Abstract
The threat of global infectious agents has the potential to cripple national and global economies, as the outbreaks of SARS, Avian Flu, H1N1, and XDR-TB have demonstrated. This article offers a Root Cause Analysis (RCA) of one public health case study – the Speaker case of XDR-TB – pinpointing the underlying causal relationships associated with this global health incident and proposing recommendations for preventing its recurrence. An RCA approach identifies corrective actions directed at the root causes of the problem and advances them as necessary to eliminate global contagion with its major international public health risks. To my knowledge, this is the first root cause analysis of a global health problem. The reform this article proposes would be to add a standardized procedure akin to the informed consent process in clinical ethics, but within a shared health governance framework. This approach, addressing infectious agents at their origins or source, is potentially a more effective strategy to reduce uncertainty and avert global health threats.
Background and Introduction
Drug-Resistant Tuberculosis and the Speaker Case
In May 2007, the United States government isolated an individual under Centers for Disease Control and Prevention (CDC) auspices for the first time since 1963 (when it quarantined a patient with smallpox). The 2007 patient was Andrew Speaker, from Atlanta, Georgia, who was thought to have extensively drug-resistant tuberculosis (XDR-TB). XDR-TB can be transmitted by air to others in close proximity and is highly fatal; in South Africa it has been found to be deadly in approximately 98 percent of cases.1
The case (hereafter called the “Speaker case”) was complicated by Speaker's extensive travels, including two trans-Atlantic flights, some five flights within Europe, and at least one cross-national car ride – an itinerary that originated in the United States and included France, Greece, Italy, the Czech Republic, and Canada before ending back in the U.S.2 During his two long trans-Atlantic flights, he could have infected other passengers, especially those within two rows of his seat. Further, county and federal health department officials (including the CDC) and Speaker himself believed he was infected with multidrug-resistant TB (MDR-TB) before he left the United States. Fulton County health officials claim they warned him of the potential danger to others before his trip, but that he disregarded their warning.3 Mr. Speaker says county officials at the time told him he was not contagious.4 In Atlanta, officials issued a written directive against travel, but did not deliver it to his home before his departure, allegedly because Mr. Speaker moved his departure date up two days.5
After Speaker's departure, officials came to believe that he had the even more serious form of drug-resistant TB, XDR-TB, an extremely rare disease: only 49 U.S. cases were identified between 1993 and 2006.6 (Later, on July 3, 2007, doctors downgraded Speaker's diagnosis from XDR-TB to MDR-TB.7) After the diagnosis, the CDC contacted him in Rome, asking him not to take commercial flights. While the CDC was making arrangements for his travel, he left Rome, took a commercial flight to Montreal, and drove to the United States by car.8 An agent at the Canadian-U.S. border let him into the country, though the agent knew that health authorities sought him.9
At first glance, the case sounds eerily similar to the SARS (Severe Acute Respiratory Syndrome) outbreak that shook the globe in 2003, spreading to over 30 countries in just a few weeks, infecting 8,096 and killing 774 people worldwide.10 Since that time, the World Health Organization (WHO) and the World Health Assembly have revised the International Health Regulations (IHR), in part to help international and domestic health agencies plan, coordinate, and communicate both within and across countries to better respond to global infectious agents and to minimize their potential consequences.11 At the U.S. federal level, Executive Order 13375 in 2005 amended the Public Health Services Act (PHSA) to add influenza to the list of quarantinable illnesses and heightened attention to the police powers of the state to isolate and contain infected individuals.12 These changes in international and U.S. federal health law notwithstanding, the Speaker case raises questions about the appropriate roles for international, federal, state, and local governments, along with health care personnel and individuals themselves, in addressing global infectious agents.
Root Cause Analysis
This article analyzes the Speaker case by employing Root Cause Analysis methodology. RCA has been used in a variety of situations, ranging from accident and failure analysis to operations and systems analysis. It holds significant promise for examining and solving global health problems. Global health encompasses complex systems and interrelated levels (global, national, local, individual), tools (laws, policies, norms), and actors (governments, nongovernmental organizations, health care personnel, individuals). RCA allows a comprehensive system-wide perspective that breaks down complex global health problems into increasingly smaller components, enabling in-depth analysis from one level and dimension to the next. RCA rests on the premise that getting at the root cause of a problem is more effective than addressing “immediately obvious” symptoms, and that a problem typically has more than one root cause. RCA is especially applicable to global health because it takes both vertical and horizontal perspectives, and its end goals are uncertainty reduction and risk avoidance. While a full description of RCA is beyond the scope of this article, central features of the methodology include recursive questioning to identify causal factors and root causes related to a problem, and identifying effective solutions to prevent recurrence.13 To my knowledge, this is the first root cause analysis of a global health problem.
In applying the RCA methodology, this article identifies the components and questions involved in dealing with infectious diseases in a globalized world and offers recommendations for uncertainty reduction and risk management, using the Speaker case as an illustration. In the spirit of the recursive inquiry central to RCA, it poses and addresses several questions. For example, are voluntary compliance and a “covenant of trust” through a voluntary memorandum of understanding sufficient to achieve infected individuals' cooperation? Are U.S. and global health communities prepared for outbreaks of influenza or acts of bioterrorism? Julie Gerberding, CDC Director during the Speaker incident, issued a public statement acknowledging that the decision to issue a federal order of isolation under the PHSA was unusual, and said the CDC was aware of the need to balance individual liberties with protecting public health.14 Was the federally mandated isolation order in this case necessary or desirable, and was the order's timing and scope appropriate and reasonable? Should the CDC, Fulton County and/or Georgia state health departments have acted sooner and taken steps to prevent the case's international ramifications? Which level of government should have spearheaded the endeavor? Did the patient act responsibly and ethically? The root causes of this international public health fiasco occupy a number of different levels and pertain to many aspects of law, ethics, governance, and the infectious agent itself.
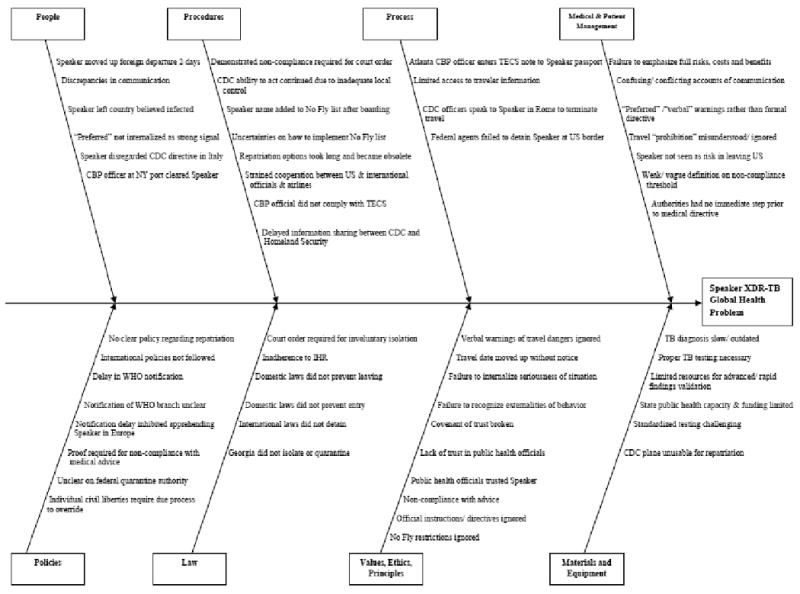
The sections that follow take up the main four steps of RCA (problem definition, data collection, identification of possible causal factors and recommendation of potential solutions). In RCA, events and systems interrelate, so I seek to trace the events in the Speaker case to discover where and how the problem commenced and how events and conditions in specific areas (e.g., XDR-TB as a source of exposure, domestic public health law, international health law, quarantine, isolation, civil and political rights and voluntary compliance) affect actions in others. I begin this analysis with what RCA analysts might call physical or material causes — in this instance, the nature of XDR-TB itself as a source of exposure. I then move to organizational or system-wide causes, here with a focus on domestic and international laws and policies that guide individuals in making decisions on actions. I conclude with human causes focused at the individual level, examining specifically the notion of voluntary compliance. An RCA method called an Ishikawa or fishbone diagram (Figure 1) breaks down these factors in greater detail to assess their potential contribution to the global health problem. The final section offers recommendations for potential solutions to prevent recurrence.
Figure 1. Ishikawa Diagram of XDR-TB Global Health Problem.
Extensively Drug-Resistant Tuberculosis as a Source of Exposure
An important question in incidences involving infectious agents is the probability of exposure to those in the general population, especially groups with immune system impairments. In justifying the isolation order, Dr. Gerberding indicated that the “precocious organism [XDR-TB] is so potentially serious and could cause such serious harm to people, especially those that have other medical conditions that would reduce their immunity, we felt that it was our responsibility to err on the side of abundant caution and issue the isolation order to assure that we were doing everything possible to protect people's health.”15 While the CDC and other health authorities cannot and do not require or compel testing for individuals who may have been exposed, health authorities do recommend that individuals in close proximity to an infected patient and with a compromised immune system receive the baseline skin test and the follow-up skin test for incubating TB infection.16 Moreover, some individuals have special TB risk because of their own medical history and are especially vulnerable. XDR-TB is particularly problematic for individuals with HIV or other conditions weakening the immune system, who are at higher risk of both TB infection upon exposure and of death upon contracting TB.17 Identifying these individuals, however, raises concerns about medical privacy and patient confidentiality.
XDR-TB is resistant both to two of the main first-line drugs (isoniazid and rifampicin) and to at least three out of six classes of available second-line drugs (fluoroquinolones and injectable agents, such as amikacin, kanamycin, and capreomycin). It most often develops when first- or second-line TB drugs are misused or mismanaged (when patients do not take the full course of treatment or doctors prescribe the wrong dosage, duration or drugs for treatment) and thus become ineffective.18 Treating XDR-TB successfully is difficult, because it requires finding an effective combination of four or more drugs.19 Currently no effective third-line drugs are available.20 Pharmaceutical companies have neglected the development of a vaccine or better TB drugs because the market is not profitable enough to justify research and development investments.21 The international community thus has only decades-old treatment options for contemporary strains of a contagious disease that can spread worldwide in a matter of hours. XDR-TB spreads like regular TB: by sneezing, coughing or talking, which propel bacteria into the air.22 Confined places like planes, where ventilation is limited even though many airlines use HEPA filters to recycle and clean the air, amplify the risk of transmission. The stage of the disease also affects the risk: latent disease is not contagious whereas active disease (including smear-negative active TB) is.23 The Speaker case underscores all persons' vulnerability in the face of uneven TB treatment quality and uncertain adherence to treatment protocols anywhere in the world. It makes the need for further investments and efforts in preventing and treating MDR-TB and XDR-TB inarguably clear. The shared health governance model put forth below offers guidelines for providers and patients to enhance the voluntary treatment adherence component of TB management.
The particulars of the Speaker case prompt scrutiny for root causes, starting with the medical circumstances surrounding it. The TB organism itself – its resistance to treatment and its deadly potential – is a serious issue. XDR-TB is a highly unusual and rare organism, extremely difficult to treat. Most XDR-TB victims do not survive. The deadliness of XDR-TB was a major factor behind the CDC's federal isolation order, to limit the potential exposure of others to this harm. The question arises as to the implications of the potential fatality of XDR-TB for the “standard of proof…by clear, cogent and convincing evidence” that U.S. courts have found to be constitutionally required to justify involuntary isolation.24 In the Speaker case, the patient did not appear to be highly infectious or contagious: he had felt and continued to feel well. He was asymptomatic, and he continued to be smear-negative for acid-fast bacilli, such that the medical evidence of the tuberculosis bacteria was uncertain. The low infectiousness of his case suggests that the transmission potential was low, although it was not zero; evidence indicates that roughly 17 percent of all TB cases are caused by exposure to smear-negative individuals.25 Moreover, after he fled the country, Mr. Speaker's test results indicated active TB, which is contagious, especially in close quarters such as airplanes. Another question is why a local, state or federal process was not in place to focus on discussion and deliberation of preliminary results while obtaining clear and convincing medical advice. Finally, Mr. Speaker himself illustrates how failure to address XDR-TB in one part of the world can inflate to a global problem. Mr. Speaker carried XDR-TB internationally, likely acquiring it overseas in a country in which poor living and health system conditions may have contributed to its prevalence.26 The potential of acquiring and spreading infectious agents thus poses particularly thorny problems world-wide, and we need a standardized process for addressing them.
Domestic Public Health Law
There are a number of laws that bear on effective public health strategies to contain, treat, and prevent the further spread of XDR-TB. The history of U.S. public health law points to the local and state levels as primarily responsible for the public's health.27 The “police power” of the state provides state governments with the authority to enact laws and promote regulations to secure the health, safety, and welfare of its citizens.28 Legal authority at the state level includes disease reporting and TB treatment. At the federal level, the CDC's quarantine authority stems from Title 42 of the U. S. Code Section 264 (Section 361 of the PHSA), which gives the Surgeon General, who acts with approval from the Secretary of Health and Human Services (HHS), responsibility for preventing “the introduction, transmission, and spread of communicable diseases from foreign countries into the United States and within the United States and its territories/possessions.”29 Regulations found at 42 CFR Parts 70 and 71 provide implementation powers. “Under its delegated authority, the CDC is empowered to” detain, medically examine and treat, isolate, quarantine, and/or “conditionally release individuals reasonably believed to be” infected with a communicable disease.30
An Executive Order of the President is required under PHSA procedures to specify the list of diseases for which quarantine is authorized. Executive Order 13295 provides the HHS with “clear legal authority” to isolate an individual to prevent that person from infecting others if that person “pose[s] a threat to public health and refuse[s] to cooperate with a voluntary request.”31 Specifically, the revised Executive Order of the President in 2003 states:
Section 1. Based upon the recommendation of the Secretary of Health and Human Services (the “Secretary”), in consultation with the Surgeon General, and for the purpose of specifying certain communicable diseases for regulations providing for the apprehension, detention, or conditional release of individuals to prevent the introduction, transmission, or spread of suspected communicable diseases, the following communicable diseases are hereby specified pursuant to section 361(b) of the Public Health Service Act:
Cholera; Diphtheria; infectious Tuberculosis; Plague; Smallpox; Yellow Fever; and Viral Hemorrhagic Fevers (Lassa, Marburg, Ebola, Crimean-Congo, South American, and others not yet isolated or named).
Severe Acute Respiratory Syndrome (SARS), which is a disease associated with fever and signs and symptoms of pneumonia or other respiratory illness, is transmitted from person to person predominantly by the aerosolized or droplet route, and, if spread in the population, would have severe public health consequences.
Sec. 2. The Secretary, in the Secretary's discretion, shall determine whether a particular condition constitutes a communicable disease of the type specified in section 1 of this order.32
In a public statement, the CDC justified the federal isolation order on the grounds that “after the patient had left the jurisdiction,” the TB organism was identified as extensively drug resistant. A federal order of isolation was executed to protect the public. The order required isolating the patient until the designated public health official decided that he was no longer infectious.33
Under PHSA authority, the CDC executed the federal isolation order in sequential stages. The CDC first made contact with Mr. Speaker when he was in Rome, just after learning that he had XDR-TB. The man immediately fled Rome and, against CDC directive, took a commercial flight from Prague to Montreal and drove by car from Montreal to the U.S. Once he had returned to the U.S., Dr. Martin Cetron, director of CDC's Division on Global Migration and Quarantine (part of CDC's National Center for Preparedness, Detection, and Control of Infectious Diseases) asked Speaker to go directly to a New York City isolation facility for evaluation. Mr. Speaker received safety instructions and voluntarily drove himself to the facility. There he was admitted, and a 72-hour provisional quarantine order was implemented while assessments took place. The CDC then used a CDC plane to “assure[] the safe transport for [his] return to Atlanta”.34 On arrival in Atlanta, the man was issued a federal isolation order “to cover the period of time for [the CDC] to hand over the jurisdiction and public health management of this case to the state and local authorities in Fulton County in the State of Georgia where he is a resident.”35 While the quarantine authorities do not obligate the CDC or other health authorities to use government resources to transport patients in government aircraft, doing so was deemed appropriate because the patient could not safely fly on a commercial plane and needed to return to Georgia.
The international dimension of this case might have further affected the U.S. response. A main reason for the federal – rather than county- or state-level – order was that federal statutes address international importation and interstate spread of infectious agents. The patient's international and interstate travel made the case one of international and federal jurisdiction. These features of the case provided justification for federal jurisdiction, governance, and action.
International Health Law: World Health Organization's International Health Regulations
The international scope of this case has multiple dimensions. The first is that the man traveled internationally in multiple countries, bringing into the decision-making process public health officials in those countries and beyond. Second, the case had potentially widespread repercussions in an increasingly globalized world, in which a contagious disease can spread worldwide in a matter of hours. Indeed, Mr. Speaker is believed to have acquired XDR-TB during previous international travel.
Just two years before this episode, in May 2005, the World Health Organization revised the IHR to provide an international framework for addressing contagion in a rapidly integrating global economy. The World Health Assembly adopted the revisions. The IHR focuses particularly on reporting and responding to diseases of international importance. Numerous aspects of the new IHR pertain to this case. First, the notification obligations in the new IHR's Article 6 require that “each State Party shall notify WHO … within 24 hours of assessment of public health information, of all events which may constitute a public health emergency of international concern within its territory in accordance with the decision instrument.”36
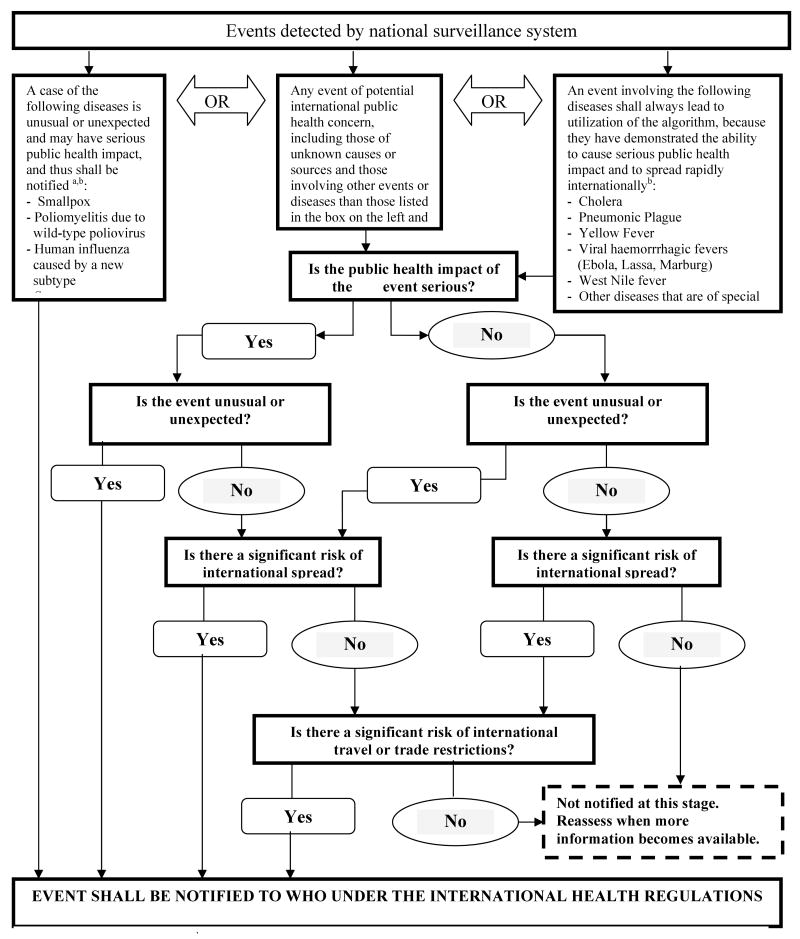
Second, the “decision instrument” (Annex 2, revised IHR, Figure 2) indicates that “any event of potential international public health concern” whereby the “public health impact of the event [is] serious” and “the event [is] unusual or unexpected” requires that the “event shall be notified to WHO under the international health regulations.”37 The Speaker case, according to the CDC, fit these criteria.
Figure 2. Decision Instrument for the Assessment and Notification of Events that May Constitute a Public Health Emergency of International Concern.
a As per WHO case definitions b The disease list shall be used only for the purpose of these Regulations
* Figure 2 taken directly from World Health Assembly Resolution WHA58.3, Revision of the International Health Regulations, Annex 2, p.50.
Third, Articles 7 and 8 stipulate “information-sharing during unexpected or unusual public health events” and “consultation.” The CDC has emphasized its collaboration with U.S. state and local health departments, foreign Ministries of Health, the airline industry, and the World Health Organization regarding appropriate notification and follow-up with individuals at risk of XDR-TB exposure. Despite these statements, accounts from officials in Canada, Greece, and Italy indicate that they did not receive information from the CDC about Mr. Speaker's case in time to take action, and Italian officials assert that they contacted the U.S. about the case and not vice-versa, contrary to IHR requirements.38 Findings from a report of the Committee on Homeland Security confirm CDC's delay in notifying WHO.39
Fourth, special provisions for travelers laid out in Articles 30, 31, and 32 in the IHR's Chapter III applied to the Speaker case, and the CDC sought to adhere to them. Mr. Speaker did not heed the CDC's recommendations, however, raising concerns about individual compliance and the CDC's inability to prevent his extensive international travel.
Fifth, the new IHR (Article 3.1) calls for implementation of the regulations to be “with full respect for the dignity, human rights and fundamental freedoms of persons.” Additionally, with regard to treatment of travelers, Article 32 stipulates the provision of arrangements and accommodations for “travelers who are quarantined, isolated or subject to medical examinations or other procedures for public health purposes,” a provision that would have applied to CDC's directives to Mr. Speaker in Italy and elsewhere.40
Sixth, the stronger declaration and recommendation powers given to WHO in IHR Articles 10-13 put pressure on nations to err on the side of notification, because WHO can step in and declare a public health emergency of international concern. According to the decision instrument (Figure 2), the U.S. XDR-TB case would likely have been declared such an emergency, possibly pressuring the U.S. to act when it otherwise might not have done so under the old IHR system. IHR Part II Articles 5 and 13 charge each state party to “develop, strengthen and maintain … the capacity to detect, assess, notify and report events” and to “develop, strengthen and maintain … the capacity to respond promptly and effectively to public health risks and public health emergencies of international concern.”41 As noted above, at both the U.S. federal and state levels, public health powers are broad and strong enough to augment and fulfill IHR Articles 5 and 13. Indeed, the U.S. would be expected to have one of the most effective public health infrastructures for the surveillance and treatment of tuberculosis worldwide. Yet despite global and domestic law, the state-level public health system emerges as a key root cause for failing to coordinate surveillance, reporting, intervention, and training of health care personnel effectively to address this infectious agent at its origins and prevent the global-level debacle that ensued. Specific recommendations regarding this state-level failure are discussed in the final section.
Seventh, beyond the IHR provisions, WHO guidelines state that individuals with MDR-TB “must not travel by public air transportation” until evidence confirms non-communicability, and they call for initiating an airline contact tracing or investigation when an individual is believed to be potentially infectious during airline travel.42 WHO TB and airline travel guidelines recommend testing for TB infection and medical care for individuals who could have been exposed. Consistent with these WHO guidelines, CDC recommended that passengers seated near Mr. Speaker be contacted by health officials in their responsible country or state and undergo testing. Before travel, however, Fulton County officials failed to apply adequately the WHO no-fly restrictions relevant to Mr. Speaker, trying instead to appeal to voluntary restrictions on travel, treatment, and isolation if necessary. Involuntary confinement is a measure of last resort. A key root cause is that Mr. Speaker did not appear to have an opportunity through a standardized process to make a fully informed and reasoned decision about his own choices. A reform procedure to provide a standardized process in the future is among the recommendations below.
Quarantine, Isolation and Civil and Political Rights
The history of quarantine dates to the 14th century, when ships – likely carrying individuals with the plague – were required to wait just outside Venetian ports for over a month in attempts to prevent the importation of infectious disease. In America, outbreaks of infectious disease like yellow fever motivated Congress in 1878 to pass federal quarantine legislation, to supplement existing state and local governments' quarantine regulations. With the turn of the century the federal government took over the bulk of state and local quarantine administration; in 1921 the system was nationalized.43 In 1944, the PHSA emphatically asserted the federal government's quarantine authority, giving the U.S. Public Health Service “the responsibility for preventing the introduction, transmission, and spread of communicable diseases from foreign countries into the United States.”44 In 1967, the CDC acquired quarantine authority.
To prevent the importation of diseases, the CDC established a surveillance system for monitoring epidemics abroad as well as inspection methods for overseeing international traffic. The CDC's Division of Global Migration and Quarantine has the power to “detain, medically examine, or conditionally release individuals and wildlife suspected of carrying a communicable disease.”45 This delegated authority makes it an extremely powerful state agent.
A state's authority to compel isolation and quarantine within its borders derives from its inherent police power. Public health emergencies highlight a trade-off between the protection of civil and political rights on the one hand, and the protection of public health on the other. The trade-off has been especially prominent in contemporary debates about public health preparedness.46 Despite the complicated nature of the interplay among international, federal, state, and county laws and regulations, and the nature and justification of the trade-offs between civil liberties and public health, the case of active TB seems straightforward. Some, for example, have argued that “a person with active, contagious tuberculosis who refuses to take medication while insisting on congregating with others” does justify the government's interference with individual civil rights.47 The problem with the Speaker case and a root cause in its analysis is that there was not “clear and convincing” evidence that it was a case of active TB, and the degree of contagion was neither well-established nor effectively communicated before international travel had commenced.
A counterfactual case illuminates root causes and potential corrective action. In the counterfactual, even if the medical evidence was not yet “clear and convincing” in pointing to active TB, the considerable threat of the disease and the potential of its international spread would warrant erring on the side of protective measures — a formal process for superseding his free choice to protect the public's health. Mr. Speaker should never have chosen to travel internationally in the first place. A standardized procedure should have been in place both to persuade him of the wisdom of the choice to forgo travel in hopes that he would act wisely and, failing that, to deny his right to travel. Neither Fulton County nor Georgia state officials had such a procedure at their disposal. The state of Georgia and local authorities did not have the power to act, nor did Mr. Speaker have the opportunity to respond: the only mechanism at the governments' disposal was obtaining a court order for detention if and only if Mr. Speaker acted against medical advice (i.e, if he traveled internationally, at which point a court order is too late). This early and cautious formalized process would have prevented the international commotion that ensued. Fulton County and Georgia public health officials should have led this effort, but in fact the legal and regulatory design placed them and the Fulton County doctor in a “Catch-22” situation, with no effective recourse.48 The last section below discusses a new standardized procedure as corrective action.
Voluntary Compliance
In a public statement, Dr. Gerberding noted that the patient failed to adhere to a “covenant of trust,” an implicit reliance on the consideration and decency of infected patients to follow medical advice and not to cause harm to others. The CDC states, “normally, when someone has tuberculosis, [he or she is influenced] through a covenant of trust so that they don't put themselves in situations where they could potentially expose others. In this case, the patient had compelling personal reasons for traveling and made the decision to go ahead and meet those personal responsibilities.”49 Dr. Gerberding, indicating that voluntary compliance is the first line of defense in tuberculosis cases, said, “this is a situation that comes up often where we have people with tuberculosis or other communicable diseases and we do not issue isolation orders under our quarantine statute, because we recognize that we have a high success record using voluntary means of information and advice.”50 Voluntary measures failed in Mr. Speaker's case, and the CDC later decided to issue the isolation order.
The case reveals a number of failings, representing root causes of this significant global health problem. First, Fulton County and Georgia public health departments failed to take the lead as primary actors, to identify the man's infection, report it, treat it, and then take preventive efforts to avoid domestic and international contagion. Second, county and state health officials failed to manage negotiations with Mr. Speaker and his family around the so-called “covenant of trust,” which relies on individuals to make ethical decisions to protect public health. That covenant proved insufficient in this case. How county and state public health officials could have more successfully managed the man's reluctance to cooperate, improved his voluntary cooperation, and solidified the “covenant of trust” is an important question. Below I put forth recommendations to make the “covenant of trust” work much more effectively. Third, had it been clear that Mr. Speaker would refuse to cooperate voluntarily, the isolation order should have been executed at the state level to prevent him from traveling in the first place, as opposed to federal execution after the fact. As one legal scholar notes, “persons suspected of having a contagious disease should have the option of being examined by physicians of their own choice and, if isolation is necessary, of being isolated in their own homes.”51 But state and local authorities had their hands tied since they could not get a court order to detain Mr. Speaker until he acted against medical advice (i.e., until he left the country). Thus, the root causes of this breakdown appear in the unworkable design of the regulations, not necessarily in implementation within that governance framework.
The CDC took the position that there are different methods for reducing the infected patient's exposure to others and for moving the patient into medical treatment in order to prevent contagion. Dr. Gerberding states in this case that, “if it was deemed necessary to move the patient for medical treatment or desirable, we have means of orchestrating that, either under the federal isolation order or through a voluntary memorandum of understanding.”52 Indeed, Mr. Speaker remained under federal isolation until, as Dr. Cetron noted, the order was “either rescinded and the responsibility is transferred over to the local jurisdiction or until determined by the Director that he is no longer a public health threat. Or until the re-negotiation of that covenant of public trust can be established in order to assure voluntary compliance.”53
Conclusions and Recommendations
To my knowledge, this is the first root cause analysis of a global health problem generally or a global infectious disease threat specifically. One would be hard pressed to find a public health case that so clearly illuminates the interplay among international, federal, state, county, and individual levels. International health law – as seen, for example, through the lens of the revised IHR – has primary responsibility for preventing the spread of communicable diseases across national boundaries. Domestic public health law vests authority in the national government (the HHS and CDC) for issuing federal isolation orders; the federal government has residual authority under the U.S. Constitution's Commerce Clause to prevent the spread of disease between states and from foreign countries.54 State and local jurisdictions have primary responsibility for isolation and quarantine within their borders. This case also implicated the U.S. Department of Homeland Security and U.S. Customs and Border Protection (CBP), which had the authority to hold “ill persons” at the U.S. border,55 but which allowed Mr. Speaker to pass through despite his having been flagged in the Treasury Enforcement Communications System (TECS) as someone to be detained. At the individual level, every person has the responsibility to act ethically in the case of infection, to weigh the costs and benefits of his actions for himself and his fellow citizens.
Elsewhere, I have argued that individuals have a responsibility to internalize public norms of ethical conduct, to respect the dignity and health of all individuals, not just themselves.56 Even though there were no “legal orders” preventing his travel and he broke no laws, Mr. Speaker's decisions raise questions about whether he placed his personal desires above others' health, and whether he had sufficient knowledge of his infection to make a rational, informed decision about rejecting the covenant of public trust.57 Did Mr. Speaker “do the right thing”? Did he have the information he needed to choose the right thing?
The conduct of county and state public health officials raises concerns about their effectiveness in assessing, communicating, and eliciting voluntary compliance from citizens. Short of creating a police state at the national and global level with legal authority to track the health status and whereabouts of every global citizen, effective strategies require individuals and their health care providers to devise plans of action that involve less restrictive alternatives to coerced confinement, but still protect the public's health and reduce the danger to others. Ethical commitments are therefore necessary at all levels – from the individual to the global – to move toward the end goal of preventing the spread of contagious disease.
The root causes of the Speaker case appear in the first links of the long chain of events leading up to the final denouement. Potential corrective actions should thus focus on the local level, both on strengthening the “covenant of trust” and on redesigning regulations. Voluntary compliance must play a central role, but as the Speaker case makes plain, we cannot rely on it alone. Failure to self-regulate can cause harm to others and significant costs to society. Nor can “voluntary compliance” be understood outside the context of the relationships that exist among patients, health providers and local health officials. As this case illustrates, informality offered by local health providers and government officials as part of the “covenant of trust” can lead to miscommunications, patient mismanagement, and failure to understand the legal repercussions of alternative courses of action. “Voluntary compliance” and the “covenant of trust” involving patients, health providers and government officials must be pursued in the context of a regulatory framework that explicitly permits legal action as a necessary next step in the event of non-compliance and breach of trust. Corrective actions must, therefore, focus specifically on the nexus between medical decision-making and individual civil liberties (in which the rights of individual patients are uppermost) on the one hand, and on the other hand, legal authority of governments and “exposed” victims' rights, with a focus on the interests of others and of society as a whole.
The current regulatory structure fails to integrate voluntary and ethical considerations with legal enforcement. The costs and benefits of patients' behavior must be thoroughly communicated to patients, who in turn must internalize them. These costs include ramifications of: (i) the government's authority to isolate, quarantine, seek and detain in domestic and international contexts and (ii) potential victims' rights to sue for damages under civil torts liability. The current structure presents a health capability failure; it failed to enhance the health functioning and health agency either of Mr. Speaker or of those he could have infected. This failure resulted in a colossal misappropriation of time, resources, and funds. The reputational consequences for Mr. Speaker, including loss of confidentiality and social sanctions, are also significant.
Broadening the regulatory framework to include both self-regulation and governmental and legal oversight in one integrated approach is essential. My view is that we should both improve regulatory design and deliberate with and educate the public about the costs, risks and benefits of health behaviors so that they can be fully and effectively internalized for individual voluntary action. As the Speaker case shows, the result of failing to fully communicate and inculcate this information was dire; Mr. Speaker made an unwise and regrettable choice. The premise here is that if Speaker had known ex ante of the state, federal and global authority to seek him out and detain him, the potential civil lawsuits by nearby travelers, and the damage to his reputation his actions would cause, even though there were still uncertainties about the type of TB he had, he would not have chosen to flee the U.S. and elude authorities in several countries. Mr. Speaker may not have had sufficient information in this case to make a reasoned decision, or perhaps he did not fully understand the consequences and implications of his actions.
Clear and standard rules and procedures for communication of the medical, ethical and legal issues at stake and effective education and deliberation about the costs, risks, and benefits of individual action are necessary. Policies must be in place to ensure that there is no miscommunication, misinformation, misrepresentation or misunderstanding by any party as events unfold. An international uniform standard for such regulations is required. Patients should be informed of and fully review with health providers and local health officials the costs, benefits and risks of their infection and their behavior for themselves and for society at large. A question-and-answer period should confirm that patients fully understand these personal and social implications and help internalize them. The full course of action for medical treatment, prevention and recovery should be discussed and agreed to. A plan should be developed for voluntary compliance with medical advice and isolation. A communication strategy should be formulated and agreed to for continual updates, review of progress and additional decision-making. A series of steps for reintegration following voluntary compliance and isolation should be discussed, and a plan for updating should be constructed. A clear line of authority and imposition of sanctions should be delineated in case the patient fails to comply voluntarily with medical advice and isolation. Patients should have the right to a representative to assist them through the entire process. Local authorities must comply with the guidelines; otherwise federal bodies should have the authority to intervene. In the U.S., the CDC's Division of Global Migration and Quarantine is the right agency for oversight at the federal level. This division would either use the existing structure or create a new office primarily for oversight of this process and for the review of local and state level cases. The review process should involve the sharing of information and findings at the international level to improve the process globally. This office should also set up a process for handling cases that cannot be dealt with at the local level, by establishing another procedure as a federal-level backup. In addition, federal oversight is necessary to establish required procedures for imposing isolation or quarantine involuntarily. New protocols are needed for medical and patient management, for the use of legal action when appropriate, and for improved coordination with international authorities.
Such a procedure would draw on the informed consent process found in clinical ethics – but with an alternative framework to enhance voluntariness for decisions affecting both the individual and society. This safeguard, one step ahead of applying for legal authority to restrict liberties through involuntary isolation, would serve both to respect individuals and to protect society. Elements of this process could come from informed consent models, such as standards for disclosure, written and signed forms of consent, and legal ramifications such as medical malpractice. The procedure must have clear and standardized requirements and entail a signed consent by the individuals and health and governmental officials involved. Figure 3 provides a rough sketch of such a process.
Figure 3. Handling Quarantinable* Communicable Diseases: A Process of Shared Health Governance.
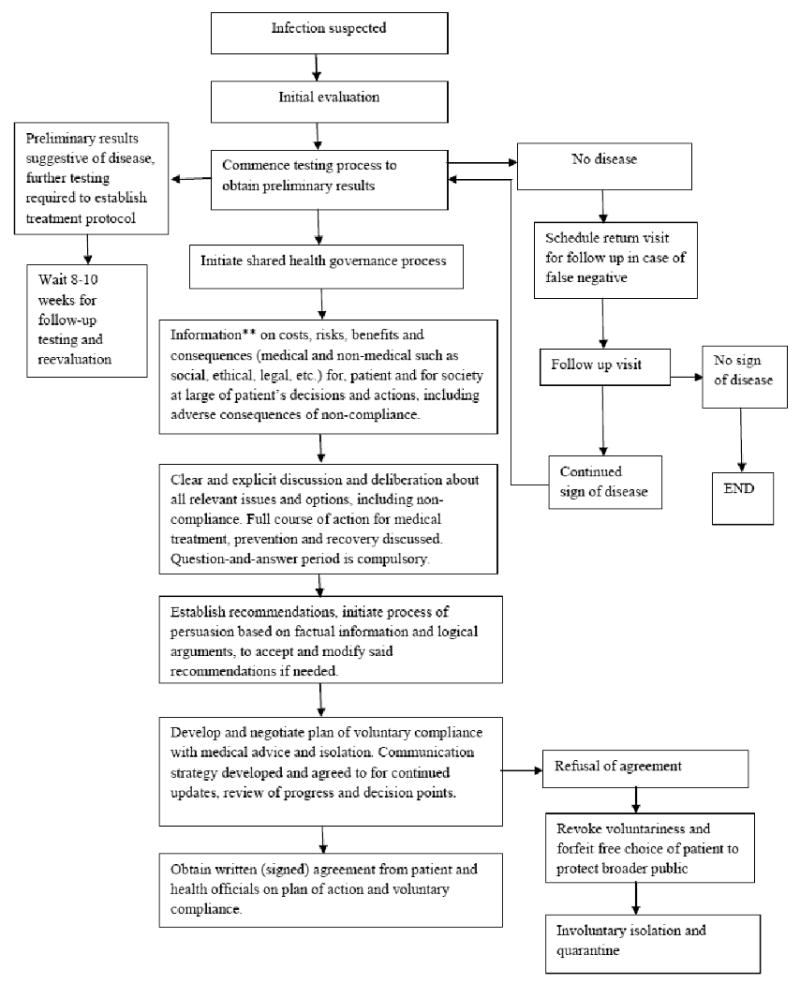
*Cholera, Diphtheria, infectious Tuberculosis, Plague, Smallpox, Yellow Fever, Viral Hemorrhagic Fever (Lassa, Marburg, Ebola, Crimean-Congo, South American, and others not yet isolated or heard), SARS or otherwise determine by IHR and US PHS Act.
**Information provided should meet ethical as well as legal standards of providing patents with relevant information to make informed choices; manipulation or misrepresentation is actionable by legal principles of negligence. International uniform standards provide guidance. misrepresentation is actionable by legal principles of negligence. International uniform standards for rules and procedures provide guidance.
The gap between voluntary compliance under a “covenant of trust” and full blown quarantine and isolation requires an additional procedure with clear and standardized rules and processes. This procedure might address the reluctance on the part of governments to implement isolation and quarantine authority by creating more compelling justifications for their use. Global standards regarding the rules and procedures of local management of such situations might also be necessary to reduce local variations that could undermine the global system. Improving this process may require recruiting psychologists and ethicists in efforts to build trust on both sides of this relationship. A systematic study of such rules and procedures to assess effectiveness and reduce unintended consequences is needed.
Investing in strengthening the role of voluntary compliance and trust, undergirded with the legal authority for involuntary restrictions, holds promise. The Speaker case illustrates that greater oversight and standardization in procedures early at the origins of infection detection and at the local level are essential. My view is that corrective actions at the earliest stage and at the most local level possible could significantly reduce the spread of infectious agents both within and among countries. In the Speaker case, local authorities were allowed too much latitude. Stronger and stricter rules at the levels of the patient, his health provider, and his local public health authority are necessary. A key reform is a new mandated standard procedure for examining, communicating, discussing, vetting and fully inculcating the medical, ethical, and legal issues and the costs, benefits, and risks to the patient and to society from an individual's contemplated actions. Indeed, global standards for patient management, communication, and implementation of isolation and quarantine at the local level may be required. Despite the need for global standards, oversight must continue to be centered on local and national authorities, with backup at the global level (through international standards of reporting), because local and national regulations are more likely to be enforceable than global standards and are closer to the point of disease origin.
In conclusion, future investments in minimizing the risks of global threats should be focused more locally, closer to the source, to obviate – to the extent possible – delayed responses to diseases that facilitate their spread. Mr. Speaker could have been stopped from traveling domestically or internationally; failure to halt him is a major root cause of this global incident. While global public health systems and cooperation are still required and must focus on better and faster information management, sharing, and response, improvements in local systems to stop epidemics at their origins are critical to effective disease containment in the future. The current focus on the global public health system of laws and governance is important and necessary, but it is not sufficient for the control of emerging global health threats.
Acknowledgments
Dr. Ruger is currently a member of the Ethics Subcommittee of the Advisory Committee to the Director of the U.S. Centers for Disease Control and Prevention (CDC). She would like to thank the participants in the Salzburg Seminar on Global Health Governance and Theodore W. Ruger for helpful discussions. This research was supported, in part, by the Open Society Institute of the Soros Foundation and the Whitney and Betty MacMillan Center for International and Area Studies. Dr. Ruger is supported in part by a Career Development Award from the U.S. National Institutes of Health (grant K01DA016358) and an Investigator Award from the Patrick and Catherine Weldon Donaghue Medical Research Foundation (grant DF06-112). She would also like to thank Nora Ng, Akriti Singh and Betsy Rogers for research and editing assistance.
References
- 1.Neel R, Gandhi, et al. Extensively Drug-Resistant Tuberculosis as a Cause of Death in Patients Co-Infected with Tuberculosis and HIV in a Rural Area of South Arica. The Lancet. 2006;36:8. 1575–80. doi: 10.1016/S0140-6736(06)69573-1. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Centers for Disease Control and Prevention. Flight Itinerary of U.S. Traveler with Extensively Drug-Resistant Tuberculosis (XDR TB) 2007 May 30; press release. Available at: http://web.archive.org/web/20080520155319/http://www.cdc.gov/tb/xdrtb/caseflighthistory.htm.
- 3.Schwartz John. Tangle of Conflicting Accounts in TB Patient's Odyssey. New York Times. 2007 June 2; Health section. Available at: http://travel.nytimes.com/2007/06/02/health/02tick.html?pagewanted=all.
- 4.Grady Denise. TB Patient Says Officials Are Trying to Blame Him to Cover Mistakes. New York Times. 2007 June 9; National section. Available at: http://www.nytimes.com/2007/06/09/us/09tb.html?pagewanted=all.
- 5.Schwartz . TB Patient's Odyssey. [Google Scholar]
- 6.Shah NS, et al. Extensively Drug-Resistant Tuberculosis – United States, 1993-2006. Morbidity and Mortality Weekly Report. 2007;56(11):250–3. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5611a3.htm. [PubMed]
- 7.Altman Lawrence K. TB Patient Has Surgery to Remove Part of Lung. New York Times. 2007 July 18; Health section. Available at: http://www.nytimes.com/2007/07/18/health/18tb.html.
- 8.Schwartz . TB Patient's Odyssey. [Google Scholar]
- 9.Altman Lawrence K, Palank Jacqueline. TB Patient Gives His Account to Congress. New York Times. 2007 June 7; National section. Available at: http://www.nytimes.com/2007/06/07/us/07tb.html.
- 10.Smith Richard D. Responding to Global Infectious Disease Outbreaks: Lessons from SARS on the Role of Risk Perception, Communication and Management. Social Science & Medicine. 2006;63:3113–23. doi: 10.1016/j.socscimed.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]; World Health Organization. Summary of Probable SARS Cases with Onset of Illness from 1 November 2002 to 31 July 2003. Available at: http://www.who.int/csr/sars/country/table2004_04_21/en/index.html.
- 11.Resolution WHA58.3, Revision of the International Health Regulations.World Health Assembly, Fifty-Eighth plenary meeting; May 23, 2005; [Google Scholar]
- 12.Executive Order 13375 of April 1, 2005: Amendment to Executive Order 13295 Relating to Certain Influenza Viruses and Quarantinable Communicable Diseases. Federal Register. 2005 April 5;70(64):17299. [Google Scholar]; McCullagh Declan. DHS Sets Guidelines for Possible Swine Flu Quarantines. CBSNews.com. 2009 April 28; Available at: http://www.cbsnews.com/blogs/2009/04/28/politics/politicalhotsheet/entry4975598.shtml.
- 13.Jones CW. 4×4 Concept: The General Theory of Unifying Dynamic Organizational Self-Regulation as Applied to System Safety. paper presented at the International System Safety Society Conference; Houston, TX. 1983. [Google Scholar]; Rasmussen J. Human Error and the Problem of Causality in Analysis of Accidents. Philosophical Transactions of the Royal Society of London, Series B, Biological Sciences. 1990;327:449–60. doi: 10.1098/rstb.1990.0088. [DOI] [PubMed] [Google Scholar]; Reason J. Human Error. New York: Cambridge University Press; 1990. [Google Scholar]; Root Cause Analysis. Available at: http://process.nasa.gov/documents/RootCauseAnalysis.pdf.; Wald Heidi, Shojania Kaveh G. Chapter 5: Root Cause Analysis. In: Shojania KG, Duncan BW, McDonald KM, et al., editors. Making Health Care Safer: A Critical Analysis of Patient Safety Practices, Evidence Report/Technology. Rockville, MD: Agency for Healthcare Research and Quality; 2001. Assessment No.43, AHRQ Publication No. 01-E058. Available at: http://archive.ahrq.gov/clinic/ptsafety/chap5.htm. [PMC free article] [PubMed] [Google Scholar]; Rzepnicki Tina L, Johnson Penny R. Examining Decision Errors in Child Protection: A New Application of Root Cause Analysis. Children and Youth Services Review. 2005;2:7. 393–407. [Google Scholar]
- 14.U.S. Centers for Disease Control and Prevention. Public Health Investigation Seeks People Who May Have Been Exposed to Extensively Drug Resistant Tuberculosis (XDR TB) Infected Person. (press briefing transcript, May 29, 2007, 2:00pm). Available at: http://www.cdc.gov/media/transcripts/2007/t070529.htm.
- 15.Ibid.
- 16.Ibid.
- 17.World Health Organization. TB/HIV Facts 2009. Available at: http://www.who.int/tb/challenges/hiv/factsheet_hivtb_2009.pdf.
- 18.World Health Organization. Frequently Asked Questions – XDR-TB. Available at: http://www.who.int/tb/challenges/xdr/faq_en.pdf.
- 19.Furin Jennifer. The Clinical Management of Drug-Resistant Tuberculosis: Treatment, Medscape. doi: 10.1097/MCP.0b013e3280f3c0b2. Available at: http://www.medscape.com/viewarticle/556083_5. [DOI] [PubMed]
- 20.Park Alice. Tuberculosis: An Ancient Disease Continues to Thrive. Time. 2008 October 2; Available at: http://www.time.com/time/health/article/0,8599,1846698,00.html.
- 21.Spigelman Melvin, Gillespie Stephen. Tuberculosis Drug Development Pipeline: Progress and Hope. The Lancet. 2006;36:7. 945–7. doi: 10.1016/S0140-6736(06)68388-8. [DOI] [PubMed] [Google Scholar]
- 22.World Health Organization. Frequently Asked Questions – XDR-TB. [Google Scholar]
- 23.Schwartz . TB Patient's Odyssey. [Google Scholar]; Ross Lisa, Meredith Goff. Latent Tuberculosis Infection and BCG Vaccination. Journal of Midwifery and Women's Health. 2005;50(4):344–7. doi: 10.1016/j.jmwh.2005.03.003. [DOI] [PubMed] [Google Scholar]; American Thoracic Society. New Test Quickly ID's Active Tuberculosis in Smear-Negative Patients. ScienceDaily. 2009 September 23; Available at: http://www.sciencedaily.com/releases/2009/09/090923102321.htm.
- 24.Green v. Edwards. 263 S. E. 2d 661. 1980;3 Available at: http://www.publichealthlaw.net/Reader/docs/Greene.pdf.; Annas George J. Control of Tuberculosis – The Law and the Public's Health. New England Journal of Medicine. 1993;328(8):585–8. doi: 10.1056/NEJM199302253280825. [DOI] [PubMed] [Google Scholar]
- 25.U.S. Centers for Diseae Control and Prevention. Public Health Investigation XDR-TB. [Google Scholar]
- 26.Grady . TB Patient. [Google Scholar]
- 27.Annas George J. Bioterrorism, Public Health, and Civil Liberties. New England Journal of Medicine. 2002;346(17):1337–42. doi: 10.1056/NEJM200204253461722. [DOI] [PubMed] [Google Scholar]
- 28.Annas . Bioterrorism Public Health, and Civil Liberties. [DOI] [PubMed] [Google Scholar]; Wing Kenneth R. The Law and the Public's Health. 5th. Chicago: Health Administration Press; 1999. pp. 23–5. [Google Scholar]
- 29.U.S. Centers for Disease Control and Prevention. Questions and Answers on the Executive Order Adding Potentially Pandemic Influenza Viruses to the List of Quarantinable Diseases. Available at: http://www.cdc.gov/quarantine/qa-executive-order-pandemic-list-quarantinable-diseases.html.
- 30.Ibid.
- 31.Ibid.
- 32.Executive Order 13295, Revised List of Quarantinable Communicable Diseases. 2003 April 4; Available at: http://www.fas.org/irp/offdocs/eo/eo-13295.htm.
- 33.U.S. Centers for Disease Control and Prevention. Public Health Investigation XDR-TB. [Google Scholar]
- 34.Ibid.
- 35.Ibid.
- 36.World Health Assembly. Revision of the International Health Regulations. p. 17. [Google Scholar]
- 37.Ibid., 50
- 38.Schwartz . TB Patient's Odyssey. [Google Scholar]
- 39.United States House of Representatives Committee on Homeland Security Majority Staff. The 2007 XDR-TB Incident: A Breakdown at the Intersection of Homeland Security and Public Health. 2007 September; 3. Available at: http://homeland.house.gov/SiteDocuments/tbreport.pdf.
- 40.World Health Assembly. Revision of the International Health Regulations. 15:30. [Google Scholar]
- 41.Ibid., 16, 20.
- 42.World Health Organization. 2nd. Geneva: World Health Organization; 2006. Tuberculosis and Air Travel: Guidelines for Prevention and Control; p. 15. Available at: http://whqlibdoc.who.int/hq/2006/WHO_HTM_TB_2006.363_eng.pdf. [PubMed] [Google Scholar]
- 43.U.S. Centers for Disease Control and Prevention. History of Quarantine. Available at: http://www.cdc.gov/quarantine/HistoryQuarantine.html.
- 44.Ibid.
- 45.Ibid.
- 46.Annas George J. Puppy Love: Bioterrorism, Civil Rights, and Public Health. Florida Law Review. 2003;55(5):1171–90. [PubMed] [Google Scholar]; Gostin Lawrence O. When Terrorism Threatens Health: How Far are Limitations on Personal and Economic Liberties Justified? Florida Law Review. 2003;55(5):1105–70. [PubMed] [Google Scholar]
- 47.Annas Puppy Love. :1179. [Google Scholar]
- 48.United States House of Representatives Committee on Homeland Security Majority Staff. The 2007 XDR-TB Incident. p. 8. [Google Scholar]
- 49.U.S. Centers for Disease Control and Prevention. Public Health Investigation XDR-TB. [Google Scholar]
- 50.Ibid.
- 51.Annas . Bioterrorism, Public Health, and Civil Liberties. p. 1340. [DOI] [PubMed] [Google Scholar]
- 52.U.S. Centers for Disease Control and Prevention. Public Health Investigation XDR-TB. [Google Scholar]
- 53.Ibid.
- 54.Annas Bioterrorism, Public Health, and Civil Liberties. :1337. doi: 10.1056/NEJM200204253461722. [DOI] [PubMed] [Google Scholar]
- 55.Memorandum of Understanding Between the Department of Health and Human Services and the Department of Homeland Security. 2005 October; Available at: http://www.aclu.org/pdfs/privacy/hhs_dhs_mou.pdf.
- 56.Ruger Jennifer Prah. Ethics and Governance of Global Health Inequalities. Journal of Epidemiology and Community Health. 2006;60(11):998–1003. doi: 10.1136/jech.2005.041947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ruger Jennifer Prah. Rethinking Equal Access: Agency, Quality, and Norms. Global Public Health. 2007;2(1):78–96. doi: 10.1080/17441690600911480. [DOI] [PubMed] [Google Scholar]