Abstract
Objective
To assess the likely benefit of the interventions under consideration for use in Mongolia during future influenza pandemics.
Methods
A stochastic, compartmental patch model of susceptibility, exposure, infection and recovery was constructed to capture the key effects of several interventions – travel restrictions, school closure, generalized social distancing, quarantining of close contacts, treatment of cases with antivirals and prophylaxis of contacts – on the dynamics of influenza epidemics. The likely benefit and optimal timing and duration of each of these interventions were assessed using Latin-hypercube sampling techniques, averaging across many possible transmission and social mixing parameters.
Findings
Timely interventions could substantially alter the time-course and reduce the severity of pandemic influenza in Mongolia. In a moderate pandemic scenario, early social distancing measures decreased the mean attack rate from around 10% to 7–8%. Similarly, in a severe pandemic scenario such measures cut the mean attack rate from approximately 23% to 21%. In both moderate and severe pandemic scenarios, a suite of non-pharmaceutical interventions proved as effective as the targeted use of antivirals. Targeted antiviral campaigns generally appeared more effective in severe pandemic scenarios than in moderate pandemic scenarios.
Conclusion
A mathematical model of pandemic influenza transmission in Mongolia indicated that, to be successful, interventions to prevent transmission must be triggered when the first cases are detected in border regions. If social distancing measures are introduced at this stage and implemented over several weeks, they may have a notable mitigating impact. In low-income regions such as Mongolia, social distancing may be more effective than the large-scale use of antivirals.
Résumé
Objectif
Évaluer le bénéfice probable des interventions à l’étude pour une utilisation en Mongolie lors des pandémies de grippes à venir.
Méthodes
Un modèle patch stochastique et compartimenté de la susceptibilité, de l’exposition, de l’infection et du rétablissement a été établi afin d’appréhender les effets clés de plusieurs interventions – restrictions de déplacement, fermeture d’école, éloignement social généralisé, mise en quarantaine des proches contacts, traitement des contacts par antiviraux et prophylaxies – sur les dynamiques des épidémies de grippe. Le bénéfice probable ainsi que le moment et la durée optimaux de chacune de ces interventions ont été évalués au moyen de techniques d’échantillonnage latin hypercube, en calculant la moyenne de nombreux paramètres de transmission possible et de mixité sociale.
Résultats
Les interventions effectuées à temps ont permis de réduire significativement la progression et la gravité de la grippe pandémique en Mongolie. En cas de scénario pandémique modéré, des mesures précoces d’éloignement social ont diminué le taux d’attaque moyen d’environ 10% à 7-8%. De même, en cas de scénario pandémique grave, de telles mesures diminuent le taux d’attaque moyen d’environ 23% à 21%. En cas de scénario pandémique tant grave que modéré, une série d’interventions non pharmaceutiques se sont révélées aussi efficaces qu’une utilisation ciblée d’antiviraux. Les campagnes ciblées sur les antiviraux se révèlent généralement plus efficaces en cas de scénario pandémique grave qu’en cas de scénario pandémique modéré.
Conclusion
Un modèle mathématique de la transmission de la grippe pandémique en Mongolie indique que, pour être efficaces, les interventions visant à prévenir la transmission doivent être déclenchées dès la détection des premiers cas dans les régions frontalières. Si des mesures d’éloignement social sont introduites à ce stade-là et appliquées durant plusieurs semaines, leur impact réductionnel pourra être significatif. Dans des régions à faible revenu telles que la Mongolie, l’éloignement social peut être plus efficace qu’une consommation d’antiviraux à grande échelle.
Resumen
Objetivo
Evaluar la eficacia posible de las intervenciones que están siendo estudiadas para ser aplicadas en Mongolia durante pandemias de gripe futuras.
Métodos
Se construyó un modelo de parche estocástico y compartimental de susceptibilidad, exposición, infección y recuperación para detectar los efectos clave de varias intervenciones (restricciones de viaje, cierre de colegios, distanciamiento social generalizado, cuarentena de contactos cercanos, tratamiento de casos con antivirales y profilaxis de los contactos) sobre la dinámica de las epidemias de gripe. Se evaluó el beneficio posible, así como la coordinación óptima y la duración de cada una de dichas intervenciones por medio de métodos de muestreo por hipercubo latino realizando un cálculo a través de numerosos parámetros posibles de transmisión y mezcla social.
Resultados
Las intervenciones oportunas pudieron reducir de manera considerable la evolución y gravedad de la gripe pandémica en Mongolia. En una hipótesis de pandemia moderada, las medidas tempranas de distanciamiento social disminuyeron la tasa de ataque de aproximadamente el 10% al 7-8%. De igual modo, en una hipótesis de pandemia grave, dichas medidas reducen la tasa media de ataque de aproximadamente el 23% al 21%. En ambas hipótesis de pandemia, tanto moderada como grave, las intervenciones no farmacéuticas demostraron ser tan efectivas como el uso focalizado de antivirales. Las campañas antivirales focalizadas parecieron por lo general más efectivas para las hipótesis de pandemia graves que para las hipótesis moderadas.
Conclusión
Un modelo matemático de transmisión de gripe pandémica en Mongolia indicó que, para que tengan éxito, las intervenciones para prevenir la transmisión deben ponerse en marcha en cuanto se detecten los primeros casos en regiones fronterizas. Las medidas de distanciamiento social podrían tener un impacto de mitigación notable si se introducen en esta fase y se aplican durante varias semanas En las regiones de ingresos bajos como Mongolia, el distanciamiento social podría ser más eficaz que el uso de antivirales a gran escala.
ملخص
الغرض
تقييم الفائدة المحتملة للتدخلات التي يتم دراسة استخدامها في منغوليا أثناء جائحات الأنفلونزا في المستقبل.
الطريقة
تم بناء نموذج رقعة مقسمة ذي تسلسل عشوائي للحساسية والتعرض والعدوى والشفاء لالتقاط التأثيرات الرئيسية للتدخلات المتعددة على ديناميكيات وباء الأنفلونزا، مثل فرض قيود على السفر، وإغلاق المدارس، والمباعدة المعممة بين الناس، فرض الحجر الصحي على الأشخاص الذين يتم الاتصال بهم عن كثب، وعلاج الحالات باستخدام المضادات الفيروسية، ووقاية الأشخاص الذين يتم الاتصال بهم عن كثب. وتم تقييم الفائدة المحتملة والتوقيت الأمثل لكل من هذه التدخلات ومدته باستخدام تقنيات عينات المكعبات اللاتينية الزائدة وحساب متوسط العديد من متثابتات الانتقال والاختلاط الاجتماعي المحتملة.
النتائج
أدت التدخلات في الوقت المناسب إلى تخفيض الفترة الزمنية للأنفلونزا الجائحة وحدتها في منغوليا. وفي سيناريو جائحة معتدلة، أدت الإجراءات المبكرة للمباعدة بين الناس إلى خفض متوسط معدل الهجوم من حوالي 10 % إلى 7-8 %. وعلى نحو مشابه، في سيناريو جائحة حادة، خفضت هذه الإجراءات متوسط معدل الهجوم من 23 % إلى 21 % تقريبًا. وفي كل من سيناريو الجائحة المعتدلة والحادة، أثبتت مجموعة التدخلات غير الدوائية فعالية تماثل فعالية الاستخدام المستهدف للمضادات الفيروسية. وبشكل عام، اتضح أن حملات مضادات الفيروسات المستهدفة أكثر فعالية في سيناريوهات الجائحة الحادة عنها في سيناريوهات الجائحة المعتدلة.
الاستنتاج
أشار نموذج حسابي لانتقال الأنفلونزا الجائحة في منغوليا إلى أن تحقيق النجاح يستلزم إحداث تدخلات لمنع الانتقال عند اكتشاف الحالات الأولى في المناطق الحدودية. وفي حالة اللجوء إلى إجراءات المباعدة بين الناس في هذه المرحلة وتنفيذها على مدار عدة أسابيع، ربما تحقق تأثيرًا تخفيفيًا ملحوظًا. وفي الأقاليم منخفضة الدخل مثل منغوليا، قد تكون المباعدة بين الناس أكثر فعالية من الاستخدام واسع النطاق لمضادات الفيروسات.
摘要
目的
评估考虑在未来流感大流行期间在蒙古实施的干预的可能益处。
方法
构建敏感性、暴露、感染和复原的随机、区划补丁模型捕捉多个干预(旅行限制、学校关闭、广义的社会疏远、密切接触者隔离、抗病毒药病例治疗和预防接触)对流行感冒力度的关键作用。使用拉丁超立方体采样技术,求出多个可能的传播和社会混合参数平均值,评估每个干预的可能益处、最佳时间和持续时间。
结果
及时干预可能显著降低蒙古大流行性流感的时间进程和严重性。在中度流行情况下,早期社会疏远方法可以将平均发病率从约 10% 降低至 7–8%。同样,在严重流行情况下,这种方法可以将平均发病率从大约 23% 降低至 21%。在中度和严重流行情况下,一系列非药物干预已证明具有和使用针对性抗病毒药一样的效果。针对性抗病毒药活动在严重流行情况下的效果一般会比中度流行情况下的效果好。
结论
蒙古大流行性流感传播的数学模型表明,要想成功,需要在边境地区检测到首个病例时触发防止传播的干预措施。如果在此阶段采用社会疏远方法并且持续多个星期,则具有显著的缓解作用。在低收入地区,如蒙古,社会疏远方法比大规模使用抗病毒药物更有效。
Резюме
Цель
Оценить предполагаемую эффективность и пользу рассматриваемых в Монголии мер, направленных на борьбу с будущими пандемиями гриппа.
Методы
Для получения основных результатов, демонстрирующих влияние на динамику распространения пандемии гриппа определенных мер, таких как ограничение поездок, закрытие школ, общее социальное дистанцирование, введение карантина для тесно контактирующих людей, лечение больных противовирусными препаратам и профилактика контактов, была создана стохастическая блоковая модель восприимчивости, контактов с источником заражения, инфицирования и восстановления. Предполагаемые выгоды, а также оптимальные сроки и продолжительность каждой из этих мер были оценены с использованием метода выборочного контроля «латинский гиперкуб», который позволяет вывести средние значения, основываясь на многих возможных путях передачи вируса и параметрах взаимодействий в обществе.
Результаты
Своевременное принятие мер может существенно сократить продолжительность и интенсивность пандемии гриппа в Монголии. В сценарии умеренной пандемии ранние меры по увеличению социальных расстояний снизили среднюю интенсивность распространения с 10% до 7–8%. Подобным образом в сценарии сильной пандемии аналогичные меры снизили среднюю интенсивность распространения приблизительно с 23% до 21%. В обоих сценариях – с умеренной и сильной пандемией – комплекс нефармацевтических мер позволил достичь такой же эффективности, как и направленное использование противовирусных средств. В сценариях с сильной пандемией направленные противовирусные кампании продемонстрировали более высокую эффективность по сравнению со сценариями с умеренной пандемией.
Вывод
Математическая модель передачи вируса гриппа в Монголии продемонстрировала, что для достижения успешных результатов применения мер по предотвращению распространения вируса, необходимо задействовать эти меры при обнаружении первых случаев обнаружения вируса в пограничных регионах. Если меры по социальному дистанцированию будут применены на этом этапе на протяжении нескольких недель, они могут в значительной степени уменьшить распространение вируса. В регионах с низким уровнем доходов, таких как Монголия, социальное дистанцирование может быть более эффективным, чем полномасштабное использование противовирусных препаратов.
Introduction
The efficient use of resources to mitigate the spread of an emerging infectious disease is of global interest. However, the most appropriate control strategies in any given area probably depend on the nature of the local population and environment. Implementing interventions against emerging infectious diseases is particularly important in developing countries, such as Mongolia, where the capacity to provide health care and undertake detailed surveillance is limited. Since the identification of highly pathogenic avian influenza in Mongolia in 2005,1 the Mongolian government has been particularly aware of the threat posed by influenza to public health. Mongolia’s vulnerability to influenza was reinforced by the impact on the country of A(H1N1)pdm09, which was no less severe than in countries affected earlier (even though the virus was not recorded in Mongolia until 4 to 5 months after the first cases of human infection were detected in China and the Russian Federation).1
Mongolia’s vast landscape of over 150 million hectares is divided into 21 provinces called aimags. Although the mean population density is only 1.5 people per square kilometre, some regions of the country are now highly urbanized and more than 30% of the country’s inhabitants reside in the capital city, Ulaanbaatar. Recognition of the threat of highly pathogenic avian influenza has been influential in overcoming the challenges of developing nationwide surveillance capabilities. Over 100 influenza sentinel surveillance sites have been designated across the country. At the Category-I surveillance sites, cases of influenza-like-illness (ILI) are reported daily and samples for virological analysis are collected routinely from each such case. At the other (Category-II and Category-III) sentinel surveillance sites, ILI cases are reported weekly and samples for virological analysis are only collected occasionally. This approach to influenza surveillance allowed a large amount of epidemiological and virological information to be collected during the 2009–2010 influenza season.
In week 40 of 2009 (i.e. at a time of year when seasonal influenza epidemics had previously occurred in Mongolia)2 sentinel surveillance sites first reported elevated levels of ILI activity: between 20 and 50 cases per 10 000. The sites reporting such activity were all Category I and in the border aimags of Dornod, Dornogovi and Khovd. A(H1N1)pdm09 was virologically confirmed among the cases from these sites. By week 42 the incidence of reported ILI exceeded 50 cases per 10 000 in Ulaanbaatar and 20 cases per 10 000 in all the eastern aimags and, nationally, most subtyped viruses were identified as A(H1N1)pdm09. The establishment of A(H1N1)pdm09 transmission in the dense population of Ulaanbaatar probably led to the rapid spread of cases in the capital and the rapid dissemination of the virus to the rest of Mongolia. The epidemic reached a distinct peak in weeks 44–45, when the reports of ILI were dominated by the cases in Ulaanbaatar, although, by then, every aimag except Bayan-Ölgii in the far west was reporting more than 50 ILI cases per 10 000 (Appendix A, available at: http://mathmodelling.sph.unimelb.edu.au/publications/Bolton-BullWorldHealthOrgan-2011-AppendixA.pdf). The period of prolonged, lower-level activity that followed the epidemic peak probably reflected the dissipation of the virus into remote areas, perhaps facilitated by the virus being brought into Mongolia again via border crossings. The A(H1N1) 2009 pandemic activity had not long subsided when influenza B cases were reported, in week 6 of 2010. New cases of infection with A(H1N1)pdm09 subsequently became rare as the population experienced a severe epidemic of influenza B.3
Sentinel surveillance reports, based on medically reported cases of ILI in 2009, reveal that the total ILI attack rate (i.e. the percentage of the population that became infected over the course of the pandemic) was about 10%. The results of the serological survey that enabled the A(H1N1)pdm09-specific attack rate to be determined have yet to be reported (A Burma, personal communication, 2011). ILI reporting rates were highest among children aged less than 5 years and young adults,2 reflecting the global experience.4 There were also high rates of ILI among teenagers, probably, at least in part, because people aged 10–20 years comprise 30% of the population.5Hospitalization rates in the hospital-based sentinel surveillance sites increased three- to fourfold during the pandemic, largely because of an increase in the number of hospitalized pneumonia cases.6 There was also a stark increase in the pneumonia mortality rate among adults aged 20–59 years.6 Disease severity during the Mongolian influenza pandemic appears to have exceeded that of similar epidemics in many developed countries, possibly because chronic conditions such as renal and cardiovascular disease, which have been identified as potential risk factors for severe respiratory disease, are relatively common in Mongolia.7
The interventions implemented against influenza virus transmission during the 2009 pandemic were triggered by the detection of elevated ILI activity in Ulaanbaatar in week 42. The first intervention was the closure of primary schools. High schools and kindergartens were also soon closed for a period of several weeks. In week 45, further social distancing measures were imposed in Ulaanbaatar. Restrictions included limiting the opening hours of shops, cafes and restaurants, banning public gatherings and closing markets. Provincial rail and road travel was interrupted for a period of several weeks. In addition to these mandatory social distancing measures, all citizens were advised to minimize activity outside of their homes and to wear facial masks, and symptomatic individuals were encouraged to stay in self-imposed quarantine at home.2 Institutions and businesses were recommended to supply staff with vitamin supplements to “build health”.8 Although no formal evaluation of public compliance is available, anecdotal evidence indicates that the intervention measures were generally well accepted. Initiatives such as the broadcasting of school lessons on national television probably facilitated compliance. While the resources and infrastructure deemed necessary for effective epidemic containment by non-pharmaceutical means are probably found in very few settings,4 less stringent measures may still usefully reduce the burden on acute health-care services. International borders remained open during the 2009 pandemic in Mongolia. Although border screening was in place in Ulaanbaatar, the first case of A(H1N1)pdm09 infection was detected through the national surveillance network.2
The Mongolian government’s stockpile of around 80 000 doses of the antiviral drug oseltamivir was exhausted during the 2009 pandemic. Although oseltamivir was taken as prophylaxis by some health-care workers, the drug was predominantly used to treat severe hospitalized cases.7 The Mongolian government purchased vaccine against A(H1N1)pdm09, which was supplemented by donations from the World Health Organization (WHO). However, vaccine roll-out only commenced in January 2010 after the epidemic peaked.4
Here we use the epidemiological data collected during the 2009 influenza pandemic in Mongolia to calibrate a computational model of influenza virus dissemination in a Mongolian pandemic, with tailoring to the country’s infrastructural and sociobehavioural characteristics. We explore the likely impact of various nationwide social distancing and pharmaceutical interventions on mitigating the spread of a pathogen, with particular emphasis on a novel influenza strain with established transmission in the human population. Earlier country-specific evaluations of the likely impact of interventions on influenza have focused on the containment of highly pathogenic avian influenza outbreaks in south-eastern Asia9,10 and the United States of America.11 There have been few recent, country-specific evaluations of strategies for the mitigation of influenza, particularly in resource-poor settings. Our results provide novel insights into the probable benefits of anti-influenza interventions in Mongolia, some of which are potentially relevant in pandemic planning in other low-income regions.
Methods
Modelling transmission during interventions
Influenza transmission was explored using a stochastic, computational model of susceptibility, exposure, infection and recovery.12,13 Large-scale spatial transmission was captured by geographically dividing the population into 14 patches chosen to isolate border crossings, sentinel surveillance sites, urbanized regions and other regions of national interest. The 14 patches, which were allowed to interact via a travel matrix, 14 were individual aimags (Bayan-Ölgii, Bulgan, Darkhan-Uul, Dornod, Khovd, Orkhon, Övörkhangai, Selenge, Uvs), combinations of two (Dornogovi + Ömnögovi, Govi-Altai + Zavkhan), three (Arkhangai + Bayankhongor + Khövsgöl) or five aimags (Dundgovi + Govisümber + Khentii + Sükhbaatar + Töv), and the municipality of Ulaanbaatar (Appendix A). Inter-patch mixing was generally only significant between neighbouring patches and between each of the other patches and Ulaanbaatar. The importation of A(H1N1)pdm09-infected cases into border patches was modelled using the time-courses of the 2009 pandemic in neighbouring countries and the relative frequency of border crossings. The basic reproduction rate (R0) used as the baseline in the model was based on epidemiological observations in other countries,15–19 but a wide range of values, including more severe scenarios with R0 varying around 2, was explored. The data were modelled and graphically displayed using Matlab (MathWorks Inc., Natick, USA).
The model was configured to allow evaluation of the likely effects of travel restrictions, school closure, generalized social distancing, quarantining of close contacts of presenting cases and distribution of an antiviral drug to the ill and their close contacts.
Assessment of intervention strategies
Pandemic scenarios beginning at week 35 were simulated. The impact of travel restrictions, school closure and generalized social distancing was assessed, with each intervention beginning at various time points ranging from week 35 to week 49 and varying in duration from 2 to 12 weeks. The effects of the ongoing quarantining of the contacts of presenting cases during the epidemic and of the continuous distribution of an antiviral drug to contacts until the national stockpile of the drug was exhausted were also investigated, with the presumption that each of these interventions would be implemented from the first case. It was conservatively assumed that the cases themselves could not be quarantined early enough to reduce their overall infectiousness.
Latin-hypercube sampling (LHS)20 was used for a sensitivity analysis of the various parameters describing the effects of intervention timing and efficiency on intervention impact. The LHS technique allowed the average impact of an intervention to be estimated despite uncertainties in the characteristics of the pathogens involved and the nature and intensity of the population mixing. Sampling was conducted over many different parameters related to travel and importation rates, the virus-dependent factors of transmission and the details of each intervention (sampling ranges in Appendix A). The LHS approach allowed us to detect possible associations between model parameters (including those characterizing an intervention measure) and various statistics capturing the severity of the pandemic, as well as to estimate the uncertainty around these associations. By using LHS we hoped to identify the intervention strategies that would be optimal across a range of potential pandemic scenarios in Mongolia.
Results
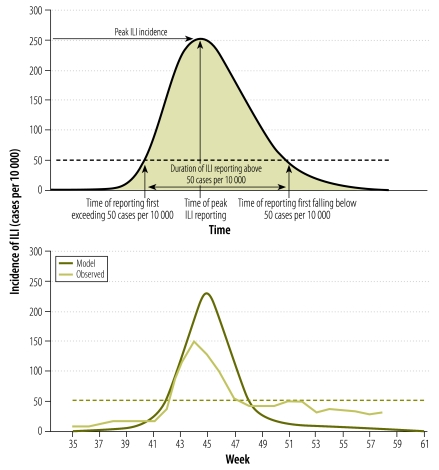
Epidemic curves for the baseline model are shown for Mongolia as a whole (Fig. 1), along with the corresponding observed data for the 2009–2010 pandemic. Our model was also able to capture the diversity in observed epidemic curves between patches (Appendix A). Patches encompassing urbanized regions (such as Ulaanbaatar) tended to exhibit early, rapidly-peaking outbreaks, whereas patches containing rural regions (e.g. Selenge) exhibited more prolonged epidemics. Patches encompassing western aimags (such as Uvs) tended to experience relatively late-peaking epidemics. Several of the patches containing border regions (such as Bulgan and Ömnögovi) displayed double-peaked epidemics.
Fig. 1.
Statistics used to characterize epidemic timing and severity and to assess intervention impact (upper panel), and observed and modelled incidences of influenza-like illness (ILI; lower panel), Mongolia, 2009–2010
Note: The final attack rate, representing the percentage of the total population infected during the epidemic, is given by the shaded area in the upper panel. The data shown in the lower panel cover the period in which A(H1N1)pdm09 was the dominant subtyped virus, with baseline parameters used in the model.
Three key measures of intervention success were evaluated in the model: the total (presenting) ILI attack rate, the peak ILI reporting rate and the time of peak ILI reporting (Fig. 1). The mean attack rates seen in the model when a single non-pharmaceutical or pharmaceutical intervention was included are shown in Fig. 2. When no intervention was included in the moderate-epidemic model, the mean attack rate was 9.7% and the mean peak ILI rate, which was seen at week 44.5, was about 240 cases per 10 000. In the severe epidemic scenario, the mean attack rate was about 23%, and the mean peak ILI rate, of 800 cases per 10 000, occurred, on average, during week 42.
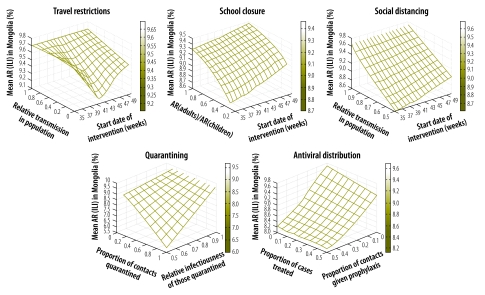
Fig. 2.
Modelled mean attack rates (AR) for influenza-like illness (ILI) when any one of five interventions is introduced in a moderate pandemic, Mongolia, 2009
Note: The attack rates shown are mean national values (over 500 simulated outbreaks) when the intervention was implemented for 4 weeks. For example, the upper left panel illustrates that the impact of 4 weeks of travel restrictions is greatest, reducing the attack rate to approximately 9.1%, when the propensity to travel is zero and the restrictions are implemented from week 42.
Non-pharmaceutical interventions
In the model, the apparent efficacy of social distancing interventions rapidly fell once the frequency of reported ILI cases exceeded approximately 20 cases per 10 000. At lower ILI reporting rates, representing the early phases of the modelled pandemic, school closures, generalized social distancing or sustained travel restrictions had a substantial mitigating effect. In the actual epidemic of 2009, an ILI reporting rate of 20 cases per 10 000 was recorded during week 40 in the border aimags of Khovd, Dornod and Dornogovi. In the model, school closures or generalized social distancing implemented before the ILI reporting rate reached 20 cases per 10 000, resulted in better mitigation than the very early implementation of travel restrictions of limited duration (which left large numbers of susceptible and infected hosts when the restrictions were relaxed). Although more prolonged interventions appeared relatively more effective in the model, the long-term implementation of any intervention in the field may be hampered by falling compliance and/or logistical challenges. Below we focus on the impact of 4-week interventions in the moderate-epidemic scenario, since the interventions used against the 2009 pandemic in Mongolia appear to have been successfully implemented for about 4 weeks.
In the model, a 50% reduction in mean travel frequency, if applied early in the epidemic (i.e. from week 40, as the ILI reporting rates reached 20 cases per 10 000), delayed the pandemic peak by approximately 1.5 weeks if maintained for 4 weeks and by about 1 week if maintained for 2 weeks. Travel restrictions increased the time-scale over which the modelled pandemic occurred by slowing the spatial spread. They also resulted in a reduction in the peak ILI rate, by about 12%, if enforced for 4 weeks. They only reduced the modelled attack rates by less than 0.1%, however, even when travel frequency was reduced by 95% (Fig. 2).
Substantial reductions in the mean attack rate could be seen, nonetheless, when prolonged school closure or generalized social distancing was added to the model. For school closure to be effective, the attack rate in children had to be over double that in adults. If, for example, schools were closed for 4 weeks from week 40, when the attack rate in children was threefold higher than in adults,21 the model indicates that the overall attack rate would decrease from 9.7% to approximately 8.6% (Fig. 2) and, perhaps more importantly, that the epidemic peak would be delayed by over a week. School closure implemented before week 40 could delay the time to the pandemic peak by as long as 2 weeks. In general, school closure had only a modest impact on the modelled mean peak ILI rate.
On average, the inclusion in the model of social distancing measures that reduced transmission probability by 50% from week 40 reduced the attack rate from 9.7% to 8.6% (Fig. 2), delayed the time to the peak ILI reporting rate by almost 2 weeks and reduced the peak case-load by about 8%.
The model indicated that the impact of the continuous quarantining of a proportion of the individuals identified as contacts of those who present with an ILI could be very substantial. In a scenario in which 50% of known contacts were traced and quarantined, for example, the peak case-load decreased by 25%, the attack rate was reduced by more than 1.5% (Fig. 2) and the time of peak incidence was delayed by around 1 week.
Targeted antiviral interventions
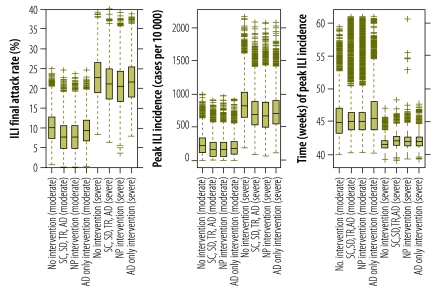
Using the model, we considered the treatment, from the first detected case, of a percentage of infected hosts and the timely prophylaxis of a proportion of their contacts, assuming a finite national stockpile of the antiviral drug used (10 000–500 000 doses). In a scenario in which half of the known contacts were traced and given the antiviral drug, such a targeted intervention reduced the mean attack rate by about 2%, delayed the peak case-load by a mean of 2–3 weeks and reduced the peak case-load by approximately 30% (Fig. 2 and Fig. 3). Although the attack rate decreased by a mean of about 1% when the modelled stockpile was increased from 50 000 doses to 500 000, the corresponding range in the expected attack rates was much greater than this mean reduction, which suggests that the specific nature of the epidemic has a larger impact on the outcome of antiviral usage than the stockpile size (Appendix A). Antiviral drug use, as an isolated measure, appeared relatively more effective in the severe pandemic scenario, where the presenting proportion is generally higher than in the moderate pandemic scenario. In both of these scenarios, however, a suite of non-pharmaceutical interventions had a slightly greater average impact on the attack rate and peak ILI incidence than antiviral drug use as a single intervention (Fig. 3).
Fig. 3.
Distributions of three different statistics capturing epidemic severity in models of influenza epidemics in Mongolia
AD, antiretroviral distribution; ILI, influenza-like illness; NP, non-pharmaceutical; SC, school closure; SD, social distancing; TR, travel restrictions.
Note: The data on ILI are based on scenarios in which Mongolia is struck by a moderate or severe pandemic of influenza and there are no interventions or non-pharmaceutical interventions – school closure, social distancing and travel restrictions – and/or targeted antiviral drug distribution. The bottom and top of each box indicate the 25th and 75th percentiles, with the height of the box therefore indicating the interquartile range. The line dissecting the box is the median value. Dashed lines (whiskers) extend 1.5 times the interquartile range, with any data points beyond the whisker length marked as crosses.
Discussion
Our model was able to capture the gross characteristics of the actual 2009 influenza pandemic in Mongolia, including the variations between aimags. Although elevated ILI activity was first registered in several border aimags (including Dornogovi) at about the same time in 2009, A(H1N1)pdm09 was probably spread into Dornogovi from northern China and Ulaanbaatar (the site of Mongolia’s sole international airport) via high rates of simultaneous importation of the virus. The particularly severe winter of 2009–2010 is suspected to have affected the pandemic in Mongolia. Our neglect of seasonal and other secondary effects, such as age-dependency in immune response and population mixing, and perhaps our failure to consider all the interventions used, limited our ability to fit the modelled data to the detailed shape of the actual epidemic curve seen in the 2009 pandemic (Fig. 1).
In models involving a range of possible nationwide mitigation strategies in moderate- and severe-pandemic scenarios, mean reductions in the attack rate of up to 2%, reductions in the peak ILI reporting rate of up to 25%, and delays to epidemic peak of over a week were observed. The modelled impact of each mitigation measure that was considered varied significantly with the nature, timing and efficacy of the intervention. Although our results indicate that Mongolia’s capacity to curtail a nationwide epidemic similar to the one in 2009 is limited, even modest reductions in epidemic severity may substantially ease the burden on health-care systems in resource-poor settings such as Mongolia.
The benefits of travel restrictions in curtailing a nationwide epidemic may be limited once the pathogen involved has reached a congested city from which, and to which, there is widespread travel. In Mongolia, for example, travel restrictions would probably have little impact if implemented only after an epidemic had been established in Ulaanbaatar, the country’s pre-eminent cultural and economic centre. The distinct temporal offsets seen between the epidemics in different states or territories during Australia’s A(H1N1) 2009 epidemic are thought largely to reflect the role of several large or capital cities in disseminating the virus to the surrounding sparsely populated regions in this country.22
Although reduced community mixing through school closures and restricted social interaction on a wider scale appears potentially useful, it is difficult to establish the required nature of effective, generalized, social distancing measures. If we assume that the attack rate in children is over twice that in adults, as expected in a pandemic scenario since children mix intensely and lack protection, school closure may delay the time to peak case-load by several weeks, as well as modestly reduce the attack rate. As sociological studies indicate that up to half of a person’s daily contacts can typically be named by that person,23 it may also often be possible to trace and quarantine sufficient case contacts to substantially reduce epidemic severity. The tracing of contacts of the very early cases, which usually occur before the threat of a pandemic has been realized, is, however, often difficult. One limitation of this study is that no allowance was made for virus transmission at the household level, which may be boosted when social distancing measures and quarantining are implemented. The apparent benefits of such measures may therefore have been somewhat overestimated.
The widespread prophylactic use of antiviral drugs has more mitigation potential than case treatment alone.12,24 Diagnostic and delivery capabilities are, however, crucial in determining the effectiveness of an antiviral campaign. The effectiveness of prophylaxis early in an epidemic is limited by the capacity to distinguish seasonal and epidemic/pandemic ILI cases, which typically requires expensive high-specificity diagnostic testing based on polymerase chain reactions. Even without considering this limitation, the present modelling indicates that the timely implementation of a combination of non-pharmaceutical interventions would be at least as effective as the distribution of an antiviral drug. Given that even developed countries struggled to use antiviral drugs to achieve a significant mitigating impact on pandemic influenza in 2009,25 the use of non-pharmaceutical interventions – instead of, or in combination with, antiviral distribution – is to be encouraged, especially in resource-poor settings.
Timeliness is key to the success of any within-country intervention strategy. Effective intervention measures need to be triggered by early case detection provided by nationwide surveillance systems with regular case reporting. Monitoring cases in areas containing border crossings, such as Dornogovi, or international travel hubs, such as Ulaanbaatar, is crucial. Containment in regions contributing significantly to border crossings, together with the routine international sharing of surveillance data as recommended by WHO,1 should also enhance within-country mitigation capabilities.
The model used in this study was tailored to the ecology of Mongolia during the 2009 pandemic. Climatic, demographic and infrastructural conditions will influence population distribution, mixing characteristics and inter-provincial travel. For example, the higher propensity to travel in summer owing to the traditional nomadic lifestyle of many Mongolians may result in more rapid spatial spread for an out-of-season influenza epidemic than for the pandemic in the winter of 2009–2010. Infrastructural evolution driven by the mining boom – such as the new rail and road networks linking Mongolia with the Russian Federation and border areas of China – may also alter the characteristic mixing between provinces and population clustering. Pandemic planning policy, even in a given country, needs to be regularly reassessed to ensure that it is relevant to the current sociobehavioural conditions.
Acknowledgements
The authors thank medical personnel in the Mongolian influenza sentinel surveillance sites for collecting morbidity and mortality data and samples for virological examination, and the Centers for Disease Control and Prevention (Atlanta, USA) for the technical and financial support of the National Influenza Centre in Mongolia, through the US/Mongolia Cooperative Agreement (projects U50/CCU024411 and IU51IP000331). The staff of the National Emergency Management Agency kindly provided support during fieldwork in Mongolia in July 2010.
Funding:
This paper reports on work commissioned by the Avian and Human Influenza Control, Preparedness and Response Project, National Emergency Management Agency, Mongolia, sponsored by The World Bank. Authors received support from a University of Melbourne McKenzie Fellowship (KJB) and a National Health and Medical Research Council Career Development Award (JM).
Competing interests:
None declared.
References
- 1.World Health Organization [Internet]. Mongolia. Geneva: WHO; 2009. Available from: http://www.who.int/csr/don/archive/country/mng/en/ [accessed 19 January 2012].
- 2.Nymadawa P. Non-pharmaceutical control measures and epidemiology of A(H1N1) 2009 pandemic influenza in Mongolia. In: Proceedings of the International Conference on Emerging Infectious Diseases; 2010 July 11–14; Atlanta, United States of America Atlanta: Centers for Disease Control and Prevention; 2010. p. 94. [Google Scholar]
- 3.Nymadawa P, Burma A, Darma B, Enkhsaikhan D, Tsatsral S, Naranzul T, et al. The first wave of influenza A(H1N1) 2009 pandemic in Mongolia. Influenza Other Respi Viruses. 2011;5(Supplement 1):163–5. [Google Scholar]
- 4.Leung GM, Nicoll A. Reflections on pandemic (H1N1) 2009 and the internatinal response. PLoS Med. 2010;7:e1000346. doi: 10.1371/journal.pmed.1000346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nukiwa N, Burmaa A, Kamigaki T, Darmaa B, Od J, Od I, et al. Evaluating influenza disease burden during the 2008-2009 and 2009-2010 influenza seasons in Mongolia. WPSAR 20112(1) 10.5365/wpsar.2010.1.1.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nymadawa P. Hospital-based influenza surveillance in Mongolia. Geneva: GABRIEL Network [Internet]. Available from: http://www.globe-network.org/documents/gabriel/newsletter/newsletter-7.pdf [accessed 19 January 2012].
- 7.Health indicators 2010 Ulaanbaatar: Implementing Agency of Health Department, Government of Mongolia; 2011. [Google Scholar]
- 8.National Influenza Center [Internet]. Recommendation from the Fifth National Influenza Workshop Bayanzurkh: National Center of Communicable Diseases, Ministry of Health; 2009. Available from: http://www.flu.mn/eng/index.php?option=com_content&task=view&id=171&Itemid=52 [accessed 18 January 2012]. [Google Scholar]
- 9.Longini IM, Nizam A, Xu S, Ungchusak K, Hanshaoworakul W, Cummings DAT, et al. Containing pandemic influenza at the source. Science. 2005;309:1083–7. doi: 10.1126/science.1115717. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson NM, Cummings DAT, Cauchemez S, Fraser C, Riley S, Meeyai A, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437:209–14. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 11.Longini IM, Halloran ME, Nizam A, Yang Y. Containing pandemic influenza with antiviral agents. Am J Epidemiol. 2004;159:623–33. doi: 10.1093/aje/kwh092. [DOI] [PubMed] [Google Scholar]
- 12.McCaw JM, McVernon J. Prophylaxis or treatment? Optimal use of an antiviral stockpile during an influenza pandemic. Math Biosci. 2007;209:336–60. doi: 10.1016/j.mbs.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Moss R, McCaw JM, McVernon J. Diagnosis and antiviral intervention strategies for mitigating an influenza epidemic. PLoS One. 2011;6:e14505. doi: 10.1371/journal.pone.0014505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riley S. Large-scale spatial-transmission models of infectious disease. Science. 2007;316:1298–301. doi: 10.1126/science.1134695. [DOI] [PubMed] [Google Scholar]
- 15.Fraser C, Donnelly C, Cauchemez S, Hanage W. Pandemic potential of a strain of influenza A (H1N1): early findings. Science. 2009;324:1557–61. doi: 10.1126/science.1176062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nishiura H, Castillo-Chavez C, Safan M, Chowell G.Transmission potential of the new influenza A (H1N1) virus and its age-specificity in Japan. Eurosurveillance 200914(22) [DOI] [PubMed] [Google Scholar]
- 17.Fielding J, Higgins N, Gregory J, Grant K.Pandemic H1N1 influenza surveillance in Victoria, Australia, April-September, 2009. Eurosurveillance 200914(42) [DOI] [PubMed] [Google Scholar]
- 18.Baker M, Kelly H, Wilson N.Pandemic H1N1 influenza lessons from the southern hemisphere. Eurosurveillance 200914(22) [DOI] [PubMed] [Google Scholar]
- 19.White LF, Wallinga J, Finelli L, Reed C, Rilez S, Lipsitch M, et al. Estimation of the reproductive number and the serial interval in early phase of the 2009 influenza A/H1N1 pandemic in the USA. Influenza Other Respi Viruses. 2009;3:267–76. doi: 10.1111/j.1750-2659.2009.00106.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoare A, Regan D. Sampling and sensitivity analyses tools (SaSAT) for computational modelling. Theor Biol Med Model. 2008;5:4. doi: 10.1186/1742-4682-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glass K, Barnes B. How much would closing schools reduce transmission during an influenza pandemic? Epidemiology. 2007;18:623–8. doi: 10.1097/EDE.0b013e31812713b4. [DOI] [PubMed] [Google Scholar]
- 22.Influenza surveillance 2009 [Internet]. Woden: Department of Health and Ageing, Australian Government. Available from: http://www.health.gov.au/internet/main/publishing.nsf/Content/cda-ozflu-no21-09.htmhttp://[accessed 19 January 2012].
- 23.Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5:e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McVernon J, McCaw JM, Nolan TM. Modelling strategic use of the national antiviral stockpile during the CONTAIN and SUSTAIN phases of an Australian pandemic influenza response. Aust NZ J Public Health. 2010;34:113–9. doi: 10.1111/j.1753-6405.2010.00493.x. [DOI] [PubMed] [Google Scholar]
- 25.Becker NG, Wang D. Can antiviral drugs contain pandemic influenza transmission? PLoS One. 2011;6:e17764. doi: 10.1371/journal.pone.0017764. [DOI] [PMC free article] [PubMed] [Google Scholar]