Abstract
Objective
Long-term outcomes after participation in a structured diabetes treatment and teaching program (DTTP) for patients with diabetes without insulin use, primarily based upon postprandial urine glucose self-monitoring (UGSM).
Methods
A total of 126 patients took part in the DTTP in a university outpatient department in 2004–2005. We re-evaluated 119 (94.4%) at baseline and at 6 months, 12 months, and 24 months. Hemoglobin A1c (HbA1c) was DCCT adjusted.
Results
HbA1c decreased significantly 6 months after education from 7.33% (±1.59%) to 6.89% (±0.98%; P = 0.001 versus baseline) and was maintained for up to 12 months (7.02% ± 1.07%; P = 0.017 versus baseline) as well as up to 24 months (6.96% ± 1.06%; P = 0.005 versus baseline). Weight decreased from 92.5 kg at baseline to 90.3 kg at 24 months (P = 0.014). A total of 36.5% of patients not on insulin therapy preferred UGSM, whereas 23.5% preferred blood glucose monitoring, at 24 months. Glucose control was similar in both groups at 24 months (HbA1c UGSM 7.03 versus blood glucose monitoring 6.97%; P = 0.807).
Conclusion
Participation in the DTTP resulted in long-term behavior modification. HbA1c of patients without insulin met the target 24 months after the DTTP, irrespective of the type of glucose self-monitoring.
Keywords: diabetes mellitus type 2, treatment and teaching program, patient education, HbA1c, body weight
Introduction
Type 2 diabetes mellitus affects about 5% of the German population.1 Eighty percent of patients with type 2 diabetes are treated with diet or oral antiglycemic drugs (OADs).2 For successful treatment of patients with diabetes, we have different therapy options, such as modification of eating behavior and physical exercise, OADs, and insulin. A necessary prerequisite of successful treatment is the active involvement of the patients in their treatment. Continuous adjustment of nutrition, exercise, and medication according to the patient’s insulin secretion and/or insulin resistance is necessary for the treatment of diabetes mellitus. Therefore, diabetes education is crucial, whatever therapeutic option is chosen.
Diabetes education contributes to better metabolic control or to preservation of good control.3,4 However, some reviews on the effectiveness of education in type 2 diabetes have also reported positive effects on patient knowledge, self- care behavior, and psychological outcomes.5–7 The duration of effective diabetes education programs is controversial. The trials evaluating the majority of these treatment and teaching programs have only a relatively short follow-up period of 6–12 months.3,4,8 Another controversial topic is whether blood glucose self-monitoring (BGSM) has advantages over urine glucose self-monitoring (UGSM) in patients not requiring insulin therapy.9–12
A structured diabetes treatment and teaching program (DTTP) for patients with type 2 diabetes not on insulin therapy was implemented in the German health care system several years ago. This program comprised four sessions of 90 minutes each. It is primarily based upon postprandial UGSM. The first evaluation of this DTTP in Germany with a follow-up of 12 months was published 20 years ago.3 Another evaluation from Austria published in 1995 had a follow-up of 6 months.4
However, longer follow-up periods have hitherto not been studied. We evaluated outcomes 24 months after participation in this DTTP.
Patients and methods
A total of 126 patients with type 2 diabetes mellitus not requiring insulin therapy took part in the DTTP in 2004–2005 in the outpatient department for endocrinology and metabolic diseases of the university hospital in Jena, Germany. All patients with newly diagnosed type 2 diabetes or problems with metabolic control were enrolled in the DTTP. Medication, type and frequency of self-monitoring, severe hypoglycemia, hemoglobin A1c (HbA1c), weight, and blood pressure were recorded before the DTTP and then at every visit, usually quarterly. We re-evaluated complete data sets from 119 patients. Data were obtained from the electronic patient record EMIL® (v4.3.9.79; Marburg, Germany) were collected from general practitioners’ files. Data are described at baseline (before DTTP) and at 6 months, 12 months, and 24 months after participation in the DTTP. HbA1c was adjusted to DCCT standards with an evaluated standardization procedure using local reference ranges.13
Diabetes treatment and teaching program
The DTTP consists of four sessions once a week of 90–120 minutes, including interactive training. The topics of the DTTP are basic information about diabetes, postprandial self-monitoring of urine glucose, physiology and pathophysiology, hypocaloric nutrition, withdrawal of insulinotropic oral agents when unnecessary, foot care, hypoglycemia, and exercise (for details, see Table 1). Patients were trained to achieve glucose-free urine 2 hours postprandially and to tailor the type and amount of their food accordingly. If postprandial glucosuria-free tests correlated with the desired level of metabolic control, this inexpensive testing was considered to be sufficient. The main teaching part of the DTTP was performed by diabetes educators (ie, nurses and dieticians with special postgraduate training).
Table 1.
Structured treatment and teaching program
| Education unit | Information topic |
|---|---|
| Unit 1 | What is diabetes? |
| Postprandial urine glucose self-monitoring | |
| Hypoglycemia | |
| Unit 2 | Pathophysiology of diabetes |
| Oral hypoglycemic agents | |
| Nonpharmacological therapy | |
| Calorie-defined diet | |
| Lifestyle changes | |
| Unit 3 | Diabetic neuropathy |
| Foot care | |
| Physical activity | |
| Unit 4 | Sick-day rules |
| Smoking | |
| Check-up for late complications |
Outcomes
Primary outcomes are changes in HbA1c, weight, and OADs 24 months after training in the DTTP. A secondary outcome is the difference in HbA1c between self-monitoring of urine glucose and blood glucose.
Statistical analysis
Statistical analysis was performed with SPSS 14.0 (SPSS, Inc, Chicago, IL). Normally distributed values were registered as mean ± standard deviation and non-normally distributed values as median and range. Differences were statistically evaluated by t-test, Mann-Whitney U Test, or χ2 test. A P-value of <0.05 was considered to be statistically significant.
Results
From the initial 126 trained patients we were able to re-evaluate 119 (94%) after 24 months. At baseline, age was 61.5 years (±10.29 years), time since diagnosis of diabetes was 5.57 years (±6.53 years), body weight was 89.89 kg (±15.88 kg), body mass index was 32.23 kg/m2 (±5.74 kg/m2), and blood pressure was 159/88 mmHg (±24.69/±12.18 mmHg). Of the patients, 39.4% (n = 47) were newly diagnosed with type 2 diabetes, and 59.7% (n = 71) were still cared for in the university outpatient department.
HbA1c decreased significantly 6 months after education from 7.33% (±1.59%) to 6.89% (±0.98%; P = 0.001 versus baseline) and was maintained for up to 12 months (7.02 ± 1.07%; P = 0.017 versus baseline), as well as up to 24 months (6.96 ± 1.06%; P = 0.005 versus baseline). Patients still attending our university outpatient department had a higher baseline HbA1c than patients of general practitioners (7.61% versus 6.94%; P = 0.024) and also a higher HbA1c 12 months (7.23% versus 6.69%; P = 0.008) and 24 months after education (7.18% versus 6.65%; P = 0.007). HbA1c decreased in both groups, but the change was significant only in patients cared for at the university hospital (P = 0.027). At baseline, 49.6% of patients had an HbA1c of ≤ 7% and 10.1% > 9%. Twelve months after participation in the DTTP, the number of patients with an HbA1c ≤ 7% increased to 60.0% (P = 0.001), whereas the number with an HbA1c > 9% decreased to 3.5% (P = 0.069). These results were maintained after 24 months, with 58.8% having an HbA1c ≤ 7% and 5% > 9% (P = 0.112 versus baseline). Body weight decreased significantly from 89.9 kg at baseline to 87.8 kg after 6 months (P = 0.001), increased to 88.9 kg at 12 months (P = 0.001 versus baseline), and was 88.5 kg 24 months later (−1.4 kg compared with baseline; P = 0.001). Blood pressure decreased from 159/87 mmHg to 140/81 mmHg (P = 0.001) 24 months after participation in the DTTP.
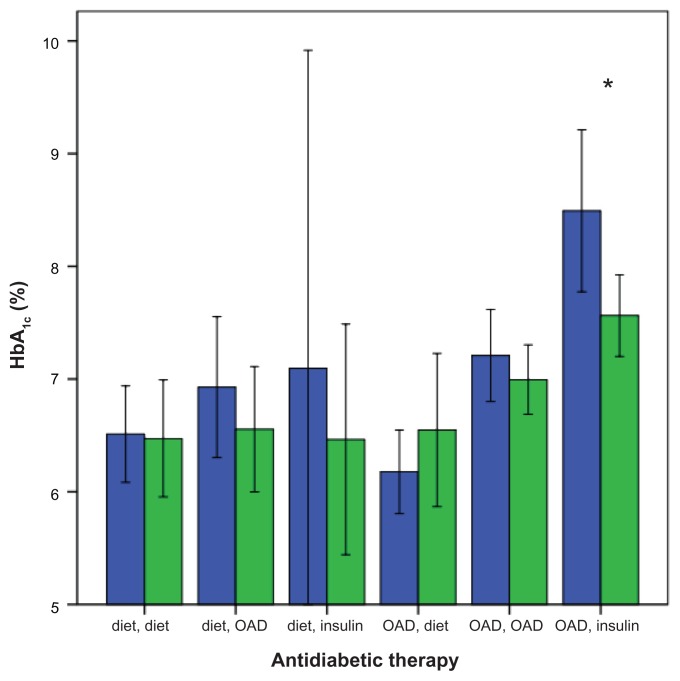
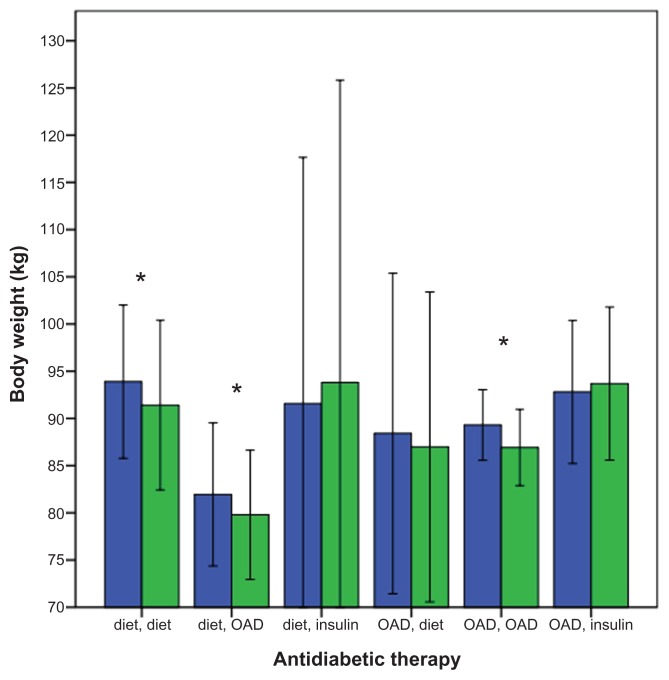
Antidiabetic medication
Changes in HbA1c and body weight are shown in Table 2, changes in HbA1c according to diabetes therapy at baseline and at 24 months are shown in Figure 1, and changes in body weight according to therapy are depicted in Figure 2. At baseline, 31.1% of the patients were not on antidiabetic medication (HbA1c 6.75%), and 68.9% were on OADs (HbA1c 7.60%). Twenty-four months after the DTTP, 19.3% were still not on antidiabetic medication. The baseline HbA1c of this subgroup was 6.42% and remained constant (6.49% at 24 months; not significant). The body weight of this group decreased significantly from 92.5 kg at baseline to 90.3 kg at 24 months (P = 0.014).
Table 2.
HbA1c and body weight according to diabetes therapy used at 24 months
| Antidiabetic therapy at 24 months | HbA1c (%) | Body weight (kg) | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Baseline | 24 months | P-value | Baseline | 24 months | P-value | |
| All patients | 7.33 | 6.96 | 0.001 | 89.9 | 88.5 | 0.001 |
| No drug (19.3%) | 6.42 | 6.49 | NS | 92.5 | 90.3* | 0.014 |
| OAD (52.1%) | 7.14 | 6.88 | NS | 87.4 | 85.1* | 0.001 |
| Insulin (28.6%) | 8.33 | 7.43* | 0.01 | 92.7 | 93.7 | 0.088 |
Abbreviations: HbA1c, hemoglobin A1c; NS, not significant; OAD, oral antiglycemic drug.
Figure 1.
Changes in HbA1c at 24 months according to antidiabetic therapy used at baseline (blue bars) and 24 months (green bars).
Note: *P < 0.05.
Abbreviations: HbA1c, hemoglobin A1c; OAD, oral antiglycemic drug.
Figure 2.
Changes in body weight at 24 months according to antidiabetic therapy used at baseline (blue bars) and 24 months (green bars).
Note: *P < 0.05.
Abbreviation: OAD, oral antiglycemic drug.
The HbA1c values of patients taking OADs at 24 months (52.1%) decreased slightly (7.14% at baseline; 6.88% at 24 months; not significant), whereas body weight decreased significantly from 87.4 kg at baseline to 85.1 kg at 24 months (P = 0.001).
HbA1c of patients with insulin treatment at 24 months (28.6%) decreased significantly from 8.33% at baseline to 7.43% (P = 0.011), but body weight increased from 92.7 kg to 93.7 kg (P = 0.088). Patients attending the university outpatient department were more often on insulin therapy at 24 months than patients in the care of a general practitioner (43.7% versus 6.3%, P = 0.001).
Self-monitoring
The methods of self-monitoring according to diabetes therapy are shown in Table 3. Only 53.8% of the patients performed self-monitoring at baseline, compared with 75.6% at 24 months. UGSM was performed at baseline by 31.1% and at 24 months by 26.1%. BGSM was performed at baseline by 18.5% and at 24 months by 44.5%. Both methods, UGSM and BGSM, were used at baseline by 4.2% and at 24 months by 5.0%. Of those patients not on insulin therapy at 24 months, more preferred UGSM (36.5% versus 23.5%, P = 0.048).
Table 3.
Methods of self-monitoring (percent patients) according to antidiabetic therapy used
| Antidiabetic therapy at 24 months | No self-monitoring | Urine glucose | Blood glucose | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Baseline | 2 years | Baseline | 2 years | Baseline | 2 years | |
| All patients | 46.2 | 24.4 | 31.1 | 26.1 | 18.5 | 44.5 |
| No drug | 67.6 | 52.2 | 16.2 | 43.5 | 10.8 | 4.3 |
| OAD | 36.6 | 27.4 | 37.8 | 33.9 | 22.0 | 30.6 |
| Insulin | 2.9 | 97.1 | ||||
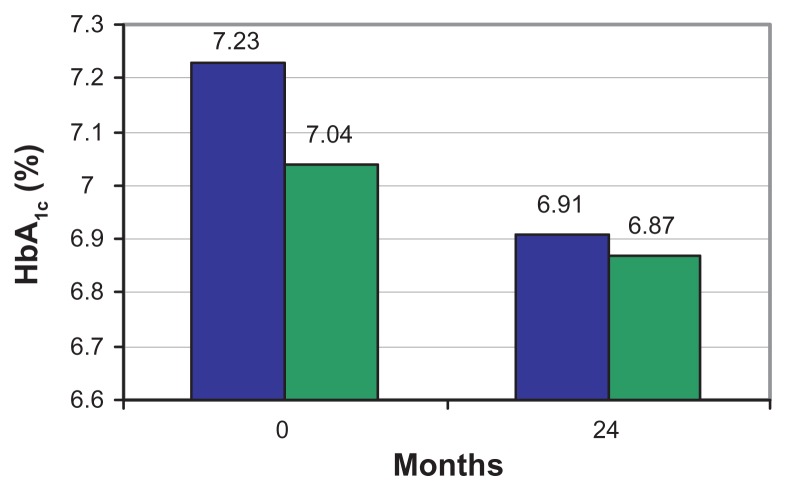
There were differences concerning the self-monitoring method applied between those patients who were exclusively treated by a general practitioner and those who also attended the university outpatient department. All patients treated in the university outpatient department used one kind of self monitoring (UGSM or BGSM), but only 39.6% of patients treated by their general practitioner performed self monitoring (P = 0.001). At 24 months, most patients not requiring insulin therapy and treated in the university outpatient department performed UGSM (UGSM 65%; BGSM 22.5%). This compares with those patients who were treated by their general practitioner with most of them performing BGSM (UGSM 11.1%; BGSM 24.4%). Comparing the HbA1c of those patients not requiring insulin therapy applying UGSM or BGSM, no difference was found either at baseline (7.23% versus 7.04%; P = 0.597) or at 24 months (6.91% versus 6.87%; P = 0.855; Figure 3).
Figure 3.
Hemoglobin A1c(HbA1c) according to the method of self-monitoring used at baseline and 24 months after participation in the diabetes treatment and teaching program (urine glucose self-monitoring [blue bars]; blood glucose self-monitoring [green bars]).
Discussion and conclusion
The first evaluation of DTTP for patients with type 2 diabetes not requiring insulin therapy was published in 1988.3 The program was primarily developed for general practitioners to improve care for diabetic patients. We studied the long-term effects of this program. The follow-up of the first evaluation was 12 months. Patients had a significant reduction in bodyweight of 2 kg and the already good HbA1c at study entry did not deteriorate in spite of 30% less OADs used and none of the patients switching to insulin. The following evaluations of this DTTP in Austria and Latin America showed reductions in HbA1c ranging from 0.4% to 1.1% after a follow-up of 6–12 months,4,16–18 and a body weight reduction of 2.5 kg. These favorable results are also shown in our study but with a considerably longer follow-up of 24 months. The recently published DESMOND (Diabetes Education and Self Management for Ongoing and Newly Diagnosed) study in the UK evaluated the effectiveness of another group education program in people with newly diagnosed type 2 diabetes mellitus19 and found that 12 months after education there was a greater weight reduction for those patients than for patients in the control group (−2.98 kg versus −1.86 kg), without there being a difference in HbA1c.
It is well known that a reduction in body weight reduces insulin resistance in patients with type 2 diabetes, which results in better metabolic control.3,8,14,18 In contrast to these results, patients in the UK Prospective Diabetes Study assigned to diet therapy only had weight gain and the worst HbA1c. The different results might be caused by the DTTP initiating behavior modification by the participating patients and the possibility of continuous feedback by self-monitoring. A further reason for encouraging results is the absence of a diet plan in the curriculum used in our study. Except for drinks with sugar and instant food, all nutrients are allowed. Type and amount of food corresponds to the endogenous insulin present and to the person’s individual insulin resistance if postprandial urine glucose tests are negative.
Lifestyle interventions are effective, particularly in obese type 2 diabetes patients, but, in the long term, insulin treatment will become necessary in many people with type 2 diabetes. 15 After 24 months, 29% of our patients were on insulin therapy. Initially, these patients had the worst baseline HbA1c but the greatest improvement in metabolic control. Before starting insulin therapy these patients took part in another DTTP conceived for patients with insulin therapy. All those patients switched to insulin after the first evaluation of this program after 12 months.3 In the evaluation from Pieber et al,4 no patient was on insulin therapy 6 months after education. However, the HbA1c value 6 months after education was 8.11% and considerably higher than in the study presented.
Not surprisingly, patients on insulin therapy gained weight, as was reported in other studies starting with insulin treatment.15 However, weight gain was only 1 kg after 2 years.
The number of sessions recommended in DTTPs is debatable. The outcome of the DTTP with only four sessions is not worse compared with a program with eight or twelve sessions.8 This program decreased HbA1c from 8.1% to 7.4% and weight from 87.8 kg to 85.3 kg. The highest decrease of HbA1c was in patients on insulin, so the significant total HbA1c reduction mainly derives from the reduction in HbA1c of patients on insulin therapy. It was not the target of the DTTP to reduce the good HbA1c, which was already at baseline in the target. The aim for these patients was to maintain good HbA1c for longer, and this aim was achieved.
It is likely that it is not the number of sessions that is important but the delivery of the program by the team who is responsible for the permanent care of the patient. This is usually the family physician or general practitioner.
In the DTTP presented and evaluated, all patients not requiring insulin therapy are trained to perform postprandial urine tests for glucose. If postprandial urine is glucose free and matches the desired level of metabolic control after 3–6 months, this inexpensive testing is considered to be sufficient. Nevertheless, some subgroups may require BGSM (eg, patients with elevated or reduced renal threshold for glucose). Whether BGSM has any advantages in patients not requiring insulin therapy treatment has been repeatedly evaluated and discussed. In a retrospective study from Germany, Martin et al10 showed a decreased diabetes-related morbidity and all-cause mortality in type 2 diabetes patients who received a prescription of BGSM material in spite of higher HbA1c, compared with those not using BGSM, and this association was also present in a subgroup of patients not receiving insulin therapy. In the Fremantle study from Australia, Davis et al11 did not find any difference in HbA1c in BGSM users or nonusers, but BGSM was associated with a 79% increased risk of cardiovascular mortality in patients not treated with insulin.20 In addition, a large survey from Austria and Germany did not show any association between HbA1c and the frequency of BGSM in type 2 diabetic patients not requiring insulin therapy.21 In the randomized controlled trials by Miles et al9 and the recently published DESMOND study, BGSM was not superior to UGSM in respect of no self-control in patients with newly diagnosed type 2 diabetes.12 The results of our study support those findings that UGSM is not inferior to BGSM in well-trained patients, considering that most patients not requiring insulin therapy performed UGSM and that no difference in HbA1c after 2 years was found.
The strongest limitation of our study is the lack of a control group. For ethical reasons, it is not possible to refuse patients participation in the DTTP over 2 years. Furthermore, there are already controlled trials that have shown the effectiveness of the DTTP but over a shorter period.3,4 Another limitation is the possibility of a negative selection of patients, because we are a specialist university outpatient department. However, the good HbA1c of the patients is contradicted.
In summary, the results of our study showed that a treatment and teaching program consisting of four sessions once a week effectively reduces HbA1c and weight over 2 years, irrespective of the method of self-monitoring applied.
Conclusion
Weight decreased significantly in patients with and without OADs. HbA1c of patients without OADs still met the target after 24 months. In patients on OADs, HbA1c fell 0.26% below the initial level. Twenty-nine percent of patients were on insulin therapy 24 months after the DTTP. Glucose control (HbA1c) was similar with UGSM (7.03%) and BGSM (6.97%; P = 0.807) at 24 months. These findings suggest that postprandial urine testing is effective, as well as blood glucose control. More research is required to assess whether there is a difference in effectiveness between these types of self-monitoring. Patient education should be an integral part of the diabetes treatment, and all patients should have the opportunity to participate in the DTTP.
Acknowledgments
Supported by the Society for the support of Structured Treatment and Teaching Programmes (registered association under German law).
Footnotes
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.Federal Statistical Office, the Robert Koch Institute. Gesund-heitsberichterstattung des Bundes] Jul, 2006. Federal Health Monitoring [Statistisches Bundesamt, Robert-Koch-Institut. [German.] [Google Scholar]
- 2.Hansen B, Altenhofen L, Haß W, Blaschy S, Kretschmann J. Report of the Disease Management Programmes 2007 in Northrhine: breast cancer, diabetes mellitus type 1 and type 2, coronary artery disease, Asthma, COPD. KV Northrhine. 2008. [Accessed January 27, 2012]. Available from: http://www.kvno.de/importiert/qualbe_dmp07.pdf.
- 3.Kronsbein P, Jörgens V, Mühlhauser I, Scholz V, Venhaus A, Berger M. Evaluation of a structured treatment and teaching programm on non-insulin- dependent diabetes. Lancet. 1988;2:1407–1411. doi: 10.1016/s0140-6736(88)90595-8. [DOI] [PubMed] [Google Scholar]
- 4.Pieber TR, Holler A, Siebenhofer A, et al. Evaluation of a structured teaching and treatment programme for type 2 diabetes in general practice in a rural area of Austria. Diabet Med. 1995;12:349–354. doi: 10.1111/j.1464-5491.1995.tb00491.x. [DOI] [PubMed] [Google Scholar]
- 5.Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: a meta-analysis and meta-regression. Patient Educ Couns. 2004;52:91–105. doi: 10.1016/s0738-3991(03)00016-8. [DOI] [PubMed] [Google Scholar]
- 6.Padgett D. Meta-analysis of the effects of educational and psychosocial interventions on management of diabetes mellitus. J Clin Epidemiol. 1988;41:1007–1030. doi: 10.1016/0895-4356(88)90040-6. [DOI] [PubMed] [Google Scholar]
- 7.Brown S. Meta-analysis of diabetes patient education research: variations in intervention effects across studies. Res Nurs Health. 1992;15:409–419. doi: 10.1002/nur.4770150603. [DOI] [PubMed] [Google Scholar]
- 8.Kulzer B, Hermanns N, Reinecker H, Haak T. Effects of self-management training in type 2 diabetes: a randomized, prospective trial. Diabet Med. 2007;24:415–423. doi: 10.1111/j.1464-5491.2007.02089.x. [DOI] [PubMed] [Google Scholar]
- 9.Miles P, Evverett J, Murphy J, Kerr D. Comparison blood or urine testing by patients with newly diagnosed non-insulin dependend diabetes: patient survey after randomised crossover trial. BMJ. 1997;315:348–349. doi: 10.1136/bmj.315.7104.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin S, Schneider B, Heinemann L, et al. Self-monitoring of blood glucose in type 2 diabetes and long-term outcome: an epidemiological cohort study. Diabetologia. 2006;49:271–278. doi: 10.1007/s00125-005-0083-5. [DOI] [PubMed] [Google Scholar]
- 11.Davis WA, Bruce DG, Davis ME. Is self monitoring of blood glucose appropriate for all type 2 diabetic patients? The Fremantle Diabetes Study. Diabetes Care. 2006;29:1764–1770. doi: 10.2337/dc06-0268. [DOI] [PubMed] [Google Scholar]
- 12.O’Kane M, Bunting B, Copeland M, Coates V. Efficacy of self monitoring of blood glucose in patients with newly diagnosed type 2 diabetes (ESMON study): randomised controlled trial. BMJ. 2008;336:1174–1177. doi: 10.1136/bmj.39534.571644.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Müller UA, Femerling M, Reinauer KM, et al. Intensified treatment and education of type 1 diabetes as clinical routine. A nationwide quality-circle experience in Germany. ASD (the working groups on structured diabetes therapy of the German Diabetes Association) Diabetes Care. 1999;22(suppl 2):B29–B34. [PubMed] [Google Scholar]
- 14.UK Prospective Diabetes Study (UKPDS) Group. Response of fasting plasma glucose to diet therapy in newly presenting type 2 diabetic patients. Metabolism. 1990;39:905–912. [PubMed] [Google Scholar]
- 15.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulfonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 16.Domenech MI, Assad D, Mazzei ME, Kronsbein P, Gagliardino JJ. Evaluation of the effectiveness of an amulatory teaching/treatment programme for non-insulin dependent (type 2) diabetic patients. Acta Diabetologica. 1995;32:143–147. doi: 10.1007/BF00838482. [DOI] [PubMed] [Google Scholar]
- 17.Gagliardino JJ, Etchegoyen G for the PEDNID-LA Research Group. A Model education programme for people with type 2 diabetes. A cooperative Latin American implementation study (PEDNIN-LA) Diabetes Care. 2001;24:1001–1007. doi: 10.2337/diacare.24.6.1001. [DOI] [PubMed] [Google Scholar]
- 18.Korsatko S, Habacher W, Rakovac I, et al. Evaluation of teaching and treatment program in over 4000 type 2 diabetic patients after introduction of reimbursement policy for physicians. Diabetes Care. 2007;30:1584–1586. doi: 10.2337/dc06-2095. [DOI] [PubMed] [Google Scholar]
- 19.Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the Diabetes Education and Self Management Ongoing and Newly Diagnosed ( DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ. 2008;336:491–495. doi: 10.1136/bmj.39474.922025.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Davis WA, Bruce DG, Davis ME. Does self-monitoring of blood glucose improve outcome in type 2 diabetes? The Fremantle Diabetes Study. Diabetologia. 2007;50:510–515. doi: 10.1007/s00125-006-0581-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schütt M, Kern W, Krause U, et al. Is the frequency of self blood glucose measurements related to longterm metabolic control? Multicenter analysis including 24,500 patients from 191 centers in Germany and Austria. Exp Clin Endocrinol Diabetes. 2006;114:384–388. doi: 10.1055/s-2006-924152. [DOI] [PubMed] [Google Scholar]