Abstract
Purpose
Many degenerative phenomena frequently result into kyphotic lumbar and thoracic deformities or cause their progression combined with deformities on the frontal plane of the spine. In these patients, the progression of the sagittal imbalance may lead to a series of disabling functional and painful consequences. The analysis of the spinopelvic parameters biases the choice of the correction surgical strategy aimed at restoring a good tri-dimensional and sagittal balance of the spine.
Materials and methods
Sample included 62 patients treated in our Operation Unit that were enrolled for evaluation; they were affected with prevailing sagittal deformities.
Results
Clinical results were evaluated through the administration of SF-36, Oswestry Disability Index (ODI), Roland Morris (RM), and visual analogical scale (VAS).
Conclusions
In our experience, patients with sagittal imbalance and short fusion areas show a higher risk of correction loss; the arthrodesis area must include the thoracolumbar junction, and it is often necessary to include the whole thoracic spine in the arthrodesis area. This is to avoid any loss of correction, implants mobilization, and proximal hyperkyphosis.
Keywords: Adult kyphosis, Spinopelvic parameters, Arthrodesis area
Purpose
Adult vertebral deformities are referred to the spine surgeon for two events (not necessarily connected): the clinical aggravation of the deformity and the onset of pain. Several degenerative phenomena cause kyphotic deformities; in the degenerative sequence, the prevailing role in the genesis of the deformity belongs to the degeneration of the intervertebral disk. Sagittal deformities (excluding those resulting from infection, post-traumatic or neoplastic processes) may be classified as follows: thoracolumbar kyphosis, hyper-rotatory kyphosis (either lumbar or thoracolumbar), junctional kyphosis, thoracic hyperkyphosis. Such deformities may be differently combined with frontal deformities; but since the sagittal imbalance is a prevalent component, the strategic surgery will be different from the one used for the scoliotic deformity alone. Almost all adult patients affected with deformities are referred to the surgeon basing on the current symptoms, as shown in the work by Pérennou et al. [13] (adulthood scoliosis was revealed by low back pain in 86% of the cases). These patients report prevalent lumbar pain as well as dorsal pain that worsen when standing and also when under strain, often combined with radicular disorders. Kyphotic deformities are often associated with frontal deformities (i.e., adult’s lumbar scoliosis); for such reasons, the surgeon’s attention is often focused on the lumbosacral spine that is the location of pain. The disk degenerative alterations together with the alteration of the sagittal balance (hyper-rotatory kyphosis) are often responsible for the impairing clinical syndrome. The sagittal balance alteration of the deformed spine may therefore originate as very serious forms of disorder (global kyphosis) that are prevalent when compared to frontal deformity. The anterior imbalance may be considered as the most difficult deformity part to be corrected; for this reason, in this study we have analyzed in adults kyphotic deformities, besides the patients’ health conditions, the spinal sagittal balance that is fundamental for the prognosis and treatment indication it should suggest. The spine sagittal alignment is as much important as its relation with the pelvis [19]. The variations in the sagittal curves are directly connected to the changes in the pelvic orientation, as observed by some authors who defined the morpho-functional features of the pelvis [5, 7, 17] by using pelvic parameters. The main pelvic parameters are: pelvic incidence (PI), sacral slope (SS), and pelvic tilt (PT) [10]. The PI, as defined by Duval-Beaupère et al. [10], plays a fundamental role in ruling the sagittal balance. It is a stable anatomic parameter in every human being. There is a geometric link among PI (morphologic parameter), PT and SS (variable functional parameters according to the orientation of sacrum and pelvis) leading to the equation: PI = PT + SS [10, 14]. The main ruling mechanism of the sagittal balance is given by the rotation ability of the pelvis around the femoral head axis. In the geometric correlation among these parameters the PI creates and changes the respective PT and SS values, so ruling the compensation of the sagittal imbalance [17]. Idiopathic scoliosis (progressive and in adult age) and de novo scoliosis are among the kyphotic deformities [6]. It is observed that the progress of such deformities be frequent in the kyphosis [1].
Methods
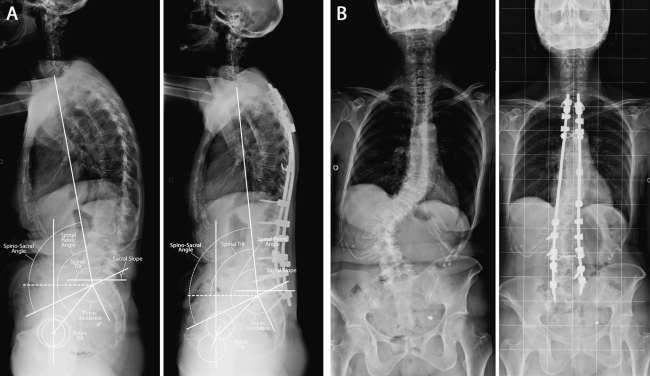
Retrospective assessment was performed on 62 patients treated at our Operation Unit; subjects suffered with painful prevailing deformities at the sagittal level: 59 female patients and three males with an average age of 59 ± 8.3 (range 45–75), average follow-up of 76.4 months (range 1–10 years). The patients may be divided into three groups. Group A (21 patients): degenerative lumbar kyphosis (five cases showed association with de novo lumbar scoliosis) → posterior surgical treatment in 20 cases (two with pedicle subtraction and one with double combined approach). Group B (21 patients): thoracolumbar kyphosis (in 10 cases associated with scoliosis) → posterior surgical treatment in 21 patients (four with pedicle subtraction) [20] (Fig. 1). Group C (20 patients): flat back syndrome as outcome of posterior correction surgery → posterior correction surgery in 20 patients (10 with pedicle subtraction, 10 with high extent of thoracic spine). All patients were treated using a hybrid system (hooks, screws, rods associated with clamps in the past few years).
Fig. 1.
S.A., aged 75, male, global thoracolumbar kyphosis, pre and post-operative lateral projection X-rays (a); pre- and postoperative a–p projection X-rays (b). Preoperative and postoperative clinical photo (c, d)
Results
Clinical results were assessed through the administration of SF-36, Oswestry Disability Index (ODI), Roland Morris (RM) questionnaires about the patients’ health conditions; the subjective evaluation of pain was performed by means of visual analogical scale (VAS).
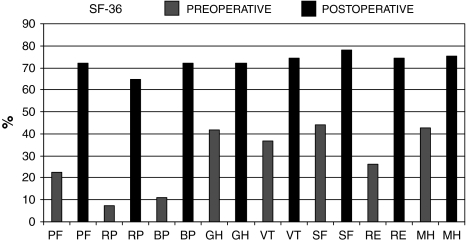
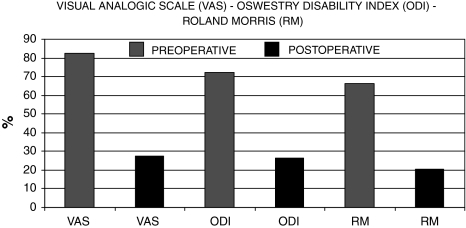
SF-36 → (PF pre 22.4%/PF post 72.2%)—(RP pre 7.4%/RP post 64.6%)—(BP pre 10.8%/BP post 72.3%)—(GH pre 42%/GH post 72%)—(VT pre 36.7%/VT post 74.2%)—(SF pre 44%/SF post 78%)—(Re pre 26.4%/RE post 74.6%)—(MH pre 42.6%/MH post 75.5%)—SF-36 average → (pre 30% ± 14.6/post 72.6% ± 30.6)—VAS → (pre 82.3/post 27.7)—ODI → (pre 72%/post 26.4%)—RM → (pre 16 ± 3.2/post 4.9 ± 5.1) (Figs. 2, 3). A statistically significant reduction in pain was observed (p < 0.0001); the other results were not statistically significant, seen the non-homogeneous groups and numbers. Moreover, the following spinopelvic parameters were evaluated: PI, PT, SS, lumbar lordosis (LL), thoracic kyphosis (TK) and C7 plumb line (C7 PL) (Fig. 4). Both TK and LL showed a statistically significant pre and post-surgery correlation; the same applies to the correlation between sacral slope and lumbar lordosis (p < 0.001). The spino-sacral angle (SSA) was evaluated afterwards.
Fig. 2.
SF-36 questionnaire results
Fig. 3.
ODI, RM questionnaire and VAS results. A statistically significant reduction in pain was observed (p < 0.0001)
Fig. 4.
Spinopelvic parameters results. Both thoracic kyphosis and lumbar lordosis showed a statistically significant correlation; the same applies to the correlation between sacral slope and lumbar lordosis (p < 0.001)
We had the following complications: three instrument mobilizations (we had to perform surgery again for restoration), two pseudarthrosis (surgery was performed again to repair), three flat back syndrome (failed integument of dorsal kyphosis), two dehiscence of surgical wound (skin plastic surgery); two neurologic complications (lower limbs paraparesis, one of which re-operated in emergency because when the patient woke up she was paraplegic) with full subsequent recovery (one in 20 days and the other in 6 months).
Conclusions
As shown in many studies, it is well known that pelvic morphology affects the spinal sagittal balance and the LL in particular [10, 12, 21]. Roussouly et al. [15] described a classification system for lordosis (four kinds) that takes into consideration the sagittal profile features given by the pelvis, sacrum, and lumbosacral junction orientation.
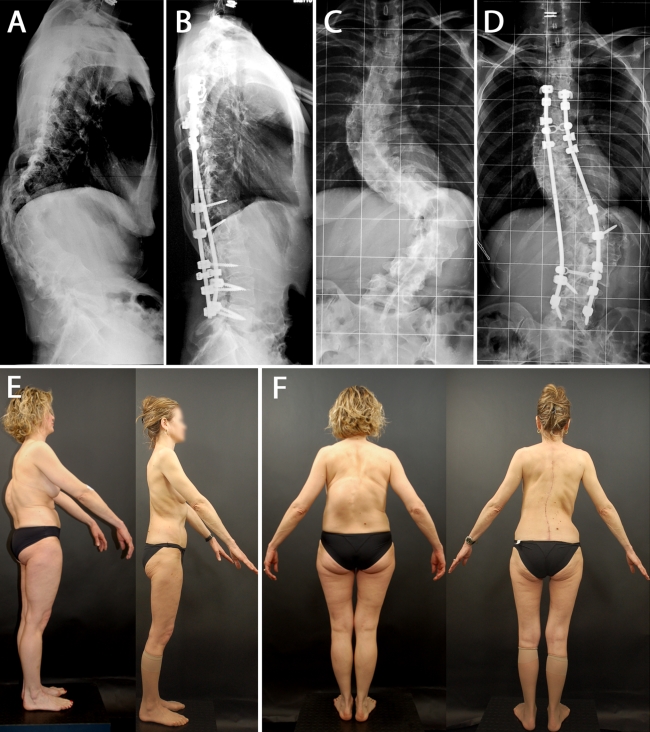
The same author believes that to assess the lordosis geometry at the best, it must be studied as a single curve but broken down into two tangent curves (upper arc and lower arc) [15, 17]. The upper arc of lumbar lordosis is same as the lower arc in thoracic kyphosis and in the degenerative spine the two angles depend on each other [17]. There is a close relation between the sagittal balance of the thoracic and lumbar spine for which all changes deriving from a degenerative evolution are interdependent and therefore need an overall analysis of the two curves. The lordosis lower arc (distal) of corresponds to SS and it is important to determine the overall lordosis [17]. The above classification (study on a population of asymptomatic volunteer adults) is divided into four kinds according to the SS variations (also considering the section of the apex and the number of lordotic vertebrae) [14, 15]. The reciprocal relation between SS and the lumbar curve features is considered as a fundamental component of the overall sagittal balance [15]. Moreover, many authors considered the middle of C7 as a fundamental point in the overall sagittal balance [2, 14, 22]. The reference parameter we used was the C7 PL, which is the vertical line starting from the middle of C7 and usually intersects the upper end (posterior) of the S1 plate (superior endplate of S1). Usually, to understand whether the sagittal balance was good, the distance between C7 PL and two sacral-pelvic reference points was calculated (the middle of the hip axis, HA and the posterior end of the sacral plate). Another method for the study of the overall spinal balance is given by the use of the spinopelvic angles: spinal tilt (ST), spinopelvic angle (SPA), and spino-sacral angle (SSA) [16–18]. The ST is the angle formed by the horizontal line and the line starting from the middle of C7 and reaching the middle of the sacral plate. The SSA is formed by the line going from the middle of C7 to the middle of the sacral plate and the surface line of the sacral plate (Fig. 5a). Spinal tilt is a functional parameter related to the spine overall balance; SSA is a morphological parameter related to the spine overall kyphosis [18]. The spinopelvic angle (SPA) is given by the line going from the middle of C7 to the middle of the sacral and the line going from the middle of the sacral plate to the middle of the femoral head and may be considered as a posture parameter (Fig. 5a). For the study of the overall spinal sagittal balance, our patients were administered X-rays to the whole spine in orthostatic position and lateral projection, with visible pelvis and femoral heads. The references for a correct diagnosis are: pelvic parameters (PI, PT, and SS), kind of LL, position of C7 PL and spinopelvic parameters (SSA, SPA) [3, 10, 15, 17]. Moreover, the pre-surgery assessment with X-rays in hyperextension on pilot is of particular importance. The latter may provide us with further information about the need of a prospective anterior approach [23]. In case of severe hyperkyphosis, a double approach may be needed for a better mobilization of the curve, to improve the surgical correction and obtain a stable and durable circumferential arthrodesis. The target of the surgical strategy is the repristination of the sagittal balance. In our experience, we noticed the importance of restoring a good lordosis also in cases of lumbar fusion, to avoid the negative consequences of the flat back syndrome, as described by many authors [8]. Among the treated patients, some cases of flat back syndrome as outcome of lumbar fusion surgery in degenerative spondylosis were referred to us. In such cases, after reviewing the preoperatory sagittal balance, in the first approach we noted the importance to extend the arthrodesis to the whole lumbar spine with coating of the thoracolumbar junction (being the area concerned with kyphosis); besides the importance of restoring a physiological lordosis during the fusion and to extend the hips during surgery. In ten cases, patients affected with flat back syndrome were treated with pedicle subtraction osteotomy [4, 20] (and in ten other cases, where only the lower lumbar spine had been treated, with extension to the upper thoracic spine to restore the sagittal imbalance with SSA values lower than 95°). As already stressed out, the recovery of the sagittal balance is of paramount importance also in case of treatment of deformities at the frontal level (Fig. 6). We believe that there are two fundamental aspects in the surgical strategy: proximal extension of instrumentation and 3D correction of deformity. As for the proximal extension, it is always (or often) needed to include the whole thoracic spine in the arthrodesis area, all this to prevent any instruments proximal mobilizations or proximal hyperkyphosis (Fig. 7). In our experience, after the assessment of the pelvic parameters and the kind of lordosis has been carried out, usually with a SSA angle lower than 103 ± 3° (low pelvic incidence) or smaller than 96 ± 3° (high pelvic incidence), we extend the arthrodesis to the whole thoracic spine (no statistic significance). The 3D correction depends on the severity of the curve and goes through the priority restoration of the sagittal balance (techniques are different according to the kind of deformity—de-rotation of the convex rod, clamps stressing, postural reduction and cantilever, pedicle subtraction osteotomy) [17]. As already said, any possible residual sagittal deformities may lead to proximal mobilizations of the instrumentation and proximal hyperkyphosis. An improvement in the pain clinical picture and in the overall 3D spinal balance may be obtained through the segmental correction of the deformity (Fig. 1). By segmental correction of the deformity we mean the correction of the following segments: (1) frontal curves (lumbar and thoracic), (2) sagittal deform segments (lumbar kyphosis, leveling of the TK, upper thoracic hyperkyphosis, overall hyperkyphosis), and (3) transition areas (lower junctional area, junctional kyphosis). As seen before, there is a direct correlation between the thoracic and the lumbar; therefore, in patients with sagittal imbalance, the restoration of lordosis is not enough but it is necessary to cover the kyphosis to give a correct balance and make sure the arthrodesis lasts as much as the correction [9]. As referred by many authors, the sagittal spinal orientation parameters are interdependent; their interaction results and leads to a stable and compensated posture [11]. Therefore, the correction of the sagittal balance in kyphotic deformities goes through a close analysis of the above listed spinopelvic parameters as well as of the kind of deformity to reach a harmonic and well-compensated restoration of the rachis overall sagittal balance.
Fig. 5.
PC, aged 57, female, lumbar scoliosis, thoracolumbar kyphosis and thoracic hyperkyphosis; preoperative (SSA = 102°) and postoperative (SSA = 112°) lateral projection X-rays (a). Preoperative and postoperative a–p projection X-rays (b)
Fig. 6.
G.A., aged 54, female; hyper-rotatory thoracolumbar kyphosis and thoracic and thoracolumbar scoliosis. Preoperative lateral projection X-rays and 2 years follow-up (a, b), performed pedicle subtraction osteotomy. Preoperative a–p projection X-rays and 2 years follow-up (c, d). Preoperative clinical photo and postoperative clinical photo (e, f)
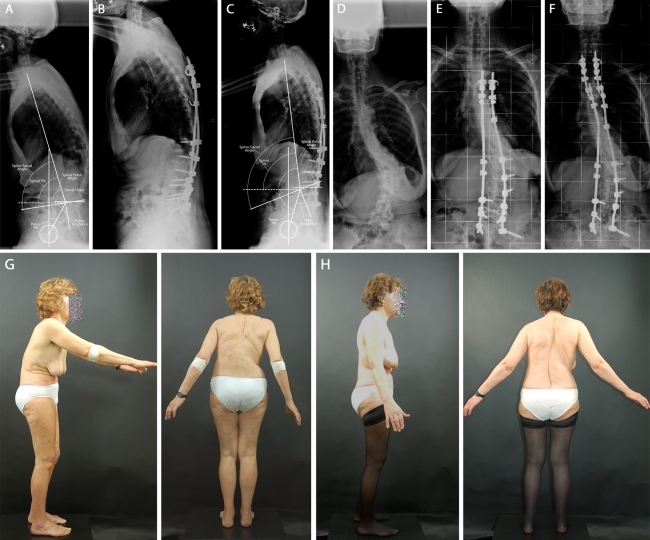
Fig. 7.
D.A.S., aged 62, female, lumbar scoliosis, thoracolumbar kyphosis; preoperative lateral projection X-rays (SSA = 81°) (a), proximal mobilization after 8 months (b), X-rays after repristination of the proximal instruments (SSA = 106°) (c). Preoperative X-rays in a–p projection (d), proximal mobilization (e), after proximal repristination (f). Preoperative and postoperative clinical photo (g, h)
Surgical treatment of kyphotic deformities has always been a reason of discussion due to its indications, for the choice of the extension of the arthrodesis area and of the approach, either posterior or combined. Kyphotic deformities are often associated with frontal deformities; this is why a thorough analysis is needed in order to reach a satisfactory tri-dimensional balance. The latter goes through the priority of restoring the overall sagittal balance that may be obtained by studying the pelvic parameters, the kind of LL and the spinopelvic parameters. Sagittal imbalance may be considered as the most difficult part of deformity to be improved. The instrument strategy must be carried out by analyzing the different segments of the deformity to implement the most suitable treatment aimed at preventing possible residual sagittal deformities that may induce any instrumentation proximal mobilizations and proximal hyperkyphosis. A careful restoration of the LL may avoid the negative effects of the flat back syndrome. According to our experience, patients with sagittal imbalance and short fusion areas show a higher risk of loss of correction; it is necessary to comprehend the thoracolumbar junction and we often need to include the whole thoracic spine in the arthrodesis area. The elements of the study for an adequate treatment of such complex deformities are the following: analysis of the overall sagittal balance, kind of deformity, degree of curve rectification, and correct extension of the arthrodesis area. We consider our experience as positive and useful in searching for more precise and appropriate indications to the treatment that must be supported by figures and confirmed by significant statistic data coming from the studies in progress.
Conflict of interest
None.
Contributor Information
Francesco M. Finocchiaro, Phone: +39-0498213367, FAX: +39-0498213366, Email: fmfinocchiaro@gmail.com
Daniele A. Fabris Monterumici, Email: daniele.fabrismonterumici@gmail.com.
References
- 1.Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 2.Barrey C (2004) Equilibre sagittal pelvi-rachidien et pathologies lombaires dégénératives. Etude comparative à propos de 100 cas. Thése Doctorat, Universitè Claude-Bernard, Lyon 1
- 3.Boulay C, Tardieu C, Hecquet J, Benain C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupère G, Péllissier J. Sagittal allignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15(4):415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bridwell KH, Lewis SJ, Rinella A, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. JBJS. 2003;85-A:454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Duval-Beaupère G, Schmidt C, Cosson P. A barycentremetric study of the sagittal shape of the spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 6.Fabris D, Costantini S, Nena U, Lo Scalzo V, Finocchiaro F. The surgical treatment of adult lumbar scoliosis. Chir Narzadow Ruchu Ortop Pol. 2004;69(4):279–285. [PubMed] [Google Scholar]
- 7.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25(5):575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 8.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine. 2001;10:314–319. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SH, Kim KT, Suk KS, Lee JH, Seo EM, Huh DS. agittal decompensation after corrective osteotomy for lumbar degenerative kyphosis: classification and risk factors. Spine. 2011;36(8):E538–E544. doi: 10.1097/BRS.0b013e3181f45a17. [DOI] [PubMed] [Google Scholar]
- 10.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J. 2007;16:227–234. doi: 10.1007/s00586-005-0013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangione P, Gomez D, Senegas J. Normal and pathologic sagittal balance of the spine and pelvis (in french) Rev Chir Orthop Reparatrice Appar Mot. 1997;83:22–32. [PubMed] [Google Scholar]
- 13.Pérennou D, Marcelli C, Hérisson C, Simon L. Adult lumbar scoliosis. Epidemiologic aspects in a low-back pain population. Spine. 1994;19(2):123–128. doi: 10.1097/00007632-199401001-00001. [DOI] [PubMed] [Google Scholar]
- 14.Roussoly P, Berthonnaud E, Dimnet J. Geometrical and mechanical analysis of lumbar lordosis in an asymptomatic population: proposed classification (in french) Rev Chir Orthop Reparatrice Appar Mot. 2003;89(7):632–639. [PubMed] [Google Scholar]
- 15.Roussoly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30(3):346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 16.Roussouly P, Nnadi C. Sagittal plane: an overwiew of interpretation and management. Eur Spine J. 2010;19:1824–1836. doi: 10.1007/s00586-010-1476-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J. 2011;20(suppl 5):S609–S618. doi: 10.1007/s00586-011-1928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine: biomechanical approach. Eur Spine J. 2011;20(suppl 5):S578–S585. doi: 10.1007/s00586-011-1924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine. 2009;34(17):1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 20.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142–152. [PubMed] [Google Scholar]
- 21.Vaz G, Roussoly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vendantam R, Lenke LG, Bridwell KH, et al. The effect of variation in arm position on sagittal spinal alignment. Spine. 2000;25:2204–2209. doi: 10.1097/00007632-200009010-00011. [DOI] [PubMed] [Google Scholar]
- 23.White AA, Panjabi MM, Thomas CL. The clinical biomechanics of kyphotic deformities. Clin Orthop Relat Res Oct. 1977;128:8–17. [PubMed] [Google Scholar]