Abstract
Plasma cell dyscrasias are frequently encountered malignancies often associated with kidney disease through the production of monoclonal immunoglobulin (Ig). Paraproteins can cause a remarkably diverse set of pathologic patterns in the kidney and recent progress has been made in explaining the molecular mechanisms of paraprotein-mediated kidney injury. Other recent advances in the field include the introduction of an assay for free light chains and the use of novel antiplasma cell agents that can reverse renal failure in some cases. The role of stem cell transplantation, plasma exchange, and kidney transplantation in the management of patients with paraprotein-related kidney disease continues to evolve.
Introduction
Monoclonal plasma cell disorders are common with monoclonal gammopathy of undetermined significance (MGUS) affecting up to 3.2% of all patients over the age of 50 and with multiple myeloma (MM) accounting for 10% of all hematologic malignancies.1,2 Renal insufficiency, defined by abnormal creatinine clearance, is present in up to half of myeloma patients at presentation, contributes to excessive early mortality, and diminishes eligibility and clinical outcomes after both systemic therapy and high-dose stem cell transplantation (SCT), as well as novel treatments.3,4 Indeed, reversibility of myeloma-associated renal impairment is a critically important prognostic factor and even supercedes response to systemic therapy as a predictor of improved survival.5 This review will discuss the mechanisms of kidney injury in monoclonal plasma cell disorders, while highlighting recent advances in the detection of monoclonal immunoglobulin (Ig), the availability of new renoprotective chemotherapeutic approaches, and the ongoing research into the roles of plasmapheresis and kidney transplantation in these diseases.
Monoclonal plasma cell disorders are a spectrum of diseases that includes premalignant MGUS, solitary plasmacytoma, Ig-mediated amyloidosis (AL amyloidosis), and both asymptomatic and symptomatic MM.6 Plasma cell clones across the entire spectrum exhibit malignant features including abnormal cell surface protein expression patterns and typically proliferate slowly, with a growth fraction of usually less than 1%.7 Virtually all myeloma cells and most clonal plasma cells associated with MGUS also have chromosomal abnormalities consisting of gene rearrangements or hyper- or hypodiploidy, which contribute to dysregulation of intracellular signaling pathways and in some cases are associated with progressive disease and a poor prognosis.8 The molecular events underlying the progression of MGUS to MM remain uncertain but may result from alterations in antitumor immunity as well as changes in the tumor-related microenvironment.9 As a paradigm of an emerging theme in myeloma as well as other areas of cancer biology, interactions among malignant plasma cells, bone marrow stromal cells, and extracellular matrix are now known to be critical to myeloma proliferation and chemotherapeutic resistance.10
Clinical presentation
Whether kidney impairment is present or not, the initial symptoms of myeloma and related plasma cell dyscrasias can be insidious and include fatigue, weight loss, and bone pain. Although most patients are older than 60 years of age, as many as 10% of myeloma patients are younger than 40 years of age (with, in 1 series, the youngest patient reported being 19 years old).11 Anemia, which is a traditional hallmark of myeloma, is present in up to 75% of patients at presentation. Patients with renal end-organ dysfunction and monoclonal Ig deposition disease (MIDD) are often hypertensive, whereas patients with amyloid may be hypotensive or orthostatic. Patients may also present with symptoms from systemic amyloid or monoclonal Ig deposition, including congestive heart failure, cardiac arrthymias, hepatomegaly, portal hypertension, and/or periorbital purpura.12 Conversely, gastrointestinal bleeding or perforation and elevated alkaline phosphatase are highly suggestive of amyloidosis affecting the gastrointestinal tract and liver, respectively.
The urine sediment is typically bland in patients with myeloma though a minority of patients with MIDD (∼ 20%) will have microscopic hematuria.12 In rare patients with monoclonal Ig-mediated glomerulonephritis, the urine sediment is active with red and white cells and cellular casts. Urine dipsticks are insensitive to cationic proteins like Ig, but tests of total urine protein are often abnormal. A simultaneously high urine total protein and low microalbumin (both normalized for urine creatinine) is highly suggestive of light chain proteinuria and should be confirmed with specific techniques to detect monoclonal Ig, as described below (see “Detection of monoclonal Ig”). Nephrotic range albuminuria suggests amyloidosis or glomerular deposition of monoclonal Ig. Myeloma may be present even when the urine is free from albumin, and so specific tests for monoclonal Ig should always be pursued if the index of suspicion is high.
Additional laboratory clues that might prompt testing for monoclonal Ig include a high or low serum globulin fraction, an abnormally low anion gap, unexplained hyponatremia, hypercalcemia, hypophosphatemia, or hyperphosphatemia, the Fanconi syndrome, distal renal tubular acidosis, a low high-density lipoprotein cholesterol, or nephrogenic diabetes insipidus.13 Complement levels are normal but may be low in cases of heavy chain or IgM deposition.14 Kidney imaging such as ultrasonography can be helpful in excluding obstruction but is of limited value in the diagnosis of monoclonal Ig-associated kidney failure, although patients with amyloid or plasma cell infiltration may have enlarged kidneys.
Myeloma is diagnosed when a serum monoclonal protein component is present (typically in excess of 3 g/dL), the fraction of bone marrow plasma cells is greater than 10% and there is evidence of end-organ injury, such as hypercalcemia, renal dysfunction, anemia, or bone disease. Patients with kidney damage from Ig deposition who have clonal plasma cells in their bone marrow are characterized as having symptomatic myeloma regardless of the size of the monoclonal protein or the percentage of bone marrow plasma cells.6
Many patients present with mild chronic kidney disease (CKD) and low levels of monoclonal Ig of unclear significance. In these cases a bone marrow aspirate and biopsy will sometimes show plasmacytosis consistent with myeloma and so provide sufficient grounds for treatment. Conventional cytogenetics, fluorescence in situ hybridization, and flow cytometry add additional prognostic information.6 If uncertainty remains, persistent or rising levels of monoclonal Ig combined with unexplained or worsening CKD may warrant kidney biopsy to document Ig deposition and provide a rationale for antiplasma cell therapy.
Mechanisms of kidney injury in plasma cell malignancies
Mechanisms of kidney injury in plasma cell malignancies can be broadly grouped into Ig-dependent and -independent categories, as shown in Table 1, though in particular patients several mechanisms often coexist and interact to produce kidney injury. As illustrated in Figure 1, the 3 most common forms of Ig-dependent kidney injury include: (1) cast nephropathy, in which casts and crystals composed of filtered monoclonal Ig and other urinary proteins obstruct distal renal tubules, often precipitously, and typically incite an accompanying tubulointerstitial nephritis; (2) AL amyloidosis, in which primarily monoclonal light chains and other proteins together form β-pleated sheets in the glomeruli; or (3) MIDD, in which intact or fragmented light chains, heavy chains, or both deposit along glomerular and/or tubular basement membranes.
Table 1.
Mechanisms of renal failure in plasma cell dyscrasias in Ig-dependent and -independent categories
| Ig-dependent mechanisms | |
|---|---|
| Mechanism | Details |
| Cast nephropathy (myeloma kidney) | Risk factors include light chain myeloma with > 10 g/day of monoclonal Ig excretion, IgD myeloma, volume depletion, sepsis, medications (see “Medication toxicity” below) |
| MIDD | Often associated with kappa light chains. Systemic syndrome may be present. |
| AL amyloidosis | Often associated with nephrotic-range albuminuria and lambda light chains. Systemic syndrome may be present. |
| Glomerulonephritis | Membranoproliferative, diffuse proliferative, crescentic, cryoglobulinemic all recognized |
| Tubulointerstitial nephritis | May also result from non-Ig mechanisms. |
| Minimal change or membranous glomerulopathy | Albuminuria is typically present, in addition to light chain proteinuria |
| Henoch-Scholein purpura/IgA nephropathy | Associated with IgA myeloma |
| Immunotactoid and fibrillary glomerulopathy | Rare conditions |
| Intracapillary monoclonal deposits of IgM thrombi | Associated with Waldenström macroglobulinemia |
| TMA | Paraprotein causes endothelial injury with resulting TMA |
| Hyperviscosity syndrome | Most common with Waldenström macroglobulinemia |
| Ig-independent mechanisms | |
|---|---|
| Mechanism | Details |
| Volume depletion or sepsis | Can cause acute tubular necrosis and/or precipitate cast nephropathy |
| Hypercalcemia | Can precipitate cast nephropathy |
| Tumor lysis syndrome | Uric acid or phosphate nephropathy |
| Medication toxicity | Zoledronate: acute renal failure |
| Pamidronate: collapsing focal segmental glomerulosclerosis | |
| Nonsteroidal anti-inflammatory drugs, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, loop diuretics, or IV contrast can precipitate cast nephropathy | |
| Direct parenchymal invasion by plasma cells | Associated with advanced or aggressive myeloma |
| Pyelonephritis | Immunodeficiency from myeloma, deficient Ig, and chemotherapy all contribute |
Ig indicates immunoglobulin; MIDD, monoclonal Ig deposition disease; TMA, thrombotic microangiopathy; and IV, intravenous.
Figure 1.
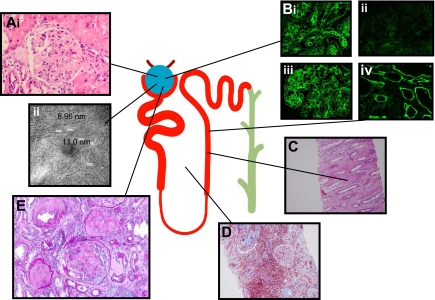
Three distinct syndromes account for most cases of Ig-mediated kidney disease but virtually all nephropathologic syndromes have been observed. Panel A shows amyloid. (i) Amyloid fibrils consisting of monoclonal Ig and serum proteins appear here as pink material disrupting glomeruli architecture. (ii) Amyloid is visible on electron microscopy as 7- to 12-nm fibrils. Panel B shows MIDD. Monoclonal light chains kappa (1) or without evidence of lambda (ii) and/or heavy chains (IgG), deposit along glomerular (iii) and tubular basement membranes (iv), altering the glomerular structure and causing dose-dependent proximal tubular toxicity. Panel C shows cast nephropathy. Filtered monoclonal Ig, Tamm-Horsfall, and other proteins form casts, which obstruct tubules and collecting ducts. Casts can rupture and result in interstitial inflammation. Panel D shows interstitial inflammation. Inflammation also results from the processing of filtered monoclonal light chains, which induces NF-κB and other signaling pathways leading to cytokine-mediated inflammatory infiltrate (shown here with a Trichrome stain) and subsequent matrix deposition and fibrosis. Panel E shows glomerular crescent. Virtually every recognized nephropathologic lesion has been described in association with paraproteinemia. Shown here is a glomerular crescent in a patient with Waldenström macroglobulinemia productive of IgMλ and amyloidosis.
It is important to note that the complete spectrum of renal disease associated with monoclonal Ig can be much broader than the 3 syndromes described in the paragraph above and includes nearly every renal pathologic entity. Glomerulonephritis may occur, of either a membranoproliferative, diffuse proliferative, crescentic, or cryoglobulinemic variety.15 Nephrotic syndrome may result from an Ig-induced minimal change or membranous lesion.16,17 Renal limited thrombotic microangiopathy can result directly from monoclonal Ig-induced endothelial injury or after chemotherapy or SCT.18 IgA myeloma can rarely result in Henoch-Schonlein purpura and IgA nephropathy.19 Patients with circulating monoclonal IgM can develop kidney injury from hyperviscosity or when deposits composed of monoclonal IgM occlude glomerular capillaries.20 Crystalline inclusions in the proximal tubule consisting of monoclonal Ig can result in a mild tubulointerstitial nephritis or the Fanconi syndrome, which is often indolent and may not require systemic therapy.21–23
Most myelomas secrete intact Ig with relatively small amounts of accompanying monoclonal light chain. However, myelomas that only secrete light chains account for approximately 20% of myeloma cases and cause 40% to 60% of severe acute kidney injury associated with the disease.6 Unsurprisingly, nonsecretory myeloma rarely causes kidney injury. Clinical experience teaches that renal dysfunction is inevitable in most patients over the course of the natural history of myeloma. Patients at particularly high risk are those with more than 10 g/day of light chain excretion and those with IgD myeloma, 70% and 100% of whom, respectively, will develop kidney injury.4 On occasion patients who do not meet the criteria for any of the monoclonal plasma cell disorders will develop MIDD as a result of a small, difficult to detect plasma cell clone producing a nephrotoxic monoclonal Ig.24
Several Ig-independent mechanisms commonly cause or contribute to kidney injury in plasma cell malignancy, including volume depletion, sepsis, pyelonephritis, hypercalcemia, uric acid nephropathy, rhabdomyolysis, direct renal parenchymal invasion by plasma cells, nonsteroidal anti-inflammatory drugs, and renin-angiotensin system inhibitors (Table 1).25 Patients with myeloma receiving the amino-bisphosphonate zoledronate have developed acute kidney injury, whereas others treated with its counterpart pamidronate have developed nephrotic syndrome from collapsing focal segmental glomerulosclerosis.26 In an autopsy series of 77 myeloma patients, acute tubular necrosis (possibly related to nephrotoxic light chains) was the single most common kidney lesion, followed by cast nephropathy, with several patients demonstrating MIDD or AL amyloidosis, which was unsuspected before death.18
Kidney biopsy should be considered early in the course of renal impairment, when the serum creatinine has risen no more than 25% to 30%, to provide a definitive diagnosis and distinguish between Ig- and non-Ig–mediated mechanisms. Special techniques such as pronase digestion and immunogold labeling may be required to detect and characterize monoclonal Ig and amyloid.27 In cast nephropathy, the dominant finding is tubular casts in the distal nephron, often with accompanying interstitial nephritis.18 In MIDD, tubular and glomerular basement membranes are thickened by refractile precipitates that are granular and dense on electron microscopy.28 Glomerular nodules resembling the Kimmelstiel-Wilson lesion of diabetic nephropathy may be present and cause the nephrotic syndrome. In AL amyloidosis, the tubular basement membranes are typically of normal thickness but the Congo red stain is positive, with characteristic green birefringence under polarizing microscopy. Electron microscopy demonstrates organized deposits of nonbranching amyloid fibrils, 7 to 10 nm in diameter.
Monoclonal Igs injure renal tissue through a diverse set of mechanisms. After filtration and clathrin-dependent endocytosis via the cubilin/megalin scavenger receptor system, light chains may resist degradation, precipitate, and cause proximal tubule dysfunction.29,30 Processing of pathologically large quantities of monoclonal light chains by proximal tubular cells may result in the production of proinflammatory cytokines such as interleukin-6 and interleukin-8, and monocyte chemoattractant protein-1.31,32 Light chain endocytosis and processing results in epithelial-mesenchymal transformation of tubular epithelial cells and catalyzes the production of hydrogen peroxide and other reactive oxygen species, further contributing to inflammatory cell infiltration, matrix deposition, and fibrosis.33 The proinflammatory cascade is mediated by mitogen-activated protein kinase (MAPK) and nuclear factor-κB (NF-κB) pathways.32,34
Light chains with a strong affinity for Tamm-Horsfall protein form casts that obstruct the flow of tubular fluid and may rupture the tubular epithelium leading to interstitial inflammation. MIDD cases are generally associated with kappa light chains of the 1, 3, or 4 subtype, which may be fragmented or abnormally large and may have atypical glycosylation or amino acid patterns that lead to misfolding, insolubility, and precipitation.35 In contrast, most Ig amyloid cases result from lambda light chains, particularly the lambda-6 subtype.36 Amino acid substitutions within the variable region of the amyloidogenic light chain mediate electrostatic aggregation with serum amyloid P protein, heparan sulfate proteoglycan and other substances, which results in a β-pleated sheet.37 Light chains from patients with AL amyloidosis undergo endocytosis at the glomerulus and subsequent delivery to lysosomes, where amyloid formation occurs, whereas those from patients with glomerular MIDD appear to induce a fibroblast phenotype in mesangial cells, which results in matrix deposition.38 Despite all that is known about the characteristics of pathogenic Ig, the risk for kidney injury in a particular patient with plasma cell malignancy cannot be reliably predicted by analyzing the monoclonal Ig present.
Detection of monoclonal Ig
The identification of monoclonal Ig in serum or urine is critical to the diagnosis of plasma cell malignancies. Protein electrophoresis is inexpensive but has relatively poor sensitivity for free light chains (FLCs) and cannot reliably differentiate monoclonal from polyclonal light chain expansion. Immunofixation is more sensitive than protein electrophoresis but does not quantify the amount of monoclonal Ig present and thus is of limited use in monitoring disease progression and response to treatment.6,39 The newer, nephelometric FLC immunoassay detects both monomers and dimers of kappa and lambda at concentrations less than 2 to 4 mg/L, without confounding from intact Ig.40 The FLC assay does not directly detect clonality, but suggests it through an increase or decrease in the kappa:lambda ratio. Kappa and lambda FLC levels may be elevated in patients with inflammatory diseases such as lupus and in those with CKD, but the kappa:lambda ratio is usually normal.39 In newly diagnosed myeloma, high serum FLC levels are associated with an increased risk of kidney injury.41 Among patients with MIDD, amyloid, or “nonsecretory” myeloma, in whom no monoclonal Ig has been identified with electrophoretic techniques, a substantial proportion will have an abnormal serum kappa:lambda ratio by the serum FLC assay.39,42 The short half-life of light chains and the quantitative nature of the serum FLC assay make it useful for monitoring the activity and response to therapy of light chain myeloma. The FLC assay is not without analytic pitfalls. When FLC quantities are very high, for example, the assay may yield paradoxically normal results because of the antigen excess, a problem common to nephelometric techniques.43 The use of the assay in urine is problematic because variability in the filtration and tubular handling of light chains have confounded attempts to define a normal range.44 Optimal strategies to combine the FLC assay with traditional techniques remain uncertain and at this juncture, the FLC assay complements rather than substitutes for traditional detection techniques.45
Management
When a patient with acute kidney injury and serum or urine monoclonal Ig presents, kidney biopsy data are typically not available and the relative contribution of Ig- and non-Ig–mediated mechanisms is uncertain. Because tubular injury is the most common underlying pathologic pattern, intravascular volume should be restored and hemodynamics optimized to ensure a steady flow of urine in non-oliguric patients if possible, avoiding the use of loop diuretics. Alkalinization of the urine is not of proven benefit and may increase the risk of metastatic calcium-phosphate deposition in the kidney and elsewhere, particularly if hypercalcemia or hyperphosphatemia are present, but repletion of bicarbonate may be necessary regardless if significant bicarbonate wasting is apparent. Hypercalcemia should be treated with intravenous saline and bisphosphonate therapy (dosed for impaired renal function). Allopurinol is effective for hyperuricemia, with rasburicase or hemodialysis reserved for uric acid levels in excess of 15 to 20 mg/dL. Nonsteroidal anti-inflammatory drugs and renin-angiotensin inhibitors must be avoided, and iodinated contrast used only if absolutely necessary, with accompanying prophylaxis. Basic medical management will correct modest degrees of renal impairment in a substantial fraction of incident patients. Additional management options are summarized in Table 2.
Table 2.
Selected therapies for plasma cell dyscrasias and accompanying renal failure
| Therapy | Basic mechanism of action | Regimen and comments | Citation data |
|---|---|---|---|
| Bortezomib | Causes apoptosis of immunoglobulin producing plasma cells and interferes with inflammatory pathways which contribute to renal failure. | Dose of 1 to 1.3 mg/m2 on days 1, 4, 8, and 11 for 21 to 28 day cycle, at median of 5 cycles, in combination with dexamethasone, thalidomide, or other agents. Dose does not need adjustment for renal failure. | Jagannath et al,57 Ostermann et al,62 Nozza et al,63 Chanan-Khan et al,58 Ludwig et al,59 Roussou et al,61 and Mohrbacher et al64 |
| Lenalidomide | Inhibits myeloma cell growth and induces apoptosis, interferes with myeloma cell-bone marrow interaction, down-regulates cytokines, up-regulates antimyeloma T-cell activity. | Patients with creatinine > 2.5 mg/dL excluded from phase 3 trials and myelosuppression is more common in renal failure. Use with caution when GFR is reduced, with dose reduction: GFR > 50 mL/min at 25 to 50 mg/day, 30 to 50 mL/min at 10 mg /day, <30 mL/min at 15 mg every other day. Dialysis patients at dose of 15 mg after each dialysis session only. | Dimopoulos et al,67 Niesvizky et al,92 and Borello et al93 |
| Thalidomide | Similar to lenalidomide. Thalidomide may be less potent inducer of apoptosis and T-cell proliferation, but a more potent antiangiogenic agent. | Associated with hyperkalemia in renal failure. Starting dose of 50 to 100 mg/day for GFR < 50 mL/min. | Harris et al68 |
| Dexamethasone | Induces apoptosis of myeloma cells through numerous mechanisms. | High dose necessary at 40 mg on days 1 to 4 and days 9 to 12. Response rates higher when used in combination with other agents. | Kastritis et al66 |
| Autologous SCT | High-dose melphalan conditioning eliminates myeloma cells. | Melphalan dose reduction (140 mg/m2) is required in renal failure and higher treatment related mortality is observed in SCT. Benefits unproven in renal failure. | Sirohi et al,74 Knudsen et al,75 Harousseau et al,76 and Jaccard et al77 |
| Plasmapheresis | Extracorporeal removal of nephrotoxic monoclonal Ig | Standard of care in many cases of IgM paraprotein. Usefulness in IgG-mediated disease remains uncertain. | Cserti et al,81 Clark et al,82 and Leung83 |
| Kidney transplantation | Alternative to dialysis for patients with end-stage renal disease. | Plasma cell dyscrasia must be in complete remission for 3 to 5 years with low and stable monoclonal Ig levels. Paraprotein deposition may recur in allograft. Immunosuppressive medications may increase risk of recurrence or progression of plasma cell dyscrasia. | Leung et al,87 Short et al,88 and Rostaing et al89 |
GFR indicates glomerular filtration rate; and SCT, stem cell transplantation.
Systemic therapy
Documentation or strong suspicion of renal deposition of monoclonal Ig requires prompt antiplasma cell therapy when renal function is impaired. Given the rapid progression and irreversible nature of monoclonal Ig-induced kidney injury, chemotherapeutic agents that act rapidly are preferred. Even dialysis-dependent patients benefit from systemic therapy, and a substantial minority of patients may experience long-term survival with reasonable quality of life.46 Although a comprehensive discussion of myeloma therapy is beyond the scope of this review, survival is improving as a result of novel agents, and those therapies that are particularly relevant to patients with kidney injury are discussed.47 In the future, new biomarkers of kidney injury may be helpful in the development of renoprotective, novel antiplasma cell agents.48
The reversible, first in class proteasome inhibitor bortezomib is a U.S. Food and Drug Administration–approved small molecule boronic acid–derived peptide that targets protein handling mediated by the ubiquitin proteasome pathway. Bortezomib has emerged along with high-dose dexamethasone as among the most effective approaches for treating myeloma when associated kidney injury is present. It is also now well established as therapy for relapsed myeloma and has recently received approval for initial therapy.49,50 Rapidly acting, it is characterized by a median time to best response of approximately 30 days in previously treated patients.49 As malignant plasma cells synthesize and assemble large quantities of Ig, they are particularly susceptible to proteasome inhibitors, which induce myeloma cell apoptosis in part by interfering with protein handling.51,52 Bortezomib also inhibits the NF-κB and MAPK pathways, which leads directly to myeloma cell apoptosis while also disrupting myeloma-stromal cell interactions and tumoral angiogenesis.53 Importantly, by inhibiting the NF-κB and MAPK pathways, bortezomib mitigates the inflammatory state induced in proximal tubule cells by excessive light chain handling and so may protect these cells from apoptosis by up-regulating heat shock and other survival-associated proteins.54,55 In contrast to traditional agents whose toxicity increases in renal impairment, the antimyeloma effects and safety profile of bortezomib appear unchanged in this setting, and renal dose adjustment is therefore not required.56–58 When combined in various regimens with dexamethasone, melphalan, doxorubicin, or thalidomide, 40% to 50% of patients who respond to therapy will experience significant recovery of renal function within 2 to 3 weeks.58–63 Improvement in renal function appears to precede the expected antiplasma cell effects of bortezomib, possibly reflecting anti-inflammatory properties of the agent.64 Bortezomib may also be useful for a range of other nephrologic conditions mediated by long-lived plasma cells, including antibody-mediated kidney allograft rejection, with studies ongoing in this regard.65
High-dose dexamethasone regimens also act rapidly and can have similarly dramatic success in reversing renal impairment.66 To improve efficacy of dexamethasone, it is often combined with thalidomide or its potent, newer derivative, lenalidomide, which interferes with myeloma cell growth, disrupts myeloma and bone marrow stromal cell interactions, down-regulates promyeloma cytokines, and up-regulates antimyeloma T-cell activity.67 Although the pharmacokinetics of thalidomide appear unaffected by renal function, hyperkalemia has been reported in the setting of renal dysfunction.68,69 Dose reduction is required with lenalidomide, as the drug's clearance falls significantly in advanced CKD.70 Importantly, patients with creatinine in excess of 2.5 mg/dL have been excluded from lenalidomide trials, and patients with lesser degrees of renal dysfunction experience more adverse events, particularly myelosuppression.71 Although further study is clearly necessary, clinical experience suggests that dose-reduced lenalidomide can be safely and effectively administered in the setting of renal impairment. Thalidomide, lenalidomide, and high-dose dexamethasone are associated with thromboembolic disease, which in turn may complicate their administration to patients with nephrotic syndrome and those receiving erythropoietin, both of which may also predispose to thrombosis.
Given that these novel agents have different mechanisms of action, their use in combination appears to result in synergistic antimyeloma effects, with some expected overlapping toxicity. Dexamethasone in combination with thalidomide is noncytotoxic and has proven particularly useful for high risk patients with renal failure who require significant cytoreduction before SCT.72 Bortezomib combined with thalidomide and dexamethasone (so-called VTD) and other agents in a tandem-transplant scheme has also proven superior to earlier combinations.73
Stem cell transplantation
SCT remains a mainstay of myeloma therapy and the availability of novel therapeutic approaches has enhanced its effectiveness while also prompting active research about its optimal timing and role.74 Patients with myeloma and renal failure can successfully receive SCT with an appropriately dose-reduced conditioning regimen, but toxicity is increased.75 Randomized trials have excluded patients whose serum creatinine exceeds approximately 2.3 mg/dL, and thus the benefits of SCT in patients with more significant renal failure are unproven.76 Autologous SCT has been used successfully in patients with Ig amyloid and MIDD, though treatment related mortality is high when systemic disease is present and in the case of amyloid, patient selection has been suggested as an explanation for the apparent advantage of SCT over conventional therapy.77 In addition, melphalan conditioning has been associated with acute kidney injury in patients with amyloid undergoing SCT.78 Although 90% of myeloma patients who undergo autologous SCT will eventually relapse, allogeneic SCT offers a potential cure because of the graft-versus-myeloma effect, with acceptable treatment related mortality when reduced intensity conditioning is used.79 Small numbers of patients with myeloma and end-stage kidney disease have successfully been treated with nonmyeloablative conditioning followed by simultaneous kidney and allogeneic SCT from an HLA-identical sibling, in some cases achieving complete remission of myeloma as well as stable kidney allograft function without a requirement for immunosuppression because immune cells from the allograft bone marrow do not reject a kidney from the same donor.80
Plasmapheresis
The value of plasma exchange in monoclonal Ig-associated kidney injury remains uncertain. The high volume of distribution of light chains and IgG results in low clearance relative to body stores, and rapid plasma refill occurs after each pheresis session.81 Initial clinical studies provided conflicting results and the largest randomized controlled trial of more than 90 patients showed no benefit of plasmapheresis compared with usual care.82 Kidney biopsy procedures were not required for entry into this latter study, however, and the high recovery rate (40%) in the control group suggests that many of the patients had kidney injury at least in part from Ig-independent mechanisms, thus obscuring the potential benefit of pheresis. An uncontrolled, retrospective analysis claimed a benefit to pheresis in the subset of patients with cast nephropathy whose light chain burden was reduced by more than 50%.83 Pheresis remains the standard of care in cases of hyperviscosity syndrome (seen with IgA or IgG3 substypes) or IgM immunoglobulin. A European-based randomized controlled trial of plasmapheresis in myeloma (MERIT, Myeloma Renal Impairment Trial; http://www.ncrn.org.uk/) ended enrollment in early 2009, and dialytic techniques to remove nephrotoxic light chain are also under study.84
Kidney transplantation
Myeloma appears to be more prevalent in dialysis patients than in the general population, possibly due to enrichment of the dialysis population with patients who have sustained myeloma-associated kidney failure.85 Kidney transplantation is occasionally contemplated as an alternative therapy to dialysis and yet multiple factors including the risk of myeloma recurrence and infection conspire against the success of transplantations in patients with plasma cell malignancies. The risk of monoclonal Ig-mediated allograft dysfunction among patients undergoing transplantation is low among patients who remain in remission if the original kidney lesion was cast nephropathy, but high among patients who had MIDD.86,87 Early, severe allograft dysfunction as a result of a monoclonal Ig-mediated necrotizing and crescentic glomerulonephritis has been reported.88 Despite the high prevalence of MGUS, there are only a handful of reported cases of kidney transplantation in such patients and concern remains that the progression to myeloma may accelerate in the context of maintenance immunosuppression.89
To be considered for kidney transplantation, most centers require that patients with myeloma achieve and maintain a durable remission, typically for 3 to 5 years. For all forms of plasma cell malignancy, including MGUS, monoclonal Ig levels must be low and stable before transplantation, Pretransplantation informed consent must address the risk of early graft loss from recurrent disease and the risk that transplant immunosuppression will accelerate the underlying malignancy or premalignant condition.86 Kidney transplantation is feasible in highly selected patients with MIDD and amyloid who achieve complete hematologic remission from SCT.90 Interestingly, both bortezomib and lenalidomide have been used successfully to treat kidney allograft MIDD, and with the impact of novel therapies in myeloma continuing to expand, the potential of newer combinations in this setting conferring benefit to patients is considerable.91
Conclusions
Plasma cell malignancies are commonly associated with kidney injury, often as a result of nephrotoxic monoclonal Ig. Traditional electrophoretic techniques remain the gold standard for identifying monoclonal Ig, whereas the serum FLC assay provides an additional tool for identifying and monitoring monoclonal Ig levels, particularly FLCs. Bortezomib, lenalidomide, and other agents appear to be more effective and selective for plasma cells and their microenvironment, with clear superiority now evident over traditional chemotherapy, and bortezomib appears to have a particular role in patients with myeloma-associated kidney injury. Autologous SCT remains a critical part of myeloma management but its use is limited in patients with kidney disease and its overall role will continue to evolve as systemic therapy improves. The value of plasma exchange for myeloma-associated kidney injury is an area of active research. Kidney transplantation is an option only in well-selected patients who have enjoyed prolonged remission and have low monoclonal Ig levels. Wider use of kidney biopsy to identify monoclonal protein deposition in patients with mild degrees of kidney dysfunction may be indicated as therapeutic options improve.
Acknowledgments
This study was supported in part by a grant from AstraZeneca (N.S.R.), a grant from Genzyme (B.D.H.), and grants from Celgene, Novartis, and Millennium (K.C.A.).
Authorship
Contribution: E.C.H. performed the initial literature search and wrote the initial manuscript; P.G.R. provided intense review and expertise and multiple other references; and N.B.G., T.R.S., N.S.R., B.D.H., and K.C.A. contributed knowledge, expertise, references, and editorial assistance with the manuscript.
Conflict-of-interest disclosure: N.S.R. reports receiving consulting/advisory board fees from Amgen, Celgene, and Novartis. K.C.A. reports receiving consulting/advisory board fees. P.G.R. reports receiving consulting/advisory board fees from Millennium, Celgene, and Johnson & Johnson. The remaining authors declare no competing financial interests.
Correspondence: Eliot C. Heher, Nephrology Division, Massachusetts General Hospital, 165 Cambridge St, Boston, MA 02114; e-mail: eheher@partners.org.
References
- 1.Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med. 2004;351(18):1860–1873. doi: 10.1056/NEJMra041875. [DOI] [PubMed] [Google Scholar]
- 2.Kyle RA, Therneau TM, Rajkumar SV, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med. 2006;354(13):1362–1369. doi: 10.1056/NEJMoa054494. [DOI] [PubMed] [Google Scholar]
- 3.Augustson BM, Begum G, Dunn JA, et al. Early mortality after diagnosis of multiple myeloma: analysis of patients entered onto the United Kingdom Medical Research Council trials between 1980 and 2002. Medical Research Council Adult Leukaemia Working Party. J Clin Oncol. 2005;23(36):9219–9226. doi: 10.1200/JCO.2005.03.2086. [DOI] [PubMed] [Google Scholar]
- 4.Knudsen LM, Hippe E, Hjorth M, Holmberg E, Westin J. Renal function in newly diagnosed multiple myeloma: a demographic study of 1353 patients. The Nordic Myeloma Study Group. Eur J Haematol. 1994;53(4):207–212. doi: 10.1111/j.1600-0609.1994.tb00190.x. [DOI] [PubMed] [Google Scholar]
- 5.Knudsen LM, Hjorth M, Hippe E. Renal failure in multiple myeloma: reversibility and impact on the prognosis. Nordic Myeloma Study Group. Eur J Haematol. 2000;65(3):175–181. doi: 10.1034/j.1600-0609.2000.90221.x. [DOI] [PubMed] [Google Scholar]
- 6.International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group [see comment]. Br J Haematol. 2003;121(5):749–757. [PubMed] [Google Scholar]
- 7.Drewinko B, Alexanian R, Boyer H, Barlogie B, Rubinow SI. The growth fraction of human myeloma cells. Blood. 1981;57(2):333–338. [PubMed] [Google Scholar]
- 8.Avet-Loiseau H, Attal M, Moreau P, et al. Genetic abnormalities and survival in multiple myeloma: the experience of the Intergroupe Francophone du Myelome. Blood. 2007;109(8):3489–3495. doi: 10.1182/blood-2006-08-040410. [DOI] [PubMed] [Google Scholar]
- 9.Jinushi M, Vanneman M, Munshi NC, et al. MHC class I chain-related protein A antibodies and shedding are associated with the progression of multiple myeloma. Proc Natl Acad Sci U S A. 2008;105(4):1285–1290. doi: 10.1073/pnas.0711293105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hideshima T, Mitsiades C, Tonon G, Richardson PG, Anderson KC. Understanding multiple myeloma pathogenesis in the bone marrow to identify new therapeutic targets. Nat Rev Cancer. 2007;7(8):585–598. doi: 10.1038/nrc2189. [DOI] [PubMed] [Google Scholar]
- 11.Kristinsson SY, Landgren O, Dickman PW, Derolf AR, Bjorkholm M. Patterns of survival in multiple myeloma: a population-based study of patients diagnosed in Sweden from 1973 to 2003. J Clin Oncol. 2007;25(15):1993–1999. doi: 10.1200/JCO.2006.09.0100. [DOI] [PubMed] [Google Scholar]
- 12.Pozzi C, D'Amico M, Fogazzi GB, et al. Light chain deposition disease with renal involvement: clinical characteristics and prognostic factors. Am J Kidney Dis. 2003;42(6):1154–1163. doi: 10.1053/j.ajkd.2003.08.040. [DOI] [PubMed] [Google Scholar]
- 13.Izzedine H, Camous L, Bourry E, Azar N, Leblond V, Deray G. The Case mid R: the case presentation. Kidney Int. 2007;72(8):1035–1036. doi: 10.1038/sj.ki.5002485. [DOI] [PubMed] [Google Scholar]
- 14.Soma J, Sato K, Sakuma T, et al. Immunoglobulin gamma3-heavy-chain deposition disease: report of a case and relationship with hypocomplementemia. Am J Kidney Dis. 2004;43(1):E10–E16. doi: 10.1053/j.ajkd.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 15.Nasr SH, Satoskar A, Markowitz GS, et al. Proliferative glomerulonephritis with monoclonal IgG deposits. J Am Soc Nephrol. 2009;20(9):2055–2064. doi: 10.1681/ASN.2009010110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanders PW, Herrera GA, Kirk KA, Old CW, Galla JH. Spectrum of glomerular and tubulointerstitial renal lesions associated with monotypical immunoglobulin light chain deposition. Lab Invest. 1991;64(4):527–537. [PubMed] [Google Scholar]
- 17.Komatsuda A, Masai R, Ohtani H, et al. Monoclonal immunoglobulin deposition disease associated with membranous features. Nephrol Dial Transplant. 2008;23(12):3888–3894. doi: 10.1093/ndt/gfn363. [DOI] [PubMed] [Google Scholar]
- 18.Herrera GA, Joseph L, Gu X, Hough A, Barlogie B. Renal pathologic spectrum in an autopsy series of patients with plasma cell dyscrasia. Arch Pathol Lab Med. 2004;128(8):875–879. doi: 10.5858/2004-128-875-RPSIAA. [DOI] [PubMed] [Google Scholar]
- 19.Zickerman AM, Allen AC, Talwar V, et al. IgA myeloma presenting as Henoch-Schonlein purpura with nephritis. Am J Kidney Dis. 2000;36(3):E19. doi: 10.1053/ajkd.2000.16221. [DOI] [PubMed] [Google Scholar]
- 20.Audard V, Georges B, Vanhille P, et al. Renal lesions associated with IgM-secreting monoclonal proliferations: revisiting the disease spectrum. Clin J Am Soc Nephrol. 2008;3(5):1339–1349. doi: 10.2215/CJN.01600408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herlitz LC, Roglieri J, Resta R, Bhagat G, Markowitz GS. Light chain proximal tubulopathy. Kidney Int. 2009;76(7):792–797. doi: 10.1038/ki.2008.666. [DOI] [PubMed] [Google Scholar]
- 22.Lacy MQ, Gertz MA. Acquired Fanconi's syndrome associated with monoclonal gammopathies. Hematol Oncol Clin North Am. 1999;13(6):1273–1280. doi: 10.1016/s0889-8588(05)70126-x. [DOI] [PubMed] [Google Scholar]
- 23.Gu X, Herrera GA. Light-chain-mediated acute tubular interstitial nephritis: a poorly recognized pattern of renal disease in patients with plasma cell dyscrasia. Arch Pathol Lab Med. 2006;130(2):165–169. doi: 10.5858/2006-130-165-LATINA. [DOI] [PubMed] [Google Scholar]
- 24.Merlini G, Stone MJ. Dangerous small B-cell clones. Blood. 2006;108(8):2520–2530. doi: 10.1182/blood-2006-03-001164. [DOI] [PubMed] [Google Scholar]
- 25.Rabb H, Gunasekaran H, Gunasekaran S, Saba SR. Acute renal failure from multiple myeloma precipitated by ACE inhibitors. Am J Kidney Dis. 1999;33(2):E5. doi: 10.1016/s0272-6386(99)70326-4. [DOI] [PubMed] [Google Scholar]
- 26.Markowitz GS, Fine PL, Stack JI, et al. Toxic acute tubular necrosis following treatment with zoledronate (Zometa). Kidney Int. 2003;64(1):281–289. doi: 10.1046/j.1523-1755.2003.00071.x. [DOI] [PubMed] [Google Scholar]
- 27.Nasr SH, Galgano SJ, Markowitz GS, Stokes MB, D'Agati VD. Immunofluorescence on pronase-digested paraffin sections: a valuable salvage technique for renal biopsies. Kidney Int. 2006;70(12):2148–2151. doi: 10.1038/sj.ki.5001990. [DOI] [PubMed] [Google Scholar]
- 28.Ronco PM, Alyanakian MA, Mougenot B, Aucouturier P. Light chain deposition disease: a model of glomerulosclerosis defined at the molecular level. J Am Soc Nephrol. 2001;12(7):1558–1565. doi: 10.1681/ASN.V1271558. [DOI] [PubMed] [Google Scholar]
- 29.Christensen EI, Birn H. Megalin and cubilin: synergistic endocytic receptors in renal proximal tubule. Am J Physiol Renal Physiol. 2001;280(4):F562–F573. doi: 10.1152/ajprenal.2001.280.4.F562. [DOI] [PubMed] [Google Scholar]
- 30.Sirac C, Bridoux F, Carrion C, et al. Role of the monoclonal kappa chain V domain and reversibility of renal damage in a transgenic model of acquired Fanconi syndrome. Blood. 2006;108(2):536–543. doi: 10.1182/blood-2005-11-4419. [DOI] [PubMed] [Google Scholar]
- 31.Kominami E, Tsukahara T, Bando Y, Katunuma N. Distribution of cathepsins B and H in rat tissues and peripheral blood cells. J Biochem. 1985;98(1):87–93. doi: 10.1093/oxfordjournals.jbchem.a135277. [DOI] [PubMed] [Google Scholar]
- 32.Sengul S, Zwizinski C, Simon EE, Kapasi A, Singhal PC, Batuman V. Endocytosis of light chains induces cytokines through activation of NF-kappaB in human proximal tubule cells. Kidney Int. 2002;62(6):1977–1988. doi: 10.1046/j.1523-1755.2002.00660.x. [DOI] [PubMed] [Google Scholar]
- 33.Wang PX, Sanders PW. Immunoglobulin light chains generate hydrogen peroxide. J Am Soc Nephrol. 2007;18(4):1239–1245. doi: 10.1681/ASN.2006111299. [DOI] [PubMed] [Google Scholar]
- 34.Sengul S, Zwizinski C, Batuman V. Role of MAPK pathways in light chain-induced cytokine production in human proximal tubule cells. Am J Physiol Renal Physiol. 2003;284(6):F1245–F1254. doi: 10.1152/ajprenal.00350.2002. [DOI] [PubMed] [Google Scholar]
- 35.Vidal R, Goni F, Stevens F, et al. Somatic mutations of the L12a gene in V-kappa(1) light chain deposition disease: potential effects on aberrant protein conformation and deposition. Am J Pathol. 1999;155(6):2009–2017. doi: 10.1016/s0002-9440(10)65520-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Solomon A, Frangione B, Franklin EC. Bence Jones proteins and light chains of immunoglobulins: preferential association of the V lambda VI subgroup of human light chains with amyloidosis AL (lambda). J Clin Invest. 1982;70(2):453–460. doi: 10.1172/JCI110635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hurle MR, Helms LR, Li L, Chan W, Wetzel R. A role for destabilizing amino acid replacements in light-chain amyloidosis. Proc Natl Acad Sci U S A. 1994;91(12):5446–5450. doi: 10.1073/pnas.91.12.5446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teng J, Russell WJ, Gu X, Cardelli J, Jones ML, Herrera GA. Different types of glomerulopathic light chains interact with mesangial cells using a common receptor but exhibit different intracellular trafficking patterns. Lab Invest. 2004;84(4):440–451. doi: 10.1038/labinvest.3700069. [DOI] [PubMed] [Google Scholar]
- 39.Katzmann JA, Clark RJ, Abraham RS, et al. Serum reference intervals and diagnostic ranges for free kappa and free lambda immunoglobulin light chains: relative sensitivity for detection of monoclonal light chains. Clin Chem. 2002;48(9):1437–1444. [PubMed] [Google Scholar]
- 40.Bradwell AR, Carr-Smith HD, Mead GP, et al. Highly sensitive, automated immunoassay for immunoglobulin free light chains in serum and urine. Clin Chem. 2001;47(4):673–680. [PubMed] [Google Scholar]
- 41.van Rhee F, Bolejack V, Hollmig K, et al. High serum-free light chain levels and their rapid reduction in response to therapy define an aggressive multiple myeloma subtype with poor prognosis. Blood. 2007;110(3):827–832. doi: 10.1182/blood-2007-01-067728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lachmann HJ, Gallimore R, Gillmore JD, et al. Outcome in systemic AL amyloidosis in relation to changes in concentration of circulating free immunoglobulin light chains following chemotherapy. Br J Haematol. 2003;122(1):78–84. doi: 10.1046/j.1365-2141.2003.04433.x. [DOI] [PubMed] [Google Scholar]
- 43.Daval S, Tridon A, Mazeron N, Ristori JM, Evrard B. Risk of antigen excess in serum free light chain measurements. Clin Chem. 2007;53(11):1985–1986. doi: 10.1373/clinchem.2007.093377. [DOI] [PubMed] [Google Scholar]
- 44.Hutchison CA, Harding S, Hewins P, et al. Quantitative assessment of serum and urinary polyclonal free light chains in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2008;3(6):1684–1690. doi: 10.2215/CJN.02290508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vermeersch P, Marien G, Bossuyt X. More studies are needed to assess the performance of serum free light chain measurement for the diagnosis of B-cell disorders in routine clinical practice. Br J Haematol. 2008;143(1):143–145. doi: 10.1111/j.1365-2141.2008.07308.x. author reply 143(1):145–146. [DOI] [PubMed] [Google Scholar]
- 46.Torra R, Blade J, Cases A, et al. Patients with multiple myeloma requiring long-term dialysis: presenting features, response to therapy, and outcome in a series of 20 cases. Br J Haematol. 1995;91(4):854–859. doi: 10.1111/j.1365-2141.1995.tb05400.x. [DOI] [PubMed] [Google Scholar]
- 47.Kumar SK, Rajkumar SV, Dispenzieri A, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood. 2008;111(5):2516–2520. doi: 10.1182/blood-2007-10-116129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dieterle F, Marrer E, Suzuki E, Grenet O, Cordier A, Vonderscher J. Monitoring kidney safety in drug development: emerging technologies and their implications. Curr Opin Drug Discov Devel. 2008;11(1):60–71. [PubMed] [Google Scholar]
- 49.Richardson PG, Sonneveld P, Schuster MW, et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005;352(24):2487–2498. doi: 10.1056/NEJMoa043445. [DOI] [PubMed] [Google Scholar]
- 50.San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med. 2008;359(9):906–917. doi: 10.1056/NEJMoa0801479. [DOI] [PubMed] [Google Scholar]
- 51.Meister S, Schubert U, Neubert K, et al. Extensive immunoglobulin production sensitizes myeloma cells for proteasome inhibition. Cancer Res. 2007;67(4):1783–1792. doi: 10.1158/0008-5472.CAN-06-2258. [DOI] [PubMed] [Google Scholar]
- 52.Bianchi G, Oliva L, Cascio P, et al. The proteasome load versus capacity balance determines apoptotic sensitivity of multiple myeloma cells to proteasome inhibition. Blood. 2009;113(13):3040–3049. doi: 10.1182/blood-2008-08-172734. [DOI] [PubMed] [Google Scholar]
- 53.Mitsiades CS, McMillin DW, Klippel S, et al. The role of the bone marrow microenvironment in the pathophysiology of myeloma and its significance in the development of more effective therapies. Hematol Oncol Clin North Am. 2007;21(6):1007–1034. vii–viii. doi: 10.1016/j.hoc.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 54.Hideshima T, Richardson P, Chauhan D, et al. The proteasome inhibitor PS-341 inhibits growth, induces apoptosis, and overcomes drug resistance in human multiple myeloma cells. Cancer Res. 2001;61(7):3071–3076. [PubMed] [Google Scholar]
- 55.Sarkozi R, Perco P, Hochegger K, et al. Bortezomib-induced survival signals and genes in human proximal tubular cells. J Pharmacol Exp Ther. 2008;327(3):645–656. doi: 10.1124/jpet.108.142604. [DOI] [PubMed] [Google Scholar]
- 56.San-Miguel JF, Richardson PG, Sonneveld P, et al. Efficacy and safety of bortezomib in patients with renal impairment: results from the APEX phase 3 study. Leukemia. 2008;22(4):842–849. doi: 10.1038/sj.leu.2405087. [DOI] [PubMed] [Google Scholar]
- 57.Jagannath S, Barlogie B, Berenson JR, et al. Bortezomib in recurrent and/or refractory multiple myeloma: initial clinical experience in patients with impared renal function. Cancer. 2005;103(6):1195–1200. doi: 10.1002/cncr.20888. [DOI] [PubMed] [Google Scholar]
- 58.Chanan-Khan AA, Kaufman JL, Mehta J, et al. Activity and safety of bortezomib in multiple myeloma patients with advanced renal failure: a multicenter retrospective study. Blood. 2007;109(6):2604–2606. doi: 10.1182/blood-2006-09-046409. [DOI] [PubMed] [Google Scholar]
- 59.Ludwig H, Drach J, Graf H, Lang A, Meran JG. Reversal of acute renal failure by bortezomib-based chemotherapy in patients with multiple myeloma. Haematologica. 2007;92(10):1411–1414. doi: 10.3324/haematol.11463. [DOI] [PubMed] [Google Scholar]
- 60.Ludwig H, Adam Z, Hajek R, et al. Recovery of renal impairment by bortezomib-doxorubicin-dexamethasone (BDD) in multiple myeloma (MM) patients with acute renal failure: results from an ongoing Phase II study [abstract]. ASH Annual Meeting Abstracts. 2007;110:3603. [Google Scholar]
- 61.Roussou M, Kastritis E, Migkou M, et al. Treatment of patients with multiple myeloma complicated by renal failure with bortezomib-based regimens. Leuk Lymphoma. 2008;49(5):890–895. doi: 10.1080/10428190801930506. [DOI] [PubMed] [Google Scholar]
- 62.Ostermann E, Schrattbauer K, Ludwig H, Graf H. Rapid recovery of kidney function in patients with multiple myeloma under bortezomib-combination therapy. [Accessed December 2009]. http://www.asn-online.org/education_and_meetings/renal_week/archives/
- 63.Nozza A, Siracusano L, Armando S. Bortezomib-dexamethasone combination in a patient with refractory multiple myeloma and impaired renal function. Clin Ther. 2006;28(6):953–959. doi: 10.1016/j.clinthera.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 64.Mohrbacher A, Levine AM. Reversal of advanced renal dysfunction on bortezomib treatment in multiple myeloma patients 2005 ASCO Annual Meeting Proceedings. J Clin Oncol. 2005;23:6714. (16S, part I of II; June 1 suppl) [Google Scholar]
- 65.Perry DK, Burns JM, Pollinger HS, et al. Proteasome inhibition causes apoptosis of normal human plasma cells preventing alloantibody production. Am J Transplant. 2009;9(1):201–209. doi: 10.1111/j.1600-6143.2008.02461.x. [DOI] [PubMed] [Google Scholar]
- 66.Kastritis E, Anagnostopoulos A, Roussou M, et al. Reversibility of renal failure in newly diagnosed multiple myeloma patients treated with high dose dexamethasone-containing regimens and the impact of novel agents. Haematologica. 2007;92(4):546–549. doi: 10.3324/haematol.10759. [DOI] [PubMed] [Google Scholar]
- 67.Dimopoulos MA, Kastritis E, Rajkumar SV. Treatment of plasma cell dyscrasias with lenalidomide. Leukemia. 2008;22(7):1343–1353. doi: 10.1038/leu.2008.123. [DOI] [PubMed] [Google Scholar]
- 68.Harris E, Behrens J, Samson D, Rahemtulla A, Russell NH, Byrne JL. Use of thalidomide in patients with myeloma and renal failure may be associated with unexplained hyperkalaemia. Br J Haematol. 2003;122(1):160–161. doi: 10.1046/j.1365-2141.2003.04395_2.x. [DOI] [PubMed] [Google Scholar]
- 69.Eriksson T, Hoglund P, Turesson I, et al. Pharmacokinetics of thalidomide in patients with impaired renal function and while on and off dialysis. J Pharm Pharmacol. 2003;55(12):1701–1706. doi: 10.1211/0022357022241. [DOI] [PubMed] [Google Scholar]
- 70.Stevens FJ, Myatt EA, Chang CH, et al. A molecular model for self-assembly of amyloid fibrils: immunoglobulin light chains. Biochemistry. 1995;34(34):10697–10702. doi: 10.1021/bi00034a001. [DOI] [PubMed] [Google Scholar]
- 71.Niesvizky R, Naib T, Christos PJ, et al. Lenalidomide-induced myelosuppression is associated with renal dysfunction: adverse events evaluation of treatment-naive patients undergoing front-line lenalidomide and dexamethasone therapy. Br J Haematol. 2007;138(5):640–643. doi: 10.1111/j.1365-2141.2007.06698.x. [DOI] [PubMed] [Google Scholar]
- 72.Barlogie B, Shaughnessy J, Tricot G, et al. Treatment of multiple myeloma. Blood. 2004;103(1):20–32. doi: 10.1182/blood-2003-04-1045. [DOI] [PubMed] [Google Scholar]
- 73.Pineda-Roman M, Zangari M, Haessler J, et al. Sustained complete remissions in multiple myeloma linked to bortezomib in total therapy 3: comparison with total therapy 2. Br J Haematol. 2008;140(6):625–634. doi: 10.1111/j.1365-2141.2007.06921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sirohi B, Powles R, Harousseau JL, Anderson KC. The evolving background for high-dose treatment for myeloma. Bone Marrow Transplant. 2007;40(12):1097–1100. doi: 10.1038/sj.bmt.1705867. [DOI] [PubMed] [Google Scholar]
- 75.Knudsen LM, Nielsen B, Gimsing P, Geisler C. Autologous stem cell transplantation in multiple myeloma: outcome in patients with renal failure. Eur J Haematol. 2005;75(1):27–33. doi: 10.1111/j.1600-0609.2005.00446.x. [DOI] [PubMed] [Google Scholar]
- 76.Harousseau JL, Moreau P. Autologous hematopoietic stem-cell transplantation for multiple myeloma. N Engl J Med. 2009;360(25):2645–2654. doi: 10.1056/NEJMct0805626. [DOI] [PubMed] [Google Scholar]
- 77.Jaccard A, Moreau P, Leblond V, et al. High-dose melphalan versus melphalan plus dexamethasone for AL amyloidosis. N Engl J Med. 2007;357(11):1083–1093. doi: 10.1056/NEJMoa070484. [DOI] [PubMed] [Google Scholar]
- 78.Leung N, Slezak JM, Bergstralh EJ, et al. Acute renal insufficiency after high-dose melphalan in patients with primary systemic amyloidosis during stem cell transplantation. Am J Kidney Dis. 2005;45(1):102–111. doi: 10.1053/j.ajkd.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 79.Bruno B, Rotta M, Patriarca F, et al. A comparison of allografting with autografting for newly diagnosed myeloma. N Engl J Med. 2007;356(11):1110–1120. doi: 10.1056/NEJMoa065464. [DOI] [PubMed] [Google Scholar]
- 80.Fudaba Y, Spitzer TR, Shaffer J, et al. Myeloma responses and tolerance following combined kidney and nonmyeloablative marrow transplantation: in vivo and in vitro analyses. Am J Transplant. 2006;6(9):2121–2133. doi: 10.1111/j.1600-6143.2006.01434.x. [DOI] [PubMed] [Google Scholar]
- 81.Cserti C, Haspel R, Stowell C, Dzik W. Light-chain removal by plasmapheresis in myeloma-associated renal failure. Transfusion. 2007;47(3):511–514. doi: 10.1111/j.1537-2995.2006.01143.x. [DOI] [PubMed] [Google Scholar]
- 82.Clark WF, Stewart AK, Rock GA, et al. Plasma exchange when myeloma presents as acute renal failure: a randomized, controlled trial. Ann Intern Med. 2005;143(11):777–784. doi: 10.7326/0003-4819-143-11-200512060-00005. [DOI] [PubMed] [Google Scholar]
- 83.Leung N, Gertz MA, Zeldenrust SR, et al. Improvement of cast nephropathy with plasma exchange depends on the diagnosis and on reduction of serum free light chains. Kidney Int. 2008;73(11):1282–1288. doi: 10.1038/ki.2008.108. [DOI] [PubMed] [Google Scholar]
- 84.Hutchison CA, Cook M, Heyne N, et al. European trial of free light chain removal by extended hemodialysis in cast nephropathy (EuLITE): a randomised control trial. Trials. 2008;9:55. doi: 10.1186/1745-6215-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Maisonneuve P, Agodoa L, Gellert R, et al. Cancer in patients on dialysis for end-stage renal disease: an international collaborative study. Lancet. 1999;354(9173):93–99. doi: 10.1016/s0140-6736(99)06154-1. [DOI] [PubMed] [Google Scholar]
- 86.Heher EC, Spitzer TR, Goes NB. Light chains: heavy burden in kidney transplantation. Transplantation. 2009;87(7):947–952. doi: 10.1097/TP.0b013e31819b9977. [DOI] [PubMed] [Google Scholar]
- 87.Leung N, Lager DJ, Gertz MA, Wilson K, Kanakiriya S, Fervenza FC. Long-term outcome of renal transplantation in light-chain deposition disease. Am J Kidney Dis. 2004;43(1):147–153. doi: 10.1053/j.ajkd.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 88.Short AK, O'Donoghue DJ, Riad HN, Short CD, Roberts IS. Recurrence of light chain nephropathy in a renal allograft: a case report and review of the literature. Am J Nephrol. 2001;21(3):237–240. doi: 10.1159/000046254. [DOI] [PubMed] [Google Scholar]
- 89.Rostaing L, Modesto A, Abbal M, Durand D. Long-term follow-up of monoclonal gammopathy of undetermined significance in transplant patients. Am J Nephrol. 1994;14(3):187–191. doi: 10.1159/000168712. [DOI] [PubMed] [Google Scholar]
- 90.Leung N, Griffin MD, Dispenzieri A, et al. Living donor kidney and autologous stem cell transplantation for primary systemic amyloidosis (AL) with predominant renal involvement. Am J Transplant. 2005;5(7):1660–1670. doi: 10.1111/j.1600-6143.2005.00920.x. [DOI] [PubMed] [Google Scholar]
- 91.Richardson PG, Mitsiades C, Schlossman R, Munshi N, Anderson K. New drugs for myeloma. Oncologist. 2007;12(6):664–689. doi: 10.1634/theoncologist.12-6-664. [DOI] [PubMed] [Google Scholar]
- 92.Niesvizky R, Jayabalan DS, Christos PJ, et al. BiRD (Biaxin [clarithromycin]/Revlimid [lenalidomide]/dexamethasone) combination therapy results in high complete- and overall-response rates in treatment-naive symptomatic multiple myeloma. Blood. 2008;111(3):1101–1109. doi: 10.1182/blood-2007-05-090258. [DOI] [PubMed] [Google Scholar]
- 93.Borrello I. Lenalidomide in renal insufficiency: balancing the risks and benefits. Br J Haematol. 2009;144(3):446–447. doi: 10.1111/j.1365-2141.2008.07002.x. author reply, 144(3):447–448. [DOI] [PMC free article] [PubMed] [Google Scholar]