Abstract
Purpose
The purpose of this study was to develop two new 2-regression models (2RM), for use in children that estimate energy expenditure (EE) using the ActiGraph GT3X: 1) mean vector magnitude (VM) counts or 2) vertical axis (VA) counts. The new 2RMs were also compared to existing ActiGraph equations for children.
Methods
Fifty-seven boys and 52 girls (mean±sd; age, 11±1.7yrs; BMI 21.4±5.5 kg.m−2) performed 30-mins supine rest and 8-mins of six different activities ranging from sedentary behaviors to vigorous physical activity (PA). Eighteen activities were split into three routines with each routine performed by 38–39 participants. Seventy-seven participants were used for the development group and 39 participants were used for the cross-validation group. During all testing, activity data was collected using an ActiGraph GT3X, worn on the right hip, and oxygen consumption was measured using a Cosmed K4b2. All EE values are expressed as METRMR (activity VO2/resting VO2).
Results
For each activity a coefficient of variation was calculated using 10-sec epochs for the VA and VM to determine if the activity was continuous walking/running or an intermittent lifestyle activity. Separate regression equations were developed for walk/run and intermittent lifestyle activity. In the cross-validation group, the VM and VA 2RMs were within 0.8 METRMR of measured METRMR for all activities except Sport Wall and running (all, P>0.05). The other existing ActiGraph equations had mean errors ranging from 0.0 to 2.6 METRMR for the activities.
Conclusion
The new 2RMs for use in children with the ActiGraph GT3X, provide a closer estimate of mean measured METRMR than other currently available prediction equations. In addition, they improve the individual prediction errors across a wide range of activity intensities.
Keywords: Motion Sensor, Physical Activity, Oxygen Consumption, Activity Counts Variability
INTRODUCTION
The accurate measurement of physical activity (PA) in children is important, since PA plays an important role in the prevention and treatment of obesity, cardiovascular disease, and other chronic diseases. One approach for measuring PA involves the use of small, waist-mounted accelerometers with internal clocks and data-storage capabilities, which allows for an objective measurement of movement duration, intensity, and frequency. Over the past decade, these devices (e.g., ActiGraph and Actical accelerometers) have become more widely used by PA researchers, which is evident by the inclusion of the ActiGraph accelerometer in the ongoing National Health and Nutrition Examination Survey (NHANES) (26) and the Actical accelerometer being included in the Canadian Health Measures Survey (24).
Generally, researchers develop regression equations that relate the movement counts to energy expenditure (EE) and based on these regression equations, estimates of EE and time spent in sedentary behaviors (< 1.5 METs), light PA (LPA; 1.5 – 2.99 METs), moderate PA (MPA; 3 – 5.99 METs), and vigorous PA (VPA ≥ 6 METs) can be obtained. There have been several single regression equations developed for use in children (12, 15, 18, 19, 25, 29); however, in general, the single regression equations developed for use in children suffer from the same limitations as what has been shown in adults in that no single regression equation is able to accurately predict EE or time spent in different intensity categories across a wide range of activities (9, 28). Alternatively, researchers have examined other approaches for analyzing accelerometer data, including, Receiver Operating Characteristics (ROC), for use in children, (11, 13, 28), while in adults approaches such as a 2-regression model (2RM) (5, 6, 8) and pattern recognition (e.g. hidden Markov models (17) and artificial neural networks (23)) have been used. Recently, we developed a 2RM, for use in adults, for both the ActiGraph (6, 8) and Actical (5, 7) accelerometers. The 2RM is able to discriminate between continuous walking/running and intermittent lifestyle activities based on the variability in the accelerometer counts and it has been shown to be a significant improvement over the more widely used single regression equations for assessment of EE and time spent in LPA, MPA, and VPA (6, 7).
Due to differences in resting metabolic rate (RMR) (14, 22), movement economy (16), and activity patterns (1) accelerometer methods developed using adult populations cannot be applied to younger age groups. Therefore, the purpose of this study was to develop two new 2RMs for children using the ActiGraph GT3X accelerometer: 1) mean vector magnitude counts, which utilizes the newest ActiGraph tri-axial accelerometers, and 2) vertical axis counts, for researchers who still want to collect ActiGraph data using older, single axis devices. A secondary purpose was to compare the new 2RMs to four commonly used single regression equations used in children for predicting EE during structured bouts of PA.
METHODS
Participants
Fifty five girls and 61 boys between the ages of 8 and 15 yrs volunteered to participate in the study. The procedures were reviewed and approved by the University of Massachusetts Boston and Boston Public School Institutional Review Board before the start of the study. The parent of each participant signed a written informed consent and filled out a health history questionnaire and each participant signed a written assent prior to participation in the study. Participants were excluded from the study if they had any contraindications to exercise, or were physically unable to complete the activities. In addition, none of the participants were taking any medications that would affect their metabolism (e.g. Concerta or Ritalin).
Procedures
Testing was performed over a two day period. On day 1, participants had their anthropometric measures taken and completed 30 minutes of rest, lying on a table in a quiet room. On day 2, participants performed various lifestyle and sporting activities that were broken into three routines (table 1). Participants were first categorized as either normal weight or overweight/obese, based on their BMI percentile. They were then randomly assigned to an activity routine based on their BMI group so that randomization to each routine was done separately for normal weight and overweight/obese participants. This was done so that there were approximately equal numbers of normal weight and overweight/obese participants performing each routine. All participants performed the resting measurement and one of the three routines (six activities). Routine 1 was completed by 38 participants and routines 2 and 3 were completed by 39 participants. Participants performed each activity in a routine for 8 minutes, with a 1 to 2 minute break between each activity. Oxygen consumption (VO2) was measured continuously throughout the resting measure and each activity by indirect calorimetry (Cosmed K4b2, Rome Italy) and simultaneously activity data was collected using an ActiGraph GT3X accelerometer positioned on the right hip. This study was part of a larger study and in addition to the ActiGraph worn on the hip, the participants also had several other accelerometers positioned at different body locations, however only the ActiGraph hip data is presented here. To account for the additional weight of the Cosmed K4b2, ActiGraph, and additional devices, 2 kg was added to the participant’s body weight.
Table 1.
Description of activities performed by routine. Lying rest was performed for 30 minutes, and all other activities were performed for 8 minutes.
| Routine | Activity | Description |
|---|---|---|
| 0 | Lying Rest | Lying on message table in supine position with arms at side, in a quiet room. |
| 1 | Reading | Seated in a chair at a desk, reading a self selected book/magazine. |
| Sweeping | Sweep dirt on wood gymnasium floor continuously with a broom. | |
| Nintendo Wii | Played Wii Boxing for half the time and Wii Tennis for half the time with a partner. | |
| Floor Light Space | Participant chooses from a variety of games that require users to follow and activate different points on a pressure sensor pad on the floor that reacts to movement. | |
| Slow Walking | Walk at a self-selected comfortable speed around an outdoor track (weather permitting) or a marked hallway perimeter inside. | |
| Brisk Walking | Walk at a self-selected comfortable speed around an outdoor track (weather permitting) or a marked hallway perimeter inside. | |
| 2 | Watching TV | Seated in a chair at a desk and watching self selected TV show on a computer. |
| Wall Light Space | Participant chooses from a variety of games that require users to follow and activate different points on a pressure sensor pad on the wall that reacts to movement. | |
| Dance Dance Revolution | Follow movement patterns on a screen that are set to music, by stepping on appropriate arrows on a pad. Songs are selected at random and were set to easy level. | |
| Playing Catch | Standing at a comfortable distance from partner, throw and catch a football. | |
| Walking with Backpack | Wearing a 4.5 kg weighted vest, walk at a self-selected comfortable speed around an outdoor track (weather permitting) or a marked hallway perimeter inside. | |
| Soccer around cones | Dribble soccer ball back and forth around 3–4 cones set up in a zig zag pattern. Play outside on grass (weather permitting) or inside in a designated space. | |
| 3 | Searching Internet | While sitting in a chair at a desk use mouse and keyboard to search self selected items on the internet. |
| Vacuuming | While standing and continuously moving around, vacuum carpet. | |
| Sport Wall | Standing 20–25 ft away from wall, run to wall and hit illuminated dot on wall, then run back to starting point and repeat. Try to get as many points as you can within timeframe. | |
| Trazer | Motion sensor belt is clipped around waist which when moved controls the screen avatars movement. Played Goalie Wars for half the time jump explosion for half the time. | |
| Workout Video | Follow along to an age specific aerobics video. | |
| Track Running | Run at a self-selected comfortable speed around an outdoor track (weather permitting) or a marked hallway perimeter inside. | |
Anthropometric measurements
Prior to testing, participants had their height and weight measured (in light clothing, without shoes) using a stadiometer and a physician’s scale, respectively. Body mass index (BMI) was calculated according to the formula: body mass (kg) divided by height squared (m2) and gender and age specific BMI percentiles were calculated using CDC algorithms (4).
Indirect calorimetry
The participants wore a Cosmed K4b2 for the duration of each routine and the resting measure. Prior to each test the oxygen and carbon dioxide analyzers were calibrated according to the manufacturer’s instructions. This consisted of performing a room air calibration and a reference gas calibration using 15.93% oxygen and 4.92% carbon dioxide. The flow turbine was then calibrated using a 3.00 L syringe (Hans-Rudolph). Finally, a delay calibration was performed to adjust for the lag time that occurs between the expiratory flow measurement and the gas analyzers.
ActiGraph accelerometer
The ActiGraph GT3X accelerometer is a small (3.8 × 3.7 × 1.8cm), lightweight (27 grams), water resistant tri-axial accelerometer. The GT3X measures accelerations in the range of 0.05 to 2 G’s, which is digitized by a 12-bit analog-to-digital converter at a rate of 30 Hz. Once digitized, the data is filtered using a band limited frequency of 0.25 to 2.5 Hz. These values correspond to the range in which most human activities are performed. During all testing the ActiGraph GT3X was worn at waist level at the right anterior axillary line attached to a nylon belt. The GT3X was initialized using 1-second epochs and the low frequency extension turned on. The GT3X time was synchronized with a digital clock so the start time could be synchronized with the Cosmed K4b2. At the conclusion of the test the GT3X data were downloaded for subsequent analysis.
Data analysis
Breath-by-breath data were collected by the Cosmed K4b2, which was averaged over a one minute period. For each activity, the VO2 (ml.min−1) was converted to VO2 (ml.kg−1.min−1). In adults, 3.5 ml.kg−1.min−1 is used to define 1 MET, however children and adolescents have higher resting metabolic rates than adults and if the standard definition of 3.5 ml.kg−1.min−1 is used in children it will result in an overestimation of the measured energy cost (i.e. MET value) of an activity (14, 22). Thus, METs were calculated by dividing the VO2 (ml.kg−1.min−1) for each activity by the participant's supine resting VO2 (ml.kg−1.min−1). Hereafter, the use of METRMR will refer to measured activity VO2 divided by measured supine resting VO2 and MET3.5 will refer to the standard definition used for adults of 1 MET=3.5 ml.kg−1.min−1. For each activity, the METRMR values for minutes 4 to 7 were averaged and used for the subsequent analysis.
The ActiGraph accelerometer data for each axis were collected in 1-second epochs. Mean vector magnitude was also calculated as the square root of the sum squared activity counts in each vector. The 1-sec epochs for each axis and vector magnitude were converted to counts per 10 seconds and counts.min−1. For each activity mean counts per 10-s, counts per minute and coefficient of variation (CV) were calculated. Following the methods we previously used in developing the refined 2RM for adults (8), aCV was calculated for each 10-s epoch by examining each 10-s epoch and the surrounding five 10-s epochs in the following manner: the 10-s epoch of interest and 1) the five 10-s epochs before, 2) the four 10-s epochs before and one 10-s epoch after, 3) the three 10-s epochs before and two 10-s epochs after, 4) the two 10-s epochs before and three 10-s epochs after, 5) the one 10-s epoch before and four 10-s epochs after, and 6) the five 10-s epochs that followed. After the CV was calculated for each condition, the lowest CV from the six possible conditions was used as the CV for that 10-s epoch. Examining each 10-s epoch and all combinations of the five surrounding 10-s epochs, in this manner, allows for the determination of whether a specific 10-s epoch falls within a continuous walking/running bout or is part of an intermittent lifestyle activity. The mean counts and CV were calculated for minutes 4–7 of each activity, to match what was done with the Cosmed data (for further detail and sample calculations see Crouter et al. (8)).
Lastly, EE was also predicted using the child-specific regression equations of Freedson et al. (12), Trost et al. (29), Treuth et al. (25), and Puyau et al. (18).(see Table, Supplemental Digital Content 1, which describes each equation.) Since we chose to express our measured EE value as METRMR, we felt it was necessary to convert all prediction equations to a comparable METRMR values to ensure a fair evaluation of the prediction equations. For the Freedson and Treuth equations, which both predict MET3.5, we multiplied the predicted MET3.5 value, for each activity, by 3.5 ml.kg−1.min−1 to obtain a predicted VO2 value, which was then divided by the supine resting VO2 to get a predicted METRMR. The Trost and Puyauequations predict kcal.min−1 and kcal.kg−1.min−1, respectively, thus they were also converted to METRMR values using the measured resting values.
Statistical treatment
Statistical analyses were carried out using SPSS version 17.0 for windows (SPSS Inc., Chicago, IL). For all analyses, an alpha level of 0.05 was used to indicate statistical significance. All values are reported as mean (standard deviation). Seventy-seven participants were randomly selected for the development of the new 2RM, leaving 39 participants for cross-validation of the new equation.
Initially, using the developmental group, the mean counts and percentile distribution were used to determine an inactivity threshold (i.e., lying, reading, video watching, and searching internet activities) and the mean CV and percentile distribution were used to determine a CV threshold to determine whether a 10-s epoch is part of a continuous walking/running bout or intermittent lifestyle activity. Regression analysis was then used to predict METRMR from the counts per 10-s based on a low CV (continuous walk/run activity) or a high CV (intermittent lifestyle activity). This process was completed using both the mean vector magnitude counts and vertical axis counts.
A one-way repeated measures ANOVA was used to compare measured (Cosmed) and predicted METRMR for each activity using the cross validation group. Pairwise comparisons with Bonferroni adjustments were performed to locate significant differences when necessary.
Modified Bland-Altman Plots were used to graphically show the variability in individual error scores (actual METRMR minus estimated METRMR) (2). This allowed for the mean error score and the 95% prediction interval to be shown. Data points below zero signify an overestimation, while points above zero signify an underestimation. The Bland–Altman plots were modified by plotting the criterion measure on the x-axis; this is different from the original method in which the x-axis is the average of two methods that attempted to measure the same construct (2).
RESULTS
Data for four participants from the developmental group and three participants from the cross-validation group were excluded due to missing a resting measurement (3 participants) or accelerometer malfunction resulting in data loss (4 participants).
Participant descriptive characteristics for the development group and cross-validation group are shown in table 2. Mean (SD) measured METRMR values and ActiGraph counts per minute and CV of the counts per 10 seconds (x-axis and vector magnitude), for each activity are shown in table 3 (developmental group only).
Table 2.
Descriptive characteristics of the participants in the development and cross-validation groups.
| Development Group (n=73) | Cross-Validation Group (n=33) | |
|---|---|---|
| Age (yrs) ± SD (range) | 11.3 ± 1.6 (8–15) | 12.1 ± 1.4 (8–14) |
| 8–9 yr olds (n) | 21 | 4 |
| 10–11 yr olds (n) | 24 | 15 |
| 12 yrs and older (n) | 28 | 14 |
| Male | 50.7% | 55.6% |
| Activity Routine | ||
| 1 (n) | 27 (10 male, 17 female) | 11 (7 male, 4 female) |
| 2 (n) | 23 (12 male, 11 female) | 13 (8 male, 5 female) |
| 3 (n) | 23 (15 male, 8 female) | 12 (5 male, 7 female) |
| BMI Classification | ||
| Normal Weight (5th–85th percentile) | 58.4% | 66.7% |
| Overweight (85th–95th percentile) | 15.6% | 12.8% |
| Obese (≥ 95th percentile) | 26.0% | 20.5% |
| Race/Ethnicity | ||
| Hispanic | 29.9% | 35.9% |
| Black/African American | 39.0% | 59.0% |
| Native American/Alaskan | 2.6% | 0.0% |
| Asian | 11.7% | 10.3% |
| White | 46.8% | 30.7% |
Table 3.
Mean (± SD) measured (Cosmed) METRMR (Measured VO2 for the activity divided by measured resting VO2) and counts.min−1 (vertical axis and vector magnitude) and coefficient of variation (CV) for the 10 second counts (vertical axis and vector magnitude) from the ActiGraph accelerometer for each activity using the developmental group.
| Activity | Measured VO2 (ml.kg−1.min−1) |
Measured METRMR |
ActiGraph Vertical Axis | ActiGraph Vector Magnitude |
||
|---|---|---|---|---|---|---|
| Counts.min−1 | CV | Counts.min−1 | CV | |||
| Supine Rest (n=73) | 4.8 (1.5) | 1.0 (0.0) | 34 (55.9) | 70 (68.5) | 84 (141.2) | 89 (72.2) |
| Watching Television (n=23) | 5.0 (1.4) | 1.1 (0.3) | 6 (11.9) | 44 (68.3) | 59 (94.0) | 105 (83.0) |
| Searching Internet (n=23) | 4.9 (1.4) | 1.1 (0.3) | 9 (28.9) | 33 (52.7) | 41 (55.9) | 107 (75.2) |
| Reading (n=27) | 4.9 (1.7) | 1.1 (0.4) | 11 (31.4) | 56 (66.4) | 61 (99.7) | 109 (63.6) |
| Workout Video (n=23) | 9.7 (3.3) | 2.1 (0.7) | 669 (483.6) | 117 (34.5) | 1637 (773.2) | 64 (23.8) |
| Nintendo Wii (n=27) | 11.4 (6.4) | 2.4 (1.1) | 372 (404.8) | 120 (37.9) | 1548 (1034.9) | 73 (24.2) |
| Vacuuming (n=23) | 11.2 (3.3) | 2.5 (0.7) | 343 (205.0) | 79 (35.8) | 2272 (677.2) | 28 (10.4) |
| Sweeping (n=27) | 12.1 (3.8) | 2.7 (1.1) | 454 (398.1) | 78 (36.8) | 2152 (1072.8) | 33 (18.4) |
| Slow Track Walking (n=27; avg. 75 m.min−1) | 14.9 (3.7) | 3.3 (1.2) | 3063 (805.0) | 13 (7.2) | 4172 (763.3) | 10 (5.5) |
| Dance Dance Revolution (n=23) | 15.7 (4.4) | 3.4 (1.0) | 1036 (568.1) | 106 (26.2) | 2107 (818.5) | 71 (18.2) |
| Playing Catch (n=23) | 17.4 (5.2) | 3.7 (1.1) | 1507 (720.5) | 79 (36.0) | 3630 (1151.6) | 46 (20.9) |
| Walk with 4.5 kg backpack (n=23; avg. 81 m.min−1) | 17.5 (4.4) | 3.8 (1.3) | 3300 (1037.4) | 16 (15.7) | 4206 (937.1) | 11 (6.4) |
| Brisk Track Walking (n=27; avg. 93 m.min−1) | 19.3 (4.3) | 4.3 (1.5) | 4061 (897.8) | 14 (7.7) | 5401 (845.7) | 12 (6.3) |
| Trazer (n=23) | 18.8 (7.1) | 4.3 (1.9) | 4193 (2358.1) | 64 (24.6) | 6627 (2071.5) | 44 (18.0) |
| Floor Light Space (n=27) | 21.5 (7.5) | 4.6 (1.7) | 2242 (1230.8) | 69 (20.2) | 4869 (1597.3) | 51 (15.6) |
| Wall Light Space (n=23) | 21.5 (6.2) | 4.8 (1.8) | 1935 (753.1) | 83 (23.9) | 4544 (1256.0) | 55 (12.0) |
| Sport Wall (n=23) | 21.7 (6.9) | 4.9 (1.9) | 3126 (1650.0) | 68 (31.7) | 5260 (1895.8) | 46 (23.5) |
| Track Running (n=23; avg. 122 m.min−1) | 21.9 (10.4) | 5.0 (2.6) | 5163 (1574.8) | 17 (11.8) | 6304 (1481.4) | 14 (8.2) |
| Soccer Around Cones (n=23) | 22.7 (8.9) | 5.1 (2.5) | 2118 (1046.8) | 41 (22.5) | 4467 (1257.9) | 23 (8.1) |
ActiGraph vertical axis model
Based on the examination of the mean CV values, for the vertical axis, and percentile distributions a CV of 35 was chosen to distinguish between continuous walking/running and intermittent lifestyle activity. Specifically, during walking and running activities the CV was less than 35% (CV ≤ 35) 96.1% of the time, whereas for intermittent lifestyle activities the CV threshold was greater than 35% (CV > 35) 94.4% of the time. One exception was for sedentary activities where count values could be zero for a full minute; thus the CV was not able to be calculated. For these activities, the CV was defined as zero and were included in the CV > 35 group for the purpose of developing the model.
For activities where the vertical axis CV was ≤ 35 an exponential equation using the vertical axis counts per 10 sec provided the best fit, while for activities where the vertical axis CV was > 35 a linear regression equation using the vertical axis counts provided the best fit. In addition, we propose an inactivity threshold of 25 vertical axis counts per 10 sec to distinguish inactivity from light activity. Thus, when the vertical axis counts per 10 sec are ≤ 25 the individual is credited with 1.0 METRMR. The 2RM to predict gross EE (METRMR) from the ActiGraph vertical axis counts consists of three parts (inactivity threshold and two separate regression models) and hereafter will be referred to as the child VA2RM:
if the vertical axis counts per 10 sec are ≤ 25, energy expenditure = 1.0 METRMR,
- if the vertical axis counts per 10 sec are > 25
- and the CV of the vertical axis counts per 10 sec ≤ 35, then energy expenditure (METRMR) = 1.982 * (exp(0.00101 * ActiGraph vertical axis counts per 10 s)) (R2 = 0.304; SEE = 0.347),
- or the CV of the vertical axis counts per 10 sec are > 35, then energy expenditure (METRMR) = 2.842 + (0.00288 * ActiGraph vertical axis counts per 10 s)(R2 = 0.222; SEE = 1.450)
Once a METRMR value has been calculated for each 10-s epoch within a minute on the ActiGraph clock, the average METRMR value of six consecutive 10-s epochs within each minute is calculated to obtain the average METRMR value for that minute.
ActiGraph vector magnitude model
Based on the examination of the mean CV values, for the mean vector magnitude, and percentile distributions a CV of 25 was chosen to distinguish between continuous walking/running and intermittent lifestyle activity. Specifically, during walking and running activities the CV was less than 25% (CV ≤ 25) 97% of the time, whereas for intermittent lifestyle activities the CV threshold was greater than 25% (CV > 25) 89.5% of the time. As described above for the model using only the vertical axis, when the CV was defined as zero they were included in the CV > 25 group for the purpose of developing the model.
For activities where the mean vector magnitude CV was ≤ 25 an exponential equation using the natural log (ln) of the mean vector magnitude counts per 10 sec provided the best fit, while for activities where the mean vector magnitude CV was > 25 a cubic equation using the ln of the mean vector magnitude counts per 10 seconds provided the best fit. In addition, we propose an inactivity threshold of 75 mean vector magnitude counts per 10 sec to distinguish inactivity from light activity. The 2RM to predict gross EE (METRMR) from the ActiGraph vector magnitude counts hereafter will be referred to as the child VM2RM:
if the vector magnitude counts per 10 sec are ≤ 75, energy expenditure = 1.0 METRMR,
- if the vector magnitude counts per 10 sec are > 75
- and the CV of the vector magnitude counts per 10 sec ≤ 25, then energy expenditure (METRMR) = 0.0137 * (exp(0.848 * (ln(ActiGraph vector magnitude counts per 10 s))) (R2 = 0.388; SEE = 0.358),
- or the CV of the vector magnitude counts per 10 sec are > 25, then energy expenditure (METRMR) = 1.219 − (0.145 * (ln(ActiGraph vector magnitude counts per 10 s) − (0.0586 * (ln(ActiGraph vector magnitude counts per 10 s))2) + (0.0229 * (ln(ActiGraph vector magnitude counts per 10 s))3) (R2 = 0.589; SEE = 1.248)
Once a METRMR value has been calculated for each 10-s epoch within a minute on the ActiGraph clock, the average METRMR value of six consecutive 10-s epochs within each minute is calculated to obtain the average METRMR value for that minute.
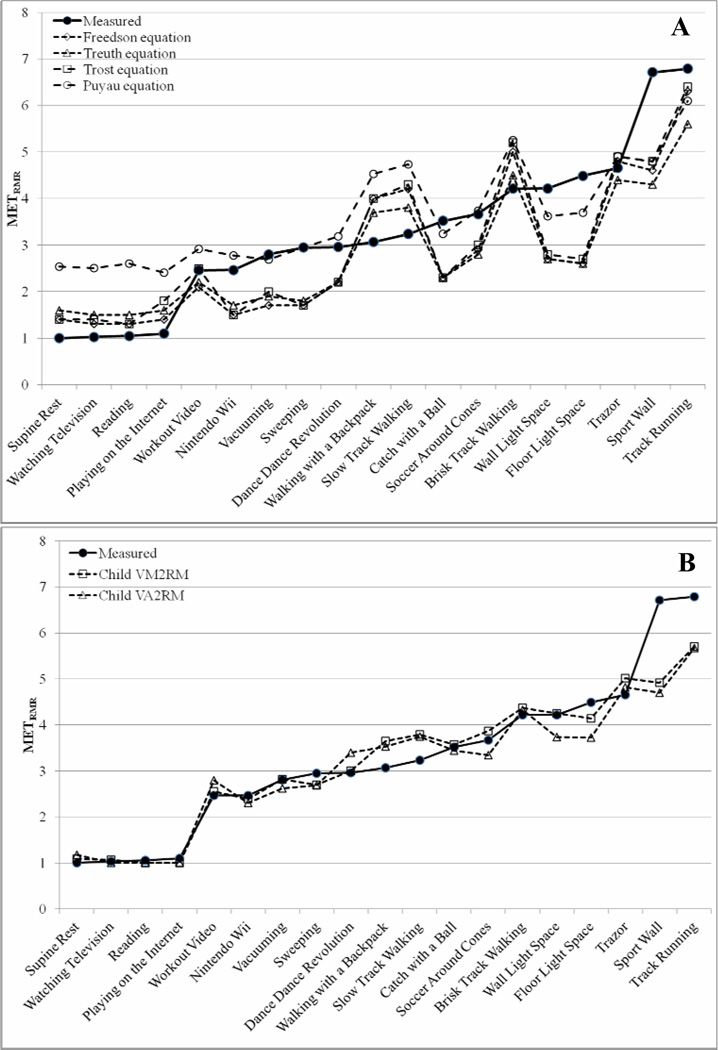
Figure 1a shows the measured and predicted METRMR values for each of the activities using the current ActiGraph single regression equations in the cross-validation group. Figure 1b shows the measured and predicted METRMR values for the cross-validation group using the child VA2RM and VM2RM. The child VM2RM was within 0.6 METRMR compared to measured METRMR for each of the 19 activities, except for Sport Wall (1.8 METRMR difference) and track running (1.1 METRMR difference) and was not significantly different from actual METRMR for any activity (all, P>0.05). The VA2RM was within 0.8 METRMR compared to measured METRMR for each of the 19 activities, except for Sport Wall (2.0 METRMR difference) and track running (1.1 METRMR difference), and was not significantly different from actual METRMR for any activity (P>0.05). The single regression equations generally overestimated activities below 2 METRMR, slow and brisk walking and walking with a 4.5 kg backpack and underestimated most other activities. The Freedson, Treuth, and Puyau equations all significantly overestimated the mean METRMR value, for all activities combined, compare to measured METRMR, (P < 0.001), while the child VA2RM and VM2RM were both within 0.2 METRMR of actual METRMR and the Trost equation was within 0.3 METRMR of actual METRMR for all activities combined (P>0.05). (see Table, Supplemental Digital Content 2, which shows the measured METRMR and estimated METRMR for the cross-validation for each activity.)
Figure 1.
Measured (Cosmed K4b2) and predicted METRMR across 19 different activities for the cross-validation group, using (A) the Treuth, Freedson, Trost, and Puyau regression equations for children and (B) the child vector magnitude 2-regression model (VM2RM) and child vertical axis 2-regression model (VA2RM).
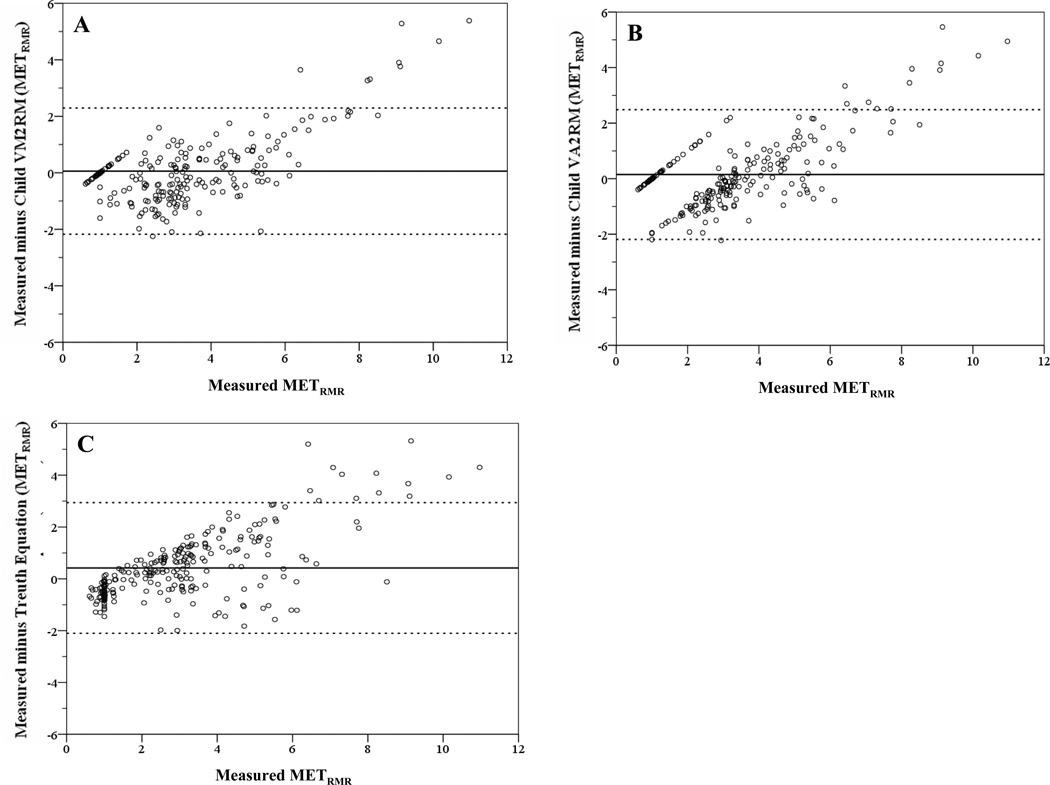
The Bland-Altman plots (figure 2a–c) show that, compared to the other models, the child VM2RM was the most accurate model with a mean bias of 0.06 METRMR (95% PI = −2.18 to 2.30), however it had a trend to have greater underestimation of measured values greater than 7 METRMR. The child VA2RM had a mean bias of 0.15 METRMR (95% PI = −2.19 to 2.49), however it had a significant trend to overestimate measured values below 4 METRMR and underestimate measured values greater than 6 METRMR. All the single regression equations performed similarly, with the Treuth equation (mean bias 0.42 METRMR; 95% PI = −2.10 to 2.94) performing the best among the single regression equations. In addition, all single regression equations showed similar trends as the child VA2RM, to overestimate light to moderate activities and underestimate moderate to vigorous activities. (see Figure, Supplemental Digital Content 3, which shows the Bland-Altman plots for the Freedson, Trost, and Puyau equations)
Figure 2.
Bland-Altman plots depicting error scores (measured minus estimation) for (A) the child vector magnitude 2-regression model (VM2RM), (B) the child vertical axis 2-regression model (VA2RM), and (C) Treuth single regression equation. The solid line represents the mean, and dashed lines represent the 95% confidence interval of the observations.
DISCUSSION
This study describes a new approach to estimating EE in children, using the ActiGraph accelerometer. In addition, this is the first study to present a 2RM, for use in children that utilizes either the vertical axis or the vector magnitude from the ActiGraph GT3X accelerometer. The main advantage of this method is that it uses the CV to distinguish between continuous walking/running and intermittent lifestyle activities and then it applies one of two regression equations to obtain improved estimates of EE during specific activities.
Previously, research has shown in adults that the use of a 2RM is a significant improvement over using single regression equations (5–8) and compares more favorably to doubly labeled water (20). We acknowledge that there are more sophisticated accelerometer analytical techniques that use pattern recognition (e.g., artificial neural networks); however, these models are not readily available for use in children. The new child VM2RM and VA2RM provide a simpler alternative to the more sophisticated pattern recognition methods that provides a more accurate prediction of EE, and can be implemented into any study that currently has either the vertical axis or vector magnitude ActiGraph data available in 10-sec epochs.
In previous research on children, it has been controversial as to whether age should be included in accelerometer prediction equation; while some studies have found that age should be included in the regression equations (12, 15), others have not (18, 25, 29). In a recent validation study, Trost and colleagues examined the validity of several currently available regression equations across a wide range of activities in participants between 5 and 15 yrs of age (28). They observed that regression equations that include age have similar accuracy for estimating time spent in various activity intensity categories, compared to equations that only include counts in the regression equations. This suggests that age is not the primary factor affecting accuracy of the prediction equations in children (28). While the current study did not investigate time in each intensity category, the results from the cross-validation group provide further evidence that all the single regression equations work in a similar fashion for estimating the energy cost of specific activities, regardless of whether age is included in the prediction model.
The current study investigated multiple regression models that included factors such as age and gender and the best models overall included only counts. Rather than chronological age, it appears that growth dependent factors (e.g. change in RMR) seem to play a greater role in the relationship between accelerometer output and EE (27). Several earlier studies involving child participants have used adult values for the estimated RMR (i.e. 1 MET3.5 = 3.5 ml.kg−1.min−1) (12, 25). When adult RMR values are used in children, this will overestimate the intensity of the activity, due to their higher RMR. For the cross validation in the current study, we chose to convert the predicted MET3.5 values for the Freedson and Treuth equations to predicted METRMR values. To illustrate the difference in the predicted values, table 4 shows the predicted MET3.5 and METRMR values for the Freedson and Treuth equations compared to the measured METRMR values. PA researchers need to be aware of how prediction equations are developed as it has implications for implementation into studies and the predictive accuracy of the equations.
Table 4.
METRMR (mean (± SD)) values of the cross-validation group for the Cosmed K4b2 (measured METs) and predicted METRMR and MET3.5 for the Freedson and Treuth prediction equations during various structured activities.
| Activity | Measured METRMR |
Freedson Equation | Treuth Equation | ||
|---|---|---|---|---|---|
| MET3.5 | METRMR | MET3.5 | METRMR | ||
| Supine Rest (n=33) | 1.0 (0.0) | 1.8 (0.2)* | 1.4 (0.3)* | 2.1 (0.1)* | 1.6 (0.4)* |
| Watching Television (n=13) | 1.0 (0.4) | 1.8 (0.1)* | 1.3 (0.3) | 2.0 (0.0)* | 1.5 (0.4)* |
| Searching Internet (n=12) | 1.1 (0.2) | 1.7 (0.1)* | 1.4 (0.2) | 2.0 (0.0)* | 1.6 (0.3)* |
| Reading (n=11) | 1.0 (0.2) | 1.8 (0.2)* | 1.3 (0.4) | 2.0 (0.0)* | 1.5 (0.4) |
| Workout Video (n=12) | 2.5 (0.6) | 2.6 (0.9) | 2.1 (0.8) | 2.8 (0.6) | 2.2 (0.6) |
| Nintendo Wii (n=11) | 2.5 (1.3) | 2.1 (0.3) | 1.5 (0.6) | 2.3 (0.3) | 1.7 (0.7) |
| Vacuuming (n=12) | 2.8 (0.5) | 2.2 (0.4) | 1.7 (0.4)* | 2.4 (0.3) | 1.9 (0.4)* |
| Sweeping (n=11) | 3.0 (1.4) | 2.4 (0.4) | 1.7 (0.5) | 2.5 (0.3) | 1.8 (0.6) |
| Slow Track Walking (n=11; avg. 75 m.min−1) | 3.2 (1.0) | 5.6 (1.3)* | 4.2 (1.9) | 5.1 (0.9)* | 3.8 (1.6) |
| Dance Dance Revolution (n=13) | 3.0 (0.9) | 2.9 (0.7) | 2.2 (0.7) | 3.0 (0.6) | 2.2 (0.7) |
| Playing Catch (n=13) | 3.5 (1.2) | 3.1 (0.7) | 2.3 (0.6)* | 3.1 (0.5) | 2.3 (0.6)* |
| Walk with 4.5 kg backpack (n=13; avg. 76 m.min−1) | 3.1 (0.4) | 5.4 (0.8)* | 4.0 (0.8) | 4.9 (0.6)* | 3.7 (0.8) |
| Brisk Track Walking (n=11; avg. 92 m.min−1) | 4.2 (1.1) | 6.6 (1.4)* | 5.0 (2.0) | 5.9 (1.0)* | 4.5 (1.8) |
| Trazer (n=12) | 4.7 (1.6) | 6.0 (2.2) | 4.8 (2.0) | 5.5 (1.8) | 4.4 (1.7) |
| Floor Light Space (n=11) | 4.5 (1.9) | 3.7 (0.8) | 2.6 (0.8) | 3.6 (0.6) | 2.6 (0.8)* |
| Wall Light Space (n=13) | 4.2 (1.2) | 3.7 (0.8) | 2.7 (0.5)* | 3.6 (0.5) | 2.7 (0.4)* |
| Sport Wall (n=12) | 6.7 (2.3) | 5.8 (1.8) | 4.6 (1.6)* | 5.4 (1.5) | 4.3 (1.5)* |
| Track Running (n=12; avg. 120 m.min−1) | 6.8 (2.0) | 8.1 (0.9) | 6.3 (1.5) | 7.2 (0.8) | 5.6 (1.5) |
| Soccer Around Cones (n=13) | 3.7 (0.9) | 3.9 (1.1) | 2.9 (0.8) | 3.8 (0.9) | 2.8 (0.7) |
| Total for all activities | 3.1 (2.0) | 3.6 (2.1)* | 2.7 (1.8)* | 3.5 (1.7)* | 2.7 (1.5)* |
METRMR, metabolic equivalents (measured VO2 divided by measured lying RMR VO2); MET3.5, metabolic equivalents (measured VO2 divided by 3.5 ml.kg−1.min−1).
Significantly different from Cosmed K4b2, P < 0.05
Previous research in children and adults has suggested that the use of triaxial accelerometers have potential to provide better estimates of PA than using a single axis accelerometer (3, 10, 21, 30). This could be potentially true for children given their inherent movement patterns during free play activities (e.g., short sporadic burst and varied movements in multiple planes) (1); however there is no conclusive evidence to suggest that using a single axis versus multiple axes is superior to the other. In the current study, a child 2RM was developed using a single axis (vertical axis) and all three axes (vector magnitude). Based on the results from the cross-validation group in the current study, both models worked in a similar fashion and had similar mean errors for the prediction of specific activities. In addition, the Bland-Altman plots show similar accuracy between the child VM2RM (mean bias, 95% PI: 0.06, −2.18–2.3 METRMR) and the child VA2RM (mean bias, 95% PI: 0.15, −2.19–2.49 METRMR). However, the child VA2RM tended to overestimate activities less than 4 METRMR and underestimate activities over 4 METRMR. Further work is needed to examine how the different models work in a true free-living environment.
The current study does have strengths and weaknesses. Strengths of the study are that the new child 2RMs were developed on a wide range of activities ranging from sedentary behaviors to vigorous exercise. In addition, we used a large sample size with a range of ages and BMI levels. This is in contrast to most previous studies that developed single regression equations on a limited number of activities (i.e. walking/running or moderate-intensity lifestyle activities), a single sex, or limited age range. In addition, while the activities were performed in a structured manner (i.e. 8-min bouts of specific activities), the participants were encouraged to perform the activity as they generally would under normal circumstances. Additionally, when possible, activities were performed outside of the laboratory in more of a free living environment. For example, the walking and running were performed over-ground at self-selected speeds. Limitations of the study include a small cross-validation group (11–13 participants per activity). In addition, the new child 2RMs were validated using the same activities that they were developed on which could influence the results to show that they work better than they might in an independent sample on different activities. Future research should be designed to validate this method in a wide range of individuals for 24-hour EE (i.e. with doubly labeled water) and with indirect calorimetry using other types of physical activities. An additional limitation to the study is that we relied on the participants to tell us when their last meal was and when they last performed previous VPA; thus it is possible that the measured resting values are higher than expected for some due to not following the protocol as asked. This has potential to affect the activity METRMR values since an elevated resting METRMR value would result in a lower activity METRMR value.
In conclusion, the new child VM2RM and VA2RM improve upon currently available methods for the prediction of EE (METRMR) in children during structured bouts of PA. The new child VM2RM was the most accurate on both a group and individual basis. It has a bias of 0.06 METRMR (95% PI of −2.18, 2.30METRMR). Further work is needed to examine the accuracy of these new models in an independent sample of children, in a free-living setting.
Supplementary Material
ACKNOWLEDGEMENTS
This research was supported by an NIH grant no. NIH 5R21HL093407. No financial support was received from any of the activity monitor manufacturers, importers, or retailers. The results of the present study do not constitute endorsement by ACSM.
The authors would like to thank the research participants and Prince Owusu, Larry Kennard, Katie Dooley, Shawn Pedicini, Rachel Mclellan, and Sarah Sullivan for help with data collection.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: There are no declared conflicts of interest for any of the authors.
REFERENCES
- 1.Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM. The level and tempo of children's physical activities: an observational study. Med Sci Sports Exerc. 1995;27(7):1033–1041. doi: 10.1249/00005768-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet North Am Ed. 1986;1:307–310. [PubMed] [Google Scholar]
- 3.Bouten CV, Westerterp KR, Verduin M, Janssen JD. Assessment of energy expenditure for physical activity using a triaxial accelerometer. Med Sci Sports Exerc. 1994;26(12):1516–1523. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) [Internet] About BMI for Children and Teens. 2011 Feb 1; Available from: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
- 5.Crouter SE, Bassett DR., Jr A new 2-regression model for the Actical accelerometer. Br J Sports Med. 2008;42(3):217–224. doi: 10.1136/bjsm.2006.033399. [DOI] [PubMed] [Google Scholar]
- 6.Crouter SE, Clowers KG, Bassett DR., Jr A novel method for using accelerometer data to predict energy expenditure. J Appl Physiol. 2006;100(4):1324–1331. doi: 10.1152/japplphysiol.00818.2005. [DOI] [PubMed] [Google Scholar]
- 7.Crouter SE, Dellavalle DM, Horton M, Haas JD, Frongillo EA, Bassett DR., Jr Validity of the Actical for estimating free-living physical activity. Eur J Appl Physiol. 2010 doi: 10.1007/s00421-010-1758-2. Online First, 13 December 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crouter SE, Kuffel E, Haas JD, Frongillo EA, Bassett DR., Jr A refined 2-regression model for the ActiGraph accelerometer. Med Sci Sports Exerc. 2010;42(5):1029–1037. doi: 10.1249/MSS.0b013e3181c37458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Graauw SM, de Groot JF, van Brussel M, Streur MF, Takken T. Review of prediction models to estimate activity-related energy expenditure in children and adolescents. [[cited 2011 November 29]];Int J Pediatr [Internet] 2010 doi: 10.1155/2010/489304. 2010(2010). Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2910404/?tool=pubmed. [DOI] [PMC free article] [PubMed]
- 10.Eston RG, Rowlands AV, Ingledew DK. Validity of heart rate, pedometry, and accelerometry for predicting the energy cost of children's activities. J Appl Physiol. 1998;84(1):362–371. doi: 10.1152/jappl.1998.84.1.362. [DOI] [PubMed] [Google Scholar]
- 11.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 12.Freedson P, Pober D, Janz KF. Calibration of accelerometer output for children. Med Sci Sports Exerc. 2005;37(11 Suppl):S523–S530. doi: 10.1249/01.mss.0000185658.28284.ba. [DOI] [PubMed] [Google Scholar]
- 13.Jago R, Zakeri I, Baranowski T, Watson K. Decision boundaries and receiver operating characteristic curves: new methods for determining accelerometer cutpoints. J Sports Sci. 2007;25(8):937–944. doi: 10.1080/02640410600908027. [DOI] [PubMed] [Google Scholar]
- 14.Malina RM, Bouchard C, Bar-Or O. Growth, Maturation, and Physical Activity. 2nd ed. Champaign, Ill: Human Kinetics; 2004. p. 728. [Google Scholar]
- 15.Mattocks C, Leary S, Ness A, Deere K, Saunders J, Tilling K, Kirkby J, Blair SN, Riddoch C. Calibration of an accelerometer during free-living activities in children. Int J Pediatr Obes. 2007;2(4):218–226. doi: 10.1080/17477160701408809. [DOI] [PubMed] [Google Scholar]
- 16.Morgan DW, Martin PE, Krahenbuhl GS. Factors affecting running economy. Sports Med. 1989;7(5):310–330. doi: 10.2165/00007256-198907050-00003. [DOI] [PubMed] [Google Scholar]
- 17.Pober DM, Staudenmayer J, Raphael C, Freedson PS. Development of novel techniques to classify physical activity mode using accelerometers. Med Sci Sports Exerc. 2006;38(9):1626–1634. doi: 10.1249/01.mss.0000227542.43669.45. [DOI] [PubMed] [Google Scholar]
- 18.Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res. 2002;10(3):150–157. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 19.Puyau MR, Adolph AL, Vohra FA, Zakeri I, Butte NF. Prediction of activity energy expenditure using accelerometers in children. Med Sci Sports Exerc. 2004;36(9):1625–1631. [PubMed] [Google Scholar]
- 20.Rothney MP, Brychta RJ, Meade NN, Chen KY, Buchowski MS. Validation of the ActiGraph Two-Regression Model for Predicting Energy Expenditure. Med Sci Sports Exerc. 2010;42(9):1785–1792. doi: 10.1249/MSS.0b013e3181d5a984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rowlands AV, Thomas PW, Eston RG, Topping R. Validation of the RT3 triaxial accelerometer for the assessment of physical activity. Med Sci Sports Exerc. 2004;36(3):518–524. doi: 10.1249/01.mss.0000117158.14542.e7. [DOI] [PubMed] [Google Scholar]
- 22.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39(Suppl 1):5–41. [PubMed] [Google Scholar]
- 23.Staudenmayer J, Pober D, Crouter S, Bassett D, Freedson P. An artificial neural network to estimate physical activity energy expenditure and identify physical activity type from an accelerometer. J Appl Physiol. 2009;107(4):1300–1307. doi: 10.1152/japplphysiol.00465.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tremblay MS, Wolfson M, Gorber SC. Canadian Health Measures Survey: rationale, background, and overview. Health Rep. 2007;18(Suppl):7–20. [PubMed] [Google Scholar]
- 25.Treuth MS, Schmitz K, Catellier DJ, McMurray RG, Murray DM, Almeida MJ, Going S, Norman JE, Pate R. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004;36(7):1259–1266. [PMC free article] [PubMed] [Google Scholar]
- 26.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 27.Trost S. State of the art reviews: Measurement of physical activity in children and adolescents. Am J Lifestyle Med. 2008;1(4):299–314. [Google Scholar]
- 28.Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–1368. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- 29.Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR. Validity of the computer science and applications (CSA) activity monitor in children. Med Sci Sports Exerc. 1998;30(4):629–633. doi: 10.1097/00005768-199804000-00023. [DOI] [PubMed] [Google Scholar]
- 30.Welk GJ, Corbin CB. The validity of the Tritrac-R3D Activity Monitor for the assessment of physical activity in children. Res Q Exerc Sport. 1995;66(3):202–209. doi: 10.1080/02701367.1995.10608834. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.