Abstract
Background
Atherosclerosis is a complex disease with hundreds of genes influencing its progression. In addition, the phenotype of the disease varies significantly depending on the arterial bed.
Methodology/Principal Findings
We characterized the genes generally involved in human advanced atherosclerotic (AHA type V–VI) plaques in carotid and femoral arteries as well as aortas from 24 subjects of Tampere Vascular study and compared the results to non-atherosclerotic internal thoracic arteries (n=6) using genome-wide expression array and QRT-PCR. In addition we determined genes that were typical for each arterial plaque studied. To gain a comprehensive insight into the pathologic processes in the plaques we also analyzed pathways and gene sets dysregulated in this disease using gene set enrichment analysis (GSEA). According to the selection criteria used (>3.0 fold change and p-value <0.05), 235 genes were up-regulated and 68 genes down-regulated in the carotid plaques, 242 genes up-regulated and 116 down-regulated in the femoral plaques and 256 genes up-regulated and 49 genes down-regulated in the aortic plaques. Nine genes were found to be specifically induced predominantly in aortic plaques, e.g., lactoferrin, and three genes in femoral plaques, e.g., chondroadherin, whereas no gene was found to be specific for carotid plaques. In pathway analysis, a total of 28 pathways or gene sets were found to be significantly dysregulated in atherosclerotic plaques (false discovery rate [FDR] <0.25).
Conclusions
This study describes comprehensively the gene expression changes that generally prevail in human atherosclerotic plaques. In addition, site specific genes induced only in femoral or aortic plaques were found, reflecting that atherosclerotic process has unique features in different vascular beds.
Introduction
Atherosclerosis is a complex disease characterized by endothelial cell dysfunction, smooth muscle cell proliferation and migration, inflammation, lipid and matrix accumulation and thrombus formation with hundreds of genes influencing its progression. Susceptibility to atherosclerosis is in turn influenced by complex gene-gene and gene-environment interactions making atherosclerosis a challenging research subject.
Gene expression techniques, such as microarrays and representational difference analysis, are powerful tools that can be used to discover the complexities underlying the development of atherosclerotic plaque. This method has previously been used to detect differentially expressed genes in normal and diseased arteries [1], [2], disease progression [3], detecting differentially expressed genes according to patient symptomatology [4] and discovering pathways affected in coronary atherosclerosis [5]. When considering the large amount of genes influencing the development of atherosclerosis focusing into pathway characterization provides a comprehensive insight about the pathological mechanisms underlying atherosclerosis. On the other hand, single-gene approach may be utilized when analyzing fundamental genes in complex signalling systems.
Although atherosclerosis has a systemic nature, the susceptibility to develop atherosclerotic lesions and the histological type of atherosclerosis differs strikingly between different sites in human vasculature. The type of atherosclerosis ranges from stable calcified plaques and fibrotic plaques all the way to unstable ulcerated plaques and the prevalence of these lesions varies according to vascular bed region. For example, ulcerated plaques in symptomatic carotid stenosis patients are common while fibrotic and calcified lesions dominate in aortic and femoral areas raising the question whether this dissimilarity could also be seen in the gene expression profiles in different vascular regions.
We, therefore, screened the global gene expression profile of advanced atherosclerotic plaques in carotid arteries, femoral arteries and aortas and compared the results to non-atherosclerotic left internal thoracic arteries (LITA) and identified most up- and down-regulated genes in each arterial bed and searched for genes that would be specific for one arterial region, and in addition, characterized genes that were generally involved in disease. Using gene set enrichment analysis (GSEA), we also analyzed pathways (available in MSigDB database) that were generally affected in atherosclerotic plaques.
Methods
Tampere Vascular Study (TVS) material
The atherosclerotic vascular sample series for GWEA consists of atherosclerotic plaques from the following arterial sites: femoral artery (n=4) carotid artery (n=9) and abdominal aorta (n=7) and control samples from internal thoracic arteries (ITA) during coronary artery bypass surgery (n=6) all together from a total of 26 patients participating in Tampere Vascular Study. All the samples were handled and obtained in a standardized fashion supervised by senior scientist in our laboratory. All the samples from atherosclerotic arteries were obtained by endarterectomy under loupe magnification obtaining a sample that consists of the plaque with intima and the inner media. All these procedures were performed by vascular surgeons under the surveillance of one of the principal investigators (NO). ITA samples consisted of arterial rings obtained during dissection and with all the arterial layers including outer media and adventitia. All the patients had a polyvascular disease (i.e. at least two major arterial beds affected by atherosclerotic plaques as evidenced by 1) previous transient ischemic attack and/or atherosclerotic plaques in the cerebral vasculature or 2) coronary atherosclerosis as evidenced by previous myocardial infarction or 3) angina pectoris and atherosclerotic plaques in coronary angiography or 4) objectively verified peripheral arterial disease by ankle-brachial pressure index <0.9 or 5) previous arterial surgery due to atherosclerosis or 6) angiographical demonstration of arterial plaques. Of these patients, only two had polyvascular disease and all the rest had monovascular disease limited to the coronary vasculature. The sample population demographics are presented as Table S1. The population had strong male predominace. The aortic group were the youngest and had seldom dyslipidemia and diabetes. The control group had more seldom hypertension and diabetes. The cholesterol levels were highest in femoral and control group. Smoking was frequent, especially in aortic group.
For the relative gene expression analysis, 24 atherosclerotic tissue samples were used (2 from the original sample set could not be recovered) and similarly, the six ITA vessels were used as controls. The vascular samples were histologically classified according to the American Heart Association classification (AHA) [6]. The carotid and femoral artery samples were type V or VI, aorta samples were type VΙ and all control vessels were healthy. The study was approved by the Ethics Committee of Tampere University Hospital (Permission number 99204). All the patients gave written informed consent. The samples were taken from patients subjected to open vascular surgical procedures at the Division of Vascular Surgery, Tampere University Hospital. All the patients gave informed consent.
RNA isolation and genome wide expression analysis
The fresh tissue samples were soaked in RNALater solution (Ambion Inc., Austin, TX, USA) and isolated with Trizol reagent (Invitrogen, Carlsbad, CA, USA) and the RNAEasy Kit (Qiagen, Valencia, CA, USA). The concentration and quality of the RNA was evaluated spectrophotometrically (BioPhotometer, Eppendorf, Wesseling-Berzdorf, Germany). More than 23,000 known and candidate genes were analyzed using Sentrix Human-8 Expression BeadChips, according to manufacturer's instructions. (Illumina, San Diego, CA, USA). In brief, a 200 ng aliquot of total RNA from each sample was amplified to cDNA using the Ambion's Illumina RNA Amplification kit according to the instructions (Ambion, Inc., Austin, TX, USA). Each sample cRNA (1500 ng) was hybridized to Illumina's Sentrix Human-8 Expression BeadChip arrays (Illumina). Hybridized biotinylated cRNA was detected with 1 µg/ml Cyanine3-streptavidine (Amersham Biosciences, Pistacataway, NJ, USA). BeadChips were scanned with the Illumina BeadArray Reader. The method has been described in more detail in our previous work [7].
Bioinformatics and statistical analyses
The data was archived using the minimum information about a microarray experiment (MIAME 1.1. Draft 6). Raw intensity data obtained from the IlluminaTM platform were normalized with R language and environment for statistical computing and related Bioconductor module [8]. Bioconductor module was also used to conduct single-probe analysis including fold-change calculations and filtering the probes. The statistical analysis was carried out using the Limma package [9]. -Pathway analysis of the expression data (all diseased vs. controls) was performed using the GSEA implemented in GSEA java desktop application version 2.0 and MsigDB (Molecular Signature Database) version 2.0. Statistical analysis was performed using SPSS version 14.0. (SPSS Inc., Chicago, IL, USA). The non-parametric Mann-Whitney U-test with post-hoc correction was used for comparison of mRNA expression between atherosclerotic and control tissues and to find differentially expressed genes. The results are presented as average fold change. The averaging was done for each arterial bed. The selection criteria were >3.0-fold change in gene expression and p-value less than 0.05. The agreement between GWEA and TLDA was evaluated by first classifying the results as down-regulated, neutral or up-regulated. Then the number of samples correctly classified into these categories was calculated and was found to be >90%.
Quantitative RT-PCR
Quantitative gene expression analyses were performed with TaqMan low density arrays (TLDAs) (Applied Biosystems, Foster City, CA, USA) using gene specific TaqMan gene expression assays. Total-RNA (500 ng) was transcribed to cDNA using the High Capacity cDNA Kit (Applied Biosystems) according to manufacturer's instructions. After the cDNA synthesis, the LDA cards were loaded with 8 µl undiluted cDNA, 42 µl H20, and 50 µl PCR Universal Master Mix (Applied Biosystems) and run according to the manufacturer's instructions. Samples were analyzed as duplicates, and both cDNA synthesis and PCR reactions were validated for inhibition of amplification in PCR and cDNA synthesis. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) was used as a housekeeping gene. The results were analyzed using SDS 2.2 Software (Applied Biosystems).
Immunohistochemistry
All samples were first dyed with haematoxyclin (HE) and classified according to Stary et al. [6]. Immunocytochemistry was performed using the N-Histofine® Simple Stain MAX PO staining method (Nichirei Biosciences Inc., Tokyo, Japan)) and paraffin-embedded vascular samples without any counterstain. Lactotransferrin (LTF)- immunoreactivity(IR) was detected with a rabbit polyclonal antibody (dil. 1∶100, Lifespan Bioscience, Seattle, WA, USA). Vascular cell types were identified with mouse anti-human muscle actin (dil. 1∶30, clone HHF35; DakoCytomation, Glostrup, Denmark), mouse anti-human endothelial cell (dil. 1∶70, CD31, clone JC70A; DakoCytomation) and mouse anti-human CD68 (dil. 1∶70, clone PG-M1, DakoCytomation) was used as marker of monocytes and macrophages. Neutrophil granulocytes were identified using mouse anti-human neutrophil elastase antibody (dil. 1∶500, DakoCytomation). T-lymphocytes were recognized with mouse anti-CD3 antibody (dil. 1∶150, eBioscience Inc., San Diego, CA) and B-lymphocytes were labelled with mouse anti-CD20 (dil. 1∶1000, DakoCytomation. The sections were subjected to microwave antigen retrieval treatment as described earlier [10] except for elastase antibody. Endogenous peroxidase activity was extinguished by treating the section with with 0.3% H2O2 for 30 min. Subsequently the sections were incubated overnight with the primary antibodies followed with appropriate N-Histofine staining reagent for 30 min. ImmPACT™ (Vector Laboratories, Burlingame, CA, USA) diaminobenzidine-solution with nickel-intensification was used as the chromogen. All antibodies were diluted in PBS containing 1% BSA and 0.3% of Triton X-100. Controls included omitting the primary antibody or replacing it with non-immune sera. No staining was seen in the controls. The co-localization of LTF with different markers was studied in adjacent 5 µm sections (mirror image sections). Sections were stained as described above. Photographs were obtained using Nikon FXA-100 microscope equipped with PCO Sensicam digital camera (PCO, Kelheim, Germany).
Results
Overall gene expression changes observed in carotid, femoral and aortic plaques
Several genes were found to have significantly altered expression in advanced atherosclerotic carotid and femoral artery plaques as well as in the aortas studied with GWEA. According to the selection criteria used (>3.0 fold change and p-value <0.05), 235 genes were up-regulated and 68 genes down-regulated in type V–VI carotid plaques. For type V–VI femoral plaques, 242 genes were up-regulated and 116 genes down-regulated. In type VI aortic plaques, 256 genes were up-regulated and 49 genes down-regulated (Table S2, S3, S4, S5, S6, S7). In order to identify globally affected genes, we combined all gene expression results and calculated average fold changes. Of these, 27 most up-regulated and 16 down-regulated genes were verified with QRT-PCR (TLDA) (Table 1 and 2). The concordance between GWEA and TLDA was over 90%.
Table 1. The most up-regulated genes generally in atherosclerotic plaques analysed with TaqMan Low Density array.
| Gene abbreviation | Gene ID | Average FC |
| MMP12 (matrix metallopeptidase 12) | 4321 | 473.7 (p<0.0001) |
| MMP7 (matrix metallopeptidase 7) | 4316 | 686.1 (p<0.0001) |
| SPP1 (secreted phosphoprotein 1) | 6696 | 173.0 (p<0.0001) |
| APOC1 (apolipoprotein C–I) | 341 | 154.8 (p<0.001) |
| MMP9 (matrix metallopeptidase 9) | 4318 | 125.3 (p<0.001) |
| CCL18 (CC chemokine ligand 18) | 6362 | 105.7 (p<0.001) |
| ACP5 (acid phosphatase 5) | 54 | 57.7 (p<0.001) |
| APOE (apolipoprotein E) | 348 | 52.9 (p<0.001) |
| IL4I1 (interleukin 4 induced 1) | 259307 | 35.2 (p<0.001) |
| RGS1 (regulator of G-protein signaling 1) | 5996 | 19.9 (p<0.001) |
| HMOX1 (heme oxygenase 1) | 3162 | 20.5 (p<0.001) |
| IFI30 (interferon, gamma-inducible protein 30) | 10437 | 23.2 (p<0.001) |
| SLAMF8 (SLAM family member 8) | 56833 | 22.0 (p<0.001) |
| MGC29506 (hypothetical protein) | 51237 | 19.2 (p=0.001) |
| THBS1 (thrombospondin 1) | 7057 | 13.8 (p=0.000) |
| LYZ (lysozyme) | 4069 | 10.8 (p<0.001) |
| IGJ (immunoglobulin J polypeptide) | 3512 | 14.1 (p=0.001) |
| TYMP (thymidine phosphorylase) | 1890 | 14.0 (p<0.001) |
| IL8 (interleukin 8) | 3576 | 12.0 (p<0.001) |
| COL1A1 (collagen, type I, alpha 1) | 1277 | 5.7 (p<0.001) |
| CAPG (capping protein) | 822 | 7.4 (p<0.001) |
| ADFB (adipose differentiation-related protein) | 123 | 6.4 (p<0.001) |
| LGALS3 (lectin, galactoside-binding, soluble, 3) | 3958 | 1.8 (p=0.001) |
| CYBA (cytochrome b-245, alpha polypeptide) | 1535 | 5.4 (p<0.001) |
| CFL1 (cofilin 1) | 1072 | 1.3 (p=0.158) |
| ALDOA (aldolase A, fructose-bisphosphate) | 226 | 1.2 (p<0.001) |
| HLA-DRP3 (major histocompatibility complex, class II, DR beta 3) | 3125 | −8.8 (p=0.561) |
The results are shown as an average fold change (FC) compared to control arteries.
Table 2. The most generally down-regulated genes in atherosclerotic plaques analysed with TaqMan Low Density array.
| Gene abbreviation | Gene ID | Average FC |
| ITLN1 (intelectin 1) | 55600 | −568.2 (p<0.001) |
| APOD (apolipoprotein D) | 347 | −103.9 (p<0.001) |
| DUSP26 (dual specificity phosphatase 26) | 78986 | −21.3 (p<0.001) |
| CASQ2 (calsequestrin 2) | 845 | −23.6 (p<0.001) |
| RGS5 (regulator of G-protein signaling 5) | 8490 | −13.0 (p<0.001) |
| TCEAL2 (transcription elongation factor A (SII)-like 2) | 140597 | −18.6 (p<0.001) |
| DES (desmin) | 1674 | −15.8 (p=0.025) |
| CALD1 (caldesmon 1) | 800 | −10.4 (p<0.001) |
| PPP1R3C (protein phosphatase 1) regulatory (inhibitor) subunit 3C) | 5507 | −9.5 (p<0.001) |
| ADRA2C (adrenergic, alpha-2C-, receptor) | 152 | −12.9 (p<0.001) |
| CSRP2 (cysteine and glycine-rich protein 2) | 1466 | −8.6 (p<0.001) |
| SPEG (SPEG complex locus) | 10290 | −4.2 (p<0.001) |
| CNN1 (calponin 1) | 1264 | −4.3 (p<0.001) |
| C6orf117 (chromosome 6 open reading frame 117) | 112609 | −8.7 (p<0.001) |
| LMOD1 (leiomodin 1) | 25802 | −6.5 (p<0.001) |
| RAMP1 (receptor activity modifying protein 1) | 10267 | −5.4 (p<0.001) |
The results are shown as an average fold change (FC) compared to control arteries.
Among the most up-regulated genes verified with QRT-PCR in atherosclerotic plaque (Table 1), we found genes already previously connected to atherosclerosis, like matrix metalloproteinases [11], apolipoproteins [12] and osteopontin [13], but we also found new genes, not found to be involved in the pathogenesis of atherosclerosis, namely interleukin 4 induced 1 (IL4I1), interferon, gamma-inducible protein (IFI30), SLAM family member 8 (SLAMF8), and immunoglobulin J polypeptide (IGJ). Previously, gene expression profiling of human atherosclerotic coronary arteries did not reveal the involvement of these genes in the pathogenesis on atherosclerosis [14], [5].
We quantitated the 16 most generally down-regulated genes in advanced atherosclerotic plaques using QRT-PCR. For most of the genes on this list there are only few studies in the literature and no information about their connection to atherosclerosis. The significantly down-regulated genes in all the plaques studied are shown in Table 2.
Site-specific gene expression alterations in different arterial beds
According to GWEA data, we found nine genes that were induced only in aortic plaques and three genes that were specifically induced in femoral plaques of which expression was verified with QRT-PCR. Genes induced predominantly in aortic plaques differed considerably from the genes induced in femoral plaques. Most of the genes induced in aortic plaques are involved in immunological processes, especially involving B cells whereas the genes induce in femoral plaques function mainly in extra-cellular matrix modifications (Table 3). The genes that were induced in carotid arteries, were also induced in aortic and femoral plaques, thus no specific gene for carotid plaques was found. To verify the predominant expression in only one arterial bed region, we ascertained the protein localization of one of the aortic plaque specific genes; LTF, a major immune system modulator [15]. Using IHC, LTF protein was found predominantly in aortic plaques mainly in necrotic debris in intima and inner media wherein localized to neutrophils, B and T lymphocytes (Figures 1 and 2). In femoral and carotid arteries, LTF was present only in sparse cells being mostly unoccupied by LTF positive cells (Figures 3 and 4).
Table 3. Genes that were induced only in aortic or femoral plaques compared to non-atherosclerotic internal thoracic arteries analyzed with genome-wide expression array (GWEA).
| Gene (ID) | Gene ID | Fold change | Function |
| Aortic plaques | |||
| CHGA, chromogranin A | 1113 | 5.8 | Secretory granules formation, immunity against microbes [66], cancer [67], hypertension and myocardial infarction [38], [68] |
| CSF3, colony stimulating factor 3 | 1440 | 4.6 | Survival/proliferation of neutrophils and macrophages [69], arteriogenesis [70] |
| GAGE12I, G antigen 12I | 26748 | 4.5 | Antigen, anti-apoptotic factor [71], [72] |
| C4orf7, choromosome 4 open reading frame 7 | 260436 | 4.3 | B cell immunity, tumorigenesis [73] |
| GAGE6, G antigen 6 | 2578 | 4.0 | Antigen, cancer [74] |
| LTF, lactotransferrin | 4057 | 3.7 | Immune modulator [15] |
| PRPH, peripherin | 5630 | 3.6 | Intermediate filament [75] |
| MS4A1, membrane-spanning 4-domains | 931 | 3.5 | B cell immunity [76], [77], cancer [78] |
| Femoral plaques | |||
| C1QTNF3, C1q and tumor necrosis factor related protein 3 | 114899 | 3.4 | Adipose tissue secreted protein, anti-inflammatory [79] |
| CHAD, chondroadherin | 1101 | 3.9 | Extracellular matrix structure modification [42], [80] |
| PTN, pleiotrophin | 5764 | 4.7 | Cell differentiation [48], angiogenesis [47], cancer [81] |
For all genes, the p-value was less than 0.05.
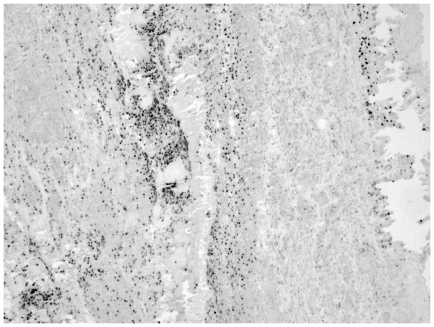
Figure 1. Immunohistochemical staining of lactoferrin (LTF) in advanced human atherosclerotic aorta.
The picture was taken with 100× magnitude.
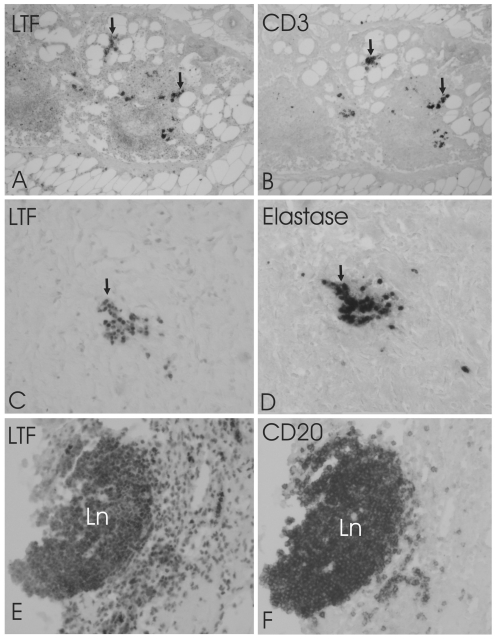
Figure 2. Co-localization of lactoferrin (LTF) with neutrophils and T and B lymphocytes.
Adjacent mirror image sections demonstration the co-localization of LTF (A, C, E) with T-cell marker CD3 (B), neutrophil granulocyte marker elastase (D) and B-cell marker CD20 (F) in aortic plaques. Arrows point cells that are both LTF and CD3-IR (A, B) or LTF and Elastane-IR (C, D). Most of the CD20-IR cells in a lymph nodule (Ln) are also LTF-IR. Large number of LTF-IR cells in surrounding tissue are not CD20-IR. The pictures were taken with 200× magnitude.
Figure 3. Immunohistochemical staining of lactoferrin (LTF) in advanced human atherosclerotic femoral artery.
The picture was taken with 100× magnitude.
Figure 4. Immunohistochemical staining of lactoferrin (LTF) in advanced human atherosclerotic carotid artery.
The picture was taken with 100× magnitude.
Altered pathways in advanced atherosclerotic lesions
In order to identify globally affected pathways in advanced atherosclerosis, we performed gene set expression analyses (GSEA) to illuminate dysregulated pathways. In the pathway analyses, 20 pathways appeared to be significantly up-regulated and 8 pathways down-regulated in advanced atherosclerotic plaques as compared to non-atherosclerotic arteries according to the criteria recommended by Subramanian et al. (FDR<0.25) [16] (Table S8). Significantly up-regulated pathways involved apoptotic and pro-inflammatory pathways as well as pathways involved in complement or B cell activation and cell movement. The significantly altered down-regulated pathways included fatty acid metabolism and amino acid metabolism pathways, glutamate receptor pathway, benzoate degradation pathway and pathway including genes of hormonal functions. Interestingly, a pathway including HOX genes related to hematopoiesis was significantly down-regulated.
Despite intensive research on the role of T cells in atherogenesis, this is the first time that all the major genes involved in T cell differentiation are described from three major atherosclerotic arterial beds. In order to verify the results of the pathway analysis, we quantitated with QRT-PCR the expression of all genes belonging to nkTPathway (Biocarta) (natural killer T-cells) containing genes involved in T cell differentiation. The pathway included a total of 29 genes of which 26 were significantly up-regulated and three genes down-regulated in plaques vs. non-atherosclerotic arteries (Table 4). In general, the highest fold changes were seen in aortas (for exact fold changes in different vascular beds, see Table S9). Despite the classical T cell genes already known to be activated, several other genes were also significantly altered in plaques, e.g., chemokine receptors 3,4, and 7 (CCR3, CCR4, CCR7), interferon gamma receptor 1–2 (IFNGR1, IFNGR2), interleukin 12 receptor beta 1–2 (IL12RB1, IL12RB2), interleukin 18 receptor 1 (IL18R1), interleukin 4 receptor (IL4R), and transforming growth factor beta 2 (TGFB2).
Table 4. The expression of nkTPathway (natural killer T-cell) genes in atherosclerotic plaques from carotid arteries, aortas and femoral arteries compared to non-atherosclerotic internal thoracic arteries analyzed with TaqMan low density array.
| Gene abbreviation | Gene ID | Average FC |
| CSF2 (colony stimulating factor 2 (granulocyte-macrophage) | 1437 | ↑↑↑* |
| IL12B (interleukin 12B) | 3593 | ↑↑* |
| CCR5 (chemokine (C-C motif) receptor 5) | 1234 | 14.9 (p<0.001) |
| CXCR4 (chemokine (C-X-C motif) receptor 4) | 7852 | 12.4 (p=0.001) |
| CCR1 (chemokine (C-C motif) receptor 1) | 1230 | 10.7 (p<0.001) |
| CD4 (CD4 molecule) | 920 | 10.2 (p<0.001) |
| CCL4 (chemokine (C-C motif) ligand 4) | 6351 | 8.4 (p=0.001) |
| CCR7 (chemokine (C-C motif) receptor 7) | 1236 | 8.1 (p=0.001) |
| CCL3 (chemokine (C-C motif) ligand 3) | 6348 | 6.6 (p<0.001) |
| IL12RB1 (interleukin 12 receptor, beta 1) | 3594 | 6.0 (p<0.001) |
| CD28 (CD28 molecule) | 940 | 5.8 (p=0.001) |
| CXCR3 (chemokine (C-X-C motif) receptor 3) | 2833 | 5.6 (p=0.001) |
| CCR4 (chemokine (C-C motif) receptor 4) | 1233 | 3.5 (p=0.033) |
| CD40LG (CD40 ligand) | 959 | 3.4 (p=0.008) |
| IFNG (interferon, gamma) | 3458 | 3.1 (p=0.022) |
| IL12RB2 (interleukin 12 receptor, beta 2) | 3595 | 3.0 (p=0.233) |
| IFNGR2 (interferon gamma receptor 2) | 3460 | 2.9 (p<0.001) |
| IL12A (interleukin 12A) | 3592 | 2.9 (p=0.009) |
| TGFB1 (transforming growth factor, beta 1) | 7040 | 2.0 (p<0.001) |
| IL18R1 (interleukin 18 receptor 1) | 8809 | 2.0 (p=0.007) |
| CCR2 (chemokine (C-C motif) receptor 2) | 1231 | 1.9 (p=0.213) |
| IFNGR1 (interferon gamma receptor 1) | 3459 | 1.7 (p=0.005) |
| IL4R (interleukin 4 receptor) | 3566 | 1.4 (p=0.002) |
| TGFB2 (transforming growth factor, beta 2) | 7042 | 1.4 (p=0.069) |
| IL5 (interleukin 5) | 3567 | 1.5 (p=0.500) |
| IL4 (interleukin 4) | 3565 | −1.2 (p=0.468) |
| IL2 (interleukin 2) | 3558 | −2.1(p=0.836) |
| TGFB3 (transforming growth factor, beta 3) | 7043 | 1.2 (p=0.350) |
| CCR3 (chemokine (C-C motif) receptor 3) | 1232 | −1.7 (p=0.108) |
Fold changes (FC) are calculated by comparing the median expression of genes in atherosclerotic arteries vs. controls. Notes.
Highly expressed in atherosclerotic plaque.
Discussion
The present scan of all known human genes in the atherosclerotic plaques from carotid and femoral arteries as well as from the aortas revealed novel genes involved generally in atherosclerosis and specifically in different vascular regions. In addition, we revealed pathways and gene sets that were significantly dysregulated in advanced atherosclerotic plaques and verified the expression of all genes in one of the most up-regulated pathways that is involved in T cell differentiation.
Many of the genes found in this study have been linked to atherosclerosis also in previous studies. Although, due to rapidly evolved whole genome microarray technology, it is challenging to directly compare the results with those of the previous studies [2], [1], [5], [3]. Furthermore, these studies have utilized samples at different stage of atherosclerosis from organ donors and autopsies [2], [1], [3] whereas pathway analysis has been done focusing only in the coronary region in the heart transplantation patients [5].
New genes involved in advanced atherosclerosis
In addition to genes already linked to atherosclerosis, we also found a new set of genes, not previously found in atherosclerotic plaques, or even otherwise connected to the disease. IL4I1 (FC+35.2), is expressed by B-cells, [17], [18] and in inflammatory conditions by macrophages and dendritic cells [19]. Interferon, gamma-inducible protein 30 (IFI30) (FC+23.2) demonstrated high expression and it has not been previously identified in atherosclerosis. Since both IL41I [19], and IFI30 [20], [21] participate in the down-regulation of Th1 mediated inflammation, a crucial element in atherosclerosis [22], [23], our results of high expression of IL41I and IFI30 may reflect a negative feedback response to Th1 mediated inflammation in the atherosclerotic process. Our results of the involvement of IFI30 and IFI30 in the regulation of Th1 cells opens new possibilities to modulate the immune reactions responsible for atherogenic processes. It is also interesting to note that even though some immunoglobulins, like IgG and IgM [24], [25], have already been linked to atherosclerosis, there is no information in the literature about IgJ, involved in B cell activation [26], in atherosclerosis. Based on the NCBI Gene Expression Omnibus database, IgJ has had elevated expression in some of the samples in gene expression profiling of atherosclerotic coronary arteries, but the results were controversial and did not support a critical role in atherosclerosis [5]. In our study though, the expression of IgJ in all three atherosclerotic arteries was obvious with 14.1-fold up-regulation in plaques and with p-value of p<0.001 warranting further studies.
We found several significantly up-regulated genes in plaques without obvious implications in atherosclerosis. These genes include e.g., CCL18 and RGS1, involved in lymphocyte attraction, migration and function [27]–[29] and CAPG that is suggested to modulate the protective effects of unidirectional shear stress [30]. BLAME, a B cell costimulator and adhesion molecule [31] that has previously found in human macrophages to be induced in response to LDL [32] and now, found +22.0 –fold in human advanced atherosclerotic plaques. Most of the significantly down-regulated genes are new with regards to atherosclerosis. The most drastically down-regulated gene was intelectin 1 (ITLN1), which was almost absent in atherosclerotic plaques compared to non atherosclerotic internal thoraci`c arteries. ITLN1 is a cell surface phagocytotic receptor that recognizes specific bacterial cell wall components [33] and the absence of ITLN1 has been suggested to alter immune responses to infection and facilitate inflammation [34]. Another significantly down-regulated gene was the regulator of G-protein signalling 5 (RGS5). Recently, the blockage of RGS5 has been suggested to provide an alternative approach to treat hypertension but the biological impact of the reduced expression of RGS5 in the plaques is not known.
Site-specific gene expression changes in vascular regions studied
After carefully examining the GWEA data, we determined nine genes specific for aortic plaques and three genes specific for femoral plaques. We did not find any gene that would have been specific for carotid plaques. It is interesting to note that the genes that were specifically induced in aortic plaques are mostly involved in immune reactions, especially in B cell immunity (Table 3).
We observed a significant up-regulation of LTF in aorta, located in B- and T-cells and in neutrophils. LTF is an iron-binding glycoprotein abundantly found in exocrine secretions of mammals and released by mucosal epithelia and neutrophils during inflammation [35] and binds to cells of the immune system [15].
The role of LTF as a negative regulator of inflammation, is a key element in the host defence system and is capable of binding to cells of the immune systems, e.g., cells of the monocyte lineage [15]. LTF interacts with monocytes and macrophages and modulates their function during inflammatory and infectious processes, e.g., increasing cytotoxic activity, cytokine production (Th1) and expression of surface molecules [36]. When considering the fundamental role of macrophages in atherosclerosis, it is interesting to speculate the reason why such a powerful macrophage regulator is induced predominantly in aortic plaques. Interestingly, serum lactoferrin has been found to associate with fatal ischemic heart disease in patients with diabetes [37]. Whether the LTF expression induce specific immunological effects in aortic plaques contributing to phenotype commonly observed in aortic plaques, needs to be clarified in the future. At least, considering the wide array of immunological functions, such speculation is justifiable.
Chromogranin A (CHGA) that acts as a prohormone giving rise to several biologically active peptides [38], was another gene found to be specific for aortic plaques. CHGA has been suggested to be a fundamental regulator of blood pressure [38] and endothelial barrier function [39] and interestingly, an independent predictor of long-term mortality and heart failure of acute coronary syndromes [40]. The biological role of CHGA in the pathogenesis of atherosclerosis is not known but the ∼6-fold up-regulation specifically in aortic plaques may inspire future research.
The three genes induced specifically in femoral plaques differed from the aortic plaque specific genes. Femoral plaques exist usually in a stable phenotype with a placid fibrous cap and therefore it is not surprising that chondroadherin, a cartilage matrix protein, was ∼4-fold induced predominantly in femoral plaques. In addition of being able to promote attachement of osteoblastic cells to solid state substrates [41], CHAD interacts with integrin alpha2beta1 (α2β1) [42] and complement [43], both involved in atherogenic processes [44]–[46].
Pleiotrophin (PTN) was ∼5-fold up-regulated in femoral plaques, has previously been found in atherosclerotic human coronary arteries and suggested to participate in intraplaque vascularization, inflammation [47] and monocyte/macrophage differentiation into endothelial cell phenotype [48].
T cell differentiation pathway in atherosclerotic plaques
We found the pathway including genes involved in the regulation of T cell chemokine pathway to be highly activated in the advanced plaques. Taken the fundamental role of T cells in the plaque formation and inflammation [49], we quantitated all the genes belonging to this pathway in order to get a comprehensive view about the extent how all the crucial T cell chemokines are actually expressed in human plaques and even more, see the trends of the pathway. Instead of focusing on well-known genes involved in T cell activation, we discuss here genes with little or no previous information at all regarding atherosclerosis.
IL12, secreted by macrophages dendritic cells and Th1 cells and acting through IL12RB1/2 [50], is considered a proatherogenic and proinflammatory cytokine contributing to chemotaxis and migration [23], [51]. IL12RB1 was 6-fold up-regulated in the plaques and IL12RB2 3-fold, respectively. It is interesting to speculate that the dissimilar expression of the two subunits of IL12R may alter the consequences of IL12 binding and even may have distinct effects of their own in the plaque immunological reactions. Actually, IL12RB2 has already found to limit cancer growth and thus proven to elicit an effect on its own [52].
IL2 and IL4 were the only interleukins on this pathway that were generally down-regulated in plaques. Previously, pro-inflammatory IL2 has been found to be associated with carotid artery intima-media thickness [53]. Locally produced IL4 has earlier expected to be protective towards an excessive pro-inflammatory response in plaques [54], [55] but there are also studies that suggest a pro-atherogenic role for IL4 [56]. Considering the low expression of IL2 and IL4 mRNA in atherosclerotic plaques, the role of these cytokines may not be significant in atherosclerosis. It is though worth on mentioning that the receptor for IL4, IL4R, was actually up-regulated in plaques. In addition of binding IL4, IL4R is also capable of binding IL13, a cytokine with potential anti-inflammatory activity [57] raising the idea whether the role of IL4R should be investigated in more detail with regards inhibiting the pathologic processes leading to atherosclerotic disease.
TGFB1–3 genes were all only mildly up-regulated in plaques studied. A study by Mallat et al. with apoE-deifcient mice suggest a major protective role for TGFB signaling in atherosclerosis. In this study, inhibition of TGFB signaling was also found to induce an unstable plaque phenotype [58]. The protective role seemed to depend on the effects of TGFB on macrophages and T cells, major players in atherosclerosis pathogenesis. As the expression of TGFB1–3 was only mildly up-regulated in plaques, the inducement of TGFB expression or signaling might offer new strategies in preventing the plaque progression.
With the exception of CCR2 and CCR3, all the other CCRs in this pathway were significantly up-regulated in plaques with fold changes varying from 14.9 to 3.5 supporting the previously suggested role of CCRs in this disease [59], [60]. CCR3, a marker for Th2 cells, showed significant down-regulation (fold change −4.5, p=0.012) only in carotid arteries suggesting that the Th2 response in carotid artery disease may differ from aortic and femoral artery atherosclerosis.
Interferon gamma has been suggested to accelerate atherosclerosis e.g. by activating macrophages and increasing their production of nitric oxide and pro-inflammatory cytokines [61]. In our study, the expression of interferon gamma receptors 1 and 2 (IFNGR1, IFNGR2) was significantly up-regulated in all atherosclerotic arteries studied. Previously, IFNGR1 and −2 have been found in carotid artery atheroma [62] but their role in the disease is not known. Its is though interesting to note that IFNGR1 acts as an major player in Th1 cell differentiation [63] and that IL4 has been found to prevent the association of IFNGRs in the antigen recognition [64]. In this study, the IL4 mRNA was low in atherosclerotic plaques. Whether the low IL4 expression could impact the function IFNGRs, remains to be evaluated in the future. In addition, it remains to be seen in the future whether the INFG mediated actions in atherosclerotic plaques could be modulated through manipulation of its receptors.
Limitations of the study
In this study, non atherosclerotic internal thoracic arteries (ITA) were used as control vessels in gene expression analysis. Even though comparison of the gene expression between healthy and diseased vessels from the same origin would have given more accurate results, unfortunately we were not able to obtain any healthy samples from the carotid or femoral arteries nor from the aortas due to ethical issues. We still believe that ITA vessels as controls provide valuable information for discovering the pathological biological processes going on in atherosclerotic plaques. It must be emphasized that the differences in hydrostatic pressure component in between the carotid and femoral territory, vascular compliance, and the differences in flow velocity in aorta compared with either carotid or femoral territory, result in huge variation in endothelial shear stress and artery wall radial load potentially modulating the gene expression. However, the present data still provides valuable information about the mechanism that hemodynamics may affect the development of atherosclerosis although the significance of this factor cannot be separately addressed in the present experimental setting. The gene expression profile may also be affected by differences in the cell type composition in different arterial beds which has not been characterized in the present study. A laser micro-dissection with appropriate mRNA quantitation method would provide cell specific information about the expression of genes. This technique has also previously been successfully applied to gene expression studies with atherosclerotic arteries [2], [65]. Another shortcoming is that the control vessels contained outer media and adventitia not present in atherosclerotic plaque samples. This approach may enrich the cell types present only in the intima and inner media of diseased vessels and thereby affecting gene expression results. Since the macrophages are the dominating type of inflammatory cells, the changes in macrophage related genes are also pronounced. It must be emphasized that the different sample groups were not adjusted for gender, age, lipid parameters or medication. At the present, the study population consisted of rather old (median age 70.0 years) subjects with a male predominance, majority having hypertension and history of smoking. This limits the generalization of the present results as the present data is limited to a high risk populations with severe symptoms and signs of atherosclerosis.
Conclusions
Atherosclerosis is a complex disease with numerous factors influencing disease development and phenotype. We analyzed advanced human atherosclerotic carotid and femoral artery plaques as well as aortas and screened all genes that were dysregulated in these arteries. In addition, we evaluated all the pathways and gene sets that were differentially expressed in diseased vessels. The study represents comprehensively the gene expression changes prevailing in three major advanced arterial beds and suggests several new, previously unknown genes to be involved in the disease pathogenesis. As the three major arterial beds; carotid, femoral, and aortic plaques were thoroughly studied in this study, the results serve also as an excellent reference for further studies in the future.
Supporting Information
Demographics of sample population.
(DOC)
Significantly up-regulated genes in human advanced atherosclerotic aorta.
(XLS)
Significantly down-regulated genes in human advanced atherosclerotic aorta.
(XLS)
Significantly up-regulated genes in human advanced atherosclerotic femoral artery.
(XLS)
Significantly down-regulated genes in human advanced atherosclerotic femoral artery.
(XLS)
Significantly up-regulated genes in human advanced atherosclerotic carotid artery.
(XLS)
Significantly down-regulated genes in human advanced atherosclerotic carotid artery.
(XLS)
Significantly altered pathways in advanced atherosclerotic plaques from arteries analyzed with gene set enrichment analysis (GSEA). All pathways are found in the MSigDB database.
(DOC)
The expression of nkTPathway genes in atherosclerotic plaques from carotid arteries, aortas and femoral arteries analyzed with TaqMan Low Density array. Fold changes are calculated by comparing the median expression of genes in atherosclerotic arteries vs. controls. Genes marked boldface represent a specific expression pattern dependable upon arterial bed.
(DOC)
Acknowledgments
The authors wish to thank Ms Nina Peltonen and Ms Ulla Jukarainen as well as Tomas Jonas and Janne Levula for their skillful technical assistance.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported with grants from the Medical Research Fund of Tampere University Hospital (TL), the Emil Aaltonen Foundation (TL), the Pirkanmaa Regional Fund of the Finnish Cultural Foundation, the Research Foundation of Orion Corporation, the Jenny and Antti Wihuri Foundation, and the Academy of Finland (grant no. 104821), the Finnish Foundation for Cardiovascular Research, the Yrjö Jahnsson Foundation and European Union 7th Framework Program, grant number 201668, Athroremo. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Tyson KL, Weissberg PL, Shanahan CM. Heterogeneity of gene expression in human atheroma unmasked using cDNA representational difference analysis. Physiol Genomics. 2002;9:121–130. doi: 10.1152/physiolgenomics.00116.2001. [DOI] [PubMed] [Google Scholar]
- 2.Tuomisto TT, Korkeela A, Rutanen J, Viita H, Brasen JH, et al. Gene expression in macrophage-rich inflammatory cell infiltrates in human atherosclerotic lesions as studied by laser microdissection and DNA array: overexpression of HMG-CoA reductase, colony stimulating factor receptors, CD11A/CD18 integrins, and interleukin receptors. Arterioscler Thromb Vasc Biol. 2003;23:2235–2240. doi: 10.1161/01.ATV.0000102551.91154.96. [DOI] [PubMed] [Google Scholar]
- 3.Seo D, Wang T, Dressman H, Herderick EE, Iversen ES, et al. Gene expression phenotypes of atherosclerosis. Arterioscler Thromb Vasc Biol. 2004;24:1922–1927. doi: 10.1161/01.ATV.0000141358.65242.1f. [DOI] [PubMed] [Google Scholar]
- 4.Randi AM, Biguzzi E, Falciani F, Merlini P, Blakemore S, et al. Identification of differentially expressed genes in coronary atherosclerotic plaques from patients with stable or unstable angina by cDNA array analysis. J Thromb Haemost. 2003;1:829–835. doi: 10.1046/j.1538-7836.2003.00113.x. [DOI] [PubMed] [Google Scholar]
- 5.King JY, Ferrara R, Tabibiazar R, Spin JM, Chen MM, et al. Pathway analysis of coronary atherosclerosis. Physiol Genomics. 2005;23:103–118. doi: 10.1152/physiolgenomics.00101.2005. [DOI] [PubMed] [Google Scholar]
- 6.Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb Vasc Biol. 1995;15:1512–1531. doi: 10.1161/01.atv.15.9.1512. [DOI] [PubMed] [Google Scholar]
- 7.Oksala N, Levula M, Airla N, Pelto-Huikko M, Ortiz RM, et al. ADAM-9, ADAM-15, and ADAM-17 are upregulated in macrophages in advanced human atherosclerotic plaques in aorta and carotid and femoral arteries–Tampere vascular study. Ann Med. 2009;41:279–290. doi: 10.1080/07853890802649738. [DOI] [PubMed] [Google Scholar]
- 8.Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, et al. Bioconductor: open software development for computational biology and bioinformatics. Genome Biol. 2004;5:R80. doi: 10.1186/gb-2004-5-10-r80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smyth G, editor. Limma: Linear Models For Microarray Data. 2005. Springer, New York.
- 10.Shi SR, Key ME, Kalra KL. Antigen retrieval in formalin-fixed, paraffin-embedded tissues: an enhancement method for immunohistochemical staining based on microwave oven heating of tissue sections. J Histochem Cytochem. 1991;39:741–748. doi: 10.1177/39.6.1709656. [DOI] [PubMed] [Google Scholar]
- 11.Raffetto JD, Khalil RA. Matrix metalloproteinases and their inhibitors in vascular remodeling and vascular disease. Biochem Pharmacol. 2008;75:346–359. doi: 10.1016/j.bcp.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenow K, Pearce NJ, Ramji DP. The key role of apolipoprotein E in atherosclerosis. J Mol Med. 2005;83:329–342. doi: 10.1007/s00109-004-0631-3. [DOI] [PubMed] [Google Scholar]
- 13.Singh M, Ananthula S, Milhorn DM, Krishnaswamy G, Singh K. Osteopontin: a novel inflammatory mediator of cardiovascular disease. Front Biosci. 2007;12:214–221. doi: 10.2741/2059. [DOI] [PubMed] [Google Scholar]
- 14.Cagnin S, Biscuola M, Patuzzo C, Trabetti E, Pasquali A, et al. Reconstruction and functional analysis of altered molecular pathways in human atherosclerotic arteries. BMC Genomics. 2009;10:13. doi: 10.1186/1471-2164-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baker EN, Baker HM. Molecular structure, binding properties and dynamics of lactoferrin. Cell Mol Life Sci. 2005;62:2531–2539. doi: 10.1007/s00018-005-5368-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci U S A. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chu CC, Paul WE. Fig1, an interleukin 4-induced mouse B cell gene isolated by cDNA representational difference analysis. Proc Natl Acad Sci U S A. 1997;94:2507–2512. doi: 10.1073/pnas.94.6.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carbonnelle-Puscian A, Copie-Bergman C, Baia M, Martin-Garcia N, Allory Y, et al. The novel immunosuppressive enzyme IL4I1 is expressed by neoplastic cells of several B-cell lymphomas and by tumor-associated macrophages. Leukemia. 2009;23:952–960. doi: 10.1038/leu.2008.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marquet J, Lasoudris F, Cousin C, Puiffe ML, Martin-Garcia N, et al. Dichotomy between factors inducing the immunosuppressive enzyme IL-4-induced gene 1 (IL4I1) in B lymphocytes and mononuclear phagocytes. Eur J Immunol. 40:2557–2568. doi: 10.1002/eji.201040428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maric M, Arunachalam B, Phan UT, Dong C, Garrett WS, et al. Defective antigen processing in GILT-free mice. Science. 2001;294:1361–1365. doi: 10.1126/science.1065500. [DOI] [PubMed] [Google Scholar]
- 21.Barjaktarevic I, Rahman A, Radoja S, Bogunovic B, Vollmer A, et al. Inhibitory role of IFN-gamma-inducible lysosomal thiol reductase in T cell activation. J Immunol. 2006;177:4369–4375. doi: 10.4049/jimmunol.177.7.4369. [DOI] [PubMed] [Google Scholar]
- 22.Zhou X. CD4+ T cells in atherosclerosis. Biomed Pharmacother. 2003;57:287–291. doi: 10.1016/s0753-3322(03)00082-9. [DOI] [PubMed] [Google Scholar]
- 23.Galkina E, Ley K. Immune and inflammatory mechanisms of atherosclerosis (*). Annu Rev Immunol. 2009;27:165–197. doi: 10.1146/annurev.immunol.021908.132620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salonen JT, Yla-Herttuala S, Yamamoto R, Butler S, Korpela H, et al. Autoantibody against oxidised LDL and progression of carotid atherosclerosis. Lancet. 1992;339:883–887. doi: 10.1016/0140-6736(92)90926-t. [DOI] [PubMed] [Google Scholar]
- 25.Lewis MJ, Malik TH, Ehrenstein MR, Boyle JJ, Botto M, et al. Immunoglobulin M is required for protection against atherosclerosis in low-density lipoprotein receptor-deficient mice. Circulation. 2009;120:417–426. doi: 10.1161/CIRCULATIONAHA.109.868158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brandtzaeg P, Johansen FE. Mucosal B cells: phenotypic characteristics, transcriptional regulation, and homing properties. Immunol Rev. 2005;206:32–63. doi: 10.1111/j.0105-2896.2005.00283.x. [DOI] [PubMed] [Google Scholar]
- 27.Hagg DA, Olson FJ, Kjelldahl J, Jernas M, Thelle DS, et al. Expression of chemokine (C-C motif) ligand 18 in human macrophages and atherosclerotic plaques. Atherosclerosis. 2008 doi: 10.1016/j.atherosclerosis.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 28.Reape TJ, Rayner K, Manning CD, Gee AN, Barnette MS, et al. Expression and cellular localization of the CC chemokines PARC and ELC in human atherosclerotic plaques. Am J Pathol. 1999;154:365–374. doi: 10.1016/S0002-9440(10)65283-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moratz C, Harrison K, Kehrl JH. Regulation of chemokine-induced lymphocyte migration by RGS proteins. Methods Enzymol. 2004;389:15–32. doi: 10.1016/S0076-6879(04)89002-5. [DOI] [PubMed] [Google Scholar]
- 30.Pellieux C, Desgeorges A, Pigeon CH, Chambaz C, Yin H, et al. Cap G, a gelsolin family protein modulating protective effects of unidirectional shear stress. J Biol Chem. 2003;278:29136–29144. doi: 10.1074/jbc.M300598200. [DOI] [PubMed] [Google Scholar]
- 31.Kingsbury GA, Feeney LA, Nong Y, Calandra SA, Murphy CJ, et al. Cloning, expression, and function of BLAME, a novel member of the CD2 family. J Immunol. 2001;166:5675–5680. doi: 10.4049/jimmunol.166.9.5675. [DOI] [PubMed] [Google Scholar]
- 32.Lim WC, Chow VT. Gene expression profiles of U937 human macrophages exposed to Chlamydophila pneumoniae and/or low density lipoprotein in five study models using differential display and real-time RT-PCR. Biochimie. 2006;88:367–377. doi: 10.1016/j.biochi.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 33.Tsuji S, Uehori J, Matsumoto M, Suzuki Y, Matsuhisa A, et al. Human intelectin is a novel soluble lectin that recognizes galactofuranose in carbohydrate chains of bacterial cell wall. J Biol Chem. 2001;276:23456–23463. doi: 10.1074/jbc.M103162200. [DOI] [PubMed] [Google Scholar]
- 34.Schaffler A, Neumeier M, Herfarth H, Furst A, Scholmerich J, et al. Genomic structure of human omentin, a new adipocytokine expressed in omental adipose tissue. Biochim Biophys Acta. 2005;1732:96–102. doi: 10.1016/j.bbaexp.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 35.Legrand D, Pierce A, Elass E, Carpentier M, Mariller C, et al. Lactoferrin structure and functions. Adv Exp Med Biol. 2008;606:163–194. doi: 10.1007/978-0-387-74087-4_6. [DOI] [PubMed] [Google Scholar]
- 36.Puddu P, Valenti P, Gessani S. Immunomodulatory effects of lactoferrin on antigen presenting cells. Biochimie. 2009;91:11–18. doi: 10.1016/j.biochi.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 37.Vengen IT, Dale AC, Wiseth R, Midthjell K, Videm V. Lactoferrin is a novel predictor of fatal ischemic heart disease in diabetes mellitus type 2: Long-term follow-up of the HUNT 1 study. Atherosclerosis. doi: 10.1016/j.atherosclerosis.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 38.Sahu BS, Sonawane PJ, Mahapatra NR. Chromogranin A: a novel susceptibility gene for essential hypertension. Cell Mol Life Sci. 67:861–874. doi: 10.1007/s00018-009-0208-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ferrero E, Magni E, Curnis F, Villa A, Ferrero ME, et al. Regulation of endothelial cell shape and barrier function by chromogranin A. Ann N Y Acad Sci. 2002;971:355–358. doi: 10.1111/j.1749-6632.2002.tb04495.x. [DOI] [PubMed] [Google Scholar]
- 40.Jansson AM, Rosjo H, Omland T, Karlsson T, Hartford M, et al. Prognostic value of circulating chromogranin A levels in acute coronary syndromes. Eur Heart J. 2009;30:25–32. doi: 10.1093/eurheartj/ehn513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mizuno M, Fujisawa R, Kuboki Y. Bone chondroadherin promotes attachment of osteoblastic cells to solid-state substrates and shows affinity to collagen. Calcif Tissue Int. 1996;59:163–167. doi: 10.1007/s002239900103. [DOI] [PubMed] [Google Scholar]
- 42.Camper L, Heinegard D, Lundgren-Akerlund E. Integrin alpha2beta1 is a receptor for the cartilage matrix protein chondroadherin. J Cell Biol. 1997;138:1159–1167. doi: 10.1083/jcb.138.5.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sjoberg AP, Manderson GA, Morgelin M, Day AJ, Heinegard D, et al. Short leucine-rich glycoproteins of the extracellular matrix display diverse patterns of complement interaction and activation. Mol Immunol. 2009;46:830–839. doi: 10.1016/j.molimm.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carlsson LE, Santoso S, Spitzer C, Kessler C, Greinacher A. The alpha2 gene coding sequence T807/A873 of the platelet collagen receptor integrin alpha2beta1 might be a genetic risk factor for the development of stroke in younger patients. Blood. 1999;93:3583–3586. [PubMed] [Google Scholar]
- 45.Grenache DG, Coleman T, Semenkovich CF, Santoro SA, Zutter MM. Alpha2beta1 integrin and development of atherosclerosis in a mouse model: assessment of risk. Arterioscler Thromb Vasc Biol. 2003;23:2104–2109. doi: 10.1161/01.ATV.0000097282.22923.EF. [DOI] [PubMed] [Google Scholar]
- 46.Haskard DO, Boyle JJ, Mason JC. The role of complement in atherosclerosis. Curr Opin Lipidol. 2008;19:478–482. doi: 10.1097/MOL.0b013e32830f4a06. [DOI] [PubMed] [Google Scholar]
- 47.Li F, Tian F, Wang L, Williamson IK, Sharifi BG, et al. Pleiotrophin (PTN) is expressed in vascularized human atherosclerotic plaques: IFN-{gamma}/JAK/STAT1 signaling is critical for the expression of PTN in macrophages. Faseb J. 24:810–822. doi: 10.1096/fj.09-140780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharifi BG, Zeng Z, Wang L, Song L, Chen H, et al. Pleiotrophin induces transdifferentiation of monocytes into functional endothelial cells. Arterioscler Thromb Vasc Biol. 2006;26:1273–1280. doi: 10.1161/01.ATV.0000222017.05085.8e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hansson GK, Robertson AK, Soderberg-Naucler C. Inflammation and atherosclerosis. Annu Rev Pathol. 2006;1:297–329. doi: 10.1146/annurev.pathol.1.110304.100100. [DOI] [PubMed] [Google Scholar]
- 50.Presky DH, Yang H, Minetti LJ, Chua AO, Nabavi N, et al. A functional interleukin 12 receptor complex is composed of two beta-type cytokine receptor subunits. Proc Natl Acad Sci U S A. 1996;93:14002–14007. doi: 10.1073/pnas.93.24.14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang X, Niessner A, Nakajima T, Ma-Krupa W, Kopecky SL, et al. Interleukin 12 induces T-cell recruitment into the atherosclerotic plaque. Circ Res. 2006;98:524–531. doi: 10.1161/01.RES.0000204452.46568.57. [DOI] [PubMed] [Google Scholar]
- 52.Pistoia V, Cocco C, Airoldi I. Interleukin-12 receptor beta2: from cytokine receptor to gatekeeper gene in human B-cell malignancies. J Clin Oncol. 2009;27:4809–4816. doi: 10.1200/JCO.2008.21.3579. [DOI] [PubMed] [Google Scholar]
- 53.Elkind MS, Rundek T, Sciacca RR, Ramas R, Chen HJ, et al. Interleukin-2 levels are associated with carotid artery intima-media thickness. Atherosclerosis. 2005;180:181–187. doi: 10.1016/j.atherosclerosis.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 54.Bogdan C, Vodovotz Y, Paik J, Xie QW, Nathan C. Mechanism of suppression of nitric oxide synthase expression by interleukin-4 in primary mouse macrophages. J Leukoc Biol. 1994;55:227–233. doi: 10.1002/jlb.55.2.227. [DOI] [PubMed] [Google Scholar]
- 55.Seder RA, Paul WE. Acquisition of lymphokine-producing phenotype by CD4+ T cells. Annu Rev Immunol. 1994;12:635–673. doi: 10.1146/annurev.iy.12.040194.003223. [DOI] [PubMed] [Google Scholar]
- 56.Davenport P, Tipping PG. The role of interleukin-4 and interleukin-12 in the progression of atherosclerosis in apolipoprotein E-deficient mice. Am J Pathol. 2003;163:1117–1125. doi: 10.1016/S0002-9440(10)63471-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nassar GM, Morrow JD, Roberts LJ, 2nd, Lakkis FG, Badr KF. Induction of 15-lipoxygenase by interleukin-13 in human blood monocytes. J Biol Chem. 1994;269:27631–27634. [PubMed] [Google Scholar]
- 58.Mallat Z, Gojova A, Marchiol-Fournigault C, Esposito B, Kamate C, et al. Inhibition of transforming growth factor-beta signaling accelerates atherosclerosis and induces an unstable plaque phenotype in mice. Circ Res. 2001;89:930–934. doi: 10.1161/hh2201.099415. [DOI] [PubMed] [Google Scholar]
- 59.Bursill CA, Channon KM, Greaves DR. The role of chemokines in atherosclerosis: recent evidence from experimental models and population genetics. Curr Opin Lipidol. 2004;15:145–149. doi: 10.1097/00041433-200404000-00007. [DOI] [PubMed] [Google Scholar]
- 60.Trogan E, Feig JE, Dogan S, Rothblat GH, Angeli V, et al. Gene expression changes in foam cells and the role of chemokine receptor CCR7 during atherosclerosis regression in ApoE-deficient mice. Proc Natl Acad Sci U S A. 2006;103:3781–3786. doi: 10.1073/pnas.0511043103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol. 2006;6:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- 62.Niedzielska I, Cierpka S. Interferon gamma in the etiology of atherosclerosis and periodontitis. Thromb Res. 126:324–327. doi: 10.1016/j.thromres.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 63.Maldonado RA, Soriano MA, Perdomo LC, Sigrist K, Irvine DJ, et al. Control of T helper cell differentiation through cytokine receptor inclusion in the immunological synapse. J Exp Med. 2009;206:877–892. doi: 10.1084/jem.20082900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maldonado RA, Irvine DJ, Schreiber R, Glimcher LH. A role for the immunological synapse in lineage commitment of CD4 lymphocytes. Nature. 2004;431:527–532. doi: 10.1038/nature02916. [DOI] [PubMed] [Google Scholar]
- 65.Stolle K, Weitkamp B, Rauterberg J, Lorkowski S, Cullen P. Laser microdissection-based analysis of mRNA expression in human coronary arteries with intimal thickening. J Histochem Cytochem. 2004;52:1511–1518. doi: 10.1369/jhc.4A6289.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Helle KB. Chromogranins: Universal proteins in secretory organelles from paramecium to man. Neurochemistry international. 1990;17:165–175. doi: 10.1016/0197-0186(90)90139-k. [DOI] [PubMed] [Google Scholar]
- 67.Corti A, Chromogranin A and the tumor microenvironment. Cellular and molecular neurobiology. 30:1163–1170. doi: 10.1007/s10571-010-9587-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Estensen ME, Hognestad A, Syversen U, Squire I, Ng L, et al. Prognostic value of plasma chromogranin A levels in patients with complicated myocardial infarction. American heart journal. 2006;152:927:e921–926. doi: 10.1016/j.ahj.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 69.Nguyen YK. Granulocyte colony stimulating factor. The Journal of the Florida Medical Association. 1994;81:467–469. [PubMed] [Google Scholar]
- 70.Sugiyama Y, Yagita Y, Oyama N, Terasaki Y, Omura-Matsuoka E, et al. Granulocyte colony-stimulating factor enhances arteriogenesis and ameliorates cerebral damage in a mouse model of ischemic stroke. Stroke; a journal of cerebral circulation. 42:770–775. doi: 10.1161/STROKEAHA.110.597799. [DOI] [PubMed] [Google Scholar]
- 71.Gjerstorff MF, Besir H, Larsen MR, Ditzel HJ. Expression, purification and characterization of the cancer-germline antigen GAGE12I: a candidate for cancer immunotherapy. Protein expression and purification. 73:217–222. doi: 10.1016/j.pep.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 72.Kular RK, Yehiely F, Kotlo KU, Cilensek ZM, Bedi R, et al. GAGE, an antiapoptotic protein binds and modulates the expression of nucleophosmin/B23 and interferon regulatory factor 1. J Interferon Cytokine Res. 2009;29:645–655. doi: 10.1089/jir.2008.0099. [DOI] [PubMed] [Google Scholar]
- 73.Marshall AJ, Du Q, Draves KE, Shikishima Y, HayGlass KT, et al. FDC-SP, a novel secreted protein expressed by follicular dendritic cells. J Immunol. 2002;169:2381–2389. doi: 10.4049/jimmunol.169.5.2381. [DOI] [PubMed] [Google Scholar]
- 74.Gjerstorff MF, Ditzel HJ. An overview of the GAGE cancer/testis antigen family with the inclusion of newly identified members. Tissue Antigens. 2008;71:187–192. doi: 10.1111/j.1399-0039.2007.00997.x. [DOI] [PubMed] [Google Scholar]
- 75.Xiao S, McLean J, Robertson J. Neuronal intermediate filaments and ALS: a new look at an old question. Biochim Biophys Acta. 2006;1762:1001–1012. doi: 10.1016/j.bbadis.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 76.Tedder TF, Klejman G, Schlossman SF, Saito H. Structure of the gene encoding the human B lymphocyte differentiation antigen CD20 (B1). J Immunol. 1989;142:2560–2568. [PubMed] [Google Scholar]
- 77.Fong KY. Immunotherapy in autoimmune diseases. Annals of the Academy of Medicine, Singapore. 2002;31:702–706. [PubMed] [Google Scholar]
- 78.Czuczman MS, Gregory SA. The future of CD20 monoclonal antibody therapy in B-cell malignancies. Leukemia & lymphoma. 51:983–994. doi: 10.3109/10428191003717746. [DOI] [PubMed] [Google Scholar]
- 79.Weigert J, Neumeier M, Schaffler A, Fleck M, Scholmerich J, et al. The adiponectin paralog CORS-26 has anti-inflammatory properties and is produced by human monocytic cells. FEBS Lett. 2005;579:5565–5570. doi: 10.1016/j.febslet.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 80.Mansson B, Wenglen C, Morgelin M, Saxne T, Heinegard D. Association of chondroadherin with collagen type II. J Biol Chem. 2001;276:32883–32888. doi: 10.1074/jbc.M101680200. [DOI] [PubMed] [Google Scholar]
- 81.Mikelis C, Koutsioumpa M, Papadimitriou E. Pleiotrophin as a possible new target for angiogenesis-related diseases and cancer. Recent patents on anti-cancer drug discovery. 2007;2:175–186. doi: 10.2174/157489207780832405. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Demographics of sample population.
(DOC)
Significantly up-regulated genes in human advanced atherosclerotic aorta.
(XLS)
Significantly down-regulated genes in human advanced atherosclerotic aorta.
(XLS)
Significantly up-regulated genes in human advanced atherosclerotic femoral artery.
(XLS)
Significantly down-regulated genes in human advanced atherosclerotic femoral artery.
(XLS)
Significantly up-regulated genes in human advanced atherosclerotic carotid artery.
(XLS)
Significantly down-regulated genes in human advanced atherosclerotic carotid artery.
(XLS)
Significantly altered pathways in advanced atherosclerotic plaques from arteries analyzed with gene set enrichment analysis (GSEA). All pathways are found in the MSigDB database.
(DOC)
The expression of nkTPathway genes in atherosclerotic plaques from carotid arteries, aortas and femoral arteries analyzed with TaqMan Low Density array. Fold changes are calculated by comparing the median expression of genes in atherosclerotic arteries vs. controls. Genes marked boldface represent a specific expression pattern dependable upon arterial bed.
(DOC)