SUMMARY
Snoring is caused by vibrating anatomical structures in the upper aerodigestive tract. It can be treated surgically and non-surgically, although resective procedures are associated with high postoperative morbidity and failure rate. We describe a new non-resective surgical procedure called the velo-uvulo-pharyngeal lift in which the soft palate is lifted, shortened, advanced and stiffened by means of permanent threads anchored to fibro-osseous attachments at the level of the posterior nasal spine and both pterygoid hamuli. Four adult patients (median age 44.5 years; range 42-65) affected by snoring and mild obstructive sleep apnoea-hypopnoea syndrome (apneoa-hypopnoea index, AHI < 20) requiring septal surgery under general anesthesia also underwent velo-uvulo-pharyngeal lift. There were no significant intra- or post-operative complications, and all of the patients reported immediate snoring relief. The main complaints were slight pain and a sensation of local fullness, both of which spontaneously disappeared within two days. The subjective clinical improvement in snoring was confirmed during post-operative follow-up (median 15.5 months; range 6-25), as was the stable reshaping of the soft velo-uvulo-pharyngeal tissues and enlargement of the mesopharyngeal space. There was also a decrease in daytime sleepiness. Our preliminary results suggest that velo-uvulo-pharyngeal lift is a simple, cost-effective and minimally invasive means of widening the mesopharyngeal space in snoring patients with or without mild sleep apnoea-hypopnoea syndrome. The widening of the mesopharyngeal space prevents contact-induced wall vibrations and its inspiratory obstruction causing hypopnoea and apnoea. It can also be combined with other procedures if indicated.
KEY WORDS: Snoring, OSAHS, Roman blinds, VUPL
RIASSUNTO
Il russamento è dovuto alla vibrazione delle strutture anatomiche delle alte vie aereo-digestive e la terapia può essere di tipo chirurgico e non, sebbene le procedure chirurgiche siano gravate da un'elevata morbidità post-operatoria e ad un elevato rischio di insuccesso. Nel presente lavoro viene descritta una nuova procedura chirurgica non demolitiva chiamata lifting velo-uvulo-faringeo, che porta alla sospensione, all'accorciamento, all'avanzamento ed all'irrigidimento del palato molle attraverso l'utilizzo di suture permanenti che hanno come punti d'ancoraggio le strutture fibro-ossee a livello della spina nasale posteriore e degli uncini pterigoidei. Quattro pazienti adulti (età mediana 44.5 anni, range 42-65 anni) con russamento associato a sindrome delle apnee ostruttive del sonno di lieve entità (indice apneaipopnea, AHI < 20) candidati a settoplastica in anestesia generale sono stati sottoposti contestualmente a lifting velo-uvulo-faringeo. Non sono accorse complicanze intra- o post-operatorie e tutti i pazienti hanno riportato un immediato beneficio successivo al trattamento. Il principale disturbo post-operatorio è stato una lieve algia associata a senso di pienezza del palato, entrambi spontaneamente risolti entro 2 giorni dalla procedura. Il miglioramento soggettivo del russamento è stato confermato nel corso del follow-up (mediana 15.5 mesi, range 6-25 mesi), così come la persistenza di un rimodellamento a carico dei tessuti molli velo-uvulo-faringei e l'allargamento dello spazio mesofaringeo. è stata altresì riportata una diminuzione della sonnolenza diurna. I nostri risultati preliminari suggeriscono che il lifting velo-uvulo-faringeo possa essere considerata una metodica semplice, economica e minimamente invasiva per l'ampliamento dello spazio mesofaringeo in pazienti russatori con e senza apnee notturne. L'ampliamento dello spazio mesofaringeo così ottenuto previene infatti il contatto e la vibrazione delle pareti mesofaringee determinanti ostruzione inspiratoria causa di apnea o ipopnea. Il lifting velo-uvulofaringeo può essere, eventualmente, associato ad ulteriori procedure chirurgiche locali in pazienti selezionati.
Introduction
Snoring is a highly prevalent condition that affects 40- 60% of adults 1 and is caused by the oscillation of the soft palate and adjacent structures due to a critical sleep-related reduction in upper airway airflow induced by varying combinations of anatomical and neuromuscular factors 2. It not only affects the quality of sleep (of both patients and their bed partners), but may also have daytime consequences such as sleepiness, neurocognitive impairment and mood disturbances that may have a significant negative impact on the quality of life. Snoring is also a precursor of obstructive sleep apnoea-hypopnoea syndrome (OSAHS) 2, which is known to predispose to cardio- and cerebro-vascular diseases, and also cause motor vehicle accidents 2. Sleep-disordered breathing, including snoring with or without OSAHS, is therefore a serious burden on public health.
The conservative management of snoring includes weight loss, and the avoidance of alcohol and sedatives; furthermore, any associated nasal obstruction should be relieved medically or surgically 3. However, the effectiveness of nasal surgery in treating snoring is controversial as it has been reported that only 12-34% of patients benefit from nasal surgery alone 4-6. The surgical procedures used to treat mild OSAHS and snoring include resection techniques such as uvulopalatopharyngoplasty 7 and laserassisted or radiofrequency-assisted uvulopalatoplasty 8-10, which all give rise to severe postoperative discomfort and morbidity 11. On the other hand, the results of non-resective techniques such as radiofrequency volume reduction of the soft palate 12, injection scleroplasty 13 or expensive palatal implants (Pillar®) 14, are only transient and require revision 11.
In 2008 11, Hur proposed a sling snoreplasty technique in an OSAHS patient to "shorten, conglomerate and tense" the redundant soft tissues of the soft palate by means of the trans-mucosal introduction of permanent threads through the fibro-muscular plane of the soft palate, but without presenting any results in his extended paper. By tightening these threads, Hur 11 was able to obtain the desired modifications in the fibro-muscular tissues encircled by the sutures.
On the basis of that report, which clearly demonstrated the perfect tolerability of such sutures, we propose a combination of nasal surgery and a new palatal lifting technique using the permanent threads proposed by Hur and widely used in plastic surgery.
However, unlike Hur's procedure, our velo-uvulo-pharyngeal lift (VUPL) or "Roman blinds" technique (as it reproduces the mechanism of Roman blinds) not only lifts and stiffens the velo-uvular complex, but also widens the mesopharyngeal space to eliminate noisy vibrations or occlusions. This is done by using permanent threads that are anchored to three bony structures (two pterygoid hamuli, and the posterior nasal spine) and looped inside the fibro-muscular palatopharyngeal tissues.
Materials and methods
Study population
This preliminary prospective study involved four adult patients affected by snoring and with polysomnographic findings indicating mild OSAHS as defined by the American Academy of Sleep Medicine 15.
Inclusion criteria were nasal obstruction due to septal deformity requiring surgical correction; a positive history of snoring for at least five years; "excess" soft tissue structures within the oropharynx upon oropharyngeal inspection during maximal mouth opening with the tongue relaxed in the mouth, and/or narrowing or collapse in the retropalatal region without narrowing in the hypopharynx both at rest and during Muller's maneuver under fibre optic endoscopy; evidence of vibration localized only at the level of the mesopharyngeal structures during sleep endoscopic assessment 16.
Exclusion criteria were obstructive tonsillar hypertrophy (tonsil size > 2 according to Brodsky) 17; severe maxillary or mandibular deformities; severe or unstable cardiopulmonary, neurological or endocrine diseases; morbid obesity (BMI > 25 kg/m2); age > 65 years; active alcohol or illicit drug abuse; active smoking; psychotropic drugs; unstable and severe psychiatric disease; previous oropharyngeal surgery; and patient refusal. The patients gave their written informed consent to the surgical procedure.
Study setting
The study was carried out at the Department of Specialist Surgical Sciences, "Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico", University of Milan, Italy, between November 2008 and June 2010.
Pre-operative assessment
A careful general and ear nose and throat (EN T) history of each patient was taken with particular attention given to sleep history. Body mass index (BMI ) was computed, and all patients underwent overnight polysomnography with the determination of the apnoea hypopnoea index (AHI) and mean oxygen saturation to establish a diagnosis of OSAHS. Snoring was assessed with a 0-9 patient snoring scale score (SSS: 0 = no snoring; 9 = maximum loudness, frequency and periodicity of snoring) 18 and a 0-10 linear analogue scale (LAS snoring: 0 = no snoring; 10 = maximum loudness of snoring) 18 administered to their bed partners. Daytime sleepiness was also evaluated using the Epworth Sleepiness Scale (ESS) 19.
All patients also underwent a complete ENT evaluation, including an oropharyngeal inspection with the grading of tonsillar size according to Brodsky 17, anterior rhinoscopy, and fibre optic endoscopy of the nasal, pharyngeal and laryngeal district, both at rest and during Muller's manoeuvre.
Sleep endoscopy
Before the induction of anaesthesia, sleep endoscopy was performed to confirm the site of vibration and/or collapse during induced sleep. The nose-oropharyngeal-hypopharyngeal- laryngeal region classification (NOHL classification) according to Vicini et al. 20 21 was used to describe the site of vibration and/or collapse. During sleep endoscopy, the grade and the pattern of collapse and/or obstruction was assessed for each region (nose, oropharynx, hypopharynx and larynx) and expressed by means of a number (indicating the severity of collapse or obstruction) and a letter (indication the pattern of collapse for oropharynx, hypopharynx and larynx) 20 21.
Surgical technique
The procedure was performed under general anaesthesia, with the surgical field exposed using Dingmann mouth gags. The nasal surgery was done first (septoplasty according to back-and-forth technique) 22.
The surgeon sat at the top of the table, with the patient's neck hyper-extended to expose the posterior palate fully. VUPL was performed as follows (Fig. 1). Three short stab incisions were made through the fibromucosa of the bony palate until bone contact, one just before and ventrally to the posterior nasal spine, and two before each pterygoid hamulus. Using a long needle-holder, a cutting needle mounted on a 2-0 non-resorbable polyester thread (Mersilene, Ethicon Inc., Somerville, New Jersey, USA) was first stuck sideways into the posterior nasal spine through the periostium and the fibromuscolar layer of the soft palate, and then guided by means of multiple in-and-out transmucosal passages (each one performed through the same mucosal hole) along a semicircular way to exit at one side of the base of the uvula emerging into the oral cavity.
Fig. 1.
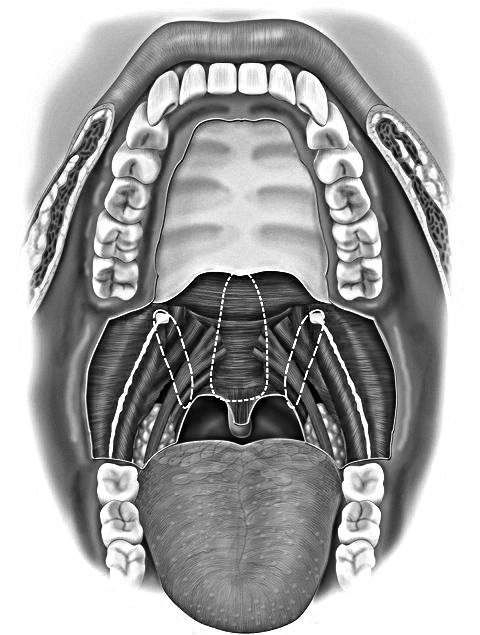
Representation of VUPL: a cutting needle was first stuck sideways into the posterior nasal spine through the periostium and the fibromuscolar layer of the soft palate, and then guided using multiple in-and-out transmucosal passages (dashed lines) to exit at one side of the base of the uvula. The needle was then re-inserted at the opposite side of the base of the uvula and driven through the fibro-muscular layer of the contralateral soft palate in a specular manner to the opposite side of the posterior nasal spine. A similar manoeuvre was performed bilaterally at the level of each pterygoid hamulus and at the level of the postero-superior face of the posterior tonsillar pillar.
The needle was then grasped with the needle-holder and re-inserted horizontally through the uvular muscle to reemerge through the buccal mucosa at the opposite side of the base of the uvula. Here, it was re-inserted through the same mucosal hole and driven through the fibro-muscular layer of the contralateral soft palate in a specular manner to the opposite side of the posterior nasal spine, where it exited through the periostium and the stab mucosal incision. The ends of the thread could then be tightly knotted and buried deeply in the stab incision which was closed with a 5-0 fast resorbable polyglactin suture (Vycril Rapide, Ethicon Inc., Somerville, New Jersey, USA).
A similar manoeuvre was performed bilaterally at the level of each pterygoid hamulus: the needle was driven through the fibrous tissue at the medial side of the pterygoid hamulus, through the soft palate musculature along a semicircular way using multiple in-and-out transmucosal passages (each one performed through the same mucosal hole) to exit through the mucosa at the level of the postero- superior face of the posterior tonsillar pillar.
Next, it was grasped with the needle holder and re-inserted through the same mucosal hole to embrace the palatopharyngeal muscle and then cross the soft palate fibromuscolar layer along a laterally convex path to reach the fibrous tissue at the lateral side of the pterygoid hamulus. The threads were then tightly knotted embracing the fibro- osseous structures of the pterygoid hamulus, and buried deep in the stab incision which was closed usinga 5-0 fast resorbable polyglactin suture (Vycril Rapide, Ethicon Inc., Somerville, New Jersey, USA).
Follow-up
An early ENT examination was made seven days after surgery, with post-operative morbidity being evaluated using a 0-10 visual analogue scale (VAS pain: 0 = no pain, and 10 = maximum pain) 23. Long-term post-operative followup included ENT examination, LAS 18, SSS 18 and ESS assessment 19. Patient satisfaction was also evaluated on the basis of a 0-10 visual analogue scale (VAS satisfaction: 0 = no patient satisfaction, and 10 = maximum patient satisfaction).
Results
Our case series consisted of four male patients with a median age of 44.5 years (range 42-65); the pre-operative demographic, clinical and polysomnographic findings are shown in Table I. All patients underwent VUPL combined with septoplasty without any significant intra- or postoperative complications.
Table I.
Demographic, clinical and polysomnographic findings.
| Patient | Gender | Age (years) | BMI (kg/m2) | Tonsillar size 17 | AHI (n/H) | Mean O2 saturation | NOHL classification 20,21 | Pre-operative ESS 19 | Post-operative ESS 19 | Pre-operative LAS 18 | Post-operative LAS 18 | Pre-operative SSS 18 | Post-operative SSS 18 | VAS pain 23 | VAS satisfaction | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 42 | 25.8 | 2 | 15 | 95.6 | N3O2cH0L0 | 10 | 8 | 8 | 0 | 8 | 0 | 3 | 10 | 25 |
| 2 | M | 46 | 28.0 | 1 | 16 | 94.0 | N2O1cH0L0 | 10 | 3 | 8 | 2 | 8 | 2 | 2 | 8.5 | 17 |
| 3 | M | 43 | 29.4 | 2 | 17 | 93.2 | N2O2cH0L0 | 13 | 3 | 7 | 2 | 6 | 2 | 4 | 10 | 14 |
| 4 | M | 65 | 29.0 | 1 | 14 | 94.5 | N2O1cH0L0 | 15 | 9 | 8 | 2 | 8 | 2 | 4 | 9 | 6 |
| Median | 44.5 | 28.5 | 2 | 15.5 | 94.2 | 11.5 | 5.5 | 8 | 2 | 8 | 2 | 3.5 | 9.5 | 15.5 |
M: male; BMI: body mass index; AHI: apnoea/hypopnoea Index; n: number; H: hour; NOHL: nose, oropharyngeal, hypopharyngeal, laryngeal region (site of vibration, site of collapse and obstruction during Sleep Endoscopy, according to Vicini et al. 20,21. In particular, pattern of collapse was evaluated according to the shape of the dynamic collapse in oropharyngeal, hypopharyngeal and laryngeal region as antero-posterior collapse (ap), transversal collapse (t), and circular collapse (c); the severity of collapse was graded as follows: grade 1 = 0-25% reduction in airways; grade 2 = 25-50% reduction in airways; grade 3 = 50-75% reduction in airways; grade 4 = 75-100% reduction in airways. Nasal obstruction was graded as follows: grade 1 = 0-25% reduction in nasal respiratory space; grade 2 = 25-50% reduction in nasal respiratory space; grade 3 = 50-75% reduction in nasal respiratory space; grade 4 = 75-100% reduction in nasal respiratory space 20,21; ESS: Epworth sleepiness scale 19; LAS: linear analogue scale 18; SSS: snoring scale score 18; VAS: visual analogue scale.
All patients reported an immediate subjective clinical improvement immediately after VULP. The most common complaints were mild oropharyngeal pain and a self-limiting sensation of velar fullness with mild swallowing pain, which spontaneously disappeared within two days. One of the patients reported a self-limiting and short-lasting sensation of a foreign oropharyngeal body.
After a median follow-up of 15.5 months (range 6-25), the improvement in snoring was confirmed by a reduction in LAS and SSS, and a reduction in daytime sleepiness as assessed by the ESS. Furthermore, all patients recorded high VAS satisfaction values. ENT examination showed a stable retraction of the soft velo-uvulo-pharyngeal tissues with enlargement of the mesopharyngeal space, and complete visualization of the posterior pharyngeal wall (Fig. 2A-B). Partial knot extrusion was discovered in one patient, but without any subjective symptoms or clinical implications. No nasopharyngeal regurgitation or voice change occurred. Table I details the post-operative findings.
Fig. 2.


In, A. pre-operative view of a "excess" soft tissue structures is shown within the oropharynx upon oropharyngeal inspection during maximal mouth opening with the tongue relaxed in the mouth. Note the velar collapse at the level of posterior oro-pharyngeal wall; in B. a post-operative view is seen (followup: 14 months) showing retraction of the soft velo-uvulo-pharyngeal tissues with enlargement of the mesopharyngeal space, and complete visualization of the posterior pharyngeal wall.
Discussion
The VUPL or "Roman blinds" technique (as it reproduces a Roman blind mechanism) shares the use of permanent threads for tissue suspension and/or mobilization with plastic surgery techniques such as rhytidectomy, rhinoplasty and blepharoplasty for ptosis 24-26, and ENT procedures such as the "endo-extralaryngeal suture technique" devised by Lichtemberger and Toohill 27.
The aim of VUPL is to lift the velo-uvular complex, enlarge and advance the oropharyngeal inlet, and widen the mesopharyngeal space by acting on the palato-pharyngeal fibromuscular tissues through the insertion of permanent threads anchored to strong and fixed structures (the fibroosseous tissue at the level of the posterior nasal spine and the pterygoid hamuli). In addition, the procedure also allows the useful stiffening and shortening of the soft palate to obtain a more rigid and less vibration-prone structure: by advancing and lateralizing each palato-pharyngeal muscle within the posterior tonsillar pillar, it is possible to widen the oropharyngeal inlet while advancing the posterior border of the soft palate.
The use of fibro-osseous structures as anchoring points is a completely new conception of the sling snoreplasty proposed by Hur 11 as a reversible and minimally-invasive technique based on the use of permanent threads coarctating the fibromuscular layer in order to "shorten, conglomerate and tense" the redundant palatal tissue. In our opinion, anchoring the threads to the strong and deep fibro-osseous structures (the posterior nasal spine and pterygoid hamuli) provides a more conspicuous benefit by lifting the palate and widening the mesopharyngeal space. The structural and dynamic modifications produced by the VUPL (increasing upper oropharyngeal and retropalatal airway size) can be compared with those offered by more invasive transpalatal advancement pharyngoplasty 28, a technique that proved to be very efficacious despite the high rate of complications. However, the theoretical effectiveness of the VUPL in the long-lasting rehabilitation of the oropharyngeal space needs to be confirmed over a longer follow-up period.
In comparison with traditional techniques of surgical resection such as uvulopalatopharyngoplasty and laser/ radiofrequency-assisted uvulopalatoplasty 7-10, VUPL is conservative and minimally invasive, has a selective action on the palato-pharyngeal mucosa, fibrous tissues and muscles, and can be combined with other surgical procedures such as septoplasty, turbinoplasty and tonsillectomy in the case of further anatomical anomalies impairing physiological airflow. Moreover, on the basis of our findings, it is simple, cost-effective and well-tolerated by patients. The main complaint was moderate oropharyngeal pain, which rapidly and spontaneously disappeared; there were no other significant postoperative morbidities or complications.
It also seems capable of providing immediate snoring relief, and it could theoretically be performed in selected patients under local anaesthesia in one-day surgery settings after adequate training and with the employment of new devices to decrease the surgical time.
VUPL also differs from non-resective surgical techniques such as radiofrequency volume reduction of the soft palate, palatal implants (Pillar®) and injection scleroplasty 12-14 insofar as it is completely reversible: in the case of patient discomfort, the previous anatomical condition can be fully restored just by cutting the thread in an outpatient setting. Moreover, as it does not definitely impair the baseline anatomical pattern, it could also be repeated even after a short time if necessary.
Conclusions
On the basis of these encouraging preliminary results, we believe that the VULP (combined with other surgical procedures if indicated) can be considered a valid surgical option to relieve snoring, although our findings need to be confirmed by studies of larger case series with longer follow-up periods.
References
- 1.Ohayon MM, Guilleminault C, Priest RG, et al. Snoring and breathing pauses during sleep: telephone interview survey of a United Kingdom population sample. BMJ. 1997;314:860–863. doi: 10.1136/bmj.314.7084.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cistulli PA, Gotsopoulos H, Marklund M, et al. Treatment of snoring and obstructive sleep apnea with mandibular repositioning appliances. Sleep Med Rev. 2004;8:443–457. doi: 10.1016/j.smrv.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Collard P, Rodenstein DO. Management of simple snoring in adults. Monaldi Arch Chest Dis. 1993;48:623–626. [PubMed] [Google Scholar]
- 4.Friedman M, Tanyeri H, Lim JW, et al. Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000;122:71–74. doi: 10.1016/S0194-5998(00)70147-1. [DOI] [PubMed] [Google Scholar]
- 5.Kim ST, Choi JH, Jeon HG, et al. Polysomnographic effects of nasal surgery for snoring and obstructive sleep apnea. Acta Otolaryngol. 2004;124:297–300. doi: 10.1080/00016480410016252. [DOI] [PubMed] [Google Scholar]
- 6.Li HY, Lee LA, Wang PC, et al. Nasal surgery for snoring in patients with obstructive sleep apnea. Laryngoscope. 2008;118:354–359. doi: 10.1097/MLG.0b013e318158f73f. [DOI] [PubMed] [Google Scholar]
- 7.Gallina S, Dispenza F, Kulamarva G, et al. Uvulopalatopharyngoplasty with tonsillectomy in the treatment of severe OSAS. B-ENT. 2009;5:245–250. [PubMed] [Google Scholar]
- 8.Halme P, Toskala E, Laurikainen E, et al. LUPP relieves partial upper airway obstruction during sleep in patients with velopharyngeal narrowing. Acta Otolaryngol. 2010;130:614–619. doi: 10.3109/00016480903311872. [DOI] [PubMed] [Google Scholar]
- 9.Kyrmizakis DE, Chimona TS, Papadakis CE, et al. Laserassisted uvulopalatoplasty for the treatment of snoring and mild obstructive sleep apnea syndrome. J Otolaryngol. 2003;32:174–179. doi: 10.2310/7070.2003.40423. [DOI] [PubMed] [Google Scholar]
- 10.Yoruk O, Akgun M, Sutbeyaz Y, et al. Treatment of primary snoring using modified radiofrequency-assisted uvulopalatoplasty. Eur Arch Otorhinolaryngol. 2009;266:1807–1814. doi: 10.1007/s00405-009-0926-7. [DOI] [PubMed] [Google Scholar]
- 11.Hur J. A new treatment for snoring: sling snoreplasty with a permanent thread. Acta Otolaryngol. 2008;128:1381–1384. doi: 10.1080/00016480801968500. [DOI] [PubMed] [Google Scholar]
- 12.Hofmann T, Schwantzer G, Reckenzaun E, et al. Radiofrequency tissue volume reduction of the soft palate and UPPP in the treatment of snoring. Eur Arch Otorhinolaryngol. 2006;263:164–170. doi: 10.1007/s00405-005-0959-5. [DOI] [PubMed] [Google Scholar]
- 13.Brietzke SE, Mair EA. Injection snoreplasty: extended follow- up and new objective data. Otolaryngol Head Neck Surg. 2003;128:605–615. doi: 10.1016/S0194-59980300229-8. [DOI] [PubMed] [Google Scholar]
- 14.Friedman M, Vidyasagar R, Bliznikas D, et al. Patient selection and efficacy of pillar implant technique for treatment of snoring and obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2006;134:187–196. doi: 10.1016/j.otohns.2005.10.032. [DOI] [PubMed] [Google Scholar]
- 15. American Academy of Sleep Medicine , author. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–689. [PubMed] [Google Scholar]
- 16.Soares MC, Sallum AC, Gonçalves MT, et al. Use of Muller's maneuver in the evaluation of patients with sleep apnea -literature review. Braz J Otorhinolaryngol. 2009;75:463–466. doi: 10.1016/S1808-8694(15)30667-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brodsky L. Modern assessment of tonsils and adenoids. Pediatr Clin North Am. 1989;36:1551–1569. doi: 10.1016/s0031-3955(16)36806-7. [DOI] [PubMed] [Google Scholar]
- 18.Lim PV, Curry AR. A new method for evaluating and reporting the severity of snoring. J Laryngol Otol. 1999;113:336–340. doi: 10.1017/s0022215100143919. [DOI] [PubMed] [Google Scholar]
- 19.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 20.Vito A, Agnoletti V, Berrettini S, et al. Drug-induced sleep endoscopy: conventional versus target controlled infusion techniques-a randomized controlled study. Eur Arch Otorhinolaryngol. 2010;268:457–462. doi: 10.1007/s00405-010-1376-y. [DOI] [PubMed] [Google Scholar]
- 21.Vicini C, Corso RM, Gambale G. Sleep endoscopy e sistema NOHL. In: Vicini C, editor. Chirurgia della Roncopatia. Lucca: Eureka; 2007. pp. 59–70. [Google Scholar]
- 22.Mantovani M, Mazzola RF, Cioccarelli MG. The back-andforth septoplasty. Plast Reconstr Surg. 1996;97:40–44. doi: 10.1097/00006534-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Briggs M, Closs JS. A descriptive study of the use of visual analogue scales and verbal rating scales for the assessment of postoperative pain in orthopedic patients. J Pain Symptom Manage. 1998;18:438–446. doi: 10.1016/s0885-3924(99)00092-5. [DOI] [PubMed] [Google Scholar]
- 24.Giampapa VC, Bernardo BE. Neck recontouring with suture suspension and liposuction: an alternative for the early rhytidectomy candidate. Aesthetic Plast Surg. 1995;19:217–223. doi: 10.1007/BF00451093. [DOI] [PubMed] [Google Scholar]
- 25.Gamboa GM, Vasconez LO. Suture suspension technique for midface and neck rejuvenation. Ann Plast Surg. 2009;62:478–481. doi: 10.1097/SAP.0b013e31818c4b45. [DOI] [PubMed] [Google Scholar]
- 26.Inanli S, Serin GM, Kantürk Y, et al. Nasal tip-suspending suture technique: cat's nape suture. J Craniofac Surg. 2010;21:863–865. doi: 10.1097/SCS.0b013e3181d7ae28. [DOI] [PubMed] [Google Scholar]
- 27.Lichtenberger G, Toohill RJ. Technique of endo-extralaryngeal suture lateralization for bilateral abductor vocal cord paralysis. Laryngoscope. 1997;107:1281–1283. doi: 10.1097/00005537-199709000-00023. [DOI] [PubMed] [Google Scholar]
- 28.Woodson BT, Toohill RJ. Transpalatal advancement pharyngoplasty for obstructive sleep apnea. Laryngoscope. 1993;103:269–276. doi: 10.1288/00005537-199303000-00006. [DOI] [PubMed] [Google Scholar]


