Abstract
Background Higher waist circumference and lower hip circumference are both associated with increased cardiovascular disease (CVD) risk, despite being directly correlated. The real effects of visceral obesity may therefore be underestimated when hip circumference is not fully taken into account. We hypothesized that adding waist and hip circumference to traditional risk factors would significantly improve CVD risk prediction.
Methods In a population-based survey among South Asian and African Mauritians (n = 7978), 1241 deaths occurred during 15 years of follow-up. In a model that included variables used in previous CVD risk calculations (a Framingham-type model), the association between waist circumference and mortality was examined before and after adjustment for hip circumference. The percentage with an increase in estimated 10-year cumulative mortality of >25% and a decrease of >20% after waist and hip circumference were added to the model was calculated.
Results Waist circumference was strongly related to mortality only after adjustment for hip circumference and vice versa. Adding waist and hip circumference to a Framingham-type model increased estimated 10-year cumulative CVD mortality by >25% for 23.7% of those who died and 15.7% of those censored. Cumulative mortality decreased by >20% for 4.5% of those who died and 14.8% of those censored.
Conclusions The effect of central obesity on mortality risk is seriously underestimated without adjustment for hip circumference. Adding waist and hip circumference to a Framingham-type model for CVD mortality substantially increased predictive power. Both may be important inclusions in CVD risk prediction models.
Keywords: Waist circumference, hip circumference, obesity, mortality, South Asian, African
Introduction
The epidemic levels of overweight and obesity observed in most developed countries are now being seen in developing countries due to urbanization and westernization. Obesity is an acknowledged risk factor both for all-cause and cardiovascular disease (CVD) mortality1–11 but is not included in most CVD risk models because body mass index (BMI) and waist circumference have not sufficiently improved the predictive properties of such equations.12–17
Hip circumference, although directly correlated with waist circumference (and BMI), has been shown to be inversely associated with blood glucose, blood pressure and lipids.18 It is also associated with reduced risk of CVDs,19–22 all-cause23,24 and cardiovascular mortality,19,25 particularly when adjusted for waist circumference.21,23,26
This difference between the adverse effects of elevated waist circumference on the one hand and the protective effects of hip circumference on the other may be due to the observation that most of the pathological influence of adiposity is due to visceral, rather than superficial, fat.27 Waist circumference is increased by increasing superficial fat, and failing to account for this may underestimate the real effects of visceral obesity. The waist-to-hip ratio attempts to do this, but assumes that this can be achieved by a simple ratio. Furthermore, a specific protective role of gluteofemoral body fat via the regulation of fatty acid release and uptake and a beneficial adipokine profile is also now being recognised.28 By improving the assessment of adiposity, we may be able to improve CVD risk prediction. We therefore hypothesized that adding waist and hip circumference to traditional risk factors would significantly improve CVD risk prediction.
We report here on the relationship between central obesity, hip circumference and mortality in a population-based cohort of almost 10 000 African and ethnically South Asian individuals from Mauritius, with measured height, weight, waist and hip circumference at studies in 1987, 1992 and 1998 and an average of 15 years of mortality follow-up.
Methods and procedures
Mauritius is an Indian Ocean island ∼800 km from Madagascar. The population is largely of South Asian Indian (68%) and African (Creole) (27%) origin. African Mauritians are of mixed East African and Malagasy ancestry (Malagasy ancestry being both Malay and East African), with some European and Indian admixture. The South Asian population are mostly of Bihari origin (North-West India).
A population-based survey was conducted in Mauritius, with measurements taken in 1987, 1992 and 1998, details of which were published previously.29–32 In 1987, 10 randomly selected clusters and a purposely selected area of Chinatown in the capital city, Port Louis, were surveyed. In 1992 and 1998, previous participants were re-surveyed, along with any new eligible residents of the 10 clusters. Three additional clusters were added in 1992 and re-surveyed in 1998. All individuals aged ≥25 years (1987 and 1992) or ≥20 years (1998) were tested. A total of 8932 individuals (71% Asian Indian, 29% African ancestry), participated in the three surveys [excluding Chinese individuals (n = 626) who were removed from this analysis]. Sixty percent participated in more than one survey and 28% in all three surveys. Response for each survey was >85%.30 Informed written consent was obtained from all participants. The mortality follow-up protocol was reviewed and approved by the local ethics committee (Ministry of Health and Quality of life, Mauritius). The 1987, 1992 and 1998 surveys were additionally approved by the ethics committee of the International Diabetes Institute (Melbourne, Australia).
Mortality follow-up was conducted between 1 April and 30 October 2007. Contact with participants (or their next of kin, other household members or neighbours when participants were not contactable) was used to determine vital and migration status. National death registries were also used to verify vital status and cause of death. Identity was validated using name, age, address, ethnicity, number of children and occupation from previous surveys. Where possible, death certificates or certified extracts of the certificate were inspected and cause of death noted.
Individuals were followed from the date of the first interview. Participants whose vital status was unknown, but who contributed some follow-up time were censored at the date of last contact (n = 333). Participants not contributing any follow-up time (attended one survey and then were lost) were excluded from all mortality analyses (n = 409), as were those with a history of prior CVD or lower limb amputation (n = 545). Vital status was established for a total of 7978 participants.
Measurements at each survey were conducted according to identical protocols, except where stated. A 75-g oral glucose-tolerance test was performed on all non-pregnant participants, except those taking insulin or oral hypoglycaemic drugs. Biochemical measurements, height, weight and blood pressure were measured as previously described.29,30,33 Hip circumference was measured as the maximum circumference at the level of the buttocks. Waist circumference was measured as the minimum circumference, in the horizontal plane, between the xiphisternum and umbilicus in 1987 and as the circumference at the mid-point between the iliac crest and the lower margin of the ribs in 1992 and 1998.34 Mean waist circumference measured at the mid-point between the ribs and the iliac crest has been shown to be higher (1.5 cm in men, 2.7 cm in women) than at the narrowest waist.35 Therefore, 1987 waist circumference values were increased accordingly. Obesity (as a dichotomous variable) was classified using recommended Asian waist circumference cut-points (≥80 cm in women and ≥90 cm in men) for the South Asian population.36 Information about smoking status, ethnicity, treatment for hypertension and previous CVD or amputation was collected by interviewer-administered questionnaire. Treatment for hypercholesterolaemia was not assessed in this study.
Consideration of the use of the words ‘confounding’ and ‘effect-measure modification’ in this study were based on the definitions of Rothman and Greenland.37 They describe a confounder as being a variable that: (i) is a risk factor for the disease; (ii) is associated with the exposure (waist circumference in this study); and (iii) is not in the causal pathway between the exposure and the disease. ‘Effect-measure modification’ refers to variation in the magnitude of a measure of exposure effect across levels of another variable. The variable across which the effect measure varies is called an effect modifier.
Statistical analyses
We used a proportional hazard model (Cox model), with current age as the underlying time scale for analysis of all-cause and CVD mortality. Entry date was the date of each participant's first survey, exit date the date of last contact, emigration or death. Explanatory variables (unless otherwise stated) were based on those used previously to investigate reclassification of risk in the Framingham Heart Study and included age, sex, total cholesterol, high-density lipoprotein (HDL) cholesterol, systolic blood pressure, diabetes mellitus, blood pressure treatment and smoking, updated on up to two occasions during the study period in addition to the baseline assessment.38 For the relationship between mortality and each of waist and hip circumference, we used natural splines with four parameters each, with knots chosen so that the number of deaths was the same between knots. Scatter plots of waist vs hip circumference were overlaid with a contour plot of the estimated hazard ratio for death (relative to a reference individual of waist 85 cm and hip 95 cm) to illustrate the joint effect of waist and hip. The linearity of the effects was tested by replacing the natural splines by a linear function, and the interaction between waist and hip circumference was tested by adding the product or the ratio of the variables to the model. All tests were likelihood ratio tests, using the χ2 approximation. We computed the 10-year cumulative mortality using models with and without waist and hip, and compared changes for persons with and without an event. We computed the fraction of the sample where cumulative mortality was increased by >25% and decreased by >20% (these values being equidistant on a relative scale: 1.25/1 = 1/0.8), separately for those with and without an event. We also plotted the cumulative mortality rates in the two models to provide a graphical impression of the improvement. Finally, we plotted the observed and the mean predicted estimated cumulative CVD mortality (a calibration plot for improvement of the model upon the addition of waist and hip circumference) in deciles of estimated cumulative mortality, as well as a smoothed version of this using a spline model in logistic regression. Analysis was conducted using R 2.11.1.39 Separate analyses were conducted for men and women, Africans and South Asians.
Results
Over a median follow-up period of 15.1 years (maximum of 20.5 years), 1241 deaths occurred (56% in men, 68% in South Asians), with 703 (56.6%) of these being attributable to CVD. Death certificates or certified extracts were obtained for 927/1241 deceased participants. Where these were not available, the cause of death was preferentially derived from adjudication of hospital files (n = 192) or next of kin (n = 100). No information on cause of death was available for 22 participants. World Health Organization International Classification of Diseases codes were not available on certificates, and rarely in hospital data. We therefore classified cause of death into 11 groups: cardiac (n = 442, 35.6%); cerebrovascular (n = 185, 14.9%); cancer (n = 165, 13.3%); trauma (n = 53, 4.3%); diabetes (n = 22, 1.8%); respiratory disease (n = 86, 6.9%); hypertension (n = 6, 0.5%); renal failure (n = 70, 5.6%); gastrointestinal/hepatic/alcohol (n = 78, 6.3%); other (n = 68, 5.5%); and not known (n = 37, 3.0%). CVD mortality included deaths categorized as cardiac, cerebrovascular, hypertension and renal failure. Cause of death from death extract or death certificate was adjudicated by a cardiologist (S.S.) for ∼19% of deaths using hospital records. Percentage agreement was 63%.
Those who died from CVD or other causes were older and had higher levels of waist circumference and waist-to-hip ratio than survivors at study entry (Table 1). Hip circumference was positively correlated with waist circumference (r = 0.76). Diabetes prevalence was 13.0% in 1987, 17.8% in 1992 and 23.3% in 1998 in this cohort.
Table 1.
Characteristics of the cohort according to vital status and cause of deatha
| CVD deaths | Non-CVD deaths | Survivors | |
|---|---|---|---|
| N | 703 | 538 | 6737 |
| Age | 57 (47.9–63.9) | 54.6 (42.7–63.1) | 36.8 (30.1–46.9) |
| Women (%) | 43.4 (39.7–47.1) | 43.7 (39.5–47.9) | 56.6 (55.4–57.8) |
| Indian (%) | 71.1 (67.8–74.5) | 63.4 (59.3–67.5) | 71.5 (70.4–72.5) |
| Creole (%) | 28.9 (25.5–32.2) | 36.6 (32.5–40.7) | 28.5 (27.5–29.6) |
| Smokers (%) | 39.4 (35.8–43) | 42.5 (38.3–46.7) | 25.6 (24.6–26.7) |
| Education (secondary or higher) (%) | 12.1 (9.7–14.5) | 15.1 (12.1–18.2) | 39.2 (38–40.3) |
| Waist circumference | 84 (75–90.5) | 81 (72.7–89.5) | 79.5 (71.8–87) |
| Hip circumference | 92 (85–98) | 89 (83–97) | 92.5 (87–98.5) |
| Waist-to-hip ratio | 0.9 (0.84–0.94) | 0.88 (0.84–0.93) | 0.85 (0.79–0.9) |
| BMI (kg/m2) | 24 (21–27.4) | 23 (19.7–26.9) | 23.7 (20.8–26.7) |
| Fasting plasma glucose (mmol/l) | 5.9 (5.2–8.0) | 5.6 (5.1–6.4) | 5.2 (4.9–5.7) |
| 2 hour plasma glucose (mmol/l) | 7.5 (6.0–10.8) | 7.0 (5.6–9.2) | 6.3 (5.3–7.5) |
| HDL cholesterol (mmol/l) | 1.2 (1.0–1.5) | 1.3 (1.1–1.5) | 1.2 (1.0–1.4) |
| Total cholesterol (mmol/l) | 5.5 (4.6–6.4) | 5.3 (4.5–6.2) | 4.9 (4.2–5.8) |
| Systolic blood pressure (mmHg) | 135 (121–155) | 129 (117–143) | 119 (109–130) |
| Diastolic blood pressure (mmHg) | 82 (73–91) | 79 (71–86) | 73 (66–82) |
aData are medians (inter-quartile range) or percentage (95% confidence interval).
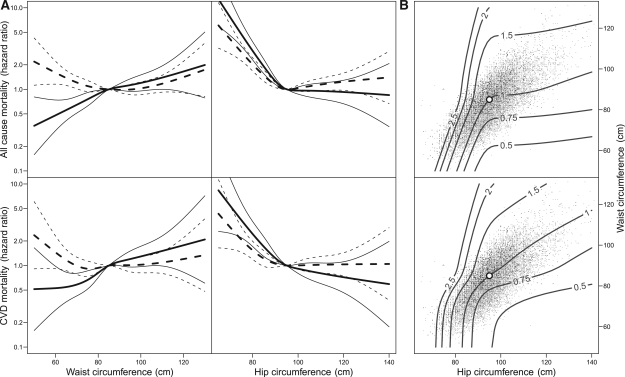
Before adjustment for hip circumference, no association was seen between waist circumference and CVD (P = 0.28) or all-cause mortality (P = 0.85) in a model also containing those variables used in risk prediction models based on the Framingham Heart Study (age, sex, total cholesterol, HDL cholesterol, systolic blood pressure, diabetes mellitus, blood pressure treatment and cigarette smoking). After additional adjustment for hip circumference, a strong and graded relationship with both all-cause and CVD mortality was seen for waist circumference (Figure 1, with sex- and ethnicity-specific results presented in Figures 2 and 3 and Supplementary Figures S1–S6 available as Supplementary Data at IJE online). Similarly, a strong negative relationship between hip circumference and both CVD and all-cause mortality was only observed once adjusted for waist circumference (Figure 1). The risk of death from both CVD and all causes was influenced by both waist circumference and hip circumference. The hazard ratio for CVD death in a fully adjusted model was 1.31 per standard deviation (SD) of waist circumference and 0.72 per SD of hip circumference (both P < 0.0001). Findings were unchanged when those with diabetes were excluded, and in subgroup analysis of those with either diabetes, impaired fasting glucose or impaired glucose tolerance or those with none of these conditions (results not shown). For men only, we found a non-linear relationship between waist circumference and all-cause and CVD mortality (in both ethnic groups, P < 0.05). A J-shaped relationship was apparent with increasing risk of death for greater waist circumference only >75 cm.
Figure 1.
(A) Hazard ratio and 95% confidence interval for all-cause and CVD mortality according to waist and hip circumference with (solid lines) and without (broken lines) adjustment for each other. (B) Contours of rate ratios for the joint effect of waist and hip circumference on all-cause and CVD death (relative to a reference individual of waist 85 cm and hip 95 cm). Waist circumference is plotted against hip circumference for persons with events (grey) and persons without events (black)
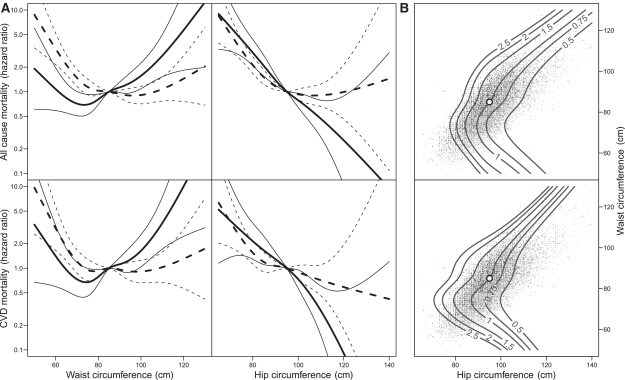
Figure 2.
(A) Hazard ratio and 95% confidence interval for all-cause and CVD mortality in Mauritian men accoding to waist and hip circumference with (solid lines) and without (broken lines) adjustment for each other. (B) Contours of rate ratios for the joint effect of waist and hip circumference on all-cause and CVD death in Mauritian men (relative to a reference individual of waist 85 cm and hip 95 cm). Waist circumference is plotted against hip circumference for persons with events (grey) and persons without events (black)
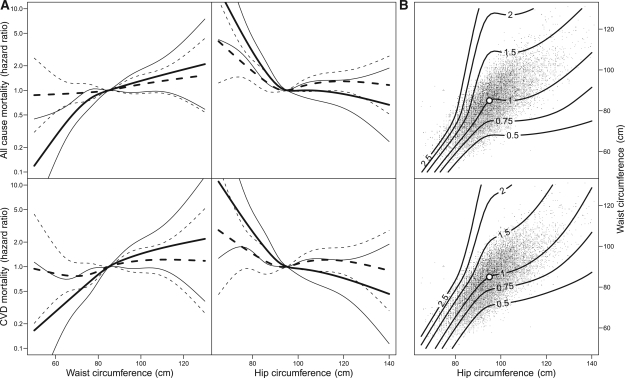
Figure 3.
(A) Hazard ratio and 95% confidence interval for all-cause and CVD mortality in Mauritian women according to waist and hip circumference with (solid lines) and without (broken lines) adjustment for each other. (B) Contours of rate ratios for the joint effect of waist and hip circumference on all-cause and CVD death in Mauritian women (relative to a reference individual of waist 85 cm and hip 95 cm). Waist circumference is plotted against hip circumference for persons with events (grey) and persons without events (black)
We tested whether the relationship of each of waist and hip circumference with mortality could be equally well described by linear effects, which was not the case (P-value for the addition of non-linear terms to a model with linear terms <0.0001 for all-cause and P = 0.026 for CVD mortality). In addition, we tested whether either waist or hip could be omitted from the model, which was strongly rejected (P-value for the addition of the second term <0.002 for both variables and both outcomes). Neither the inclusion of waist-to-hip ratio (P = 0.242 for all-cause; P = 0.171 for CVD) nor the product of waist and hip circumference [P = 0.08 (all-cause) and P = 0.083 (CVD)] improved the model with non-linear terms of waist and hip circumference. We tested whether waist-to-hip ratio could replace the non-linear waist and hip circumference terms and this was also strongly rejected (for the addition of waist and hip terms to a model containing waist-to-hip ratio, P < 0.0001 for all-cause; P = 0.010 for CVD). Finally, the effect on the relationship of waist circumference and CVD mortality upon the addition to the model of height rather than hip circumference was estimated, with waist circumference remaining non-significant following the addition of height (P = 0.26).
To assess change in predictive power of a Framingham-type model upon the addition of waist and hip circumference, estimated 10-year cumulative CVD mortality was calculated for the base model, and for an extended model including non-linear terms of waist and hip circumference. These were plotted against each other separately for those with and without an event (Supplementary Figure S7 available as Supplementary Data at IJE online) with the figure also including the quartiles, 10th and 90th centiles of the distributions. This figure shows that adding waist and hip circumference decreased the estimated cumulative CVD mortality in those without events, and increased it for those who died, thereby increasing predictive power. A calibration plot of observed and predicted 10-year cumulative CVD mortality risk for these two models (Supplementary Figure S8 available as Supplementary Data at IJE online) shows improvement in model fit upon the addition of waist and hip circumference.
Of those who died from cardiovascular causes, 23.7% had an increase in estimated risk >25% upon the addition of waist and hip circumference to the model, whereas 4.5% had a decrease in estimated risk of >20% (Table 2). Estimated mortality risk increased for two-thirds of those who died from CVD upon addition of waist and hip to the model. For those who were censored (i.e. remained alive or died of a non-CVD cause), the percentage whose estimated risk increased by >25% and the percentage whose estimated risk decreased by >20% was similar, at ∼15%. A similar pattern was observed for all-cause mortality.
Table 2.
Percentage of individuals whose estimated 10-year cumulative mortality risk increased (by 0–25% and by >25%) or decreased (by 0–20% and by >20%) following the addition of waist and hip circumference to a base Framingham-type model for all-cause and CVD death, stratified by whether they actually died or were censored during the study period
| All-cause mortality |
CVD mortality |
|||
|---|---|---|---|---|
| Change in risk | Censored | Dead | Censored | Dead |
| >20% reduction | 17.2 | 7.0 | 14.8 | 4.5 |
| 0–20% reduction | 41.9 | 35.3 | 36.3 | 31.7 |
| 0–25% increase | 24.0 | 29.1 | 33.2 | 40.1 |
| >25% increase | 16.9 | 28.6 | 15.7 | 23.7 |
| Total | 100.0 | 100.0 | 100.0 | 100.0 |
Using the same Framingham-type model in the South Asian population only, those above the recommended Asian waist circumference cut-points for obesity (80 cm in women, 90 cm in men) had a hip-adjusted risk of CVD death 1.8 [95% confidence interval (CI) 1.2–2.7] times greater in women and 1.5 (95% CI 1.1–2.2) times greater in men, compared with those below the obesity cut-point. Before the inclusion of hip circumference, central obesity according to the relevant cut-points was not associated with CVD mortality [women: 1.3 (95% CI 1.0–1.8), P = 0.078; men: 1.0 (95% CI 0.8–1.3), P = 0.947]. In the Creole population, a similar effect of the Asian obesity cut-point was seen, although the increase in the relative risk upon the inclusion of hip circumference in the model was less marked among women (see Supplementary Table S1 available as Supplementary Data at IJE online).
In a model not containing potential mediator variables (i.e. only adjusting for age, sex and smoking status), waist circumference was significantly associated with CVD mortality before adjustment for hip circumference (hazard ratio per SD 1.16, P < 0.0001); however, this relationship was strengthened with the addition of hip circumference to the model (hazard ratio per SD 1.52, P < 0.0001; P-value for the addition of hip circumference <0.0001). In a model containing only age, sex and BMI, BMI was not associated with CVD mortality in this cohort (P = 0.82). The addition of hip circumference to the model did not change this association (P = 0.62).
Discussion
Our results demonstrate the strong confounding effect of hip circumference on the relationship between obesity and both cardiovascular and all-cause mortality. In this study of South Asian and African Mauritians, the positive relationship of waist circumference with CVD death in a fully adjusted model only became apparent upon adjustment for hip circumference (and vice versa). Hip-adjusted waist circumference was a strong predictor of CVD and all-cause mortality in both men and women, South Asians and Africans. When waist and hip circumference were both added to a risk model for CVD death, which contained those variables used in risk calculators based on the Framingham Heart Study, predictive capacity increased substantially.
Narrow hip circumference has been shown to be a strong risk factor for mortality in several previous studies among Europid populations,19,23–26 although in one study this finding was among men only.19 A small number of studies have noted that, as we found here, the strength of the relationship between hip circumference and either heart disease or mortality only becomes apparent following adjustment for waist circumference.20,21,23 Almost no attention has been given, however, to the impact of adjusting waist circumference for hip circumference. Only two studies that we are aware of have replicated our finding that the effect of waist circumference was underestimated (or absent) before adjustment for hip circumference. Canoy et al.,21 in their report on the effects of body fat on risk of coronary heart disease in the European Prospective Investigation of Cancer-Norfolk study, noted that ‘adjustment for hip circumference increased the risk prediction afforded by using waist circumference alone by ≈10% to ≈18% in men and women’.21 Likewise, in the large and multi-ethnic Epidemiological arm of the Diabetes Reduction Assessment with Ramipril and Rosiglitazone Medication (DREAM) trial (EpiDREAM) cohort, De Koning et al.40 observed that the true effect of waist circumference on glucose levels only became apparent after adjustment for both waist and hip circumferences. We are not aware of any studies that have previously reported the effect on mortality risk of waist circumference adjusted for hip circumference.
Several mechanisms may explain our findings. The first is hinted at by the positive correlation between hip and waist circumference, despite increases in one measure being protective and increases in the other detrimental. Specifically, waist circumference effectively measures both visceral and subcutaneous adipose tissue, whereas hip circumference provides a more specific measure of subcutaneous gluteofemoral adipose tissue. Adjusting a measure of visceral and subcutaneous adiposity for a measure of subcutaneous adiposity may therefore provide a more precise measure of visceral adipose tissue than is possible by measurement of waist circumference alone. Physiological explanations for our findings may also be important, and include previously observed differences in the effect of gluteofemoral subcutaneous adipose and visceral subcutaneous adipose tissue on metabolic health,28,41,42 and the possibility that larger hip circumference reflects greater muscle mass. Manolopolous et al.28 noted in their review on the topic that based on emerging evidence from in vitro and in vivo studies of adipose tissue physiology, ‘gluteofemoral fat may protect our bodies, irrespective of gender, by trapping excess fatty acids and preventing chronic exposure to elevated lipid levels’. In addition, a beneficial adipokine profile (leptin and adiponectin in particular) was also suggested as a potential protective mechanism. Whether the effects of lower body adipose tissue differ between Europid and non-Europid populations is largely unknown. On the one hand, Chowdhury et al.,43 in their study of Indian and Swedish men of the same age and BMI, found higher glucose levels in the South Asian men were due to differences in lower leg muscle mass rather than differences in visceral fat, potentially suggesting that physiological differences between ethnic groups may lead to different effects of hip circumference on mortality risk. On the other hand, a powerful confounding effect of hip circumference on the relationship of waist circumference with glucose was observed in the multi-ethnic EpiDREAM study [including Europid (53%), African (6.5%), Latin American (8.1%), South Asian (20.3%) and indigenous (12.1%) participants], which is suggestive of a similar effect in populations other than the South Asian and African populations included here.40 Further studies including both waist and hip circumference in different population groups and with different outcomes are clearly required.26
Our finding of a marked increase in the predictive capacity of a Framingham Heart Study-based model for CVD or all-cause mortality following the addition of waist and hip circumference suggests that these anthropometric measures may be a useful addition to such models in these populations. Taking account of both waist and hip separately, rather than as a ratio measure, has been shown in this study to be a more powerful risk marker of premature death. This supports the previous conclusion of Seidell et al.42 that the waist-to-hip ratio is a poor reflection of the specific effects of each measurement,23 as individuals with an identical waist-to-hip ratio can have different waist and hip circumferences,44 and using a ratio measure prohibits examination of non-linear associations between the numerator (waist) and the denominator (hip).20
The relationship between obesity and premature mortality has not been widely studied in South Asian populations. A large study from India, and two studies from Bangladesh, found leanness, rather than being overweight or obese, to be a major mortality risk factor.45–47 Those studies, however, were conducted in lean, rural populations and did not account for the protective effect of hip circumference. In rural populations from less developed countries (a large percentage of the native South Asian populations), low BMI reflects under-nutrition, low socio-economic status, poor hygiene and higher resultant mortality.45,48 Urbanization, ageing of populations and increasingly Western lifestyles mean that overweight and obesity are becoming increasingly important causes of death and disease in the developing world.49 A very recent pooled analysis of obesity and risk of death that included two of the cohorts mentioned above, as well as a cohort study from Mumbai with 13 001 deaths, also failed to show an association between BMI and risk of death.50 Again, this study did not account for the protective effect of hip circumference, with their finding mirroring our observation of no association between abdominal obesity and premature mortality before hip circumference was taken into account.
The strengths of our study include response to the baseline surveys of >85%, mortality follow-up of >91%, cause of death data for >98% of the cohort, and the updating of risk factor status on up to two occasions during the study period. The use of physician adjudication of hospital files (15.7%) or next-of-kin interviews (8.2%) for ascertainment of cause of death in some cases is a potential limitation. Since the relationship between central obesity and CVD mortality was strong, however, any misclassification of CVD death is unlikely to have altered our interpretation. It should be noted that the variables included in our study were based on Framingham risk prediction equations for fatal and non-fatal CVD,16 even though only fatal CVD was reported in this study (data on non-fatal CVD were not available). Furthermore, our analysis of the change in estimated risk upon the addition of waist and hip circumference to the model was based on relative change from baseline (e.g. the proportion of individuals whose risk increased by >25%) rather than more commonly used methods that are dependent upon the cut-points chosen and the baseline risk of the population, such as the Net Reclassification Index.51 Since the Mauritius cohort used here has a particular age and risk factor profile, comparisons with other cohorts from more developed countries using such a measure are not likely to be meaningful. Table 2 clearly shows that, in this study, predicted risk increases considerably among those who died, and decreases considerably among those who were censored (did not die) once waist and hip circumference are added to the model.
Conclusions
Central obesity was a strong risk factor for death in this cohort of African and ethnically South Asian Mauritians, but only after adjustment for hip circumference. The effect of central obesity on mortality may be under-estimated without adjustment for hip circumference, and with such adjustment appears to significantly improve the prediction of CVD and all-cause mortality. Hip and waist circumference should be considered jointly for inclusion in CVD risk prediction models and in the assessment of obesity-related risk of future death.
Supplementary Data
Supplementary Data are available at IJE online.
Funding
The baseline surveys were supported by the Ministry of Health and Quality of life (Mauritius), the World Health Organization (Geneva, Switzerland), Baker IDI Heart and Diabetes Institute (formerly the International Diabetes Institute) (Melbourne, Australia), the University of Newcastle upon Tyne (UK), and the National Public Health Institute (Helsinki, Finland). The baseline studies were partially funded by US National Institutes of Health Grant DK-25446. The mortality follow-up was supported by Baker IDI Heart and Diabetes Institute and the Government of Mauritius. AC is supported by a postdoctoral training fellowship from the Australian National Health and Medical Research Council (NHMRC). S.S. is supported by grants from the Västerbotten County Council (ALF), Swedish Heart and Lung Foundation and the Swedish Society of Medicine. J.E.S. is supported by an Australian National Health and Medical Research Council (NHMRC) fellowship (grant number 586623). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Supplementary Material
Acknowledgements
We are most grateful to the participants for volunteering their valuable time, the work of the staff at the Ministry of Health and Quality of Life in Mauritius and the many people involved in organizing and conducting the Mauritius studies. In particular, we thank Gary Dowse, Max De Courten, Ray Spark and Pierrot Chitson for their valuable contributions to the study. The study concept was devised by A.C., D.M. and S.S. All authors contributed to the preparation of the report. The data were analysed by A.C. and B.C. A.C. is the guarantor of this work. Data sharing: no additional data available. A.C. has checked the completeness and validity of the references. This work has not been previously published in the same or a substantively different form.
Conflict of interest: None declared.
KEY MESSAGES.
The effect of central obesity (waist circumference) on mortality risk may be seriously underestimated without adjustment for hip circumference.
Adding waist and hip circumference to a Framingham-type risk model for CVD mortality increased predictive capacity substantially in this study.
All previous studies of obesity and mortality in South Asian populations have reported no association. However, after adjustment for hip circumference, we have shown that this association is, in fact, extremely strong.
Both waist and hip circumference may be important inclusions in CVD risk prediction models, and should be considered in studies of obesity and mortality.
References
- 1.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arnlov J, Ingelsson E, Sundstrom J, Lind L. Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation. 2009;121:230–36. doi: 10.1161/CIRCULATIONAHA.109.887521. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. J Am Med Assoc. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 4.Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL. The effect of age on the association between body-mass index and mortality. N Engl J Med. 1998;338:1–7. doi: 10.1056/NEJM199801013380101. [DOI] [PubMed] [Google Scholar]
- 5.Manson J, Willett W, Stampfer M, et al. Body weight and mortality among women. N Engl J Med. 1995;333:677–85. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 6.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 7.Jee SH, Sull JW, Park J, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355:779–87. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- 8.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 9.Pischon T, Boeing H, Hoffmann K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–20. doi: 10.1056/NEJMoa0801891. [DOI] [PubMed] [Google Scholar]
- 10.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117:1658–67. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 11.Welborn TA, Dhaliwal SS, Bennett SA. Waist-hip ratio is the dominant risk factor predicting cardiovascular death in Australia. Med J Aust. 2003;179:580–85. doi: 10.5694/j.1326-5377.2003.tb05704.x. [DOI] [PubMed] [Google Scholar]
- 12.Anderson KM, Wilson PW, Odell PM, Kannel WB. An updated coronary risk profile. A statement for health professionals. Circulation. 1991;83:356–62. doi: 10.1161/01.cir.83.1.356. [DOI] [PubMed] [Google Scholar]
- 13.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 14.Wallis EJ, Ramsay LE, Ul Haq I, et al. Coronary and cardiovascular risk estimation for primary prevention: validation of a new Sheffield table in the 1995 Scottish health survey population. BMJ. 2000;320:671–76. doi: 10.1136/bmj.320.7236.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D'Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. J Am Med Assoc. 2001;286:180–87. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 16.D'Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 17.Grundy SM, Balady GJ, Criqui MH, et al. Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the AHA Task Force on Risk Reduction. American Heart Association. Circulation. 1998;97:1876–87. doi: 10.1161/01.cir.97.18.1876. [DOI] [PubMed] [Google Scholar]
- 18.Snijder MB, Zimmet PZ, Visser M, Dekker JM, Seidell JC, Shaw JE. Independent and opposite associations of waist and hip circumferences with diabetes, hypertension and dyslipidemia: the AusDiab Study. Int J Obes Relat Metab Disord. 2004;28:402–409. doi: 10.1038/sj.ijo.0802567. [DOI] [PubMed] [Google Scholar]
- 19.Lissner L, Bjorkelund C, Heitmann BL, Seidell JC, Bengtsson C. Larger hip circumference independently predicts health and longevity in a Swedish female cohort. Obes Res. 2001;9:644–46. doi: 10.1038/oby.2001.85. [DOI] [PubMed] [Google Scholar]
- 20.Parker ED, Pereira MA, Stevens J, Folsom AR. Association of hip circumference with incident diabetes and coronary heart disease: the Atherosclerosis Risk in Communities study. Am J Epidemiol. 2009;169:837–47. doi: 10.1093/aje/kwn395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Canoy D, Boekholdt SM, Wareham N, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation. 2007;116:2933–43. doi: 10.1161/CIRCULATIONAHA.106.673756. [DOI] [PubMed] [Google Scholar]
- 22.Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–49. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 23.Bigaard J, Frederiksen K, Tjonneland A, et al. Waist and hip circumferences and all-cause mortality: usefulness of the waist-to-hip ratio? Int J Obes Relat Metab Disord. 2004;28:741–47. doi: 10.1038/sj.ijo.0802635. [DOI] [PubMed] [Google Scholar]
- 24.Mason C, Craig CL, Katzmarzyk PT. Influence of central and extremity circumferences on all-cause mortality in men and women. Obesity. 2008;16:2690–95. doi: 10.1038/oby.2008.438. [DOI] [PubMed] [Google Scholar]
- 25.Heitmann BL, Frederiksen P, Lissner L. Hip circumference and cardiovascular morbidity and mortality in men and women. Obes Res. 2004;12:482–87. doi: 10.1038/oby.2004.54. [DOI] [PubMed] [Google Scholar]
- 26.Heitmann BL, Lissner L. Hip Hip Hurrah! Hip size inversely related to heart disease and total mortality. Obes Rev. 2011;12:478–81. doi: 10.1111/j.1467-789X.2010.00794.x. [DOI] [PubMed] [Google Scholar]
- 27.Despres JP, Lemieux I, Prud'homme D. Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ. 2001;322:716–20. doi: 10.1136/bmj.322.7288.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manolopoulos KN, Karpe F, Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes. 2010;34:949–59. doi: 10.1038/ijo.2009.286. [DOI] [PubMed] [Google Scholar]
- 29.Soderberg S, Zimmet P, Tuomilehto J, et al. Increasing prevalence of Type 2 diabetes mellitus in all ethnic groups in Mauritius. Diabet Med. 2005;22:61–68. doi: 10.1111/j.1464-5491.2005.01366.x. [DOI] [PubMed] [Google Scholar]
- 30.Soderberg S, Zimmet P, Tuomilehto J, et al. High incidence of type 2 diabetes and increasing conversion rates from impaired fasting glucose and impaired glucose tolerance to diabetes in Mauritius. J Intern Med. 2004;256:37–47. doi: 10.1111/j.1365-2796.2004.01336.x. [DOI] [PubMed] [Google Scholar]
- 31.Cameron AJ, Boyko EJ, Sicree RA, et al. Central obesity as a precursor to the Metabolic Syndrome in the AusDiab study and Mauritius. Obesity. 2008;16:2707–16. doi: 10.1038/oby.2008.412. [DOI] [PubMed] [Google Scholar]
- 32.Cameron AJ, Zimmet PZ, Soderberg S, et al. The metabolic syndrome as a predictor of incident diabetes mellitus in Mauritius. Diabet Med. 2007;24:1460–69. doi: 10.1111/j.1464-5491.2007.02288.x. [DOI] [PubMed] [Google Scholar]
- 33.Soderberg S, Zimmet P, Tuomilehto J, et al. Leptin predicts the development of diabetes in Mauritian men, but not women: a population-based study. Int J Obes. 2007;31:1126–33. doi: 10.1038/sj.ijo.0803561. [DOI] [PubMed] [Google Scholar]
- 34.Dowse G, Zimmet P, Gareeboo H, et al. Abdominal obesity and physical inactivity as risk factors for NIDDM and impaired glucose tolerance in Indian, Creole and Chinese Mauritians. Diabe Care. 1991;14:271–82. doi: 10.2337/diacare.14.4.271. [DOI] [PubMed] [Google Scholar]
- 35.Wang J, Thornton JC, Bari S, et al. Comparisons of waist circumferences measured at 4 sites. Am J Clin Nutr. 2003;77:379–84. doi: 10.1093/ajcn/77.2.379. [DOI] [PubMed] [Google Scholar]
- 36.Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and international association for the Study of Obesity. Circulation. 2009;120:1640–45. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 37.Rothman KJ, Greenland S. Modern Epidemiology. 2nd. Philadelphia, PA: Lippincott-Raven; 1998. [Google Scholar]
- 38.Wilson PW, Pencina M, Jacques P, Selhub J, D'Agostino R, Sr, O'Donnell CJ. C-reactive protein and reclassification of cardiovascular risk in the Framingham Heart Study. Circ Cardiovasc Qual Outcomes. 2008;1:92–97. doi: 10.1161/CIRCOUTCOMES.108.831198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2010. [Google Scholar]
- 40.de Koning L, Gerstein HC, Bosch J, et al. Anthropometric measures and glucose levels in a large multi-ethnic cohort of individuals at risk of developing type 2 diabetes. Diabetologia. 2010;53:1322–30. doi: 10.1007/s00125-010-1710-3. [DOI] [PubMed] [Google Scholar]
- 41.Snijder MB, van Dam RM, Visser M, Seidell JC. What aspects of body fat are particularly hazardous and how do we measure them? Int J Epidemiol. 2006;35:83–92. doi: 10.1093/ije/dyi253. [DOI] [PubMed] [Google Scholar]
- 42.Seidell JC, Perusse L, Despres JP, Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: The Quebec Family Study. Am J Clin Nutr. 2001;74:315–21. doi: 10.1093/ajcn/74.3.315. [DOI] [PubMed] [Google Scholar]
- 43.Chowdhury B, Lantz H, Sjostrom L. Computed tomography-determined body composition in relation to cardiovascular risk factors in Indian and matched Swedish males. Metabolism: clinical and experimental. 1996;45:634–44. doi: 10.1016/s0026-0495(96)90036-0. [DOI] [PubMed] [Google Scholar]
- 44.Allison DB, Paultre F, Goran MI, Poehlman ET, Heymsfield SB. Statistical considerations regarding the use of ratios to adjust data. Int J Obes Relat Metab Disord. 1995;19:644–52. [PubMed] [Google Scholar]
- 45.Sauvaget C, Ramadas K, Thomas G, Vinoda J, Thara S, Sankaranarayanan R. Body mass index, weight change and mortality risk in a prospective study in India. Int J Epidemiol. 2008;37:990–1004. doi: 10.1093/ije/dyn059. [DOI] [PubMed] [Google Scholar]
- 46.Hosegood V, Campbell OM. Body mass index, height, weight, arm circumference, and mortality in rural Bangladeshi women: a 19-y longitudinal study. Am J Clin Nutr. 2003;77:341–47. doi: 10.1093/ajcn/77.2.341. [DOI] [PubMed] [Google Scholar]
- 47.Pierce BL, Kalra T, Argos M, et al. A prospective study of body mass index and mortality in Bangladesh. Int J Epidemiol. 2010;39:1037–45. doi: 10.1093/ije/dyp364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105:260–75. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 49.Beaglehole R, Bonita R. Global public health: a scorecard. Lancet. 2008;372:1988–96. doi: 10.1016/S0140-6736(08)61558-5. [DOI] [PubMed] [Google Scholar]
- 50.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–29. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. doi: 10.1002/sim.2929. discussion 207–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.