Abstract
OBJECTIVES
Locus of control (LOC) is a psychological construct reflecting the degree to which one perceives circumstances to be controlled by personal actions (internal LOC) versus outside factors (external LOC). Because LOC could influence a patient's medical decision-making and health behaviors, our objective is to describe the association between an increasing number of co-existing conditions and LOC in older adults.
DESIGN
Cross-sectional study using survey data from the North Carolina Established Population for Epidemiologic Studies of the Elderly (NC EPESE) dataset.
SETTING and PARTICIPANTS
Community-dwelling older adults aged 68 and older (N=3,212).
MEASUREMENTS
Nine common medical conditions were assessed by self-report. LOC was measured by standard questionnaire. Analyses adjusted for demographics, functional status (self-reported activities of daily living), cognition (Short Portable Mental Status Questionnaire), and depression score (Center for Epidemiologic Studies Depression Scale).
RESULTS
A higher number of chronic conditions was associated with external LOC (β=0.37, p<0.001). This relationship persisted after adjustment for age, race, sex, functional status, cognition, and depression (β=0.17, p <0.0001). Most individual conditions were not associated with LOC, although vision impairment (p<0.001) and arthritis (p<0.05) were associated with more internal LOC.
CONCLUSION
These results suggest that medically complex patients tend to exhibit a more external LOC, meaning that they perceive little personal control over circumstances and environment. Clinicians should be aware of this tendency, as external LOC may impede an older adult's willingness to engage in the considerable task of managing multiple chronic conditions.
Keywords: Multimorbidity, locus of control, medical decision-making, older adults
INTRODUCTION
A large body of literature has demonstrated that patients with multimorbidity (i.e., multiple simultaneous medical conditions) are at high risk of adverse health outcomes such as disability, utilization, and mortality1. Moreover, multimorbidity is associated with staggering healthcare costs and recent literature highlights the need for management strategies that promote more coordinated, patient-centered, and cost-effective care to this growing population of older adults2. Although prevailing models of chronic care emphasize the importance of patient engagement and participation in health decisions and care plans3, little is known about patient factors that may influence perceived level of control over health and well-being. In order to inform the delivery of care that is maximally responsive to the comprehensive needs of medically complicated patients, a more complete understanding is needed of the relationship between multimorbidity and psychosocial traits that may impact a patient's decision-making styles and preferences. .4
One such trait is locus of control (LOC), defined as the extent to which one believes he or she can determine one's own fate or control events5. Individuals with internal LOC tend to perceive that they have substantial influence over their circumstances, whereas individuals with external LOC tend to ascribe their circumstances to the effects of outside factors, not under their personal control. Previous research has shown that patients with more internal LOC are more compliant with medical advice6–8 and more likely to be adherent to physician recommendations9. By contrast, external locus of control has been associated with distress related to decisions about hospital discharge planning10. However, research is mixed. Another study found LOC has no association with compliance in orthodontic treatment, but LOC became more internal after treatment, indicating patients' LOC is malleable11. Another study found that patient LOC was potentially influenced by physician communication style12.
Because older adults with multimorbidity receive many medical recommendations and face many health-related options and choices regarding health practices, understanding the association between multiple conditions and LOC is especially important. Multimorbidity has been associated with more external LOC and an increased risk or susceptibility for general disease13. However, that research utilized a dichotomous definition of multimorbidity (≥ 2 conditions), thus did not fully explore the impact of an increasing number of conditions on LOC. Other research found that internal LOC was associated with a decreased risk for heart problems14,chronic headaches15, and is a protective factor for incident morbidity16 indicating a connection between LOC and risk of specific medical conditions but does not shed light on the relationship between the sheer number of existing medical conditions and LOC.
The current study examines the relationship between multimorbidity burden and LOC using data from a large, diverse cohort of community-dwelling older men and women. It was hypothesized that an increasing number of comorbid medical conditions would be associated with more external LOC, either because individuals with external LOC are less likely to invest in preventive behaviors (diet, exercise, smoking cessation) over a lifetime or because increasing illness diminishes one's sense of control and mastery. Secondary objectives were to explore the relationship between each individual condition and LOC and to determine whether the relationship between multimorbidity burden and LOC differed in men and women.
METHODS
Participants
This study evaluated archival data from the North Carolina Established Population for Epidemiologic Studies of the Elderly (NC EPESE) dataset. The NC EPESE cohort study was designed to investigate the association(s) between medical, demographic, psychosocial, and health behavior with outcomes associated with an aging population and to provide a resource for future evaluation of these variables. Multiple waves of data collection occurred from 1986–1997. The study included a population-based sample of community-dwelling adults 65 years and older at the time of enrollment. Further details on sampling procedures and data collection have been published previously.17 All participants signed informed consent and the study was approved by the Duke University Medical Center Institutional Review Board.
The current analyses are restricted to data collected during the second in-person wave of the study (1989–90). Data from the 1989–90 wave were used because they included several health and comorbid condition variables which are pertinent to this analysis and were not assessed at other waves. Participants were excluded if their information was obtained by proxy or the participant did not have data available from the 1989–90 data collection (n=347).
Medical Conditions
Information on the following nine medical conditions was available: heart attack or myocardial infarction (MI), stroke, diabetes, high blood pressure, obesity, cancer, arthritis, hearing impairment, and vision impairment. Obesity was determined by calculating the body-mass index (BMI) from self-reported height and weight. Obesity was defined as BMI greater or equal to 30. Hearing impairment included those participants who reported that, due to their hearing, they could not usually understand speech without seeing a person. Visual impairment included those participants who reported difficulty recognizing a friend across the street or reading ordinary newspaper print, even with their best corrective lenses. The remaining conditions were assessed by participant's response to the question, “has a physician ever told you that you have [X condition].” Medical condition variables were dichotomized to identify the presence or absence of the specific condition. Morbidity burden was calculated by summing the number of the nine medical condition(s) that were present. The highest number of conditions present for any one participant was six but the sample size for that category was small (n=8); thus, the presence of five or more conditions was combined into one category labeled “5+”.
Physical Function Variables
Three measures of physical ability were available: Activities of Daily Living (ADL), Independent Activities of Daily Living (IADL), and the Rosow-Breslau Mobility Scale.18–20 ADLs included: walking across a small room, bathing, personal grooming, dressing, eating, getting from a bed to a chair, and using the toilet. IADLs included: using the phone, driving, shopping, preparing meals, handling housework, taking medications, and handling money. The Rosow-Breslau scale evaluates the ability to do heavy work around the house, walk up and down stairs, and walk half a mile. Each of these measures was calculated by producing a sum of reported activity limitations in each domain, such that higher values indicate worse functioning. Limitation was defined as difficulty in performing that task or inability to perform the task without the aid of another person.
Psychosocial Variables
Depressive symptoms were measured with the Center for Epidemiologic Studies Depression Scale (CES-D), which uses a 20-item inventory of statements addressing mood (e.g., Are you bothered by things that do not normally bother you?). Cognitive functioning was measured with the 10-item Short Portable Mental Status Questionnaire (SPMSQ). Locus of control (LOC) was measured using an 8-item scale adapted form of the Pearlin et al. (1981)21 measure, evaluating the degree to which participants perceive their life circumstances to be under their own control versus determined by external forces (e.g., I feel I have little control over things.). This measure captures both internal and external LOC on a continuum, with higher values indicating more external LOC and lower values indicating more internal LOC.
All psychosocial variables were transformed such that higher values indicate less desirable psychological states (more depressive symptoms, lower cognitive performance, more external LOC).
Statistical Analysis
Descriptive statistics were used to characterize the cohort at the 1989–90 interview wave. A series of linear regression analyses were performed to evaluate models of increasing complexity, with the number of comorbid medical conditions as the primary independent variable and LOC as the dependent variable. Initial models adjusted for age, gender, race, physical limitations (i.e., ADL, IADL, and mobility disability), cognition, and depression. Next, individual medical conditions were added to the model to determine which (if any) medical conditions contributed to this relationship. Last, the relationship between increasing number of medical conditions and LOC was evaluated for gender effects using a gender-stratified analysis. When the stratified analysis suggested that the association between multimorbidity burden and LOC differed in men and women, the significance of a multiplicative interaction term (number of medical conditions x gender) was evaluated in a final model. In addition to the interaction term, that model included the independent variables of age, race, functional status, cognitive score, depression, gender, and number of medical conditions. All analyses were performed with JMP version 7 (SAS Institute, Cary, NC).
RESULTS
In this sample of older adults (N = 3212), the mean age was 76 years and two in three were female (67.0%). Table 1 provides additional descriptive information about the sample, stratified by their number of medical conditions. Most participants (54.6%) endorsed at least two of the nine chronic health conditions assessed, whereas only 42 (1.3%) participants reported having five or six of the nine conditions.
Table 1.
Descriptive Information for the Total Cohort and According to Multimorbidity Category.
| Age, years | % White | % Female | Educ., years | |
|---|---|---|---|---|
| Total Cohort (N=3212) | 76 | 45% | 67% | 9 |
| Medical Conditions Score* 0 (N=469) | 75 | 54% | 49% | 10 |
| Medical Conditions Score 1 (N=990) | 76 | 51% | 62% | 10 |
| Medical Conditions Score 2 (N=1030) | 76 | 41% | 72% | 9 |
| Medical Conditions Score 3 (N=516) | 77 | 37% | 77% | 8 |
| Medical Conditions Score 4 (N=165) | 77 | 35% | 81% | 7 |
| Medical Conditions Score 5+ (N=42) | 77 | 29% | 71% | 10 |
Medical Condition Score is equal to the number of 9 medical conditions (heart attack or myocardial infarction (MI), stroke, diabetes, high blood pressure, obesity, cancer, arthritis, hearing impairment, and vision impairment) endorsed by a participant.
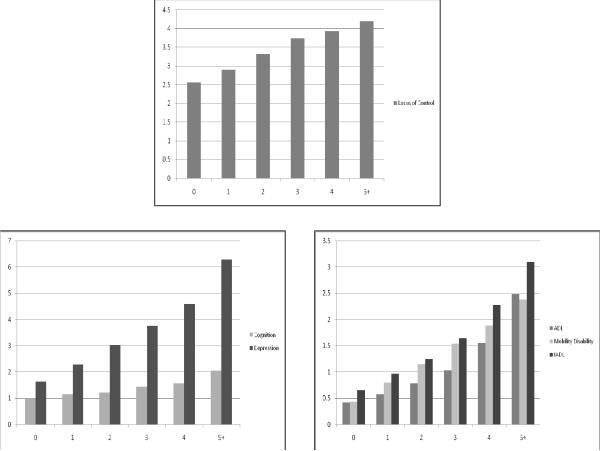
The associations between physical and psychosocial variables in this cohort ranged from small (r=0.08 for LOC and ADL score) to moderate (r=0.69 for ADL and IADL scores). In general, an increase in number of medical conditions was associated with higher (worse) scores on measures of physical ability and the psychosocial variables (Figure 1).
Figure 1.
Average values of the physical and psychosocial parameters as number of comorbid conditions increases. Higher values represent worse function or well-being.
A higher number of chronic conditions was associated with more external LOC (β=0.37, p<0.001; Table 2). This relationship persisted after adjustment for age, race, sex, physical limitations, cognition, and depression (β=0.17, p <0.0001). When individual medical conditions were evaluated for associations with LOC, the only significant associations were between LOC and vision impairment (β=−0.56, p<0.001) and arthritis (β=−0.08, p<0.05), indicating a more internal LOC is associated with these medical conditions. The relationship between increasing number of conditions and external LOC was stronger among females (β=0.19, p<.0001) than males (β=0.12, p=.0290). In these stratified models, age was more strongly associated with external LOC in women, whereas race was more linked to LOC in men. However, in a full model using data from the entire cohort, a multiplicative interaction term (number of chronic conditions x gender) yielded a p value of 0.4753.
Table 2.
The Association Between Morbidity Score and LOC in Successive Regression Models.
| Independent Variables | Model 1 (unadjusted) | Model 2 | Model 3 | Model 4 | Model 5 |
|---|---|---|---|---|---|
| Parameter estimate (p value) | Parameter estimate (p value) | Parameter estimate (p value) | Parameter estimate (p value) | Parameter estimate (p value) | |
| Morbidity Score | 0.37 (<.0001) | 0.36 (<.0001) | 0.29 (<.0001) | 0.28 (<.0001) | 0.17 (<.0001) |
| Age | −0.01 (.2448) | −0.00 (.6206) | 0.00 (.7945) | 0.01 (.0639) | |
| Gender | 0.02 (.5541) | 0.10 (.0130) | 0.10 (.0087) | 0.14 (<.0001) | |
| Race | −0.20 (.1851) | −0.21 (.1626) | −0.26 (.0710) | −0.16 (.2390) | |
| ADL | −0.12 (<.0001) | −0.12 (<.0001) | −0.12 (<.0001) | ||
| IADL | −0.23 (<.0001) | −0.15 (<.0001) | −0.18 (<.0001) | ||
| Mobility Disability | 0.57 (<.0001) | 0.55 (<.0001) | 0.37 (<.0001) | ||
| Cognitive Score | −0.13 (<.0001) | −0.14 (<.0001) | |||
| Depression | 0.25 (<.0001) |
All models include number of comorbid conditions (0 to 5+) as an independent variable with the psychosocial characteristic (LOC) as the dependent variable.
Model 2 - adjusts for age, gender, race
Model 3 - adjusts for age, gender, race, ADL disability, IADL disability, mobility disability
Model 4 - adjusts for age, gender, race, ADL disability, IADL disability, mobility disability, and cognitive score
Model 5 - adjusts for age, gender, race, ADL disability, IADL disability, mobility disability, cognitive score, and depression (CES-D).
Note: LOC = Locus of Control; ADL = Activities of Daily Living; IADL = Independent Activities of Daily Living
DISCUSSION
To the authors' knowledge, this is the first study to evaluate the association between increasing number of chronic conditions and LOC. In this large, community-based sample of older adults, an increasing morbidity burden was associated with a progressively more external LOC, or the perception that circumstances are controlled by external forces. The nine medical conditions included a wide spectrum of body systems (e.g., cardiovascular disease, sensory impairments, arthritis) and most were not significantly associated with LOC on their own. The individual conditions which were independently associated with LOC (vision impairment and arthritis) were associated with internal LOC, not external LOC. This argues against the possibility that the observed relationship between multimorbidity and external LOC was the result of confounding, as does the fact that the relationship persisted after adjusting for demographics, functional and cognitive status, and depression. These results support previous work indicating internal LOC is a protective factor for the development of new disease.16
These findings suggest a potential point of intervention for maximizing psychological well-being and promoting high quality, autonomous decision-making in medically complex older adults. To the extent that LOC is potentially modifiable11,12, efforts aimed at increasing a patient's sense of personal control over his health may facilitate shared decision-making and adaptive health behaviors in patients with multiple medical conditions. For example, diabetes self-management programs for older adults may incorporate educational elements that strongly emphasize personal control by detailing the degree of change expected in disease parameters (such as BMI, Hgb AIC, or LDL) following various behavioral changes that are within the participant's control (diet, exercise, medication adherence). Alternatively, physicians could be prepared to tailor their interventions and delivery styles for varying levels of LOC. Interestingly, cognitive status and LOC were not strongly correlated (R = −.014), although individuals with the most severe cognitive impairment were likely excluded from this sample because their information was collected by proxy. Patients with any degree of cognitive impairment or external LOC may benefit, for different reasons, from the involvement of a supportive friend or family member when making medical decisions or receiving health recommendations. Further, cognitive training interventions improve one's sense of personal control22, suggesting that cognitive status may influence the dynamic nature of LOC.
The causal direction of the associations observed in this cross-sectional analysis cannot be determined. It is plausible that external LOC lends itself to worse health choices over a lifetime such that people with external LOC are more likely to accumulate multiple chronic conditions14,15. However, if external LOC in early adulthood increased the risk of multimorbidity in old age, one would expect some of the individual conditions would also be associated with external LOC in this sample, which was not the case. Alternatively, an increasing morbidity burden and declining health could diminish a patient's sense of personal control over his circumstances, such that a person who once had relatively internal LOC develops a more external LOC as his morbidity count increases. Regardless of the etiology of this relationship, the finding that higher morbidity burden was associated with a more external LOC highlights the importance of attending to the psychological needs of patients with multimorbidity, particularly as providers engage patients in decision-making processes and care plans.
Several limitations may impact the interpretation of the findings. While most important common medical conditions were considered, use of an existing dataset prevented the inclusion of other potentially important conditions, such as pulmonary conditions. Also, available data did not allow for an evaluation of the patient-reported impact of the medical condition(s) on everyday life which might have provided further insight into the relationship between medical comorbidity and patient perceptions. Many conditions were assessed by self-report of physician diagnosis, which is subject to inaccuracy. Finally, as mentioned above, the causal direction of associations cannot be inferred from cross-sectional analysis.
Despite these limitations, the results of this study provide evidence that patients with multimorbidity are more likely to perceive that circumstantial control rests with external forces rather than internally, a view that may negatively influence health behaviors and decision-making. Even in adjusted models, increasing morbidity burden was associated with external LOC, particularly among women. In light of these findings, the high prevalence of multimorbidity in older adults may partially explain earlier reports that older adults tend to prefer others to make medical decisions on their behalf.23–25 Attention to LOC (and potentially other psychological parameters) might ameliorate some or all of this perception, thus improving a complicated patient's capacity to participate meaningfully and comfortably in health decisions. Further, clinicians should recognize that medically complicated patients – even if cognitively intact - are at increased risk of externalizing their medical circumstances, which might interfere with self-directed, internally oriented treatment plans. Such patients, who are frequently presented with many options and self care recommendations, might benefit from evaluation of LOC to help guide the most appropriate approach toward promoting their health.
ACKNOWLEDGMENTS
We would like to thank Bruce Burchett for his assistance with data retrieval.
Debra E. Henninger was supported by NIH Grant T32-AG000029. The work was further supported by NIH Grant K23-AG-032867, a Hartford Foundation Geriatrics Outcomes Research Award, the Durham VA Geriatric Research Education and Clinical Center (GRECC), and NIH Grant P30-AG-028716.
Sponsor's Role: The sponsor had no role in the design, methods, subject recruitment, data collections, analysis or preparation of paper.
Footnotes
Conflict of Interest: The authors declare no conflicts of interest.
Author Contributions: All authors contributed to the study concept and design. Debra E. Henninger performed all analyses, all authors contributed to the interpretation of the results, Debra E. Henninger and Heather E. Whitson drafted the manuscript, and all authors contributed to final manuscript preparation.
REFERENCES
- 1.Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: Iimplications for improved targeting and care. J Gerontology A Boil Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 2.Parekh AK, Barton MB. The challenge of multiple comorbidity for the US health care system. JAMA. 2010;303:1303–1304. doi: 10.1001/jama.2010.381. [DOI] [PubMed] [Google Scholar]
- 3.Wagner EH, Austin BT, Davis C, et al. Improving chronic illness case“ translating evidence into action. Health Aff (Millwood) 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 4.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: A systematic review of the literature. Ageing Res Rev. 2011;10:430–439. doi: 10.1016/j.arr.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Lefcourt H. Locus of control: Current trends in theory and research. 2nd ed. Lawrence Erlbaum; Hillsdale, NJ: 1982. [Google Scholar]
- 6.Ono R, Higashi T, Suzukamo Y, et al. Higher internality of health locus of control is associated with the use of complementary and alternative medicine providers among patients seeking care for acute low-back pain. Clin J Pain. 2008;24:725–730. doi: 10.1097/AJP.0b013e3181759261. [DOI] [PubMed] [Google Scholar]
- 7.Rappaport L, Landman G, Fenton T, et al. Locus of control as predictor of compliance and outcome in treatment of encopresis. J Pediatr. 1986;109:1061–1064. doi: 10.1016/s0022-3476(86)80300-6. [DOI] [PubMed] [Google Scholar]
- 8.Gopinath B, Radhakrishnan K, Sarma PS, et al. A questionnaire survey about doctor-patient communication, compliance and locus of control among south Indian people with epilepsy. Epilepsy Res. 2000;39:73–82. doi: 10.1016/s0920-1211(99)00112-6. [DOI] [PubMed] [Google Scholar]
- 9.Kaya Z, Erkan F, Ozkan M, et al. Self-management plans for asthma control and predictors of patient compliance. J Asthma. 2009;46:270–275. doi: 10.1080/02770900802647565. [DOI] [PubMed] [Google Scholar]
- 10.Coulton CJ, Dunkle RE, Haug M, et al. Locus of control and decision making for posthospital care. Gerontologist. 1989;29:627–632. doi: 10.1093/geront/29.5.627. [DOI] [PubMed] [Google Scholar]
- 11.Lee SJ, Sug-Joon A, Tae-Woo K. Patient compliance and locus of control in orthodontic treatment: A prospective study. Am J Orthodontic Dentofacial Orthop. 2008;133:354–358. doi: 10.1016/j.ajodo.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 12.Schneider A, Komer T, Mehring M, et al. Impact of age, health locus of control and psychological co-morbidity on patients' preferences for shared decision making in general practice. Patient Educ Couns. 2006;61:292–298. doi: 10.1016/j.pec.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 13.van der Linden M, van den Akker M, Buntinx F, et al. The relation between health locus of control and multimorbidity: A case-control study. Personality Individual Differences. 2001;30:1189–1197. [Google Scholar]
- 14.Sturmer T, Hasselbach P, Amelang M. Personality, lifestyle, and risk of cardiovascular disease and cancer: follow-up of population based cohort. BMJ. 2006;332:1359. doi: 10.1136/bmj.38833.479560.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nicholson R. Chronic headache: The role of the psychologist. Curr Pain Headache Rep. 2010;14:47–54. doi: 10.1007/s11916-009-0087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van den Akker M, Buntinx F, Metsemakers JFM, et al. Psychosocial patient characteristics and GP-registered chronic morbidity. J Psychosom Res. 2001;50:95–102. doi: 10.1016/s0022-3999(00)00227-0. [DOI] [PubMed] [Google Scholar]
- 17.Cornoni-Huntley JC, Ostfeld AM, Taylor JO, et al. Established populations for epidemiologic studies of the elderly: Study design and methodology. Aging (Milano) 1993;5:27–37. doi: 10.1007/BF03324123. [DOI] [PubMed] [Google Scholar]
- 18.Fillenbaum GG, Smyer MA. The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. J Gerontol. 1981;36:428–434. doi: 10.1093/geronj/36.4.428. [DOI] [PubMed] [Google Scholar]
- 19.Katz S, Downs T, Cash H. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 20.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 21.Pearlin L, Menaghan EG, Lieberman MA, et al. The stress process. J Health Soc Behav. 1981;22:337–356. [PubMed] [Google Scholar]
- 22.Wolinsky FD, Vander Weg MW, Martin R, et al. Does cognitive training improve internal locus of control among older adults? J Gerontol B Psychol Sci Soc Sci. 2009;65B:591–598. doi: 10.1093/geronb/gbp117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making. Arch Intern Med. 1996;156:1414–1420. [PubMed] [Google Scholar]
- 24.Mather M. A review of decision-making processes: Weighing the risks and benefits of aging. In: Carstensen LL, Hartel CR, editors. When I'm 64. The National Academics Press; Washington D.C.: 2006. [Google Scholar]
- 25.Zwahr MD, Park DC, Shifren K. Judgment about estrogen replacement therapy: The role of age, cognitive abilities, and beliefs. Psychol Aging. 1999;14:179–191. doi: 10.1037//0882-7974.14.2.179. [DOI] [PubMed] [Google Scholar]