Abstract
Natural killer (NK) cells were first described as immune leukocytes that could kill tumor cells and soon after were reported to kill virus-infected cells. In the mid-1980s, 10 years after their discovery, NK cells were also demonstrated to contribute to the fight against bacterial infection, particularly because of crosstalk with other leukocytes. A wide variety of immune cells are now recognized to interact with NK cells through the production of cytokines such as interleukin (IL)-2, IL-12, IL-15 and IL-18, which boost NK cell activities. The recent demonstration that NK cells express pattern recognition receptors, namely Toll-like and nucleotide oligomerization domain (NOD)-like receptors, led to the understanding that these cells are not only under the control of accessory cells, but can be directly involved in the antibacterial response thanks to their capacity to recognize pathogen-associated molecular patterns. Interferon (IFN)-γ is the predominant cytokine produced by activated NK cells. IFN-γ is a key contributor to antibacterial immune defense. However, in synergy with other inflammatory cytokines, IFN-γ can also lead to deleterious effects similar to those observed during sepsis. Accordingly, as the main source of IFN-γ in the early phase of infection, NK cells display both beneficial and deleterious effects, depending on the circumstances.
ANTIBACTERIAL INNATE IMMUNITY
Microbial invasion into sterile body compartments causes infectious diseases that are locally addressed by cells of the innate immune system (1). Although actors of humoral immunity such as natural antibodies, pentraxins and factors of the complement system contribute to fight microbes in the early steps of innate immune response, cellular immunity does play a key role (2). As sensors of pathogenic microbial agents, innate immune cells recognize microbial-associated or pathogen-associated molecular patterns (PAMPs) by intracellular or cell surface receptors. PAMPs are microbial molecules such as the endotoxin of gram-negative bacteria (lipopolysaccharide [LPS]), the lipoteichoic acid of gram-positive bacteria and many other components (for example, lipoproteins, outer-membrane proteins, flagellin, fimbriae and peptidoglycan). In addition, bacterial lysis results in the release of internal motifs (for example, heat-shock proteins, RNA, and DNA fragments), which are additional PAMPs recognized by immune cells. These cells express pattern recognition receptors (PRRs), specifically recognizing PAMPs. The activation of PRRs initiates the innate immune antiinfectious response and the early production of cytokines, which orchestrate this response (3). Among PRRs, the discovery of Toll-like receptors (TLRs) and nucleotide oligomerization domain (NOD)-like receptors (NLRs) has led to an understanding of the interaction between microorganisms and hosts, as well as the very early steps of the innate immune response. TLRs are expressed either on the cell surface (TLR1, -2, -4, -5 and -6) or within endosomes (TLR3, -7, -8 and -9). NLRs are cytoplasmic sensors. In addition to cytokine production, the interaction of different PAMPs with their respective TLRs or NLRs initiates numerous intracellular signaling pathways that result in the activation of immune and inflammatory genes, including costimulatory molecules, adhesion molecules and antimicrobial mediators (2,4,5).
After infection, after PAMP recognition by immune cells, there are two well- characterized steps of the immune response illustrated by the production of pro- and antiinflammatory cytokines. In the most severe cases of infection (e.g., during sepsis), an overzealous release of proinflammatory cytokines and inflammatory mediators by activated leukocytes, epithelial cells and endothelial cells, known as a “cytokine storm,” leads to deleterious effects such as organ dysfunction and even death. Almost concomitantly, this proinflammatory response is accompanied by the release of antiinflammatory cytokines and neuro-mediators aimed to dampen the inflammatory process. The side effect of this antiinflammatory response is the alteration of immune status known as the “compensatory antiinflammatory response syndrome” (6), favoring the occurrence of nosocomial infections (7,8). The early cellular immune response involves the contribution of mast cells, mononuclear phagocytes and polymorphonuclear phagocytes (9). More recently, it became evident that natural killer (NK) cells were also key players in early immunity (10). The fact that TLRs were recently discovered to be expressed by NK cells has opened a new interest for their putative involvement in innate immune response to bacterial infections. It seems that in contrast to phagocytes, the activation of NK cells by PAMPs can only occur within a complex crosstalk with other immune cells that offer the cytokine microenvironment required for NK cell responsiveness (11). Accordingly, similar to any other cellular or molecular participant in infectious diseases, NK cells can play an “angel” or “devil” role, depending on the circumstances. The same actors, which contribute to fight infection, can act in synergy, leading to acute deleterious inflammation. This is particularly the case of γ-interferon (IFN-γ), which is one of the main cytokines produced by NK cells (12).
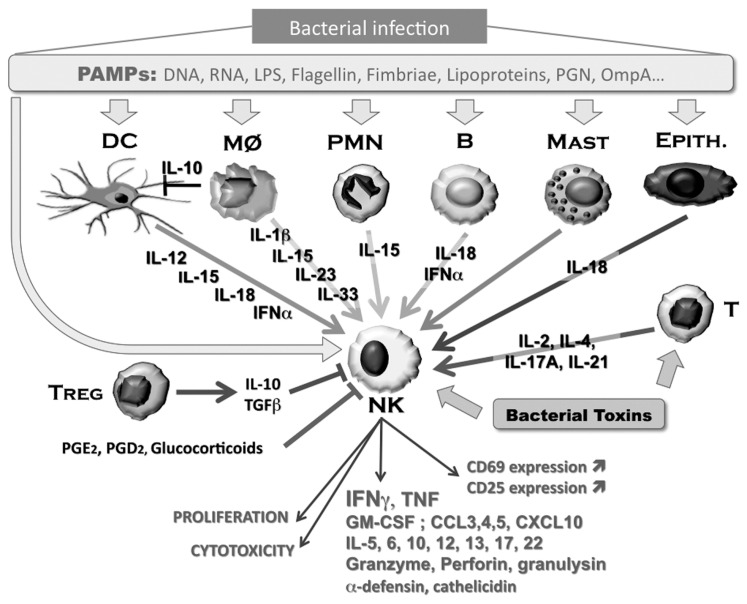
The concept of NK cells was first reported in 1975 by Hans Wigzell’s group, which established that leukemia cell lines could be lysed by cells with the morphology of small lymphocytes and devoid of T- and B-cell characteristics (13). Their expression of Fcγ receptors (14), and their capacity to kill target cells through antibody-dependent cell cytotoxicity, was demonstrated thereafter (15). Soon after, it was reported that NK cells were also active against virus-infected cells (16), opening a new field of investigation to be explored. In contrast, it took more time to accept the role of NK cells in bacterial infection. The lack of natural antibacterial activity against Salmonella typhimurium of beige mice, known to be deficient in NK activity, was not recognized as evidence supporting the role of NK effector cells in natural antibacterial activity (17). The first report on the role of NK cells during bacterial infection was related to their capacity to lyse either Shigella flexneri–infected HeLa cells (18), Legionella pneumophila–infected monocytes (19) or Mycobacterium avium–infected monocytes (20). The latter study also reported that NK cells could help macrophages to inhibit growth or kill intracellular bacilli (21). Similar findings were reported for Mycobacterium lepraemurium (22). The key in vivo role of NK cells during a bacterial infection was initially established in M. avium infection: an in vivo depletion of NK activity using antibodies provided direct evidence on their role in the control of intra-cellular mycobacterial pathogens (23). Since then, the role of NK cells in bacterial infection has been clearly established, including the cytokine microenvironment and the cellular crosstalks required for an active contribution of these cells in innate antibacterial immunity (Figure 1).
Figure 1.
Activation of NK cells by bacterial PAMPs. NK cells are activated within a network of accessory cells that sense bacterial PAMPs. Activation of accessory cells leads to the production of cytokines that contribute to the functional activation of NK cells, while sensing of PAMPs by NK cells themselves further enhances NK cell reactivity. All listed cytokines have been shown to amplify NK cell activity, either alone or in synergy. Negative signals can be directly delivered to NK cells (for example, IL-10 and TGF-β produced by Tregs, prostaglandins or glucocorticoids) or indirectly by downregulating the function of accessory cells. PGN, peptidoglycan; OmpA, outer-membrane protein A, MØ, macrophages; PMN, polymorphonuclear leukocytes (neutrophils); B, B lympocytes; MAST, mast cell; EPITH., epithelial cell; PGE2, prostaglandin E2; PGD2, prostaglandin D2.
It is possible that all NK cell subsets are not equivalent in their antibacterial activity. However, human and mouse NK cell subsets will not be detailed in this review (for detailed reviews about NK cell subsets, see Huntington et al. [24] and Wilk et al. [25]). For example, it has been shown that in response to BCG (bacillus Calmette-Guérin), human CD56BRIGHT NK cells were cells mainly involved in IFN-γ production, whereas the CD56DIM subset contained higher levels of perforin and granzyme A (26). In addition, NK cell differentiation and function are influenced by tissue environment. Specific cellular and molecular environments in the uterus, liver, spleen, lungs or blood influence the precise nature of NK cells. Furthermore, differences have been noticed between species. However, it should be mentioned that most studied human and murine NK cells are generally derived from different compartments. Most parameters of human NK cells have been acquired from cells derived from the blood compartment, whereas murine NK cells are mostly derived from spleen. It is interesting to note that the blood environment in mice and humans are greatly different, with murine plasma favoring the resilience of mice to bacterial infection (27).
BACTERIAL SENSING BY NK CELLS AND EXPRESSION OF PRRS
A large part of the knowledge on TLR expression in human NK cells was initially acquired in studies on the basis of mRNA detection. In human NK cells, divergent observations were reported. In pooled purified NK T cell–like (NKT cell–like) and NK cells (CD3+CD56+ and NK CD3−CD56+, respectively), the expression of all TLR mRNA (TLR1–9) was found (28), but in isolated NK cells, mRNA expression levels of TLR1 were highest, followed by moderate levels of TLR2, TLR3, TLR5 and TLR6 (29). One group demonstrated a lack of TLR9 mRNA expression in two different sorted populations (NKT cell–like CD3+CD56+, NK CD3−CD56dim and NK CD3−CD56bright) (10). Regarding murine NK cells, divergences in mRNA expression were also reported. One study reported that all TLR mRNAs were expressed in splenic murine NK cells (30), whereas in the other, only TLR2, TLR4, TLR8 and TLR9 were found, but not TLR3 and TLR7 (31).
Of course mRNA expression is not always a reflection of the protein expression, because of posttranscriptional, translational and posttranslational events. Furthermore, cellular localization may also influence the cell surface expression. Studying human uterine NK cells, Eriksson et al. (32) showed that TLR2 was not localized on the cell surface but was expressed intracellularly. For circulating human NK cells, the surface expression of this receptor remains controversial. Flo et al. (33) failed to detect TLR2 expression by flow cytometry on a freshly isolated human NK cell surface using two different monoclonal antibodies. In contrast, Becker et al. (34) showed that after 24 h of culture, purified NK cells displayed TLR2 surface expression, as revealed by staining with a polyclonal antibody. Interestingly, TLR3 expression by human NK cells was shown to be expressed both on the cell surface (35) and intracellularly (36). TLR9 was found either in all human blood NK cells (36) or only in a small subpopulation, of which the percent could be increased after yellow fever vaccination (37). Concerning mouse spleen NK, a recent study showed that cell surface expression of TLR2 was present on ~65% of negatively selected freshly isolated NK cells and was not significantly modified after 48 h of culture in the presence of IL-2 and IFN-α with or without the Vaccinia virus (31).
The presence of any TLRs can be demonstrated indirectly by the activation of NK cells by TLR agonists (Table 1). For example, flagellin, the ligand of TLR5, favors NK cell recruitment in lymph nodes, upregulates CD69 expression on NK cells and induces NK-cell proliferation and IFN-γ production (38). In contrast, flagellin abrogates cytosine–phosphate–guanine (CpG) oligonucleotide-induced cytolytic activity of NK cells (39). However, CpG oligonucleotide, a TLR9 ligand, failed to directly activate isolated NK cells (28,29) because most of these activations are accessory cells and/or accessory cytokine- dependent (see below).
Table 1.
Response of NK cells to TLR agonists and other PAMPs.
| Bacteria or bacterial PAMPs | PRRs | Experimental settings | Species | Nature of NK cell activation | Reference |
|---|---|---|---|---|---|
| Legionella pneumophila | ND | MØ or IL-2 | m | Cytotoxicity, IFN-γ production | Blanchard et al. Infect Immun., 1988, 56, 1187a |
| LPS | ND | PBMC | h | Cytotoxicity | Conti et al. J. Immunol. 1991, 73, 450 |
| S. aureus | ND | PBMC | h | CD25 and CD69 expression, IFN-γ production | Yoshihara et al. Infect. Immun. 1993, 61, 3117 |
| L. monocytogenes | ND | SCID splenocytes + peritoneal MØ | m | IFN-γ production | Tripp et al. PNAS 1993, 90, 3725 |
| Mycobacterium bovis BCG | ND | Spleen cells | m | IFN-γ production | Yang et al. J. Immunol. 1995, 155, 5728 |
| E. coli DNA | ND | in vivo | m | IFN-γ production | Cowdery et al. J. Immunol. 1996, 156, 4570 |
| E. coli DNA | ND | + MØ or IL-12 | m | IFN-γ production | Chace et al. Clin. Immunol. Immunopathol. 1997, 84, 185 |
| LPS | ND | in vivo | m | IFN-γ production | Nguyen et al. J. Immunol. 1999, 162, 5238 |
| E. coli, Lactobacillus | ND | + MØ | h | CD25 and CD69 expression, IFN-γ production, proliferation | Haller et al. Infect. Immun. 2000, 68, 752 |
| CgG oligonucleotide | TLR9 | pDC or pDC supernatant | h | CD69 expression | Hornung et al. J. Immunol. 2002, 168, 4531 |
| Poly(I:C) | TLR3 | IL-2 or IL-12 | h | Cytotoxicity, CXCL10 and IFN-γ production | Pisegna et al. Blood. 2004, 104, 4157 |
| K. pneumoniae OmpA, flagellin | TLR2 and TLR5 | ± IL-1, IL-2, IL-12, IL-15, IFN-α | h | IFN-γ and α-defensin production | Chalifur et al. Blood. 2004, 104, 1778 |
| Poly(I:C) and CpG | TLR3 and TLR9 | + IL-12 or IL-8 | h | CD69 and CD25 expression, cytotoxity, IFN-γ and TNF production | Sivori et al. PNAS. 2004, 101, 10116 |
| L. monocytogenes | ND | in vivo | m | IFN-γ production | Thäle et al. Immunobiology. 2005, 210, 673 |
| H. pylori lysates | ND | IL-12 | h | IFN-γ production | Yun et al. Infect. Immun. 2005, 73, 1482 |
| Flagellin | ND | in vivo, in vitro ± DC | m | CD69 expression, IFN-γ production proliferation | Tsujimoto et al. J. Leuk. Biol. 2005, 78, 888 |
| Secreted mycobacterial (proteins ESAT-6 and MPP14) | ND | Bovine whole blood or PBMC | b | IFN-γ production | Olsen et al. Infect. Immun. 2005, 73, 5628 |
| Peptidoglycan, poly(I:C) LPS, flagellin | TLR2, -3, -4, -5 | IL-2 | h | IFN-γ production and cytotoxity | Lauzon et al. Cell. Immunol. 2006, 241, 102 |
| Lactobacillus casei | ND | + MØ or IL-12 | h | Cytotoxicity | Takeda et al. Clin. Exp. Immunol. 2006, 146, 109 |
| Poly(I:C), loxoribine | TLR3 and TLR7 | IL-12 | h | IFN-γ production and cytotoxity | Girart et al. J. Immunol. 2007, 179, 3472 |
| Peptidoglycan, poly(I:C) (loxoribine) | TLR2, -3 and -7 | IL-12 | m | IFN-γ production and cytotoxity | Sawaki et al. Int. Immunol. 2007, 19, 311 |
| M. tuberculosis | TLR2 + TLR4 | IL-12 + APC contact | h | IFN-γ production | Schierloh et al. Infect. Immun. 2007, 75, 5325 |
| M. bovis | TLR2 | ± IL-12 | h | CD69 and CD25 expression, IFN-γ and TNF production | Marcenaro et al. Int. Immunol. 2008, 20, 1155 |
| MDP | NOD2 | IL-12 or IFN-α | h | CD69 expression, IFN-γ production | Athie-Morales et al. J. Immunol. 2010, 185, 2080 |
| CgG oligonucleotide | TLR9 | Infected MØ | m | Control of intracellular bacterial growth | Elkins et al. Microbes Infect. 2009, 11, 49 |
| Poly(I:C) | RIG-like receptor not TLR3 | IL-12 and IFN-α | h | IFN-γ production and cytotoxity | Perrot et al. J. Immunol. 2010, 185, 1379 |
| E. coli Fimbriae FimH | TLR4 agonist | IL-2 | m and h | CD69 expression, cytotoxity and IFN-γ production | Mian et al. Mol. Ther. 2010, 18, 1379 |
| H. pylori (HpaA lipoprotein) | TLR2 | IL-12 | h | IFN-γ production | Lindgren et al. Innate Immun. 2010, 17, 191 |
| Diacyl lipopeptide | TLR2 | + BMDC contact | m | IFN-γ production and cytotoxity | Azuma et al. PLoS One. 2010, 5, e12550 |
| Lactobacillus acidophilus | ND | PBMC | h | Cytotoxicity and granule exocytosis | Cheon et al. Immunol. Lett. 2011, 136, 171 |
ND, not determined; PBMC, human peripheral blood mononuclear cells; MØ, monocytes or macrophages; pDC, plasmacytoid dendritic cells; APC, antigen presenting cells; BMDC, bone marrow derived dendritic cells; b, bovine; h, human; m, murine.
The second number in each reference citation indicates the volume; the last number indicates the beginning page number.
The method for NK cell purification is a technical limitation that can explain some of the controversial observations. Often used, the positive selection with magnetic microbeads may either induce cellular activation and modification of cell surface marker expression (40) or be associated with the presence of contaminating dendritic cells (41). Divergent results are similarly obtained in vivo depending on the antibody used for NK cell depletion (42). For example, in vivo cell depletion with anti-NK1.1 antibodies leads to the elimination of both NK and NKT cells, whereas the use of the anti–asialo monosialotetrahexosylgan-glioside (GM1) antibody depletes NK cells and basophils (43). Thus, the purification method (and possible cellular activation) may indeed contribute to the controversial reports published when studying the expression of TLRs in NK cells. Furthermore, analysis performed either extemporaneously or after cell culture can also lead to divergent results.
Others PRRs have been expressed by NK cells, including the families of cytoplasmic sensors, the NOD-like receptors (NLRs) and the retinoic acid inducible gene I (RIG-I)-like receptors. NLRs include NOD1, NOD2 and NOD-like receptor family, pyrin domain containing 3 (NLRP3). NOD1 is a receptor for small motifs derived from peptidoglycan, such as diaminopimelic acid-containing muramyl tripeptide (mur-tri-DAP), more frequently found among gram-negative bacteria. NOD2 is a receptor for muramyl dipeptide (MDP), the smallest active part of peptidoglycans from both gram-negative and gram-positive bacteria. NLRP3 is a key member of the in-flammasome and a sensor for many toxic agents. Human NK cells express high levels of intracellular NOD2, and NLRP3, whereas NOD1 is expressed at very low levels (36). Human NK cells naturally internalize MDP, which together with IFN-α and IL-12 stimulate the secretion of IFN-γ (44). Studies on the activation of NK cells by synthetic double-strand RNA (poly I:C) led to the conclusion that RIG-I–like receptor expression but not TLR3 was involved in NK cell activation (45). The use of mice deficient for MDA5 (another member of the RIG-I–like receptor family, a key intracellular sensor of double-stranded RNA), and that of mice deficient for interferon-promoter stimulator-1 (an adaptor molecule of the MDA5 pathway), led to the conclusion that this pathway was mainly involved in accessory cells (46,47).
In addition, toxins released by bacteria can directly activate NK cells. Some of them are known as superantigens. In 1982, we showed for the first time that the streptococcal erythrogenic toxin, renamed streptococcal pyrogenic exotoxin A (SPEA) later, was able to induce in vivo circulating IFN-γ (48). The first link of this toxin with NK cells was probably reported in 1991 by Sacks et al. (49), who showed that SPEA increased NK cell cytotoxic activity. The capacity of SPEA to activate NK cells and induce IFN-γ was further confirmed (50). Staphylococcal enterotoxin B is another superantigen able to induce the release of IFN-γ by purified NK cells (51). In contrast to staphylococcal enterotoxin B, studies suggest that NK cells were not directly activated by staphylococcal enterotoxin A. Staphylococcal enterotoxin A–activated T cells and monocytes contribute to the cytokine environment required for the activation of NK cells (52,53). A similar observation was reported for listeriolysin O, a cytolytic virulence factor of Listeria monocytogenes that induced IFN-γ production by NK cells through the stimulation by IL-12 and IL-18 produced by macrophages (54). The exotoxin A produced by Pseudomonas aeruginosa was shown to activate in vivo NK cell cytotoxicity (55). In contrast, in vitro studies on peripheral blood mononuclear cells revealed that P. aeruginosa exerts an inhibitory action on NK cells, preventing IFN-γ production and cytotoxicity (56).
If NK cells are key actors of the innate immune defense, it makes sense that some pathogens have developed strategies to limit the action and activation of these cells. This is the case of the leukotoxin produced by Actinobacillus actino-mycetemcomitans, which inhibits the up-regulation of cell surface markers associated with NK cell activation (57). More drastically was the case of Yersinia pestis, in which the yersinial outer membrane protein-11 (YopM) molecule, a 41.5-kDa virulence protein, interferes with innate immunity by causing a global depletion of NK cells, possibly by affecting the expression of IL-15 receptor α and IL-15 (58).
NK CELLS AS A SOURCE OF INFLAMMATORY CYTOKINES AND ANTIMICROBIAL MEDIATORS
NK cells produce cytokines that contribute to the inflammatory environment during an infection. IFN-γ, granulocyte-macrophage colony-stimulating factor (GM-CSF), and tumor necrosis factor (TNF)-α are the main cytokines generated by activated NK cells (24,59). For example, in the cecal ligation and puncture (CLP) model of polymicrobial peritonitis, it was established that liver NK cells were the main source of IFN-γ (60). Whether these cytokine productions are accessory cell–dependent remains a controversial issue. Nonetheless, there are numerous reports showing that purified NK cells can directly respond to PAMPs in the absence of accessory cells, but in the presence of cytokines such as IL-2, IL-12, IL-15 or IL-18 (see Table 1). Whereas most cytokines are undetectable in the bloodstream of healthy subjects during homeostasis, there is a low and different expression in various tissues. This expression creates a microenvironment that modulates the precise nature of different NK cells. During infection and sepsis, a large panel of cytokines is generated, offering NK cells the appropriate environment to respond to PAMPs, allowing contribution to the cytokine cascade and eventually to the cytokine storm (1,61).
Activation of NK cells can lead to different changes including cytotoxity associated with the release of perforin and granzyme and the production of cytokines. The secretion of cellular granules containing cytotoxic mediators (for example, perforin and granzyme) and cytokines (for example, IFN-γ) are not achieved similarly. The release of cytotoxic molecules is polarized toward a target cell, whereas that of cytokines is not (62). NK cells can be rapidly activated by some of the cytokines present in the early stages of infection, such as IL-12, IL-15 or IL-18, allowing the secretion of large amounts of IFN-γ and GM-CSF. NK cells also generate other cytokines such as IL-5 (63), IL-6 (64), IL-10 (65,66), transforming growth factor (TGF)-β (67), IL-12 (68), IL-13 (69), IL-16 (25), IL-17 (70) and IL-22 (71). Similarly, NK cells are source of various chemokines such as XCL1, CCL1, CCL2 and CXCL16 (72); CXCL8, CCL8, CCL26 and CCL17 (25); CXCL10 (73); CCL3 and CCL4 (74); and CCL5 (75). NK cells also release soluble TNF-α (76) and express its membrane form (77), as well as other members of the TNF family (that is, lymphotoxin [LT]-α, LT-β, Fas ligand, CD27L, CD30L, OX40L, 4-1BB ligand (4-1BBL), TNF-related apoptosis-inducing ligand (TRAIL) and LIGHT (homologous to lymphotoxins, exhibits inducible expression, competes with HSV glycoprotein D for HVEM, a receptor expressed on T-lymphocytes) (72,78).
The fact that NK cells are an important source of proinflammatory cytokines, particularly IFN-γ, illustrates how these cells are both contributing to the antiinfectious process and amplifying the inflammatory response that can lead to organ failure and death, as seen in polymicrobial sepsis. NK cells have been identified in numerous studies as the main source of IFN-γ during infection by different bacterial pathogens such as Francisella tularensis (79), L. monocytogenes (80–82), Chlamydia pneumoniae (83), and Yersinia enterocolitica (84) and in experimental endotoxin-induced lethal shock (85) and polymicrobial sepsis (86) (Tables 1 and 2). The protective role of IFN-γ was shown in murine salmonellosis, particularly in synergy with TNF-α when injected 6 h before S. typhimurium (87). This beneficial role was also demonstrated in IFN-γ receptor–deficient mice, which were more sensitive to group B Streptococcus (88) or to ascendens stent peritonitis (89) than wild-type mice. In contrast, neutralization of IFN-γ prevented lethality in primate gram-negative bacteriemic shock (90) and protected mice infected intravenously with Staphylococcus aureus (91). The deleterious role of IFN-γ was demonstrated by its capacity to increase death when injected in mice, particularly when acting in synergy with TNF-α (12). This deleterious effect was also shown in the CLP model of polymicrobial peritonitis (92) and in a CLP model followed by a P. aeruginosa infection (93). Polymicrobial peritonitis performed in IFN-γ receptor–deficient mice (94) or in rats given anti–IFN-γ antibodies (95) led to the similar demonstration of this negative role. In mice injected with LPS, the ambiguous role of IFN-γ was demonstrated: IFN-γ protected against LPS- induced lung edema but acted in synergy with LPS to enhance the occurrence of death (96).
Table 2.
Some examples of cellular crosstalk allowing NK cell response during bacterial infections or PAMP challenge.
| Cellular crosstalk with NK cells and type of infection or activation | NK cell functions | References |
|---|---|---|
| Dentritic cells | ||
| LPS | Proliferation, cytotoxicity, IFN-γ production | Goodier et al. J. Immunol. 2000, 165, 139a |
| LPS or M. tuberculosis | CD69 expression, IFN-γ production | Gerosa et al. J. Exp. Med. 2002, 195, 327 |
| TLR3, -4, -7 and -9 agonists | IFN-γ production and cytotoxicity | Lucas et al. Immunity. 2007, 26, 503 |
| L. monocytogenes | IFN-γ production | Lucas et al. Immunity. 2007, 26, 503; Kang et al. Immunity. 2008, 29, 819; Humann and Lenz. J. Immunol. 2010, 184, 5172 |
| Pam2Cys lipopeptides | CD69 expression, cytotoxicity and IFN-γ production | Azuma et al. PLoS One. 2010, 5, e12550 |
| Chlamydia muridarum | IFN-γ production | Jiao et al. J. Immunol. 2011, 187, 401 |
| Monocytes/macrophages | ||
| CpG DNA | IFN-γ production | Chace et al. Clin. Immun. Immunopathol. 1997, 84, 185 |
| Legionella pneumophila | IFN-γ production and cytotoxicity | Blanchard et al. Infect. Immun., 1988, 56, 1187 |
| L. monocytogenes | IFN-γ production | Wherry et al. Infect. Immun. 1991, 59, 1709; Tripp et al. PNAS. 1993, 90, 3725 |
| P. aeruginosa exotoxin A | IFN-γ production and cytotoxicity | Michalkiewicz et al., Immunol. Lett. 1999, 69, 359 |
| S. aureus; L. johnsonii | CD69 expression, IFN-γ production | Haller et al. Clin. Diag. Lab. Immun. 2002, 9, 649 |
| LPS | CD69 expression | Scott et al. Clin. Exp. Immunol. 2004, 137, 469 |
| TLR2, -3 and -4 agonists | IFN-γ production | Tu et al. J. Exp. Med. 2008, 205, 233 |
| Salmonella | CD69 expression, cytotoxicity and IFN-γ | Lapaque et al. J. Immunol. 2009, 182, 4339 |
| Kupffer cells | ||
| TLR2, -3 and -4 agonists | IFN-γ production | Tu et al. J. Exp. Med. 2008, 205, 233 |
| Poly I:C + D-GalN in vivo | IFN-γ production | Hou et al. Hepatology. 2009, 49, 940 |
| Neutrophils | ||
| Legionella | IFN-γ production | Sporri et al., J. Immunol. 2008, 181, 7121 |
| LPS + IL-2 or IL-15/IL-18 | IFN-γ production | Costantini et al. Blood. 2011, 117, 1677 |
| T-lymphocytes | ||
| Staphylococcal enterotoxin B–activated T cells | IFN-γ production and cytotoxicity | D’Orazio et al. J. Immunol. 1995, 154, 1014 |
| LPS-treated γδ T cells | IFN-γ production | Andrews et al. Immunol. Cell. Biol. 2011, 89, 739 |
| B-lymphocytes | ||
| L. monocytogenes | IFN-γ production | Bao et al. Eur. J. Immunol. 2011, 41, 657 |
| Mast cells | ||
| LPS, Poly(I:C), CpG | IFN-γ production | Vosskuhl et al. J. Immunol. 2010, 119, 25 |
| Epithelial cells | ||
| Chlamydia trachomatis | IFN-γ production | Hook et al. FEMS Immunol. Med. Microb. 2005, 45, 113 |
The second number in each reference citation indicates the volume; the last number indicates the beginning page number.
NK cells were also recognized as a source of α-defensins and cathelicidin (LL37), well-known antibacterial peptides (97). NK cells can also generate indoleamine 2,3-dioxygenase (IDO) and nitric oxide (NO), two other mediators known to limit the infectious process (98,99). So far, the generation of IDO by NK cells has not been demonstrated in the context of bacterial infection, but has been in a transplantation model after IL-4 treatment (100). Similarly, the production of NO has not been demonstrated in infectious models, but rather in response to IL-2 (101), IL-12 and TNF-α (102). In both cases, the authors showed activation of inducible NO synthase. In addition, NK cells express endothelial NO synthase and thus can constitutively produce NO (103). Most interestingly, it was recently shown that NK cells can also be a source of resolvin E1, suggesting that they can also contribute to the resolution phase of inflammation (104).
NK CELLS AND ACCESSORY CYTOKINES
Despite the fact that NK cells are equipped to recognize bacterial patterns, it is well established that accessory cells contribute both indirectly (through soluble factors) and directly (through cell-to-cell contact) to trigger the cellular response. Several studies have demonstrated the NK cell activation by TLR agonists can occur in the absence of accessory cells but in the presence of their soluble cytokines. IL-2, IFN-α/β, IL-12, IL-15, IL-18 and IL-21 are the main cytokines that trigger NK cells, either alone or in a synergistic combination (105,106). Other cytokines have also been reported to amplify the survival, the proliferation, the IFN-γ production or the cytotoxicity of NK cells. This is the case for TNF-α (107), IL-4 (100,108), IL-1β (109), IL-7 (71), IL-23 (110) and IL-33 (111). NK cells respond to chemoattractant signals delivered by numerous chemokines, particularly CCL2 (macrophage-chemoattractant protein [MCP]-1), CCL3 (macrophage inflammatory protein [MIP]-1α), CCL4 (MIP-1β), CCL5 (regulated upon activation, normal T-cell expressed and [presumably] secreted [RANTES]), CCL7 (MCP-3), CCL8 (MCP-2) and CXCL10 (interferon γ–induced protein [IP]-10) (112). In the case of CCL6 (C10), transgenic mice overexpressing this chemokine were shown to be protected against an otherwise lethal CLP, associated with an enhanced recruitment of NK cells in the peritoneal cavity (113). Furthermore, these chemokines enhance the cytolytic response of NK cells. Whereas IL-15 is the prerequisite cytokine for NK cell maturation and differentiation from bone marrow cells (114), it is also required for an optimal IFN-γ production (115). Interestingly, IL-15 can be delivered to NK cells in a trans-presentation manner (116,117). IL-15 and IL-2 share a common receptor chain (IL-2Rβ) (118), and NK cells are also responsive to IL-2 (119). Such a responsiveness is not only an illustration of the crosstalk between NK cells and T lymphocytes, the main source of IL-2, but also with dendritic cells (DCs), which have been shown to contribute to NK cell activation through the release of IL-2 (120). IL-12 was recognized as an important cytokine to fight infectious diseases (121,122), particularly through its capacity to induce IFN-γ production, as shown in mice infected with Y. enterocolitica (84) or S. typhimurium (123). Salmonella was also shown to induce the production of IL-1β and IL-23 by macrophages favoring the production of IFN-γ by NK cells (124). A similar synergy between IL-1β and IL-12 leading to an enhanced production of IFN-γ was also reported in response to LPS and L. monocytogenes (109). It is interesting to note that in return, IFN-γ can favor the production of IL-12, as shown during the activation of macrophages by Mycobacterium bovis (125). Similarly, IL-18, known to contribute to the antiinfectious response and neutralization during an infection with Y. enterocolitica or S. typhimurium, was shown to be deleterious (126). This study suggested that the role of IL-18 depends on its capacity to induce the production of IFN-γ. In IL-18–deficient mice injected with Propioni-bacterium acnes, IFN-γ production in response to LPS was markedly reduced and NK cell activity was significantly impaired (127). Interestingly, during infection, MyD88-deficient NK cells fail to produce IFN-γ (128). Because MyD88 is a signaling molecule shared by most TLR and also by IL-18 receptor, it is conceivable that its absence could affect both pathways during an immune response to infection. The use of IL-12/IL-18 double KO mice and combined experiments with anti–IL-12 and anti–IL-18 antibodies demonstrated that both IL-12 and IL-18 cooperate to activate NK cells (127,129). A recent report showed that IL-18 primes NK cells to become responsive to IL-12 and to release IFN-γ (130). A coordinated action with other cytokines such as IFN-α/β has been demonstrated during viral infection. TLR4 agonists can also generate the release of IFN-α/β; it is most probable that IFN-α/β also contributes to the activation of NK cells during bacterial infection (131).
Of course, NK cells are also responsive to antiinflammatory mediators such as IL-4 (106), IL-10 (132), TGF-β (133), prostaglandin E2 (134,135), prostaglandin D2 (136) and glucocorticoids (137,138). In mice, in vivo blocking of IL-10 reverted the hyporesponsive status of NK cells in the lungs or the liver (139,140). In patients with chronic hepatitis B virus infection, in ex vivo experiments, blockade of IL-10 or TGF-β restored the altered capacity of NK to produce IFN-γ (141). However, IL-10 may not always be a direct inhibitor for NK cells. Particularly, IL-10 was shown to enhance IL-18–induced IFN-γ production and IL-18– and IL-12–induced NK cell cytotoxicity and proliferation (142,143). Such a paradoxical effect of IL-10 was confirmed when regulatory DCs were added to NK cells (144). These cocultures led to enhanced NK cell–dependent cytotoxicity and IFN-γ production. When regulatory DCs were derived from IL-10 KO mice, their amplificatory role was significantly lower.
NK CELLS WITHIN A CELLULAR CROSSTALK
The activation of NK cells in bacterial infection has often been linked to a cellular crosstalk with accessory cells that allows NK cell activation after direct interaction or accessory and NK cells with PAMPs (145). Several accessory cells have been described as a source of activating signals for NK cells, such as DCs, polymorphonuclear neutrophils, macrophages, mast cells, epithelial cells and B and T lymphocytes, including regulatory T-cells (Tregs) (see Table 2).
In vitro production of IFN-γ by spleen cells stimulated with S. typhimurium requires the help of adherent cells or adherent cell-derived factors (146). In this early study, NK cells were not identified as a source of IFN-γ, and adherent cells could have been either DCs or macrophages, making this report among the first to demonstrate that a cellular crosstalk was required for IFN-γ production. Since then, the requirement of accessory cells for NK cell activation was well documented (see Newman and Riley [145] for a review). DCs were identified as a key partner for NK cells, particularly because they are a major source of IL-12 and can also produce IL-15, IL-18 and IFN-α (11,147). For example, proliferation, cytotoxic activity and IFN-γ production by LPS-stimulated NK cells depended on major histocompatibility complex (MHC) class II+ B7+ CD14− accessory cells, most probably DCs (148). Studying the response of NK cells to L. monocytogenes, it was demonstrated that both cytokines and cell contact with infected DCs were required for optimal IFN-γ production by NK cells (149). CX3CL1 (fractalkine) expressed on mature DCs is another player in the synapses formed between DCs and NK cells (150). Such contact was visualized by clustering of DCs, not only with NK cells, but also with granulocytes and monocytes/macrophages (151) and involved the priming of NK cells by IFN-α/β and a trans-presentation of IL-15 (147).
Although the contribution of monocytes was shown to counteract the effects of DCs (148), other reports demonstrated a positive effect of monocytes/macrophages. For example, in Legionella pneumophila or L. monocytogenes infection, macrophages favored the production of IFN-γ by NK cells (152,153). In vitro, the presence of macrophages was fundamental for the expression of CD69 by NK cells in the presence of LPS (154). Crosstalk between human NK cells and macrophages infected with intracellular Salmonella was also demonstrated. These macrophage-activated NK cells caused the secretion of IFN-γ and degranulation. The NK cell activation required the release of IL-2, IL-12, IL-15 and IL-18 and contact between NK cells and infected macrophages (155). Liver macrophages (Kupffer cells) were also shown to crosstalk with NK cells during activation in the presence of TLR2, TLR3 or TLR4 agonists, either in vitro or in vivo (156,157). The activation was shown to depend on IL-18 and cell-to-cell contact. Similar to the reciprocal activation identified between DCs and NK cells (158), the crosstalk between macrophages and NK cells is bidirectional. For example, NK cells promote phagocytosis of Escherichia coli by the macrophages through a CD40/CD154 interaction (154). NK cell activation leads to a dramatic reduction in the number of intramacrophagic live Salmonella (155). In a CLP model of peritonitis, macrophage phagocytosis, NO production and IL-6 levels were decreased in NK cell–depleted mice compared with controls (159). Indeed, coculture of NK cells and macrophages significantly increased activation levels of both cell types, an activation determined to be cell-to-cell contact–dependent (154). Of note is that the activation of monocyte and macrophages by TLR agonists leads to the expression of MHC class I–related chain A (MICA), a ligand for NK group 2 (NKG2) of receptors, member D (NKG2D) and the ligand for the NKG2D receptor, constitutively expressed on all NK cells (160,161). The NKG2D receptor is expressed predominantly on NK cells, NK T cells and T cells. This receptor recognizes infected cells through surface ligand expression on stressed cells. The proposed role of the NKG2D receptor in innate immune responses to cellular and tissue stress is based on the ability of the receptor to stimulate cytotoxic effects of NK and T cells and the production of IFN-γ and TNF-α. In P. aeruginosa lung infection, NKG2D is also involved in epithelial cell sloughing (162), whereas on the other hand, IFN-γ production by NK cells and bacterial clearance depends on the NKG2D ligand (163).
Neutrophils are central players during innate immunity against infection. Their interaction with NK cells is not surprising. During L. monocytogenes infection, granulocytes produce IL-12 and favor IFN-γ production by NK cells (164). During L. pneumophila infection, neutrophils immediately produce IL-18, which is indispensable for NK cell activation (165). As mentioned above for macrophages, NK cells can also activate neutrophils and promote their survival; upregulate cell surface expression of CD64, CD11b and CD69; and enhance the production of superoxide anions and heparin-binding epidermal growth factor (166). This property observed when NK cells were exposed to IL-15 and IL-18 partially depended on their production of GM-CSF. The detailed nature of the bidirectional crosstalk between neutrophils and NK cells is now provided in an extensive review (167).
Similarly, mast cells are key actors of innate immunity, thanks to their capacity to release preformed cytokines, particularly TNF-α (168). It was reported that, in the presence of agonists for TLR3, TLR4 and TLR9, mast cells in coculture experiments stimulated NK cells to produce IFN-γ in a contact-dependent and TNF-α–independent manner (169).
Lymphocytes also interact with NK cells. B-lymphocytes were recognized long ago as accessory cells for the production of IFN-γ by NK cells (170). In return, IFN-γ inhibits polyclonal B-cell proliferation but favors the IgG2a response (171). Recently, it was reported during a L. monocytogenes infection that a subpopulation of B-lymphocytes (PDCA-1+ Siglec-H− CD19+) activated NK cells via secretion of IFN-α (172). T lymphocytes also dialogue with NK cells in a reciprocal fashion. For example, NK cells derived from pleural fluids of patients with tuberculosis pleurisy induce T-lymphocyte activation through ICAM-1 engagement (173). After lethal injection of LPS, IL-18 was shown as fundamental to trigger γδT cells to produce IL-17A, which together with IL-18, contribute to the IFN-γ production by NK cells (174). Tregs constitute another T-cell subtype characterized as CD4+CD25+Foxp3+ and able to secrete antiinflammatory cytokines (for example, IL-10 and TGF-β1) and thus behaving as suppressor cells. Alteration of the immune system after sepsis is in part consecutive to the action of Tregs (175). Tregs and their cytokines behave as inhibitors of NK cell function (cytotoxicity and IFN-γ production) (176,177). Of course, cells other than Tregs can down-regulate NK cell function through the production of IL-10, despite its contradictory properties on NK cells (see above); this is particularly the case of macrophages (148) and B-lymphocytes (178). Myeloid-derived suppressor cells can impair NK cell development and function (179) as well as Kupffer cells (156) and alveolar macrophages (135) via the release of IL-10, TGF-β or prostaglandin E2.
Most interestingly, nonimmune cells can release NK-activating cytokines. This is the case of epithelial cells, which on infection with Chlamydia trachomatis can release IL-18, thus favoring the production of IFN-γ by NK cells (180). In addition, epithelial cells upon infection can increase their expression of NKG2D ligand, thus favoring a crosstalk with NK cells (162).
BENEFITS VERSUS DISADVANTAGES OF NK CELL ACTIVATION DURING BACTERIAL INFECTION
As previously mentioned, NK cells are closely associated with both the fight against bacterial infection and the damages associated with an overzealous inflammatory response. According to experimental models, a beneficial or a deleterious contribution has been attributed to NK cells (Table 3). For example, when L. monocytogenes infection was investigated, Dunn and North (181) showed that the early production of IFN-γ by NK cells was essential for resistance to listeriosis. In contrast, Teixeira and Kaufmann (80) reported that NK cell depletion led to an enhanced listerial clearing. The fact that the route of infection (subcutaneous and intravenous, respectively) and the mouse strains were different may explain such a discrepancy. Indeed, it was proposed that CD8+ T lymphocytes may play a more important role than NK cells after intravenous L. monocytogenes infection (81). In addition, phenotypic differences in NK cells were illustrated in C3H/HeN and BALB/c mice with P. aeruginosa chronic lung infection (182).
Table 3.
Examples of the half-angel half-devil role of NK cells during bacterial infections.
| Role of NK cells and experimental model | Proof for NK cell role | Reference |
|---|---|---|
| Beneficial | ||
| M. avium | NK cell lysis of infected monocytes, NK cell lysis of infected macrophages, Anti-NK1.1 depletion | Katz et al. J. Clin. Immunol. 1990, 10, 71a; Bermudez et al. J. Leuk. Biol. 1990, 47, 135; Harshan et al. Infect. Immun. 1991, 59, 2818 |
| Mycobacterium lepraemurium | NK cell lysis of infected macrophages | Denis Int. J. Immunopharmacol. 1991, 13, 881 |
| Mycobacterium tuberculosis | Lysis of infected MØ by NK cells, Rag KO mice | Vankayalapati et al. J. Immunol. 2005, 175, 4611; Feng et al. J. Immunol. 2006, 177, 7086 |
| Mycobacterium bovis | IL-15 transgenic mice, reduced intracellular bacterial growth | Umemura et al. J. Immunol. 2001, 167, 946; Denis et al. Tuberculosis. 2007, 87, 53 |
| L. monocytogenes | Anti–NK cell depletion | Dunn and North Infect. Immun. 1991, 59, 2892 |
| S. typhimurium | Anti–asialo GM-1 depletion | Schafer et al. Infect. Immun. 1992, 60, 791 |
| Salmonella choleraesuis | Anti–IL-15 administration | Hirose et al. J. Leuk. Biol. 1999, 66, 382 |
| Salmonella enterica | Anti-NK1.1 depletion | Ashkar et al. Infect. Immun. 2009, 77, 214 |
| Chlamydia trachomatis | Anti–asialo GM-1 depletion, lysis of infected epithelial cells | Tseng et al. Infect. Immun. 1998, 66, 5867; Hook et al. Clin. Exp. Immunol. 2004, 138, 54 |
| Chlamydia muridarum | Anti–asialo GM-1 depletion | Jiao et al. J. Immunol. 2011, 187, 401 |
| Staphylococcus aureus | Anti-NK1.1 depletion, IL-15 KO mice | Nilsson et al. Clin. Exp. Immunol. 1999, 117, 63; Small et al. J. Immunol. 2008, 180, 5558 |
| Polymicrobial peritonitis | Anti–asialo GM-1 depletion | Godshall et al. Shock. 2003, 19, 144 |
| Bordetella pertussis | Anti–asialo GM-1 depletion | Byrne et al. Eur. J. Immunol. 2004, 34, 2579 |
| Chlamydophila abortus | Anti–asialo GM-1 depletion | Buendia et al. J. Comp. Path. 2004, 130, 48 |
| Shigella flexneri | Rag KO mice | Le-Barillec et al. J. Immunol. 2005, 175, 1735 |
| Legionella pneumophila | Anti–asialo GM-1 depletion | Spörri et al. J. Immunol. 2006, 176, 6162 |
| Haemophilus influenza | IL-15 KO mice | Miyazaki et al. J. Immunol. 2007, 179, 5407 |
| Pseudomonas aeruginosa | NKG2D activation and bacterial clearance | Wesselkamper et al. J. Immunol. 2008, 1891, 5481 |
| Francisella tularensis | Anti–asialo GM1 depletion (granuloma formation) | Bokhari et al. Infect. Immun. 2008, 76, 1379 |
| Deleterious | ||
| Pseudomonas aeruginosa | Anti-NK1.1 depletion, role of NKG2D in epithelial cell injury | Newton et al. Nat. Immun. 1992, 11, 335; Borchers et al. Infect. Immun. 2006, 74, 2578 |
| L. monocytogenes | Anti-NK1 + depletion | Teixeira and Kaufmann J. Immunol. 1994, 152, 1873 |
| LPS-induced Shwarzman reaction | Anti-NK1.1 or anti–asialo GM-1 | Heremans et al. Eur. J. Immunol. 1994, 24, 1155 |
| LPS-induced lethal shock | NK1 + cells depletion | Emoto et al. J. Immunol. 2002, 169, 1426 |
| E. coli | Anti–asialo GM-1 depletion | Badgwell et al. Surgery. 2002, 132, 205 |
| Polymicrobial peritonitis | β2M KO + anti–asialo GM-1, anti-NK1.1 or anti–asialo GM-1 | Sherwood et al. Lab. Invest. 2004, 84, 1655; Etogo et al. J. Immunol. 2008, 180, 6334 |
| Severe sepsis | Enhanced levels of Granzyme | Zeerleder et al. Clin. Immunol. 2005, 116, 158 |
| Streptococcus pyogenes | Anti–asialo GM-1 depletion | Goldmann et al. J. Infect. Dis. 2005, 191, 1280 |
| Streptococcus pneumoniae | Scid mice + anti–asialo GM-1 | Kerr et al. Microbes Infect. 2005, 7, 845 |
| H. pylori | Increased infiltration of NK cells | Kuo et al. World J. Gastroenterol. 2005, 11, 4357 |
| Mycobacteria induced-colitis | IL-10 KO mice | Singh et al. BMC Immunol. 2008, 9, 25 |
| Ehrlichia chaffeensis | NK cell depletion | Stevenson et al. Am. J. Pathol. 2010, 177, 766 |
The second number in each reference citation indicates the volume; the last number indicates the beginning page number.
In the CLP model of peritonitis, NK cells were shown to contribute to the early local and systemic control of the bacterial burden (183). In this study, however, depletion of NK cells by anti–asialo GM1 antibodies did not significantly modify the survival curves. In contrast, NK cells contribute to the overzealous production of inflammatory cytokines associated with mortality of septic shock (86,184). Most interestingly, in the latter study, the beneficial effect of the deletion of NK cells by either anti–asialo GM1 or anti-NK1.1 antibodies was only seen when mice were treated with antibiotics. Furthermore, in this CLP model, when bacterial clearance was investigated, discordant results were obtained depending on the nature of the antibodies used for the NK cell depletion (42).
Deleterious effects of NK cell activation were reported after infection with both gram-negative (for example, E. coli [185] and Ehrlichia chaffensis [186]) and gram-positive bacteria (for example, Streptococcus pneumoniae [187] and Streptococcus pyogenes [188]) independent of the site of infection (systemic, peritoneal or pulmonary). Most interestingly, NK cells may also contribute to adverse evolution of the infectious diseases as shown by their association with a Helicobacter pylori–dependent state of early-stage high-grade gastric mucosa–associated lymphoid tissue lymphoma (189) and Mycobacteria-mediated colitis in susceptible hosts (190). Of course and as expected, NK cells contribute to the deleterious effects seen after LPS injections (85,191). Deleterious contribution of NK cells was also demonstrated in the case of murine polytrauma (192) and in the model of cytokine-induced fatal shock (193).
In contrast, numerous reports have clearly defined beneficial roles of NK cells in various models of bacterial infectious diseases (see Table 3). For example, the protective role of NK cells was demonstrated in infections induced by M. avium, M. lepraemurium or M. tuberculosis (20–23,194,195). The protective role of NK cells was also demonstrated in models of infection with different strains of Salmonella (196–198). Similarly, NK cells were shown to play a critical protective role against S. aureus in septic arthritis and pulmonary models of infection (199,200). In the later case, an elegant study revealed that H1N1 influenza virus infection leads to weakened NK cell activity, particularly in terms of TNF-α production, rendering the host more susceptible to a secondary lung infection by S. aureus (201). The defect of NK cells particularly affected the phagocytic function of alveolar macrophages.
IMMUNE STATUS OF NK CELLS DURING SEPSIS
In humans, sepsis is associated with a severe lymphopenia that also affects circulating NK cells (202). The decreased number of circulating NK cells persists over 1 wk (203). The most severe depletion of NK cells was found among the patients with the highest mortality (204). During sepsis, the “compensatory antiinflammatory response syndrome” is illustrated by a reprogramming of immune cells (205). Immune status of NK cells is also affected during sepsis. NK cell cytotoxic activity in adult and newborn sepsis patients was decreased (206–208). A similar observation was reported in trauma (209) and burn patients (210). It was suggested that circulating endotoxin is involved in the suppression of NK cell activity observed in burns (210). In the thermally injured patients with the most severe depressed levels of NK cell activity, IL-2 and IFN-α failed to amplify this response (211). Similar observations were reproduced in animal models after surgery or injection of LPS or other TLR agonists (212–214). Whereas these observations were reported for spleen and liver NK cells, the peak of the CLP-induced acute lung injury was associated with severe dysfunction of lung NK cells (215). In this study, the authors showed a decrease in cell cytotoxicity, a decrease of the percentage of perforin-positive NK cells and a decrease of IFN-γ–positive cells. We recently showed that IFN-γ and GM-CSF ex vivo productions were altered in splenic NK cells after polymicrobial sepsis murine model (CLP) (Souza- Fonseca-Guimaraes F, Parlato M, Fitting C, Cavaillon J-M, Adib-Conquy M. NK cell tolerance to Toll-like receptor agonists mediated by regulatory T cells after polymicrobial sepsis [submitted]). Enhanced apoptosis of spleen NK cells was reported after CLP and was reversed by injection of IL-15 (216).
CONCLUDING REMARKS
NK cells initially described for their role in immunosurveillance against tumor cells are fully part of the innate immune response against infection, whatever the type of pathogen (145). Unanswered questions remain: How do PAMPs activate NK cells? If the full signaling cascade downstream of TLRs is present, why do purified NK cells respond poorly to the PAMPs, and how do the accessory cytokines allow them to be activated? If some TLRs are not expressed on the cell surface, what type of PAMP internalization process allows their activation? A great number of intracellular molecules downregulate the TLR-dependent signaling pathways, providing negative signals to turn off cellular activation (217). Are these molecules also acting within NK cells, explaining their dysfunctions noticed in sepsis (207,215)? NK cells are able to release IDO and NO. Could these molecules be part of their arsenal to fight pathogens? Would it be possible in the future to act on NK cells, either to boost their beneficial role during infection or to limit their deleterious effects during sepsis or other acute inflammatory syndrome? In other words, would it be possible to limit the half-devil role of NK cells to only favor their half-angel side?
ACKNOWLEDGMENTS
The authors thank Brian Mozeleski for critical review and English corrections. F Souza-Fonseca-Guimaraes was supported by a Pasteur fellowship (Pasteur University International PhD Program).
Footnotes
Online address: http://www.molmed.org
DISCLOSURE
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
REFERENCES
- 1.Hargreaves DC, Medzhitov R. Innate sensors of microbial infection. J Clin Immunol. 2005;25:503–10. doi: 10.1007/s10875-005-8065-4. [DOI] [PubMed] [Google Scholar]
- 2.Kapetanovic R, Cavaillon JM. Early events in innate immunity in the recognition of microbial pathogens. Expert Opin Biol Ther. 2007;7:907–18. doi: 10.1517/14712598.7.6.907. [DOI] [PubMed] [Google Scholar]
- 3.Adib-Conquy M, Cavaillon JM. Stress molecules in sepsis and systemic inflammatory response syndrome. FEBS Lett. 2007;581:3723–33. doi: 10.1016/j.febslet.2007.03.074. [DOI] [PubMed] [Google Scholar]
- 4.Martinon F, Tschopp J. NLRs join TLRs as innate sensors of pathogens. Trends Immunol. 2005;26:447–54. doi: 10.1016/j.it.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Adib-Conquy M, Cavaillon JM. Compensatory anti-inflammatory response syndrome. Thromb Haemost. 2009;101:36–47. [PubMed] [Google Scholar]
- 7.Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005;365:63–78. doi: 10.1016/S0140-6736(04)17667-8. [DOI] [PubMed] [Google Scholar]
- 8.Monneret G, Venet F, Pachot A, Lepape A. Monitoring immune dysfunctions in the septic patient: a new skin for the old ceremony. Mol Med. 2008;14:64–78. doi: 10.2119/2007-00102.Monneret. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cavaillon JM, Adib-Conquy M. Monocytes/macrophages and sepsis. Crit Care Med. 2005;33:S506–509. doi: 10.1097/01.ccm.0000185502.21012.37. [DOI] [PubMed] [Google Scholar]
- 10.Chalifour A, et al. Direct bacterial protein PAMP recognition by human NK cells involves TLRs and triggers alpha-defensin production. Blood. 2004;104:1778–83. doi: 10.1182/blood-2003-08-2820. [DOI] [PubMed] [Google Scholar]
- 11.Beutler B, et al. Genetic analysis of resistance to viral infection. Nat Rev Immunol. 2007;7:753–66. doi: 10.1038/nri2174. [DOI] [PubMed] [Google Scholar]
- 12.Doherty GM, et al. Evidence for IFN-gamma as a mediator of the lethality of endotoxin and tumor necrosis factor-alpha. J Immunol. 1992;149:1666–70. [PubMed] [Google Scholar]
- 13.Kiessling R, Klein E, Pross H, Wigzell H. “Natural” killer cells in the mouse. II. Cytotoxic cells with specificity for mouse Moloney leukemia cells. Characteristics of the killer cell. Eur J Immunol. 1975;5:117–21. doi: 10.1002/eji.1830050209. [DOI] [PubMed] [Google Scholar]
- 14.Herberman RB, et al. Fc receptors on mouse effector cells mediating natural cytotoxicity against tumor cells. J Immunol. 1977;119:322–6. [PubMed] [Google Scholar]
- 15.Ojo E, Wigzell H. Natural killer cells may be the only cells in normal mouse lymphoid cell populations endowed with cytolytic ability for antibody-coated tumour target cells. Scand J Immunol. 1978;7:297–306. doi: 10.1111/j.1365-3083.1978.tb00457.x. [DOI] [PubMed] [Google Scholar]
- 16.Macfarlan RI, Burns WH, White DO. Two cytotoxic cells in peritoneal cavity of virus-infected mice: antibody-dependent macrophages and non-specific killer cells. J Immunol. 1977;119:1569–74. [PubMed] [Google Scholar]
- 17.Tagliabue A, Nencioni L, Villa L, Boraschi D. Genetic control of in vitro natural cell-mediated activity against Salmonella typhimurium by intestinal and splenic lymphoid cells in mice. Clin Exp Immunol. 1984;56:531–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Klimpel GR, Niesel DW, Klimpel KD. Natural cytotoxic effector cell activity against Shigella flexneri-infected HeLa cells. J Immunol. 1986;136:1081–6. [PubMed] [Google Scholar]
- 19.Blanchard DK, Stewart WE, 2nd, Klein TW, Friedman H, Djeu JY. Cytolytic activity of human peripheral blood leukocytes against Legionella pneumophila-infected monocytes: characterization of the effector cell and augmentation by interleukin 2. J Immunol. 1987;139:551–6. [PubMed] [Google Scholar]
- 20.Katz P, Yeager H, Jr, Whalen G, Evans M, Swartz RP, Roecklein J. Natural killer cell-mediated lysis of Mycobacterium-avium complex-infected monocytes. J Clin Immunol. 1990;10:71–7. doi: 10.1007/BF00917500. [DOI] [PubMed] [Google Scholar]
- 21.Bermudez LE, Kolonoski P, Young LS. Natural killer cell activity and macrophage-dependent inhibition of growth or killing of Mycobacterium avium complex in a mouse model. J Leukoc Biol. 1990;47:135–41. doi: 10.1002/jlb.47.2.135. [DOI] [PubMed] [Google Scholar]
- 22.Denis M. Activated murine natural killer cells control growth of Mycobacterium lepraemurium in mouse macrophages; in vitro and in vivo evidence. Int J Immunopharmacol. 1991;13:881–7. doi: 10.1016/0192-0561(91)90040-e. [DOI] [PubMed] [Google Scholar]
- 23.Harshan KV, Gangadharam PR. In vivo depletion of natural killer cell activity leads to enhanced multiplication of Mycobacterium avium complex in mice. Infect Immun. 1991;59:2818–21. doi: 10.1128/iai.59.8.2818-2821.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huntington ND, Vosshenrich CAJ, Di Santo JP. Developmental pathways that generate natural-killer-cell diversity in mice and humans. Nat Rev Immunol. 2007;7:703–14. doi: 10.1038/nri2154. [DOI] [PubMed] [Google Scholar]
- 25.Wilk E, Kalippke K, Buyny S, Schmidt RE, Jacobs R. New aspects of NK cell subset identification and inference of NK cells’ regulatory capacity by assessing functional and genomic profiles. Immunobiology. 2008;213:271–83. doi: 10.1016/j.imbio.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Batoni G, et al. Human CD56bright and CD56dim natural killer cell subsets respond differentially to direct stimulation with Mycobacterium bovis bacillus Calmette-Guerin. Scand J Immunol. 2005;62:498–506. doi: 10.1111/j.1365-3083.2005.01692.x. [DOI] [PubMed] [Google Scholar]
- 27.Warren HS, et al. Resilience to bacterial infection: difference between species could be due to proteins in serum. J Infect Dis. 2010;201:223–32. doi: 10.1086/649557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lauzon NM, Mian F, MacKenzie R, Ashkar AA. The direct effects of toll-like receptor ligands on human NK cell cytokine production and cytotoxicity. Cell Immunol. 2006;241:102–12. doi: 10.1016/j.cellimm.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Hornung V, et al. Quantitative expression of toll-like receptor 1–10 mRNA in cellular subsets of human peripheral blood mononuclear cells and sensitivity to CpG oligodeoxynucleotides. J Immunol. 2002;168:4531–7. doi: 10.4049/jimmunol.168.9.4531. [DOI] [PubMed] [Google Scholar]
- 30.Sawaki J, et al. Type 1 cytokine/chemokine production by mouse NK cells following activation of their TLR/MyD88-mediated pathways. Int Immunol. 2007;19:311–320. doi: 10.1093/intimm/dxl148. [DOI] [PubMed] [Google Scholar]
- 31.Martinez J, Huang X, Yang Y. Direct TLR2 signaling is critical for NK cell activation and function in response to vaccinia viral infection. PLoS Pathog. 2010;6:e1000811. doi: 10.1371/journal.ppat.1000811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eriksson M, et al. TLRs mediate IFN-gamma production by human uterine NK cells in endometrium. J Immunol. 2006;176:6219–24. doi: 10.4049/jimmunol.176.10.6219. [DOI] [PubMed] [Google Scholar]
- 33.Flo TH, et al. Differential expression of Toll-like receptor 2 in human cells. J Leukoc Biol. 2001;69:474–81. [PubMed] [Google Scholar]
- 34.Becker I, et al. Leishmania lipophosphoglycan (LPG) activates NK cells through toll-like receptor-2. Mol Biochem Parasitol. 2003;130:65–74. doi: 10.1016/s0166-6851(03)00160-9. [DOI] [PubMed] [Google Scholar]
- 35.Hart OM, Athie-Morales V, O’Connor GM, Gardiner CM. TLR7/8-mediated activation of human NK cells results in accessory cell-dependent IFN-gamma production. J Immunol. 2005;175:1636–42. doi: 10.4049/jimmunol.175.3.1636. [DOI] [PubMed] [Google Scholar]
- 36.Qiu F, Maniar A, Quevedo Diaz M, Chapoval AI, Medvedev AE. Activation of cytokine-producing and antitumor activities of natural killer cells and macrophages by engagement of toll-like and NOD-like receptors. Innate Immun. 2011;17:375–87. doi: 10.1177/1753425910372000. [DOI] [PubMed] [Google Scholar]
- 37.Neves PC, Matos DC, Marcovistz R, Galler R. TLR expression and NK cell activation after human yellow fever vaccination. Vaccine. 2009;27:5543–9. doi: 10.1016/j.vaccine.2009.07.028. [DOI] [PubMed] [Google Scholar]
- 38.Tsujimoto H, et al. Flagellin enhances NK cell proliferation and activation directly and through dendritic cell-NK cell interactions. J Leukoc Biol. 2005;78:888–97. doi: 10.1189/jlb.0105051. [DOI] [PubMed] [Google Scholar]
- 39.Merlo A, Calcaterra C, Menard S, Balsari A. Cross-talk between toll-like receptors 5 and 9 on activation of human immune responses. J Leukoc Biol. 2007;82:509–18. doi: 10.1189/jlb.0207100. [DOI] [PubMed] [Google Scholar]
- 40.Oren A, Husebo C, Iversen AC, Austgulen R. A comparative study of immunomagnetic methods used for separation of human natural killer cells from peripheral blood. J Immunol Methods. 2005;303:1–10. doi: 10.1016/j.jim.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 41.Costantini C, Calzetti F, Perbellini O, Cassatella MA. On the co-purification of 6-sulfo Lac-NAc(+) dendritic cells (slanDC) with NK cells enriched from human blood. Immunobiology. 2009;214:828–34. doi: 10.1016/j.imbio.2009.06.017. [DOI] [PubMed] [Google Scholar]
- 42.Scott MJ, Hoth JJ, Gardner SA, Peyton JC, Cheadle WG. Natural killer cell activation primes macrophages to clear bacterial infection. Am Surg. 2003;69:679–86. discussion 686–77. [PubMed] [Google Scholar]
- 43.Nishikado H, Mukai K, Kawano Y, Minegishi Y, Karasuyama H. NK cell-depleting anti-Asialo GM1 antibody exhibits a lethal off-target effect on basophils in vivo. J Immunol. 2011;186:5766–71. doi: 10.4049/jimmunol.1100370. [DOI] [PubMed] [Google Scholar]
- 44.Athie-Morales V, O’Connor GM, Gardiner CM. Activation of human NK cells by the bacterial pathogen-associated molecular pattern muramyl dipeptide. J Immunol. 2008;180:4082–9. doi: 10.4049/jimmunol.180.6.4082. [DOI] [PubMed] [Google Scholar]
- 45.Perrot I, et al. TLR3 and Rig-like receptor on myeloid dendritic cells and Rig-like receptor on human NK cells are both mandatory for production of IFN-gamma in response to double-stranded RNA. J Immunol. 2010;185:2080–8. doi: 10.4049/jimmunol.1000532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCartney S, et al. Distinct and complementary functions of MDA5 and TLR3 in poly(I:C)-mediated activation of mouse NK cells. J Exp Med. 2009;206:2967–76. doi: 10.1084/jem.20091181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miyake T, et al. Poly I:C-induced activation of NK cells by CD8 alpha+ dendritic cells via the IPS-1 and TRIF-dependent pathways. J Immunol. 2009;183:2522–8. doi: 10.4049/jimmunol.0901500. [DOI] [PubMed] [Google Scholar]
- 48.Cavaillon JM, Riviere Y, Svab J, Montagnier L, Alouf JE. Induction of interferon by streptococcus pyogenes extracellular products. Immunol Lett. 1982;5:323–6. doi: 10.1016/0165-2478(82)90121-3. [DOI] [PubMed] [Google Scholar]
- 49.Sacks LV, et al. A streptococcal erythrogenic toxin preparation augments natural killer activity of peripheral blood mononuclear cells. J Infect Dis. 1991;164:522–6. doi: 10.1093/infdis/164.3.522. [DOI] [PubMed] [Google Scholar]
- 50.Dobashi H, et al. Activation of mouse liver natural killer cells and NK1.1(+) T cells by bacterial superantigen-primed Kupffer cells. Hepatology. 1999;30:430–6. doi: 10.1002/hep.510300209. [DOI] [PubMed] [Google Scholar]
- 51.D’Orazio JA, Burke GW, Stein-Streilein J. Staphylococcal enterotoxin B activates purified NK cells to secrete IFN-gamma but requires T lymphocytes to augment NK cytotoxicity. J Immunol. 1995;154:1014–23. [PubMed] [Google Scholar]
- 52.Lando PA, Hedlund G, Dohlsten M, Kalland T. Bacterial superantigens as anti-tumour agents: induction of tumour cytotoxicity in human lymphocytes by staphylococcal enterotoxin A. Cancer Immunol Immunother. 1991;33:231–7. doi: 10.1007/BF01744942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ami K, et al. Activation of human T cells with NK cell markers by staphylococcal enterotoxin A via IL-12 but not via IL-18. Clin Exp Immunol. 2002;128:453–9. doi: 10.1046/j.1365-2249.2002.01854.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nomura T, et al. Essential role of interleukin-12 (IL-12) and IL-18 for gamma interferon production induced by listeriolysin O in mouse spleen cells. Infect Immun. 2002;70:1049–55. doi: 10.1128/IAI.70.3.1049-1055.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mühlen KA, et al. NK cells, but not NKT cells, are involved in Pseudomonas aeruginosa exotoxin A-induced hepatotoxicity in mice. J Immunol. 2004;172:3034–41. doi: 10.4049/jimmunol.172.5.3034. [DOI] [PubMed] [Google Scholar]
- 56.Michalkiewicz J, et al. Effect of Pseudomonas aeruginosa exotoxin A on IFN-gamma synthesis: expression of costimulatory molecules on monocytes and activity of NK cells. Immunol Lett. 1999;69:359–66. doi: 10.1016/s0165-2478(99)00121-2. [DOI] [PubMed] [Google Scholar]
- 57.Shenker BJ, et al. Flow cytometric analysis of the cytotoxic effects of Actinobacillus actino-mycetemcomitans leukotoxin on human natural killer cells. J Leukoc Biol. 1994;55:153–60. doi: 10.1002/jlb.55.2.153. [DOI] [PubMed] [Google Scholar]
- 58.Kerschen EJ, Cohen DA, Kaplan AM, Straley SC. The plague virulence protein YopM targets the innate immune response by causing a global depletion of NK cells. Infect. Immun. 2004;72:4589–602. doi: 10.1128/IAI.72.8.4589-4602.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lunemann A, Lunemann JD, Munz C. Regulatory NK-cell functions in inflammation and autoimmunity. Mol Med. 2009;15:352–8. doi: 10.2119/molmed.2009.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Seki S, et al. Role of liver NK cells and peritoneal macrophages in gamma interferon and interleukin-10 production in experimental bacterial peritonitis in mice. Infect Immun. 1998;66:5286–94. doi: 10.1128/iai.66.11.5286-5294.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cavaillon JM, Adib-Conquy M, Fitting C, Adrie C, Payen D. Cytokine cascade in sepsis. Scand J Infect Dis. 2003;35:535–44. doi: 10.1080/00365540310015935. [DOI] [PubMed] [Google Scholar]
- 62.Reefman E, et al. Cytokine secretion is distinct from secretion of cytotoxic granules in NK cells. J Immunol. 2010;184:4852–62. doi: 10.4049/jimmunol.0803954. [DOI] [PubMed] [Google Scholar]
- 63.Walker C, Checkel J, Cammisuli S, Leibson PJ, Gleich GJ. IL-5 production by NK cells contributes to eosinophil infiltration in a mouse model of allergic inflammation. J Immunol. 1998;161:1962–9. [PubMed] [Google Scholar]
- 64.Hall LJ, Clare S, Dougan G. NK cells influence both innate and adaptive immune responses after mucosal immunization with antigen and mucosal adjuvant. J Immunol. 2010;184:4327–37. doi: 10.4049/jimmunol.0903357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mehrotra PT, et al. Production of IL-10 by human natural killer cells stimulated with IL-2 and/or IL-12. J Immunol. 1998;160:2637–44. [PubMed] [Google Scholar]
- 66.Perona-Wright G, et al. Systemic but not local infections elicit immunosuppressive IL-10 production by natural killer cells. Cell Host Microbe. 2009;6:503–12. doi: 10.1016/j.chom.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gray JD, Hirokawa M, Horwitz DA. The role of transforming growth factor beta in the generation of suppression: an interaction between CD8+ T and NK cells. J Exp Med. 1994;180:1937–42. doi: 10.1084/jem.180.5.1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Marquez ME, et al. CD16 cross-linking induces increased expression of CD56 and production of IL-12 in peripheral NK cells. Cell Immunol. 2010;264:86–92. doi: 10.1016/j.cellimm.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 69.Sinha SK, Gao N, Guo Y, Yuan D. Mechanism of induction of NK activation by 2B4 (CD244) via its cognate ligand. J Immunol. 2010;185:5205–10. doi: 10.4049/jimmunol.1002518. [DOI] [PubMed] [Google Scholar]
- 70.Passos ST, et al. IL-6 promotes NK cell production of IL-17 during toxoplasmosis. J Immunol. 2010;184:1776–83. doi: 10.4049/jimmunol.0901843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cella M, et al. A human natural killer cell subset provides an innate source of IL-22 for mucosal immunity. Nature. 2009;457:722–5. doi: 10.1038/nature07537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wendt K, et al. Gene and protein characteristics reflect functional diversity of CD56dim and CD56bright NK cells. J Leukoc Biol. 2006;80:1529–41. doi: 10.1189/jlb.0306191. [DOI] [PubMed] [Google Scholar]
- 73.Pisegna S, et al. p38 MAPK activation controls the TLR3-mediated up-regulation of cytotoxicity and cytokine production in human NK cells. Blood. 2004;104:4157–64. doi: 10.1182/blood-2004-05-1860. [DOI] [PubMed] [Google Scholar]
- 74.Fehniger TA, et al. Differential cytokine and chemokine gene expression by human NK cells following activation with IL-18 or IL-15 in combination with IL-12: implications for the innate immune response. J Immunol. 1999;162:4511–20. [PubMed] [Google Scholar]
- 75.Sawaki J, et al. Type 1 cytokine/chemokine production by mouse NK cells following activation of their TLR/MyD88-mediated pathways. Int Immunol. 2007;19:311–20. doi: 10.1093/intimm/dxl148. [DOI] [PubMed] [Google Scholar]
- 76.Jewett A, Gan XH, Lebow LT, Bonavida B. Differential secretion of TNF-alpha and IFN-gamma by human peripheral blood-derived NK subsets and association with functional maturation. J Clin Immunol. 1996;16:46–54. doi: 10.1007/BF01540972. [DOI] [PubMed] [Google Scholar]
- 77.Caron G, et al. Human NK cells constitutively express membrane TNF-alpha (mTNFal-pha) and present mTNFalpha-dependent cytotoxic activity. Eur J Immunol. 1999;29:3588–95. doi: 10.1002/(SICI)1521-4141(199911)29:11<3588::AID-IMMU3588>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 78.Kashii Y, Giorda R, Herberman RB, Whiteside TL, Vujanovic NL. Constitutive expression and role of the TNF family ligands in apoptotic killing of tumor cells by human NK cells. J Immunol. 1999;163:5358–66. [PubMed] [Google Scholar]
- 79.Lopez MC, Duckett NS, Baron SD, Metzger DW. Early activation of NK cells after lung infection with the intracellular bacterium, Francisella tularensis LVS. Cell Immunol. 2004;232:75–85. doi: 10.1016/j.cellimm.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 80.Teixeira HC, Kaufmann SH. Role of NK1.1+ cells in experimental listeriosis: NK1+ cells are early IFN-gamma producers but impair resistance to Listeria monocytogenes infection. J Immunol. 1994;152:1873–82. [PubMed] [Google Scholar]
- 81.Berg RE, Crossley E, Murray S, Forman J. Relative contributions of NK and CD8 T cells to IFN-gamma mediated innate immune protection against Listeria monocytogenes. J Immunol. 2005;175:1751–7. doi: 10.4049/jimmunol.175.3.1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Thäle C, Kiderlen AF. Sources of interferon-gamma (IFN-gamma) in early immune response to Listeria monocytogenes. Immunobiology. 2005;210:673–83. doi: 10.1016/j.imbio.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 83.Rottenberg ME, et al. Regulation and role of IFN-gamma in the innate resistance to infection with Chlamydia pneumoniae. J Immunol. 2000;164:4812–8. doi: 10.4049/jimmunol.164.9.4812. [DOI] [PubMed] [Google Scholar]
- 84.Bohn E, Autenrieth IB. IL-12 is essential for resistance against Yersinia enterocolitica by triggering IFN-gamma production in NK cells and CD4+ T cells. J Immunol. 1996;156:1458–68. [PubMed] [Google Scholar]
- 85.Emoto M, et al. Critical role of NK cells rather than V alpha 14(+)NKT cells in lipopolysaccharide-induced lethal shock in mice. J Immunol. 2002;169:1426–32. doi: 10.4049/jimmunol.169.3.1426. [DOI] [PubMed] [Google Scholar]
- 86.Etogo AO, Nunez J, Lin CY, Toliver-Kinsky TE, Sherwood ER. NK but not CD1-restricted NKT cells facilitate systemic inflammation during polymicrobial intra-abdominal sepsis. J Immunol. 2008;180:6334–45. doi: 10.4049/jimmunol.180.9.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nakano Y, Onozuka K, Terada Y, Shinomiya H, Nakano M. Protective effect of recombinant tumor necrosis factor-alpha in murine salmonellosis. J Immunol. 1990;144:1935–41. [PubMed] [Google Scholar]
- 88.Mancuso G, et al. Type I IFN signaling is crucial for host resistance against different species of pathogenic bacteria. J Immunol. 2007;178:3126–33. doi: 10.4049/jimmunol.178.5.3126. [DOI] [PubMed] [Google Scholar]
- 89.Zantl N, et al. Essential role of gamma interferon in survival of colon ascendens stent peritonitis, a novel murine model of abdominal sepsis. Infect Immun. 1998;66:2300–9. doi: 10.1128/iai.66.5.2300-2309.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lainée P, et al. Delayed neutralization of interferon-gamma prevents lethality in primate Gram-negative bacteremic shock. Crit Care Med. 2005;33:797–805. doi: 10.1097/01.ccm.0000159090.80228.57. [DOI] [PubMed] [Google Scholar]
- 91.Nakane A, Okamoto M, Asano M, Kohanawa M, Minagawa T. Endogenous gamma interferon, tumor necrosis factor, and interleukin-6 in Staphylococcus aureus infection in mice. Infect Immun. 1995;63:1165–72. doi: 10.1128/iai.63.4.1165-1172.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Miles RH, Paxton TP, Dries DJ, Gamelli RL. Interferon-gamma increases mortality following cecal ligation and puncture. J Trauma. 1994;36:607–11. doi: 10.1097/00005373-199405000-00001. [DOI] [PubMed] [Google Scholar]
- 93.Murphey ED, Herndon DN, Sherwood ER. Gamma interferon does not enhance clearance of Pseudomonas aeruginosa but does amplify a proinflammatory response in a murine model of postseptic immunosuppression. Infect Immun. 2004;72:6892–901. doi: 10.1128/IAI.72.12.6892-6901.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Romero CR, et al. The role of interferon-gamma in the pathogenesis of acute intra-abdominal sepsis. J Leukoc Biol. 2010;88:725–35. doi: 10.1189/jlb.0509307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yin K, Gribbin E, Wang H. Interferon-gamma inhibition attenuates lethality after cecal ligation and puncture in rats: implication of high mobility group box-1. Shock. 2005;24:396–401. doi: 10.1097/01.shk.0000175556.03300.c6. [DOI] [PubMed] [Google Scholar]
- 96.Heremans H, Dillen C, Groenen M, Matthys P, Billiau A. Role of interferon-gamma and nitric oxide in pulmonary edema and death induced by lipopolysaccharide. Am J Respir Crit Care Med. 2000;161:110–7. doi: 10.1164/ajrccm.161.1.9902089. [DOI] [PubMed] [Google Scholar]
- 97.Agerberth B, et al. The human antimicrobial and chemotactic peptides LL-37 and alpha-defensins are expressed by specific lymphocyte and monocyte populations. Blood. 2000;96:3086–93. [PubMed] [Google Scholar]
- 98.Zelante T, Fallarino F, Bistoni F, Puccetti P, Romani L. Indoleamine 2,3-dioxygenase in infection: the paradox of an evasive strategy that benefits the host. Microbes Infect. 2009;11:133–41. doi: 10.1016/j.micinf.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 99.Bogdan C. Nitric oxide and the immune response. Nat Immunol. 2001;2:907–16. doi: 10.1038/ni1001-907. [DOI] [PubMed] [Google Scholar]
- 100.Wang C, et al. Donor IL-4-treatment induces alternatively activated liver macrophages and IDO-expressing NK cells and promotes rat liver allograft acceptance. Transpl Immunol. 2010;22:172–8. doi: 10.1016/j.trim.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 101.Jyothi MD, Khar A. Interleukin-2-induced nitric oxide synthase and nuclear factor-kappaB activity in activated natural killer cells and the production of interferon-gamma. Scand J Immunol. 2000;52:148–55. doi: 10.1046/j.1365-3083.2000.00762.x. [DOI] [PubMed] [Google Scholar]
- 102.Salvucci O, Kolb JP, Dugas B, Dugas N, Chouaib S. The induction of nitric oxide by interleukin-12 and tumor necrosis factor-alpha in human natural killer cells: relationship with the regulation of lytic activity. Blood. 1998;92:2093–102. [PubMed] [Google Scholar]
- 103.Furuke K, et al. Human NK cells express endothelial nitric oxide synthase, and nitric oxide protects them from activation-induced cell death by regulating expression of TNF-alpha. J Immunol. 1999;163:1473–80. [PubMed] [Google Scholar]
- 104.Haworth O, Cernadas M, Levy BD. NK cells are effectors for resolvin E1 in the timely resolution of allergic airway inflammation. J Immunol. 2011;186:6129–35. doi: 10.4049/jimmunol.1004007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Strengell M, et al. IL-21 in synergy with IL-15 or IL-18 enhances IFN-gamma production in human NK and T cells. J Immunol. 2003;170:5464–9. doi: 10.4049/jimmunol.170.11.5464. [DOI] [PubMed] [Google Scholar]
- 106.Brady J, et al. The interactions of multiple cytokines control NK cell maturation. J Immunol. 2010;185:6679–88. doi: 10.4049/jimmunol.0903354. [DOI] [PubMed] [Google Scholar]
- 107.Orange JS, Biron CA. Characterization of early IL-12, IFN-alphabeta, and TNF effects on antiviral state and NK cell responses during murine cytomegalovirus infection. J Immunol. 1996;156:4746–56. [PubMed] [Google Scholar]
- 108.Morris SC, et al. IL-4 induces in vivo production of IFN-gamma by NK and NKT cells. J Immunol. 2006;176:5299–305. doi: 10.4049/jimmunol.176.9.5299. [DOI] [PubMed] [Google Scholar]
- 109.Hunter CA, Chizzonite R, Remington JS. IL-1 beta is required for IL-12 to induce production of IFN-gamma by NK cells: a role for IL-1 beta in the T cell-independent mechanism of resistance against intracellular pathogens. J Immunol. 1995;155:4347–54. [PubMed] [Google Scholar]
- 110.van de Wetering D, de Paus RA, van Dissel JT, van de Vosse E. IL-23 modulates CD56+/CD3− NK cell and CD56+/CD3+ NK-like T cell function differentially from IL-12. Int Immunol. 2008;21:145–53. doi: 10.1093/intimm/dxn132. [DOI] [PubMed] [Google Scholar]
- 111.Smithgall MD, et al. IL-33 amplifies both Th1- and Th2-type responses through its activity on human basophils, allergen-reactive Th2 cells, iNKT and NK cells. Int Immunol. 2008;20:1019–30. doi: 10.1093/intimm/dxn060. [DOI] [PubMed] [Google Scholar]
- 112.Taub DD, Sayers TJ, Carter CR, Ortaldo JR. Alpha and beta chemokines induce NK cell migration and enhance NK-mediated cytolysis. J Immunol. 1995;155:3877–88. [PubMed] [Google Scholar]
- 113.Coelho AL, et al. The chemokine CCL6 promotes innate immunity via immune cell activation and recruitment. J Immunol. 2007;179:5474–82. doi: 10.4049/jimmunol.179.8.5474. [DOI] [PubMed] [Google Scholar]
- 114.Mrozek E, Anderson P, Caligiuri MA. Role of interleukin-15 in the development of human CD56+ natural killer cells from CD34+ hematopoietic progenitor cells. Blood. 1996;87:2632–40. [PubMed] [Google Scholar]
- 115.Carson WE, et al. Endogenous production of interleukin 15 by activated human monocytes is critical for optimal production of interferon-gamma by natural killer cells in vitro. J Clin Invest. 1995;96:2578–82. doi: 10.1172/JCI118321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Koka R, et al. Cutting edge: murine dendritic cells require IL-15R alpha to prime NK cells. J Immunol. 2004;173:3594–8. doi: 10.4049/jimmunol.173.6.3594. [DOI] [PubMed] [Google Scholar]
- 117.Ma A, Koka R, Burkett P. Diverse functions of IL-2, IL-15, and IL-7 in lymphoid homeostasis. Annu Rev Immunol. 2006;24:657–79. doi: 10.1146/annurev.immunol.24.021605.090727. [DOI] [PubMed] [Google Scholar]
- 118.Carson WE, et al. Interleukin (IL) 15 is a novel cytokine that activates human natural killer cells via components of the IL-2 receptor. J Exp Med. 1994;180:1395–403. doi: 10.1084/jem.180.4.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Murphy WJ, Keller JR, Harrison CL, Young HA, Longo DL. Interleukin-2-activated natural killer cells can support hematopoiesis in vitro and promote marrow engraftment in vivo. Blood. 1992;80:670–7. [PubMed] [Google Scholar]
- 120.Granucci F, et al. A contribution of mouse dendritic cell-derived IL-2 for NK cell activation. J Exp Med. 2004;200:287–95. doi: 10.1084/jem.20040370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhan Y, Cheers C. Endogenous interleukin-12 is involved in resistance to Brucella abortus infection. Infect Immun. 1995;63:1387–90. doi: 10.1128/iai.63.4.1387-1390.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhou P, et al. IL-12 prevents mortality in mice infected with Histoplasma capsulatum through induction of IFN-gamma. J Immunol. 1995;155:785–95. [PubMed] [Google Scholar]
- 123.Mastroeni P, Harrison JA, Chabalgoity JA, Hor-maeche CE. Effect of interleukin 12 neutralization on host resistance and gamma interferon production in mouse typhoid. Infect Immun. 1996;64:189–96. doi: 10.1128/iai.64.1.189-196.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.van de Wetering D, de Paus R, van Dissel J, van de Vosse E. Salmonella induced IL-23 and IL-1beta allow for IL-12 production by monocytes and Mphi1 through induction of IFN-gamma in CD56 NK/NK-like T cells. PLoS One. 2009;4:e8396. doi: 10.1371/journal.pone.0008396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Matsumoto H, et al. Interleukin-12 gene expression in human monocyte-derived macrophages stimulated with Mycobacterium bovis BCG: cytokine regulation and effect of NK cells. Infect Immun. 1997;65:4405–10. doi: 10.1128/iai.65.11.4405-4410.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bohn E, et al. IL-18 (IFN-gamma-inducing factor) regulates early cytokine production in, and promotes resolution of, bacterial infection in mice. J Immunol. 1998;160:299–307. [PubMed] [Google Scholar]
- 127.Takeda K, et al. Defective NK cell activity and Th1 response in IL-18-deficient mice. Immunity. 1998;8:383–90. doi: 10.1016/s1074-7613(00)80543-9. [DOI] [PubMed] [Google Scholar]
- 128.Nagarajan UM, et al. MyD88 deficiency leads to decreased NK cell gamma interferon production and T cell recruitment during Chla-mydia muridarum genital tract infection, but a predominant Th1 response and enhanced monocytic inflammation are associated with infection resolution. Infect Immun. 2011;79:486–98. doi: 10.1128/IAI.00843-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Garcia VE, et al. IL-18 promotes type 1 cytokine production from NK cells and T cells in human intracellular infection. J Immunol. 1999;162:6114–21. [PubMed] [Google Scholar]
- 130.Chaix J, et al. Cutting edge: priming of NK cells by IL-18. J Immunol. 2008;181:1627–31. doi: 10.4049/jimmunol.181.3.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nguyen KB, et al. Coordinated and distinct roles for IFN-alpha beta, IL-12, and IL-15 regulation of NK cell responses to viral infection. J Immunol. 2002;169:4279–87. doi: 10.4049/jimmunol.169.8.4279. [DOI] [PubMed] [Google Scholar]
- 132.Scott MJ, Hoth JJ, Turina M, Woods DR, Cheadle WG. Interleukin-10 suppresses natural killer cell but not natural killer T cell activation during bacterial infection. Cytokine. 2006;33:79–86. doi: 10.1016/j.cyto.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 133.Bellone G, Aste-Amezaga M, Trinchieri G, Rodeck U. Regulation of NK cell functions by TGF-beta 1. J Immunol. 1995;155:1066–73. [PubMed] [Google Scholar]
- 134.Leung KH, Koren HS. Regulation of human natural killing. II. Protective effect of interferon on NK cells from suppression by PGE2. J Immunol. 1982;129:1742–7. [PubMed] [Google Scholar]
- 135.Lauzon W, Lemaire I. Alveolar macrophage inhibition of lung-associated NK activity: involvement of prostaglandins and transforming growth factor-beta 1. Exp Lung Res. 1994;20:331–49. doi: 10.3109/01902149409064391. [DOI] [PubMed] [Google Scholar]
- 136.Chen Y, Perussia B, Campbell KS. Prostaglandin D2 suppresses human NK cell function via signaling through D prostanoid receptor. J Immunol. 2007;179:2766–73. doi: 10.4049/jimmunol.179.5.2766. [DOI] [PubMed] [Google Scholar]
- 137.Gatti G, et al. Inhibition by cortisol of human natural killer (NK) cell activity. J Steroid Biochem. 1987;26:49–58. doi: 10.1016/0022-4731(87)90030-6. [DOI] [PubMed] [Google Scholar]
- 138.Shakhar G, Blumenfeld B. Glucocorticoid involvement in suppression of NK activity following surgery in rats. J Neuroimmunol. 2003;138:83–91. doi: 10.1016/s0165-5728(03)00118-8. [DOI] [PubMed] [Google Scholar]
- 139.Chiu BC, Stolberg VR, Chensue SW. Mononuclear phagocyte-derived IL-10 suppresses the innate IL-12/IFN-gamma axis in lung-challenged aged mice. J Immunol. 2008;181:3156–66. doi: 10.4049/jimmunol.181.5.3156. [DOI] [PubMed] [Google Scholar]
- 140.Lassen MG, Lukens JR, Dolina JS, Brown MG, Hahn YS. Intrahepatic IL-10 maintains NKG2A+Ly49− liver NK cells in a functionally hyporesponsive state. J Immunol. 2010;184:2693–701. doi: 10.4049/jimmunol.0901362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Peppa D, et al. Blockade of immunosup-pressive cytokines restores NK cell antiviral function in chronic hepatitis B virus infection. PLoS Pathog. 2010;6:e1001227. doi: 10.1371/journal.ppat.1001227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Shibata Y, et al. Immunoregulatory roles of IL-10 in innate immunity: IL-10 inhibits macrophage production of IFN-gamma-inducing factors but enhances NK cell production of IFN-gamma. J Immunol. 1998;161:4283–8. [PubMed] [Google Scholar]
- 143.Cai G, Kastelein RA, Hunter CA. IL-10 enhances NK cell proliferation, cytotoxicity and production of IFN-gamma when combined with IL-18. Eur J Immunol. 1999;29:2658–65. doi: 10.1002/(SICI)1521-4141(199909)29:09<2658::AID-IMMU2658>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 144.Qian C, et al. TLR agonists promote ERK-mediated preferential IL-10 production of regulatory dendritic cells (diffDCs), leading to NK-cell activation. Blood. 2006;108:2307–15. doi: 10.1182/blood-2006-03-005595. [DOI] [PubMed] [Google Scholar]
- 145.Newman KC, Riley EM. Whatever turns you on: accessory-cell-dependent activation of NK cells by pathogens. Nat Rev Immunol. 2007;7:279–91. doi: 10.1038/nri2057. [DOI] [PubMed] [Google Scholar]
- 146.Ramarathinam L, Niesel DW, Klimpel GR. Ity influences the production of IFN-gamma by murine splenocytes stimulated in vitro with Salmonella typhimurium. J Immunol. 1993;150:3965–72. [PubMed] [Google Scholar]
- 147.Lucas M, Schachterle W, Oberle K, Aichele P, Diefenbach A. Dendritic cells prime natural killer cells by trans-presenting interleukin 15. Immunity. 2007;26:503–17. doi: 10.1016/j.immuni.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Goodier MR, Londei M. Lipopolysaccha-ride stimulates the proliferation of human CD56+CD3– NK cells: a regulatory role of monocytes and IL-10. J Immunol. 2000;165:139–47. doi: 10.4049/jimmunol.165.1.139. [DOI] [PubMed] [Google Scholar]
- 149.Humann J, Lenz LL. Activation of naive NK cells in response to Listeria monocytogenes requires IL-18 and contact with infected den-dritic cells. J Immunol. 2010;184:5172–8. doi: 10.4049/jimmunol.0903759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Pallandre JR, et al. Dendritic cell and natural killer cell cross-talk: a pivotal role of CX3CL1 in NK cytoskeleton organization and activation. Blood. 2008;112:4420–4. doi: 10.1182/blood-2007-12-126888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kang SJ, Liang HE, Reizis B, Locksley RM. Regulation of hierarchical clustering and activation of innate immune cells by dendritic cells. Immunity. 2008;29:819–33. doi: 10.1016/j.immuni.2008.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Blanchard DK, Friedman H, Stewart WE, 2nd, Klein TW, Djeu JY. Role of gamma inter-feron in induction of natural killer activity by Legionella pneumophila in vitro and in an experimental murine infection model. Infect Immun. 1988;56:1187–93. doi: 10.1128/iai.56.5.1187-1193.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wherry JC, Schreiber RD, Unanue ER. Regulation of gamma interferon production by natural killer cells in scid mice: roles of tumor necrosis factor and bacterial stimuli. Infect. Immun. 1991;59:1709–15. doi: 10.1128/iai.59.5.1709-1715.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Scott MJ, et al. interactions between macrophages and natural killer cells during sepsis are critical for macrophage activation and are not interferon gamma dependent. Clin Exp Immunol. 2004;137:CD40–154. 469–77. doi: 10.1111/j.1365-2249.2004.02547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lapaque N, Walzer T, Meresse S, Vivier E, Trowsdale J. Interactions between human NK cells and macrophages in response to Salmonella infection. J Immunol. 2009;182:4339–48. doi: 10.4049/jimmunol.0803329. [DOI] [PubMed] [Google Scholar]
- 156.Tu Z, et al. TLR-dependent cross talk between human Kupffer cells and NK cells. J Exp Med. 2008;205:233–44. doi: 10.1084/jem.20072195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hou X, Zhou R, Wei H, Sun R, Tian Z. NKG2D-retinoic acid early inducible-1 recognition between natural killer cells and Kupffer cells in a novel murine natural killer cell-dependent fulminant hepatitis. Hepatology. 2009;49:940–9. doi: 10.1002/hep.22725. [DOI] [PubMed] [Google Scholar]
- 158.Gerosa F, et al. Reciprocal activating interaction between natural killer cells and den-dritic cells. J Exp Med. 2002;195:327–33. doi: 10.1084/jem.20010938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Godshall CJ, Scott MJ, Burch PT, Peyton JC, Cheadle WG. Natural killer cells participate in bacterial clearance during septic peritonitis through interactions with macrophages. Shock. 2003;19:144–9. doi: 10.1097/00024382-200302000-00010. [DOI] [PubMed] [Google Scholar]
- 160.Hamerman JA, Ogasawara K, Lanier LL. Cutting edge: toll-like receptor signaling in macrophages induces ligands for the NKG2D receptor. J Immunol. 2004;172:2001–5. doi: 10.4049/jimmunol.172.4.2001. [DOI] [PubMed] [Google Scholar]
- 161.Kloss M, et al. Interaction of monocytes with NK cells upon Toll-like receptor-induced expression of the NKG2D ligand MICA. J Immunol. 2008;181:6711–9. doi: 10.4049/jimmunol.181.10.6711. [DOI] [PubMed] [Google Scholar]
- 162.Borchers MT, et al. The NKG2D-activating receptor mediates pulmonary clearance of Pseudomonas aeruginosa. Infect Immun. 2006;74:2578–86. doi: 10.1128/IAI.74.5.2578-2586.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wesselkamper SC, et al. NKG2D is critical for NK cell activation in host defense against Pseudomonas aeruginosa respiratory infection. J Immunol. 2008;181:5481–9. doi: 10.4049/jimmunol.181.8.5481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Emoto M, et al. Highly biased type 1 immune responses in mice deficient in LFA-1 in Listeria monocytogenes infection are caused by elevated IL-12 production by granulocytes. J Immunol. 2003;171:3970–6. doi: 10.4049/jimmunol.171.8.3970. [DOI] [PubMed] [Google Scholar]
- 165.Sporri R, Joller N, Hilbi H, Oxenius A. A novel role for neutrophils as critical activators of NK cells. J Immunol. 2008;181:7121–30. doi: 10.4049/jimmunol.181.10.7121. [DOI] [PubMed] [Google Scholar]
- 166.Costantini C, et al. Neutrophil activation and survival are modulated by interaction with NK cells. Int Immunol. 2010;22:827–38. doi: 10.1093/intimm/dxq434. [DOI] [PubMed] [Google Scholar]
- 167.Costantini C, Cassatella MA. The defensive alliance between neutrophils and NK cells as a novel arm of innate immunity. J Leukoc Biol. 2011;89:221–33. doi: 10.1189/jlb.0510250. [DOI] [PubMed] [Google Scholar]
- 168.Echtenacher B, Mannel DN, Hultner L. Critical protective role of mast cells in a model of acute septic peritonitis. Nature. 1996;381:75–7. doi: 10.1038/381075a0. [DOI] [PubMed] [Google Scholar]
- 169.Vosskuhl K, Greten TF, Manns MP, Korangy F, Wedemeyer J. Lipopolysaccharide-mediated mast cell activation induces IFN-gamma secretion by NK cells. J Immunol. 2010;185:119–25. doi: 10.4049/jimmunol.0902406. [DOI] [PubMed] [Google Scholar]
- 170.Michael A, Hackett JJ, Bennett M, Kumar V, Yuan D. Regulation of B lymphocytes by natural killer cells: role of IFN-gamma. J Immunol. 1989;142:1095–101. [PubMed] [Google Scholar]
- 171.Yuan D, Koh CY, Wilder JA. Interactions between B lymphocytes and NK cells. FASEB J. 1994;8:1012–8. doi: 10.1096/fasebj.8.13.7926365. [DOI] [PubMed] [Google Scholar]
- 172.Bao Y, Han Y, Chen Z, Xu S, Cao X. IFN-alpha-producing PDCA-1+ Siglec-H- B cells mediate innate immune defense by activating NK cells. Eur J Immunol. 2011;41:657–68. doi: 10.1002/eji.201040840. [DOI] [PubMed] [Google Scholar]
- 173.Schierloh P, et al. NK cells from tuberculous pleurisy express high ICAM-1 levels and exert stimulatory effect on local T cells. Eur J Immunol. 2009;39:2450–8. doi: 10.1002/eji.200939515. [DOI] [PubMed] [Google Scholar]
- 174.Andrews DM, et al. Homeostatic defects in interleukin 18-deficient mice contribute to protection against the lethal effects of endotoxin. Immunol Cell Biol. 2011;89:739–46. doi: 10.1038/icb.2010.168. [DOI] [PubMed] [Google Scholar]
- 175.Cavassani KA, et al. The post sepsis- induced expansion and enhanced function of regulatory T cells create an environment to potentiate tumor growth. Blood. 2010;115:4403–11. doi: 10.1182/blood-2009-09-241083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ghiringhelli F, et al. CD4+CD25+ regulatory T cells inhibit natural killer cell functions in a transforming growth factor-beta-dependent manner. J Exp Med. 2005;202:1075–85. doi: 10.1084/jem.20051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Smyth MJ, et al. CD4+CD25+ T regulatory cells suppress NK cell-mediated im-munotherapy of cancer. J Immunol. 2006;176:1582–7. doi: 10.4049/jimmunol.176.3.1582. [DOI] [PubMed] [Google Scholar]
- 178.Neves P, et al. Signaling via the MyD88 adaptor protein in B cells suppresses protective immunity during Salmonella typhimurium infection. Immunity. 2010;33:777–90. doi: 10.1016/j.immuni.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 179.Elkabets M, et al. IL-1beta regulates a novel myeloid-derived suppressor cell subset that impairs NK cell development and function. Eur J Immunol. 2010;40:3347–57. doi: 10.1002/eji.201041037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hook CE, Matyszak MK, Gaston JS. Infection of epithelial and dendritic cells by Chla-mydia trachomatis results in IL-18 and IL-12 production, leading to interferon-gamma production by human natural killer cells. FEMS Immunol Med Microbiol. 2005;45:113–20. doi: 10.1016/j.femsim.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 181.Dunn PL, North RJ. Early gamma interferon production by natural killer cells is important in defense against murine listeriosis. Infect Immun. 1991;59:2892–900. doi: 10.1128/iai.59.9.2892-2900.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Calum H, Moser C, Jensen PO, Shirai R, Hoiby N. Cytokine and surface receptor diversity of NK cells in resistant C3H/HeN and susceptible BALB/c mice with chronic Pseudomonas aeruginosa lung infection. APMIS. 2003;111:891–7. doi: 10.1034/j.1600-0463.2003.1110907.x. [DOI] [PubMed] [Google Scholar]
- 183.Godshall CJ, Scott MJ, Burch PT, Peyton JC, Cheadle WG. Natural killer cells participate in bacterial clearance during septic peritonitis through interactions with macrophages. Shock. 2003;19:144–9. doi: 10.1097/00024382-200302000-00010. [DOI] [PubMed] [Google Scholar]
- 184.Sherwood ER, Enoh VT, Murphey ED, Lin CY. Mice depleted of CD8+ T and NK cells are resistant to injury caused by cecal ligation and puncture. Lab Invest. 2004;84:1655–65. doi: 10.1038/labinvest.3700184. [DOI] [PubMed] [Google Scholar]
- 185.Badgwell B, et al. Natural killer cells contribute to the lethality of a murine model of Escherichia coli infection. Surgery. 2002;132:205–12. doi: 10.1067/msy.2002.125311. [DOI] [PubMed] [Google Scholar]
- 186.Stevenson HL, Estes MD, Thirumalapura NR, Walker DH, Ismail N. Natural killer cells promote tissue injury and systemic inflammatory responses during fatal ehrlichia-induced toxic shock-like syndrome. Am J Pathol. 2010;177:766–76. doi: 10.2353/ajpath.2010.091110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kerr AR, et al. Identification of a detrimental role for NK cells in pneumococcal pneumonia and sepsis in immunocompromised hosts. Microbes Infect. 2005;7:845–52. doi: 10.1016/j.micinf.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 188.Goldmann O, Chhatwal GS, Medina E. Contribution of natural killer cells to the pathogenesis of septic shock induced by Streptococcus pyogenes in mice. J Infect Dis. 2005;191:1280–6. doi: 10.1086/428501. [DOI] [PubMed] [Google Scholar]
- 189.Kuo SH, et al. Expression of CD86 and increased infiltration of NK cells are associated with Helicobacter pylori-dependent state of early stage high-grade gastric MALT lym-phoma. World J Gastroenterol. 2005;11:4357–62. doi: 10.3748/wjg.v11.i28.4357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Singh UP, et al. CXCL10+ T cells and NK cells assist in the recruitment and activation of CXCR3+ and CXCL11+ leukocytes during My-cobacteria-enhanced colitis. BMC Immunol. 2008;9:25. doi: 10.1186/1471-2172-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Heremans H, Dillen C, van Damme J, Billiau A. Essential role for natural killer cells in the lethal lipopolysaccharide-induced Shwartzman-like reaction in mice. Eur J Immunol. 1994;24:1155–60. doi: 10.1002/eji.1830240522. [DOI] [PubMed] [Google Scholar]
- 192.Barkhausen T, et al. Depletion of NK cells in a murine polytrauma model is associated with improved outcome and a modulation of the inflammatory response. Shock. 2008;30:401–10. doi: 10.1097/SHK.0b013e31816e2cda. [DOI] [PubMed] [Google Scholar]
- 193.Carson WE, et al. A fatal cytokine-induced systemic inflammatory response reveals a critical role for NK cells. J Immunol. 1999;162:4943–51. [PubMed] [Google Scholar]
- 194.Vankayalapati R, et al. Role of NK cell-activating receptors and their ligands in the lysis of mononuclear phagocytes infected with an in-tracellular bacterium. J Immunol. 2005;175:4611–7. doi: 10.4049/jimmunol.175.7.4611. [DOI] [PubMed] [Google Scholar]
- 195.Feng CG, et al. NK cell-derived IFN-gamma differentially regulates innate resistance and neutrophil response in T cell-deficient hosts infected with Mycobacterium tuberculosis. J Immunol. 2006;177:7086–93. doi: 10.4049/jimmunol.177.10.7086. [DOI] [PubMed] [Google Scholar]
- 196.Schafer R, Eisenstein TK. Natural killer cells mediate protection induced by a Salmonella aroA mutant. Infect Immun. 1992;60:791–7. doi: 10.1128/iai.60.3.791-797.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Hirose K, Nishimura H, Matsuguchi T, Yoshikai Y. Endogenous IL-15 might be responsible for early protection by natural killer cells against infection with an avirulent strain of Salmonella choleraesuis in mice. J Leukoc Biol. 1999;66:382–90. doi: 10.1002/jlb.66.3.382. [DOI] [PubMed] [Google Scholar]
- 198.Ashkar AA, Reid S, Verdu EF, Zhang K, Coombes BK. Interleukin-15 and NK1.1+ cells provide innate protection against acute Salmonella enterica serovar Typhimurium infection in the gut and in systemic tissues. Infect Immun. 2009;77:214–22. doi: 10.1128/IAI.01066-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Nilsson N, Bremell T, Tarkowski A, Carlsten H. Protective role of NK1.1+ cells in experimental Staphylococcus aureus arthritis. Clin Exp Immunol. 1999;117:63–9. doi: 10.1046/j.1365-2249.1999.00922.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Small CL, et al. NK cells play a critical protective role in host defense against acute extracellular Staphylococcus aureus bacterial infection in the lung. J Immunol. 2008;180:5558–68. doi: 10.4049/jimmunol.180.8.5558. [DOI] [PubMed] [Google Scholar]
- 201.Small CL, et al. Influenza infection leads to increased susceptibility to subsequent bacterial superinfection by impairing NK cell responses in the lung. J Immunol. 2010;184:2048–56. doi: 10.4049/jimmunol.0902772. [DOI] [PubMed] [Google Scholar]
- 202.Venet F, et al. Early assessment of leukocyte alterations at diagnosis of septic shock. Shock. 2010;34:358–63. doi: 10.1097/SHK.0b013e3181dc0977. [DOI] [PubMed] [Google Scholar]
- 203.Holub M, et al. Lymphocyte subset numbers depend on the bacterial origin of sepsis. Clin Microbiol Infect. 2003;9:202–11. doi: 10.1046/j.1469-0691.2003.00518.x. [DOI] [PubMed] [Google Scholar]
- 204.Giamarellos-Bourboulis EJ, et al. Early changes of CD4-positive lymphocytes and NK cells in patients with severe gram-negative sepsis. Crit Care. 2006;10:R166. doi: 10.1186/cc5111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Cavaillon JM, Adrie C, Fitting C, Adib-Conquy M. Reprogramming of circulatory cells in sepsis and SIRS. J Endotoxin Res. 2005;11:311–20. doi: 10.1179/096805105X58733. [DOI] [PubMed] [Google Scholar]
- 206.Maturana P, et al. Natural killer cell activity in patients with septic shock. J Crit Care Med. 1991;6:42–5. [Google Scholar]
- 207.Puente J, et al. In vitro studies of natural killer cell activity in septic shock patients: response to a challenge with alpha-interferon and interleukin-2. Int J Clin Pharmacol Ther Toxicol. 1993;31:271–5. [PubMed] [Google Scholar]
- 208.Georgeson GD, et al. Natural killer cell cytotoxicity is deficient in newborns with sepsis and recurrent infections. Eur J Pediatr. 2001;160:478–82. doi: 10.1007/s004310100773. [DOI] [PubMed] [Google Scholar]
- 209.Blazar BA, et al. Suppression of natural killer-cell function in humans following thermal and traumatic injury. J Clin Immunol. 1986;6:26–36. doi: 10.1007/BF00915361. [DOI] [PubMed] [Google Scholar]
- 210.Bender BS, et al. Depressed natural killer cell function in thermally injured adults: successful in vivo and in vitro immunomodulation and the role of endotoxin. Clin Exp Immunol. 1988;71:120–5. [PMC free article] [PubMed] [Google Scholar]
- 211.Klimpel GR, et al. Defective NK cell activity following thermal injury. Clin Exp Immunol. 1986;66:384–92. [PMC free article] [PubMed] [Google Scholar]
- 212.Toft P, Dagnaes-Hansen F, Tonnesen E, Basse PM. The effect of surgical stress and endotoxin-induced sepsis on the NK-cell activity, distribution and pulmonary clearance of YAC-1 and melanoma cells. APMIS. 1999;107:359–64. doi: 10.1111/j.1699-0463.1999.tb01565.x. [DOI] [PubMed] [Google Scholar]
- 213.Melder RJ, Ho M. Modulation of natural killer cell activity in mice after interferon induction: depression of activity and depression of in vitro enhancement by interferon. Infect Immun. 1982;36:990–5. doi: 10.1128/iai.36.3.990-995.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Vaknin I, et al. A common pathway mediated through toll-like receptors leads to T- and natural killer-cell immunosuppression. Blood. 2008;111:1437–47. doi: 10.1182/blood-2007-07-100404. [DOI] [PubMed] [Google Scholar]
- 215.Hirsh M, Kaplan V, Dyugovskaya L, Krausz MM. Response of lung NK1.1-positive natural killer cells to experimental sepsis in mice. Shock. 2004;22:40–5. doi: 10.1097/01.shk.0000129758.81361.45. [DOI] [PubMed] [Google Scholar]
- 216.Inoue S, et al. IL-15 prevents apoptosis, reverses innate and adaptive immune dysfunction, and improves survival in sepsis. J Immunol. 2010;184:1401–9. doi: 10.4049/jimmunol.0902307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Cavaillon JM, Adib-Conquy M. Bench-to-bedside review: endotoxin tolerance as a model of leukocyte reprogramming in sepsis. Crit Care. 2006;10:233. doi: 10.1186/cc5055. [DOI] [PMC free article] [PubMed] [Google Scholar]