Abstract
Introduction
Cervical degenerative pathology can produce pain and disability and, in case of failure of conservative treatment surgery is indicated.
Materials and methods
107 patients affected by single level cervical degenerative pathology were surgically treated by Cloward procedure. On radiographs, the sagittal segmental alignment (SSA) of the affected level and sagittal alignment of the cervical spine were measured.
Results
Preoperatively, mean SSA was 0.6° and at the last follow-up 1.8°. In particular, adjacent-level degeneration occurred more frequently in Group A than in Group B.
Conclusion
Lordotic SSA angle can be considered a protective factor against adjacent-level degeneration.
Keywords: Cervical spondylosis, Cervical disc herniation, Single level, Cloward procedure, Cervical anterior approach, Long-term follow-up
Introduction
Cervical disc herniation and spondylosis can present in patients over 50 years with pain, cervical radiculopathy, or cervical myelopathy and lead to disability [1, 2]. In case of failure of conservative treatment with intractable pain, worsening of radiculopathy, and myelopathy surgery is indicated [3, 4]. Cervical fusion by anterior approach was first described by Robinson and Smith [5] and by Cloward [6, 7]. These techniques have been widely used by many authors, with satisfactory short-term results [8–10]. The aim of this study was to report the clinical and radiological results of 107 patients operated by discectomy and one-level anterior cervical fusion according to the Cloward procedure, with a minimum 10-year follow-up.
Materials and methods
107 patients (14 females and 93 males) aged between 35 and 55 years (mean 46 ± 7 years) affected by single level disease between C4 and C7 (C4–C5 in 46 patients, C5–C6 in 33 patients, and C6–C7 in 28 patients) with intractable pain, worsening of radiculopathy, and myelopathy were operated by discectomy and one-level anterior cervical fusion according to the Cloward procedure between 1980 and 1995.
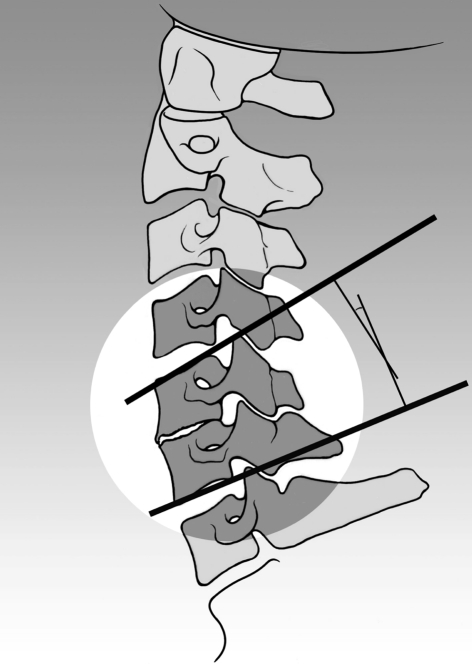
All patients were radiographically evaluated by standard cervical spine X-rays; on lateral images, the sagittal segmental alignment (SSA) of the affected intervertebral disc space was measured. The SSA (Fig. 1) was defined as the angle between the line parallel to the upper vertebral end-plate of the proximal vertebra to the involved disc space and the line parallel to the lower vertebral end-plate of the underlying vertebra with a positive value in case of lordosis and a negative value in case of kyphosis. By use of this definition, we considered the patients as two groups: A with kyphosis (SSA ≤ 0) and B with lordosis (SSA > 0).
Fig. 1.
The SSA angle measurement: a line parallel to the upper vertebral end-plate of the proximal vertebra to the involved disc space and a line parallel to the lower vertebral end-plate of the underlying vertebra were drown. The SSA angle is the angle formed by these two lines
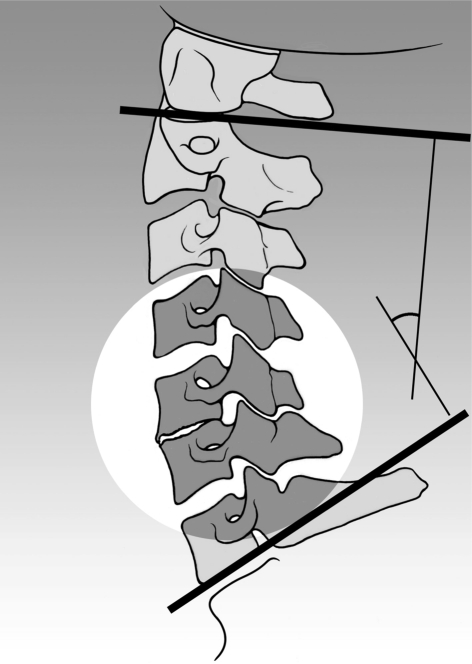
Sagittal alignment of the cervical spine (SACS) angle (Fig. 2) was calculated according to a graphic equivalent of the method by Katsuura et al. and measured as the angle between the line parallel to the upper border of the C2 vertebral body and the line parallel to the lower border of the C7 vertebral body. SACS describes the alignment of the whole cervical segment, and this value is positive in the case of lordotic alignment.
Fig. 2.
The SACS angle measurement: a line parallel to the upper border of the C2 vertebral body and the line parallel to the lower border of the C7 vertebral body
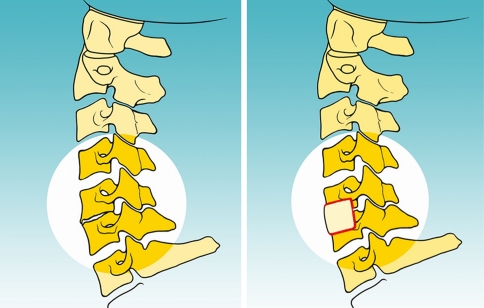
Before the spinal procedure, a bicortical iliac autograft was harvested from the anterior iliac crest [11]. An anterior, oblique, skin incision was performed; the trachea and the esophagus were retracted medially, whereas the neurovascular bundle with the sternocleidomastoid muscle was retracted laterally. After fluoroscopic confirmation of the affected level, a complete discectomy was performed; then, the bone graft was drilled into the intervertebral space (Fig. 3a, b) [6, 7, 12–15, 17]. After surgery, standard radiographs of the cervical spine were performed. Postoperative immobilization consisted of a neck collar for 40 days [10, 16]. At follow-up, patients were rated from excellent to poor depending on resolution, improvement, or persistence of preoperative symptoms according to Odom et al. [2]. Height of intervertebral segment was also measured on lateral radiographic.
Fig. 3.
a Image representing the preoperative radiographic aspect of spondylosis involving C5–C6 level with kyphotic alignment of the cervical spine. b Image representing the postoperative radiograph aspect after Cloward procedure showing the restoration of the physiologic lordosis
Results
No complications were encountered in this series. 1 month after surgery, no patients presented radiographical sign of fusion; 80 % of patients (86) presented evident signs of fusion at 3 months, 97 % (104) at 6 months, and 100 % (107) at 12 months.
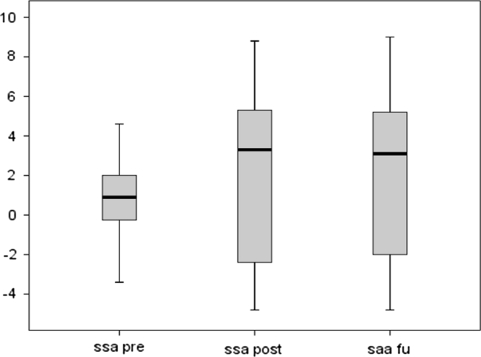
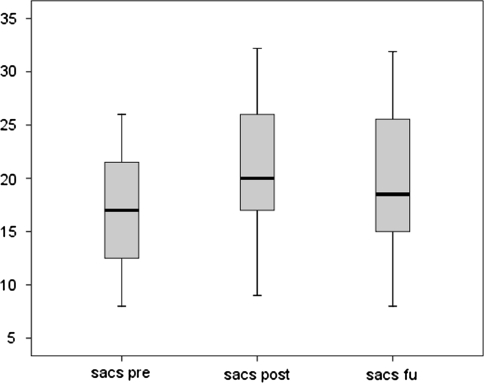
Preoperatively, mean SSA was 0.6° ± 2.0°; at the last follow-up, the mean SSA was 1.8° ± 4.1° (Figs. 4, 5). Preoperatively, average SACS was 16.5° ± 4.0°; at the last follow-up, average SACS was 19.7° ± 6.6° (Fig. 5; Table 1).
Fig. 4.
Preoperative SSA, postoperative SSA, and SSA at the last follow-up: mean, maximal and minimal value, and standard deviation value
Fig. 5.
Preoperative SACS, postoperative SACS, and SACS at the last follow-up: mean, maximal and minimal value, and standard deviation value
Table 1.
Preoperative SSA and SACS and the value at the last follow-up (average and standard deviation): comparison between the groups A (alignment of the affected cervical level in kyphosis, SSA ≤ 0) and B (alignment of the affected cervical level in lordosis, SSA > 0)
| Preoperative | Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| SSA | SACS | SSA | SACS | |||||
| A | B | A | B | A | B | A | B | |
| Average | −3.0 | 5.0 | 15.9 | 24.3 | −2.8 | 4.8 | 14.0 | 23.5 |
| SD | 1.2 | 1.9 | 3.8 | 5.1 | 1.2 | 2.3 | 6.0 | 7.0 |
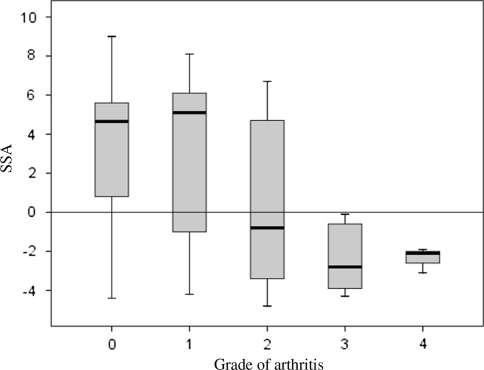
At the last follow-up, adjacent-level degeneration was present in 40 % of patients in the whole series. In particular, adjacent-level degeneration occurred more frequently in Group A than in Group B: 61 versus 27 %, respectively. No patients presented a poor outcome at long-term follow-up (Fig. 6).
Fig. 6.
Grade of adjacent level degeneration in patients treated by Cloward procedure—the line shows that the value of SSA is 0: patients under the line have a negative SSA that represents the alignment in kyphosis of the level (Group A); patients on top of this line have a positive SSA that represents the alignment in lordosis of the level (Group B). Grade 1 was considered as physiological arthritis
Discussion
When conservative treatment for cervical disc herniation and spondylosis fails, surgical treatment is indicated, and anterior decompression and fusion is considered as the treatment of choice [11, 12, 15]. The Cloward procedure proved to be a suitable and effective technique for the treatment of segmental cervical degenerative pathology. We found that a lordotic SSA angle can be considered a protective factor against adjacent-level degeneration. In particular, it is concluded that for each positive degree of SSA angle, there is a reduced risk of adjacent-level degeneration. Instead, at the presence of cervical kyphosis, there is a greater risk of adjacent-level degeneration formation. The SACS angle cannot be considered as a good predictor of adjacent-level degeneration formation. In this study, a reduction in grade of lordosis and height of fused segments were seen because of subside of the bone graft.
Acknowledgments
We thank Professor Pier Giorgio Marchetti and Professor Alessandro Faldini, the treating surgeons who performed the procedure in the reported patients.
Conflict of interest
None.
References
- 1.Macnab I. Cervical spondylosis. Clin Orthop Relat Res. 1975;109:69–77. doi: 10.1097/00003086-197506000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Odom GL, Finney W, Woodhall B. Cervical disc lesions. J Am Med Assoc. 1958;166:23–28. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 3.Bailey RW, Badgley CE. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am. 1960;42:565–594. [PubMed] [Google Scholar]
- 4.Lunsford DL, Bissonette DJ, Janetta PJ, Sheptak PE, Zorub DS. Anterior surgery for cervical disc disease. J Neurosurg. 1980;53:1–11. doi: 10.3171/jns.1980.53.1.0001. [DOI] [PubMed] [Google Scholar]
- 5.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Cloward RB. The anterior surgical approach to the cervical spine: the Cloward procedure: past, present and future. Spine. 1998;13:823–827. doi: 10.1097/00007632-198807000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 8.Lofgren H, Johannsson V, Olsson T, Ryd L, Levander B. Rigid fusion after Cloward operation for cervical disc disease using autograft, allograft or xenograft: a randomized study with radiostereometric and clinical follow-up assessment. Spine. 2000;25:1908–1916. doi: 10.1097/00007632-200008010-00008. [DOI] [PubMed] [Google Scholar]
- 9.Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A. A prospective randomized comparison between the Cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine. 2002;27:1694–1701. doi: 10.1097/00007632-200208150-00003. [DOI] [PubMed] [Google Scholar]
- 10.Faldini C, Pagkrati S, Leonetti D, Miscione MT, Giannini S. Sagittal segmental alignment as predictor of adjacent-level degeneration after a Cloward procedure. Clin Orthop Relat Res. 2011;469(3):674–681. doi: 10.1007/s11999-010-1614-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martins AN, Colonel MC. Anterior cervical discectomy with and without interbody bone graft. J Neurosurg. 1044;44:290–295. doi: 10.3171/jns.1976.44.3.0290. [DOI] [PubMed] [Google Scholar]
- 12.Clements DH, O’Leary PF. Anterior cervical discectomy and fusion. Spine. 1990;15:1023–1025. doi: 10.1097/00007632-199015100-00008. [DOI] [PubMed] [Google Scholar]
- 13.Herkowitz HN, Kurz LT, Overholt DP. Surgical management of cervical soft disc herniation. Spine. 1990;15:1027–1031. doi: 10.1097/00007632-199015100-00009. [DOI] [PubMed] [Google Scholar]
- 14.Bartolozzi P, Salvi M. Anterior surgery of the lower cervical spine. Chir Organi Mov. 1992;77:81–85. [PubMed] [Google Scholar]
- 15.Palit M, Schofferman J, Goldthwaite N, Reynolds J, Kerner M, Keaney D, Lawrence-Miyasaki L. Anterior discectomy and fusion for the management of neck pain. Spine. 1999;24:2224–2228. doi: 10.1097/00007632-199911010-00009. [DOI] [PubMed] [Google Scholar]
- 16.Faldini C, Leonetti D, Nanni M, Martino A, Denaro L, Denaro V, Giannini S. Cervical disc herniation and cervical spondylosis surgically treated by Cloward procedure: 10-year-minimum follow-up study. J Orthop Traumatol. 2010;11(2):99–103. doi: 10.1007/s10195-010-0093-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Denaro V, Papalia R, Denaro L, Martino A, Maffulli N. Cervical spinal disc replacement. J Bone Joint Surg. 2009;91:713–719. doi: 10.1302/0301-620X.91B6.22025. [DOI] [PubMed] [Google Scholar]