single institution. Head Neck. 2004;26:1018–1023. doi: 10.1002/hed.20101. [DOI] [PubMed] [Google Scholar]
- Urken M L. Trapezius system. In: In: Urken ML, Cheney ML, Sullivan MJ, Biller HF, editor. Atlas of Regional and Free Flaps for Head and Neck Reconstruction. New York, NY: Raven Press; 1995. pp. 29–48. [Google Scholar]
- Haas F, Weiglein A, Schwarzl F, Scharnagl E. The lower trapezius musculocutaneous flap from pedicled to free flap: anatomical basis and clinical applications based on the dorsal scapular artery. Plast Reconstr Surg. 2004;113:1580–1590. doi: 10.1097/01.prs.0000117188.03152.10. [DOI] [PubMed] [Google Scholar]
- Chen W L, Li J S, Yang Z H, Huang Z Q, Wang J Q. Extended vertical lower trapezius island myocutaneous flap for repairing extensive oropharyngeal defects. J Oral Maxillofac Surg. 2009;67:1349–1353. doi: 10.1016/j.joms.2006.11.048. [DOI] [PubMed] [Google Scholar]