Abstract
Background
The role of renin-angiotensin inhibition in older systolic heart failure patients with chronic kidney disease remains unclear.
Methods
Of the 1665 patients, age ≥65 years, with systolic heart failure (ejection fraction <45%) and chronic kidney disease (estimated glomerular filtration rate <60 ml/min/1.73 m2), 1046 received angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Propensity scores for the receipts of these drugs, estimated for each of the 1665 patients, were used to assemble a matched cohort of 444 pairs of patients receiving and not receiving these drugs who were balanced on 56 baseline characteristics.
Results
During over 8 years of follow-up, all-cause mortality occurred in 75% and 79% of matched patients with chronic kidney disease receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, respectively (hazard ratio {HR}, 0.86; 95% confidence interval {CI}, 0.74–0.996; p=0.045). There was no significant association with heart failure hospitalization (HR, 0.86; 95% CI, 0.72–1.03; p=0.094). Similar mortality reduction (HR, 0.83; 95% CI, 0.70–1.00; p=0.046) occurred in a subgroup of matched patients with estimated glomerular filtration rate <45 ml/min/1.73 m2. Among 171 pairs of propensity-matched patients without chronic kidney disease, the use of these drugs was associated with significant reduction in all-cause mortality (HR, 0.72; 95% CI, 0.55–0.94; p=0.015) and heart failure hospitalization (HR, 0.71; 95% CI, 0.52–0.95; p=0.023).
Conclusions
Discharge prescription of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers was associated with a significant modest reduction in all-cause mortality in older systolic heart failure patients with chronic kidney disease including those with more advanced chronic kidney disease.
Keywords: systolic heart failure, chronic kidney disease, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers
Inhibition of the renin-angiotensin system using angiotensin-converting enzyme inhibitors or angiotensin II type-1 receptor blockers improves outcomes in systolic heart failure.1,2 Chronic kidney disease is common in heart failure and is associated with poor outcomes.3,4 Although renin-angiotensin system suppression has been shown to improve outcomes in chronic kidney disease,5 systolic heart failure patients with chronic kidney disease are less likely to receive angiotensin-converting enzyme inhibitors or angiotensin receptor blockers.6 In addition to the elevation of serum creatinine after initiation of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, a key reason for the underuse of these drugs is the apparent lack of randomized clinical trials evidence of their benefit in systolic heart failure patients with chronic kidney disease.7–9 Systolic heart failure patients with renal dysfunction were often excluded from randomized clinical trials of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers and it is unlikely that the role of these drugs in these patients will be definitely resolved in randomized clinical trials due to ethical concerns of randomizing systolic heart failure patients, albeit with chronic kidney disease, to placebo, and lack of industry interests to sponsor such randomized clinical trials. However, when randomized clinical trials are unethical or impractical, propensity score matching can be used to design non-randomized studies to assemble balanced cohorts while remaining blinded to study outcomes.10–13 Therefore, the objective of the current study is to examine the association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with outcomes in a propensity-matched balanced cohort of systolic heart failure patients with chronic kidney disease.
Methods
Data source and study patients
We used the Alabama Heart Failure Project data for the current study, the details of which have been described previously.14 Briefly, medical records of fee-for-service Medicare beneficiaries discharged with a principle discharge diagnosis of heart failure from 106 Alabama hospitals between July 1, 1998 and October 31, 2001 were identified.14,15 A diagnosis of heart failure was based on the International Classification of Diseases, 9th Revision, Clinical Modification, codes for heart failure. Copies of the 9649 charts were abstracted by trained technicians who directly entered data into a computer database. The 9649 hospitalizations occurred in 8555 unique patients. For patients with multiple hospitalizations, charts from the first hospitalization were used.
Of the 8555 patients, 8049 were discharged alive, of whom 7058 (88%) were 65 years of age or older and of which, 2608 (37%) had left ventricular ejection fraction less than 45%. Of these, 2573 patients had data on baseline (admission, 2557 and in-hospital, 16) serum creatinine, of whom 1665 had chronic kidney disease, defined as estimated glomerular filtration rate <60 ml/min/1.73 m2 and 908 had no chronic kidney disease.16 Extensive data on baseline demographics, medical history including use of medications, hospital course, discharge disposition including medications, and physician specialty were collected.
Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use
Of the 1665 systolic heart failure patients with chronic kidney disease, 1046 (63%) were prescribed angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Of these, 83% (866/1046) received angiotensin-converting enzyme inhibitors, and 23% (180/799) of those not receiving angiotensin-converting enzyme inhibitors, received angiotensin receptor blockers. Seventeen patients received both drugs. Of the 908 systolic heart failure patients without chronic kidney disease, 693 (76%) received angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Of these, 89% (619/693) received angiotensin-converting enzyme inhibitors, and 26% (74/289) of those not receiving angiotensin-converting enzyme inhibitors received angiotensin receptor blockers. Considering the benefit of higher doses of angiotensin-converting enzyme inhibitors in heart failure,17 we categorized patients into receiving below-target or (at or above) target doses of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, using guideline recommendations based on doses used in large randomized clinical trials.18
Mortality and hospitalization
The primary outcome of the current analysis was all-cause mortality through to April 2, 2007. Secondary outcomes included all-cause and heart failure hospitalizations. Data on outcomes and time to events were obtained from the Centers for Medicare and Medicaid Services Denominator File, Medicare Provider Analysis and Review File and Inpatient Standard Analytical File.
Assembly of a balanced cohort
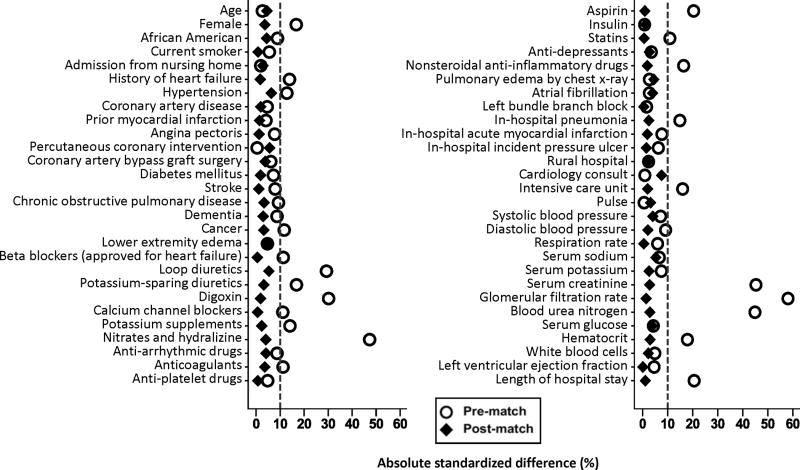
Because of the imbalances in baseline characteristics between patients receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (Table 1 and Figure 1), we used propensity scores to assemble a cohort in which those receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers would be well-balanced on all measured baseline covariates.10–13 We began by estimating propensity scores or probability of receiving discharge prescription of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for each of the 1665 systolic heart failure patients with chronic kidney disease given that patient’s measured baseline characteristics.19 We used a non-parsimonious multivariable logistic regression model in which receipt of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers was the dependent variable, and 56 baseline characteristics displayed in Figure 1 were used as covariates.20–22
Table 1.
Baseline patient characteristics of older systolic heart failure patients with chronic kidney disease by discharge prescription of angiotensin-converting enzyme inhibitor (ACEIs) or angiotensin receptor blockers (ARBs), before and after propensity score matching
| n (%) or mean (±SD) | Before propensity score matching Use of ACEIs or ARBs | After propensity score matching Use of ACEIs or ARBs | ||||
|---|---|---|---|---|---|---|
| No (n=619) | Yes (n=1046) | P value | No (n=444) | Yes (n=444) | P value | |
| Age (years) | 78 (±7) | 78 (±7) | 0.610 | 78 (±8) | 78 (±7) | 0.509 |
| Female | 283 (46) | 565 (54) | 0.001 | 221 (50) | 229 (52) | 0.639 |
| African American | 142 (23) | 202 (19) | 0.077 | 99 (22) | 91 (21) | 0.565 |
| Current smoker | 58 (9) | 82 (8) | 0.277 | 37 (8) | 36 (8) | 1.000 |
| Nursing home residents | 34 (6) | 53 (5) | 0.706 | 30 (7) | 27 (6) | 0.791 |
| Left ventricular ejection fraction (%) | 29 (±9) | 28 (±9) | 0.367 | 29 (±9) | 29 (±9) | 0.985 |
| Past medical history | ||||||
| Prior heart failure | 513 (83) | 809 (77) | 0.007 | 356 (80) | 353 (80) | 0.868 |
| Hypertension | 416 (67) | 764 (73) | 0.011 | 301 (68) | 314 (71) | 0.375 |
| Coronary artery disease | 431 (70) | 706 (68) | 0.366 | 306 (69) | 302 (68) | 0.835 |
| Myocardial infarction | 215 (35) | 343 (33) | 0.417 | 150 (34) | 153 (35) | 0.889 |
| Angina pectoris | 103 (17) | 145 (14) | 0.124 | 68 (15) | 70 (16) | 0.925 |
| Percutaneous coronary intervention | 98 (16) | 167 (16) | 0.943 | 73 (16) | 64 (14) | 0.460 |
| Coronary artery bypass graft | 201 (33) | 370 (35) | 0.228 | 149 (34) | 141 (32) | 0.629 |
| Left bundle branch block | 138 (22) | 240 (23) | 0.759 | 96 (22) | 97 (22) | 1.000 |
| Diabetes mellitus | 286 (46) | 446 (43) | 0.157 | 192 (43) | 196 (44) | 0.831 |
| Atrial fibrillation | 173 (28) | 305 (29) | 0.598 | 129 (29) | 121 (27) | 0.602 |
| Stroke | 145 (23) | 211 (20) | 0.118 | 103 (23) | 101 (23) | 0.937 |
| Chronic obstructive pulmonary disease | 220 (36) | 326 (31) | 0.066 | 148 (33) | 155 (35) | 0.661 |
| Dementia | 68 (11) | 88 (8) | 0.082 | 52 (12) | 48 (11) | 0.744 |
| Cancer | 10 (2) | 36 (3) | 0.028 | 10 (2) | 8 (2) | 0.815 |
| Clinical findings | ||||||
| Pulse (beats per minute) | 92 (±24) | 91 (±23) | 0.902 | 92 (±25) | 93 (±23) | 0.628 |
| Systolic blood pressure (mmHg) | 142 (±34) | 145 (±31) | 0.152 | 143 (±34) | 145 (±32) | 0.551 |
| Diastolic blood pressure (mmHg) | 78 (±20) | 79 (±18) | 0.067 | 79 (±20) | 79 (±18) | 0.762 |
| Respiration (breaths per minute) | 24 (±6) | 24 (±7) | 0.239 | 24 (±6) | 24 (±6) | 0.938 |
| Peripheral edema | 429 (69) | 702 (67) | 0.354 | 297 (67) | 307 (69) | 0.523 |
| Pulmonary edema by chest x-ray | 452 (73) | 751 (72) | 0.590 | 320 (72) | 311 (70) | 0.554 |
| Tests and procedures | ||||||
| Serum sodium (mEq/L) | 138 (±5) | 139 (±5) | 0.185 | 138 (±5) | 139 (±5) | 0.423 |
| Serum potassium (mEq/L) | 4.4 (±0.7) | 4.4 (±0.7) | 0.136 | 4.4 (±0.7) | 4.4 (±0.7) | 0.702 |
| Serum creatinine (mEq/L) | 2.3 (±1.4) | 1.7 (±1.0) | <0.001 | 2.0 (±1.1) | 2.0 (±1.3) | 0.652 |
| Estimated glomerular filtration rate (ml/min/1.73m2) | 35 (±14) | 42 (±12) | <0.001 | 38 (±13) | 37 (±13) | 0.800 |
| Blood urea nitrogen (mg/dL) | 40 (±22) | 31 (±16) | <0.001 | 36 (±19) | 36 (±20) | 0.631 |
| Serum glucose (mg/dL) | 153 (±70) | 156 (±72) | 0.394 | 153 (±72) | 151 (±68) | 0.546 |
| Hematocrit (%) | 36 (±6) | 37 (±6) | <0.001 | 37 (±6) | 37 (±6) | 0.647 |
| White blood cell (103/μL) | 10 (±8) | 9 (±6) | 0.321 | 9 (±5) | 9 (±7) | 0.739 |
| Hospital and care characteristics | ||||||
| Pneumonia | 196 (32) | 261 (25) | 0.003 | 119 (27) | 124 (28) | 0.765 |
| Acute myocardial infarction | 44 (7) | 55 (5) | 0.123 | 29 (7) | 27 (6) | 0.888 |
| Pressures ulcer | 66 (11) | 92 (9) | 0.209 | 44 (10) | 46 (10) | 0.911 |
| Rural hospital | 143 (23) | 231 (22) | 0.631 | 106 (24) | 110 (25) | 0.818 |
| Cardiology consult | 424 (69) | 712 (68) | 0.856 | 302 (68) | 286 (64) | 0.291 |
| Intensive care unit | 44 (7) | 37 (4) | 0.001 | 24 (5) | 26 (6) | 0.883 |
| Length of stay (days) | 8 (±5) | 7 (±6) | <0.001 | 7.5 (±4.5) | 7.4 (±7.0) | 0.864 |
| Discharge medications | ||||||
| Beta blockers (heart failure) | 148 (24) | 302 (29) | 0.028 | 110 (25) | 109 (25) | 1.000 |
| Loop diuretics | 483 (78) | 929 (89) | <0.001 | 368 (83) | 359 (81) | 0.444 |
| Potassium-sparing diuretics | 87 (14) | 213 (20) | 0.001 | 67 (15) | 62 (14) | 0.696 |
| Digoxin | 275 (44) | 621 (59) | <0.001 | 226 (51) | 222 (50) | 0.833 |
| Calcium channel blockers | 126 (20) | 168 (16) | 0.026 | 90 (20) | 91 (21) | 1.000 |
| Potassium supplements | 240 (39) | 478 (46) | 0.006 | 186 (42) | 191 (43) | 0.780 |
| Nitrates and hydralazine | 95 (15) | 24 (2) | <0.001 | 26 (6) | 22 (5) | 0.572 |
| Anti-arrhythmic drugs | 130 (21) | 184 (18) | 0.086 | 85 (19) | 78 (18) | 0.603 |
| Anti-coagulants | 150 (24) | 305 (29) | 0.029 | 117 (26) | 110 (25) | 0.639 |
| Anti-platelet drugs | 64 (10) | 124 (12) | 0.345 | 54 (12) | 55 (12) | 1.000 |
| Aspirin | 223 (36) | 481 (46) | <0.001 | 169 (38) | 167 (38) | 0.944 |
| Insulin | 94 (15) | 156 (15) | 0.881 | 70 (16) | 68 (15) | 0.923 |
| Statins | 86 (14) | 187 (18) | 0.034 | 67 (15) | 66 (15) | 1.000 |
| Anti-depressants | 122 (20) | 221 (21) | 0.489 | 94 (21) | 99 (22) | 0.750 |
| Non-steroidal anti-inflammatory drugs | 30 (5) | 94 (9) | 0.002 | 25 (6) | 27 (6) | 0.883 |
Figure 1.
Absolute standardized differences comparing 56 baseline characteristics between older systolic heart failure patients with chronic kidney disease receiving and not receiving discharge prescription of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, before and after propensity score matching
Using a greedy matching protocol, we were able to match 444 or 72% of the 619 patients not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with 444 patients receiving these drugs who had similar propensity scores.23–25 We then estimated absolute standardized differences of the 56 measured covariates for those receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and presented the percentages of pooled standard deviations as Love plots. 26–29 An absolute standardized difference of 0% indicates no residual bias and differences <10% are considered inconsequential.
We repeated the above process on 908 systolic heart failure patients without chronic kidney disease, matching 171 or 80% of the 215 patients not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with 171 patients receiving these drugs who had similar propensity scores, thus assembling a balanced cohort of 171 pairs of systolic heart failure patients without chronic kidney disease.
Statistical analysis
For descriptive analyses, we used Pearson Chi square and Wilcoxon rank-sum tests for the pre-match, and McNemar’s test and paired sample t-test for post-match comparisons, as appropriate. Kaplan-Meier plots and Cox regression analyses were used to determine the associations of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with outcomes during over 8 years of follow-up. To quantify the degree of a hidden bias that would be required to explain away a significant association among matched patients we conducted a formal sensitivity analysis. Subgroup analyses were conducted to determine the homogeneity of association. We then examined the associations of below-target and target doses of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with outcomes using patients not receiving these drugs as reference. Finally, we examined the associations of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with outcomes in those with chronic kidney disease Stage ≥3B (estimated glomerular filtration rate <45 ml/min/1.73 m2). All statistical tests were two-tailed with a p-value <0.05 considered significant. Statistical analyses were performed using SPSS-18 for Windows (SPSS, Inc., 2009, Chicago, IL).
Results
Baseline characteristics
Matched systolic heart failure patients with chronic kidney disease (n=888) had a mean age (±SD) of 78 (±7) years, 51% were women, and 21% were African American. Pre-match imbalances in the distribution of gender, comorbidities and treatment between patients receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers were well-balanced after matching (Table 1 and Figure 1). Of the 888 matched patients, 591 had chronic kidney disease stage ≥3B. These patients had a mean age (±SD) of 78 (±7) years, 51% were women, and 24% were African American. Matched systolic heart failure patients without chronic kidney disease (n=342) had a mean age (±SD) of 77 (±8) years, 45% were women, and 26% were African American. Pre-match imbalances in various baseline characteristics in these patients were also well balanced after matching (Table 2).
Table 2.
Baseline patient characteristics of older systolic heart failure patients without chronic kidney disease by discharge prescription of angiotensin-converting enzyme inhibitor (ACEIs) or angiotensin receptor blockers (ARBs), before and after propensity score matching
| n (%) or mean (±SD) | Before propensity score matching Use of ACEIs or ARBs | After propensity score matching Use of ACEIs or ARBs | ||||
|---|---|---|---|---|---|---|
| No (n=215) | Yes (n=693) | P value | No (n=171) | Yes (n=171) | P value | |
| Age (years) | 77 (±7) | 76 (±7) | 0.227 | 77 (±7) | 77 (±8) | 0.962 |
| Female | 91 (42) | 319 (46) | 0.340 | 73 (43) | 82 (48) | 0.412 |
| African American | 51 (24) | 200 (29) | 0.141 | 43 (25) | 46 (27) | 0.795 |
| Current smoker | 26 (12) | 101 (15) | 0.359 | 19 (11) | 20 (12) | 1.000 |
| Nursing home residents | 8 (4) | 24 (4) | 0.858 | 5 (3) | 10 (6) | 0.302 |
| Left ventricular ejection fraction (%) | 29 (±9) | 28 (±9) | 0.043 | 30 (±9) | 29 (±9) | 0.600 |
| Past medical history | ||||||
| Prior heart failure | 136 (63) | 457 (66) | 0.469 | 110 (64) | 105 (61) | 0.630 |
| Hypertension | 131 (61) | 467 (67) | 0.081 | 105 (61) | 109 (64) | 0.741 |
| Coronary artery disease | 134 (62) | 386 (56) | 0.086 | 100 (59) | 84 (49) | 0.085 |
| Myocardial infarction | 57 (27) | 193 (73) | 0.701 | 46 (27) | 39 (23) | 0.419 |
| Angina pectoris | 38 (18) | 110 (16) | 0.532 | 30 (18) | 25 (15) | 0.551 |
| Percutaneous coronary intervention | 29 (14) | 107 (15) | 0.484 | 23 (14) | 18 (11) | 0.487 |
| Coronary artery bypass graft | 74 (34) | 176 (25) | 0.010 | 50 (29) | 45 (26) | 0.644 |
| Left bundle branch block | 46 (21) | 159 (23) | 0.635 | 37 (22) | 41 (24) | 0.704 |
| Diabetes mellitus | 67 (31) | 300 (43) | 0.002 | 54 (32) | 59 (35) | 0.620 |
| Atrial fibrillation | 62 (29) | 190 (27) | 0.685 | 50 (29) | 48 (28) | 0.909 |
| Stroke | 41 (19) | 112 (16) | 0.320 | 31 (18) | 28 (16) | 0.775 |
| Chronic obstructive pulmonary disease | 85 (40) | 242 (35) | 0.218 | 68 (40) | 61 (36) | 0.505 |
| Dementia | 15 (7) | 49 (7) | 0.962 | 10 (6) | 12 (7) | 0.832 |
| Cancer | 9 (4) | 22 (3) | 0.476 | 7 (4) | 5 (3) | 0.774 |
| Clinical findings | ||||||
| Pulse (beats per minute) | 95 (±24) | 93 (±22) | 0.346 | 94 (±22) | 94 (±24) | 0.726 |
| Systolic blood pressure (mmHg) | 144 (±28) | 150 (±29) | 0.017 | 146 (±27) | 145 (±30) | 0.388 |
| Diastolic blood pressure (mmHg) | 80 (±17) | 83 (±17) | 0.021 | 79 (±17) | 80 (±18) | 0.431 |
| Respiration (breaths per minute) | 24 (±7) | 24 (±6) | 0.538 | 24 (±6) | 24 (±6) | 0.813 |
| Peripheral edema | 140 (65) | 450 (65) | 0.961 | 110 (64) | 115 (67) | 0.672 |
| Pulmonary edema by chest x-ray | 151 (70) | 488 (70) | 0.958 | 118 (69) | 119 (70) | 1.000 |
| Tests and procedures | ||||||
| Serum sodium (mEq/L) | 138 (±5) | 138 (±5) | 0.911 | 139 (±5) | 138 (±5) | 0.092 |
| Serum potassium (mEq/L) | 4.1 (±0.5) | 4.2 (±0.6) | 0.497 | 4.1 (±0.6) | 4.2 (±0.5) | 0.831 |
| Serum creatinine (mEq/L) | 1.0 (±0.2) | 1.0 (±0.2) | 0.955 | 1.0 (±0.2) | 1.0 (±0.2) | 0.239 |
| Estimated glomerular filtration rate (ml/min/1.73m2) | 77 (±15) | 77 (±15) | 0.838 | 77 (±15) | 77 (±15) | 0.227 |
| Blood urea nitrogen (mg/dL) | 19 (±7) | 18 (±7) | 0.022 | 18 (±7) | 19 (±7) | 0.909 |
| Serum glucose (mg/dL) | 147 (±67) | 153 (±69) | 0.237 | 146 (±56) | 146 (±66) | 0.727 |
| Hematocrit (%) | 38 (±5) | 38 (±5) | 0.527 | 37 (±6) | 38 (±5) | 0.675 |
| White blood cell (103/μL) | 9 (±4) | 9 (±5) | 0.380 | 9 (±7) | 9 (±4) | 0.740 |
| Hospital and care characteristics | ||||||
| Pneumonia | 58 (27) | 163 (24) | 0.302 | 49 (29) | 46 (27) | 0.810 |
| Acute myocardial infarction | 17 (8) | 33 (5) | 0.077 | 8 (5) | 12 (7) | 0.503 |
| Pressures ulcer | 20 (9) | 50 (7) | 0.316 | 15 (9) | 19 (11) | 0.608 |
| Rural hospital | 44 (21) | 166 (24) | 0.289 | 36 (21) | 41 (24) | 0.620 |
| Cardiology consult | 145 (67) | 484 (70) | 0.505 | 116 (68) | 114 (67) | 0.908 |
| Intensive care unit | 9 (4) | 28 (4) | 0.925 | 6 (4) | 7 (4) | 1.000 |
| Length of stay (days) | 8 (±6) | 6 (±4) | <0.001 | 7.2 (±4.7) | 6.8 (±4.6) | 0.052 |
| Discharge medications | ||||||
| Beta blockers (heart failure) | 33 (15) | 203 (29) | 0.000 | 31 (18) | 31 (18) | 1.000 |
| Loop diuretics | 164 (76) | 636 (92) | <0.001 | 145 (85) | 138 (81) | 0.337 |
| Potassium-sparing diuretics | 23 (11) | 171 (25) | 0.000 | 21 (12) | 28 (16) | 0.311 |
| Digoxin | 92 (43) | 444 (64) | <0.001 | 85 (50) | 88 (52) | 0.813 |
| Calcium channel blockers | 37 (17) | 104 (15) | 0.436 | 27 (16) | 33 (19) | 0.497 |
| Potassium supplements | 96 (45) | 350 (51) | 0.134 | 86 (50) | 81 (47) | 0.734 |
| Nitrates and hydralazine | 4 (2) | 3 (0) | 0.037 | 1 (1) | 2 (1) | 1.000 |
| Anti-arrhythmic drugs | 34(16) | 93 (13) | 0.377 | 28 (16) | 28 (16) | 1.000 |
| Anti-coagulants | 60 (28) | 202 (29) | 0.726 | 47 (28) | 43 (25) | 0.699 |
| Anti-platelet drugs | 18 (8) | 69 (10) | 0.490 | 14 (8) | 19 (11) | 0.487 |
| Aspirin | 64 (30) | 314 (45) | <0.001 | 58 (34) | 56 (33) | 0.901 |
| Insulin | 15 (7) | 97 (14) | 0.006 | 15 (9) | 15 (9) | 1.000 |
| Statins | 24 (11) | 120 (17) | 0.031 | 20 (12) | 19 (11) | 1.000 |
| Anti-depressants | 44 (21) | 107 (15) | 0.084 | 32 (19) | 36 (21) | 0.678 |
| Non-steroidal anti-inflammatory drugs | 21 (10) | 57 (8) | 0.481 | 16 (9) | 18 (11) | 0.860 |
All-cause mortality in systolic heart failure patients with chronic kidney disease
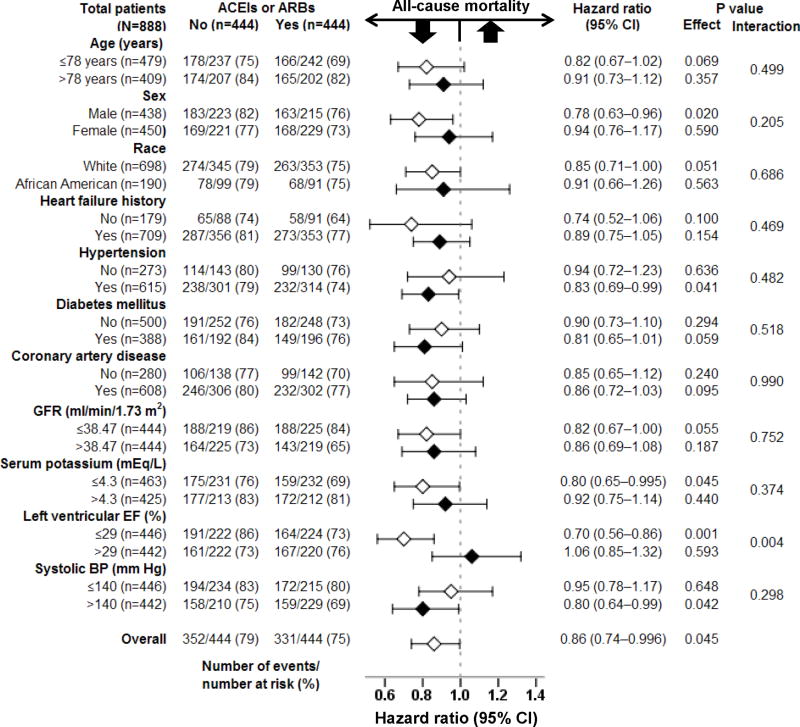
All-cause mortality occurred in 75% and 79% of matched systolic heart failure patients with chronic kidney disease receiving and not receiving discharge prescriptions for angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, respectively, during 8 years of follow-up (hazard ratio {HR} when the use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers was compared with their non-use, 0.86; 95% confidence interval {CI}, 0.74–0.996; p=0.045; Table 3 and Figure 2). A hidden covariate that is a near-perfect predictor of all-cause mortality may potentially explain away this association if it would increase the odds of discharge prescription of these drugs by about 2%. This association was homogeneous across various subgroups of patients except for that by left ventricular ejection fraction (p for interaction, 0.004; Figure 3). Similar risk-adjusted associations were also observed among the 1665 pre-match patients with chronic kidney disease (Table 3).
Table 3.
Association of discharge prescription of angiotensin-converting enzyme inhibitor (ACEIs) or angiotensin receptor blockers (ARBs) with all-cause mortality in older systolic heart failure patients with and without chronic kidney disease
| All-cause mortality | % (total events/total patients) Use of ACEIs or ARBs | Absolute risk difference* (%) | Hazard ratio† (95% confidence interval) | P value | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Chronic kidney disease | |||||
| Pre-match unadjusted | 81% (503/619) | 72% (753/1046) | −9 | 0.71 (0.64–0.80) | <0.001 |
| Pre-match multivariable-adjusted | --- | --- | --- | 0.85 (0.75–0.97) | 0.016 |
| Pre-match propensity-adjusted | --- | --- | --- | 0.88 (0.78–1.00) | 0.050 |
| Post-match | 79% (352/444) | 75% (331/444) | −4 | 0.86 (0.74–0.996) | 0.045 |
| No chronic kidney disease | |||||
| Pre-match unadjusted | 70% (151/215) | 58% (399/693) | −12 | 0.69 (0.58–0.84) | <0.001 |
| Pre-match multivariable-adjusted | --- | --- | --- | 0.73 (0.59–0.91) | 0.005 |
| Pre-match propensity-adjusted | --- | --- | --- | 0.76 (0.62–0.95) | 0.013 |
| Post-match | 70% (119/171) | 56% (96/171) | −14 | 0.72 (0.55–0.94) | 0.015 |
Absolute risk differences were calculated by subtracting percent events in patients not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with from those receiving those drugs
Hazard ratios comparing patients receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with those not receiving those drugs
Figure 2.
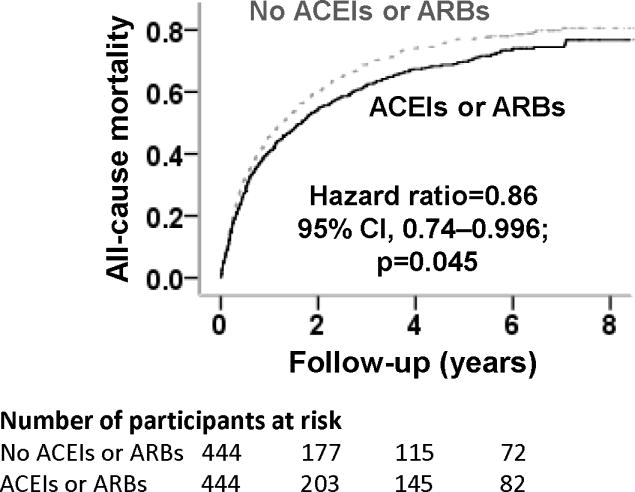
Kaplan-Meier plots for all-cause mortality in a propensity-matched cohort of older systolic heart failure patients with chronic kidney disease receiving and not receiving discharge prescription of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (CI=confidence interval)
Figure 3.
Association of discharge prescription of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with all-cause mortality in subgroups of propensity-matched older systolic heart failure patients with chronic kidney disease
Among the 487 matched patients without pre-admission use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, all-cause mortality occurred in 77% and 78% of those receiving and not receiving a new discharge prescription for angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, respectively (HR, 0.97; 95% CI, 0.78–1.21; p=0.780). In contrast, among the 401 matched patients receiving pre-admission angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, all-cause mortality occurred in 73% and 83% of those receiving and not receiving continuation therapy with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, respectively (HR, 0.73; 95% CI, 0.56–0.94; p=0.013).
Of the 444 matched patients receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, data on dosages were available for 324 (73%) patients. Of these, 107 (24%) patients received at or above target doses and 217 (49%) received below-target doses of these drugs. Compared with matched patients not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (79% mortality, reference), 75% of those receiving below-target doses (HR, 0.90; 95% CI, 0.74–1.08; p=0.248) and 67% of those receiving target doses (HR, 0.69; 95% CI, 0.53–0.89; p=0.004) died. Among pre-match patients, multivariable-adjusted HRs associated with below-target and target doses of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers were 0.88 (95% CI, 0.75–1.02; p=0.077) and 0.77 (95% CI, 0.63–0.94; p=0.012), respectively.
Hospitalization in systolic heart failure patients with chronic kidney disease
Among matched systolic heart failure patients with chronic kidney disease, discharge prescription of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers had no significant association with heart failure hospitalization (HR, 0.86; 95% CI, 0.72–1.03; p=0.094) or all-cause hospitalization (HR, 0.89; 95% CI, 0.77–1.02; p=0.101; Tables 4 and 5). HRs for heart failure hospitalization associated with below-target and target doses of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers were 0.76 (95% CI, 0.61–0.95; p=0.017) and 0.74 (95% CI, 0.55–0.92; p=0.037), respectively.
Table 4.
Association of discharge prescription of angiotensin-converting enzyme inhibitor (ACEIs) or angiotensin receptor blockers (ARBs) with heart failure hospitalization in older systolic heart failure patients with and without chronic kidney disease
| Heart failure hospitalization | % (total events/total patients) Use of ACEIs or ARBs | Absolute risk difference* (%) | Hazard ratio† (95% confidence interval) | P value | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Chronic kidney disease | |||||
| Pre-match unadjusted | 57% (354/619) | 58% (601/1046) | +1 | 0.76 (0.67–0.87) | <0.001 |
| Pre-match multivariable-adjusted | --- | --- | --- | 0.82 (0.71–0.95) | 0.009 |
| Pre-match propensity-adjusted | --- | --- | --- | 0.85 (0.74–0.99) | 0.032 |
| Post-match | 57% (253/444) | 55% (245/444) | −2 | 0.86 (0.72–1.03) | 0.094 |
| No chronic kidney disease | |||||
| Pre-match unadjusted | 55% (118/215) | 54% (372/693) | −1 | 0.76 (0.62–0.94) | 0.010 |
| Pre-match multivariable-adjusted | --- | --- | --- | 0.79 (0.62–1.00) | 0.052 |
| Pre-match propensity-adjusted | --- | --- | --- | 0.77 (0.61–0.97) | 0.029 |
| Post-match | 55% (94/171) | 46% (79/171) | −9 | 0.71 (0.52–0.95) | 0.023 |
Absolute risk differences were calculated by subtracting percent events in patients not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with from those receiving those drugs
Hazard ratios comparing patients receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with those not receiving those drugs
Table 5.
Association of discharge prescription of angiotensin-converting enzyme inhibitor (ACEIs) or angiotensin receptor blockers (ARBs) with all-cause hospitalization in older systolic heart failure patients with and without chronic kidney disease
| All-cause hospitalization | % (total events/total patients) Use of ACEIs or ARBs | Absolute risk difference* (%) | Hazard ratio† (95% confidence interval) | P value | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Chronic kidney disease | |||||
| Pre-match unadjusted | 83% (503/619) | 85% (753/1046) | +2 | 0.79 (0.70–0.88) | <0.001 |
| Pre-match multivariable-adjusted | --- | --- | --- | 0.88 (0.78–0.99) | 0.040 |
| Pre-match propensity-adjusted | --- | --- | --- | 0.89 (0.79–1.01) | 0.061 |
| Post-match | 85% (376/444) | 83% (369/444) | −2 | 0.89 (0.77–1.02) | 0.101 |
| No chronic kidney disease | |||||
| Pre-match unadjusted | 84% (181/215) | 85% (592/693) | +1 | 0.79 (0.67–0.93) | 0.006 |
| Pre-match multivariable-adjusted | --- | --- | --- | 0.78 (0.64–0.94) | 0.010 |
| Pre-match propensity-adjusted | --- | --- | --- | 0.82 (0.68–0.99) | 0.039 |
| Post-match | 83% (141/171) | 85% (145/171) | +2 | 0.94 (0.75–1.19) | 0.603 |
Absolute risk differences were calculated by subtracting percent events in patients not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with from those receiving those drugs
Hazard ratios comparing patients receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers with those not receiving those drugs
Outcomes in systolic heart failure patients with chronic kidney disease stage ≥3B
Among the subset of 591 matched systolic heart failure patients with chronic kidney disease stage ≥3B, all-cause mortality occurred in 80% and 83% of those receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, respectively (HR, 0.83; 95% CI, 0.70–1.00; p=0.046). Relative to non-use of these drugs, HRs for all-cause mortality associated with their use in below-target and target doses were 0.90 (95% CI, 0.72–1.12; p=0.326) and 0.67 (95% CI, 0.49–0.91; p=0.011), respectively. Respective HRs for heart failure hospitalization associated with below-target and target doses were 0.75 (95% CI, 0.57–0.98; p=0.038) and 0.60 (95% CI, 0.40–0.88; p=0.009), respectively.
Outcomes in systolic heart failure patients without chronic kidney disease
All-cause mortality occurred in 56% and 70% of matched systolic heart failure patients without chronic kidney disease receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, respectively (HR, 0.72; 95% CI, 0.55–0.94; p=0.015; Table 3). Heart failure hospitalization occurred in 46% and 55% of these patients receiving and not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (HR, 0.71; 95% CI, 0.52–0.95; p=0.023; Table 4).
Discussion
Summary and relevance of the key findings
Findings of the current analysis demonstrate that in a propensity-matched balanced cohort of older systolic heart failure patients with chronic kidney disease, discharge prescriptions of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers were associated with a modest but significant reduction in all-cause mortality, and that these associations were stronger for those receiving target doses of these drugs. We also observed that these associations persisted in those with more advanced chronic kidney disease. However, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers had no significant associations with heart failure hospitalizations in systolic heart failure patients with chronic kidney disease. In contrast, in systolic heart failure patients without chronic kidney disease, the use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers was associated with a significant and robust reduction in both all-cause mortality and heart failure hospitalization. These findings based on rigorous propensity matching designs provide further evidence that despite concerns for worsening kidney function in systolic heart failure patients with chronic kidney disease receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, discharge prescription of these drugs may be safe and associated with improved outcomes.
Potential explanation and mechanism of the key findings
A large body of evidence from randomized clinical trials supports an intrinsic beneficial effect of renin-angiotensin system inhibition in systolic heart failure.30 Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers reduce ventricular preload and after load, attenuate myocardial fibrosis and maladaptive remodeling, and improve left ventricular ejection fraction and functional capacity.31,32 Renin-angiotensin system inhibition also delay disease progression and improve clinical outcomes in patients with chronic kidney disease,5,33 and improve renal function in systolic heart failure patients with advanced chronic kidney disease.34 Therefore, it is possible that angiotensin-converting enzyme inhibitors or angiotensin receptor blockers improved outcomes in those with both systolic heart failure and chronic kidney disease by improving both cardiac and renal function. Although residual bias is possible but unlikely as propensity-matched patients in our study were well-balanced on key baseline confounders.
Although treatment effect is generally more pronounced in those with more severe or advanced disease,35 it was modest in those patients with systolic heart failure and chronic kidney disease in our study. Considering that systolic heart failure patients with chronic kidney disease had more advanced disease, it is likely that pump failure was a more common cause of death than sudden death.36,37 Although angiotensin-converting enzyme inhibitors reduce both forms of death in heart failure,2 they may be less effective in reducing disease progression in those with chronic kidney disease. This notion is also supported by the lack of a significant reduction in heart failure hospitalization in those with chronic kidney disease, but not in those without chronic kidney disease. Another potential explanation for a more modest effect in those with chronic kidney disease is that more severe adverse effects (namely, renal insufficiency, hyperkalemia or hypotension) leading to a higher rate of drug discontinuation thus leading to an attenuated benefit. Although we had no data on medication use during follow-up, a post-hoc analysis demonstrated a higher admission-to-discharge discontinuation among those with chronic kidney disease stage ≥3B (24%) than with stage 3A (10%; p <0.001).
Comparison with findings from relevant published literature
In patients with coronary artery disease, systolic heart failure and chronic kidney disease, angiotensin-converting enzyme inhibitor use had no association with mortality.38 In post-acute myocardial infarction patients with reduced left ventricular ejection fraction, on the other hand, angiotensin-converting enzyme inhibitor use was associated with reduced mortality.39 Several small observational studies in systolic heart failure patients with chronic kidney disease have also suggested potential benefits of these drugs.40–42 However, the current study is distinguished from the prior studies by its larger sample size, longer follow-up, use of a more rigorous methodology, inclusion of both angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, and the use of contemporary therapy for systolic heart failure. Cumulative findings from these studies, taken together with the evidence of their benefit in systolic heart failure as well as in chronic kidney disease, suggest that the use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers should be expanded to include systolic heart failure patients with chronic kidney disease, including those with more advanced chronic kidney disease.
Clinical and public health importance
Nearly half of all systolic heart failure patients have chronic kidney disease, which is associated with poor outcomes and underuse of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. Physicians often attribute this to lack of evidence of benefit and concern for potential harmful effects.7–9 Findings from the current study should attenuate these concerns and lead to increased use of these drugs in older systolic heart failure patients with chronic kidney disease. We also observed that the benefit of these drugs was similar in those with more advanced chronic kidney disease. Nonetheless, these drugs should be prescribed with caution in those with low systolic blood pressure or high serum potassium. Because mild hypokalemia is common in heart failure patients with chronic kidney disease and is associated with poor outcomes,43 elevation of serum potassium during therapy with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers may be beneficial in these patients. However, close monitoring of serum potassium is advisable, especially if serum potassium is above 5.5 mEq/L or concomitant aldosterone antagonists are prescribed.44
Potential limitations and future direction
Our study has several limitations. Despite balance in all measured baseline covariates, bias due to imbalances in unmeasured covariates is possible. Sensitivity analysis suggests that mortality reduction associated with angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use in our study was rather sensitive to a potential unmeasured confounder. However, sensitivity analysis cannot determine if such an unmeasured confounder exists or not. Further, to act as a confounder, an unmeasured covariate that is a near-perfect predictor of mortality must also be associated with discharge prescription of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers and not be strongly correlated with any of the 56 measured baseline covariates used in our study. Loss of data in the matching process may limit external validity but enhances internal validity. Further, over 72% of patients not receiving angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (the smaller of the two groups) were matched. Patients discharged on angiotensin-converting enzyme inhibitors or angiotensin receptor blockers may have discontinued their use and vice versa. However, this is likely to be minimal,45 and the resultant regression dilution may have underestimated the observed associations.46 Findings of the current study based on a single state may limit generalizability but may have important implication for Alabama that has one of the highest heart failure mortality.47
Conclusions
A discharge prescription for angiotensin-converting enzyme inhibitors or angiotensin receptor blockers was associated with a significant but modest reduction in all-cause mortality in older systolic heart failure patients with chronic kidney disease including those with more advanced chronic kidney disease, and this association seemed stronger among those receiving these drugs at or above target doses. The use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers was also associated with a trend toward lower heart failure hospitalization in those with chronic kidney disease. These findings suggest that angiotensin-converting enzyme inhibitors or angiotensin receptor blockers are safe and beneficial in older systolic heart failure patients with chronic kidney disease.
Acknowledgments
Funding/Support: Dr. Ahmed is supported by the NIH through grants (R01-HL085561, R01-HL085561-S and R01-HL097047) from the NHLBI and a generous gift from Ms. Jean B. Morris of Birmingham, Alabama. Dr. Allman is supported by the NIH through grant (5UL1 RR025777). Dr. Sanders is supported by the NIH through grant (R01-DK46199) and by the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:e391–479. doi: 10.1161/CIRCULATIONAHA.109.192065. [DOI] [PubMed] [Google Scholar]
- 2.The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed A, Rich MW, Sanders PW, et al. Chronic kidney disease associated mortality in diastolic versus systolic heart failure: a propensity matched study. Am J Cardiol. 2007;99:393–398. doi: 10.1016/j.amjcard.2006.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahmed A, Campbell RC. Epidemiology of chronic kidney disease in heart failure. Heart Fail Clin. 2008;4:387–399. doi: 10.1016/j.hfc.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hou FF, Zhang X, Zhang GH, et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med. 2006;354:131–140. doi: 10.1056/NEJMoa053107. [DOI] [PubMed] [Google Scholar]
- 6.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998–1999 to 2000–2001. JAMA. 2003;289:305–312. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- 7.Bart BA, Gattis WA, Diem SJ, O’Connor CM. Reasons for underuse of angiotensin-converting enzyme inhibitors in patients with heart failure and left ventricular dysfunction. American Journal of Cardiology. 1997;79:1118–1120. doi: 10.1016/s0002-9149(97)00060-x. [DOI] [PubMed] [Google Scholar]
- 8.Bakris GL, Weir MR. Angiotensin-converting enzyme inhibitor-associated elevations in serum creatinine: is this a cause for concern? Arch Intern Med. 2000;160:685–693. doi: 10.1001/archinte.160.5.685. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed A. Use of angiotensin-converting enzyme inhibitors in patients with heart failure and renal insufficiency: how concerned should we be by the rise in serum creatinine? J Am Geriatr Soc. 2002;50:1297–1300. doi: 10.1046/j.1532-5415.2002.50321.x. [DOI] [PubMed] [Google Scholar]
- 10.Rosenbaum PR, Rubin DB. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 11.Rubin DB. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001;2:169–188. [Google Scholar]
- 12.Michels KB, Braunwald E. Estimating treatment effects from observational data: dissonant and resonant notes from the SYMPHONY trials. JAMA. 2002;287:3130–3132. doi: 10.1001/jama.287.23.3130. [DOI] [PubMed] [Google Scholar]
- 13.Heinze G, Juni P. An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J. 2011;32:1704–1708. doi: 10.1093/eurheartj/ehr031. [DOI] [PubMed] [Google Scholar]
- 14.Feller MA, Mujib M, Zhang Y, et al. Baseline characteristics, quality of care, and outcomes of younger and older Medicare beneficiaries hospitalized with heart failure: Findings from the Alabama Heart Failure Project. Int J Cardiol. 2011 doi: 10.1016/j.ijcard.2011.05.003. [Epub ahead of print] doi:10.1016/j.ijcard.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Fonarow GC, Sanders PW, et al. A propensity-matched study of the comparative effectiveness of angiotensin receptor blockers versus angiotensin-converting enzyme inhibitors in heart failure patients age ≥65 years. Am J Cardiol. 2011;108:1443–1447. doi: 10.1016/j.amjcard.2011.06.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Kidney F. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266. [PubMed] [Google Scholar]
- 17.Packer M, Poole-Wilson PA, Armstrong PW, et al. Comparative effects of low and high doses of the angiotensin-converting enzyme inhibitor, lisinopril, on morbidity and mortality in chronic heart failure. ATLAS Study Group. Circulation. 1999;100:2312–2318. doi: 10.1161/01.cir.100.23.2312. [DOI] [PubMed] [Google Scholar]
- 18.Heywood JT, Fonarow GC, Yancy CW, et al. Comparison of medical therapy dosing in outpatients cared for in cardiology practices with heart failure and reduced ejection fractionwith and without device therapy: report from IMPROVE HF. Circ Heart Fail. 2010;3:596–605. doi: 10.1161/CIRCHEARTFAILURE.109.912683. [DOI] [PubMed] [Google Scholar]
- 19.Ahmed A, Husain A, Love TE, et al. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27:1431–1439. doi: 10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mujib M, Desai RV, Ahmed MI, et al. Rheumatic heart disease and risk of incident heart failure among community-dwelling older adults: A prospective cohort study. Ann Med. 2011 doi: 10.3109/07853890.2010.530685. [Epub ahead of print] doi:10.3109/07853890.2010.530685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mujib M, Rahman AA, Desai RV, et al. Warfarin use and outcomes in patients with advanced chronic systolic heart failure without atrial fibrillation, prior thromboembolic events, or prosthetic valves. Am J Cardiol. 2011;107:552–557. doi: 10.1016/j.amjcard.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmed MI, Lainscak M, Mujib M, et al. Gender-related dissociation in outcomes in chronic heart failure: reduced mortality but similar hospitalization in women. Int J Cardiol. 2011;148:36–42. doi: 10.1016/j.ijcard.2009.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banach M, Bhatia V, Feller MA, et al. Relation of baseline systolic blood pressure and long-term outcomes in ambulatory patients with chronic mild to moderate heart failure. Am J Cardiol. 2011;107:1208–1214. doi: 10.1016/j.amjcard.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Filippatos GS, Ahmed MI, Gladden JD, et al. Hyperuricaemia, chronic kidney disease, and outcomes in heart failure: potential mechanistic insights from epidemiological data. Eur Heart J. 2011;32:712–720. doi: 10.1093/eurheartj/ehq473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gheorghiade M, Flaherty JD, Fonarow GC, et al. Coronary artery disease, coronary revascularization, and outcomes in chronic advanced systolic heart failure. Int J Cardiol. 2011;151:69–75. doi: 10.1016/j.ijcard.2010.04.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Austin PC. Primer on statistical interpretation or methods report card on propensity-score matching in the cardiology literature from 2004 to 2006: a systematic review. Circ Cardiovasc Qual Outcomes. 2008;1:62–67. doi: 10.1161/CIRCOUTCOMES.108.790634. [DOI] [PubMed] [Google Scholar]
- 27.Ekundayo OJ, Dell’Italia LJ, Sanders PW, et al. Association between hyperuricemia and incident heart failure among older adults: a propensity-matched study. Int J Cardiol. 2010;142:279–287. doi: 10.1016/j.ijcard.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giamouzis G, Agha SA, Ekundayo OJ, et al. Incident coronary revascularization and subsequent mortality in chronic heart failure: a propensity-matched study. Int J Cardiol. 2010;140:55–59. doi: 10.1016/j.ijcard.2008.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iyer AS, Ahmed MI, Filippatos GS, et al. Uncontrolled hypertension and increased risk for incident heart failure in older adults with hypertension: findings from a propensity-matched prospective population study. J Am Soc Hypertens. 2010;4:22–31. doi: 10.1016/j.jash.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA. 1995;273:1450–1456. [PubMed] [Google Scholar]
- 31.Cohn JN. Physiologic basis of vasodilator therapy for heart failure. Am J Med. 1981;71:135–139. doi: 10.1016/0002-9343(81)90276-x. [DOI] [PubMed] [Google Scholar]
- 32.Pfeffer JM, Pfeffer MA. Angiotensin converting enzyme inhibition and ventricular remodeling in heart failure. Am J Med. 1988;84:37–44. doi: 10.1016/0002-9343(88)90203-3. [DOI] [PubMed] [Google Scholar]
- 33.Hebert LA. Optimizing ACE-inhibitor therapy for chronic kidney disease. N Engl J Med. 2006;354:189–191. doi: 10.1056/NEJMe058295. [DOI] [PubMed] [Google Scholar]
- 34.Dzau VJ, Colucci WS, Williams GH, Curfman G, Meggs L, Hollenberg NK. Sustained effectiveness of converting-enzyme inhibition in patients with severe congestive heart failure. N Engl J Med. 1980;302:1373–1379. doi: 10.1056/NEJM198006193022501. [DOI] [PubMed] [Google Scholar]
- 35.Rothwell PM. Treating individuals 2. Subgroup analysis in randomised controlled trials: importance, indications, and interpretation. Lancet. 2005;365:176–186. doi: 10.1016/S0140-6736(05)17709-5. [DOI] [PubMed] [Google Scholar]
- 36.Gheorghiade M, Bonow RO. Introduction and overview: beta-blocker therapy in the management of chronic heart failure. Am J Med. 2001;110(Suppl 7A):1S–5S. doi: 10.1016/s0002-9343(00)00553-2. [DOI] [PubMed] [Google Scholar]
- 37.Carson P, Anand I, O’Connor C, et al. Mode of death in advanced heart failure: the Comparison of Medical, Pacing, and Defibrillation Therapies in HeartFailure (COMPANION) trial. J Am Coll Cardiol. 2005;46:2329–2334. doi: 10.1016/j.jacc.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 38.Ezekowitz J, McAlister FA, Humphries KH, et al. The association among renal insufficiency, pharmacotherapy, and outcomes in 6,427 patients with heart failure and coronary artery disease. J Am Coll Cardiol. 2004;44:1587–1592. doi: 10.1016/j.jacc.2004.06.072. [DOI] [PubMed] [Google Scholar]
- 39.Frances CD, Noguchi H, Massie BM, Browner WS, McClellan M. Are we inhibited? Renal insufficiency should not preclude the use of ACE inhibitors for patients with myocardial infarction and depressed left ventricular function. Arch Intern Med. 2000;160:2645–2650. doi: 10.1001/archinte.160.17.2645. [DOI] [PubMed] [Google Scholar]
- 40.Ahmed A, Kiefe CI, Allman RM, Sims RV, DeLong JF. Survival benefits of angiotensin-converting enzyme inhibitors in older heart failure patients with perceived contraindications. J Am Geriatr Soc. 2002;50:1659–1666. doi: 10.1046/j.1532-5415.2002.50457.x. [DOI] [PubMed] [Google Scholar]
- 41.Ahmed A, Centor R, Weaver MT, DeLong JF. A propensity score analysis of the impact of ACE inhibitors on 4-year survival of older adults with heart failure and perceived contraindications. American Heart Journal. 2005;149:737–743. doi: 10.1016/j.ahj.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 42.Ahmed A, Love TE, Sui X, Rich MW. Effects of angiotensin-converting enzyme inhibitors in systolic heart failure patients with chronic kidney disease: a propensity score analysis. J Card Fail. 2006;12:499–506. doi: 10.1016/j.cardfail.2006.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bowling CB, Pitt B, Ahmed MI, et al. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: findings from propensity-matched studies. Circ Heart Fail. 2010;3:253–260. doi: 10.1161/CIRCHEARTFAILURE.109.899526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ahmed MI, Ekundayo OJ, Mujib M, et al. Mild hyperkalemia and outcomes in chronic heart failure: a propensity matched study. Int J Cardiol. 2010;144:383–388. doi: 10.1016/j.ijcard.2009.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Butler J, Arbogast PG, Daugherty J, Jain MK, Ray WA, Griffin MR. Outpatient utilization of angiotensin-converting enzyme inhibitors among heart failure patients after hospital discharge. J Am Coll Cardiol. 2004;43:2036–2043. doi: 10.1016/j.jacc.2004.01.041. [DOI] [PubMed] [Google Scholar]
- 46.Clarke R, Shipley M, Lewington S, et al. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. American journal of epidemiology. 1999;150:341–353. doi: 10.1093/oxfordjournals.aje.a010013. [DOI] [PubMed] [Google Scholar]
- 47.Mujib M, Zhang Y, Feller MA, Ahmed A. Evidence of a “heart failure belt” in the southeastern United States. Am J Cardiol. 2011;107:935–937. doi: 10.1016/j.amjcard.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]