Abstract
Injection drug use (IDU) into central veins, most common among long-term IDUs with no other options, can lead to severe infectious, vascular, and traumatic medical consequences. To follow-up on anecdotal reports of femoral vein injection and related medical problems in Seattle, we analyzed data from the annual survey of a community-based syringe exchange program. A total of 276 (81%) of 343 program attendees completed the survey in August 2010. Among 248 IDUs, 66% were male, 78% white, and 86% primarily injected opiates. One hundred respondents (40%) had injected into the femoral vein, 55% of whom were actively doing so, and 58% of whom reported medical complications that they attributed to the practice. Most (66%) used the femoral vein due to difficulty accessing other veins, although 61% reported other veins they could access and 67% reporting using other sites since initiating femoral injection. While injecting into muscle was more frequent among older IDUs with longer injection careers, the prevalence of femoral injection was highest among respondents in their late twenties with 2.5–6 years of injecting drugs. Multivariate analysis demonstrated an increased risk of initiating femoral injection each calendar year after 2007. Injecting into the femoral vein was also associated with white versus other race (odds ratio [OR] 2.7, 95% CI 1.3–5.4) and injection of primarily opiates versus other drugs (OR 6.3, 95% CI 1.2–32.9) and not associated with age, length of IDU career, or a history of injecting into muscle. These findings suggest a secular trend of increasing femoral injection among Seattle-area IDUs with a high rate of related medical problems. Interventions, such as education regarding the hazards of central venous injection and guidance on safe injection into peripheral veins, are needed to minimize the health consequences of femoral injection.
Keywords: Injection drug use, Femoral injection, Femoral vein, Syringe exchange
Introduction
Injection drug users (IDUs) frequently have difficulty sustaining venous access.1 Black tar heroin, the principal form of the drug found in the western half of the United States, is particularly caustic to veins.2 IDUs often resort to intramuscular injection or skin-popping when peripheral veins become difficult to access, resulting in a high frequency of skin and soft tissue infections. 2,3 Accessing central veins, often the internal jugular vein, is traditionally felt to be a “last resort” among long-term IDUs with no other options.4
Central venous injection into the deep femoral vein (“femoral injection”) has been considered a rare phenomenon among IDUs5 that, when reported, occurred late in an injection career.6 A recent report from the UK, however, documented the practice in about half of IDUs in selected cities7 relatively early in their injecting careers,8 and a qualitative analysis determined that femoral injection may have emerged as an “acceptable risk” among crack-heroin speedball users.9 Femoral injection may be preferred over peripheral injection not only due to difficulty finding other veins, but also due to access that is quick (to avoid detection), easy (due to large size of femoral vein and development of a sinus tract) and reliable (less likely to miss the vein altogether or have to repeat injection), a possibly superior “rush,” and the lack of visible track marks when clothed.9 On the other hand, femoral injection has been associated with a number of deleterious medical consequences, including deep vein thrombosis,10 septic thrombophlebitis,11 abscesses,12 damage of the femoral nerve,13 femoral artery necrosis,14 and arteriovenous fistula5 or pseudoaneurysm.15
It is not known whether the increase in femoral injection observed in the UK is an isolated phenomenon or more widespread. Femoral vein injection and related medical complications have been reported anecdotally recently in the Seattle area. To evaluate the prevalence, correlates, and consequences of this practice, the Peoples’ Harm Reduction Alliance (PHRA), collected data on the practice as part of their annual program evaluation.
Methods
We analyzed data from a cross-sectional, anonymous survey undertaken as an evaluation activity by the PHRA, a community-based syringe exchange and harm reduction program that serves IDUs and crack smokers. The evaluation consisted of a survey administered by trained interviewers who volunteer at PHRA, and was developed by staff and piloted with five participants prior to finalization. Survey questions collected data on participants’ gender, age, race, sexual preference, drug preference, preferred route of administration, length of injection drug use, and experiences with opioid overdose. Questions addressing femoral injection included whether the respondent had “ever injected” into their femoral vein, how long they had been doing so, if they were “still injecting” into their femoral vein, reasons for initiating femoral injection, where they learned about the practice, and what, if any, medical problems they had experienced that they attributed to femoral injection. Staff approached each participant after completion of exchange services during all 40 operating hours over 2 weeks in August 2010 and asked if they would be interested in completing an approximately 2-min survey. Consent was verbal and a piece of candy was provided as incentive. Participants who had previously completed the survey were excluded. If participants refused, staff visually estimated age and race on the survey form. The University of Washington Human Subjects Division determined that this analysis was exempt from review due to the use of anonymous, secondary data.
Data analysis was conducted with STATA 11.1, utilizing descriptive statistics, Pearson’s chi-square, unpaired t-test, and logistic regression. Length of time injecting and length of time femoral injecting were grouped as quartiles for bivariate analysis. For multivariate analysis, we generated dummy variables for length of time injecting drugs and for femoral injection for each year from 2004, the most remote year in which participants reported femoral injection. Data were censored each year after the first year respondents reported femoral injection. Logistic regression was performed with basic demographics and variables significant on bivariate analysis. Missing values were excluded.
Results
Staff approached all persons receiving syringe exchange or crack kit services through the program and 276 (81%) of 343 completed the survey. There were no significant differences in age or race, as estimated by staff, between those who completed the survey and those who declined (data not shown). We analyzed data from the 248 respondents who had injected drugs (see Table 1 for detailed demographics). A majority of respondents (56%) had ever muscled and 40% had injected into the femoral vein.
Table 1.
Characteristics of injection drug users by history of femoral injection
| No femoral | Femoral | Total | |
|---|---|---|---|
| Number (%) | Number (%) | Number (%) | |
| Total | 148 (59.7) | 100 (40.3) | 248 (100%) |
| Gender | |||
| Male | 94 (64.0) | 70 (70.0) | 164 (66.4) |
| Female | 52 (35.4) | 30 (30.0) | 82 (33.2) |
| Transgender | 1 (0.7) | 0 (0.0) | 1 (0.4) |
| Age* | |||
| Under 25 | 46 (31.5) | 26 (26.3) | 72 (29.4) |
| 26–30 | 24 (16.4) | 24 (24.2) | 48 (19.6) |
| 31–45 | 31 (21.2) | 32 (32.3) | 63 (25.7) |
| Over 45 | 45 (30.8) | 17 (17.2) | 62 (25.3) |
| Race/ethnicity | |||
| White | 108 (73.0) | 85 (85.9) | 193 (78.1) |
| African-American | 6 (4.1) | 4 (4.0) | 10 (4.1) |
| Asian/Pacific Islander | 6 (4.1) | 3 (3.0) | 9 (3.6) |
| Native American | 10 (6.8) | 3 (3.0) | 13 (5.3) |
| Latino | 11 (7.4) | 1 (1.0) | 12 (4.9) |
| Mixed | 7 (4.7) | 3 (3.0) | 10 (4.1) |
| Drug of Choice (sum exceeds 100%) | |||
| Opiates*** | 116 (80.0) | 94 (95.9) | 210 (86.4) |
| Cocaine | 34 (23.5) | 22 (22.5) | 56 (23.1) |
| Methamphetamine* | 24 (16.6) | 7 (7.1) | 31 (12.8) |
| Other | 21 (8.6) | ||
| Length of time injecting (in quartiles) | |||
| 1 month to 2 years | 58 (39.2) | 19 (19.9) | 77 (31.2) |
| 2.5 to 6 years | 22 (14.9) | 27 (27.3) | 50 (20.2) |
| 7 to 15 years | 38 (25.7) | 28 (28.3) | 67 (27.1) |
| 16 to 48 years | 30 (20.3) | 25 (25.3) | 53 (21.5) |
| Ever muscled** | |||
| No | 73 (50.7) | 32 (33.3) | 105 (43.8) |
| Yes | 71 (49.3) | 64 (66.7) | 135 (56.3) |
*p < 0.05, **p < 0.01, ***p < 0.001
Among 100 lifetime femoral injectors (see Table 2), 55 (55%) reported that they were “still injecting” into their femoral vein. In response to an open-ended query, 58 (66%) reported femoral injection because they had problems accessing other veins, although 14 (16%) did so because it was quick or easy; only two (2%) were trying to avoid track marks. Reason for using the femoral vein was collapsed into a binary variable (see Table 2) of vein problems (N = 68, 77%) versus other reasons (N = 20, 23%) for further analysis and showed no association with age or length of time injecting drugs. Fifty-nine (61%) of those who ever injected into their femoral vein reported that they still had other veins that they could access and 64 (67%) had used other sites since accessing the femoral vein; despite this, almost half of each of these groups (44% and 47%, respectively) reported continuing to inject into the femoral vein.
Table 2.
Characteristics of injection drug users with a history of femoral injection (N = 100)
| Still injecting into femoral vein | Number (%) |
| No | 45 (45.0) |
| Yes | 55 (55.0) |
| Time since first femoral injection | |
| 1 day to 1 month | 27 (29.7) |
| 1.5 to 6 months | 21 (23.1) |
| 8 months to 2 years | 27 (29.7) |
| 3 to 6 years | 16 (17.6) |
| Source of femoral injecting information | |
| Friend/acquaintance/family | 76 (79.2) |
| Self-taught/Internet | 17 (17.7) |
| Healthcare worker | 5 (5.2) |
| Reason for femoral injecting | |
| Vein problems | |
| Difficulty accessing veins | 58 (65.9) |
| No other options/problems with muscling | 6 (6.8) |
| No veins and didn’t want to muscle | 4 (4.6) |
| Other reasons | |
| Quick or easy | 14 (15.9) |
| Recommended by another person/wanted to try something new | 6 (6.8) |
| Avoid track marks | 2 (2.3) |
| Better rush | 1 (1.1) |
| No small needles available at time of injection | 1 (1.1) |
| Had other veins that could be used | |
| No | 38 (39.2) |
| Yes | 59 (60.8) |
| Injected into other sites since femoral | |
| No | 31 (32.6) |
| Yes | 64 (67.4) |
Among the 100 respondents reporting femoral injection, 58 (58%) reported medical problems that they attributed to femoral injection. Complications included pain at the site (28%), skin or soft tissue infections (27%), swelling in the legs (23%), blood clots (17%), femoral artery or nerve injury (10%), hospitalization (10%), leg ulceration (5%), endocarditis (5%), and other problems (10%). Complications related to blood clots or venous stasis disease were reported by 35 femoral injectors. Seven reported no problems other than pain at the site.
We conducted exploratory bivariate analyses of femoral injectors, those who continued to inject into the femoral vein, and those who experienced problems related to the practice. Persons who injected into their femoral vein were more likely to be non-Hispanic whites compared to other race or ethnicity (44% vs. 26%, p < 0.05), to use primarily opiates (45%) compared to cocaine (39%) or methamphetamines (23%, p < 0.001), and to have muscled compared to never having muscled (47% vs. 31%, p < 0.01). Those who were actively injecting into the femoral vein were more likely to be younger (p < 0.05) and to report not having other veins to use (p < 0.01). Those who reported medical problems from femoral injection were less likely to report having other veins they could use (p < 0.05) and more likely to still be injecting into the femoral vein at the time of the survey (p < 0.05).
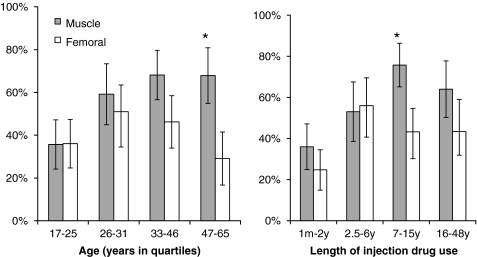
Femoral injecting and muscling displayed different associations with age and number of years injecting. While muscling was associated with older age and higher number of years injecting, femoral injecting was most common among IDUs aged 26–31 years and persons who had been injecting 2.5–6 years (Figure 1). Given that cocaine injection might produce different patterns of vein and muscle use than opiate injection, we compared rates of femoral injection among respondents reporting only opiates as their primary injected drug (43%) to those who reported both opiates and cocaine (51%), and found no significant difference.
Figure 1.
Proportion of injection drug users that have ever muscled or injected into the femoral vein by age and length of injection career; *p < 0.001 by unpaired t-test.
The median length of time injecting drugs was 5 years (range 1 month–48 years) and of femoral injecting was 8 months (range 1 day–6 years). No respondent reported femoral injection more than 6 years prior to the time of the survey and increasing numbers reported femoral injection each subsequent year, thus we generated a multivariate logistic regression model to examine the effect of calendar year on the likelihood of initiating femoral injection. Compared to calendar year 2004, the first year any respondent reported femoral injection, calendar years 2008 (odds ratio [OR] 5.32, 95% CI 1.23–24.99) and 2009 (OR 10.99, 95% CI 2.46–49.11) and 2010 (OR 40.75, 95% CI 9.57–173.47) were significantly associated with initiating femoral injection. Adjusting for demographics and significant findings on bivariate analysis, initiation of femoral injection was more likely for white versus non-white respondents (OR 2.69, 95% CI 1.33–5.43) and those whose drug of choice was opiates versus other drugs (OR 6.30, 95% CI 1.21–32.93); sex, age, a history of muscling, and the number of years injecting drugs by calendar year were not associated with the outcome.
Discussion
We found that a high proportion of IDUs attending a community-based syringe exchange program in Seattle reported injecting into their femoral vein and that most had initiated the practice within the past several years. These findings suggest that femoral injection may be becoming more common in this region and confirm a high frequency of related health consequences.
Our findings differ from older data in which long-term IDUs access central veins as a last resort16 and are consistent with recent trends toward normalization of femoral injection seen in Australia and the United Kingdom.9,17,18 Although many femoral injectors in our study had trouble finding veins, most still had peripheral venous options and there was no association with muscling, a common practice for IDUs that have lost venous access. Most of our respondents who reported femoral injection learned the practice from friends, family, or acquaintances, consistent with a report from South East England which found that current femoral injectors train others.19 Given the association of femoral injection with calendar year after controlling for duration of IDU, these findings suggest that increasing femoral injection is not simply a consequence of respondents losing venous access after years of injection.
The appropriate public health response to femoral injection is uncertain. First, providers must determine if preventing or reducing femoral injection is necessary and achievable. The medical consequences of femoral injection can be substantial and, even with optimal medical care, lower extremity venous stasis can have serious long-term consequences such as post-thrombotic syndrome.20 For those IDUs with no other venous options, reducing femoral injection may require cessation of IDU altogether, but the significant proportion of our respondents with other venous options may respond to harm reduction interventions. The only study examining cessation of femoral injection found older age, increased time in opiate agonist substitution treatment, and severity of venous stasis disease to be associated with stopping the practice.19 Prohibition of femoral injection implemented at a UK-based supervised injection facility successfully prevented the practice on-site but did nothing to deter ongoing femoral injection by participants when outside of the facility.7 Initial steps in the Seattle area might include education on the risks of femoral injection and one-on-one interventions, using harm reduction program staff trained in vein care or phlebotomy, to assist participants in locating and caring for peripheral veins. Increasing the availability of opioid agonist maintenance therapy is likely to be beneficial in the long term.
There are several limitations to this study. First, we do not know how representative our study population was of all IDUs in Seattle. Likewise, the high prevalence of femoral injection we observed and the trend toward more femoral injection seen in our study population may not be generalizable to other areas, although investigators in the UK have reported similar trends. The nature of the Northwest heroin market (i.e., low-quality and black tar heroin that is caustic to veins)2 and possibly local social networks might contribute to femoral injection practices. Second, our data were collected as part of a cross-sectional program evaluation. The findings related to participants’ length of time injecting drugs and femoral injecting are imprecise due to the rudimentary nature of the measures and could be influenced by recall bias. Moreover, our findings could also be limited by survivor bias. None of our survey respondents reported initiating femoral injection more than 6 years prior to the survey and half no longer used their femoral vein for injection, suggesting that few IDUs continue the practice for many years. Thus, if femoral injection is an event that rapidly leads to death or discontinuation of IDU, what we have interpreted as a secular trend toward increasing femoral injection could in fact represent the natural history of IDU in Seattle. Third, the survey did not routinely differentiate between heroin and other injected opioids, although black tar heroin is overwhelmingly the dominant opioid at the site where the survey was conducted. Finally, we did not conduct a physical exam or access respondents’ medical records to evaluate for or confirm reported medical sequelae of femoral injection.
Conclusion
In summary, Seattle-area IDUs may be experiencing a secular trend of increasing femoral injection, the motivation for which may be distinct from that for muscling and less dependent on limited venous access. This practice is associated with a high rate of medical complications. Additional investigations are needed to understand the reasons for initiating and maintaining femoral injection and to develop strategies to minimize resultant medical sequelae.
Acknowledgement
Dr. Coffin was supported by National Institute of Allergy and Infectious Diseases training grant (5T32AI007140-33) during the conduct of this research.
References
- 1.Kral AH, Bluthenthal RN, Erringer EA, Lorvick J, Edlin BR. Risk factors among IDUs who give injections to or receive injections from other drug users. Addiction. 1999;94(5):675–683. doi: 10.1046/j.1360-0443.1999.9456755.x. [DOI] [PubMed] [Google Scholar]
- 2.Ciccarone D. Heroin in brown, black and white: structural factors and medical consequences in the US heroin market. Int J Drug Policy. 2009;20(3):277–282. doi: 10.1016/j.drugpo.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lloyd-Smith E, Kerr T, Hogg RS, Li K, Montaner JS, Wood E. Prevalence and correlates of abscesses among a cohort of injection drug users. Harm Reduct J. 2005;2:24. doi: 10.1186/1477-7517-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maggi P, Fullone M, Federico M, Angarano G, Pastore G, Regina G. Drug injection in jugular veins: a new risk factor for vascular diseases in HIV-infected patients? A case report. Angiology. 1995;46(11):1049–1052. doi: 10.1177/000331979504601112. [DOI] [PubMed] [Google Scholar]
- 5.Roszler MH, McCarroll KA, Donovan KR, Rashid T, Kling GA. The groin hit: complications of intravenous drug abuse. Radiographics. 1989;9(3):487–508. doi: 10.1148/radiographics.9.3.2727357. [DOI] [PubMed] [Google Scholar]
- 6.Darke S, Kaye S, Ross J. Geographical injecting locations among injecting drug users in Sydney, Australia. Addiction. 2001;96(2):241–246. doi: 10.1046/j.1360-0443.2001.9622416.x. [DOI] [PubMed] [Google Scholar]
- 7.Zador D, Lintzeris N, van der Waal R, Miller P, Metrebian N, Strang J. The fine line between harm reduction and harm production—development of a clinical policy on femoral (groin) injecting. Eur Addict Res. 14(4):213–218. [DOI] [PubMed]
- 8.Maliphant J, Scott J. Use of the femoral vein (‘groin injecting’) by a sample of needle exchange clients in Bristol, UK. Harm Reduct J. 2005;2(1):6. doi: 10.1186/1477-7517-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhodes T, Briggs D, Kimber J, Jones S, Holloway G. Crack-heroin speedball injection and its implications for vein care: qualitative study. Addiction. 2007;102(11):1782–1790. doi: 10.1111/j.1360-0443.2007.01969.x. [DOI] [PubMed] [Google Scholar]
- 10.McColl MD, Tait RC, Greer IA, Walker ID. Injecting drug use is a risk factor for deep vein thrombosis in women in Glasgow. Br J Haematol. 2001;112(3):641–643. doi: 10.1046/j.1365-2141.2001.02633.x. [DOI] [PubMed] [Google Scholar]
- 11.Kozelj M, Kobilica N, Flis V. Infected femoral pseudoaneurysms from intravenous drug abuse in young adults. Wien Klin Wochenschr. 2006;118(Suppl 2):71–75. doi: 10.1007/s00508-006-0546-9. [DOI] [PubMed] [Google Scholar]
- 12.Mackenzie AR, Laing RB, Douglas JG, Greaves M, Smith CC. High prevalence of iliofemoral venous thrombosis with severe groin infection among injecting drug users in North East Scotland: successful use of low molecular weight heparin with antibiotics. Postgrad Med J. 2000;76(899):561–565. doi: 10.1136/pmj.76.899.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaku DA, So YT. Acute femoral neuropathy and iliopsoas infarction in intravenous drug abusers. Neurology. 1990;40(8):1317–1318. doi: 10.1212/wnl.40.8.1317. [DOI] [PubMed] [Google Scholar]
- 14.Mullan MJ, Magowan H, Weir CD. Femoral artery necrosis due to parenteral intravascular drug misuse: a case report and literature review. Ulster Med J. 2008;77(3):203–204. [PMC free article] [PubMed] [Google Scholar]
- 15.Manekeller S, Tolba RH, Schroeder S, Lauschke H, Remig J, Hirner A. Analysis of vascular complications in intra-venous drug addicts after puncture of femoral vessels. Zentralbl Chir. 2004;129(1):21–28. doi: 10.1055/s-2004-44871. [DOI] [PubMed] [Google Scholar]
- 16.Hoda Z, Kerr T, Li K, Montaner JS, Wood E. Prevalence and correlates of jugular injections among injection drug users. Drug Alcohol Rev. 2008;27(4):442–446. doi: 10.1080/09595230802089701. [DOI] [PubMed] [Google Scholar]
- 17.Miller PG, Lintzeris N, Forzisi L. Is groin injecting an ethical boundary for harm reduction? Int J Drug Policy. 2008;19(6):486–491. doi: 10.1016/j.drugpo.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Higgs P, Dwyer R, Duong D, et al. Heroin-gel capsule cocktails and groin injecting practices among ethnic Vietnamese in Melbourne, Australia. Int J Drug Policy. 2009;20(4):340–346. doi: 10.1016/j.drugpo.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Senbanjo R, Hunt N, Strang J. Cessation of groin injecting behaviour among patients on oral opioid substitution treatment. Addiction. 2011;196(2):376–382. doi: 10.1111/j.1360-0443.2010.03168.x. [DOI] [PubMed] [Google Scholar]
- 20.Kahn SR. The post thrombotic syndrome. Thromb Res. 2011;127(Suppl 3):S89–S92. doi: 10.1016/S0049-3848(11)70024-X. [DOI] [PubMed] [Google Scholar]