Abstract
The HIV/AIDS epidemic remains a major public health issue across the globe, and it is of particular concern in sub-Saharan Africa. Utilization of sexual and reproductive health (SRH) services can significantly impact HIV prevention, transmission, and treatment. SRH service utilization may be determined by individual characteristics, such as education and economic status, but also by the location and accessibility of health care facilities. Using population-based survey data, this study applies exploratory spatial analysis techniques to examine spatial patterns of SRH service utilization among rural married women in southern Mozambique. Clustering among those using services is found as are spatial associations, indicating significant spatial variability in the utilization of health services. The findings provide valuable insights for current and future health care program planning and configuration.
Keywords: HIV testing, Family planning, Health care utilization, GIS, Spatial analysis
Introduction
Enduring public health challenges, especially in the area of sexual and reproductive health (SRH), in resource-limited sub-Saharan African countries call for improvement of health care services in the region. Because utilization of these services is affected by individuals’ access to health care clinics (Higgs, 2009), it is important to better understand how utilization of services is influenced by spatial accessibility and geographic interactions.
Health outcomes have an inherently geographic nature because influencing factors generally vary across space. Studies have found that spatial variation in the number of doctors, quality and capacity of health services can be critical for service utilization and associated health outcomes (e.g., Chaix, Merlo, & Chauvin, 2005; Fisher et al., 2000). In particular, past research has found that geographic proximity to health services is associated with primary care utilization (Tanser, Gijsbertsen, & Herbst, 2006), contraceptive use and method choice (Brauner-Otto, Axinn, & Ghimire, 2007; Entwisle, Rindfuss, Walsh, Evans, & Curran, 1997), child health (Lavy, Strauss, Thomas, & de Vreyer, 1996), vaccination (Acharya & Cleland, 2000), and delivery care (Rahman, Mosley, Ahmed, & Akhter, 2008). The influence of distance to health services has been less studied for HIV-related services, given the relative recentness of the introduction of these services in much of the developing world. Distance to a facility has been shown to be negatively associated with finding out the results of HIV tests in rural Malawi (Thornton, 2008) and with receiving an HIV test among low-income Los Angeles residents (Leibowitz & Taylor, 2007).
This study investigates utilization of SRH services in Mozambique, an impoverished nation in southeast Africa, through analysis of health outcomes and underlying factors, especially proximity to the health services, in relation to observed utilization patterns. HIV infection rates among adults in Mozambique are high, with some rural areas seeing one in four adults being infected. The focus here is on rural women of reproductive age and whether they have been tested for HIV as well as whether they are using a modern family planning method. We selected these two outcomes as examples of key SRH services offered to rural women. Both family planning and HIV testing are the target of national and international efforts to increase uptake, and more importantly serve to decrease the impacts and spread of HIV/AIDS.
Family planning services have existed in Mozambique for a long time. The National Family Planning Program was launched in 1980 with the main goal of improving the health of women and children (Ministry of Health, 2010a). Most family planning services, especially in rural areas, are delivered through a network of state-run maternal and child health clinics, which offer oral hormonal contraceptives (the Pill), injectable contraceptives (such as Depo-Provera), intra-uterine devices (IUDs), and male condoms free of charge; condoms can also be obtained from private outlets for a low price (Prata, Sreenivas, & Bellows, 2008). Female condoms and female sterilization are also available but their use remains very low. Between the two Demographic and Health Surveys conducted in Mozambique in 1997 and 2003, modern contraceptive prevalence among women rose from 5.1% to 14.2%. However, the rural-urban differentials in modern contraceptive use remain substantial: in rural areas, contraceptive prevalence between the two surveys increased from 2.3% to 7.0% (Instituto Nacional de Estatística and Macro International, 1999, 2005).
In contrast to family planning, HIV counseling, testing and treatment services are relatively new. Voluntary counseling and testing (VCT) and prevention of mother-to-child transmission (PMTCT) were introduced in Mozambique in 2001 (Pfeiffer et al., 2010) and a nationwide program of antiretroviral treatment was started in 2004 (Audet, Burlison, Moon, Sidat, & Vergara, 2010). Most HIV counseling and testing and all antiretroviral treatment are provided through the state health sector free of charge, and the majority of users are women undergoing prenatal care (Ministry of Health, 2006). Funded largely through the US President’s Emergency Fund for AIDS Relief (PEPFAR) and other foreign and international agencies, these services have expanded rapidly. However, by 2006, the year in which the survey data used in this study were collected, only 281 HIV counseling and testing units were operating in Mozambique (Ministry of Health, 2006: 4) for a population of approximately 22 million (World Bank, 2011). Despite a continuous and rapid expansion of HIV services, their supply still lags behind need in a country where the estimated national HIV prevalence among adults aged 15–49 is 12%, reaching as high as 25% in Gaza province, where the data for our study were gathered (Ministry of Health, 2010b: 7).
As geographic context plays a critical role in health outcomes, geographical information systems (GIS) have been widely applied in health related studies (see Cromley & McLafferty, 2002; Curtis & Leitner, 2006). Mapping and visualization have been used to display geographic information since Snow’s disease map of London’s cholera outbreak in 1854. New systems for desktop mapping using GIS have made it easy and straightforward to visualize and display geographic information. In addition, spatial analysis using GIS can provide insights into spatial relationships among different factors for subsequent hypothesis testing regarding space-time patterns that otherwise cannot be detected. Exploratory spatial data analysis (ESDA) is a collection of techniques to describe and visualize spatial patterns by graphic and map-based visualization that facilitates hypotheses formulation and testing without prior knowledge of the study context (Anselin, 1994, 1998; Anselin & Bao, 1997; Murray, 2010). The exploratory process can therefore benefit the etiologic investigation seeking possible underlying factors associated with disease clusters, outbreaks, and similar outcomes.
This study will provide an enhanced understanding of SRH utilization variability, enabling services to be better targeted and clinic placement to be more effective. The remainder of the paper is structured as follows. First, we describe the study area and the data. We then provide an overview of the spatial analysis methods utilized in this study and present application results. We conclude with a discussion of the results and implications of the study.
Methods
Data and study area
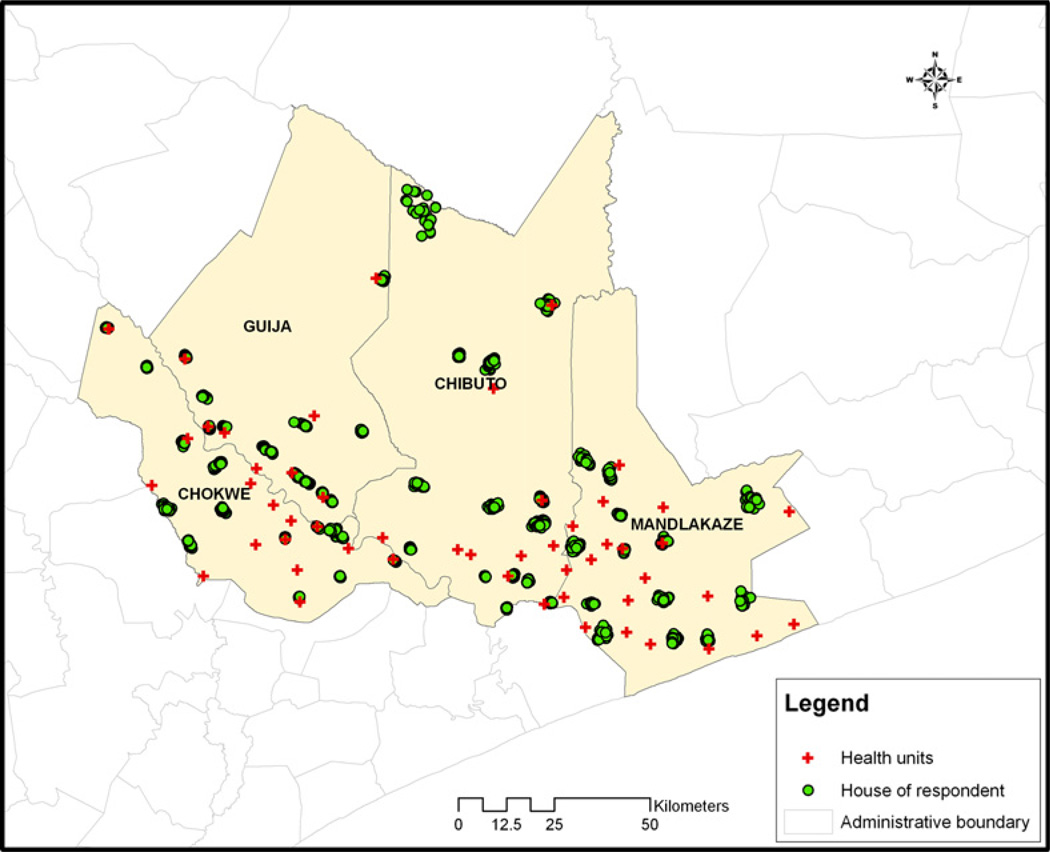
The data used in this study come from a survey conducted in 2006 in rural areas of four districts (Chibuto, Chokwe, Guija and Mandlakaze) of Gaza province in southern Mozambique. The study area is approximately 5900 square miles with a population of about 625,000. Fifty-three primary health clinics serve the region, among which only five provided HIV testing at the time of the survey. The area’s economy is characterized by subsistence agriculture and high levels of male labor out-migration (primarily to neighboring South Africa). Fertility in the area remains high and family planning use is relatively low. Gaza province has the highest HIV prevalence in Mozambique, 25% (Ministry of Health, 2010c), which is often attributed to high rates of labor migration, but the availability of HIV testing and treatment remained limited until recently.
The survey sample included 1680 married women aged 18–40 from 56 villages (14 villages per district, selected with probability proportional to size). Within each village, 30 married women, more or less evenly divided between those married to migrants and those married to non-migrants, were selected through probability sampling. The geographical location of each respondent was recorded as point-based spatial data (latitude and longitude), along with information on age, educational level, household characteristics, husband’s migration status, and reproductive and HIV/AIDS-related characteristics. The spatial distribution of the respondents’ residences as well as health services is shown in Fig. 1. Most women in the sample live in the southern part of the study area, as the northern part is relatively sparsely populated. A similar pattern can be observed for health services, with most located in the south.
Fig. 1. Study Area.
This figure describes the study area, the location of respondents and the health units.
Spatial analysis
This study employs both exploratory spatial data analysis (ESDA) and confirmatory analysis.1 Specifically, ESDA is used to detect potential spatial patterns and associations in health outcomes. Confirmatory analysis then tests the causal relationship among health outcomes and possible influencing factors. Generally, it is necessary to engage in initial exploratory analysis before any formal inquiry about the factors that might account for the spatial patterns identified using ESDA can be assessed.
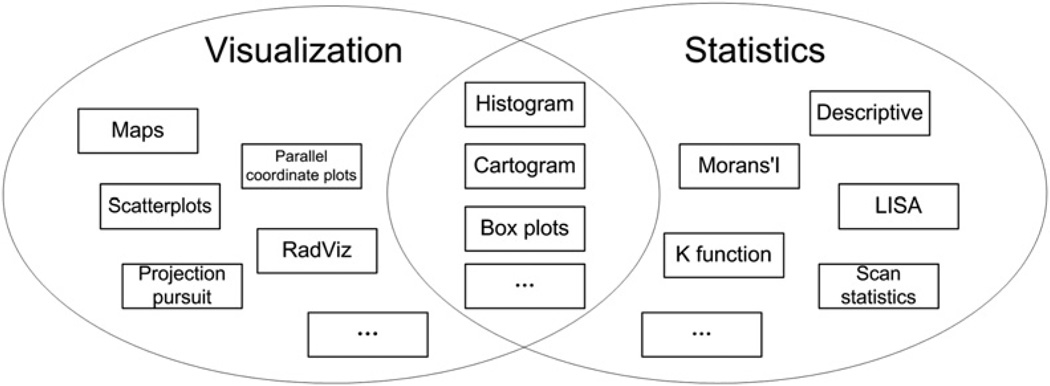
ESDA is the extension of exploratory data analysis (EDA) (Tukey, 1977) to a geographic context, emphasizing the spatial characteristics of the data. Effectively, ESDA is a collection of techniques to describe and visualize spatial distributions, identify atypical observations or spatial outliers, discover patterns of spatial association, clusters, or hot spots, and suggest spatial regimes (Anselin, 1994, 1998; Murray, 2010). A diagram summarizing and categorizing techniques associated with ESDA is given in Fig. 2. Approaches include graphic and map-based visualization, as well as statistics to facilitate hypotheses formulation and testing. Usually, the tools employed in visualization are maps, box plots, scatterplots, histograms, and cartograms, among others. Common statistical techniques in ESDA include traditional descriptive measures as well as spatial approaches, such as Moran’s I, K function, scan statistics, etc. ESDA is distinctive because it brings together all of these techniques, allowing for the interaction/integration of visualization and statistical measures. This interaction is reflected in the overlapping area of approaches in Fig. 2. The connection and interaction among different methods/displays is commonly structured using dynamic graphics with linking and brushing, making ESDA a powerful tool for exploration.
Fig. 2. ESDA Overview.
ESDA is primarily comprised of two important components: visualization and statistics. Tools of visualization include maps, scatterplots, RadViz (a method mapping high-dimensional data onto two dimensional space) and projection pursuit (a technique finding projections that can reveal structures in high-dimensional data), etc. Common statistics include basic descriptive, Moran’s I, and LISA. In addition, some elements are in the intersection of those two parts, such as histogram and cartogram.
Because the survey data are discrete points representing the residence of the respondents, two ESDA methods for point data, Ripley’s K function and the spatial scan statistic (see Rogerson & Yamada, 2009), are initially employed to evaluate the spatial distribution of respondent behavior and attributes. Of interest here is whether the distribution is clustered or not. The K function is used to detect global clustering as compared to a random distribution. The estimated K function values are based on measuring the average number of other events within a certain distance of an event divided by the intensity of the events in the study area. Since the values of the outcomes are binary, the difference of the two K functions, KD(d) = Kcase(d) − Kcontrol(d), is used as an indicator of the actual risk of receiving the health service in question (Gatrell, Bailey, Diggle, & Rowlingson, 1996; Wheeler, 2007). The spatial scan statistic is based on a probability model. It employs a scanning window of predefined shape (circular or elliptical) and variable size that moves over the entire study area to detect whether the rates inside the window are unusually higher than those outside of the window using a log-likelihood ratio test. The spatial scan statistic used here is the Bernoulli model proposed by Kulldorff (1997). These tests describe only spatial associations. Of course, demographic, social and environmental factors associated with geographic areas may play an influential role as well; we examine these factors explicitly in the confirmatory analyses.
Beyond point data, we also consider aggregate village-level summaries. Two spatial autocorrelation statistics, Moran’s I and Local Indicator of Spatial Association (LISA) (see Anselin, 1995), are used to assess spatial dependency among village-level observations. Moran’s I is a commonly used statistic to assess global spatial autocorrelation for a given variable. The value of this statistic ranges from –1 to 1, where positive values indicate observations with similar values being close to each other and negative values suggest observations with high values are near those with low values, or vice versa. The LISA effectively decomposes a global measure of spatial autocorrelation for each spatial unit, enabling assessment of statistical significance for each unit. Accordingly, the global Moran’s I is the mean of the local Moran’s I. We therefore seek to find out whether the respondents living closer to each other exhibit similar behavior or similar health outcomes.
In contrast to ESDA, confirmatory analysis seeks to test an a priori hypothesis. One of the most common confirmatory methods is correlation testing, especially regression analysis, which concerns the relationship between one dependent variable and one or more explanatory variables. Confirmatory analysis is utilized in this study to identify the potential underlying demographic and socio-environmental factors, especially proximity to health facilities, that might account for the spatial patterns suggested through ESDA. Our particular interest here relates to accessibility of health services. We fit a logistic regression model to investigate the influence of woman’s education, husband’s migration status, and distance, among other factors, on the use of health services. A spatial smoothing function is used to express the residual spatial variation (see Kelsall and Diggle (1998) for an introduction of the basic approach).
Given previous research findings about the relationship between female education and health care utilization and outcomes (Elo, 1992; Raghupathy, 1996) as well as connections between migration and reproductive and health behavior and outcomes (Agadjanian, Arnaldo, & Cau, 2011; Agadjanian, Yabiku, & Cau, 2011), education (dichotomized as five years or more of education vs. fewer than five years) and husband’s migration status (distinguishing women married to migrants from those with non-migrant husbands) are included as key non-spatial predictors (independent variables). In addition, the models account for individual and village-level characteristics: age, household wealth, the village-specific sample average of the household wealth index, the proportion of women with five or more years of education in the village sample, and the percent of women with any religious affiliation in the village sample. Because household wealth and income are notoriously difficult to measure in developing country settings, to account for differences in household economic resources, we use a scale with values ranging from one to four representing household possession of common durable goods (radio, bicycle, motorcycle, car).
The ESDA methods used in this analysis were structured using ArcGIS as well as other publically accessible packages and subroutines. Ripley’s K function and the logistic regression model are implemented in R. The spatial scan statistics are accessed using SaTScan. Moran’s I and LISA results are derived using GeoDa.
Results
A basic descriptive summary of the 1678 respondents included in the analysis is provided in Table 1. The study area has low rates of health care utilization for both key outcomes: 17.9% of respondents had been tested for HIV and 14.1% were using family planning. The average distance from the residence to the nearest primary clinic is about 5.50 km. This average distance increases to approximately 22.98 km for the nearest clinic that provides HIV testing. Further, 53.4% women have no primary clinics and 95.5% women have no clinics providing HIV testing within 5 km of their residence. This indicates generally poor accessibility of clinics due to long travel distances that would be necessary to obtain certain health services, in part explaining the low ratio of positive responses in the outcomes.
Table 1.
Basic description of the survey sample. Sample size: 1678.
| Variable | N | Percent |
|---|---|---|
| Having had an HIV test | 300 | 17.9 |
| Using a modern family planning method | 236 | 14.1 |
| More than 5 years of education | 469 | 28.0 |
| Husband’s migrant status | 690 | 41.1 |
| Age (under 20) | 267 | 15.9 |
| Age (21–25) | 470 | 28.0 |
| Age (26–30) | 469 | 28.0 |
| Age (31 plus) | 472 | 28.1 |
| Household possessions index = 1 | 563 | 33.6 |
| Household possessions index = 2 | 546 | 32.5 |
| Household possessions index = 3 | 424 | 25.3 |
| Household possessions index = 4 | 145 | 8.6 |
| With religious affiliation | 1445 | 86.1 |
| Mean | Std. | |
| Distance to closest primary clinic (km) | 5.50 | 4.46 |
| Distance to closest clinic providing HIV testing (km) | 22.98 | 16.88 |
In addition to descriptive statistics, visualization is an important ESDA component and is often used as an initial step to help formulate hypothesis when examining spatial data. As noted above, the map in Fig. 1 suggests that more of the survey respondents are in the south and there health facilities are concentrated in the south as well, especially those providing HIV testing. Spatial patterns are therefore investigated further using two ESDA methods: K function and spatial scan statistics. In addition, also of interest in this study is whether women with similar health outcomes share geographic ties (or neighborhood effects). Such spatial dependence is assessed using two spatial autocorrelation statistics: Moran’s I and LISA. Finally, since the villages in the north of the study area are far away from all five clinics providing HIV tests, it is possible that the geographic accessibility of those services could affect the observed outcomes and patterns. This possibility is explored using the logistic regression model.
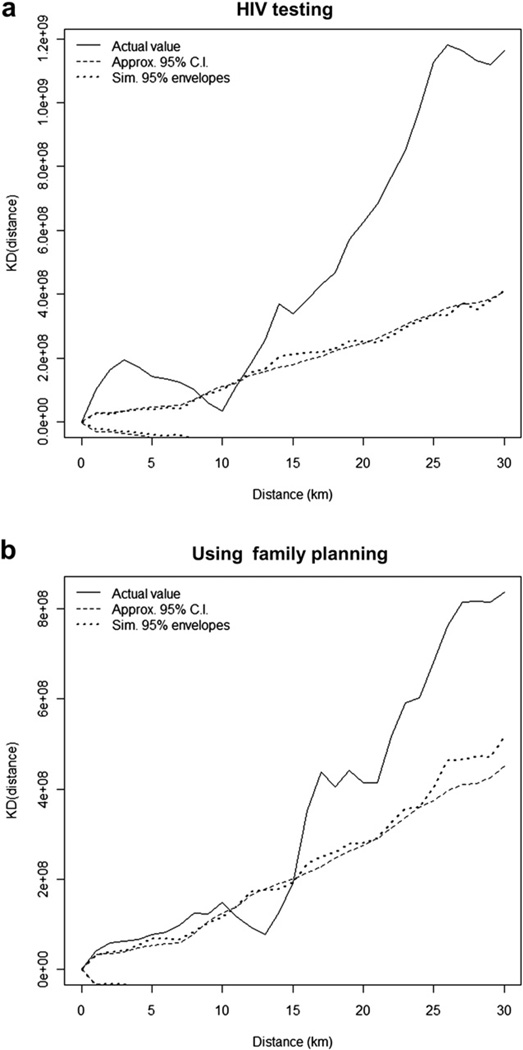
As to the outcome of HIV testing, both the K function and the spatial scan statistic analyses show significant spatial clustering. The effect of this K function difference on HIV testing is shown in Fig. 3(a), along with the approximate 95% confidence intervals and 95% simulation envelopes. Usually, the estimated K function values are compared with those produced by a random distribution representing complete random spatial process, and larger estimated values indicate spatial clustering at that distance. The general spatial pattern indicates significant clustering at smaller (less than 8 km) or larger distances (larger than 12 km). No significant clustering is found in intermediate distances ([8 km, 12 km]) as the curve of actual values falls within the confidence bands.
Fig. 3. Differences of K Functions.
This figure describes the differences of K functions for the two outcomes. Both outcomes have a similar spatial pattern, indicating significant clustering at smaller (less than 8 km in (a) and 10 km in (b)) or larger distances (larger than 12 km in (a) and 15 km in (b)) where estimated values are larger than those from a random distribution. No significant clustering is found in intermediate distances ([8 km, 12 km] in (a) and [10 km, 15 km] in (b)) as the curve of actual values falls within the confidence bands.
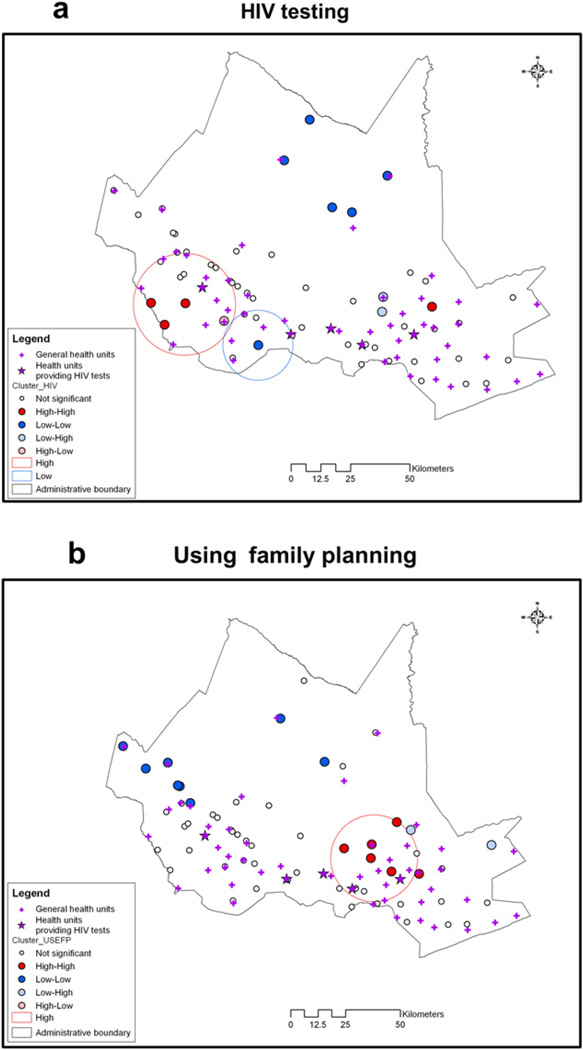
The spatial scan statistic detected both high risk and low risk clusters for having had an HIV test; these clusters are shown in Fig. 4(a). The red circle indicates the higher than expected response cluster. In this case there are 271 women of whom 31.9% had been tested. This proportion is significantly higher than the expected rate (p-value < .001). The blue circle identifies a low likelihood cluster containing 123 women of whom only 4.1% had been tested. This proportion is significantly lower than the expected rate (p-value < .001).
Fig. 4. Local Cluster Maps.
The circles are clusters from spatial scan statistic, where red circles are high value clusters and blue circles are low value clusters. The dots are village-level cluster centers from LISA analysis, where red dots are high–high cluster centers and blue dots are low–low cluster centers. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
In the analysis of data aggregated at the village-level, both Moran’s I and LISA detected spatial dependence. Moran’s I is 0.164 for HIV testing (p-value < .01). At a more local level, LISA found both high–high and low–low local clusters. Again, given the health services shown in Fig. 4 the five villages of low values in the north are far away from the five health care facilities providing HIV tests. The poor accessibility of health services could explain low HIV testing rates. However, for other cluster centers in Fig. 4(a), it is hard to tell whether there is such a distance effect because the low–low cluster in the south has a clinic providing HIV tests nearby, and the high–high clusters are not closest to villages near clinics.
Results from logistic regression are largely consistent with exploratory results. Table 2a shows coefficients and p-values resulting from logistic regression of HIV testing. Distance has a significant impact on HIV testing, partially consistent with the LISA analysis. Education also has a positive influence. Compared to the lowest level household (index = 1), more household (index = 2, 4) can increase the odds of HIV testing as well. In contrast, age and husband’s migration status has no significant effect. For the community level variables, only education has a significant impact.
Table 2.
Results from logistic regression model analysis.
| Estimate | Std. Error | p-value | |
|---|---|---|---|
| (a) HIV testing | |||
| (Intercept) | 0.890 | 1.460 | 0.542 |
| Distance to closest clinic (km) | −0.054* | 0.027 | 0.046 |
| 5 or more years of education | 0.458** | 0.162 | 0.005 |
| Husband is a migrant | −0.002 | 0.139 | 0.987 |
| Age (years) | −0.017 | 0.012 | 0.168 |
| Household possessions index = 2 | 0.383* | 0.170 | 0.025 |
| Household possessions index = 3 | 0.166 | 0.196 | 0.397 |
| Household possessions index = 4 | 0.600* | 0.250 | 0.016 |
| Community average household possessions index | −0.337 | 0.425 | 0.427 |
| Percent in community with 5 or more years of education | 1.926* | 0.926 | 0.038 |
| Percent in community with religious affiliation | −1.315 | 1.187 | 0.268 |
| (b) Using family planning | |||
| (Intercept) | −4.789*** | 1.274 | 0.000 |
| Distance to closest clinic (km) | −0.027 | 0.025 | 0.269 |
| 5 or more years of education | 0.500** | 0.174 | 0.003 |
| Husband is a migrant | −0.158 | 0.153 | 0.303 |
| Age (years) | 0.033** | 0.013 | 0.008 |
| Household possessions index = 2 | −0.073 | 0.183 | 0.691 |
| Household possessions index = 3 | 0.096 | 0.214 | 0.653 |
| Household possessions index = 4 | 0.574* | 0.267 | 0.031 |
| Community average household possessions index | 0.544 | 0.410 | 0.185 |
| Percent in community with 5 or more years of education | 0.487 | 0.856 | 0.569 |
| Percent in community with religious affiliation | 0.737 | 1.121 | 0.511 |
Sample size: 1678.
Significance codes: p < 0.001 ‘***’, p < 0.01 ‘**’, p < 0.1 ‘*’.
Similar to the outcome of HIV testing, family planning use also follows spatial clustering, shown in Fig. 3(b) and Fig. 4(b). In terms of the K function differences, significant clustering is at smaller (less than 10 km) or larger distances (larger than 15 km), and no significant clustering is found in intermediate distances ([10 km, 15 km]). The spatial scan statistic detected only one cluster of high likelihood, represented by the red circle in Fig. 4(b). This high-prevalence cluster (p-value < .001) includes 224 women, 32.1% of whom were using family planning. In the spatial dependency analysis, Moran’s I is 0.371 (p-value < .01), indicating a stronger global spatial autocorrelation than that of HIV testing. In addition, LISA found both high–high and low–low local clusters. As can be seen in Fig. 4(b), most of those clusters with low values seem quite close to health facilities, so the geographic proximity associated with family planning use might not be as important as it is for HIV testing.
As shown by the results of logistic regression in Table 2b, distance has no significant influence on using family planning, neither husband’s migration status nor community level variables. Both education and age have positive effect here. In addition, only the largest amount of household (index = 4) can increase the possibility of using family planning in comparison with the lowest level household (index = 1).
Given the discussion above, the spatial clustering found in those two outcomes would suggest likely regional variations in respondents’ utilization of associated health services. Further, the spatial dependence detected implies that women tend to have similar health outcome responses based on geographic proximity. In addition, different geographical locations of the local clusters in Fig. 4 suggests that HIV testing and use of contraception have different spatial response distributions. Again, for local clusters found by LISA, some of high–high clusters and low–low clusters reaffirm the clusters detected using the K function approach. Finally, through logistic regression, distance has a significant impact on HIV testing but not on use of modern contraception, and education has a positive influence on both outcomes while the husband’s migration status has no significant effect on either. The highly significant smoothing terms (p-value < .001) in both models indicate that the explanatory variables included do not fully account for the spatial patterns of those two outcomes. Specifically, the spatial clustering of HIV testing and family planning use is not fully explained by distance from health services.
Discussion
In this study we employed spatial analysis to study sexual and reproductive health service utilization in southern Mozambique. One objective of this study was to assess the spatial distribution and associations for HIV testing and family planning use. We found global clustering and autocorrelation as well as local clusters associated with outcomes. The regional inequity in utilization of HIV and family planning services illustrates the disadvantage of relatively sparsely populated areas and suggests the need for enhanced efforts to increase the provision of HIV testing and other related services in targeted areas.
Another objective of our study was to investigate the potential factors responsible for varied geographic accessibility of services. Our results for HIV testing were mixed. Consistent with other studies demonstrating the importance of distance to services for utilization of these services and health outcomes (e.g., Jack, Gulliford, Ferguson, & Moller, 2003; Jones et al., 2008a, 2008b), logistic regression analyses found that distance to clinics has an impact on utilization of HIV testing services in the regression analysis. However, ESDA did not suggest a consistent conclusion. It is possible that the relationship between geographic proximity and utilization of health services could be more complicated, which will be further discussed in the following paragraph. The analysis of family planning did not find a significant role for distance. One possible reason for the difference in results between the two outcomes may be the earlier mentioned recency of HIV testing services compared to more established family planning services. Another reason for this may be the reliance on Euclidean distance as it may not accurately reflect travel time in the study area. Without information on road networks or travel times, it was not possible to test other measures of travel.
In this study, we did not explore regional variation in distance effects. Although distance is an important factor, its influence can be complex. For instance the five villages of low values in the north of study area had poor access to the health facilities providing HIV tests in terms of distance, but the low–low cluster in the south had a clinic nearby. Field and Briggs (2001) found that the influence of distance on the utilization of health services is not necessarily linear. Jones et al. (2008a, 2008b) suggested the impact of the distance on health outcomes can vary depending on the particular geographical setting and measures of accessibility. Also, underlying contributing factors, including distance, can have a local or regional impact (Fotheringham, Brunsdon, & Charlton, 2002). In the present case, distance may have a greater effect on the five villages in the north than on the low–low cluster in the south, possibly due to other factors such as education. Alternatively, utilization variability may reflect stages of adopting new health care practices, where distance becomes less important when new practices become widely accepted as part of social norms. The extensive literature on the diffusion of contraceptive and reproductive innovations illustrates the importance of social interactions in the spread of novel health technologies and practices (e.g., Behrman, Kohler, & Watkins, 2002; Casterline, 2001; Kohler, 1997; Montgomery & Casterline, 1996; Rutenberg & Watkins, 1997).
Our analysis of health services utilization was limited to only two outcomes. Other health outcomes, such as child delivery at a health facility, may be added in the future. Likewise, as suggested by the confirmatory analysis, additional predictors should also be included as access to health services can be affected by factors other than distance, such as transportation and availability and quality of roads.
Conclusions
Ensuring access to SRH services in poor rural settings in sub-Saharan Africa is of great importance for improving health outcomes in general and mitigating the impact of the HIV/AIDS epidemic in particular. This study shows that spatial analysis approaches including ESDA and confirmatory analysis can help reveal regional variations in outcomes and detect potential contributing factors. The results can help inform service delivery and infrastructure development programs in resource-limited sub-Saharan settings. As considerable efforts to increase SRH service utilization in such settings continue, these efforts should take into full consideration the geographic dimensions of the demand for and supply of these services.
Acknowledgments
We thank the support of the Eunice Kennedy Shriver National Institute of Child Health & Human Development (grants #R21HD048257; R01HD058365; R01HD058365-03S1).
Footnotes
While for the sake of convenience we make a distinction between exploratory and confirmatory methods, in practice the differences can be less than clear. In fact, many of the methods used in ESDA are confirmatory methods that can be used to test specific hypothesis. As a result, it is often the issue of how the method is used, and in our particular case the approaches noted as part of ESDA are used for exploratory analysis.
Contributor Information
Jing Yao, Email: jingyao@asu.edu.
Alan T. Murray, Email: atmurray@asu.edu.
Victor Agadjanian, Email: victor.agadjanian@asu.edu.
Sarah R. Hayford, Email: sarah.hayford@asu.edu.
References
- Acharya LB, Cleland J. Maternal and child health services in rural Nepal: does access or quality matter more? Health Policy and Planning. 2000;15(2):223–229. doi: 10.1093/heapol/15.2.223. [DOI] [PubMed] [Google Scholar]
- Agadjanian V, Arnaldo C, Cau B. Health costs of wealth gains: labor migration and perceptions of HIV/AIDS risks in Mozambique. Social Forces. 2011;89(4):1097–1117. doi: 10.1093/sf/89.4.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agadjanian V, Yabiku ST, Cau B. Men’s migration and women’s fertility in rural Mozambique. Demography. 2011;48(3):1029–1048. doi: 10.1007/s13524-011-0039-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anselin L. Exploratory spatial data analysis and geographic information systems. In: Painho M, editor. New tools for spatial analysis. Luxembourg: Eurostat; 1994. pp. 45–54. [Google Scholar]
- Anselin L. Local indicators of spatial association - LISA. Geographical Analysis. 1995;27:93–115. [Google Scholar]
- Anselin L. Exploratory spatial data analysis in a geocomputational environment. In: Longley P, Brooks S, Macmillan B, McDonnell R, editors. Geocomputation, a primer. New York: Wiley; 1998. pp. 77–94. [Google Scholar]
- Anselin L, Bao S. Exploratory spatial data analysis linking SpaceStat and ArcView. In: Fisher M, Getis A, editors. Recent developments in spatial analysis. Berlin: Springer; 1997. pp. 35–59. [Google Scholar]
- Audet CM, Burlison J, Moon TD, Sidat M, Vergara AE. Sociocultural and epidemiological aspects of HIV/AIDS in Mozambique. BMC International Health and Human Rights. 2010;10(15):1–10. doi: 10.1186/1472-698X-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrman JR, Kohler HP, Watkins SC. Social networks and changes in contraceptive use over time: evidence from a longitudinal study in rural Kenya. Demography. 2002;39(4):713–738. doi: 10.1353/dem.2002.0033. [DOI] [PubMed] [Google Scholar]
- Brauner-Otto SR, Axinn WG, Ghimire DJ. The spread of health services and fertility transition. Demography. 2007;44(4):747–770. doi: 10.1353/dem.2007.0041. [DOI] [PubMed] [Google Scholar]
- Casterline J. Diffusion processes and fertility transition: Selected perspectives. Washington, D.C: National Academy Press; 2001. [PubMed] [Google Scholar]
- Chaix B, Merlo J, Chauvin P. Comparison of a spatial approach with the multi-level approach for investigating place effects on health: the example of healthcare utilisation in France. Journal of Epidemiology and Community Health. 2005;59:517–526. doi: 10.1136/jech.2004.025478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cromley EK, McLafferty S. GIS and public health. New York, NY: Guilford Publications; 2002. [Google Scholar]
- Curtis A, Leitner M. Geographic information systems and public health: Eliminating perinatal disparity. Hershey, PA: Idea Group Inc.; 2006. [Google Scholar]
- Elo IT. Utilization of maternal health-care services in Peru: the role of women’s education. Health Transition Review. 1992;2:49–69. [PubMed] [Google Scholar]
- Entwisle B, Rindfuss RR, Walsh SJ, Evans TP, Curran SR. Geographic information systems, spatial network analysis, and contraceptive choice. Demography. 1997;34:171–188. [PubMed] [Google Scholar]
- Field K, Briggs DJ. Socio-economic and locational determinants of accessibility and utilisation of primary health care. Health and Social Care in the Community. 2001;9(5):294–308. doi: 10.1046/j.0966-0410.2001.00303.x. [DOI] [PubMed] [Google Scholar]
- Fisher LS, Wennberg JE, Stukel TA, Skinner JS, Sharp SM, Freeman JL, et al. Associations among hospital capacity, utilization, and mortality of US medicare beneficiaries, controlling for socio-demographic factors. Health Services Research. 2000;34(6):1351–1362. [PMC free article] [PubMed] [Google Scholar]
- Fotheringham AS, Brunsdon C, Charlton ME. Geographically weighted regression: The analysis of spatially varying relationships. Chichester: Wiley; 2002. [Google Scholar]
- Gatrell AC, Bailey TC, Diggle PJ, Rowlingson BS. Spatial point pattern analysis and its application in geographical epidemiology. Transactions of the Institute of British Geographers New Series. 1996;21(1):256–274. [Google Scholar]
- Higgs G. The role of GIS for health utilization studies: literature review. Health Services and Outcomes Research Methodology. 2009;9(2):84–99. [Google Scholar]
- Instituto Nacional de Estatística and Macro International. Mozambique demographic and health survey 1997. Calverton, MD, U.S.A: Instituto Nacional de Estatística, Maputo, Mozambique and Macro International; 1999. (in Portuguese). [Google Scholar]
- Instituto Nacional de Estatística and Macro International. Mozambique demographic and health survey 2003. Calverton, MD, U.S.A.: Instituto Nacional de Estatística, Maputo, Mozambique and Macro International; 2005. (in Portuguese). [Google Scholar]
- Jack RH, Gulliford MC, Ferguson J, Moller H. Geographical inequalities in lung cancer management and survival in South East England: evidence of variation in access to oncology services? British Journal of Cancer. 2003;88(7):1025–1031. doi: 10.1038/sj.bjc.6600831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AP, Haynes R, Sauerzapf VA, Crawford SM, Zhao H, Forman D. Travel time to hospital and treatment for breast, colon, rectum, lung, ovary and prostrate cancer. European Journal of Cancer. 2008a;44:992–999. doi: 10.1016/j.ejca.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Jones AP, Haynes R, Sauerzapf VA, Crawford SM, Zhao H, Forman D. Travel times to health care and survival from cancers in Northern England. European Journal of Cancer. 2008b;44:269–274. doi: 10.1016/j.ejca.2007.07.028. [DOI] [PubMed] [Google Scholar]
- Kelsall JE, Diggle PJ. Spatial variation in risk: a nonparametric binary regression approach. Applied Statistics. 1998;47:559–573. [Google Scholar]
- Kohler HP. Learning in social networks and contraceptive choice. Demography. 1997;34(3):369–383. [PubMed] [Google Scholar]
- Kulldorff M. A spatial scan statistic. Communications in Statistics: Theory and Methods. 1997;26:1487–1496. [Google Scholar]
- Lavy V, Strauss J, Thomas D, de Vreyer P. Quality of health care, survival, and health outcomes in Ghana. Journal of Health Economics. 1996;15(3):333–357. doi: 10.1016/0167-6296(95)00021-6. [DOI] [PubMed] [Google Scholar]
- Leibowitz AA, Taylor SL. Distance to public test sites and HIV testing. Medical Care Research and Review. 2007;64(5):568–584. doi: 10.1177/1077558707304634. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. Health counseling and testing: Annual report, 2006. Maputo, Mozambique: Ministry of Health; 2006. http://www.misau.gov.mz/pt/hiv_sida/relatorio_anual_da_informacao_do_aconselhamento_e_testagem_em_saude (in Portuguese). [Google Scholar]
- Ministry of Health. Strategy for family planning and contraception, 2011–2015(2020) Maputo, Mozambique: Ministry of Health; 2010a. (in Portuguese). [Google Scholar]
- Ministry of Health. National survey of HIV/AIDS prevalence, behavioral risks, and information (INSIDA), 2009. Final Report. Maputo, Mozambique: Ministry of Health; 2010b. (in Portuguese). [Google Scholar]
- Ministry of Health. Inquérito nacional de prevalência, riscos comportamentais e informação sobre o HIV e SIDA (INSIDA), 2009. Relatório final [National Survey of HIV/AIDS prevalence, behavioural risks, and information, 2009: Final report] Maputo, Mozambique: Ministry of Health of Mozambique; 2010c. [Google Scholar]
- Montgomery MR, Casterline JB. Population and Development Review. Vol. 22. 1996. Social learning, social influence, and new models of fertility; pp. 151–175. (Supplement: Fertility in the United States: New Patterns, New Theories) [Google Scholar]
- Murray AT. Quantitative geography. Journal of Regional Science. 2010;50:143–163. [Google Scholar]
- Pfeiffer J, Montoya P, Baptista AJ, Karagianis M, Pugas MD, Micek M, et al. Integration of HIV/AIDS services into African primary health care: lessons learned for health system strengthening in Mozambique - a case study. Journal of the International AIDS Society. 2010;13(3):1–9. doi: 10.1186/1758-2652-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata N, Sreenivas A, Bellows B. Potential of dual-use policies to meet family planning and HIV prevention needs: a case study of Zimbabwe and Mozambique. Journal of Family Planning and Reproductive Health Care. 2008;34(4):219–226. doi: 10.1783/147118908786000406. [DOI] [PubMed] [Google Scholar]
- Raghupathy S. Education and the use of maternal health care in Thailand. Social Science and Medicine. 1996;43:459–471. doi: 10.1016/0277-9536(95)00411-4. [DOI] [PubMed] [Google Scholar]
- Rahman MH, Mosley WH, Ahmed S, Akhter HH. Does service accessibility reduce socioeconomic differentials in maternity care seeking? Evidence from rural Bangladesh. Journal of Biosocial Science. 2008;40(1):19–33. doi: 10.1017/S0021932007002258. [DOI] [PubMed] [Google Scholar]
- Rogerson PA, Yamada I. Statistical detection and surveillance of geographic clusters. CRC Press; 2009. [Google Scholar]
- Rutenberg N, Watkins SC. The buzz outside the clinics: conversations and contraception in Nyanza Province, Kenya. Studies in Family Planning. 1997;28(4):290–307. [PubMed] [Google Scholar]
- Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilization in rural South Africa: an exploration using a geographical information system. Social Science and Medicine. 2006;63(3):691–705. doi: 10.1016/j.socscimed.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Thornton RL. The demand for, and impact of, learning HIV status. American Economic Review. 2008;98(5):1829–1863. doi: 10.1257/aer.98.5.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tukey JW. Exploratory data analysis. Addison-Wesely; 1977. [Google Scholar]
- Wheeler DC. A comparison of spatial clustering and cluster detection techniques for childhood leukemia incidence in Ohio, 1996–2003. International Journal of Health Geographics. 2007;6:13. doi: 10.1186/1476-072X-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. [Accessed 06.06.11];World Data Bank: health, nutrition, and population statistics. 2011 http://databank.worldbank.org/ddp/home.do.