Abstract
The somatic mutation theory of aging posits that the accumulation of mutations in the genetic material of somatic cells as a function of time results in a decrease in cellular function. In particular, the accumulation of random mutations inactivates genes that are important for the functioning of the somatic cells of various organ systems of the adult, which results in a decrease in organ function. When the organ function decreases below a critical level, death occurs. A significant amount of research has shown that somatic mutations play an important role in aging and a number of age related pathologies. In this review, we explore evidence for increases in somatic nuclear mutation burden with age and the consequences for aging, cancer, and neurodegeneration. We then review evidence for increases in mitochondrial mutation burden and the consequences for dysfunction in the disease processes.
Introduction
The essence of life is the organization and regulation of genetic information encoded in DNA, fueled by energy harvested from solar and chemical sources, and honed by mutation, selection, sex, and recombination. To maintain the evolutionary innovations of the past, biological organisms invest heavily in a wide variety of DNA repair mechanisms that promote accurate DNA replication during cell division and removal of DNA damage (Friedberg et al., 2006). Evidence, reviewed here, suggests that random mutations nevertheless accumulate in genomes and contribute to diminished fitness with age.
It has been proposed that aging results from a defined program that ensures old individuals are eliminated for the good of the species (Longo et al., 2005). The rationale for this line of thinking comes from theories of group selection and observations from numerous model organisms that multiple conserved genetic pathways modulate lifespan (Kenyon, 2010; Longo et al., 2005; Mitteldorf and Pepper, 2009). Nearly all organisms experience lifespan extension when subjected to caloric restriction or when carrying mutations in the TOR or insulin/IGF1 signaling pathways, which regulate metabolic rate, growth, and nutrient utilization (Kenyon, 2010; Stanfel et al., 2009). However, no combination of mutant alleles and treatments extends life indefinitely, which suggests that the ability of somatic cells to resist entropy is inherently finite (Kirkwood, 2005). The onset of aging phenotypes usually follows a curve rather than a cliff, suggesting a dominant role for stochastic events like somatic DNA damage and mutation in promoting the aging phenotype (Kenyon, 2010). Evolution rewards the investment of energy in somatic maintenance insofar as it promotes the fitness of the germ line. Once an organism reproduces, the selective pressure for somatic maintenance begins to wane.
Germ-line mutations provide essential genetic variation for evolution, yet pose significant risks for the fitness of a species. The germ-line mutation rate is an order of magnitude lower than somatic cell mutation rates, suggesting that multicellular organisms vary the investments in DNA maintenance to maximize both short-term and long-term benefit (Lynch, 2010). Most deleterious germ-line mutations can be vetted in each generation by natural selection. However, evolution lacks the power to select against those deleterious mutations that produce defects with advanced age (Medawar, 1952; Medawar, 1946). Humans carry a substantial number of genetic differences in their germ-line, differing from each other in roughly 15 million of the 6 billion base-pairs of the genome (Pennisi, 2007). Around 12,000 of these single nucleotide polymorphisms affect protein coding sequence (Ng et al., 2008). Although most of these are neutral, 700 to 1500 heterozygous polymorphisms are predicted to be deleterious to protein function (Ng et al., 2008). In addition to these potentially late-acting deleterious alleles, it has been proposed that some genetic traits may exhibit ‘antagonistic pleiotropy’, or phenotypes that improve survival earlier in life, but become deleterious with increasing age (Williams, 1957). Induction of cellular senescence or apoptosis in response to DNA damage may function in this manner by preventing cancer in the young, but contributing to reduced tissue homeostasis in the old (Campisi, 2008).
The above genetic susceptibilities to aging form the background upon which many forms of aging-associated diseases are manifested. During their lifetime, aging cells accumulate DNA mutations and unrepaired lesions, progressively shortened telomeres, defective mitochondria, heterochromatic silencing, misfolded or carbonylated proteins, and oxidized lipids to name a few (Campisi and Vijg, 2009; Kirkwood, 2005). Aging differences between organisms have been hypothesized to reflect variable investments in damage control measures, optimized to exploit different ecological niches (Kirkwood, 2005). There are energetic trade-offs between reproduction and somatic maintenance. Maintaining the correct balance for a given niche is crucial for maximizing competitive fitness. Thus, no single form of damage likely accounts for aging. Moreover, multiple damage control processes may erode concurrently, raising the possibility for synergistic interactions during aging. As such, when the balance between DNA damage and repair is altered, it could enhance the frequency of age-associated diseases. This suggests that the accuracy of DNA synthetic processes is critical for the maintenance of both the nuclear and mitochondrial genomes and is necessary to minimize the deleterious effects of aging. We will explore evidence for increases in somatic nuclear mutation burden with age and the consequences for aging, cancer, and neurodegeneration. We then review evidence for increases in mitochondrial mutation burden and the consequences for dysfunction in the disease processes.
Nuclear Mutation Burden and Aging
An increase in mutations has long been proposed as an aging mechanism (Failla, 1958; Morley, 1998; Szilard, 1959; Vijg, 2000). Evidence from numerous sources indicates that nuclear mutation burden increases with age. Early work demonstrated an aging-dependent increase in mutation frequency in human lymphocytes at loci encoding HLA-A (Grist et al., 1992), hypoxanthine phosphoribosyl transferase (HPRT) (Branda et al., 1993; Curry et al., 1999; Davies et al., 1992; Finette et al., 1994; Jones et al., 1993; Jones et al., 1995; Morley et al., 1982; Robinson et al., 1994; Tates et al., 1991; Trainor et al., 1984), T-cell receptor (Akiyama et al., 1995), and glycophorin A (Akiyama et al., 1995). The magnitude of the increase in mutation frequency at the HPRT locus is similar with respect to age in lymphocytes in human and mice despite a fifty-fold difference in lifespan (Morley, 1998). HPRT mutation frequency increases exponentially in human renal epithelial cells with age, to levels that are higher than T-lymphocytes (Martin et al., 1996), suggesting that mutation accumulation also varies with tissue type. Such mutational mosaicism may be important in explaining tissue specific susceptibility to different age related diseases (Frank, 2010) This may be correlated with DNA damage and replicative index (Colgin et al., 2002). Experiments with transgenic reporter mouse strains confirm variable increases in mutation in different tissues with age (Buettner et al., 1999; Dolle et al., 2000; Hill et al., 2004; Ono et al., 2000). Mutation spectra from these studies reveal a range of mutation types including base-substitutions, frameshifts, insertions, deletions, and rearrangements (Dolle et al., 2000; Hill et al., 2004; Ono et al., 2000). Increases in mutation frequency in the short-lived senescence-accelerated mouse (Odagiri et al., 1998) and decreases in mutation accumulation in the long-lived Ames dwarf mouse (Garcia et al., 2008) further strengthens the correlation between mutations and aging. Correlation, of course, does not prove causation.
Evidence that DNA damage and/or mutations can accelerate aging comes from the observation that patients with rare inherited DNA repair defects exhibit premature aging-like syndromes [reviewed in (Monnat, 2010; Niedernhofer, 2008)]. Werner syndrome patients have mutations that result in loss of the WRN gene product, which contains both RecQ helicase and 3′→5′ exonuclease activities. Patients with these mutations exhibit reduced stature, early onset cataracts, schleroderma, thinning grey hair, artherosclerosis, diabetes mellitus, myocardial infarction and stroke, osteoporosis and increased incidence of certain types of cancer [reviewed in (Monnat, 2010)]. The Werner syndrome protein participates in a variety of DNA transactions including homologous recombination, telomere maintenance and DNA repair. Its absence has been shown to increase the incidence in genomic rearrangements (Fukuchi, 1989). Cockayne syndrome patients have mutations that abolish transcription-coupled nucleotide excision repair (TCR). These patients exhibit a different constellation of symptoms including reduced growth, diverse neuropathologies, sarcopenia, osteopenia, joint contractures, and a premature-aged appearance, although there is no increased incidence of cancer (Niedernhofer, 2008). Unexpectedly, studies of TCR-defective mice indicate that they have reduced insulin/IGF-1 signaling (Niedernhofer et al., 2006; van der Pluijm et al., 2007). Inactivation of this hormonal pathway extends life-span of worms, flies, and certain strains of mice (Kenyon, 2010). Thus, suppression of the growth hormonal axis may be a systemic response to DNA damage, which promotes longevity if activated early in life (Niedernhofer et al., 2006; van der Pluijm et al., 2007).
The relative contributions of DNA damage and somatic mutation accumulation in aging remain unresolved. Unrepaired DNA damage induces cells to undergo apoptosis or senescence, which may diminish tissue homeostasis with age by reducing the number of stem cell lineages (Campisi and Vijg, 2009). Somatic mutation burden continues to increase in the remaining stem cell lineages, which must divide more frequently to maintain the tissue. Although the mutation burden they carry is not lethal, it may influence replicative fitness: ten to twenty percent of diploid yeast strains that are heterozygous for deletion of just one of the 6200 genes are at a growth disadvantage in competition assays (Delneri et al., 2008). Heterozygous mutation burden may also make cells more susceptible to stochastic gene-inactivating events during normal aging. Importantly, the inactivation of a gene by random mutations and genomic rearrangements will not affect only that gene product, but may also affect all genes that are in the same pathway, thus potentially amplifying its effect (Vijg, 2002). Thus, mutations that causes changes in epigenetic silencing, persistent DNA damage, or functional alleles may all work in concert with existing mutation burden to contribute to cell attrition and loss of replicative homeostasis. In the absence of sex and recombination, Muller’s rachet hypothesis predicts that deleterious mutations will accumulate in small populations by genetic drift and reduce fitness (Muller, 1964). Thus, increased mutation burden over time could, in theory, induce some stem cell lineages to lose pluripotentiality, function or even become extinct. Of course, in some rare instances, certain combinations of mutations may increase the fitness and proliferation of stem cell lineages, generating cancer cells that ultimately compromise the fitness of the organism.
Nuclear Mutations in Cancer
The most significant risk factor for cancer is aging; the incidence of adult human cancers increases exponentially with age (Armitage and Doll, 1954). Several competing hypotheses have been proposed to explain this increase, but most theories center on the accumulation of mutations in the nuclear genome. However, the rate and extent of this accumulation is under considerable debate. By plotting the slope of cancer incidence against age, Armitage and coworkers concluded that there are between four and six rate limiting events required for progenitor cells to form tumors (Armitage and Doll, 1954). In some cancers, such as prostatic carcinomas, the age of detection is later and, by the same logic, suggests that 9 to 12 alterations may be required (Renan, 1993).
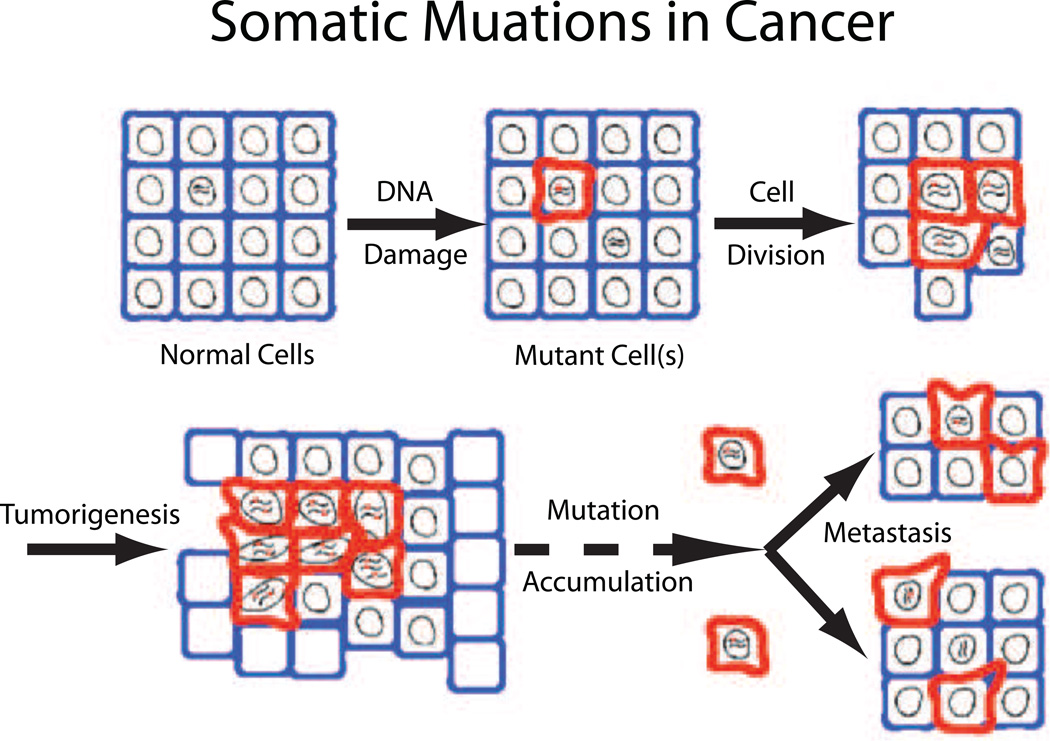
However, given the size of the human genome and the mutation rate attributed to normally dividing cells, it has become clear that a higher mutation frequency is required to obtain the minimum number of mutations that lead to cancer. It was hypothesized many years ago that the thousands of mutations in most human cancers do not result from the low mutation rates exhibited by normal cells. Instead, the mutation rate of non-malignant cells is insufficient to generate a large number of mutations that must be present in human cancers (Loeb et al., 1974). As a result, cancer cells are thought to express a mutator phenotype that rapidly and progressively accumulates large numbers of mutations. Amongst these mutations are driver mutations that enhance cell proliferation (Figure 1). It takes some twenty years for a sufficient number of somatic mutations to endow the cell the ability to divide where it ought not, to invade, to metastasize and kill the host. During that time, somatic evolution continually acts on this burgeoning genetic diversity to select for cells able to bypass many of the defense measures that limit unrestricted cell proliferation, such as availability of nutrition, adequate blood supply, hypoxia, and barriers that prevent invasion into adjacent tissues.
Figure 1. Accumulation of somatic mutations during cancer formation.
During normal organismal aging, cells (blue) are continually exposed to DNA damaging events, that eventually results in cells harboring multiple mutations (red). Some mutations occur in regions of the genome that lead to uncontrolled cell proliferation. The acquisition of a mutator phenotype allows for more rapid somatic evolution that continually acts to select for cells able to bypass many of the defense mechanisms that limit unrestricted cell proliferation.
Several lines of evidence suggest that cancer cells express a mutator phenotype. Some of the first evidence to suggest that cancer cells harbor an increased mutational burden is the observation that the length of microsatellite repeats is highly variable in tumor DNA from patients with hereditary nonpolyposis coli (Fishel et al., 1993; Kolodner and Marsischky, 1999; Perucho, 1996). These results are further supported by the fact that mutations that inactivate DNA mismatch repair genes result in lack of correction of slippage errors by DNA polymerases in copying repetitive DNA sequences throughout the genome (Modrich, 1987). More subtle changes in expression of mismatch repair proteins occur in a variety of other tumors that exhibit microsatellite instability (Gao et al., 1994; Salk et al., 2009). In fact, it can be argued that slippage during the copying of repetitive sequences is the most frequent manifestation of genetic instability.
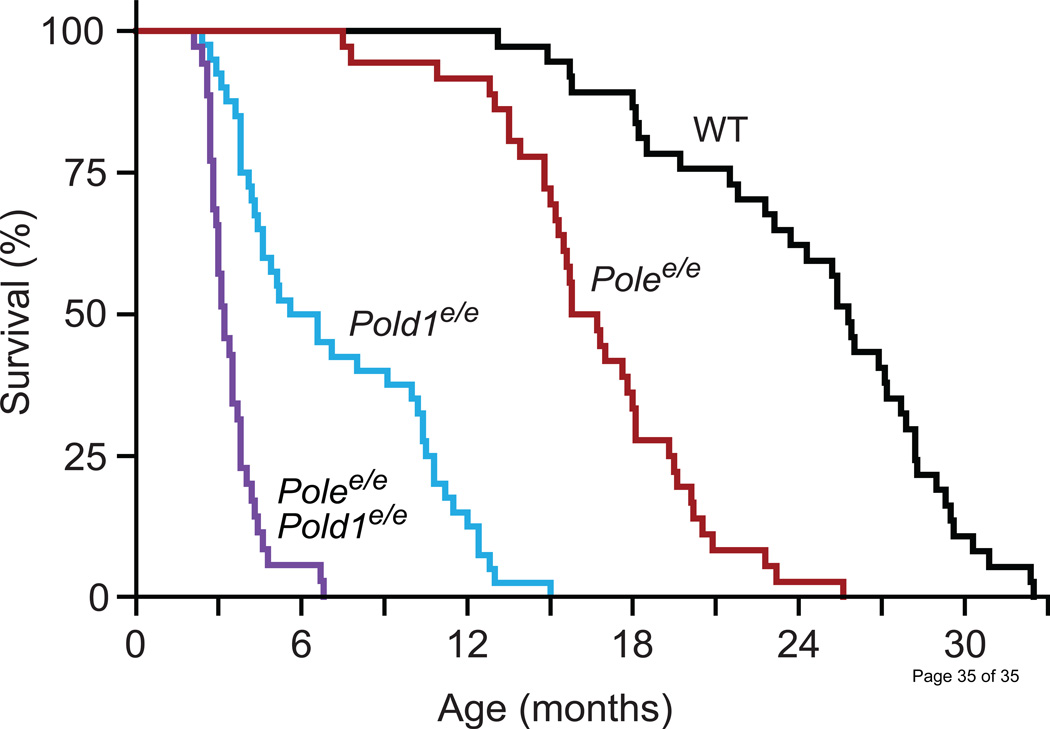
Several mouse models have been created that directly assess the question of random mutagenesis and cancer. The Preston laboratory has created mice in which the endogenous genes encoding the replicative DNA polymerases, Pold1 (Pol δ) and Pole (Pol ε), are replaced by genes harboring mutations that inactivate proofreading by the DNA polymerase (Albertson et al., 2009). The mice with homozygous mutations have strong spontaneous mutator and cancer phenotypes. In addition, mice heterozygous for a mutation encoding a L604K substitution in Pol δ, exhibit an elevated mutation frequency and also exhibit enhanced tumor progression (Venkatesan et al., 2007). By accelerating tumorigenesis, these mutator mouse strains augment one important manifestation of aging: cancer. The mouse strains do not display an obvious acceleration of other aging phenotypes, although the diminished life- and health-span of the strongest mutators due to cancer preclude a proper comparison with WT mice (Figure 2) (Albertson et al., 2009). This idea is further supported by the fact that a number of mouse lines that are deficient in DNA damage repair that show an aging phenotype, some of which also exhibit increased rates of cancer (Hasty et al., 2003)
Figure 2. Heavy mutation load limits the lifespan and health-span of mutator mice.
Due to the dramatically reduced lifespan of these mutator mice, it has not been established whether they age more rapidly than do wild type mice. WT=wild-type; Polee/e=homozygous exonuclease deficient pol ε; Pold1e/e=homozygous exonuclease deficient pol δ. Data are reported in Albertson et. al.
While observations of microsatellite instability and increased cancer in mutator mice are highly supportive of the mutator phenotype, a direct observation of an increased mutation frequency in sporadic tumors would be most supportive. However, until recently, this has been technically challenging. Using the highly sensitive technique of Random Mutation Capture, Bielas et al. were able to quantitate random mutations in nuclear DNA (Bielas et al., 2006). In normal human cells adjacent to a tumor, the frequency of single base substitutions was observed to be approximately 10−8 errors per base-pair. By comparison, the average frequency of random single base substitutions in five adjacent tumors was 2×10−6 mutations per base pair (Bielas et al., 2006). Similar results were reported in studies of both lung adenocarcinomas in mice and humans (Zheng et al., 2007). Additionally, extensive studies on the sequencing of nuclear DNA from human tumors has indicated that there are large numbers of mutations in each tumor analyzed. A compilation of mutations in exons indicates that there are approximately 50–100 mutations in most tumors (Fox and Loeb, 2010). The results of whole genome sequencing indicates that, on average, each tumor contains thousands to hundreds of thousands of mutations (Salk et al., 2010). It is important to emphasize that most current methods for DNA sequencing identify only clonal mutations and do not score for changes in repetitive sequences, sequences with exceptionally high GC content, and teleomeric regions. Thus, by using conventional DNA sequencing techniques, we may only be seeing only the tip of an iceberg
Work with bacteria and yeast indicates that extreme mutation burden can drive cell populations to extinction (Fijalkowska and Schaaper, 1996; Greene and Jinks-Robertson, 2001; Morrison and Sugino, 1993; Tran et al., 1999). In haploid yeast, defects in Pol ε or Pol δ proofreading activity are synthetically lethal with mismatch repair (MMR), while the double mutant diploids grow slowly and have mutation rates consistent with the two fidelity mechanisms acting in series on polymerase errors (Greene and Jinks-Robertson, 2001; Morrison and Sugino, 1993, 1994; Tran et al., 1999). Haploid cells suffering from extremely high mutation rates appear to die from the effects of the mutations themselves and not because of replication stress (Morrison and Sugino, 1993). Following sporulation, double mutant haploids deficient in Pol δ proofreading and MMR undergo several mitotic divisions before arresting at all stages of the cell cycle. The diverse phenotypes suggest that random mutations drive the loss in viability. Diploid genomes are buffered against mutation load (Sliwa et al., 2004); however, recent observations suggest that the protection is limited. Double mutant mouse embryos, deficient in MMR and Pol δ or Pol ε proofreading, fail to fully development in utero, implicating haplo-insufficiency, synthetic genetic interactions, or dominant-lethal mutations in this developmental catastrophe (Albertson et al., 2009). Of great interest is whether the mutation-induced error extinction seen in yeast and bacteria can be harnessed in humans as a target for cancer treatment. For instance, since cancers seem to express a mutator phenotype and exhibit a heavy mutational burden, it may be possible to ‘lethally mutagenize’ these cells by further increasing the mutation load to the point that they are no longer viable (Fox and Loeb, 2010; Prindle et al., 2010).
Nuclear Somatic Mutations in Neurodegeneration
As with cancer, the single greatest risk factor in neurological disease is age. There is increasing evidence that randomly acquired DNA damage and/or mutations in the nuclear genome may play a role in the age-associated loss of a number of post-mitotic tissues. The vast majority of cells in the central nervous system are post-mitotic and produce high levels of DNA-damaging ROS due to high metabolism (Barja, 2004). The brain may be especially sensitive to the accumulation of DNA damage. It is estimated that, on average, the nuclear genome sustains greater than 10,000 sites of damage per day (Lindahl and Nyberg, 1972). The cell employs a variety of DNA repair mechanisms that correct these damage events before they lead to mutations. As a result, most DNA damage and errors due to DNA synthetic processes are sanitized prior to the next round of replication. Studies on DNA repair have mostly been focused on the nuclear genome in proliferating cells. Surprisingly little information exists about DNA repair processes in neurological tissues. DNA repair pathways, such as nucleotide-excision repair and base-excision repair, exhibit a reduction in activity with increasing age (Atamna et al., 2000; Imam et al., 2006; Intano et al., 2003; Krishna et al., 2005).
A number of rare heritable diseases involve the loss of DNA-repair processes. Xeroderma pigmentosum, Cockayne syndrome, and ataxia telangiectasia are the most well studied. These diseases exhibit a progressive neurodegenerative phenotype and profound neurological deficits that, to a certain extent, resembles age-associated neurodegeneration. Both xeroderma pigmentosum and Cockayne syndrome stem from a lack of nucleotide-excision repair, which results in increased steady-state levels of DNA damage and overall genomic instability (Cooper et al., 1997; Leadon and Cooper, 1993). Ataxia telangiectasia results from inactivation of the ATM gene product, which is one of the primary components of the double-stranded DNA break repair pathway and is responsible for the downstream induction of multiple genes involved in DNA repair processes. The absence of this repair pathway leads to a lack of cell-cycle arrest and failure to execute the apoptotic program. It has been hypothesized that the failure of apoptosis leads to an accumulation of functionally impaired cells during brain development, thus leading to the neurodegenerative phenotype (Lee et al., 2001). Further supporting the role of nuclear mutations in neurodegeneration is the observation that brain tissue from ataxia telangiectasia patients exhibits an increased frequency of double-strand DNA breaks (Iourov et al., 2009a).
In addition to an observed increase in the steady-state levels of DNA damage and mutations in a number of neurodegenerative diseases, there have a been a number of reports showing that a significant population of neurons exhibit aneuploidy in both mice and humans (Rehen, et al., 2001; Rehen, et al., 2005). The level of aneuploidy has been reported to be as high as 1–3% in adult brain (Rehen, et al., 2005). What is unclear from these studies is whether these aneuploidy events are part of normal cellular variation within the brain or are they functionally important in the brain. Interestingly, these aneuploid cells are known to be functional with the brain; albeit with an altered gene expression profile (Kaushal et al., 2003; Kingsbury et al., 2005). Should the level of aneuploidy cells within the brain reach a certain level, it is certainly possible that they may play an important role in neurodegenerative processes. Consistent with this idea is the observation that brain tissue from both Alzheimer’s disease and ataxia telangiectasia both exhibit increased levels of aneuploidy, relative to unaffected brain (Iourov et al., 2009b). For a more comprehensive review on the role of nuclear genome mutagenesis and neurodegeneration, see Jeppensen et. al. (Jeppesen et al., 2011).
mtDNA Mutation accumulation in aging
In addition to the nuclear genome, eukaryotic cells also harbor a second genome in their mitochondria. While the size of this genome can vary widely among different organisms, it universally encodes a number of subunits that are essential components of the electron transport chain. Proper functioning of mtDNA, either through faithful replication or expression, is required for the overall health of the organism. Failure to transmit the encoded information to the daughter mitochondrial genomes during mtDNA replication leads to the production of dysfunctional electron transport proteins, a decline in energy production, and a loss of organismal fitness. Thus, it is not surprising that mutations in mtDNA have been associated with a number of pathological conditions.
The accumulation of damage and loss of mitochondrial genome integrity is hypothesized to play a central role in the aging process. One consequence of oxidative phosphorylation in mitochondria is that electrons escape the electron transport chain and form reactive oxygen species (ROS). These free radicals damage a variety of cellular components, including proteins, lipids, and DNA. The proximity of mtDNA to the electron transport chain and its lack of protective histones renders mtDNA especially vulnerable to ROS-mediated damage. Because DNA repair in the mitochondria is not as robust as the nuclear genome, mtDNA is believed to be highly susceptible to mutagenesis. The gradual accumulation of mutations to mtDNA over time results in mutant electron transport proteins encoded in the mtDNA that, in turn, leads to the release of more electrons and increased ROS production. Thus, a ‘vicious cycle’ of ROS damage-induced ROS production may play a critical role in the aging process (Harman, 1956, 1972).
A significant body of work, accumulated over the years, strongly suggests that mtDNA mutations contribute to aging. Several initial studies observed that mtDNA deletion mutations increase in frequency in a variety of aged human tissues (Cao et al., 2001; Corral-Debrinski et al., 1992; Cortopassi and Arnheim, 1990; Kraytsberg et al., 2006; Lee et al., 1994). Importantly, many of these mutations lead to a pathogenic loss of respiratory capacity in the cell (Cao et al., 2001; Hsieh et al., 1994; Kraytsberg et al., 2006; Lezza et al., 1994). Studies with model organisms have found a similar age-dependent accumulation of mtDNA mutations, suggesting that these mutations may be a universal component of aging (Brossas et al., 1994; Schwarze et al., 1995; Vermulst et al., 2008).
Mice engineered to have a proofreading defect in Pol-γ, the DNA polymerase responsible for replicating mtDNA, provided the first strong experimental evidence linking mtDNA mutations and aging (Kujoth et al., 2005; Trifunovic et al., 2004). Mice homozygous for exonuclease deficiency, but not heterozygous littermates, exhibited a premature aging phenotype. Surprisingly, measurements of point mutations carried out on both the heterozygous and homozygous mice indicated that they had similar mutation frequencies – approximately 500-fold times higher than age-matched controls. Because the heterozygous mice were born with a 30-fold higher mutation burden than the oldest wild-type animals without suffering premature aging, it was concluded that the threshold at which mitochondrial point mutations become life-span limiting is unlikely to be reached in wild-type mice (Vermulst et al., 2007). However, deletions in the Pol-γ exo−/− mice were 7- to 11-fold higher than either wild-type or Pol-γ exo+/− heterozygote, suggesting that deletions may drive the premature aging phenotypes of these mice (Vermulst et al., 2008). These conclusions are controversial. Recent studies involving the use of next-generation sequencing techniques to deep-sequence the mtDNA from the pol-γ mutator mouse failed to show an increase in the frequency of deletion mutations (Ameur et al., 2011; Williams et al., 2010). However, cells exhibiting dysfunctional oxidative phosphorylation due to mutated genomes would be vastly outnumbered by ‘healthy’ cells with intact genomes. Therefore, it is unclear if these studies sequenced mtDNA at a sufficient depth to observe random deletions.
Another mouse model, which harbors a human catalase gene targeted to the mitochondria (mCAT), corroborates the role of ROS in aging. The mCAT mouse exhibits increased H2O2 scavenging and a reduction in ROS-based damage to cellular components. These mice experience a ~20% extension of mean and maximal lifespan, while mice over-expressing catalase targeted to peroxisomes or the nucleus had a ≤5% extension of mean lifespan, with no effect on maximal lifespan (Schriner et al., 2005). In addition, these mice show an extended ‘healthspan’, including decreased age-associated insulin-resistance and cardiomyopathy (Dai et al., 2010; Dai et al., 2009; Lee et al., 2010). Importantly, mCAT mice show a 4-fold reduction in the frequency of mtDNA mutations (Vermulst et al., 2008). As with the Pol-γ mutator mouse, lifespan changes observed in the mCAT mouse may be driven by another process besides the accumulation of mtDNA mutations.
mtDNA Mutations in Cancer
Cancer cells have long been known to produce ATP through glycolysis and lactic acid fermentation rather than oxidative phosphorylation (Warburg, 1956). Given that mitochondria are central to a cell’s metabolic processes, it has been hypothesized that mtDNA mutations play a role in carcinogenesis. Indeed, an increase in mtDNA mutations has been observed in a variety of cancer types, including colon cancer, bladder cancer, head and neck cancers, lung cancer, and a number of blood cancers (Copeland et al., 2002; Fliss et al., 2000; Polyak et al., 1998).
Intriguing observations with cellular hybrids or ‘cybrids’, suggest that mutations in mtDNA may play a role in the progression of some cancers. Mitochondria derived from a high metastatic lung carcinoma cell line were introduced into cell lines with low metastatic potential. Remarkably, the low metastatic cell lines acquired robust metastatic potential. Furthermore, when the cell fusions were reversed (i.e mitochondria from low metastatic cells were moved into high metastatic cells), the lung cancer cells lost metastatic potential (Ishikawa et al., 2008). Other, more recent, experiments involving cybrids have shown similar results (Ma et al., 2010).
The role of mtDNA mutations, however, in carcinogenesis is not as clear as it might seem. One of the major counter arguments for the role of mtDNA in carcinogenesis stems from the Pol-γ mutator mouse (Kujoth et al., 2005; Trifunovic et al., 2004). While Pol-γ mutator mice exhibit an aging phenotype and a number of age-associated pathologies, they do not have an increased incidence of cancer. This observation, along with the cybrid experiments, strongly suggests that mtDNA mutations are not the initial drivers of carcinogenesis. Instead, mtDNA mutations may play other roles in carcinogenesis, such as tissue susceptibility to cancer or metastatic potential. In support of this idea is the observation that mCAT mice, which target catalase to the mitochondria, show an altered tumor spectrum, while the overall tumor burden is not significantly reduced (Treuting et al., 2008).
mtDNA Somatic Mutations in Neurodegeneration
Mutations in the mitochondrial genome are associated with a number of clinical syndromes. Because the central nervous system has intense metabolic requirements, reduced energy production can have a severe impact on neural functioning. Patients with elevated levels of mtDNA mutations often show signs of severe neurological impairment, with the degree and pattern of neurodegeneration varying dramatically depending on the type of mutation and mutation load of the mtDNA throughout brain.
Increased ROS and oxidative damage often accompany neurodegenerative diseases and are associated with mutations in mtDNA (Beal, 2005). Mitochondrial dysfunction and increased ROS production in neurodegenerative processes are reported to affect mitochondrial functions like ATP production, membrane potential, permeability transition pore activation, and calcium uptake [reviewed in (Arundine and Tymianski, 2003) and (Cassarino and Jr, 1999)]. These processes, in turn, act as retrograde signals to various cellular compartments that are involved in cell homeostasis, disruption of which can eventually lead to cell death (Liu and Butow, 2006). In addition, as discussed earlier, ROS may trigger accumulation of secondary mtDNA mutations, thereby exacerbating mitochondrial respiratory defects and further increasing the production of ROS, eventually leading to cell death. Reduction in the levels of ROS, either through genetic models or antioxidant mimetics, are known to reduce mtDNA mutations, cellular damage, and extend lifespan (Schriner et al., 2005; Zhao et al., 2004).
There is increasing evidence that mtDNA mutations are involved in the pathogenesis of several neurodegenerative diseases, including Parkinson’s disease and Alzheimer’s disease (Bender et al., 2006; Coskun et al., 2004; Kraytsberg et al., 2006). The evidence for the involvement of mitochondrial dysfunction and mtDNA mutations is perhaps strongest in Parkinson’s disease. Identification of familial forms of the disease show that a number of mutant proteins are associated with mitochondria and are involved in pathways involving oxidative stress, free radical damage, and mitochondrial quality control (Banerjee et al., 2009; Schapira, 2008; Thomas and Beal, 2007). Of particular interest are reports of several families with polymorphisms in the DNA polymerase γ gene that exhibit a progressive Parkinson’s-like phenotype, suggesting that mitochondrial genome instability may lead to some forms of Parkinson’s disease (Betts-Henderson et al., 2009; Galassi et al., 2008; Mancuso et al., 2004). While these cases are familial in nature and may not extend to the idiopathic form of Parkinson’s, it is to be noted that brain samples from patients with idiopathic PD show reduced mitochondrial Complex I activity in conjunction with increased mtDNA mutatations, suggesting the link between the two is quite strong (Bender et al., 2006; Gu et al., 2002; Shoffner et al., 1991).
Similarly to Parkinson’s disease, Alzheimer’s disease also appears to involve mitochondrial dysfunction. Electron microscopy of AD brain samples reveals morphological changes in the mitochondria (Baloyannis, 2006; Hirai et al., 2001). These changes are often accompanied by increased ROS production, reduced ATP levels, and release of mtDNA and cytochrome c oxidase into the cytosol leading to Aβ toxicity (Baloyannis, 2006; Cardoso et al., 2004; Cardoso et al., 2001; Hirai et al., 2001; Pereira et al., 1998). While the connection between the two is not as strong as with Parkinson’s disease, mtDNA mutations are thought to play an important part in the pathogenesis of Alzheimer’s disease. The 4977-bp ‘common deletion’ has been shown to be elevated in Alzheimer’s brain tissue, relative to age-matched controls (Corral-Debrinski et al., 1994). Interestingly, this same mutation is known to increase in frequency as a function of age; the primary risk factor for neurodegenerative diseases (Simonetti et al., 1992). In addition to the ‘common deletion’, mutations in the control region of the mitochondrial genome have been associated with Alzheimer’s disease. Specifically, heteroplasmic levels of the T414G and T477C mutations where found in the brain tissues of Alzheimer’s patients, but not found in the control group (Coskun et al., 2004). Patients with these mutations were also shown to have reduction in the mtDNA L-strand ND6 transcript and in the mtDNA/nuclear DNA ratio, suggesting that these bases may play an important role in genome maintenance and/or expression and could, in part, explain the reduction in copy number and oxidative phosphorylation so often observed in Alzheimer’s disease.
Finally, it has been suggested that somatic mtDNA mutations may play an important role in the pathogenesis of a variety of other neurological disorders. Increased levels of mutations have been suggested to be involved in the pathogenesis of amyotrophic lateral sclerosis (Ro et al., 2003), multiple schlerosis (Campbell et al., 2011), and even neuropsychiatric disorders (Kato et al., 2011; Verge et al., 2011). Such findings strongly suggest that mitochondria are an important component to the overall health of the nervous system.
Conclusions
Life has evolved a number of redundant strategies to maintain a population of somatic cells for the purpose of passing their genetic information to the next generation via the germ-line. However, the slow and relentless accumulation of DNA damage and mutations eventually erodes away the genetic information that maintains homeostasis of the somatic cell population, thus leading to aging and age-associated pathologies such as cancer and neurodegeneration.
While the somatic mutation theory of aging may explain, in part, the mechanisms behind aging and its associated pathologies, it also predicts that a reduction in the rate of accumulation of somatic mutations will slow the aging process. For example, a reduction in the amount of DNA damage from environmental agents could reduce many age-associated diseases. Similarly, drugs could be used to reduce endogenous damage to DNA by reactive oxygen species. Indeed, several recent studies show that mitochondrially targeted anti-oxidant peptides reduce ROS production and are neuroprotective against ROS-producing chemical insults in both a model of Parkinson’s disease and Alzheimer’s disease (Manczak et al., 2010; Yang et al., 2009). In addition, inhibition of mutagenesis by either increase the fidelity of DNA polymerases or the enhancing DNA repair may in the future provide useful mechanisms to reduce the accumulation of somatic mutations during aging.
Highlights.
> In this review we discuss the somatic mutation theory of aging. > We review the evidence for nuclear mutations in ageing, cancer, and neurodegeneration. > We review the case for somatic mutation in mtDNA in these same disease processes.
Acknowledgements
Support for Lawrence Loeb and Scott Kennedy comes from the following NIH/NIA grants: R01 CA115802, R01 CA77852, and P01,AG01751. Scott Kennedy is further supported by the Genetic Approaches to Aging Training Grant (T32 AG000057). Alan Herr has been supported by NIH grants R03 AG037081, P30 AG13280 and a Hitchings-Elion Fellowship from the Burroughs Wellcome Fund.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akiyama M, Kyoizumi S, Hirai Y, Kusunoki Y, Iwamoto KS, Nakamura N. Mutation frequency in human blood cells increases with age. Mutat. Res. 1995;338:141–149. doi: 10.1016/0921-8734(95)00019-3. [DOI] [PubMed] [Google Scholar]
- Albertson TM, Ogawa M, Bugni JM, Hays LE, Chen Y, Wang Y, Treuting PM, Heddle JA, Goldsby RE, Preston BD. DNA polymerase ε and δ proofreading suppress discrete mutator and cancer phenotypes in mice. Proc. Natl. Acad. Sci. USA. 2009;106:17101–17104. doi: 10.1073/pnas.0907147106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameur A, Stewart JB, Freyer C, Hagström E, Ingman M, Larsson N-G, Gyllensten U. Ultra-deep sequencing of mouse mitochondrial DNA: Mutational patterns and their origins. PLOS Genet. 2011;7 doi: 10.1371/journal.pgen.1002028. e1002028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage P, Doll R. The age distribution of cancer and a multi-stage theory of carcinogenesis. Br. J. Cancer. 1954;8:1–12. doi: 10.1038/bjc.1954.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arundine M, Tymianski M. Molecular mechanisms of calcium-dependent neurodegeneration in excitotoxicity. Cell Calcium. 2003;34:325–337. doi: 10.1016/s0143-4160(03)00141-6. [DOI] [PubMed] [Google Scholar]
- Atamna H, Cheung I, Ames BN. A method for detecting abasic sites in living cells: Age-dependent changes in base excision repair. Proc. Nat. Acad. Sci. USA. 2000;97:686–691. doi: 10.1073/pnas.97.2.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baloyannis SJ. Mitochondrial alterations in Alzheimer's disease. J. Alzheimers Dis. 2006;9:119–126. doi: 10.3233/jad-2006-9204. [DOI] [PubMed] [Google Scholar]
- Banerjee R, Starkov AA, Beal MF, Thomas B. Mitochondrial dysfunction in the limelight of Parkinson's disease pathogenesis. BBA-Mol. Basis. Dis. 2009;1792:651–663. doi: 10.1016/j.bbadis.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barja G. Free radicals and aging. Trends Neurosci. 2004;27:595–600. doi: 10.1016/j.tins.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Beal MF. Mitochondria take center stage in aging and neurodegeneration. Ann. Neurol. 2005;58:495–505. doi: 10.1002/ana.20624. [DOI] [PubMed] [Google Scholar]
- Bender A, Krishnan KJ, Morris CM, Taylor GA, Reeve AK, Perry RH, Jaros E, Hersheson JS, Betts J, Klopstock T, Taylor RW, Turnbull DM. High levels of mitochondrial DNA deletions in substantia nigra neurons in aging and Parkinson disease. Nat. Genetics. 2006;38:515–517. doi: 10.1038/ng1769. [DOI] [PubMed] [Google Scholar]
- Betts-Henderson J, Jaros E, Krishnan K, Perry R, Reeve A, Schaefer A, Taylor R, Turnbull D. Alpha-synuclein pathology and Parkinsonism associated with POLG1 mutations and multiple mitochondrial DNA deletions. Neuropath. Appl. Neuro. 2009;35:120–124. doi: 10.1111/j.1365-2990.2008.00981.x. [DOI] [PubMed] [Google Scholar]
- Bielas JH, Loeb KR, Rubin BP, True LD, Loeb LA. Human cancers express a mutator phenotype. Proc. Natl. Acad. Sci. USA. 2006;103:18238–18242. doi: 10.1073/pnas.0607057103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branda RF, Sullivan LM, O'Neill JP, Falta MT, Nicklas JA, Hirsch B, Vacek PM, Albertini RJ. Measurement of HPRT mutant frequencies in T-lymphocytes from healthy human populations. Mutat. Res. 1993;285:267–279. doi: 10.1016/0027-5107(93)90115-v. [DOI] [PubMed] [Google Scholar]
- Brossas J-Y, Barreau E, Courtois Y, Tréton J. Multiple deletions in mitochondrial DNA are present in senescent mouse brain. Biochem. Bioph. Res. Co. 1994;202:654–659. doi: 10.1006/bbrc.1994.1980. [DOI] [PubMed] [Google Scholar]
- Buettner VL, Hill KA, Halangoda A, Sommer SS. Tandem-base mutations occur in mouse liver and adipose tissue preferentially as G:C to T:A transversions and accumulate with age. Environ. Mol. Mutagen. 1999;33:320–324. doi: 10.1002/(sici)1098-2280(1999)33:4<320::aid-em9>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Campbell GR, Ziabreva I, Reeve AK, Krishnan KJ, Reynolds R, Howell O, Hans Lassmann, Turnbull DM, Mahad DJ. Mitochondrial DNA deletions and neurodegeneration in multiple sclerosis. Ann. Neurol. 2011;69:481–492. doi: 10.1002/ana.22109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campisi J. Aging and cancer cell biology, 2008. Aging Cell. 2008;7:281–284. doi: 10.1111/j.1474-9726.2008.00383.x. [DOI] [PubMed] [Google Scholar]
- Campisi J, Vijg J. Does damage to DNA and other macromolecules play a role in aging? If so, how? J. Gerontol. A. Biol. Sci. Med. Sci. 2009;64A:175–178. doi: 10.1093/gerona/gln065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Z, Wanagat J, McKiernan SH, Aiken JM. Mitochondrial DNA deletion mutations are concomitant with ragged red regions of individual, aged muscle fibers: Analysis by laser-capture microdissection. Nuc. Acid. Res. 2001;29:4502–4508. doi: 10.1093/nar/29.21.4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardoso SM, Proença MT, Santos S, Santana I, Oliveira CR. Cytochrome c oxidase is decreased in Alzheimer's disease platelets. Neurobiol. Aging. 2004;25:105–110. doi: 10.1016/s0197-4580(03)00033-2. [DOI] [PubMed] [Google Scholar]
- Cardoso SM, Santos S, Swerdlow RH, Oliveira CR. Functional mitochondria are required for amyloid β-mediated neurotoxicity. FASEB J. 2001;15:1439–1441. doi: 10.1096/fj.00-0561fje. [DOI] [PubMed] [Google Scholar]
- Cassarino DS, Jr, JPB An evaluation of the role of mitochondria in neurodegenerative diseases: mitochondrial mutations and oxidative pathology, protective nuclear responses, and cell death in neurodegeneration. Brain Res. Rev. 1999;29:1–25. doi: 10.1016/s0165-0173(98)00046-0. [DOI] [PubMed] [Google Scholar]
- Colgin LM, Hackmann AFM, Emond MJ, Monnat RJ. The unexpected landscape of in vivo somatic mutation in a human epithelial cell lineage. Proc. Nat. Acad. Sci. USA. 2002;99:1437–1442. doi: 10.1073/pnas.032655699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper PK, Nouspikel T, Clarkson SG, Leadon SA. Defective transcription-coupled repair of oxidative base damage in Cockayne syndrome patients from XP group G. Science. 1997;275:990–993. doi: 10.1126/science.275.5302.990. [DOI] [PubMed] [Google Scholar]
- Copeland WC, Wachsman JT, Johnson F, Penta JS. Mitochondrial DNA alterations in cancer. Cancer Invest. 2002;20:557–569. doi: 10.1081/cnv-120002155. [DOI] [PubMed] [Google Scholar]
- Corral-Debrinski M, Horton T, Lott MT, Shoffner JM, Beal MF, Wallace DC. Mitochondrial DNA deletions in human brain: Regional variability and increase with advanced age. Nat Genetics. 1992;2:324–329. doi: 10.1038/ng1292-324. [DOI] [PubMed] [Google Scholar]
- Corral-Debrinski M, Horton T, Lott MT, Shoffner JM, McKee AC, Beal MF, Graham BH, Wallace DC. Marked changes in mitochondrial DNA deletion levels in Alzheimer brains. Genomics. 1994;23:471–476. doi: 10.1006/geno.1994.1525. [DOI] [PubMed] [Google Scholar]
- Cortopassi G, Arnheim N. Detection of a specific mitochondrial DNA deletion in tissues of older humans. Nuc. Acid. Res. 1990;18:6927–6933. doi: 10.1093/nar/18.23.6927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coskun PE, Beal MF, Wallace DC. Alzheimer's brains harbor somatic mtDNA control-region mutations that suppress mitochondrial transcription and replication. Proc. Nat. Acad. Sci. USA. 2004;101:10726–10731. doi: 10.1073/pnas.0403649101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry J, Karnaoukhova L, Guenette GC, Glickman BW. Influence of sex, smoking and age on human hprt mutation frequencies and spectra. Genetics. 1999;152:1065–1077. doi: 10.1093/genetics/152.3.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai D-F, Chen T, Wanagat J, Laflamme M, Marcinek DJ, Emond MJ, Ngo CP, Prolla TA, Rabinovitch PS. Age-dependent cardiomyopathy in mitochondrial mutator mice is attenuated by overexpression of catalase targeted to mitochondria. Aging Cell. 2010;9:536–544. doi: 10.1111/j.1474-9726.2010.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai D-F, Santana LF, Vermulst M, Tomazela DM, Emond MJ, MacCoss MJ, Gollahon K, Martin GM, Loeb LA, Ladiges WC, Rabinovitch PS. Overexpression of catalase targeted to mitochondria attenuates murine cardiac aging. Circulation. 2009;119:2789–2797. doi: 10.1161/CIRCULATIONAHA.108.822403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies MJ, Lovell DP, Anderson D. Thioguanine-resistant mutant frequency in T-lymphocytes from a healthy human population. Mutat. Res. 1992;265:165–171. doi: 10.1016/0027-5107(92)90045-4. [DOI] [PubMed] [Google Scholar]
- Delneri D, Hoyle DC, Gkargkas K, Cross EJM, Rash B, Zeef L, Leong H-S, Davey HM, Hayes A, Kell DB, Griffith GW, Oliver SG. Identification and characterization of high-flux-control genes of yeast through competition analyses in continuous cultures. Nat. Genet. 2008;40:113–117. doi: 10.1038/ng.2007.49. [DOI] [PubMed] [Google Scholar]
- Dollé ME, Snyder WK, Gossen JA, Lohman PH, Vijg J. Distinct spectra of somatic mutations accumulated with age in mouse heart and small intestine. Proc. Natl. Acad. Sci. U S A. 2000;97:8403–8408. doi: 10.1073/pnas.97.15.8403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Failla G. The aging process and cancerogenesis. Ann NY Acad Sci. 1958:1124–1140. doi: 10.1111/j.1749-6632.1958.tb46828.x. [DOI] [PubMed] [Google Scholar]
- Fijalkowska IJ, Schaaper RM. Mutants in the exo I motif of Escherichia coli dnaQ: Defective proofreading and inviability due to error catastrophe. Proc. Natl. Acad. Sci. U S A. 1996;93:2856–2861. doi: 10.1073/pnas.93.7.2856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finette BA, Sullivan LM, O'Neill JP, Nicklas JA, Vacek PM, Albertini RJ. Determination of hprt mutant frequencies in T-lymphocytes from a healthy pediatric population: statistical comparison between newborn, children and adult mutant frequencies, cloning efficiency and age. Mutat. Res. 1994;308:223–231. doi: 10.1016/0027-5107(94)90157-0. [DOI] [PubMed] [Google Scholar]
- Fishel R, Lescoe MK, Rao MRS, Copeland NG, Jenkins NA, Garber J, Kane M, Kolodner R. The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell. 1993;75:1027–1038. doi: 10.1016/0092-8674(93)90546-3. [DOI] [PubMed] [Google Scholar]
- Fliss MS, Usadel H, Caballero OvL, Wu L, Buta MR, Eleff SM, Jen J, Sidransky D. Facile detection of mitochondrial DNA mutations in tumors and bodily fluids. Science. 2000;287:2017–2019. doi: 10.1126/science.287.5460.2017. [DOI] [PubMed] [Google Scholar]
- Fox EJ, Loeb LA. Lethal mutagenesis: targeting the mutator phenotype in cancer. Semin. Cancer Biol. 2010;20:353–359. doi: 10.1016/j.semcancer.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank SA. Somatic evolutionary genomics: Mutations during development cause highly variable genetic mosaicism with risk of cancer and neurodegeneration. Proc. Natl. Acad. Sci. U S A. 2010;107:1725–1730. doi: 10.1073/pnas.0909343106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedberg EC, Walker GC, Siede W, Wood RD, Schultz RA, Ellenberger T. DNA Repair and Mutagenesis. 2nd ed. Washington, DC: ASM Press; 2006. [Google Scholar]
- Fukuchi F, Martin GM, Monnat RJ. Mutator phenotype of Werner syndrome is characterized by extensive deletions. Proc. Natl. Acad. Sci. U S A. 1989;86:5893–5897. doi: 10.1073/pnas.86.15.5893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galassi G, Lamantea E, Invernizzi F, Tavani F, Pisano I, Ferrero I, Palmieri L, Zeviani M. Additive effects of POLG1 and ANT1 mutations in a complex encephalomyopathy. Neuromuscular Disord. 2008;18:465–470. doi: 10.1016/j.nmd.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Gao X, Wu N, Grignon D, Zacharek A, Liu H, Salkowski A, Li G, Sakr W, Sarkar F, Porter AT, Chen YQ, Honn KV. High frequency of mutator phenotype in human prostatic adenocarcinoma. Oncogene. 1994;9:2999–3003. [PubMed] [Google Scholar]
- Garcia AM, Busuttil RA, Calder RB, Dolle ME, Diaz V, McMahan CA, Bartke A, Nelson J, Reddick R, Vijg J. Effect of Ames dwarfism and caloric restriction on spontaneous DNA mutation frequency in different mouse tissues. Mech. Ageing Dev. 2008;129:528–533. doi: 10.1016/j.mad.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene CN, Jinks-Robertson S. Spontaneous frameshift mutations in Saccharomyces cerevisiae: Accumulation during DNA replication and removal by proofreading and mismatch repair activities. Genetics. 2001;159:65–75. doi: 10.1093/genetics/159.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grist SA, McCarron M, Kutlaca A, Turner DR, Morley AA. In vivo human somatic mutation: Frequency and spectrum with age. Mutat. Res. 1992;266:189–196. doi: 10.1016/0027-5107(92)90186-6. [DOI] [PubMed] [Google Scholar]
- Gu G, Reyes PF, Golden GT, Woltjer RL, Hulette C, Montine TJ, Zhang J. Mitochondrial DNA deletions/rearrangements in parkinson disease and related neurodegenerative disorders. J. Neuropath. Exp. Neurol. 2002;61:634–639. doi: 10.1093/jnen/61.7.634. [DOI] [PubMed] [Google Scholar]
- Harman D. Aging: A Theory Based on Free Radical and Radiation Chemistry. J. Gerontol. 1956;11:298–300. doi: 10.1093/geronj/11.3.298. [DOI] [PubMed] [Google Scholar]
- Harman D. The biologic clock: the mitochondria? J Am Geriatr Soc. 1972:145–147. doi: 10.1111/j.1532-5415.1972.tb00787.x. [DOI] [PubMed] [Google Scholar]
- Hasty P, Campisi J, Hoeijmakers J, van Steeg H, Vijg J. Aging and genome maintenance: Lessons from the mouse? Science. 2003:1355–1359. doi: 10.1126/science.1079161. [DOI] [PubMed] [Google Scholar]
- Hill KA, Buettner VL, Halangoda A, Kunishige M, Moore SR, Longmate J, Scaringe WA, Sommer SS. Spontaneous mutation in Big Blue® mice from fetus to old age: Tissue-specific time courses of mutation frequency but similar mutation types. Environ. Mol. Mutagen. 2004;43:110–120. doi: 10.1002/em.20004. [DOI] [PubMed] [Google Scholar]
- Hirai K, Aliev G, Nunomura A, Fujioka H, Russell RL, Atwood CS, Johnson AB, Kress Y, Vinters HV, Tabaton M, Shimohama S, Cash AD, Siedlak SL, Harris PL, Jones PK, Petersen RB, Perry G, Smith MA. Mitochondrial abnormalities in Alzheimer's disease. J. Neurosci. 2001;21:3017–3923. doi: 10.1523/JNEUROSCI.21-09-03017.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh R, Hou J, Hsu H, Wei W. Age-dependent respiratory function decline and DNA deletions in human muscle mitochondria. Biochem. Mol. Biol. Int. 1994;32:1009–1022. [PubMed] [Google Scholar]
- Imam SZ, Karahalil B, Hogue BA, Souza-Pinto NC, Bohr VA. Mitochondrial and nuclear DNA-repair capacity of various brain regions in mouse is altered in an age-dependent manner. Neurobiol. Aging. 2006;27:1129–1136. doi: 10.1016/j.neurobiolaging.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Intano GW, Cho EJ, McMahan CA, Walter CA. Age-related base excision repair activity in mouse brain and liver nuclear extracts. J. Gerontol. 2003;58:205–211. doi: 10.1093/gerona/58.3.b205. [DOI] [PubMed] [Google Scholar]
- Iourov IY, Vorsanova SG, Liehr T, Kolotii AD, Yurov YB. Increased chromosome instability dramatically disrupts neural genome integrity and mediates cerebellar degeneration in the ataxia-telangiectasia brain. Hum. Mol. Genet. 2009a;18:2656–2669. doi: 10.1093/hmg/ddp207. [DOI] [PubMed] [Google Scholar]
- Iourov IY, Vorsanova SG, Liehr T, Yurov YB. Aneuploidy in the normal, Alzheimer's disease and ataxia-telangiectasia brain: Differential expression and pathological meaning. Neurobiol. Dis. 2009b;34:212–220. doi: 10.1016/j.nbd.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Ishikawa K, Takenaga K, Akimoto M, Koshikawa N, Yamaguchi A, Imanishi H, Nakada K, Honma Y, Hayashi J-I. ROS-generating mitochondrial DNA mutations can regulate tumor cell metastasis. Science. 2008;320:661–664. doi: 10.1126/science.1156906. [DOI] [PubMed] [Google Scholar]
- Jeppesen DK, Bohr VA, Stevnsner T. DNA repair deficiency in neurodegeneration. Prog Neurobiol. 2011;94:166–200. doi: 10.1016/j.pneurobio.2011.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones IM, Moore DH, Thomas CB, Thompson CL, Strout CL, Burkhart-Schultz K. Factors affecting HPRT mutant frequency in T-lymphocytes of smokers and nonsmokers. Cancer. Epidem. Biomar. 1993;2:249–260. [PubMed] [Google Scholar]
- Jones IM, Thomas CB, Tucker B, Thompson CL, Pleshanov P, Vorobtsova I, Moore DH., 2nd Impact of age and environment on somatic mutation at the hprt gene of T lymphocytes in humans. Mutat. Res. 1995;338:129–139. doi: 10.1016/0921-8734(95)00018-2. [DOI] [PubMed] [Google Scholar]
- Kato M, Nakamura M, Ichiba M, Tomiyasu A, Shimo H, Higuchi I, Ueno S-i, Sano A. Mitochondrial DNA deletion mutations in patients with neuropsychiatric symptoms. Neurosci. Res. 2011;69:331–336. doi: 10.1016/j.neures.2010.12.013. [DOI] [PubMed] [Google Scholar]
- Kaushal D, Contos JJ, Treuner K, Yang AH, Kingsbury MA, Rehen SK, McConnell MJ, Okabe M, Barlow C, Chun J. Alteration of gene expression by chromosome loss in the postnatal mouse brain. J. Neurosci. 2003;23:5599–5606. doi: 10.1523/JNEUROSCI.23-13-05599.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenyon CJ. The genetics of ageing. Nature. 2010;464:504–512. doi: 10.1038/nature08980. [DOI] [PubMed] [Google Scholar]
- Kingsbury MA, Friedman B, McConnell MJ, Rehen SK, Yang AH, Kaushal D, Chun J. Aneuploid neurons are functionally active and integrated into brain circuitry. Proc. Natl. Acad. Sci. U.S.A. 2005;102:6143–6147. doi: 10.1073/pnas.0408171102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkwood TBL. Understanding the odd science of aging. Cell. 2005;120:437–447. doi: 10.1016/j.cell.2005.01.027. [DOI] [PubMed] [Google Scholar]
- Kolodner RD, Marsischky GT. Eukaryotic DNA mismatch repair. Curr. Opin. Genet. Dev. 1999;9:89–96. doi: 10.1016/s0959-437x(99)80013-6. [DOI] [PubMed] [Google Scholar]
- Kraytsberg Y, Kudryavtseva E, McKee AC, Geula C, Kowall NW, Khrapko K. Mitochondrial DNA deletions are abundant and cause functional impairment in aged human substantia nigra neurons. Nat. Genetics. 2006;38:518–520. doi: 10.1038/ng1778. [DOI] [PubMed] [Google Scholar]
- Krishna TH, Mahipal S, Sudhakar A, Sugimoto H, Kalluri R, Rao KS. Reduced DNA gap repair in aging rat neuronal extracts and its restoration by DNA polymerase β and DNA-ligase. J. Neurochem. 2005;92:818–823. doi: 10.1111/j.1471-4159.2004.02923.x. [DOI] [PubMed] [Google Scholar]
- Kujoth GC, Hiona A, Pugh TD, Someya S, Panzer K, Wohlgemuth SE, Hofer T, Seo AY, Sullivan R, Jobling WA, Morrow JD, Remmen HV, Sedivy JM, Yamasoba T, Tanokura M, Weindruch R, Leeuwenburgh C, Prolla TA. Mitochondrial DNA mutations, oxidative stress, and apoptosis in mammalian aging. Science. 2005;309:481–484. doi: 10.1126/science.1112125. [DOI] [PubMed] [Google Scholar]
- Leadon SA, Cooper PK. Preferential repair of ionizing radiation-induced damage in the transcribed strand of an active human gene is defective in Cockayne syndrome. Proc. Nat. Acad. Sci. USA. 1993;90:10499–10503. doi: 10.1073/pnas.90.22.10499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H-C, Pang C-Y, Hsu H-S, Wei Y-H. Differential accumulations of 4,977 bp deletion in mitochondrial DNA of various tissues in human ageing. BBA-Mol. Basis Dis. 1994;1226:37–43. doi: 10.1016/0925-4439(94)90056-6. [DOI] [PubMed] [Google Scholar]
- Lee H-Y, Choi CS, Birkenfeld AL, Alves TC, Jornayvaz FR, Jurczak MJ, Zhang D, Woo DK, Shadel GS, Ladiges W, Rabinovitch PS, Santos JH, Petersen KF, Samuel VT, Shulman GI. Targeted expression of catalase to mitochondria prevents age-associated reductions in mitochondrial function and insulin resistance. Cell Metab. 2010;12:668–674. doi: 10.1016/j.cmet.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Chong M, McKinnon P. Ataxia telangiectasia mutated-dependent apoptosis after genotoxic stress in the developing nervous system is determined by cellular differentiation status. J. Neurosci. 2001;21:6687–6693. doi: 10.1523/JNEUROSCI.21-17-06687.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezza A, Boffoli D, Cantatore P, Gadaleta M. Correlation between mitochondrial DNA 4977-bp deletion and respiratory chain enzyme activities in aging human skeletal muscles. Biochem. Bioph. Res. Co. 1994;205:772–779. doi: 10.1006/bbrc.1994.2732. [DOI] [PubMed] [Google Scholar]
- Lindahl T, Nyberg B. Rate of depurination of native deoxyribonucleic acid. Biochemistry. 1972;11:3610–3618. doi: 10.1021/bi00769a018. [DOI] [PubMed] [Google Scholar]
- Liu Z, Butow RA. Mitochondrial retrograde signaling. Annu. Rev. Genet. 2006;40:159–185. doi: 10.1146/annurev.genet.40.110405.090613. [DOI] [PubMed] [Google Scholar]
- Loeb LA, Springgate CF, Battula N. Errors in DNA replication as a basis of malignant change. Cancer Res. 1974;34:2311–2321. [PubMed] [Google Scholar]
- Longo VD, Mitteldorf J, Skulachev VP. Programmed and altruistic ageing. Nat. Rev. Genet. 2005;6:866–872. doi: 10.1038/nrg1706. [DOI] [PubMed] [Google Scholar]
- Lynch M. Evolution of the mutation rate. Trends Genet. 2010;26:345–352. doi: 10.1016/j.tig.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y, Bai R-K, Trieu R, Wong L-JC. Mitochondrial dysfunction in human breast cancer cells and their transmitochondrial cybrids. BBA-Bioenergetics. 2010;1797:29–37. doi: 10.1016/j.bbabio.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancuso M, Filosto M, Oh SJ, DiMauro S. A novel polymerase γ mutation in a family with ophthalmoplegia, neuropathy, and parkinsonism. Arch Neurol. 2004;61:1777–1779. doi: 10.1001/archneur.61.11.1777. [DOI] [PubMed] [Google Scholar]
- Manczak M, Mao P, Calkins MJ, Cornea A, Reddy AP, Murphy MP, Szeto HH, Park B, Reddy PH. Mitochondria-Targeted Antioxidants Protect Against Amyloid-β Toxicity in Alzheimer’s Disease Neurons. J. Alzheimers Dis. 2010;20:S609–S631. doi: 10.3233/JAD-2010-100564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin GM, Ogburn CE, Colgin LM, Gown AM, Edland SD, Monnat RJ. Somatic mutations are frequent and increase with age in human kidney epithelial cells. Hum. Mol. Genet. 1996;5:215–221. doi: 10.1093/hmg/5.2.215. [DOI] [PubMed] [Google Scholar]
- Medawar P. An unsolved problem in biology. London: Lewis; 1952. [Google Scholar]
- Medawar PB. Old age and natural death. Modern Quart. 1946;2:30–56. [Google Scholar]
- Mitteldorf J, Pepper J. Senescence as an adaptation to limit the spread of disease. J. Theor. Biol. 2009;260:186–195. doi: 10.1016/j.jtbi.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Modrich P. DNA mismatch correction. Annu. Rev. Biochem. 1987;56:435–466. doi: 10.1146/annurev.bi.56.070187.002251. [DOI] [PubMed] [Google Scholar]
- Monnat RJ. Human RECQ helicases: Roles in DNA metabolism, mutagenesis and cancer biology. Semin. Cancer Biol. 2010;20:329–339. doi: 10.1016/j.semcancer.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley A. Somatic mutation and aging. Ann. NY Acad. Sci. 1998;854:20–22. doi: 10.1111/j.1749-6632.1998.tb09888.x. [DOI] [PubMed] [Google Scholar]
- Morley AA, Cox S, Holliday R. Human lymphocytes resistant to 6-thioguanine increase with age. Mech. Ageing Dev. 1982;19:21–26. doi: 10.1016/0047-6374(82)90046-x. [DOI] [PubMed] [Google Scholar]
- Morrison A, Sugino A. DNA polymerase II, the epsilon polymerase of Saccharomyces cerevisiae. Prog Nucleic Acid Res Mol Biol. 1993;46:93–120. doi: 10.1016/s0079-6603(08)61019-3. [DOI] [PubMed] [Google Scholar]
- Morrison A, Sugino A. The 3'→5' exonucleases of both DNA polymerases δ and ε participate in correcting errors of DNA replication in Saccharomyces cerevisiae. Mol. Gen. Genet. 1994;242:289–296. doi: 10.1007/BF00280418. [DOI] [PubMed] [Google Scholar]
- Muller HJ. The relation of recombination to mutational advance. Mutat. Res. 1964;106:2–9. doi: 10.1016/0027-5107(64)90047-8. [DOI] [PubMed] [Google Scholar]
- Ng PC, Levy S, Huang J, Stockwell TB, Walenz BP, Li K, Axelrod N, Busam DA, Strausberg RL, Venter JC. Genetic variation in an individual human exome. PLoS Genet. 2008;4 doi: 10.1371/journal.pgen.1000160. e1000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedernhofer LJ. Tissue-specific accelerated aging in nucleotide excision repair deficiency. Mech. Ageing Dev. 2008;129:408–415. doi: 10.1016/j.mad.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niedernhofer LJ, Garinis GA, Raams A, Lalai AS, Robinson AR, Appeldoorn E, Odijk H, Oostendorp R, Ahmad A, van Leeuwen W, Theil AF, Vermeulen W, van der Horst GT, Meinecke P, Kleijer WJ, Vijg J, Jaspers NG, Hoeijmakers JH. A new progeroid syndrome reveals that genotoxic stress suppresses the somatotroph axis. Nature. 2006;444:1038–1043. doi: 10.1038/nature05456. [DOI] [PubMed] [Google Scholar]
- Odagiri Y, Uchida H, Hosokawa M, Takemoto K, Morley AA, Takeda T. Accelerated accumulation of somatic mutations in the senescence-accelerated mouse. Nat. Genet. 1998;19:116–117. doi: 10.1038/468. [DOI] [PubMed] [Google Scholar]
- Ono T, Ikehata H, Nakamura S, Saito Y, Hosoi Y, Takai Y, Yamada S, Onodera J, Yamamoto K. Age-associated increase of spontaneous mutant frequency and molecular nature of mutation in newborn and old lacZ-transgenic mouse. Mutat. Res. 2000;447:165–177. doi: 10.1016/s0027-5107(99)00200-6. [DOI] [PubMed] [Google Scholar]
- Pennisi E. BREAKTHROUGH OF THE YEAR: Human Genetic Variation. Science. 2007;318:1842–1843. doi: 10.1126/science.318.5858.1842. [DOI] [PubMed] [Google Scholar]
- Pereira C, Santos MS, Oliveira C. Mitochondrial function impairment induced by amyloid β-peptide on PC12 cells. NeuroReport. 1998;9:1749–1755. doi: 10.1097/00001756-199806010-00015. [DOI] [PubMed] [Google Scholar]
- Perucho M. Cancer of the microsatellite mutator phenotype. Biol. Chem. 1996;377:675–684. [PubMed] [Google Scholar]
- Polyak K, Li Y, Zhu H, Lengauer C, Willson JK, Markowitz SD, Trush MA, Kinzler KW, Vogelstein B. Somatic mutations of the mitochondrial genome in human colorectal tumours. Nat. Genet. 1998;20:291–293. doi: 10.1038/3108. [DOI] [PubMed] [Google Scholar]
- Prindle MJ, Fox EJ, Loeb LA. The mutator phenotype in cancer: Molecular mechanisms and targeting strategies. Curr. Drug Targets. 2010 doi: 10.2174/1389450111007011296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renan MJ. How many mutations are required for tumorigenesis? Implications from human cancer data. Mol. Carc. 1993;7:139–146. doi: 10.1002/mc.2940070303. [DOI] [PubMed] [Google Scholar]
- Rehen SK, McConnell MJ, Kaushal D, Kingsbury MA, Yang AH, Chun J. Chromosomal variation in neurons of the developing and adult mammalian nervous system. Proc. Natl. Acad. Sci. U.S.A. 2001;98:13361–13366. doi: 10.1073/pnas.231487398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehen SK, Yung YC, McCreight MP, Kaushal D, Yang AH, Almeida BS, Kingsbury MA, Cabral KM, McConnell MJ, Anliker B, Fontanoz M, Chun J. Constitutional aneuploidy in the normal human brain. J. Neurosci. 2005;25:2176–2180. doi: 10.1523/JNEUROSCI.4560-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ro L-S, Lai S-L, Chen C-M, Chen S-T. Deleted 4977-bp mitochondrial DNA mutation is associated with sporadic amyotrophic lateral sclerosis: A hospital-based case-control study. Muscle Nerve. 2003;28:737–743. doi: 10.1002/mus.10504. [DOI] [PubMed] [Google Scholar]
- Robinson DR, Goodall K, Albertini RJ, O'Neill JP, Finette B, Sala-Trepat M, Moustacchi E, Tates AD, Beare DM, Green MH, et al. An analysis of in vivo hprt mutant frequency in circulating T-lymphocytes in the normal human population: a comparison of four datasets. Mutat. Res. 1994;313:227–247. doi: 10.1016/0165-1161(94)90053-1. [DOI] [PubMed] [Google Scholar]
- Salk JJ, Fox EJ, Loeb LA. Mutational heterogeneity in human cancers: Origin and consequences. Annu. Rev. Pathol.-Mech. 2010;5:51–75. doi: 10.1146/annurev-pathol-121808-102113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk JJ, Salipante SJ, Risques RA, Crispin DA, Li L, Bronner MP, Brentnall TA, Rabinovitch PS, Horwitz MS, Loeb LA. Clonal expansions in ulcerative colitis identify patients with neoplasia. Proc. Natl. Acad. Sci. USA. 2009;106:20871–20876. doi: 10.1073/pnas.0909428106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schapira AH. Mitochondria in the aetiology and pathogenesis of Parkinson's disease. Lancet Neurol. 2008;7:97–109. doi: 10.1016/S1474-4422(07)70327-7. [DOI] [PubMed] [Google Scholar]
- Schriner SE, Linford NJ, Martin GM, Treuting P, Ogburn CE, Emond M, Coskun PE, Ladiges W, Wolf N, Remmen HV, Wallace DC, Rabinovitch PS. Extension of murine life span by overexpression of catalase targeted to mitochondria. Science. 2005;308:1909–1911. doi: 10.1126/science.1106653. [DOI] [PubMed] [Google Scholar]
- Schwarze SR, Lee CM, Chung SS, Roecker EB, Weindruch R, Aiken JM. High levels of mitochondrial DNA deletions in skeletal muscle of old rhesus monkeys. Mech. Ageing Dev. 1995;83:91–101. doi: 10.1016/0047-6374(95)01611-3. [DOI] [PubMed] [Google Scholar]
- Shoffner JM, Watts RL, Juncos JL, Torroni A, Wallace DC. Mitochondrial oxidative phosphorylation defects in parkinson's disease. Ann. Neurol. 1991;30:332–339. doi: 10.1002/ana.410300304. [DOI] [PubMed] [Google Scholar]
- Simonetti S, Chen X, DiMauro S, Schon EA. Accumulation of deletions in human mitochondrial DNA during normal aging: Analysis by quantitative PCR. BBA-Mol. Basis Dis. 1992;1180:113–122. doi: 10.1016/0925-4439(92)90059-v. [DOI] [PubMed] [Google Scholar]
- Sliwa P, Kluz J, Korona R. Mutational load and the transition between diploidy and haploidy in experimental populations of the yeast Saccharomyces cerevisiae. Genetica. 2004;121:285–293. doi: 10.1023/b:gene.0000039846.12313.98. [DOI] [PubMed] [Google Scholar]
- Stanfel MN, Shamieh LS, Kaeberlein M, Kennedy BK. The TOR pathway comes of age. Biochim. Biophys. Acta. 2009;1790:1067–1074. doi: 10.1016/j.bbagen.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilard L. On the nature of the aging process. Proc. Natl. Acad. Sci. USA. 1959;45:30–45. doi: 10.1073/pnas.45.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tates AD, van Dam FJ, van Mossel H, Schoemaker H, Thijssen JC, Woldring VM, Zwinderman AH, Natarajan AT. Use of the clonal assay for the measurement of frequencies of HPRT mutants in T-lymphocytes from five control populations. Mutat. Res. 1991;253:199–213. doi: 10.1016/0165-1161(91)90133-s. [DOI] [PubMed] [Google Scholar]
- Thomas B, Beal MF. Parkinson's disease. Hum. Mol. Genet. 2007;16:R183–R194. doi: 10.1093/hmg/ddm159. [DOI] [PubMed] [Google Scholar]
- Trainor KJ, Wigmore DJ, Chrysostomou A, Dempsey JL, Seshadri R, Morley AA. Mutation frequency in human lymphocytes increases with age. Mech. Ageing Devel. 1984;27:83–86. doi: 10.1016/0047-6374(84)90084-8. [DOI] [PubMed] [Google Scholar]
- Tran HT, Gordenin DA, Resnick MA. The 3'→5'exonucleases of DNA polymerases δ and ε and the 5'→3' exonuclease ExoI have major roles in postreplication mutation avoidance in Saccharomyces cerevisiae. Mol. Cell Biol. 1999;19:2000–2007. doi: 10.1128/mcb.19.3.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treuting PM, Linford NJ, Knoblaugh SE, Emond M, Morton JF, Martin GM, Rabinovitch PS, Ladiges WC. Reduction of age-associated pathology in old mice by overexpression of catalase in mitochondria. J. Gerontol. A-Biol. 2008;63A:813–824. doi: 10.1093/gerona/63.8.813. [DOI] [PubMed] [Google Scholar]
- Trifunovic A, Wredenberg A, Falkenberg M, Spelbrink JN, Rovio AT, Bruder CE, Bohlooly-Y M, Gidlö S, Oldfors A, Wibom R, Törnell J, Jacobs HT, Larsson N-G. Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature. 2004;429:417–423. doi: 10.1038/nature02517. [DOI] [PubMed] [Google Scholar]
- van der Pluijm I, Garinis GA, Brandt RM, Gorgels TG, Wijnhoven SW, Diderich KE, de Wit J, Mitchell JR, van Oostrom C, Beems R, Niedernhofer LJ, Velasco S, Friedberg EC, Tanaka K, van Steeg H, Hoeijmakers JH, van der Horst GT. Impaired genome maintenance suppresses the growth hormone--insulin-like growth factor 1 axis in mice with Cockayne syndrome. PLoS Biol. 2007;5:e2. doi: 10.1371/journal.pbio.0050002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesan RN, Treuting P, Fuller ED, Norwood TH, Ladiges W, Preston BD, Loeb LA. Mutation at the polymerase active site of mouse DNA polymerse δ increases genomic instability and accelerates carcinogenesis. Mol. Cell. Biol. 2007;27:7669–7682. doi: 10.1128/MCB.00002-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verge B, Alonso Y, Valero J, Miralles C, Vilella E, Martorell L. Mitochondrial DNA (mtDNA) and schizophrenia. Eur. Psychiat. 2011;26:45–56. doi: 10.1016/j.eurpsy.2010.08.008. [DOI] [PubMed] [Google Scholar]
- Vermulst M, Bielas JH, Kujoth GC, Ladiges WC, Rabinovitch PS, Prolla TA, Loeb LA. Mitochondrial point mutations do not limit the natural lifespan of mice. Nat. Genetics. 2007;39:540–543. doi: 10.1038/ng1988. [DOI] [PubMed] [Google Scholar]
- Vermulst M, Wanagat J, Kujoth GC, Bielas JH, Rabinovitch PS, Prolla TA, Loeb LA. DNA deletions and clonal mutations drive premature aging in mitochondrial mutator mice. Nat. Genetics. 2008;40:392–394. doi: 10.1038/ng.95. [DOI] [PubMed] [Google Scholar]
- Vijg J. Somatic mutations and aging: A re-evaluation. Mutat. Res. 2000;447:117–135. doi: 10.1016/s0027-5107(99)00202-x. [DOI] [PubMed] [Google Scholar]
- Vijg J, Dollé ME. Large genome rearrangements as a primary cause of aging. Mech. Age. Devel. 2002;123:907–915. doi: 10.1016/s0047-6374(02)00028-3. [DOI] [PubMed] [Google Scholar]
- Warburg O. On respiratory impairment in cancer cells. Science. 1956;124:269–270. [PubMed] [Google Scholar]
- Williams GC. Pleiotropy, natural selection, and the evolution of senescence. Evolution. 1957;11:398–411. [Google Scholar]
- Williams SL, Huang J, Edwards YJ, Ulloa RH, Dillon LM, Prolla TA, Vance JM, Moraes CT, Züchner S. The mtDNA mutation spectrum of the progeroid Polg mutator mouse includes abundant control region multimers. Cell Metab. 2010;12:675–682. doi: 10.1016/j.cmet.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Zhao K, Calingasan NY, Luo G, Szeto HH, Beal MF. Mitochondria targeted peptides protect against 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine neurotoxicity. Antioxid. Redox Sign. 2009;11:2095–2104. doi: 10.1089/ars.2009.2445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao K, Zhao G-M, Wu D, Soong Y, Birk AV, Schiller PW, Szeto HH. Cell-permeable peptide antioxidants targeted to inner mitochondrial membrane inhibit mitochondrial swelling, oxidative cell death, and reperfusion injury. J. Biol. Chem. 2004;279:34682–34690. doi: 10.1074/jbc.M402999200. [DOI] [PubMed] [Google Scholar]
- Zheng L, Dai H, Zhou M, Li M, Singh P, Qiu J, Tsark W, Huang Q, Kernstine K, Zhang X, Lin D, Shen B. Fen1 mutations result in autoimmunity, chronic inflammation and cancers. Nature Med. 2007;13:812–819. doi: 10.1038/nm1599. [DOI] [PubMed] [Google Scholar]