Abstract
Introduction
The paraduodenal hernia is an internal hernia that might cause a small bowel obstruction. The laparoscopic repair of paraduodenal hernia is sporadically reported for its safety, convenience, and patient's satisfaction.
Presentation of case
We performed the laparoscopic treatment of the left paraduodenal hernia in two children, a 3-months old boy and 12-year old girl. The girl had a left upper quadrant pain for one month with postprandial nausea after eating. The 3-months boy presented with an intermittent severe irritability. Small bowel series and computed tomography showed the left paraduodenal hernia in two patients. We successfully did the laparoscopic paraduodenal hernia repair using 5 mm and 3 mm laparoscope. They discharged within 5 days, uneventfully.
Discussion
Despite of technical difficulties in pediatrics such as small working space and less pneumoperitoneum, the laparoscopic repair for paraduodenal hernia leads to patient's earlier intake of diet and rapid recovery with cosmetic satisfaction. The 3 mm laparoscopic repair needs longer operation time, but it is feasible in infants.
Conclusion
Laparoscopic repair of paraduodenal hernia in children and infants is safe and feasible. We recommend the laparoscopic repair as the first surgical option for paraduodenal hernia.
Keywords: Paraduodenal hernia, Internal hernia, Mesocolic hernia
1. Introduction
The safety of laparoscopic interventions in pediatrics has been confirmed for the past 10 years.1 Smaller and shorter instruments have been developed and the 3 mm laparoscope is currently available for neonates and infants. This leads to widening of the surgical options in pediatric patients, consistently. In the literature, reports of laparoscopic repair of paraduodenal hernia are sporadic, because of the rarity of paraduodenal hernia. In particular, in pediatric surgery, it is extremely rare. We experienced two cases of left paraduodenal hernia in a 3-months boy and a 12-year old girl. Herein, we present the laparoscopic repair as the surgical option for paraduodenal hernia in children.
2. Case 1
A 12-year old girl visited our clinic because of left upper quadrant abdominal pain. Since one month prior to admission, she had to have a rest in the school infirmary 4 times per week. The pain spontaneously subsided after a time. Usually, she was eating small meal frequently because of postprandial nausea and epigastric discomfort. The X-ray revealed severely distended stomach without ileus. On abdominal computed tomography, the stomach was distended, with separated loop of jejunum by a membrane, at the left upper quadrant. There was neither strangulation nor mesenteric anomaly (Fig. 1). Small bowel series showed that the localized small bowel loop was fixated in the left upper quadrant. Both the afferent and efferent loops were visible within the hernia defect, without bowel obstruction (Fig. 2). We had a diagnosis as left paraduodenal hernia and planned the laparoscopic exploration. Under general anesthesia, the patient was laid in lithotomy position. The 5 mm laparoscope was inserted via infraumbilical trocar. The ports were placed in all 4 abdominal quadrants. At exploration, most of the small bowel loops were laying within hernia sac, covered with the mesocolon. At lifting the mesocolon, the entrapped small bowel in the hernia was reduced and we could identify the inferior mesenteric vein (Fig. 3A and B). The length of the defect was 5 cm. We approximated the fourth portion of the duodenum with the medial border of the sac, taking care not to injure the inferior mesenteric vein. Thus, we created the new duodenojejunal junction (Fig. 3C). The operation time was 90 min. At postoperative day 1, she started sips of water. At 5 days, she was discharged uneventfully.
Fig. 1.
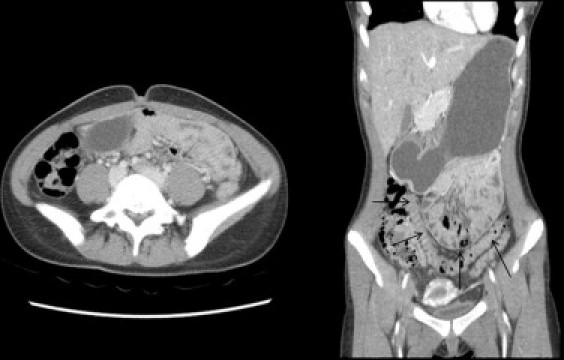
Computed tomography shows distended stomach, with loculated small bowel loop in the left upper abdominal quadrant. (Arrow indicates the hernia sac.)
Fig. 2.

Small bowel series showed that the localized small bowel loop was fixated in the left upper quadrant. Both the afferent and efferent loops were visible within the hernia sac, without bowel obstruction.
Fig. 3.
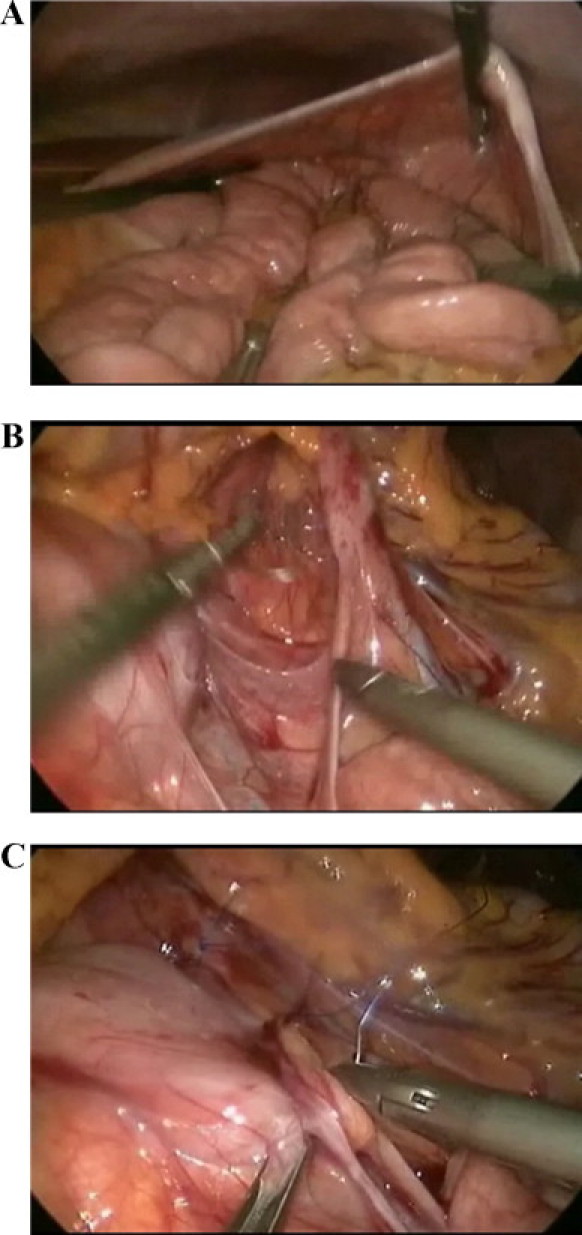
The laparoscopic photographs showed the left paraduodenal hernia sac (A) and the inferior mesenteric vein as a medial margin of sac (B). It created the new duodenojejunal junction (C).
3. Case 2
The boy was born at full term, with a birth weight of 3400 g. At 3-months old, he was admitted for RSV (respiratory syncitial virus) pneumonia. During the period of admission, he showed intermittent, severe irritability. On the X-ray, the bowel loop was deviated to the left upper abdominal quadrant and distal small bowel gas was not visible. The abdominal computed tomography showed the loculated small bowel loop at the left upper quadrant, separated from the distal bowel mesentery. Small bowel series showed the separated small bowel loop, just lateral to the fourth portion of the duodenum. After recovery from pneumonia, he underwent laparoscopic repair of the left paraduodenal hernia. We used the 3 mm laparoscope and instrument. The operative procedure was the same as in case 1. However, the pneumoperitoneum was maintained around 7–8 mm Hg. The operation time was 180 min. The next day after operation, he started breast milk feeding and was discharged uneventfully four days after surgery.
4. Discussion
An internal hernia is a protrusion of the bowel through a normal or abnormal orifice in either the peritoneum or the mesentery. Lack of fixation of the mesentery of the right and left sides of both the colon and the duodenum results in the formation of potential mesenteric defects and hernia pouches.2,3 Two internal hernias, i.e. the right and the left paraduodenal hernia (mesocolic hernia), are the most common forms, accounting for 53% of all internal hernias.4,5 The left paraduodenal hernia is about three times more frequent than the right paraduodenal hernia. However, in general, the paraduodenal hernia is very rare, just under 1% of all causes of small bowel obstruction.6
The right paraduodenal hernia leads to the entrapment of the intestine by the mesentery of the cecum and colon, because the pre-arterial limb of the duodeno-jejunal loop fails to rotate around the superior mesenteric artery.2 The left paraduodenal hernia occurs if the small intestine invaginates the connective tissue beyond the descending mesocolon, after failing to fully rotate counterclockwise around the superior mesenteric vein.7,8 The anterior edge of the hernia sac is the mesocolon that contains the inferior mesenteric vein and the left colic artery. The inferior mesenteric vein forms the neck of the hernia sac.2,7
Clinical diagnosis is usually difficult because of the vague symptoms. Most of the patients are asymptomatic.9 The chronic symptoms include recurrent and vague abdominal complaints, such as nausea, vomiting, and postprandial pain.10 The acute abdominal pain is caused by either obstruction or strangulation. The lifetime risk of incarceration of paraduodenal hernia is up to 50%. The mortality for acute presentations ranges from 20% to 50%.10 It is highly recommended to surgical correction of incidentally found paraduodenal hernia.
To make the diagnosis, radiologic studies are essential. The upper gastrointestinal series usually reveals that dilated loops of the small bowel within the upper quadrant of the abdomen, delay of contrast, or the point of obstruction.4 The abdominal computed tomography can reveal a cluster of dilated loops behind the pancreas, or the thickened peritoneum forming the hernia sac and containing the bowel loops entrapped in a particular area of the abdomen.11,12
The treatment of choice in paraduodenal hernia is operation, which includes the reduction of the herniated bowel loops, restoration of normal anatomy, and closure of the hernia orifice. During the elective operation, the reduction of small bowel is relatively easy, because the hernia orifice is not narrow and the small bowel is not dilated. To repair the hernia orifice, it should be careful not to injure the inferior mesenteric vein, left colic artery, and duodenum.13
In case of pediatrics, a few technical difficulties are present. The mesocolon is narrow and thin, which is very close to retroperitoneum. It makes a very narrow working space leading to difficulty in suturing of hernia sac. Especially, the 3 mm laparoscope and instruments used in neonates and infants make it more difficult. The pneumoperitoneum should be maintained about 7–8 mm Hg in infants. Also, the small optic view might cause a long operation time than using 5 mm laparoscope.
Until 2012, we found the 21 cases of laparoscopic repair of paraduodenal hernia described in 17 published reports based on electronic Medline search for all English articles (Table 1). They consistently pointed out that the laparoscopic repair of paraduodenal hernia resulted in a shorter hospital stay, earlier intake of diet, less postoperative ileus, and a better cosmetic results. The operative complications were inferior mesenteric vein injury, ileus, and one case of recurrence in the direct defect closure group.4,7,11,13–26 This is the first report for laparoscopic paraduodenal hernia repair for infant. Though the operation time for infant is longer than for children, the laparoscopic approach in paraduodenal hernia is safe and feasible. The hospital stay is short and the time to per os diet is just one day. The 3 mm trocar wound is nearly invisible after one month. Therefore, we recommend the laparoscopic repair of paraduodenal hernia as the first surgical option in children.
Table 1.
Reported cases of laparoscopic paraduodenal hernia repairs in the English medical literature.
| Year | Publications | Cases | Gender/Age | Affected site | Hospital day | Complication | Recurrence |
|---|---|---|---|---|---|---|---|
| 1998 | Uematsu et al. [7] | 1 | M/44 | L | 8 | n | n |
| 2000 | Finck et al. [14] | 1 | NA | L | |||
| 2004 | Fukunaga et al. [13] | 1 | M/51 | L | 7 | n | n |
| 2004 | Rollins et al. [15] | 1 | M/21 | L | 2 | n | n |
| 2004 | Antedomenico et al. [16] | 1 | F/24 | L | 3 | n | n |
| 2006 | Moon et al. [11] | 1 | M/18 | L | 1 | n | n |
| 2007 | Dassinger et al. [17] | 1 | M/13 | R | ? | n | n |
| 2007 | Shoji et al. [18] | 1 | M/60 | L | 7 | n | n |
| 2008 | Jeong et al. [19] | 2 | M/52, F/58 | L:2 | 5/5 | n | n |
| 2008 | Palanivelu et al. [20] | 4 | 3 male, 1 female | 3:L1:R | 2–6 | 1:ileus/1:IMVinjury | 1 |
| 2009 | Uchiyama et al. [21] | 1 | F/80 | L | 7 | n | n |
| 2009 | Bittner et al. [22] | 1 | F/26 | R | 1 | n | n |
| 2009 | Poultsides et al. [23] | 1 | F/67 | L | ? | n | n |
| 2010 | Parmar et al. [24] | 1 | M/38 | L | 3 | n | n |
| 2010 | Khalaileh et al. [4] | 1 | F/53 | L | 3 | n | n |
| 2011 | Al-Mufarrej et al. [25] | 1 | M/42 | L | n | n | |
| 2012 | Hussein et al. [26] | 1 | M/59 | L | 3 | n | n |
| 2012 | Nam et al. (presented case) | 2 | F/12, M/3 mo | L:2 | 5/4 | n | n |
5. Conclusion
Laparoscopic repair of paraduodenal hernia in children and infants is safe and feasible. We recommend the laparoscopic repair as the first surgical option for paraduodneal hernia.
Conflict of interest statement
None.
Funding
None.
Ethical approval
We obtained the informed consent from the patient for publication of this case report and accompanying images.
Author contributions
Kwan Woo Kim and Jin Soo Kim worked as co-operator, and Ki Hoon Kim and Sung Jin Park reviewed reference and manuscript of this article authored by So-Hyun Nam.
References
- 1.Ponsky T.A., Rothenberg S.S. Minimally invasive surgery in infants less than 5 kg: experience of 649 cases. Surg Endosc. 2008;22:2214–2219. doi: 10.1007/s00464-008-0025-7. [DOI] [PubMed] [Google Scholar]
- 2.O’Neill J.A., Grosfeld J.L., Fonkalsrud E.W., Coran A.G., Caldamone A.A. Principles of pediatric surgery. 2nd ed. Mosby Elsevier; Philadelphia: 2004. Rotational anomalies and volvulus. p. 477–83. [Google Scholar]
- 3.Estrada R.L. The paraduodenal hernias. Can J Surg. 1982;25:7–8. [PubMed] [Google Scholar]
- 4.Khalaileh A., Schlager A., Bala M. Left laparoscopic paraduodenal hernia repair. Surg Endosc. 2010;24:1486–1489. doi: 10.1007/s00464-009-0794-7. [DOI] [PubMed] [Google Scholar]
- 5.Brigham R.A., Fallon W.F., Saunders J.R. Paraduodenal hernia: diagnosis and surgical management. Surgery. 1984;96:498–502. [PubMed] [Google Scholar]
- 6.Berardi R.A. Paraduodenal hernias. Surg Gynecol Obstet. 1981;152:99–110. [PubMed] [Google Scholar]
- 7.Uematsu T., Kitamura H., Iwase M. Laparoscopic repair of a paraduodenal hernia. Surg Endosc. 1998;12:50–52. doi: 10.1007/s004649900591. [DOI] [PubMed] [Google Scholar]
- 8.Tireli M. Left paraduodenal hernia. Br J Surg. 1982;69:114. doi: 10.1002/bjs.1800690219. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan L.P., Davidson P.G., Berliner L.F. Left paraduodenal hernia. NY State J Med. 1991;91:315–317. [PubMed] [Google Scholar]
- 10.Tong R.S.K., Sengupta S., Tjandra J.J. Left paraduodenal hernia: case report and review of the literature. ANZ J Surg. 2002;72:69–71. doi: 10.1046/j.1445-2197.2002.02300.x. [DOI] [PubMed] [Google Scholar]
- 11.Moon C.H., Chung M.H., Lin K.M. Diagnostic laparoscopy and laparoscopic repair of a left paraduodenal hernia can shorten hospital stay. JSLS. 2006;10:90–93. [PMC free article] [PubMed] [Google Scholar]
- 12.Passas V., Karavias D., Grilias D. Computed tomography of left paraduodenal hernia. J Comput Assist Tomogr. 1986;10:542–543. [PubMed] [Google Scholar]
- 13.Fukunaga M., Kidokoro A., Iba T. Laparoscopic surgery for left paraduodenal hernia. J Laparoendosc Adv Surg Tech A. 2004;14:111–115. doi: 10.1089/109264204322973907. [DOI] [PubMed] [Google Scholar]
- 14.Finck C.M., Barker S., Simon H. A novel diagnosis of left paraduodenal hernia through laparoscopy. Surg Endosc. 2000;14:87. doi: 10.1007/s004649901201. [DOI] [PubMed] [Google Scholar]
- 15.Rollins M.D., Glasgow R.E. Left paraduodenal hernia. J Am Coll Surg. 2004;198:492–493. doi: 10.1016/j.jamcollsurg.2003.07.025. [DOI] [PubMed] [Google Scholar]
- 16.Antedomenico E., Singh N.N., Zagorski S.M. Laparoscopic repair of a right paraduodenal hernia. Surg Endosc. 2004;18:165–166. doi: 10.1007/s00464-003-4516-2. [DOI] [PubMed] [Google Scholar]
- 17.Dassinger M.S., Eubanks J.W. Laparoscopic repair of a right paraduodenal hernia in a child. JSLS. 2007;11:266–267. [PMC free article] [PubMed] [Google Scholar]
- 18.Shoji T., Nishiyama R., Oba K. Left paraduodenal hernia successfully treated with laparoscopic surgery: a case report. Case Rep Gastroenterol. 2007;1:71–76. doi: 10.1159/000107595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeong G.A., Cho G.S., Kim H.C. Laparoscopic repair of paraduodenal hernia comparison with conventional open repair. Surg Laparosc Endosc Percutan Tech. 2008;18:611–615. doi: 10.1097/SLE.0b013e3181825733. [DOI] [PubMed] [Google Scholar]
- 20.Palanivelu C., Rangarajan M., Jategaonkar P.A. Laparoscopic management of paraduodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia. 2008;12:649–653. doi: 10.1007/s10029-008-0376-y. [DOI] [PubMed] [Google Scholar]
- 21.Uchiyama S., Imamura N., Hidaka H. An unusual variant of a left paraduodenal hernia diagnosed and treated by laparoscopic surgery: report of a case. Surg Today. 2009;39:533–535. doi: 10.1007/s00595-008-3875-7. [DOI] [PubMed] [Google Scholar]
- 22.Bittner J.G., 4th, Edwards M.A., Harrison S.J. Laparoscopic repair of a right paraduodenal hernia. JSLS. 2009;13:242–249. [PMC free article] [PubMed] [Google Scholar]
- 23.Poultsides G.A., Zani S., Bloom G.P. Image of the month left paraduodenal hernia. Arch Surg. 2009;144:287–288. doi: 10.1001/archsurg.2008.551-a. [DOI] [PubMed] [Google Scholar]
- 24.Parmar B.P., Parmar R.S. Laparoscopic management of left paraduodenal hernia. J Minim Access Surg. 2010;6:122–124. doi: 10.4103/0972-9941.72601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Mufarrej F., Kaza J., Ahari J. Image of the month left-sided paraduodenal hernia. Arch Surg. 2011;146:233–234. doi: 10.1001/archsurg.2010.344-a. [DOI] [PubMed] [Google Scholar]
- 26.Hussein M., Khreiss M., Al-Helou G. Laparoscopic repair of a left paraduodenal hernia presenting with acute bowel obstruction: report of a case. Surg Laparosc Endosc Percutan Tech. 2012;22:e28–e30. doi: 10.1097/SLE.0b013e31823f3798. [DOI] [PubMed] [Google Scholar]


