Abstract
Chronic hepatitis B virus (HBV) infection is a preventable cause of liver failure, cirrhosis, and liver cancer; estimated chronic HBV infection prevalence is 0.3–0.5% in the USA. Prevalence in New York City (NYC) is likely higher because foreign-born persons, who represent 36% of NYC’s population versus 11% nationwide, bear a disproportionate burden of chronic HBV infection. However, because no comprehensive, population-based survey of chronic HBV infection has been conducted in NYC, a reliable prevalence estimate is unavailable. We used two approaches to estimate chronic HBV infection prevalence in NYC: (1) a census-based estimate, combining local and national prevalence data for specific populations, and (2) a surveillance-based estimate, using data from NYC’s Department of Health and Mental Hygiene Hepatitis B Surveillance Registry and adjusting for out-migration and deaths. Results from both the census-based estimate and the surveillance-based estimate were similar, with an estimated prevalence of chronic HBV in NYC of 1.2%. This estimate is two to four times the estimated prevalence for the USA as a whole. According to the census-based estimate, >93% of all cases in NYC are among persons who are foreign-born, and approximately half of those are among persons born in China. These findings underscore the importance of local data for tailoring programmatic efforts to specific foreign-born populations in NYC. In particular, Chinese-language programs and health education materials are critical. Reliable estimates are important for policymakers in local jurisdictions to better understand their own population’s needs and can help target primary care services, prevention materials, and education.
Keywords: Hepatitis B, Chronic, Prevalence, New York City
Introduction
Chronic hepatitis B virus (HBV) infection is a preventable cause of liver failure, cirrhosis, and liver cancer; estimated chronic HBV infection prevalence is 0.3–0.5% nationwide.1 Prevalence in New York City (NYC) is likely higher because foreign-born persons, who represent 36% of NYC’s population versus 11% nationwide,2 have a higher prevalence of chronic HBV infection.1,3 An understanding of the prevalence of chronic HBV in NYC is necessary for effective public health efforts. However, because no comprehensive, population-based survey of chronic HBV infection has been conducted in NYC, the prevalence is unknown.
The NYC Health Code requires healthcare providers and laboratories to report hepatitis B cases to the NYC Department of Health and Mental Hygiene (DOHMH). However, surveillance data cannot be used directly to measure prevalence for multiple reasons. First, persons who have been reported to the system might have died or moved away from NYC since the time of their last report; these cases are counted in the surveillance database but do not contribute to current prevalence. Second, persons with chronic HBV infection might be asymptomatic4,5 and, therefore, never tested or diagnosed. Consequently, they will not have been reported to the surveillance system.
The only population group in NYC that is mandated to be universally screened for HBV is pregnant women; by New York State law, all pregnant women in NYC and throughout the state are to be tested for hepatitis B surface antigen (HBsAg), the serologic marker of chronic hepatitis B infection, as part of routine prenatal care or at the time of delivery. Hepatitis B-positive pregnant and postpartum women are reported to the NYC DOHMH, Bureau of Immunization, Perinatal Hepatitis B Prevention Program. This program compiles this case report data along with additional demographic data that are collected from patient interview and medical chart reviews. It can be used to calculate hepatitis B prevalence; however, these data only reflect prevalence among pregnant women, who are not representative of the population at large.
We used two approaches to estimate the prevalence of chronic HBV infection in NYC: (1) a surveillance-based estimate, adjusting for out-migration and deaths, and (2) a census-based estimate, combining local and national prevalence data for specific population subgroups.
Methods
Method 1: Surveillance-Based Prevalence Estimate
The NYC Health Code requires healthcare providers and laboratories to report hepatitis B cases to the DOHMH, including positive results for: HBV surface antigen, HBV e antigen, and HBV nucleic acid test. Providers and laboratories report cases to the health department electronically, by fax, or by mail.6 All persons reported to the NYC DOHMH chronic HBV surveillance system during January 1, 1999–December 31, 2008, were included in an initial surveillance dataset. This dataset had previously been de-duplicated by using an automated probabilistic patient de-duplication algorithm, QualityStage® (International Business Machines, Corporation, Armonk, NY, USA). For each person, only the most recent report was retained in the dataset. Because a person who had been reported to the surveillance system might have died or migrated out of NYC since the time of last report, we adjusted for both death and out-migration. Additionally, we adjusted for duplicate records that were not identified by the automated de-duplication algorithm.
Adjusting for Death
To identify persons in the chronic HBV surveillance database who had died in NYC between the date of the last report through December 31, 2007, we matched records from the surveillance database to death certificate records from the NYC DOHMH Bureau of Vital Statistics. An automated algorithm, developed using SAS® 9.1 (SAS Institute, Cary, NC, USA), evaluated key patient identifiers from each dataset (e.g., name, date of birth, and address). Each potential match was assigned a score based on the number of identical and similar variables; higher scores reflected stronger matches. A threshold was determined by examining a sample of potential matches; potential matches with scores above the threshold were considered to be matches, and potential matches below the threshold were manually reviewed by two independent human reviewers to decide if they were matches. Ties were broken by a third reviewer.
Adjusting for Out-Migration from NYC
For each person in the surveillance database, we estimated the probability that that person had moved out of NYC between the date of last report and December 31, 2007 (Table 1). The yearly proportion of NYC residents who had moved out of NYC was estimated from the US Internal Revenue Service (IRS) annual tax return data.7 For each year from 2004 to 2007, the probability that a person had moved away from NYC (out-migration) was calculated directly from IRS data. Data for each year during 1999–2003 were unavailable; for those years, the probability that a person had moved away from NYC was assumed to be the average of the probability of out-migration during each of the years 2004–2007.
Table 1.
Estimating the probability that a person reported to the surveillance database during January 1, 1999–December 31, 2007, did not migrate out of New York City (NYC) during the time between the last report to the hepatitis B virus surveillance database and December 31, 2007
| Year of last report | Number of unique persons | Probability still in NYC in 2008a | Estimated number still in NYC in 2008 |
|---|---|---|---|
| 1999 | 6,145 | 0.6693 | 4,113 |
| 2000 | 5,720 | 0.6999 | 4,003 |
| 2001 | 6,502 | 0.7319 | 4,759 |
| 2002 | 7,634 | 0.7653 | 5,842 |
| 2003 | 7,316 | 0.8003 | 5,855 |
| 2004 | 8,944 | 0.8368 | 7,485 |
| 2005 | 9,795 | 0.8774 | 8,594 |
| 2006 | 11,000 | 0.9193 | 10,112 |
| 2007 | 13,044 | 0.9600 | 12,522 |
| 2008 | 18,263 | 1 | 18,263 |
| 2009 | 25,787 | 1 | 25,787 |
| 2010b | 1,832 | 1 | 1,832 |
| Total | 121,982 | 109,167 |
In cases where the year of last report was after December 31, 2007, the probability that that person was in NYC on December 31, 2007, was considered to be 1
aThe probability that a person was still in NYC in 2008 was calculated by multiplying the year-specific probabilities for each year since the person was last reported to the surveillance database. These probabilities, derived from US Internal Revenue Service data, were as follows: 2007–2008, 0.9600; 2006–2007, 0.9576; 2005–2006; 0.9544; 2004–2005, 0.9538; 2004–2005. For year intervals from 1999–2000 to 2003–2004, US Internal Revenue Service data were unavailable; for those years, an average of the probability of migration for 2004–2005 to 2007–2008 (0.9563) was used
bPartial data
Cases in the surveillance dataset that did not match to a NYC death certificate were stratified by the year of last report and multiplied by the probability that the person had moved from NYC since the year of last report. On the basis of these probabilities, an estimate of the number of reported cases still living in NYC as of 2008 was generated (Table 1).
Adjusting for Duplicates in the HBV Surveillance Database
To estimate the number of duplicate records in the HBV surveillance database after the automated de-duplication process, we calculated the proportion of death certificates that matched to two or more records in the surveillance dataset.
Method 2: Census-Based Prevalence Estimate
NYC’s population, as estimated from the 2008 US Census Bureau’s American Community Survey, was stratified into mutually exclusive groups, according to demographic factors relevant to chronic HBV infection risk. These groups were US-born non-institutionalized, foreign-born non-institutionalized, institutionalized in correctional facilities, and institutionalized not in correctional facilities. The foreign-born, non-institutionalized population was further stratified by country of birth.
For each group, we estimated the total population size in 2008 and reviewed local public health program data to identify the best source of chronic hepatitis B prevalence data; where local data were unavailable, estimates were drawn from national data. The best identified prevalence measure for each group was then multiplied by the 2008 population estimate for that group to generate an estimated number of persons in that group with chronic HBV in 2008. Estimated case counts were summed over all groups and divided by the total 2008 NYC population count to generate the final NYC prevalence estimate.
Estimating 2008 Population Size for Each Group
The total 2008 population of NYC was drawn from the 2008 American Community Survey.8 The proportion of the population in each group, including country of birth for those born outside the USA, was drawn from the 2000 US decennial census.9,10 For each group, we multiplied the proportion represented by that group in the 2000 Census by the total NYC population from the 2008 American Community Survey.
Estimating Chronic HBV Prevalence for Each Group
US-Born Non-Institutionalized Population
For the US-born non-institutionalized population, we used the same estimated prevalence that had been used previously in a national estimate for the USA;1 this estimate was derived from the National Health and Nutrition Survey.
Foreign-Born Non-Institutionalized Population
For the foreign-born non-institutionalized population, prevalence estimates were drawn from NYC DOHMH’s Perinatal Hepatitis B Prevention Program (PHBPP) for births to NYC residents during 1995–2006. For each specific country of origin, a country-specific prevalence estimate was calculated as the number of chronic HBV-positive cases identified among women born in country X who gave birth in NYC, divided by the total number of births in NYC to women born in country X during the same period. The 95% confidence interval (CI) for each country-specific prevalence estimate was calculated using the normal approximation method of the binomial CI. PHBPP data reflect the prevalence among women who gave birth in NYC. The prevalence of chronic HBV has been observed to be consistently higher among men than women, with a prevalence ratio ranging from 1.4 to 2.3;3,11,12 therefore, we adjusted the prevalence estimate to account for the sex disparity, conservatively assuming a prevalence ratio of 1.5 between men and women.
For each country i, Pi-sex-adjusted is the sex-adjusted prevalence, as follows:
 |
where, for each country i, mi is the measured prevalence of HBV among women born in that country who gave birth in NYC during 1995–2006, and R is the estimated ratio of HBV among males compared with females. The lower and upper bounds of the 95% CI for each country-specific prevalence estimate were similarly adjusted in order to determine low and high estimates. R was assumed to be 1.5 for all countries.
For each country, we calculated the expected case count by multiplying the country-specific prevalence by size of the population of NYC residents who were born in that country; low and high estimates of expected case counts were similarly calculated using low and high country-specific prevalence estimates. These country-specific counts were then summed over all countries and divided by the total population size of NYC’s foreign-born population to derive a prevalence estimate, as follows:
Pforeign-born is the estimated prevalence among the foreign-born,
 |
where, C is the number of foreign-born persons residing in NYC, and n is the number of distinct countries of birth represented. For each country i→n, pi is the measured country-specific prevalence, and ci is the number of NYC residents who were born in that country. Low and high prevalence estimates for NYC’s foreign-born population were similarly calculated by summing country-specific low and high counts, respectively, over all countries and dividing by the total population size of NYC’s foreign-born population.
Institutionalized Population in Correctional Facilities
For the correctional population, the HBV prevalence measure was drawn from a 2006 serosurvey at the main jail in NYC, which was conducted by NYC DOHMH as part of a larger survey that included human immunodeficiency virus and hepatitis C testing (Farah Parvez, personal communication, 2008).13 The 95% CI was calculated using the normal approximation method of the binomial CI.
Other Institutionalized Population
The other institutionalized population includes persons under the care or supervision of trained staff and classified as “patients” or “inmates” in juvenile institutions, nursing homes, and hospitals for the chronically ill. Because no data sources exist for this population, the prevalence was estimated to be the mean estimated prevalence of the other groups combined (non-institutionalized US- and foreign-born and the institutionalized population in correctional facilities). To determine the sensitivity of our final estimate to this assumption, we conducted a sensitivity analysis, varying the prevalence for this population from that of the lowest prevalence group (US-born, non-institutionalized), to that of the highest prevalence group (institutionalized population in correctional facilities).
Calculating the Full NYC Census-Based Prevalence Estimate
Group-specific prevalence figures were multiplied by the estimated population size for that group to generate an estimated number of persons with chronic HBV infection. These case counts were then summed across all groups and divided by the total 2008 NYC estimated population to estimate the HBV prevalence for the full population of NYC in 2008. To calculate low and high prevalence estimates for the full population of NYC in 2008, low and high case counts, respectively, for each group were summed and divided by the total 2008 NYC estimated population.
Results
Surveillance-Based Estimate
A total of 126,418 unique persons were reported to the NYC DOHMH chronic HBV surveillance system during January 1, 1999–December 31, 2008, as determined by the automated de-duplication algorithm. Of these, 4,436 (3.5%) matched to an NYC death certificate with a date of death on or before December 31, 2007, leaving 121,982 persons. Additionally, this match revealed that among the 4,436 matching death certificates, 415 (9.4%) matched with two or more records in the surveillance dataset.
Of 121,982 remaining persons, we used IRS data to estimate that 12,815 had outmigrated from NYC since the time that they were last reported to the chronic HBV surveillance system, leaving an estimated 109,167 still living in NYC as of January 1, 2008. The estimate was reduced by 9.4% (10,262), which was the estimated number of duplicate records in the database after the automated de-duplication algorithm. This left 98,905 cases; this number was divided by the 2008 population estimate for NYC to generate a final estimated prevalence of diagnosed chronic hepatitis B in NYC of 1.2%.
Census-Based HBV Prevalence Estimate
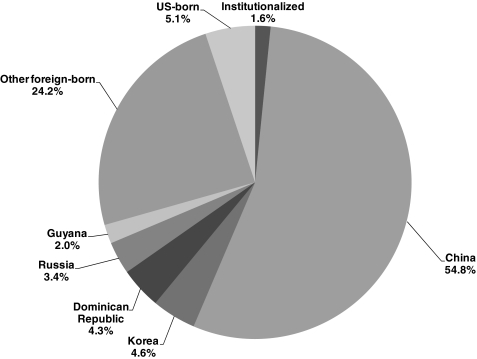
The census-based estimate for the prevalence of chronic hepatitis B in NYC was 1.2% (range, 1.1–1.4%). Among foreign-born NYC residents, the census-based prevalence estimate was 3.2% (range 2.9–3.4%). NYC residents born in China accounted for 55% of all estimated NYC cases (Figure 1). Prevalence for other population groups ranged from 0.1% among the US-born non-institutionalized population to 4.3% among the correctional population (Table 2).
FIGURE 1.
Distribution of country of birth and institutionalized status among residents of NYC with chronic hepatitis B, 2008, as calculated by using the census-based estimation method.
Table 2.
Estimated prevalence of chronic hepatitis B in New York City (NYC), January 1, 2008, as calculated by using the census-based estimation method
| Group | NYC population estimate | Data source (year) | Prevalence (%) | Expected count no. |
|---|---|---|---|---|
| Non-institutionalized | ||||
| US born | 5,286,015 | NHANES (1999–2004) | 0.1 (95% CI = 0.1–0.2) | 5,286 (5,286–10,572) |
| Foreign born | 2,998,457 | PHBPPa data (1995–2006) | 3.2 (range = 2.9–3.4) | 95,951 (86,955–101,948) |
| Institutionalized | ||||
| Correctional facility | 22,352 | NYC correctional health screening data (2006) | 4.3 (95% CI = 3.8–4.8) | 961 (849–1,073) |
| Other group living quarters | 56,886 | b | 1.2 (range = 1.1–1.4) | 671 (626–796) |
| Total | 8,363,710 | 1.2 (range = 1.1–1.4) | 102,869 (93,716–114,389) | |
CI confidence interval, NHANES National Health and Nutrition Examination Survey
aNew York City DOHMH Perinatal Hepatitis B Prevention Program (PHBPP).
bThe prevalence among NYC residents institutionalized in other group living quarters was estimated as the mean prevalence of other groups combined
A sensitivity analysis of the impact of the assumption that the prevalence among the other institutionalized population was the mean prevalence of all other groups combined demonstrated that the impact of this assumption was minimal. Varying the prevalence for this group from 0.1% to 4.3% resulted in final estimates for the prevalence of chronic HBV in NYC of 1.2–1.3%.
Discussion
We estimated the prevalence of chronic HBV in NYC to be 1.2% by using two independent methods: a census-based method and a surveillance-based method. Our estimate was two to four times the estimated prevalence in the USA overall, where the prevalence has been estimated to be 0.3–0.5%.1
The true prevalence of chronic HBV in NYC might be higher than these estimates indicate. The surveillance-based method, based on NYC DOHMH’s chronic HBV surveillance data, captures only those cases reported to the health department; it does not capture cases among persons who have never been tested or who were tested but not reported in NYC. The number of cases among persons who have never been tested is unknown, but likely substantial. A cross-sectional study of hepatitis B among Asian–Americans in California reported that half to two thirds of chronically infected adults were not aware of their infection.12 If a similar number of chronically infected persons in NYC remain undiagnosed, the surveillance-based approach indicates the true prevalence of chronic HBV in NYC might be ≥2.4%. By contrast, we might have underestimated the number of persons with reported chronic HBV infection who migrated out of NYC. County-to-county migration data from the IRS only captures migration among those who file yearly federal tax returns. This might not accurately represent migration among NYC residents with hepatitis B, many of whom are recent immigrants, and might therefore be more mobile and more likely to move out of NYC in a given year. Those who are not required to file federal income tax returns (e.g., the poor and older persons) are underrepresented in this data source.14 In addition, those who are required but do not file federal income tax returns will not be represented in this data source. The surveillance-based approach cannot be used to estimate the distribution of country of birth because the reporting source of surveillance data is mainly from laboratories that do not receive and therefore cannot report patient country of birth data.
The census-based estimate is not limited by biases in testing or reporting because it relies upon prevalence estimates generated through universal screening among specific populations or stratified random samples. However, the populations that were screened (e.g., pregnant women) might not accurately reflect the population in NYC. Our adjustment for differences in the prevalence by sex among the foreign-born might have limitations; for example, the prevalence ratio between men and women might differ in different countries, and the prevalence ratios we identified in the literature might not reflect the true prevalence ratio among NYC’s foreign-born. Reliance on PHBPP data to estimate chronic HBV prevalence among the foreign-born population also meant that we did not capture differences in prevalence among foreign-born persons who are younger or older than reproductive age; prevalence among these groups is likely different from that observed among the reproductive-age population. Additionally, PHBPP does not reflect prevalence among all reproductive-age women. Differences in risk might exist between women who become pregnant and those who do not become pregnant, or differences might exist in HBV prevalence between pregnant women who choose to give birth versus those who terminate their pregnancy before they have prenatal care and are tested for hepatitis B.
Women giving birth to multiple children in NYC during 1995–2006 were represented multiple times in the PHBPP dataset. This is unlikely to impact our estimate, however, unless the prevalence of chronic HBV among women with multiple births during 1995–2006 differed substantially from the prevalence of chronic HBV among women with only a single birth during 1995–2006. Additionally, PHBPP data for the period 2007–2008 was not available; if the prevalence of chronic HBV among women giving birth in NYC during 2007–2008 was substantially higher or lower in some groups than it was during 1995–2006, it is possible that this would result in a higher or lower estimate of the overall prevalence in 2008. However, we have no information that suggests that this is the case. Finally, certain populations with a higher chronic HBV prevalence are not accounted for in our approach (e.g., men who have sex with men who might be disproportionately infected with HBV).15
An advantage of the census-based estimate is that it allowed us to estimate HBV prevalence among different population groups and therefore understand how to most effectively distribute resources. According to this approach, >93% of all cases in NYC are among persons who are foreign-born; of these, >50% are among persons born in China. This finding underscores the need to prioritize programmatic efforts tailored to specific foreign-born populations in NYC; Chinese-language programs and health-education materials are especially critical. Recent evidence suggests that prevalence of chronic HBV infection declined in the USA between 1988–2004 and 1999–2008 among younger age groups, likely resulting from the introduction of an effective vaccine against HBV and routine vaccination of infants beginning in the early 1990s.16 Because >93% of chronic HBV cases in NYC are among persons born outside of the USA, these trends are unlikely to have a substantial impact on the prevalence of HBV in NYC.
Such estimates as these, which are based primarily on local data, are important for policymakers in local jurisdictions to better understand the patterns of disease in their area. This knowledge provides information on which to base decisions about which population groups need to be prioritized in the delivery of primary care services and development of prevention programs and educational materials. With these data, local jurisdictions are able to prioritize and request support for programs that serve the language and cultural needs of those specific foreign-born populations who are disproportionately affected. For example, local data provide jurisdictions justification to request support for (1) programs that work directly with the infected population, (2) programs having the bilingual staff who are also sensitive to cultural concerns, (3) health education programs that are able to develop culturally appropriate health-education materials in languages other than English, and (4) media programs that are able to produce translated and culturally appropriate public service announcements.
The surveillance-based estimate also demonstrates the utility of chronic hepatitis B surveillance. Although surveillance for chronic hepatitis can be resource-intensive because of the vast number of reports, de-duplication challenges, and the need to make adjustments to the data to estimate prevalence, such estimates are important for developing disease control programs at the local level. This study demonstrates that with adjustment, surveillance data can provide reliable estimates of local prevalence. National estimates do not always help local jurisdictions with planning, especially in the case of such diseases as hepatitis B for which the prevalence is highly influenced by immigration; local prevalence might differ substantially from national prevalence. Additionally, surveillance systems allow for in-depth investigation of a sample to better understand the clinical and epidemiologic characteristics of the disease among the local population; such an investigation is under way in NYC. Finally, surveillance datasets can be valuable in investigating outbreaks of hepatitis B that have occurred with increasing frequency in health care settings17 by providing data on which patients have been reported with chronic hepatitis B previously.
This analysis demonstrates that approximately 100,000 persons, a prevalence of 1.2%, have chronic hepatitis B infection in NYC. Increased support is needed to strengthen surveillance systems, both locally and nationally, and improve treatment and prevention programs that can reach affected immigrant communities effectively.
Acknowledgments
The authors thank Kevin Konty, PhD, at the New York City Department of Health and Mental Hygiene, Bureau of Epidemiology, for consultation on the methods used in these analyses as well as for helpful feedback on the manuscript.
Funding
This study was made possible in part by funding from the Centers for Disease Control and Prevention Emerging Infections Program.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Centers for Disease Control and Prevention Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57(No. RR-8):1–20. [PubMed] [Google Scholar]
- 2.US Census Bureau. State & county QuickFacts: New York City, New York. Washington, DC: US Census Bureau. http://quickfacts.census.gov. Accessed December 10, 2010.
- 3.McQuillan GM, Coleman PJ, Kruszon-Moran D, Moyer LA, Lambert SB, Margolis HS. Prevalence of hepatitis B virus infection in the United States: the National Health and Nutrition Examination Surveys, 1976 through 1994. Am J Public Health. 1999;89:14–18. doi: 10.2105/AJPH.89.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright TL. Introduction to chronic hepatitis B infection. Am J Gastroenterol. 2006;101(Suppl 1):S1–S6. doi: 10.1111/j.1572-0241.2006.00469.x. [DOI] [PubMed] [Google Scholar]
- 5.Carey WD. The prevalence and natural history of hepatitis B in the 21st century. Clevel Clin J Med. 2009;76(Suppl 3):S2–S5. doi: 10.3949/ccjm.76.s3.01. [DOI] [PubMed] [Google Scholar]
- 6.New York City Department of Health and Mental Hygiene. Hepatitis A, B and C Surveillance Report, New York City, 2008 and 2009. New York, NY: New York City Department of Health and Mental Hygiene. http://www.nyc.gov/html/doh/downloads/pdf/cd/cd-hepabc-surveillance-report-08-09.pdf. Accessed June 29, 2011.
- 7.US Internal Revenue Service (IRS). County to county migration data: 2004–2008. Washington, DC: IRS. http://www.irs.gov/taxstats/article/0,,id=212695,00.html. Accessed January 6, 2011.
- 8.US Census Bureau. 2008 American Community Survey 1-year estimates, table B01003. total population—universe: total population, New York City, 2008. Washington, DC: US Census Bureau. http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=ACS&_lang=en&_ts=?. Accessed January 6, 2011.
- 9.US Census Bureau. Census 2000 summary file 1: New York City, 2001. Washington, DC: US Census Bureau. http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=DEC&_submenuId=datasets_2&_lang=en&_ts=. Accessed January 6, 2011.
- 10.US Census Bureau. Census 2000 summary file 3: New York City, 2001. Washington, DC: US Census Bureau. http://factfinder.census.gov/servlet/DatasetMainPageServlet?_program=DEC&_submenuId=datasets_2&_lang=en&_ts=. Accessed January 6, 2011.
- 11.Centers for Disease Control and Prevention Screening for chronic hepatitis B among Asian/Pacific Islander populations—New York City, 2005. MMWR Morb Mortal Wkly Rep. 2006;55:505–509. [PubMed] [Google Scholar]
- 12.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46:1034–1040. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 13.Begier EM, Bennani Y, Forgione L, Punsalang A, Hanna DB, Herrera J, Torian L, Gbur M, Sepkowitz KA, Parvez F. Undiagnosed HIV infection among New York City jail entrants, 2006: results of a blinded serosurvey. J Acquir Immune Defic Syndr. 2010;54:93–101. doi: 10.1097/QAI.0b013e3181c98fa8. [DOI] [PubMed] [Google Scholar]
- 14.Gross E. US population migration data: strengths and limitations; Statistics of Income Division, Internal Revenue Service; 2005. www.irs.gov/pub/irs-soi/99gross_update.doc. Accessed January 6, 2011.
- 15.Gunn RA, Murray PJ, Ackers ML, Hardison WG, Margolis HS. Screening for chronic hepatitis B and C virus infections in an urban sexually transmitted disease clinic: rationale for integrating services. Sex Transm Dis. 2001;28:166–170. doi: 10.1097/00007435-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Ioannou GN. Hepatitis B virus in the United States: infection, exposure, and immunity rates in a nationally representative survey. Ann Intern Med. 2011;154:319–328. doi: 10.7326/0003-4819-154-5-201103010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Lanini S, Puro V, Lauria FN, Fusco FM, Nisii C, Ippolito G. Patient to patient transmission of hepatitis B virus: a systematic review of reports on outbreaks between 1992 and 2007. BMC Med. 2009;7:15–23. doi: 10.1186/1741-7015-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]