Abstract
Purpose
Anterior decompression of the craniovertebral junction is reserved to patients with irreducible ventral bulbo-medullary lesions and rapidly deteriorating neurological functions. Classically performed through the transoral approach, the exposure of this region can be now achieved by a minimally invasive endonasal endoscopic approach (EEA).
Methods
Four patients with irreducible, anterior bulbo-medullary compression due to rheumatoid pannus and basilar invagination were enrolled. The imaged-guided EEA was used to resect the odontoid process, trying to preserve the C1 anterior arch.
Results
Neurological improvement and adequate bulbo-medullary decompression were obtained in all patients. In two cases, anterior C1 ring was preserved. These patients did not required a posterior fusion.
Conclusions
Compared with the standard transoral technique, the EEA provides the same good exposure but with potentially less complications. The preservation of the anterior C1 arch can contribute to avoid cranial settling and posterior fusion with its related risk of subaxial instability.
Keywords: Odontoidectomy, Basilar invagination, Endoscopy, Transnasal approach, Craniocervical junction, Minimally invasive surgery
Introduction
Anterior approaches to the craniovertebral junction (CVJ) have traditionally involved open surgical procedures. The transoral odontoidectomy is the treatment of choice in a variety of diseases affecting the CVJ, including basilar invagination, rheumatoid arthritis or neoplastic processes [1, 2]. This approach provides a wide exposure with large working angles, but it includes some disadvantages like a deep surgical corridor and the risk of a postoperative dysphonia, an oral flora contamination, and a prolonged intubation [3]. The necessity to overcome these issues and the recent advances in endoscopic technology have led to an increasing use of less invasive surgical procedures [4, 5]. In this paper, we report our experience with the pure endoscopic neuronavigation-assisted transnasal approach for resection of odontoid process and rheumatoid pannus removal in four elderly patients presenting with symptomatic anterior bulbo-medullary compression. The peculiarities of this technique are the minimal invasiveness offered by endoscopy and the possibility to avoid the damages related to tongue retraction, palate splitting and upper airway swelling. Furthermore, this approach allows a better working angle with the possibility to preserve the anterior arch of C1 that is critical for the biomechanical stability of the occiput-C2 segment [6, 7]. This technical nuance can contribute to avoid the phenomenon of cranial settling and the need for a posterior fusion with its related risks of subaxial subluxation development [8].
Materials and methods
From January 2009 to August 2010, we recruited four elderly patients with irreducible, symptomatic, anterior bulbo-medullary compression due to rheumatoid pannus or basilar invagination. One patient, surgically treated 2 years before for an basilar invagination by a transoral approach and posterior occipito-cervical fusion, was treated again for persistent spinal cord compression by residual odontoid process invagination. All patients underwent a transnasal image-guided fully endoscopic resection of odontoid process to decompress the bulbo-medullary junction (Fig. 1). CVJ evaluation was always obtained by magnetic resonance imaging (MRI), computerized tomography (CT) scan and dynamic X-ray (Fig. 2). Pre- and postoperative neurologic disability assessment was obtained by Ranawat classification for patients with rheumatoid arthritis and by Nurick classification for the other ones [9, 10]. Postoperative neuroradiologic workup was scheduled by an immediate CT scan and by a 6-month and every year MRI and dynamic X-ray (Figs. 3, 4). For patients details, see Table 1.
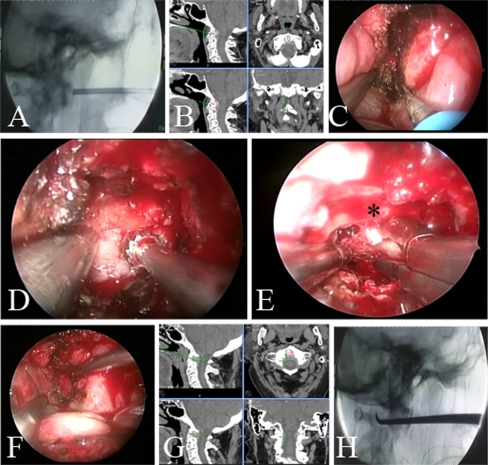
Fig. 1.
Intraoperative images. a, b After identification of anterior C1 tubercle by anatomical landmarks, its detection is confirmed by fluoroscopy and neuronavigation. c Linear incision in the midline of the nasopharyngeal mucosa and subperiosteal preparation of anterior C1 arch. d, e Drilling out the base of odontoid process with preservation of the anterior C1 arch (asterisk). This weakens the apex of dens that can be now easily pulled down by curette and removed by forceps. f–h Pulsating surgical cavity after decompression with anatomical limits of resection verified by neuronavigation and fluoroscopy
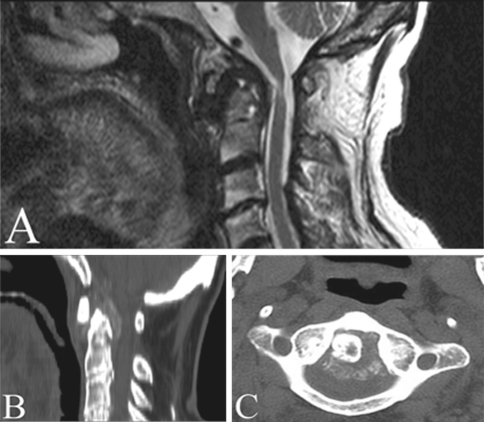
Fig. 2.
Preoperative neuroimaging studies. a, b Sagittal T2 MRI image and sagittal CT scan showing bulbo-medullary compression by rheumatoid pannus and the associated area of myelopathy. Cervicomedullary angle (CMA) measured on sagittal T2 MRI image was 137°. c Axial CT scan reveals the odontoid process with its backward rheumatoid pannus
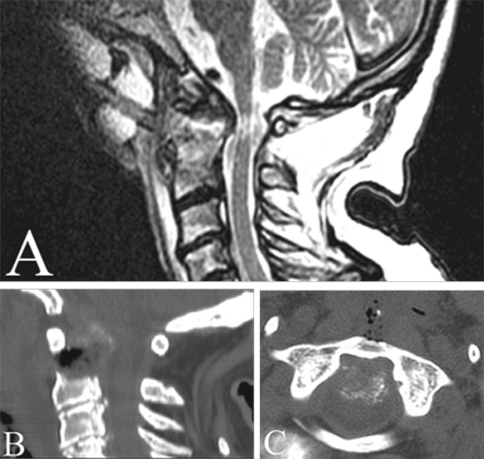
Fig. 3.
Postoperative neuroimaging studies. a Sagittal T2 MRI image showing adequate spinal cord decompression with an improved CMA (151°) and realignment of the medulla. After the decompression, the area of myelopathy was better visualized. b, c Sagittal and axial CT scans showed the odontoidectomy emphasizing the anterior C1 arch integrity
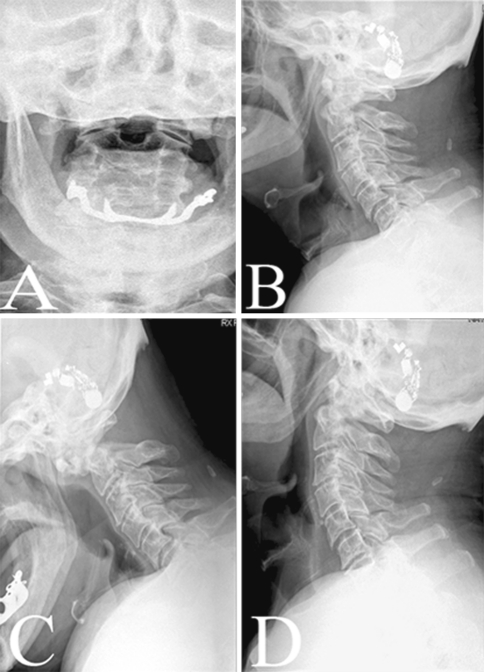
Fig. 4.
One-year follow-up cervical X-ray. a Transoral view showing the odontoidectomy. b–d Neutral and dynamic X-rays demonstrate the absence of cranial settling and subaxial instability
Table 1.
Summary of patients’ profile
| Patient initials, case no. | Age (sex) | Primary disease | Treatment | C1 arch integrity | Posterior fusion | Pre/postop disability class | External orthosis | Follow-up (months) | Tracheostomy/extubation (days) | Re-start oral feeding (days) |
|---|---|---|---|---|---|---|---|---|---|---|
| CC 1 | 72 (F) | Rheumatoid arthritis | Endoscopic transnasal odontoidectomy and rheumatoid pannus removal | No | Yes | IIIb/IIIa (Ranawat Class) | Rigid collar for 1 month | 31 | No/2 | 4 |
| PS 2 | 80 (M) | Rheumatoid arthritis | Endoscopic transnasal odontoidectomy and rheumatoid pannus removal | Yes | No | IIIb/IIIa (Ranawat class) | Soft collar for 15 days | 27 | No/2 | 3 |
| CC 3 | 69 (F) | Basilar invagination | Endoscopic transnasal odontoidectomy (transoral odontoidectomy and posterior occipital–cervical fusion 2 years before) | No | Already done at previous surgical procedure | VI/V (Nurick class) | No | 18 | No/2 | 5 |
| PP 4 | 76 (F) | Basilar invagination | Endoscopic transnasal odontoidectomy | Yes | No | IV/III (Nurick class) | Soft collar for 10 days | 12 | No/1 | 2 |
Surgical procedure
Multislice CT scan of the cervical spine was performed in all cases, along with dynamic X-ray and MRI images, to study the neurovascular structures of the craniocervical junction, the extent of the lesion, and the potential cervical flexion reachable during surgery. These imaging data were also used for registration of the neuronavigation system (BrainLAB, Heimstetten, Germany). A C-arm fluoroscope was set up for a true lateral view of the region of interest before surgery and was kept available throughout the procedure. Evoked potentials were monitored throughout the surgical procedure. The patient was placed in supine position with the head placed free in neutral position, with the possibility of slight flexion during the procedure to facilitate dens resection. The procedure started with immediate endoscopic view of the choana and retropharyngeal wall. A zero-degree endoscope was used as the primary working endoscope and mounted on a digital video camera system (Karl Storz GmbH & Co., Tuttlingen, Germany). A small portion of the posterior edge of the nasal septum was resected to ease bilateral application of dedicated long instrumentation [11]. In one patient, the right inferior turbinate was removed. In another one, the posterior part of the hard palate was thinned by drilling out the outer bone layer, making the hard palate more flexible to enhance the angle of “nasopalatine line” (K-line). After the identification of anterior C1 tubercle by anatomical landmarks, neuronavigation, and fluoroscopy (Fig. 1a, b), a small linear incision (about 3 cm) was made in the midline of the nasopharyngeal mucosa using a Bovie cautery (Bovie Medical Corp., St. Petersburg, FL), as first reported by Wu [12]. The present approach is straightforward to the midline of the nasopharynx rather than making a U-shaped flap, as in the procedure originally described by Kassam et al. [11]. This can decrease the risk of injury to the adjacent structures and facilitate the wound healing process, providing an adequate working area, as well. After subperiosteal preparation, any effort was spent to preserve the anterior arch of the atlas or, if needed, to drill only its anterior–inferior portion around the midline, but still maintaining the continuity of the C1 ring (Fig. 1c, d). At this stage, the drilling of the odontoid base weakens its apical part that can be then easily pulled downward in the working area and removed along with any remaining compressive inflammatory lesions, using a combination of high-speed drill, Sonopet ultrasonic bone curette (Synergetics, USA), and standard kerrison rongeurs (Fig. 1e). Adequate decompression was confirmed by good pulsations of the tectorial membrane. The wide surgical cavity was subsequently inspected by angled lens endoscope and anatomical limits of resection were verified by neuronavigation and fluoroscopy (Fig. 1f–h). Finally, the nasopharyngeal defect was reapproximated and just covered with fibrin glue. Lumbar drainage, intra- or postoperatively, was not used. Tracheostomy was never needed as well as enteric tube feeding.
Results
In this short series of patients, adequate decompression of the bulbo-medullary junction was achieved by transnasal image-guided fully endoscopic approach. Anterior C1 ring was preserved in two patients with no need for a posterior fusion, until now. No major complications occurred after surgery, intensive care unit (ICU) staying was short and uneventful, and oral feeding was rapidly re-started. Length of hospitalization was usually less than 1 week. In only one case, submitted to a posterior occipito-cervical fusion 2 days later the endonasal surgery, the hospital stay was 9 days. At 1-year follow-up, all patients showed neurological improvement, with no signs of spinal instability among the two patients with anterior C1 arch preservation and no posterior fusion. For further details, see Table 1.
Discussion
Treatment of anterior bulbo-medullary junction compressions can be performed by different surgical procedures being the type of the approach dictated by the nature and the extension of the lesion [3]. The most important issue to consider is whether or not the abnormality is reducible [13]. When preoperative dynamic X-ray demonstrates a reducible compression, patients may require only a surgical reduction and a posterior occipital–cervical or C1–C2 fusion [14, 15]. Nevertheless, in case of patients affected by a ventral irreducible spinal cord lesion and progressive neurological deterioration, surgical removal of the compression is required and it can be reached by an anterior approach, usually associated to a posterior fusion [16]. The transoral-transpharyngeal technique, with or without the addition of extensive variations (such as a transmandibular–circumglossal approach or Le Fort osteotomies), is considered the standard anterior approach to the CVJ [1, 2]. However, this surgical technique often involves the splitting of structures such as the soft palate, mandible, and maxilla and, even though the recent refinements in the surgical steps improved results, some severe drawbacks still exist. These include the risk of bacterial contamination secondary to oral cavity penetration, prolonged postoperative intubation and nasogastric tube feeding, along with potential effects on phonation. Closure of the oropharyngeal incision can be difficult after a transoral approach because of wound contamination by saliva and heavy bacterial flora. In addition, patients with an oral aperture of less than 3 cm might not be suitable for transoral approach [16]. All these issues have served as an impetus to explore alternative and less invasive treatment options, especially in fragile, elderly patients [11, 17]. Advances in endoscopic technology and equipment have allowed the use of minimally invasive techniques in the craniocervical junction, as well. In 2007, Wolinsky et al. [17] reported three odontoidectomies performed by the endoscopic transcervical approach. They preserved the integrity of the pharyngeal mucosa, which greatly minimized the risk of contamination by bacterial flora, but the limitation of this approach was its longer working distance and the difficulty in performing the procedure in obese or barrel-chest patients and in kyphotic cervical spine. Transcervical odontoidectomy also involves the destruction of the C2 body and may cause more soft tissue swelling of the posterior oropharyngeal wall. In 2005, Kassam et al. [11] first reported the endoscopic endonasal approach for resection of odontoid process and rheumatoid pannus in a 73-year-old woman. We used this technique for our patients, albeit with some modifications. These include a midline linear incision of the nasopharyngeal mucosa rather than the creation of a flap, the non-opening of the sphenoid sinus, and the attempt to preserve the anterior C1 arch continuity. This can greatly contribute to reduce the risk of spinal biomechanical instability and the need for a posterior fusion. To our knowledge, 17 cases of endoscopic endonasal odontoidectomy for different diseases have been reported up to now and in all patients posterior fixation was performed, even in the only four cases with the anterior C1 arch preservation [11, 12, 18–24]. In our opinion and according to the literature, anterior C1 arch preservation is an important issue for craniocervical stability as it could avoid the phenomenon of cranial settling and the need for a posterior surgical procedure, with its related risk of subaxial subluxation development [6–8]. Otherwise, in the transoral approach, the anterior ring of C1 and the base of the odontoid process are almost always completely resected as well as in the transcervical approach, where C1 ring removal is essential to gain access to the lower clivus [3]. Despite literature reports describe the risk of instability secondary to disruption of craniocervical junction ligamentous attachments beside bony preservation, our cases did not present such complication [7]. It might possibly be due to the reciprocal important stabilizing role of C1, with the attachment of residual membranes and ligaments, and the muscle, as described in the report by Panjabi [25]. Transoral, transnasal, and transcervical approaches have different trajectories, working angles and extents of exposure; therefore, several considerations should be taken into account to tailor the most appropriate surgical strategy. The pure endoscopic endonasal approach represents, in our opinion, a significant advancement in the management of irreducible compressive lesion of the anterior craniocervical junction. Based on our preliminary experience, we believe that this technique may offer a good working area from the clivus to the odontoid process and an adequate decompression that is at least as effective as that obtained with the other approaches but with potentially lower morbidity, lesser patient discomfort, and shorter ICU and hospital stay. This can be ascribed to an earlier extubation, prompt oral feeding and lesser risk of bacterial wound contamination, because the mucosal defect created by a transnasal approach is linear, smaller and above the level of the soft palate [11]. Furthermore, by this approach, we were able to spare the hard and soft palate and to remove only a small portion of the posterior nasal septum preserving most of the nasal mucosa, thus leaving unaffected physiological mechanisms of breathing and phonation. Finally, the use of endoscopes has some advantages in itself, including the close-up vision and a large field of view, benefits enhanced by the use of dedicated angled lenses. However, it should be noted that there are some limitations in this approach. Regardless the learning curve, the lesion must be located almost in the midline and above the “nasopalatine line” and, occasionally, a partial posterior drilling of the hard palate is needed to gain a more caudal access.
Conclusions
The transnasal fully endoscopic technique, due to its reduced invasiveness, may represent an interesting alternative to transoral approach for resection of odontoid process in patients with bulbo-medullary compression caused by rheumatoid arthritis, basilar invagination, or other lesions. This statement is particularly true for elderly patients, with various associated comorbidities related to the age itself and to the other diseases. As usually, long-term clinical studies will be needed to better elucidate indications, clinical advantages, and disadvantages of this technique.
Acknowledgments
Conflict of interest
None.
Contributor Information
Maurizio Gladi, Email: mauriziogladi@gmail.com.
Maurizio Iacoangeli, Phone: +39-715964567, FAX: +39-715964575, Email: neurotra@tiscali.it.
Lorenzo Alvaro, Email: alvaneuro81@alice.it.
References
- 1.Crockard HA. The transoral approach to the base of the brain and upper cervical cord. Ann R Coll Surg Engl. 1985;67:321–325. [PMC free article] [PubMed] [Google Scholar]
- 2.Blazier CJ, Hadley MN, Spetzler RF. The transoral surgical approach to craniovertebral pathology. J Neurosci Nurs. 1986;18:57–62. doi: 10.1097/01376517-198604000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Baird CJ, Conway JE, Sciubba DM, Prevedello DM, Quiñones-Hinojosa A, Kassam AB. Radiographic and anatomic basis of endoscopic anterior craniocervical decompression: a comparison of endonasal, transoral, and transcervical approaches. Neurosurgery. 2009;65(6 Suppl):158–163. doi: 10.1227/01.NEU.0000345641.97181.ED. [DOI] [PubMed] [Google Scholar]
- 4.Alfieri A, Jho HD, Tschabitscher M. Endoscopic endonasal approach to the ventral cranio-cervical junction: anatomical study. Acta Neurochir (Wien) 2002;144:219–225. doi: 10.1007/s007010200029. [DOI] [PubMed] [Google Scholar]
- 5.Cavallo LM, Messina A, Cappabianca P, Esposito F, Divitiis E, Gardner P, Tschabitscher M. Endoscopic endonasal surgery of the midline skull base: anatomical study and clinical considerations. Neurosurg Focus. 2005;19:E2. [PubMed] [Google Scholar]
- 6.Naderi S, Crawford NR, Melton MS, Sonntag VK, Dickman CA. Biomechanical analysis of cranial settling after transoral odontoidectomy. Neurosurg Focus. 1999;6(6):E7. doi: 10.3171/foc.1999.6.6.10. [DOI] [PubMed] [Google Scholar]
- 7.Steinmetz MP, Mroz TE, Benzel EC. Craniovertebral junction: biomechanical considerations. Neurosurgery. 2010;66(3 Suppl):7–12. doi: 10.1227/01.NEU.0000366109.85796.42. [DOI] [PubMed] [Google Scholar]
- 8.Ito H, Neo M, Sakamoto T, Fujibayashi S, Yoshitomi H, Nakamura T. Subaxial subluxation after atlantoaxial transarticular screw fixation in rheumatoid patients. Eur Spine J. 2009;18:869–876. doi: 10.1007/s00586-009-0945-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranawat CS, O’Leary P, Pellicci P, Tsairis P, Marchisello P, Dorr L. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am. 1979;61:1003–1010. [PubMed] [Google Scholar]
- 10.Revanappa KK, Rajshekhar V. Comparison of Nurick grading system and modified Japanese Orthopaedic Association scoring system in evaluation of patients with cervical spondylotic myelopathy. Eur Spine J. 2011;20:1545–1551. doi: 10.1007/s00586-011-1773-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kassam AB, Snyderman C, Gardner P, Carrau R, Spiro R. The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report. Neurosurgery. 2005;57(1 Suppl):E213. doi: 10.1227/01.NEU.0000163687.64774.E4. [DOI] [PubMed] [Google Scholar]
- 12.Wu JC, Huang WC, Cheng H, Liang ML, Ho CY, Wong TT, Shih YH, Yen YS (2008) Endoscopic transnasal transclival odontoidectomy: a new approach to decompression: technical case report. Neurosurgery 63(1 Suppl 1):ONSE92–ONSE94 [DOI] [PubMed]
- 13.Visocchi M, Doglietto F, Della Pepa GM, Esposito G, Rocca G, Rocco C, Maira G, Fernandez E. Endoscope-assisted microsurgical transoral approach to the anterior craniovertebral junction compressive pathologies. Eur Spine J. 2011;20:1518–1525. doi: 10.1007/s00586-011-1769-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grob D, Würsch R, Grauer W, Sturzenegger J, Dvorak J. Atlanto-axial fusion and retrodental pannus in rheumatoid arthritis. Spine (Philadelphia, PA, 1976) 1997;22:1580–1583. doi: 10.1097/00007632-199707150-00010. [DOI] [PubMed] [Google Scholar]
- 15.Zygmunt S, Säveland H, Brattström H, Ljunggren B, Larsson EM, Wollheim F. Reduction of rheumatoid periodontoid pannus following posterior occipito-cervical fusion visualised by magnetic resonance imaging. Br J Neurosurg. 1988;2:315–320. doi: 10.3109/02688698809001001. [DOI] [PubMed] [Google Scholar]
- 16.Mummaneni PV, Haid RW. Transoral odontoidectomy. Neurosurgery. 2005;56:1045–1050. doi: 10.1227/01.NEU.0000157103.15608.82. [DOI] [PubMed] [Google Scholar]
- 17.Wolinsky JP, Sciubba DM, Suk I, Gokaslan ZL. Endoscopic image-guided odontoidectomy for decompression of basilar invagination via a standard anterior cervical approach. Technical note. J Neurosurg Spine. 2007;6:184–191. doi: 10.3171/spi.2007.6.2.184. [DOI] [PubMed] [Google Scholar]
- 18.Hankinson TC, Grunstein E, Gardner P, Spinks TJ, Anderson RC. Transnasal odontoid resection followed by posterior decompression and occipitocervical fusion in children with Chiari malformation Type I and ventral brainstem compression. J Neurosurg Pediatr. 2010;5:549–553. doi: 10.3171/2010.2.PEDS09362. [DOI] [PubMed] [Google Scholar]
- 19.Gempt J, Lehmberg J, Meyer B, Stoffel M. Endoscopic transnasal resection of the odontoid in a patient with severe brainstem compression. Acta Neurochir (Wien) 2010;152:559–560. doi: 10.1007/s00701-009-0481-4. [DOI] [PubMed] [Google Scholar]
- 20.Gempt J, Lehmberg J, Grams AE, Berends L, Meyer B, Stoffel M. Endoscopic transnasal resection of the odontoid: case series and clinical course. Eur Spine J. 2011;20:661–666. doi: 10.1007/s00586-010-1629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leng LZ, Anand VK, Hartl R, Schwartz TH. Endonasal endoscopic resection of an os odontoideum to decompress the cervicomedullary junction: a minimal access surgical technique. Spine (Philadelphia, PA, 1976) 2009;34:E139–E143. doi: 10.1097/BRS.0b013e31818e344d. [DOI] [PubMed] [Google Scholar]
- 22.Cornelius JF, Kania R, Bostelmann R, Herman P, George B. Transnasal endoscopic odontoidectomy after occipito-cervical fusion during the same operative setting—technical note. Neurosurg Rev. 2011;34:115–121. doi: 10.1007/s10143-010-0295-0. [DOI] [PubMed] [Google Scholar]
- 23.Lee A, Sommer D, Reddy K, Murty N, Gunnarsson T. Endoscopic transnasal approach to the craniocervical junction. Skull Base. 2010;20:199–205. doi: 10.1055/s-0029-1246220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Magrini S, Pasquini E, Mazzatenta D, Mascari C, Galassi E, Frank G. Endoscopic endonasal odontoidectomy in a patient affected by Down syndrome: technical case report. Neurosurgery. 2008;63:E373–E374. doi: 10.1227/01.NEU.0000315285.84524.74. [DOI] [PubMed] [Google Scholar]
- 25.Panjabi MM. The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord. 1992;5:383–389. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]